Abstract
Purpose:
Multiple treatments for dorsal wrist ganglia (DWG) exist but have high recurrence rates. We investigated whether aspiration followed by injection of Tisseel is more effective at reducing the DWG recurrence rate than aspiration alone.
Methods:
Adults with untreated DWG were randomly assigned to aspiration alone (A) or aspiration followed by Tisseel injection (AT). Patients were measured at baseline, 1, 6, and 12 months. Primary outcome was the rate of recurrence. Secondary outcomes included recurrent ganglion size and maximum pain experienced from the ganglion. Continuous data were compared with Student t tests and Mann-Whitney U tests. Categorical data were compared with χ2 tests and Fisher exact tests. Treatment effect was reported as relative risk or mean differences (MD) with 95% confidence intervals.
Results:
Seventy-nine patients were randomized to the A (n = 39) or AT (n = 40) group. Twenty-five patients were lost to follow-up. There were no differences in recurrence risk between groups at 1, 6, or 12 months (P > .05). Ganglia were significantly smaller for both groups at 1 month versus baseline (P < .001). The A group demonstrated a significantly larger decrease in size at 1 month versus the AT group (MD = 0.75 cm2, 95% confidence interval: 0.07-1.43, P = .03). Both groups experienced significantly less pain at 1, 6, and 12 months (P < .03), but this was not significantly different between groups.
Conclusion:
Aspiration and Tisseel injection does not decrease DWG recurrence versus aspiration alone. Both interventions produced a significant decrease in pain. Although aspiration alone carries a high recurrence risk, it may provide sufficient symptomatic relief for patients with DWG.
Keywords: aspiration, fibrin tissue adhesive, ganglion, pain, recurrence, treatment, wrist
Abstract
Objectif :
Malgré les nombreux traitements des ganglions de la face dorsale du poignet (GFDP), les taux de récurrence sont élevés. Les auteurs ont évalué si la ponction suivie d’une injection de Tisseel réduisait le taux de récurrence de GFDP avec plus d’efficacité que la ponction seule.
Méthodologie :
Les adultes présentant un GFDP non traité ont été répartis au hasard entre la ponction seule (P) et la ponction suivie par une injection de Tisseel (PT). Les chercheurs les ont mesurés au départ, puis au bout de un, six et 12 mois. Le taux de récurrence représentait le résultat clinique primaire, et la taille des ganglions récurrents et la douleur maximale provoquée par le ganglion, les résultats cliniques secondaires. Les chercheurs ont comparé les données continues avec les tests de Student et les tests Mann-Whitney et les données catégorielles avec les tests du chi carré et les tests exacts de Fisher. Ils ont déclaré l’effet du traitement sous forme de risque relatif (RR) ou de différences moyennes (DM), selon des intervalles de confiance à 95 %.
Résultats :
Au total, les chercheurs ont réparti 79 patients au hasard entre le groupe P (n = 39) ou PT (n = 40). Ils ont perdu 25 patients au suivi. Ils n’ont constaté aucune différence quant au risque de récurrence entre les groupes au bout de un, six ou 12 mois (P > .05). Les ganglions étaient beaucoup plus petits dans les deux groupes au bout d’un mois qu’au départ (P < .001). La taille du ganglion avait diminué davantage dans le groupe P que dans le groupe PT au bout d’un mois (DM = 0.75 cm2, IC à 95 %: 0,07 à 1,43, P = .03). Les deux groupes ressentaient beaucoup moins de douleur au bout de un, six et 12 mois (P < .03), mais cette différence n’était pas significative entre les groupes.
Conclusions :
La ponction et l’injection de Tisseel ne réduisent pas la récurrence de GFDP par rapport à la ponction seule. Les deux interventions entraînaient une diminution significative de la douleur. Même si la ponction seule s’associe à un fort risque de récurrence, elle peut apporter un soulagement symptomatique suffisant pour les patients ayant un GFDP.
Introduction
Ganglia are the most common benign tumours of the hand. Ganglia consist of extra-articular accumulations of thick gelatinous and synovial-like fluid surrounded by a pseudocapsule of compressed collagen, but without a true epithelial or synovial lining. The majority (61%) of ganglia occur on the dorsal wrist and tend to arise from the scapholunate joint.1 Ganglia usually arise spontaneously, but approximately 10% of patients may present with an antecedent history of trauma.2 No association has been found between ganglia development and occupations involving repetitive work.1 Although arthrographic injections of the wrist have proven a communication between the joint space and ganglion, cystography has not consistently demonstrated a communication between the ganglion cavity and the joint space.3 These collective findings have led to the theory of 1-way flow from the joint to the ganglion with a 1-way valve mechanism.
The most common clinical presentation of a ganglion is a firm, painless mass. However, some patients may experience severe pain from a ganglion. This may be due to the close proximity of the posterior interosseous nerve or due to a pressure phenomenon. Patients tend to present to their general practitioner due to concerns of the mass, such as pain, complaints of the aesthetic appearance, or worries that it may represent a malignant lesion.
Due to the common nature of ganglia, many treatment methods have been developed and applied.4 However, many of these methods have variable success rates and high recurrence rates.4 Nonoperative interventions include aspiration alone,5-10 aspiration and corticosteroid injection,7,10-16 aspiration and ethanol injection,7 aspiration and hyaluronidase injection,12,17 aspiration and sclerosing agent injection,12,18,19 aspiration and multiple punctures,9 and aspiration and electrocautery.20 Operative interventions include both open and arthroscopic approaches, and these have been shown to have comparable recurrence rates 1 year postoperatively.21 Although operative management has decreased recurrence rates in comparison to aspiration alone,4 nonoperative management may be preferred by patients due to its less invasive nature and faster return to work post-procedure.
Tisseel (Baxter Canada) is a fibrin adhesive system containing 2 components pooled from multidonor plasma. One component consists of highly concentrated human fibrinogen solution combined with factor XIII, fibronectin, and aprotinin, which inhibits thrombolysis. The second component consists of human thrombin and calcium chloride. When the 2 components are mixed, thrombin converts fibrinogen into insoluble fibrin, which is the final stable form of the sealant that is ultimately used.
Tisseel is currently used as an adjunct to hemostasis in adult and pediatric surgical patients as well as an adjunct to seal and prevent leakages from colonic anastomoses. However, Tisseel has also been applied for off-label use in multiple surgical specialties. With regard to plastic surgery, Tisseel has been used as an adjunct in nerve repairs,22 promoting split thickness skin graft adherence and reducing donor site pain,23,24 minimizing edema and hematoma formation following facelifts,25 and seroma prevention.26 The safety of intra-articular injection of Tisseel has also been demonstrated via sealing Baker cysts.27
To date, the current treatment strategies for dorsal wrist ganglia (DWG) have high recurrence rates. There has been no documented literature investigating Tisseel as a possible treatment strategy for DWG. We hypothesize that following the aspiration of the contents of DWG, the injection of Tisseel will act to seal the 1-way valve communication between the ganglion cavity and joint space. As a result, we hypothesize that compared to aspiration alone, aspiration followed by injection of Tisseel is more effective at (1) reducing the recurrence rate of DWG, (2) reducing maximal pain experienced, and (3) reducing the size of the DWG, if it recurs. To test our hypotheses, we performed a randomized controlled trial comparing the current standard DWG treatment of aspiration alone with aspiration followed by Tisseel injection.
Methods
Study Population
From October 2002 to June 2015, 79 adult patients referred to the primary investigator’s (senior author) outpatient plastic surgery clinic with a confirmed diagnosis of a DWG that was symptomatic (ie, produced associated pain at rest or with activity) were enrolled in this study. Patients were excluded if they were less than 18 years of age, were completely asymptomatic from the ganglion, had received prior treatment for the ganglion, had a ganglion less than 1.5 cm in diameter, opted for surgical management, or declined participation in the study. The Hamilton Integrated Research Ethics Board (HIREB #01-2016) approved this study. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all individual participants included in this study.
Randomization
Patients were randomly assigned to receive aspiration alone (A) or aspiration and Tisseel injection (AT) via sealed envelopes using random blocked sizes of computer generated randomization sequence by independent research personnel.
Treatment Techniques
All treatments were completed by the primary investigator. Under aseptic technique, both groups received local filtration of local anesthetic followed by aspiration of the DWG with an 18-gauge needle. Following aspiration, the AT group received a Tisseel injection (0.2 mL; mixed according to the manufacturer protocol) into the cavity of the DWG. Specifically, once the aspiration had been completed, the 18-gauge needle was left in situ within the DWG cavity. The syringe with the aspirate was then immediately exchanged for a syringe containing the Tisseel, and the Tisseel was subsequently injected. Baxter Canada provided the Tisseel product free of charge for the purpose of the study and had no role in data collection, statistical analysis, or manuscript writing. A dry dressing was applied over the treatment site for both groups.
Patients were measured at baseline, 1, 6, and 12 months posttreatment. At each of these visits, the presence or absence of the DWG was noted, the size of the DWG was measured (if applicable), and patients rated their maximal pain experienced due to the DWG using the Numerical Rating Scale (0-10).
Sample Size Calculation
Based upon the literature, at least a 50% recurrence rate at 12 months can be expected following aspiration alone.4 A survey of 9 local plastic surgeons revealed that a 30% recurrence rate at 12 months (ie, a 20% reduction in recurrence rate) in the AT group would be a clinically relevant result that would change practice patterns. Therefore, based on an α value of .05 and a β value of .2, a total of 76 patients (38 per treatment group) would be required for adequate power.
Statistical Analyses
Patient demographics and outcome variables at baseline were compared between treatment groups to ensure comparability of the groups. Continuous variables were described using means and standard deviations or medians with minimums and maximums, whereas percentages were used to describe categorical variables. Continuous data were compared with the Student t test and Mann-Whitney U test, while categorical data were compared with the χ2 test and Fisher exact test. Relative risks (RRs) with 95% confidence intervals (CI) were calculated to compare recurrence rates, whereas mean differences (MD) with 95% CI were calculated to compare pain scores adjusted for baseline values.
Results
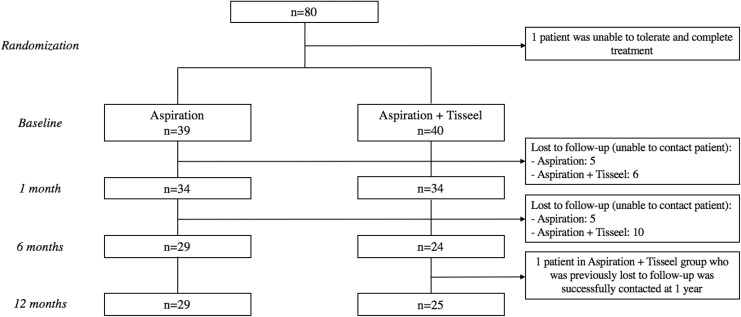
Seventy-nine patients were randomized to the A (n = 39) or AT (n = 40) group and completed treatment (Figure 1). Eleven patients (A = 5 and AT = 6) were lost to follow-up at 1 month, 26 patients (A = 10 and AT = 16) were lost to follow-up at 6 months, and 25 patients (A = 10 and AT = 15) were lost to follow-up at 12 months (Figure 1).
Figure 1.
Flow diagram of the study protocol.
There were no significant differences between groups at baseline (Table 1). Both groups were primarily women, right-handed, nonsmokers, and performed office-related jobs. Both groups had an initial mean ganglion size of 4.0 cm2, where the ganglion had been present for an average of 17 to 21 months prior to the initial visit.
Table 1.
Baseline Characteristics of the Aspiration With Tisseel and Aspiration Alone Groups.
| Aspiration + Tisseel (n = 40) | Aspiration (n = 39) | P Value | |
|---|---|---|---|
| Mean age (SD) | 37.1 (14.0) | 32.2 (12.2) | .1 |
| Sex, n (%) | .5 | ||
| Men | 18 (45.0%) | 14 (35.9%) | |
| Women | 22 (55.0%) | 25 (64.1%) | |
| Hand dominance, n (%) | .4 | ||
| Right | 39 (97.5%) | 36 (92.3%) | |
| Left | 1 (2.5%) | 3 (7.7%) | |
| Active smoking status, n (%) | 9 (22.5%) | 10 (25.6%) | .8 |
| Medical comorbidities, n (%) | 14 (35.0%) | 8 (20.5%) | .2 |
| Occupation, n (%) | .4 | ||
| Manual jobs | 7 (17.5%) | 10 (25.6%) | |
| Office/desk work | 26 (65.0%) | 25 (64.1%) | |
| Retired | 5 (12.5%) | 1 (2.6%) | |
| Other | 2 (5.0%) | 3 (7.7%) | |
| Ganglion side, n (%) | .7 | ||
| Right | 18 (45.0%) | 20 (51.3%) | |
| Left | 22 (55.0%) | 19 (48.7%) | |
| Mean ganglion duration, month (SD) | 17.3 (18.7) | 21.3 (22.6) | .4 |
| History of wrist trauma, n (%) | 3 (7.5%) | 5 (12.8%) | .5 |
| Median maximum amount of pain experienced (minimum–maximum) | 2.5 (0-8) | 3 (0-9) | .5 |
| Mean ganglion size, cm (SD) | 4.0 (1.6) | 4.0 (1.9) | 1.0 |
| Mean amount of ganglion aspirated, mL (SD) | 1.1 (1.0) | 0.9 (0.8) | .3 |
Abbreviation: SD, standard deviation.
There were no differences in recurrence rate between groups at 1 month (A = 79.4%, AT = 85.3%; RR = 1.04, 95% CI: 0.84-1.30), 6 months (A = 75.9%, AT = 62.5%; RR = 0.68, 95% CI: 0.43-1.10), or 12 months (A = 72.4%, AT = 64.0%; RR = 0.76, 95% CI: 0.50-1.19; Table 2).
Table 2.
Ganglion Recurrence Rates and Relative Risk Ratios Between the Aspiration With Tisseel and Aspiration Alone Groups at 1, 6, and 12 Months as Well as Total Number of Recurrences Between Groups.
| Aspiration + Tisseel | Aspiration | Relative Risk Ratio (95% CI) | P Value | |
|---|---|---|---|---|
| 1-month recurrence, n (%) | n = 34 | n = 34 | 1.04 | .752 |
| 29 (85.3%) | 27 (79.4%) | (0.84-1.30) | ||
| 6-month recurrence, n (%) | n = 24 | n = 29 | 0.68 | .372 |
| 15 (62.5%) | 22 (75.9%) | (0.43-1.10) | ||
| 12-month recurrence, n (%) | n = 25 | n = 29 | 0.76 | .566 |
| 16 (64.0%) | 21 (72.4%) | (0.50-1.19) | ||
| Total number of recurrences | .352 | |||
| Median (minimum–maximum) | 2.0 (0-3) | 2.0 (0-3) | ||
| 0 recurrence, n (%) | 5 (14.3%) | 3 (8.3%) | ||
| 1 recurrence, n (%) | 10 (28.6%) | 10 (27.8%) | ||
| 2 recurrences, n (%) | 10 (28.6%) | 9 (25.0%) | ||
| 3 recurrences, n (%) | 10 (28.6%) | 14 (39.0%) |
Abbreviation: CI, confidence interval.
Both groups had a significant decrease in ganglia size at 1 month compared to baseline (P < .001; Table 3). The A group demonstrated a significantly larger decrease in size at 1 month versus the AT group (MD = 0.75 cm2, 95% CI: 0.07-1.43, P = .03; Table 3). Both groups experienced a significant reduction in maximum pain at 1, 6, and 12 months (P < .03), but this was not significantly different between groups (Table 4).
Table 3.
Mean Ganglion Size at Baseline, 1, 6, and 12 Months for Both Groups as Well as Mean Difference in Ganglion Size Between Follow-Up Visits Within and Between Groups.
| Aspiration + Tisseel | Aspiration | Mean Difference Between Groups (95% CI) | P Value | |
|---|---|---|---|---|
| Mean baseline ganglion size, cm2 (SD) | n = 40 | n = 39 | .974 | |
| 4.0 (1.6) | 4.0 (1.9) | |||
| Mean ganglion size at 1 month cm2 (SD) | n = 29 | n = 27 | 0.75 (0.07-1.43) |
.029 |
| 2.8 (1.5) | 2.1 (0.9) | |||
| Mean difference in ganglion size at 1 month within groups, cm2 (95% CI) | −1.2 (−1.6 to −0.8) | −1.8 (−2.4 to −1.2) | ||
| P < .001 | P < .001 | |||
| Mean ganglion size at 6 months cm2 (SD) | n = 15 | n = 22 | 0.46 (−1.02 to 1.95) |
.529 |
| 3.7 (2.3) | 3.2 (2.1) | |||
| Mean difference in ganglion size at 6 months within groups, cm2 (95% CI) | −0.6 (−1.6 to 0.4) | −0.6 (−1.6 to 0.3) | ||
| P = .209 | P = .206 | |||
| Mean size (cm [SD]) at 1 year | n = 14 | n = 21 | 0.83 (−0.59 to 2.26) |
.3 |
| 3.6 (2.5) | 2.8 (1.7) | |||
| Mean difference in ganglion size at 12 months within groups (cm2 [95% CI]) | −0.4 (−1.8 to 0.9) | −1.65 (−2.9 to −0.3) | ||
| P = .471 | P = .016 |
Abbreviations: CI, confidence interval; SD, standard deviation.
Table 4.
Maximum Pain Experienced Due to the Ganglion by Both Groups at Baseline, 1, 6, and 12 Months and Mean Difference of Pain Experienced Between Follow-Up Visits Within and Between Groups.
| Aspiration + Tisseel | Aspiration | Mean Difference Between Groups (95% CI) | P Value | |
|---|---|---|---|---|
| Mean maximum pain experienced at baseline (SD) | n = 40 | n = 39 | .5 | |
| 2.9 (2.7) | 3.3 (2.7) | |||
| Mean maximum pain experienced at 1 month (SD) | n = 34 | n = 34 | −0.94 (−2.10 to 0.21) |
.2 |
| 1.1 (2.0) | 2.1 (0.9) | |||
| Mean difference in pain experienced at 1 month within groups (95% CI) | −2.0 (−1.6 to −0.8) | −1.2 (−2.3 to −0.1) | ||
| P < .001 | P = .039 | |||
| Mean maximum pain experienced at 6 months (SD) | n = 24 | n = 29 | −0.63 (−2.24 to 0.98) |
.4 |
| 1.5 (2.7) | 2.1 (3.8) | |||
| Mean difference in pain experienced at 6 months within groups (95% CI) | −1.2 (−1.6 to −0.8) | −1.0 (−1.7 to −0.3) | ||
| P < .001 | P = .006 | |||
| Mean maximum pain experienced at 12 months (SD) | n = 22 | n = 29 | −0.34 (−1.76 to 1.10) |
.5 |
| 1.4 (2.4) | 2.7 (1.6) | |||
| Mean difference in pain experienced at 12 months within groups (95% CI) | −1.2 (−1.6 to −0.8) | −1.1 (−2.1 to −0.2) | ||
| P <.001 | P = .022 |
Abbreviations: CI, confidence interval; SD, standard deviation.
Discussion
Overall, there were no differences in recurrence rates of DWG at 1, 6, or 12 months regardless of whether patients received aspiration alone or aspiration followed by an injection of Tisseel. Both groups experienced a significant decrease in ganglia size at 1 month compared to baseline, but the A group demonstrated a significantly larger decrease in size compared to the AT group. Finally, regardless of the treatment received, all patients experienced a significant reduction in maximum pain experienced at 1, 6, and 12 months compared to baseline.
Despite treatment, 72% of DWG treated with aspiration alone and 64% of DWG treated with aspiration and Tisseel recurred by 12 months. Based upon a recent meta-analysis incorporating the current literature regarding both volar and DWG,4 the mean recurrence rate following aspiration of wrist ganglia is 59%. Therefore, our recurrence rate appears to be slightly higher than what the literature suggests. However, these slight differences may be due to our smaller sample size, different aspiration techniques, or our sole inclusion of DWG.
Previous studies have also assessed pain as a secondary measure when evaluating treatment strategies for wrist ganglia and have generally shown an improvement in pain following treatment.5,6,15,17 Pain may be considered a quality of life indicator for patients. Health-related quality-of-life indicators are increasingly recognized as important outcomes to measure when assessing clinical treatments in order to capture patients’ perspectives and burden of disease on patients’ functioning.28-30 It is important to recognize that although our 2 treatments for DWG were unable to definitively treat DWG in a large number of patients, all patients experienced a significant decrease in perceived pain at all time points. This reduction in patients’ pain may be translated into a perceived improvement in quality of life due to ameliorating bothersome symptoms and the ability to return to regular daily activities and work activities in a timely manner.
Although surgical excision of ganglia has a lower recurrence rate than aspiration techniques,4 surgical interventions carry a higher risk of complications. Damage to dorsal branches of the radial sensory nerve, scapholunate instability, hypertrophic or keloid scarring, as well as wrist pain and stiffness are potential complications of surgical treatment of DWG.5,6,31-33 Therefore, if we are able to improve patients’ quality of life without incurring the risks of a surgical intervention, less invasive treatments, such as aspiration, may be viable treatment options for patients seeking relief from their DWG.
Unfortunately, one of the major limitations to our study was the number of patients lost to follow-up, which led to small sample sizes at follow-up visits. Thus, the ultimate results of our study were underpowered. Upon a closer review, more patients were lost to follow-up from the AT group in comparison to the A group. Unfortunately, we are unable to determine whether the patients lost to follow-up were systematically different from those who remained in the trial. Therefore, our results should be interpreted with caution due to increased risk to the internal validity of the study. Furthermore, although we compared the AT group with the A group, we did not have a true negative control group where no active intervention was performed. The natural history of DWG suggests that 42% of DWG spontaneously resolve over the long term and up to 6 years.5 Given that no true negative control group was used, we are unable to definitely conclude whether the outcomes of the A and AT interventions are truly better compared to the outcomes achieved with no active intervention.
Despite these limitations, this is the first known study to evaluate the novel use of Tisseel for the treatment of DWG. We completed this study as a randomized controlled trial, while the majority of current studies investigating wrist ganglia treatment are cohort studies. We used objective measures and validated scales, such as the Numerical Rating Scale for pain, in order to investigate both our primary and secondary outcomes and reduce the risk of bias and confounding factors. Finally, our follow-up period was 12 months from the initial treatment. Although this lengthy follow-up period may have contributed to a greater number of patients lost to follow-up, we believe it allowed us to capture the majority of recurrences experienced by patients.
In the current Canadian health-care climate where finances are tight and resources are scarce, it is imperative to consider economically feasible treatment options for patients. Since DWG are one of the most common tumours of the hand, it is important to continue to evaluate our current as well as new potential treatment strategies for this condition. Future studies performing cost analyses of different ganglion treatments may be beneficial to discern which treatments are both effective for patients and sustainable within the current health economic climate.
Overall, Tisseel injection following aspiration does not decrease the risk of recurrence compared to aspiration alone. However, both interventions resulted in a significant decrease in pain that persisted at 12 months. Although aspiration alone carries a high recurrence risk, it may provide sufficient symptomatic relief for patients with DWG who wish to proceed with a less invasive treatment strategy rather than surgical management.
Footnotes
Level of Evidence: Level 1, Therapeutic
Authors’ Note: Baxter Canada provided the Tisseel product free of charge for the purpose of the study and had no role in data collection, statistical analysis, or the manuscript writing.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. McEvedy BV. The simple ganglion: a review of modes of treatment and an explanation of the frequent failures of surgery. Lancet. 1954;266(6803):135–136. [DOI] [PubMed] [Google Scholar]
- 2. Nelson CL, Sawmiller S, Phalen GS. Ganglions of the wrist and hand. J Bone Joint Surg Am. 1972;54(7):1459–1464. [PubMed] [Google Scholar]
- 3. Andrén L, Eiken O. Arthrographic studies of wrist ganglions. J Bone Joint Surg Am. 1971;53(2):299–302. [PubMed] [Google Scholar]
- 4. Head L, Gencarelli JR, Allen M, Boyd KU. Wrist ganglion treatment: systematic review and meta-analysis. J Hand Surg Am. 2015;40(3):546–553.e548. [DOI] [PubMed] [Google Scholar]
- 5. Dias JJ, Dhukaram V, Kumar P. The natural history of untreated dorsal wrist ganglia and patient reported outcome 6 years after intervention. J Hand Surg Eur Vol. 2007;32(5):502–508. [DOI] [PubMed] [Google Scholar]
- 6. Head L, Allen M, Boyd KU. Long-term outcomes and patient satisfaction following wrist ganglion aspiration. Plast Surg(Oaky). 2015;23(1):51–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nasab SAM, Mashhadizadeh E, Sarrafan N. Comparative study between three methods of aspiration alone, aspiration plus steroid injection and aspiration plus ethanol injection for treatment of dorsal wrist ganglions. Pak J Med Sci. 2012;28(3):404–407. [Google Scholar]
- 8. Singhal R, Angmo N, Gupta S, Kumar V, Mehtani A. Ganglion cysts of the wrist: a prospective study of a simple outpatient management. Acta Orthop Belg. 2005;71(5):528–534. [PubMed] [Google Scholar]
- 9. Stephen AB, Lyons AR, Davis TR. A prospective study of two conservative treatments for ganglia of the wrist. J Hand Surg Br. 1999;24(1):104–105. [DOI] [PubMed] [Google Scholar]
- 10. Varley GW, Needoff M, Davis TR, Clay NR. Conservative management of wrist ganglia. Aspiration versus steroid infiltration. J Hand Surg Br. 1997;22(5):636–637. [DOI] [PubMed] [Google Scholar]
- 11. Breidahl WH, Adler RS. Ultrasound-guided injection of ganglia with corticosteroids. Skeletal Radiol. 1996;25(7):635–638. [DOI] [PubMed] [Google Scholar]
- 12. Chatterjee S, Basu A, Gupta S, Biswas S. Comparative study of recurrence and complications using various sclerosants by single dart technique in treatment of ganglion cysts. Indian J Surg. 2014;76(5):350–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hussain S, Akhtar S, Aslam V, Khan SM. Efficacy of aspiration and steroid injection in treatment of ganglion cyst. Pak J Med Health Sci. 2015;9(4):1403–1405. [Google Scholar]
- 14. Khan PS, Hayat H. Surgical excision versus aspiration combined with intralesional triamcinolone acetonide injection plus wrist immobilization therapy in the treatment of dorsal wrist ganglion; a randomized controlled trial. J Hand Microsurg. 2011;3(2):55–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Limpaphayom N, Wilairatana V. Randomized controlled trial between surgery and aspiration combined with methylprednisolone acetate injection plus wrist immobilization in the treatment of dorsal carpal ganglion. J Med Assoc Thai. 2004;87(12):1513–1517. [PubMed] [Google Scholar]
- 16. Muddu BN, Morris MA, Fahmy NR. The treatment of ganglia. J Bone Joint Surg Br. 1990;72(1):147. [DOI] [PubMed] [Google Scholar]
- 17. Jagers Op Akkerhuis M, Van Der Heijden M, Brink PR. Hyaluronidase versus surgical excision of ganglia: a prospective, randomized clinical trial. J Hand Surg Br. 2002;27(3):256–258. [DOI] [PubMed] [Google Scholar]
- 18. Ajekigbe L, Stothard J. The effectiveness of sodium tetradecyl sulfate in the treatment of wrist ganglia. Can J Plast Surg. 2006;14(1):28–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ashindoitiang JA. Preliminary report of the effectiveness of tetracycline sclerotherapy in treatment of ganglion. Plast Surg Int. 2012;2012624209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gümüş N. A new sclerotherapy technique for the wrist ganglion: transcutaneous electrocauterization. Ann Plast Surg. 2009;63(1):42–44. [DOI] [PubMed] [Google Scholar]
- 21. Kang L, Akelman E, Weiss AP. Arthroscopic versus open dorsal ganglion excision: a prospective, randomized comparison of rates of recurrence and of residual pain. J Hand Surg Am. 2008;33(4):471–475. [DOI] [PubMed] [Google Scholar]
- 22. Sameem M, Wood TJ, Bain JR. A systematic review on the use of fibrin glue for peripheral nerve repair. Plast Reconstr Surg. 2011;127(6):2381–2390. [DOI] [PubMed] [Google Scholar]
- 23. Foster K, Greenhalgh D, Gamelli RL, et al. Efficacy and safety of a fibrin sealant for adherence of autologous skin grafts to burn wounds: results of a phase 3 clinical study. J Burn Care Res. 2008;29(2):293–303. [DOI] [PubMed] [Google Scholar]
- 24. Healy C, Greig AV, Murphy AD, et al. Prospective randomized controlled trial: fibrin sealant reduces split skin graft donor-site pain. Plast Reconstr Surg. 2013;132(1):139e–146e. [DOI] [PubMed] [Google Scholar]
- 25. Giordano S, Koskivuo I, Suominen E, Veräjänkorva E. Tissue sealants may reduce haematoma and complications in face-lifts: a meta-analysis of comparative studies. J Plast Reconstr Aesthet Surg. 2017;70(3):297–306. [DOI] [PubMed] [Google Scholar]
- 26. Janis JE, Khansa L, Khansa I. Strategies for postoperative seroma prevention: a systematic review. Plast Reconstr Surg. 2016;138(1):240–252. [DOI] [PubMed] [Google Scholar]
- 27. Hempfling H, Frisbie EJ. Arthroscopically controlled sealing of Baker’s cysts In Schlag G, Bösch P, Matras H, ed. Fibrin Sealing in Surgical and Nonsurgical Fields. Berlin, Heidelberg, Germany: Springer; 1994:76–84. [Google Scholar]
- 28. Carr AJ, Higginson IJ. Are quality of life measures patient centred? BMJ. 2001;322(7298):1357–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Higginson IJ, Carr AJ. Measuring quality of life: using quality of life measures in the clinical setting. BMJ. 2001;322(7297):1297–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Muldoon MF, Barger SD, Flory JD, Manuck SB. What are quality of life measurements measuring? BMJ. 1998;316(7130):542–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mehdian H, McKee MD. Scapholunate instability following dorsal wrist ganglion excision: a case report. Iowa Orthop J. 2005;25:203–206. [PMC free article] [PubMed] [Google Scholar]
- 32. Rocchi L, Canal A, Pelaez J, Fanfani F, Catalano F. Results and complications in dorsal and volar wrist ganglia arthroscopic resection. Hand Surg. 2006;11(1-2):21–26. [DOI] [PubMed] [Google Scholar]
- 33. Watson HK, Rogers WD, Ashmead D. Reevaluation of the cause of the wrist ganglion. J Hand Surg Am. 1989;14(5):812–817. [DOI] [PubMed] [Google Scholar]