Abstract
Background:
Patient-driven innovation in diabetes management has resulted in a group of people with type 1 diabetes who choose to build and share knowledge around a do-it-yourself (DIY) open source artificial pancreas systems (OpenAPS). The purpose of this study was to examine Twitter data to understand how patients, caregivers, and care partners perceive OpenAPS, the personal and emotional ramifications of using OpenAPS, and the influence of OpenAPS on daily life.
Methods:
Qualitative netnography was used to analyze #OpenAPS on Twitter over a two-year period.
Results:
There were 328 patients, caregivers, and care partners who generated 3347 tweets. One overarching theme, OpenAPS changes lives, and five subthemes emerged from the data: (1) OpenAPS use suggests self-reported A1C and glucose variability improvement, (2) OpenAPS improves sense of diabetes burden and quality of life, (3) OpenAPS is perceived as safe, (4) patient/caregiver–provider interaction related to OpenAPS, and (5) technology adaptation for user needs.
Conclusions:
As users of a patient-driven technology, OpenAPS users are self-reporting improved A1C, day-to-day glucose levels, and quality of life. Safety features important to individuals with diabetes are perceived to be embedded into OpenAPS technology. Twitter analysis provides insight on a patient population driving an innovative solution to improve their quality of diabetes care.
Keywords: OpenAPS, artificial pancreas, patient innovation, Twitter, social media, diabetes
Diabetes can pose complex challenges for people with type 1 diabetes (PWD). Despite advances in technology and commercialization of products, the pace of innovation and regulation can feel slow to PWD. Because of this, PWD frequently self-experiment to make diabetes management easier, more predictable, and less time-consuming. The result is often personalization of solutions that range from simple life hacks to challenging the status quo of diabetes treatment options available on the commercial market. One example of this is the development of an open source artificial pancreas (OpenAPS) or hybrid closed-loop automated insulin delivery system.1
The hashtag #WeAreNotWaiting is specific to patient innovation in the diabetes online community. First stated in 2013,2 #WeAreNotWaiting became an ongoing theme encompassing the many efforts and desires reflected in the patient community to accelerate development, access, and adoption of diabetes-related tools. OpenAPS is one project that emerged from the #WeAreNotWaiting movement.
Launched in February 2015, OpenAPS focuses on facilitating access to artificial pancreas technology through do-it-yourself (DIY), patient-developed innovations that bridge communication between existing insulin pumps and continuous glucose monitors (CGM).1 OpenAPS and related DIY systems must be self-built, are not regulated or approved by the Food and Drug Administration, and are not managed by any commercial entity. As of July 2018, an estimated 725+ PWD worldwide were reporting using a DIY hybrid closed-loop system, such as OpenAPS.3
There is a paucity of research evaluating patient-developed technology, such as OpenAPS. Most reports focus on the technical development, implementation, safety, security, usability, and open-source nature of systems.4 To date, there has been no analysis of the impact, interactions, and outcomes associated with OpenAPS, particularly within the diabetes online community. As OpenAPS originates from interactions from a primarily online community, it is meaningful to examine related social media conversations. Thus, the purpose of this study was to examine Twitter data to understand how patients, caregivers, and care partners perceive OpenAPS, the personal and emotional ramifications of using OpenAPS, and the influence OpenAPS on daily life.
Methods
Research Design
We conducted a qualitative netnography study of conversations in the OpenAPS community. Netnography, an ethnography-inspired qualitative research method,5 was used to focus on the observation and recontextualization of conversational discourse mediated by text online. Utilizing netnography supports analyzing a myriad of online information and is dependent on the phenomenon of interest. Unlike the typical retrospective evaluation of text in traditional qualitative methods, netnographic methods call for participation of real conversations, establishing a “sense of community” for both the participants and the researchers.6 Due to the technology involved and large volumes of data, computer-aided data extraction and assistance with analysis can be used to augment the traditional ethnographic approaches.6,7 Similar to other fields of qualitative research, data saturation is reached when no new ideas or themes emerge.8
Data Collection
University of Utah ethics approval was sought; however, this work was considered exempt due to the public availability of tweets. Using a netnography approach, we conducted fieldwork over one year in three stages. In the first stage, the researchers became involved and familiarized themselves with (MLL, PMG) or were a part of the OpenAPS community (DL, LAK).9 The second stage consisted of data collection in three approaches: (1) exhaustive analysis of #OpenAPS on Twitter including prospective discovery and retrospective analysis, which is further described below, (2) written field notes of interactions between OpenAPS users on Twitter, in-person and online discussions about OpenAPS at various conferences or meet-up groups the researchers had attended, and (3) supporting documentation, such as news reports, blogs, and special press articles. In stage 3, data were reviewed and contextualized to address the purpose of the study.
The analysis of the #OpenAPS Twitter conversation occurred after extracting data through Symplur Signals (Los Angeles, CA).10 Symplur Signals uses a proprietary algorithm to extrapolate demographic information from Twitter account biographies to assign type of stakeholder (e.g., patient, caregiver, care partner, etc.), language use in tweets, and geographic location. We used fixed demographic markers to extract patients, caregivers and care partners data only. Tweets by patients, caregivers, and care partners written in English between January 1, 2016, and January 1, 2018 were included in the analysis. These dates were chosen based on when #OpenAPS was registered with Symplur Signals. Tweets authored by other health stakeholders (e.g., HCP, industry, researchers) or written in a language other than English were excluded.
Deidentified tweets with original links to the tweets were downloaded into an Excel file. If tweets were part of a conversation, the original tweet link was accessed to contextually examine the entire conversation to enhance understanding. Tweets were analyzed using an open-code approach. A codebook was developed that included codes, categories, and corresponding themes. Field notes were reviewed throughout the coding process.
Trustworthiness
Netnography relies on the researcher being transparent in disclosing any potential conflict of interest or influence on the data analysis based on personal interests, experiences, and interactions with online content; this concept is known as reflexivity.6,7 Each researcher acknowledged their connection to the OpenAPS community. The lead researcher (MLL), a nurse practitioner, has been exposed to OpenAPS through patients who are using or inquiring about OpenAPS. Other researchers (DL and LAK) are immersed in the OpenAPS community as a personal user of OpenAPS (DL) or caregiver for someone who uses OpenAPS (LAK). It is important to note that one of the researchers (DL) helped to develop OpenAPS technology. In order to decrease potential bias, all tweets from any of the researchers related to #OpenAPS were removed from the final analysis. The final researcher (PMG) is a nurse scientist focused on online communities and is also a member of an OpenAPS online community. In acknowledging individual relationship with OpenAPS, the research team frequently assessed procedures for data collection, analysis and presentation to reflect objectivity and nonbias.
Analysis
Tweets in English were read by two independent investigators (MLL and PMG). A codebook was initially developed by one investigator (MLL), then reviewed by a second investigator (PMG) to establish credibility. Codes, a label assigned to give meaning to the text,11 were documented in the codebook, allowing for an open code approach.12,13 The codes were then collapsed into categories and corresponding themes.14 The frequency of codes, uniquely identified in Twitter research as retweets, were used to assess the content of the data but not to determine data saturation.8 Member matching was employed among #OpenAPS community members including a PWD (DL) and a caregiver to a child with T1D (LAK) in the #OpenAPS community to confirm the accuracy of findings.15 To protect the privacy of individuals, quotes are slightly altered, while maintaining the meaning of the tweet.
Results
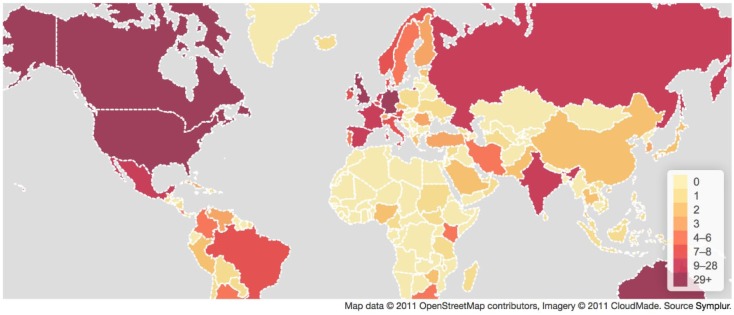
During the studied two-year time period, the total sample included 3347 tweets generated by 328 patients, caregivers, and care partners. The majority of individuals tweeted fewer than 25 times (see Table 1). While only examining tweets written in English, the #OpenAPS conversation included tweets from 92 countries (see Figures 1 and 2).
Table 1.
Tweets per User (N = 329).
| Number of tweets | Users |
|---|---|
| >500 | 2 |
| 150-499 | 6 |
| 50-149 | 15 |
| 25-49 | 17 |
| 5-24 | 49 |
| <5 | 241 |
Figure 1.
Global map of #OpenAPS Twitter users.
Figure 2.
US map of #OpenAPS Twitter users.
The #OpenAPS discussion on Twitter included stakeholders influenced by DIY technology in varying ways, including (1) patient innovators (“developers”) who have developed various forms of OpenAPS; (2) active OpenAPS users from the standpoint of a PWD, care partner, or caregiver; (3) individuals interested starting OpenAPS in the near future who were learning from current OpenAPS users and developers; and (4) individuals who supported OpenAPS and participated in discussions, but did not announce plans to start OpenAPS.
The analysis resulted in one overarching theme, OpenAPS changes lives. There were five major subthemes (Table 2).
Table 2.
Themes.
| Overarching theme | OpenAPS changes lives |
| Subthemes | 1. OpenAPS use suggests self-reported A1C and glucose variability improvement 2. OpenAPS improves sense of diabetes burden and improves quality of life 3. OpenAPS is perceived as safe 4. Patient/caregiver–provider interaction related to OpenAPS 5. Technology adaptation for user needs |
1. OpenAPS Use Suggests Self-Reported A1C and Glucose Variability Improvement
OpenAPS users indicated improvements in A1C. Some tweets indicated their A1C was at their personal all-time low, while other tweets reported they had achieved the best A1C they’d seen in quite some time or their entire life. Among those who did tweet about their A1C in the current tense, the range was 4.9-6.8% (n = 110). One person tweeted, “Finding OpenAPS literally changed my life. My numbers have been astounding. Last A1C was 5.4!” This improvement in A1C related to positive sentiment about one’s self and the OpenAPS community at large.
Beyond A1C, individuals tweeted about time in range. Individuals reported that OpenAPS allowed them to experience decreased glucose variability. One person tweeted, “Boring glucose is beautiful [photo of CGM with 96 → and flat glucose pattern for the previous 3 hours].” Challenges that would have previously resulted in glucose variability (high levels of stress, illness, or hormonal fluctuations) were mitigated by OpenAPS. One person tweeted, “Received a steroid injection yesterday. I’m running high, but #OpenAPS is working hard. Could be way worse [photo of CGM with glucose of 187 →].”
2. OpenAPS Improves Sense of Diabetes Burden and Quality of Life
Beyond A1C, the greatest impact appeared to be on the emotional impact OpenAPS had on individuals and families affected by diabetes. Overall, OpenAPS users and their caregivers and care partners reported they felt a reduction of diabetes-related “burden” or “distress.” The automatic adjustment by OpenAPS freed the PWD from being constantly mentally tasked. One person noted that diabetes was a full-time job, however “90%” was taken care of by OpenAPS while another person echoed the sentiment by tweeting, “This is amazing. Great levels, not killing myself to get it!” In a singular case, one person tweeted, “I don’t even think about my diabetes on most days.”
Individuals reported that OpenAPS allowed them to live their lives with minimal disruptions. Activities pursued included engaging in sports, eating out at a restaurant, frequent snacking at a party, and travel. In addition, improvement in sleep quality was highlighted. One person tweeted, “I haven’t woken up in the middle of the night once since I started looping,” while a parent tweeted, “First day with #OpenAPS. Result: already saved [prevented] 1 low and 1 high. Real result: boy smiling, dad in tears of joy!” While the overall sentiment was positive, there were a few negative comments related to lack of access.
3. OpenAPS Is Perceived as Safe
As individuals developed OpenAPS for their own personal use or contributed on behalf of loved ones, safety appeared to be critical within the open source community. Individuals reported a confidence in their ability to live with diabetes due to improvements in glucose levels and safety features embedded into OpenAPS. Features described within OpenAPS included “extra security against untreated overnight hypos” and allowing PWD to travel alone or sleep without fear. One tweet described the safety features that are built into OpenAPS in which the insulin pump will revert back to usual basal rates, “For those times when I’ve lost [connection to] CGM readings . . . fallback [to standard] basal.” In addition, users described smaller details such as the time setting auto-adjusting for daylight savings. Although there is no research to support the safety of this, and some may find it distracting, one tweet highlighted the ability to visualize CGM readings on the digital dashboard while driving as providing a level of safety. As a result of the safety features reported, individuals described feeling more comfortable with lower glucose levels that may have previously resulted in hypoglycemia fear. One tweet stated, “For those who are afraid of a A1c of 5.3, I would be too w/out loop.”
OpenAPS was not touted as a cure. Similar to commercial artificial pancreas systems, OpenAPS requires individuals to be engaged with their diabetes management through maintenance of equipment, carbohydrate counting, insulin boluses, and ongoing monitoring of glucose levels. Users tweeted about the importance of calibration in order to keep CGM levels accurate since OpenAPS uses CGM data to calculate insulin dosage. One tweet likened management of diabetes with OpenAPS to flying an aircraft that may or may not have autopilot, indicating that the user still needed to be aware of the diabetes management and troubleshooting strategies in case of OpenAPS failure. OpenAPS failure could occur if cellular service was poor or nonexistent. While there were many tweets indicating OpenAPS was built for patient safety, there were a few tweets expressing concerns about security based on reliance of older-model insulin pumps that must be used.
4. Patient/Caregiver–Provider Interaction Related to OpenAPS
OpenAPS users are active participants in their diabetes management and are in a position to educate their health care provider (HCP) about OpenAPS technology. PWD who use OpenAPS reported being received by HCPs with varied reactions. However, some tweets indicated PWD were hesitant to bring up OpenAPS with their HCP, while others sought advice about how to approach HCPs about their OpenAPS use. Multiple tweets indicated that individuals had already shared the information with their HCP, who supported their use of OpenAPS because of the impact on A1C. One person reported, “My endo totally loooved #OpenAPS. My endo said he’s not waiting either #wearenotwaiting. So happy.” There were several tweets focused on the positive patient/caregiver-HCP interactions. These patient/caregiver-provider interactions appeared to relate to the positive A1C levels patients were experiencing from using OpenAPS.
There were reports of HCPs who were resistant to the idea of OpenAPS. HCPs who were hesitant wanted more information about how OpenAPS would operate in specific scenarios, such as high carbohydrate consumption. One tweet described how some HCPs had become “visibly upset that they hadn’t heard of OpenAPS” or other similar patient-driven innovations. This suggests some HCPs are frustrated that they have not been made aware of OpenAPS. OpenAPS users wanted their HCPs to be supportive. As such, they were willing to change HCPs if necessary. One tweet stated, “I couldn’t imagine sticking with a doc that didn’t support such advances.”
5. Technology Adaptation for User Needs
Users discussed the ability of OpenAPS to be customized to support varying system and tools to meet their individual needs. As such, various types of DIY closed loops were discussed, along with their related technology components. There were some tweets that focused on individuals who had difficulties getting all of the supplies needed to operate OpenAPS (ie, specific insulin pump model) or challenges in getting the technology to work. In response to tweets requesting technical assistance, several individuals provided various types of help. Help included (1) links to specific OpenAPS directions, (2) answers to specific questions, (3) encouraging words of support, or (4) connections to individuals or websites where OpenAPS supplies could be purchased. Of those who had difficulty getting OpenAPS working, challenges were described as “growing pains.”
Specific OpenAPS developers and active contributors in the community were recommended for their ongoing support and help. There were tweets about upcoming in-person gatherings for individuals to get support. Individuals contemplating OpenAPS and new OpenAPS users were encouraged to seek out the community. One individual noted his own success and desire to help another, “365 days after closing my loop, splendid A1c [of 5.4% per photograph], now helping another guy to close his loop.” “Pro-Tips” were provided to those who were just starting to use OpenAPS. The community had come together because of the need for diabetes solutions; however, they willingly stayed in the OpenAPS community because of the interconnectedness of the individuals. Tweets of gratitude for the OpenAPS developers and other community members who provided ongoing support occurred frequently. One person tweeted, “As brilliant as the technology is, it’s the kindness and generosity of the #OpenAPS community.”
Discussion
This article aimed to understand how patients, caregivers and care partners perceive OpenAPS, the personal and emotional ramifications of using OpenAPS and the influence OpenAPS had on daily life, based on publicly shared online conversations. Clinical implications are discussed below.
In this study, reported A1C levels were within the American Diabetes Association,16 American Association of Clinical Endocrinologist, and American College of Endocrinology goals17 and were self-reported to be improvements compared to A1C levels prior to OpenAPS use. Given the nature of our dataset, we were unable to obtain and link pre- and post-OpenAPS data. However, three small recent studies indicate the use of OpenAPS demonstrates improved A1C in a pre-post analysis.18-20
Beyond A1C, our results suggest OpenAPS improves the issues Gopisetty et al21 found to most profoundly impact daily life for PWD: (1) time commitment and burden, (2) difficulty managing BG overall, and (3) hypoglycemia. Improvements in these three areas along with embedded safety features resulted in improvement to quality of life. Others have found a relationship between patient-driven innovation and improvements to quality of life22,23 and glucose outcomes.18-20
Oftentimes, when an individual starts a new diabetes technology, a clinician provides the training. In the case of OpenAPS, individuals/families are relying on written instructions and support from the OpenAPS community. There are some individuals who may have less technical skills or literacy that may have difficulty initiating OpenAPS on their own. There is also difficulty obtaining compatible pumps. PWD also reported concerns about relying on out-of-warranty technology. There may be individuals who tried OpenAPS and stopped due to technical challenges or untoward effects. However, this was not identified in the dataset.
HCPs should be aware that some patients are currently engaging or plan to engage in patient-driven innovation, such as OpenAPS. Although HCPs were not assessed in this manuscript, HCPs are participating in the #OpenAPS discussion on Twitter in a positive way.24 HCPs may want to consider becoming more informed about OpenAPS and other patient-driven innovations to support positive patient-provider interactions.
Limitations
We examined retrospective Twitter data only, although OpenAPS is discussed on numerous other social media platforms. Therefore, we are not able to identify specific demographic information, such as gender, age, education level, or diabetes duration. We are also not able to determine how many participants in our sample were actual OpenAPS users, or care partners or caregivers supporting OpenAPS users. Since Symplur captures hashtags only after they are registered, we were not able to examine data prior to January 1, 2016.
As identified by others,25,26 positive bias can exist within online communities, resulting in like-minded users to unify around a specific sentiment. In addition, social responsibility in reporting a variety of experiences, including negative ones, is more likely to occur with sufficient levels of community feedback.27 Although not identified in this study, there may be individuals who tried and stopped OpenAPS due to challenges obtaining or maintaining technology, safety issues, or other negative experiences. Furthermore, there may have been OpenAPS users who did not share A1C levels on Twitter due to possible social pressure to report positive experiences. In this study, A1Cs higher than 6.8% were not self-reported. However, there were also reports of A1Cs improving without distinct numbers, which may or may not have met ADA and AACE recommendations. Self-report of A1C may also affect reliability of data. However, previous work has identified concordance between self-reported A1C and registry data.28,29 Transparency is important to OpenAPS users,30 as such OpenAPS users in this study sometimes shared photographs of their A1C data. However, photographs did not accompany tweets frequently enough to validate each A1C reported.
Future Studies
Future research should focus on the impact of OpenAPS on clinical and psychosocial outcomes in a fully powered trial using validated tools. OpenAPS users have donated anonymized data to a “Data Commons” to support additional research studies.31 Since diabetes is often managed in a social context, the impact of OpenAPS on caregivers and care partners should continue to be explored.
Conclusion
Twitter analysis of #OpenAPS suggests improved A1C, day-to-day glucose levels, and quality of life while being safe for its users. Future studies should explore the impact of OpenAPS on PWD, their caregivers, and care partners.
Footnotes
Abbreviations: CGM, continuous glucose monitor; DIY, do it yourself; HCP, health care provider; OpenAPS, open artificial pancreas system; PWD, people with diabetes.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: MLL and PMG have no conflict of interest disclosures to report. DL is an OpenAPS developer and user. LAK has a child who is using OpenAPS. DL and LAK have not received any financial benefits related to OpenAPS development or use and have no other disclosures to report.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. OpenAPS. Open APS. 2017. Available at: https://openaps.org/ Accessed February 28, 2018.
- 2. Diabetes Mine. “We Are Not Waiting” = Diabetes Data Innovation Now! N.d. Available at: https://www.healthline.com/health/diabetesmine/innovation/we-are-not-waiting Accessed February 28, 2018.
- 3. OpenAPS. OpenAPS Outcomes. 2018. Available at: https://openaps.org/outcomes/ Accessed July 27, 2018.
- 4. White K, Gebremariam A, Lewis D, et al. Motivations for participation in an online social media community for diabetes. J Diabetes Sci Technol. 2018:12(3):712-718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kozinets RV. The field behind the screen: using netnography for marketing research in online communities. J Mark Res. 2002;39(1):61-72. [Google Scholar]
- 6. Costello L, McDermott ML, Wallace R. Netnography: range of practices, misperceptions, and missed opportunities. Int J Qual Methods. 2017;16(1):1-12. [Google Scholar]
- 7. Kozinets RV. Netnography: Redefined. London, UK: Sage; 2015. [Google Scholar]
- 8. Morse JM. The Significance of Saturation. Qual Health Res. Thousand Oaks, CA: Sage; 1995; 5(2): 147-149. [Google Scholar]
- 9. Kozinets RV. Netnography: Doing Ethnographic Research Online. London:, UK Sage; 2010. [Google Scholar]
- 10. Audun UM. Symplur Signals, a health care social media analytics platform. 2018. Available at: https://www.symplur.com/signals/. Accessed February 8, 2018.
- 11. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105-112. [DOI] [PubMed] [Google Scholar]
- 12. Morgan DL. Qualitative content analysis: a guide to paths not taken. Qual Health Res. 1993;3(1):112-121. [DOI] [PubMed] [Google Scholar]
- 13. Sandelowski M. Focus on research methods-whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334-340. [DOI] [PubMed] [Google Scholar]
- 14. Tesch R. Qualitative Research: Analysis Types and Software Tools. New York, NY: Psychology Press; 1990. [Google Scholar]
- 15. Creswell JW, Miller DL. Determining validity in qualitative inquiry. Theory Pract. 2000;39(3):124-130. [Google Scholar]
- 16. American Diabetes Association. Standards of medical care in diabetes—2018 abridged for primary care providers. Clinical Diabetes. 2018;36(1):14-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Handelsman Y, Bloomgarden ZT, Grunberger G, et al. American Association of Clinical Endocrinologists and American College of Endocrinology—clinical practice guidelines for developing a diabetes mellitus comprehensive care plan—2015. Endocr Pract. 2015;21(suppl 1):1-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lewis DM, Swain RS, Donner TW. Improvements in A1C and time-in-range in DIY closed-loop (OpenAPS) users. Diabetes. 2018;67(suppl 1). Available at: 10.2337/db18-352-OR. [DOI] [Google Scholar]
- 19. Provenzano V, Guastamacchia E, Brancato D, et al. Closing the loop with OpenAPS in people with type 1 diabetes—experience from Italy. Diabetes. 2018;67(suppl 1). Available at: 10.2337/db18-993-P. [DOI] [Google Scholar]
- 20. Choi SB, Hong ES, Noh YH. Open artificial pancreas system reduced hypoglycemia and improved glycemic control in patients with type 1 diabetes. Diabetes. 2018;67(suppl 1). Available at: 10.2337/db18-964-P [DOI] [Google Scholar]
- 21. Gopisetty D, Levine B, Liu N, et al. How does diabetes affect daily life? A beyond-A1C perspective on unmet needs. Clin Diabetes. 2018;36(2):133-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lewis D, Leibrand S. Real-world use of open source artificial pancreas systems. J Diabetes Sci Technol. 2016;10(6):1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lee JM, Newman MW, Gebremariam A, et al. Real-world use and self-reported health outcomes of a patient-designed do-it-yourself mobile technology system for diabetes: lessons for mobile health. Diabetes Technol Ther. 2017;19(4):209-219. [DOI] [PubMed] [Google Scholar]
- 24. Litchman ML, Gabel H, Fitzgerald C, Hoyos MG, Lewis D, Gee P. #WeAreNotWaiting: “I Want Life”—The Medical Device Hacking Patient Movement. Palo Alto, CA: Stanford Medicine X; 2017. [Google Scholar]
- 25. Askay DA. Silence in the crowd: the spiral of silence contributing to the positive bias of opinions in an online review system. New Media Soc. 2015;17(11):1811-1829. [Google Scholar]
- 26. Cabling ML, Turner JW, Hurtado-de-Mendoza A, et al. Sentiment analysis of an online breast cancer support group: communicating about tamoxifen. Health Commun. 2018;33(9):1158-1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kim H-S, Sundar SS. Can online buddies and bandwagon cues enhance user participation in online health communities? Comput Human Behav. 2014;37:319-333. [Google Scholar]
- 28. Schneider AL, Pankow JS, Heiss G, Selvin E. Validity and reliability of self-reported diabetes in the Atherosclerosis Risk in Communities Study. Am J Epidemiol. 2012;176(8):738-743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Løvaas KF, Cooper JG, Sandberg S, Røraas T, Thue G. Feasibility of using self-reported patient data in a national diabetes register. BMC Health Serv Res. 2015;15(1):553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Omer T. Empowered citizen “health hackers” who are not waiting. BMC Med. 2016;14(1):118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. OpenAPS. Data Commons. 2018. Available at: https://openaps.org/data-commons/. Accessed on July 27, 2018. [Google Scholar]