Abstract
Introduction:
Patients with diabetes often generate large amounts of data specifically related to the disease and to their general health. Cross-institutional sharing of patient health care data is complex, and as a consequence, data are not always available to the health care provider treating the patient. Accommodating this challenge could lead to better clinical effectiveness and improve clinical research. This work aims to present an approach for a blockchain-based platform for sharing health care data. The approach considers privacy concerns, data sharing, and patients as the center for governing their own data.
Methods:
The concept of this blockchain-based platform consists of using the NEM multi-signature blockchain contracts for access control of data management and the sharing and encryption of data to allow privacy and control of health care data. The architecture is built around cryptography, tokens, and multi-signature contracts. The multi-signature contract enables several entities to administrate the activity of an account and control the assets of one account. Multi-signature generates a contract that assigns the rights and powers of a certain account to other accounts; this contract can be edited to allow or remove entities.
Discussion:
Using blockchain could lead to improvements in diabetes data management. In the coming years, this technology should be implemented in existing small-scale diabetes health care system to explore its real-world benefits and challenges.
Conclusion:
This new approach could potentially lead to more efficient sharing of data between institutions and utilization of new types of data and research possibilities.
Keywords: blockchain, diabetes, health care, access management
Diabetes is a chronic disease that involves many actors other than the patient. For instance, the general practitioner, endocrinologist, diabetes nurse, relatives, caretakers, and various specialists at the hospital, such as eye specialists, nephrologists (if end-stage kidney disease has developed), cardiologists, among others. Thus, patients with diabetes often generate large amounts of data specifically related to the disease as well as to their general health, such a health records, physical activity, self-measurement of blood glucose, home measures of the urine for glucose and acetoacetate, blood tests for 3-hydroxy-butyrate, continuous glucose monitoring (CGM), blood pressure, and so on, all of which are relevant to diagnose and treat the disease.1-3 Cross-institutional sharing of patient health care data is complex, and consequently, data are not always available to the health care provider treating the patient. Accommodating this challenge may lead to better clinical effectiveness and improve clinical research.4-6
There is a challenge with sharing health care data because health care institutions are unwilling to share data due to privacy concerns, the fear of giving other institutions competitive advantages, and technical barriers (there is no common platform for sharing these complex and heterogenous data).7 Furthermore, patients are often left without control of their own data and excluded from the decision of which entities have access to which aspects of their personal data.8 Preferably, the patient would have control over his or her data, which could potentially empower the patient to be more involved in treatment. This is not to neglect the fact that many patients already are highly motivated to participate in this process. Many already measure a broad range of disease indicators, such as vital signs (blood pressure, glucose measurements, etc), medicine, exercise, sleep quality, physical functioning, and quality of life. However, these data are not always utilized by the health care provider because of technical difficulties in sharing and securing data.9
Blockchain, or a distributed ledger, is the technology that enables cryptocurrencies such as bitcoin,10 which is pushing us into a new era of transparency and decentralization. While the first wave of blockchain technology focused on creating a global decentralized currency, emerging technologies such as Ethereum, NEO, and NEM are developing platforms to build blockchain-based applications that have a variety of complex uses.11 These use cases expand beyond financial applications (such as payment) into business management, logistics, access control, governance, anticounterfeiting, voting, and health care management.12
One of the interesting cases for applying this technology is within the health care domain where the use of blockchain technology has the potential to disrupt and improve the way we use and share patient data.13 Moreover, using the blockchain for access control could potentially be a means to comply with the new European General Data Protection Regulation (GDPR).
This work aims to present and discuss an approach for the implementation of a blockchain-based platform for sharing health care data. The approach considers privacy concerns and resolves around the patient being the center for governing personal data to relevant health care entities. The basis of this approach is centered around the NEM platform, as this technology has several appealing features for health care applications.
Background
What Is the Blockchain?
A blockchain is a distributed transaction/data ledger composed of blocks, with each block representing data linked to the previous block (layers of increasingly complex data secured by cryptographic hashing layers the data chronologically). For use as a distributed ledger, a blockchain is often managed by a peer-to-peer network cooperatively adhering to a protocol for authenticating new blocks into the blockchain.10 The concept itself is rather simple, but has several interesting features. The blocks are immutable because each block contains a hash of the previous blocks content, which means that the entire blockchain is effectively linked together. Changing one block in the historical chain also changes the content of all other blocks in the chain. The blockchain consensus mechanism among the nodes in the network ensures the immutability of data because, in practice, it would be impossible to alter the entire blockchain in the network. The authenticating process of including new block in the chain was originally implemented in the bitcoin protocol as a proof of work. Other emerging blockchain platforms have used other mechanisms, such as proof of stake or proof of importance, that have shown to be more efficient.14 The nature of the blockchain makes the validity of data very high and there are several other advantages regarding security. There is no single point of failure, as in many ordinary systems, and the use of encryption makes it practically impossible to hack as long as the encryption key is not compromised.
Smart Blockchain Platforms
The new generation of smart blockchains, such as Ethereum, NEO and NEM,15 are interesting platforms that offer several useful features for developing blockchain-based health care data management.
There is both a public chain and a private chain. The private chains could store private data, maintaining control of the network with the benefit of blockchain technology. Smart blockchains have asset functionality, which means that new tokens (assets) can be created and distributed on the network; these assets could be assigned different purposes (eg, in the context of a health care applications, such assets could be used to appoint roles or permissions to health care institutions or label the functionality of an account).
Another integrated feature is multi-signature contracts, which enable an interaction between accounts. Multi-signature contracts refer to the requirement of more than one key to authorize a transaction on the blockchain. A multi-signature contract can be developed to control which entities have access to an account and can be modified in a way such that several of the affiliated entities need to approve a change or transaction to the account before it will be effectuated. A change to an account could, for example, be a change of permission such that a new health care institution gains access. This functionality is essential for building a health care data management platform (this is further described in the implementation section).
The interaction with the NEM blockchain is available through simple web calls (to an API gateway server), which simplifies the creation of client apps. This means that the blockchain can be accessed and altered using any programming language, which is important because various systems from different clinical facilities should be able to add and/or read patient data to and from the blockchain. Other blockchains, such as Ethereum, are much more complex and the rules for interaction are written in a specialized programming language and uploaded to the blockchain.
Implementing Data Management
This proposal involves the use of a smart blockchain. We use the NEM public or private blockchain to develop patient-centered governance of health data stored on and off the chain. The concept consists of using multi-signature contracts for access control of data management and data encryption to allow privacy and control of health care data. The other blockchain platforms mentioned (Ethereum & NEO) could likewise be used for implementations.
The patient will have full access to personal data and control over which entities it is shared with. The patient can set access permissions and designate who can read and write health care data to the account. This access-control management could be used with off-chain applications. The application would allow the patient to see which entities have access to the personal data and allow the patient to assign new permits and revoke access. The permissions could be flexible both with respect to permission time frame and data types. The off-chain management application would ensure that time-dependent contracts were executed and allow an intuitive interface for the blockchain. This concept would provide transparency and allow the patient to make central decisions about the health care data collected and how the data are shared between relevant entities.
For example, if Jack would like to share his health data with the hospital, he can grant it full access to all data. If he would also like to share some relevant information with his chiropractor, he invokes this person partial access. To do this, he would log in and interact with the system using an app and a personal password; thus, Jack would not need coding skills or experience any direct interaction with the blockchain.
When a health care entity is awarded access to the patients’ health data, it queries the blockchain for the data and uses the account-bound key to decrypt the data. The health care entity could use a customized application to view and analyze the data. Querying the blockchain based on an API, which would allow any programming application to interface with the blockchain. This means that a hospital using an electronic patient journal system could integrate their system with the blockchain. This API-based approach makes it very easy to integrate data from new devices and records. In the future, we can imagine the integration of data from emerging technologies, such as pulse watches, intelligent earplugs, and CGM devices.
Architecture
The architecture is built around cryptography, mosaics (a token on the blockchain), and the multi-signature contracting available on the platform. The multi-signature contract enables several entities to administer the activity of an account, control assets from one account (such as mosaics), or create additional contracts. NEM’s multi-signature feature makes an editable contract that assigns the rights and powers of a certain account to other accounts. The multi-signature contract can be created so that any number of the signatures needs to sign a transaction; this is called m-of-n multi-signatures, where m can be any number equal to or less than n. In the architecture of the health care blockchain, a 2-of-n multi-signature contract would be applied. The patient would control 2 keys in the contract and each health care entity included in the contract associated with the patient’s account would hold 1 key. This means that the patient will remain in control of the account by having the required number of keys to edit the contract. Health care entities still have the ability to view account information (such as messages, treatments, etc) and initiate transactions. The concept is illustrated in Figure 1. The patient would still need cosign transactions initiated by other entities but this could be set to be done automatically or within rules in the off-chain application layer.
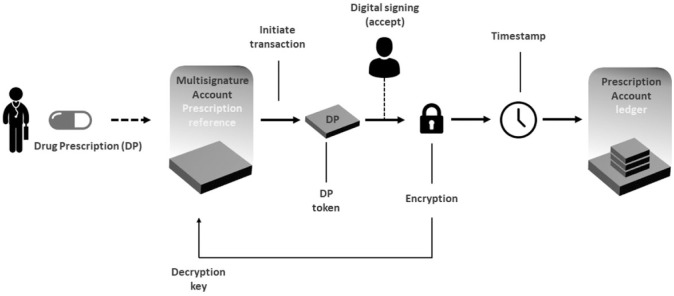
Figure 1.
The concept of an entity that prescribes a drug for a patient. The transaction is initiated by the entity, accepted by the patient manually or automatically within certain rules, encrypted, and time stamped. The encryption key is sent to the patient’s multi-signature account so that only entities with access can read the prescription from the prescription ledger.
New data would be stored on the blockchain in the following manner: the patient or a health care entity, with at least one key associated to the patient’s multi-signature account, would initiate a transaction, sending a data mosaic containing data as a message. The message would be encrypted, and the decryption key would be sent to the multi-signature account in a separate transaction. When the data mosaic transaction is cosigned manually or automatically, the transaction is sent to an account related to that specific data type. This ensures that only entities with access to the multi-signature account can read the patient’s data using the decryption key. In practice, the patient would control several multi-signature accounts—each allocated to a specific type of data. This architecture would allow the access differentiation for different types of data between health care entities. In practice, this architecture would be affected “under the hood,” and the patient and health care entity would interact with a frontend system.
Trusted Party
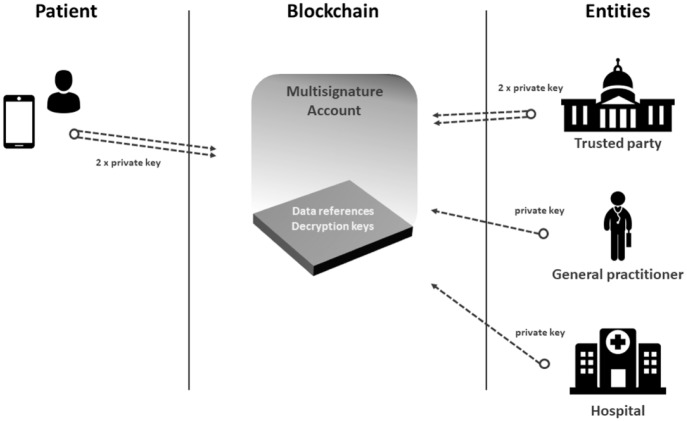
A challenge with self-governance is when the patient is unable to make the necessary access permits. This could be related to treatment of acute critical illness, dementia, or loss of personal keys. This needs to be considered to determine if a blockchain implementation is feasible in the real world. A solution could allow trusted parties to hold an additional keypair for emergencies. A trusted party could be a close relative to the patient or a special government organ that is separate from the health care sector. In case of emergency (eg, if the patient is involved in a car accident and needs acute treatment), the medical staff could invoke the procedure to allow medical data access using the trusted party. Regulation and legislation would ensure the procedure and protect against misuse. This concept is illustrated in Figure 2
Figure 2.
The concept of access management. The patient and a trusted party control the number of keys needed to change the multi-signature contract. Other entities only hold one key, which means they can only initiate transactions and read from the ledger related to the patient.
Data Lake
Storing large data files, such as raw ECG and medical images files, is not directly suitable for storage on the blockchain. These type of patient data are common in the health care sector and the solution for including these data could be to establish a repository with references in the blockchain.
All large collection of medical data could be stored off the blockchain in a data repository called a data lake.8 Data lakes are highly scalable and can store a wide variety of data, such as images and timeseries data. The data lake would be accessible for all health care providers and only used for the storage of encrypted data. In this setup, the patient would still have control of who has access to the personal data in the data lake because the data would not be readable without the decryption key, which is stored on the patient’s blockchain account. The concept of the data lake is illustrated in Figure 3.
Figure 3.
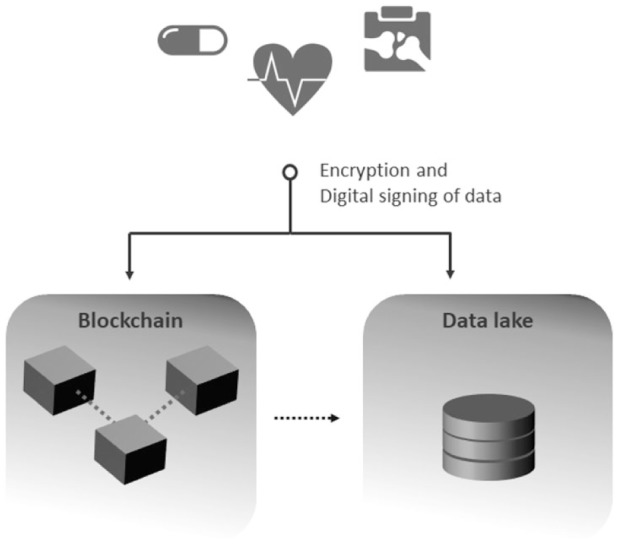
How blockchain could be used for access management for encrypted data stored in a data lake.
Conclusion
Usage of the blockchain could lead to several improvements in the health care sector. This paper describes an architecture for implementing data and access management using an existing blockchain platform. This is relevant for patients with diabetes, a group of chronic patients prone to generating a variety of health-related data.
The use of blockchain technology would allow patients with diabetes, health care providers, and researchers to access patient data from an updated and extensive data pool. In relation to research, this could enable the possibility to find patterns between patient specific features and outcomes, which may lead to a better understanding of diseases and treatments. Blockchain data and access management combined with the use of data lakes could support a wide range of health care data, including data generated by primary and secondary sectors, such as blood samples, vital signs, medical images, diagnoses, and so on. Moreover, the inclusion of patient-generated data, such as data from wearable sensors and patient-reported outcome measures (PROM), could improve the treatment and understanding of patient health.9
From a patient perspective, two major advantages could be highlighted. First, the patient would be in control of his or her data. For instance, an elderly diabetes patient could easily share access to his son so he could view critical information from the hospital as a means for assistance. Second, it will be in the patient’s interest for the cross-intuitional sharing of health data to be a possibility, and with blockchain implementation, it would is also possible to easily share data from home devices.
One of the main improvements in using the blockchain regards the privacy of the patient’s data. The architecture would allow patients to be in power of their own data and to control which entities can access the personal data at a given time. The decentralization of the blockchain with the digitally signed transactions based on strong encryption guarantees that a hacker cannot manipulate with data, shut down the network, or gain access to unencrypted data that can be crucial for patient treatment.
Many challenges not discussed in this work related to implementing blockchain technology in the health care sector exist and should not be neglected. One example is the need for rapid access to personal data during acute treatment of a patient, which could be solved using a trusted third party. Another question involves which data could and should be store in a blockchain. Form a technical perspective, large time series data could be unpractical to store in numerous copies on a blockchain. Therefore, one solution for implementation could be to only use the blockchain for access management and let the data be store in data lakes. This approach seems to fit with the new European GDPR, which is a regulation in EU law on data protection and privacy for all individuals. GDPR aims to give citizens control over their personal data and simplify the regulatory environment. One of the new initiatives states that every citizen has the right to request an institution that stores their personal data to delete these data. However, if health care data would be stored directly on the blockchain, they would be immutable, which could be problematic for complying to the GDPR regulations.
However, using blockchain for health care data and access management has potential comprehensive advantages, and not much research has been conducted in this area. In the coming years, we this technology should be implemented in existing small-scale diabetes health care systems to explore its real-world benefits and challenges.
Appendix
Technology Terminology
API: application programming interface; a set of clearly defined methods for communicating between various software components
Data lake: a method of storing data within a system or repository in its natural format
Hash: a cryptographic hash function with properties that make it suitable for use in cryptography; it is designed to have a one-way function, wherein the output is infeasible to invert
Key: an encryption key used to control an account
Mosaics/assets/tokens: transferable objects on a blockchain; for instance, an ether is a token on the Ethereum blockchain.
Multi-signature: requirement of more than one key to authorize a transaction on the blockchain
Node: a computer or server in a network
Peer-to-peer network: a distributed application architecture that share workloads between peers in the network
Public/private chains: a public blockchain consists of a network, typically thousands of nodes, and everyone can participate
Footnotes
Abbreviations: API, application programming interface; CGM, continuous glucose monitoring; GDPR, General Data Protection Regulation; PROM, patient-reported outcome measures.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Simon Lebech Cichosz  https://orcid.org/0000-0002-3484-7571
https://orcid.org/0000-0002-3484-7571
References
- 1. Cichosz SL, Fleischer J, Hoeyem P, et al. Objective measurements of activity patterns in people with newly diagnosed type 2 diabetes demonstrate a sedentary lifestyle. Diabet Med. 2013;30:1063-1066. [DOI] [PubMed] [Google Scholar]
- 2. Cichosz SL, Fleischer J, Hoeyem P, et al. Assessment of postprandial glucose excursions throughout the day in newly diagnosed type 2 diabetes. Diabetes Technol Ther. 2012;15:78-83. [DOI] [PubMed] [Google Scholar]
- 3. Cichosz SL, Johansen MD, Hejlesen O. Toward big data analytics: review of predictive models in management of diabetes and its complications. J Diabetes Sci Technol. 2016;10(1):27-34. doi: 10.1177/1932296815611680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ivan D. Moving Toward a Blockchain-Based Method for the Secure Storage of Patient Records. healthit.gov. 2016.
- 5. Ge Y, Ahn DK, Unde B, Gage HD, Carr JJ. Patient-controlled sharing of medical imaging data across unaffiliated healthcare organizations. J Am Med Inf Assoc. 2013;20:157-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Walker J, Pan E, Johnston D, Adler-Milstein J, Bates DW. The value of health care information exchange and interoperability. Heal Aff. 2005: 1-3. doi: 10.1377/hlthaff.W5.10 [DOI] [PubMed] [Google Scholar]
- 7. Clifton C, Elmagarmid A, Schadow G, Suciu D. Privacy-Preserving Data Integration and Sharing. New York: ACM; 2004; 19-26. [Google Scholar]
- 8. Linn LA, Koo MB. Blockchain for Health Data and Its Potential Use in Health IT and Health Care Related Research. http://healthit.gov. 2014:1-10.
- 9. Goldwater JC. The use of a blockchain to foster the development of patient-reported outcome measures. Natl Qual Forum. 2016: 1-10. [Google Scholar]
- 10. Nakamoto S. Bitcoin: A Peer-to-Peer Electronic Cash System; 2008:1-9. [Google Scholar]
- 11. Wood G. Ethereum: a secure decentralised generalised transaction ledger; 2017:1-32. [Google Scholar]
- 12. Tapscott D, Tapscott A. Realizing the potential of blockchain a multistakeholder approach to the stewardship of blockchain and cryptocurrencies. World Econ Forum. 2017: 1-45 [Google Scholar]
- 13. Peterson K, Deeduvanu R, Kanjamala P, Boles K. A blockchain-based approach to health information exchange networks. In: Proceedings of the NIST Workshop Blockchain Healthcare Mayo Clinic; 2016:1-10. [Google Scholar]
- 14. Swan M. Blockchain: Blueprint for a New Economy. Sebastopol, CA: O’Reilly Media, Inc; 2015. [Google Scholar]
- 15. Rookie Bloody, Jaguar0625 Gimre, Makoto NEM technical reference. White paper; 2015: 1-54. [Google Scholar]