Abstract
Background
In patients with Normal Glucose Tolerance (NGT) some causes of ischemic heart disease (IHD) were not completely investigated. The role both of metabolic milieu and adipokines in IHD progression was not fully investigated. Our aim was to assess the link between adipokines plasma levels, insulin resistance (IR) and IHD in NGT patients undergoing Percutaneous Coronary Intervention (PCI).
Methods
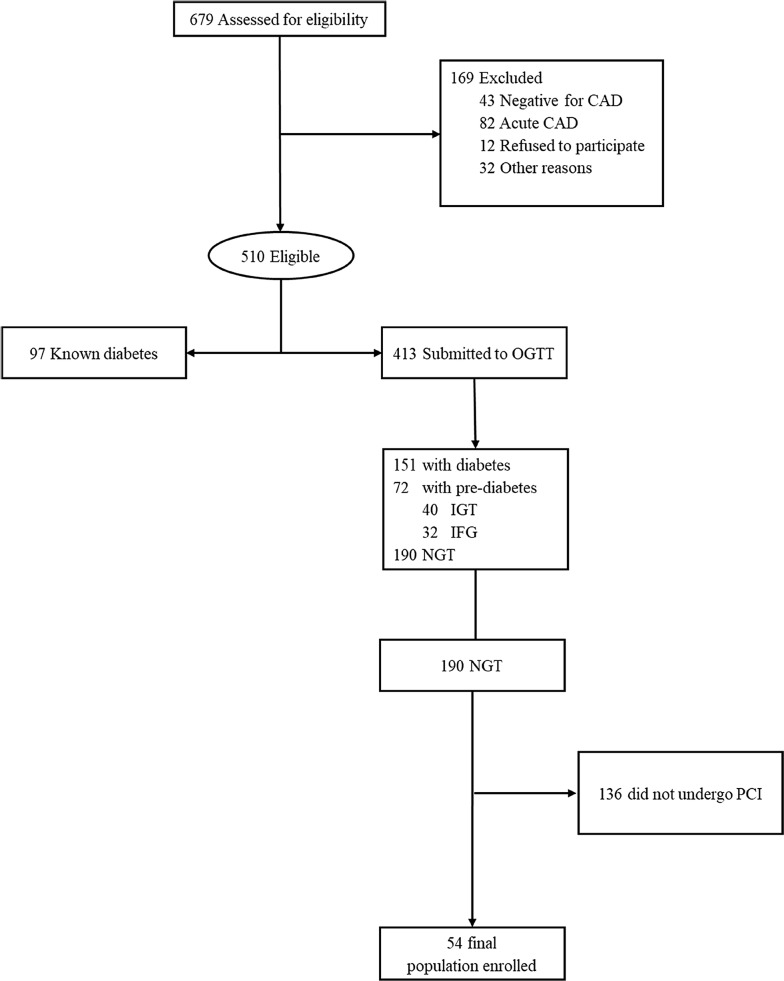
AIRE is a single-center prospective longitudinal observational study investigating the IHD outcome of NGT subjects who underwent coronary revascularization by PCI in a third level cardiology center at A.O. dei Colli Hospital, University of Campania “Luigi Vanvitelli”. Six hundred seventy-nine subjects hospitalized in 2015 for coronary arteriography not suffering from Acute Coronary Syndrome (ACS) in the previous 4 weeks, as well as from all conditions could affect glycemic plasma levels and IR status, were assessed for eligibility. Fifty-four patients with neither history of diabetes nor Altered Fasting Glucose (AFG)/Impaired Fasting Glucose (IGT) after Oral Glucose Tolerance Test (OGTT) were finally enrolled. Primary endpoint was the assessment of the relationship of adipokines and HOMA-IR with the occurrence of restenosis in NGT subjects. As secondary endpoint we assessed the association of the same adipokines and IR with overall ACS events after PCI in NGT subjects.
Results
The 54 NGT patients enrolled were mainly males (85%), with a median age of 60 years [IQR 58–63 years]. Only 4 patients (7.4%) experimented restenosis. Median follow-up was equal to 29.5 months [IQR 14.7–34 months]. Adiponectin levels were independently associated to restenosis (OR 0.206; 95% CI 0.053–0.796; p = 0.000). Instead HOMA-IR and adiponectin appeared independently associated both to de novo IHD (OR 9.6*1013; 95% CI 3.026–3.08*1027; p = 0.042 and OR 0.206; 95% CI 0.053–0.796; p = 0.000, respectively) and overall new PCI (OR 1.5*1011; 95% CI 2.593–8.68*1021; p = 0.042 and OR 0.206; 95% CI 0.053–0.796; p = 0.000, respectively). Moreover, we fixed a potential cut-off for adiponectin for risk of restenosis (≤ 8.5 µg/mL) and overall new PCI (≤ 9.5 µg/mL).
Conclusion
IR and cytokines play a role in progression of any stage of IHD also in NGT subjects. Our results in this setting of patients, though the relatively small sample size, represent a novelty. Future studies on larger populations are needed to analyze more in depth adipokines and insulin resistance role on IHD progression in non-diabetic people.
Electronic supplementary material
The online version of this article (10.1186/s12933-019-0826-0) contains supplementary material, which is available to authorized users.
Keywords: Percutaneous coronary intervention, Insulin resistance, Adipokines, Restenosis, Glucose tolerance
Background
Cardiovascular disease (CVD) represents the most common cause of death among adult people [1]. Therefore, it is important to reassess cardiovascular risk factors and evaluate new strategies to improve CVD prognosis. When considering metabolic risk factors for CVD, emphasis is usually placed on the role played by insulin resistance (IR) [2]. In fact, IR shows a cluster of abnormalities which might increase the risk of ischemic heart disease (IHD) [2].
To date, several studies confirmed the central role played by IR in enhancing the CVD risk in prediabetes and insulin-resistant individuals, with a relative risk approximately twice higher than non-insulin resistant subjects [3–6]. On the other hand, a reduced insulin resistance by altered inflammation/oxidative stress may even be found in patients with Normal Glucose Tolerance (NGT), and they still bear increased risks for cardiovascular disease [7, 8]. Insulin resistance is usually measured through the HOMA IR index, which takes into account both fasting glycemia and insulinemia [9]. Recent analysis of a wide cohort showed substantial similarities in the inflammatory profiles as well as insulin-resistance background associated with DM and CVD, confirming a “common soil” which needs to be investigated also in patients with normal glucose tolerance [10]. Therefore, it is intriguing to evaluate the relationship between inflammation/oxidative stress and cytokines milieu and IHD in NGT patients. In this setting, recent advances established a fundamental role for inflammation as an important component of IHD [11], with a clear association existing between inflammatory cytokines relapsed by adipose tissue, inflammation and atherosclerosis [12–14]. Indeed, adipose tissue secretes many biologically active mediators such as TNF-α, plasminogen activator inhibitor type 1 (PAI-1), IL-6, leptin, adiponectin and resistin [15]. Among these, known as adipokines, particularly adiponectin seems to be directly connected to IHD [16]. Intriguingly, adiponectin is the unique adipokine exclusively secreted from adipose tissue which improves insulin sensitivity and favorably modulates the endothelial inflammatory response to vascular injury [17]. Through its insulin-sensitizing, anti-inflammatory and anti-atherogenic properties, lower plasma levels of adiponectin can be therefore IHD independent predictors [18, 19]. Thereafter, most recent studies on NGT patients showed that neointimal tissue proliferation after Percutaneous Coronary Intervention (PCI) was greater in Impaired Glucose Tolerant (IGT) patients than in NGT patients at follow-up, and that the best predictor of restenosis was insulin level after oral glucose tolerance test (OGTT) [20, 21]. Finally, as relationship between type 2 diabetes mellitus (T2DM) and IR/adipokines has been widely investigated, our attention was focused on NGT patients. Therefore, aim of this paper was to assess the link between adipokines plasma levels, insulin resistance and IHD in NGT patients undergoing PCI, and particularly the relationship between adipokines/IR and restenosis, as well as overall Acute Coronary Syndrome (ACS) after PCI.
Methods
Design of the study
A single center prospective longitudinal observational study investigated the IHD outcome of NGT subjects who underwent coronary revascularization by PCI. Inclusion criteria were: age > 18 years, elective indication to receive a PCI in patients with suspect of IHD. Instead, subjects were considered not eligible if they suffered from Acute Coronary Syndrome (ACS) in the previous 4 weeks, in the case of recent steroid administration (last 3 months), and chronic inflammatory diseases (all these conditions could affect glycemic plasma levels as well as IR). Moreover, alcohol or drug assumption, known psychiatric/neoplastic diseases were further exclusion criteria, as well as known DM, altered fasting glycaemia (AFG) or an Impaired Glucose Tolerance (IGT) response at standard OGTT.
The study consisted in two phases. During the screening/enrollment phase, all patients hospitalized in a third level cardiology center at the A.O. dei Colli Hospital, University of Campania “Luigi Vanvitelli” in Naples for an elective coronary angiography for suspected IHD in 2015 were evaluated for eligibility. Eligible patients underwent OGTT, with blood samples taken at time 0′ and 120′ after oral 75 grams glucose administration for plasma glucose and insulin assay, as well as glycated hemoglobin (HbA1c), total HDL/cholesterol, triglycerides, creatinine, adiponectin, resistin and TNF-alpha dosage. To avoid potential influences on cytokines and IR, coronary angiography in election was performed at least 24 h after blood sampling. Only subjects with neither history of diabetes nor AFG/IGT after OGTT were enrolled in the study. Moreover, from enrollment and during entire follow-up all patients were under optimized medical therapy: ACE inhibitors, beta-blockers, statin and antiplatelets. The follow-up phase, instead, consisted in periodically scheduled visits after 3, 6 and 12 months from PCI. During each visit, anamnestic data, blood pressure and standard ECG were recorded. In addition, at 12 months patients also underwent cardiological examination (stress test) and blood sampling. Subsequently, the follow-up was annually performed clinically or by phone. A new coronary angiography at follow-up was performed in the case of new symptoms onset or evidence of ischemia/coronary disease progression at non-invasive imaging tests (including stress test or coronary computed tomography angiography). The use of additional invasive tests to assess coronary lesions characteristic (quantitative coronary analysis [QCA], intravascular ultrasound [IVUS], optical coherence tomography [OCT], fractional flow reserve [FFR]) was strongly recommended, but left to the discretion of the operator. All subjects gave written informed consent to participate to the study. The protocol was approved by the Ethical Committee of University of Campania.
Endpoints of the study
Primary endpoint was the assessment of the relationship of adipokines, particularly adiponectin, resistin and TNF-alpha, and IR with the occurrence of clinically-driven target lesion revascularization due to in-stent restenosis (TLR-IS) in NGT subjects. TLR-IS was defined as either repeat percutaneous or surgical revascularization for a lesion anywhere within the stent, including focal, extended, totally occluding lesions.
As secondary endpoint, instead, we assessed the association of the same adipokines and IR with overall ACS events after PCI in NGT subjects (re-PCI and new PCI).
PCI procedure
PCI was performed according to the current AHA/ACC guidelines [22], through radial or femoral approach using small size arterial sheaths. The analyses of all angiographic data were performed by interventional cardiologists and followed by PCI with angioplasty and drug eluting stent (DES) in case of critical angiographic stenosis [23]. Informed consent was obtained from each patient before coronary angiography. All patients received heparin (50 IU/kg intravenously) before the PCI. Angiographic lesion morphology was classified according to the AHA/ACC classification [22]. All PCIs were performed with second generation DES implantation. At clinical follow-up the restenosis was treated either with balloon angioplasty or new DES implantation, whilst PCI of new stenosis was performed exclusively with DES. All patients were on aspirin (100 mg daily) and clopidogrel (75 mg daily for 12 months) treatment after coronary artery stenting.
Biochemical assays
ELISA tests
Plasma samples were collected using either heparin or EDTA as anticoagulant. They were centrifuged for 15 min at 1000×g within 30 min of collection and stored at − 20 °C until assayed. Plasma TNF-alpha and adiponectin levels were determined using commercially available human ELISA tests, from R&D systems (D6050, DTA00 and DRP300 respectively, Abingdon, UK) and following the manufacturer’s instructions; whilst plasmatic resistin levels with a commercially human ELISA assay from Ray Biotechinc (ELH-Resistin-1 Norcross, GA). These kits show negligible cross-reactivity (< 0.5%) and high sensitivity (detection limit 0.891 ng/mL for adiponectin; 2 pg/mL for resistin and 5.5 pg/mL for TNF-alpha, data by the manufacturer).
Statistical analysis
Categorical variables were presented as number and percentages, whilst continuous variables were instead presented as median and interquartile range [IQR]. The normal/not normal distribution was preliminarily assessed through a Kolmogorov–Smirnov Goodness-of-Fit K-S test. Categorical variables were compared using the Chi square test, as the sample size was > 50 subjects, while the Mann–Whitney U Test and the Wilcoxon test were used for continuous variables. All variables emerged as significant at the univariate analysis were furtherly included in a logistic regression model to assess if there was a parameter independently associated with the occurrence of coronary events, adjusting for HbA1c, hypertension, smoke and age. The risk of re-PCI/new PCI was analyzed using the Kaplan–Meier (K–M) method, and the log-rank test was used to compare the cumulative risk between the two groups. A two-sided probability P value < 0.05 was considered statistically significant. In addition, ROC Curves were performed in order to find a potential cut-off for the three cytokines analyzed (TNF-alpha, resistin and adiponectin). The found cut-offs were used to dichotomize the cytokines and perform a further K–M analysis in order to assess the risk of PCI according to the level of each cytokine. All analyses were performed using SPSS statistical software (Version 24.0, SPSS Chicago, Il, USA)and R software (CRAN ® 3.3.4).
Results
General characteristics and follow-up of the study population
Six hundred seventy-nine subjects hospitalized for coronary arteriography were assessed for eligibility, 169 did not meet inclusion criteria. Among the 510 eligible, 97 were excluded due to diabetes mellitus (DM) history and 223/413 after OGTT (151 DM and 72 pre-DM). Therefore, only 190 were found NGT. However, due to the mandatory inclusion criteria, 136 NGT were further excluded, for a final enrolled population of 54 patients (Fig. 1). Anthropometric, clinical and biochemical characteristics are shown in Table 1. In particular, they were mainly males (46 cases; 85%), with a median age of 60 years [IQR 58–63 years] and a median BMI of 27 kg/m2 [IQR 25.5–28.1 kg/m2]. All patients presented a median fasting glycemia at baseline equal to 87 mg/dL [IQR 80–90.2 mg/dL], a median glycated hemoglobin (HbA1c) of 5.2% [IQR 5.1–5.5%] and the 80% were smokers. Median follow-up was equal to 29.5 months [IQR 14.7–34 months]. In 4 patients we observed the occurrence of re-stenosis (median time-from-event: 8.5 months [IQR 4–15.75 months]). Three patients with restenosis of previous PCI of LAD and one case of restenosis of right coronary artery were observed. Two of these restenosis of LAD involving DES implanted in long lesion of distal part of coronary with diameter 2.5 mm. The other restenosis of LAD involving a previous DES implantation in bifurcation with diagonal branch, while the only restenosis of right coronary artery involving previous PCI in distal part of coronary with small diameter. Of note, no stent thrombosis occurred during follow-up. In five cases, instead, de novo coronary lesions were reported at coronary angiography during follow-up, and in one case treated with PCI. All new stenosis were focal lesions significantly worse than those found in the previous coronary angiography (median time from event: 29 months [IQR 12–33.5 months]). All new PCI were performed either after positive echo-stress or in case of an ACS. Moreover, three subjects suffering from angina with no troponin elevation nor echo-stress with signs of inducible ischemia did not undergo PCI and were strictly clinically followed. None subject experienced different major cardiovascular events (CV death, fatal or no fatal stroke, amputation). Overall death was equal to the 2% (1 case), due to lung cancer.
Fig. 1.
Flow-chart of the study
Table 1.
General characteristics at baseline and clinical findings during follow-up of the study population (n = 54)
| Parameter | |
|---|---|
| Age (years), median [IQR] | 60 [58–63] |
| Sex, no. (%) | |
| M/F | 46 (85)/8 (15) |
| BMI, kg/m2, median [IQR] | 27 [25.5–28.1] |
| Blood pressure (mmHg), median [IQR] | |
| Systolic | 130 [120–131.2] |
| Diastolic | 80 [70–80] |
| Hypertension, no. (%) | 15 (28) |
| Smoke, no. (%) | 43 (80) |
| Cholesterol (mg/dL), median [IQR] | |
| Total | 172 [149.5–189] |
| HDL | 42.5 [35–51] |
| LDL | 103 [68–128] |
| Triglycerides (mg/dL), median [IQR] | 127 [105.2–151.5] |
| Glycemia (mg/dL), median [IQR] | |
| Baseline | 87 [80–90.2] |
| 2 h | 109 [93–126.7] |
| Glycated hemoglobin (%), median [IQR] | 5.2 [5.1–5.5] |
| Insulin (µU/mL), median [IQR] | 3.8 [3–6] |
| HOMA IR, median [IQR] | 0.78 [0.59–1.31] |
| Creatinine (mg/dL), median [IQR] | 1 [0.87–1.1] |
| Hemoglobin (mg/dL), median [IQR] | 14.3 [13.3–15.2] |
| Adiponectin (µg/mL), median [IQR] | 11 [9.7–13.2] |
| Adiponectin, no. (%) | |
| Pathologic | 13 (24) |
| Resistin (ng/mL), median [IQR] | 7 [4–9] |
| Resistin, no. (%) | |
| Pathologic | 8 (15) |
| TNF-alpha (ng/mL), median [IQR] | 8.5 [7–11] |
| TNF-alpha, no. (%) | |
| Pathologic | 6 (11) |
| Site of stenosis at first PCI, no. (%) | |
| IVA | 25 (46) |
| CX | 10 (19) |
| DX | 19 (35) |
| Follow-up duration (months), median [IQR] | 29.5 [14.7–34] |
| Re-PCI, no. (%) | 4 (7) |
| Time re-PCI, median [IQR] | 8.5 [4–15.75] |
| Site of re-PCI, no. (%) | |
| IVA | 3 (75) |
| CX | 0 (−) |
| DX | 1 (25) |
| New PCI, no. (%) | 5 (9) |
| Time new PCI, median [IQR] | 29 [IQR 12–33.5] |
| Site of new-PCI, no. (%) | |
| IVA | 2 (40) |
| CX | 1 (20) |
| DX | 2 (40) |
| Death, no. (%) | |
| Cardiovascular/other causes | − /1 (2) |
Restenosis risk assessment: a univariate and multivariate analysis
We assessed the distribution of the collected variables according to the occurrence or not of restenosis. At univariate analysis, restenosis events resulted significantly associated with higher levels of insulin (median 9.8 µU/mL vs 3.6 µU/mL; p = 0.003) and HOMA-IR (median 2.23 vs 0.75; p = 0.003), as well as higher glucose levels at 120 min (median 132.5 mg/dL vs 106 mg/dL; p = 0.021). Higher TNF-alpha levels revealed significantly associated with the development of restenosis (median 18.5 ng/mL vs 8 ng/mL; p = 0.008); the same in the case of lower adiponectin values (median 7 vs 11.5 µg/mL; p = 0.000). As expected, also time-from-event was significantly lower in subjects who experimented re-PCI (median 8.5 vs 29.5 months; p = 0.019). Only adiponectin levels demonstrated independently associated at the multivariate analysis (OR 0.206; 95% CI 0.053–0.796; p = 0.000). We also performed ROC Curves (Additional file 1: Fig. S1—upper panel) to find a potential cut-off for the three cytokines analyzed. For adiponectin, the AUROC was highly accurate (AUROC 0.965; p = 0.002; 95% CI 0.913–1.000) and allowed us to fix a potential cut-off at8.5 µg/mL (sensitivity 100%; specificity 90%), hence, values ≤ 8.5 µg/mL could be considered pathological. Resistin AUROC was instead equal to 0.730, not reaching the statistical significance. Instead, TNF-alpha AUROC was 0.878 (p = 0.013; 95% CI 0.709–1.000) and the found cut-off was around 14 ng/mL (sensitivity 75%; specificity ≈ 94%). Values > 14 ng/mL could hence be defined as pathological. Thus, we dichotomized adiponectin and TNF-alpha and performed a K–M analysis to evaluate the cumulative risk of restenosis according to the level of cytokine. For both the cytokines analyzed the log-rank p was highly statistically significant (p = 0.000) (Fig. 2—upper panel).
Fig. 2.
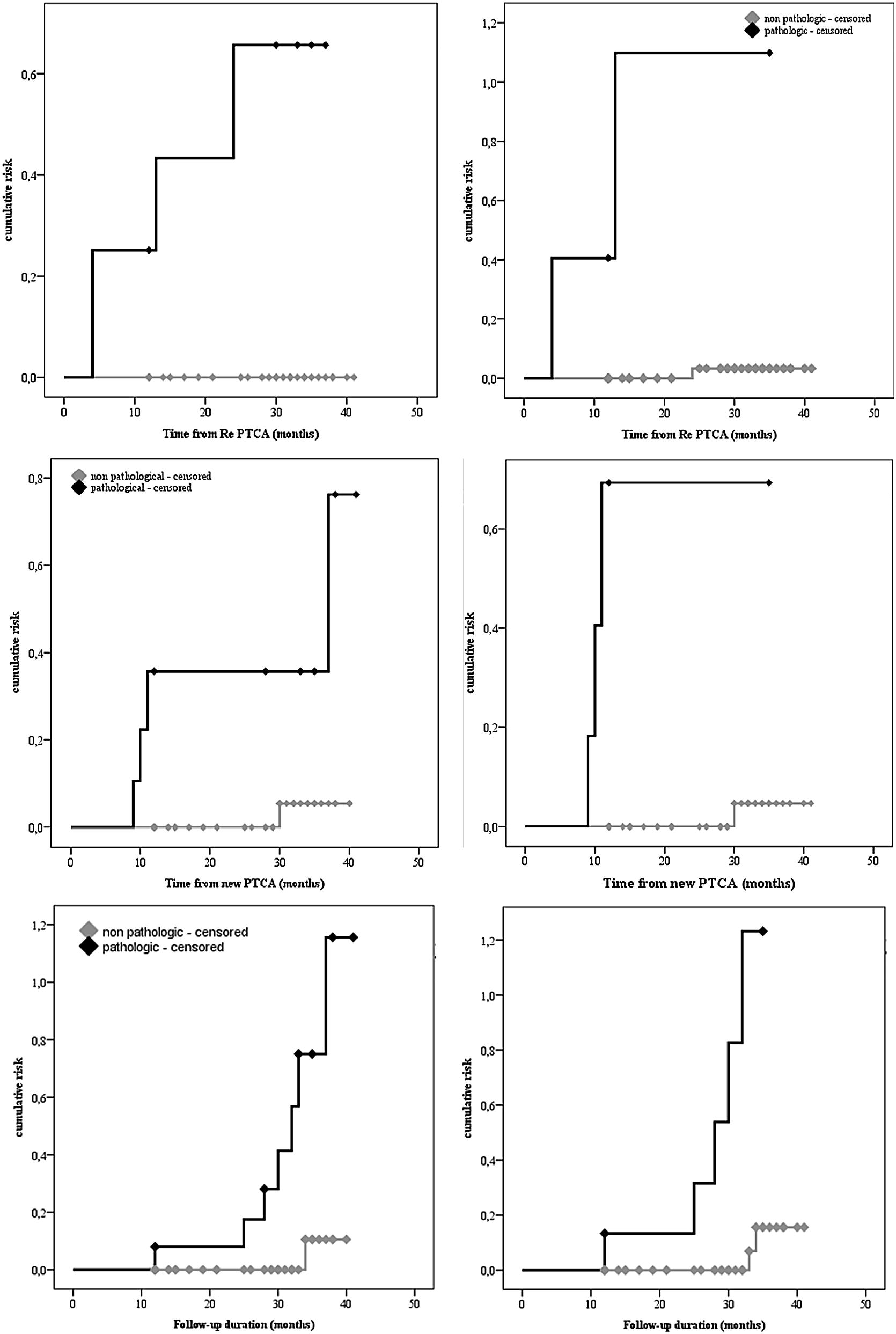
(Upper panel) K–M curves describing the risk of re-stenosis according to the values of the analyzed cytokines. Respectively adiponectin (left) and TNF-alpha (right). (Central panel) K–M curves describing the risk of new stenosis according to the values of the analyzed cytokines. Respectively adiponectin (left), resistin (right). (Lower panel) K–M curves describing the risk of any coronary event according to the values of the analyzed cytokines. Respectively adiponectin (left), resistin (right)
Risk assessment of de novo IHD: a univariate and multivariate analysis
We also assessed the occurrence or not of new stenosis, excluding patients who had restenosis (n = 51). At the univariate analysis de novo IHD revealed significantly associated with higher levels of insulin (median 9.8 µU/mL vs 3.5 µU/mL; p = 0.008) and HOMA-IR (median 2.34 vs 0.74; p = 0.012), as well as higher glucose levels both at baseline and at 120 min (median 97 mg/dL vs 86.5 mg/dL; p = 0.038 and median 135 mg/dL vs 102.5 mg/dL; p = 0.045, respectively) and HbA1c levels (median 5.6% vs 5.2%; p = 0.001). Differently from restenosis risk, higher levels of TNF-alpha did not reveal significantly associated with the development of new; conversely in the case of higher resistin levels (median 15 ng/mL vs 6 ng/mL; p = 0.012) and in the case of lower values of adiponectin (median 8 vs 12 µg/mL; p = 0.001). Only HOMA-IR (OR 9.6*1013; 95% CI 3.026–3.08*1027; p = 0.042) and adiponectin appeared independently associated at the multivariate analysis (OR 0.206; 95% CI 0.053–0.796; p = 0.000). All data are shown in Additional file 2: Table S1. Also in this case we performed ROC Curves (Additional file 1: Fig. S1—central panel). Adiponectin AUROC expressed a high accuracy (AUROC 0.911; p = 0.003; 95% CI 0.814–1.000), hence we fixed a potential cut-off of 9.5 (sensitivity 80%; specificity 87%); hence, values ≤ 9.5 could be considered pathological. TNF-alpha AUROC was equal to 0.607 and did not reach the statistical significance; instead, for resistin AUROC was 0.833 (p = 0.015; 95% CI 0.555–1.000) and the found cut-off around 10.5 (sensitivity 80%; specificity ≈ 96%). Values > 10.5 could hence be defined as pathological. Dichotomized adiponectin and resistin were analyzed by a K–M analysis to evaluate the cumulative risk of new stenosis. For both the cytokines the log-rank p reached a high statistical significance (log-rank p = 0.002 and log-rank p = 0.000, respectively) (Fig. 2—central panel) (Table 2).
Table 2.
Characteristics of the study population, according to the occurrence or not of restenosis (n = 54)
| Parameter | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|
| Re-PCI | p | OR [95% CI] | p | ||
| Yes (n = 4) | No (n = 50) | ||||
| Age (years), median [IQR] | 59.5 [58.2–60.7] | 60 [57.7–63] | 0.714 | ||
| Sex, no. (%) | 0.386 | ||||
| M | 4 (100) | 42 (84) | |||
| F | 0 (−) | 8 (16) | |||
| BMI, kg/m2, median [IQR] | 25.3 [24.8–26.7] | 27.2 [25.8–28.1] | 0.159 | ||
| Blood pressure (mmHg), median [IQR] | |||||
| Systolic | 130 [115–137.5] | 130 [120–131.2] | 1.000 | ||
| Diastolic | 80 [72.5–80] | 80 [70–80] | 0.714 | ||
| Hypertension, no. (%) | 1 (25) | 14 (28) | 0.897 | ||
| Smoke, no. (%) | 4 (100) | 39 (78) | 0.293 | ||
| Cholesterol (mg/dL), median [IQR] | |||||
| Total | 157 [147.5–180.7] | 174.5 [147.5–192] | 0.555 | ||
| HDL | 34.5 [31.7–41] | 43 [35–51.2] | 0.066 | ||
| LDL | 90.5 [86–116] | 109 [70.2–122.5] | 0.874 | ||
| Triglycerides (mg/dL), median [IQR] | 141.5 [121.5–166.7] | 125.5 [103–151.5] | 0.327 | ||
| Glycemia (mg/dL), median [IQR] | |||||
| Baseline | 93.5 [86.2–102.2] | 87 [79.7–90] | 0.066 | ||
| 2 h | 132.5 [117.7–136.7] | 106 [93–123] | 0.021 | ||
| Glycated hemoglobin (%), median [IQR] | 5.6 [5.3–5.8] | 5.2 [5–5.5] | 0.051 | ||
| Insulin (µU/mL), median [IQR] | 9.8 [9.4–10] | 3.6 [2.8–4.7] | 0.003 | ||
| HOMA IR, median [IQR] | 2.23 [2.1–2.4] | 0.75 [0.57–0.97] | 0.003 | ||
| Creatinine (mg/dL), median [IQR] | 1 [1–1.16] | 1 [0.8–1.1] | 0.266 | ||
| Hemoglobin (mg/dL), median [IQR] | 14.2 [13.2–14.5] | 14.3 [13.3–15.2] | 0.534 | ||
| Adiponectin (µg/mL), median [IQR] | 7 [6–8] | 11.5 [10–14] | 0.000 | 0.206 [0.053–0.796] | 0.022 |
| Resistin (ng/mL), median [IQR] | 13 [5.2–15.5] | 6.5 [4–8.2] | 0.137 | ||
| TNF-alpha (ng/mL), median [IQR] | 18.5 [11–20.7] | 8 [7–10] | 0.008 | ||
| Time RE-PCI, median [IQR] | 8.5 [4–21.2] | 29.5 [13.5–34] | 0.019 | ||
| Follow-up duration (months), median [IQR] | 30 [25.7–32.7] | 29.5 [13.5–34] | 1.000 | ||
| Death, no. (%) | |||||
| Cardiovascular/other causes | 0 (−)/− | 0 (−)/1 (2) | 0.775 | ||
Risk assessment of overall new PCI: a univariate and multivariate analysis
Finally, we assessed the overall occurrence or not of coronary events. At the univariate analysis coronary events resulted significantly associated with higher levels of insulin (median 9.8 vs 3.5 µU/mL; p = 0.000) and HOMA-IR (median 2.23 vs 0.74; p = 0.000), as well as higher glucose levels both at baseline and at 120 min (median 95.5 vs 86.5 mg/dL; p = 0.015 and 132 vs 102.5 mg/dL; p = 0.007) and HbA1c levels (median 5.6% vs 5.2%; p = 0.001). Higher levels of resistin revealed significantly associated with the development of coronary events (median 13 vs 6 ng/mL; p = 0.013); the same in the case of lower adiponectin values (median 8 vs 12 µg/mL; p = 0.000). At the multivariate analysis HOMA IR (OR 1.5*1011; 95% CI 2.593–8.68*1021; p = 0.042) and adiponectin levels appeared independently associated (OR 0.206; 95% CI 0.053–0.796; p = 0.000). All data are shown in Table 3. Even in this case, we performed ROC Curves (Additional file 1: Fig. S1—lower panel). For adiponectin, the AUROC expressed a high accuracy (AUROC 0.931; p = 0.000; 95% CI 0.857–1.000) and we fixed a potential cut-off at 9.5 µg/mL (sensitivity 87.5%; specificity 87%), with values ≤ 9.5 µg/mL considered as pathological. For what concerns TNF-alpha the AUROC was 0.700 and did not reach the statistical significance; instead resistin AUROC was 0.772 (p = 0.015; 95% CI 0.513–1.000) and we fixed the cut-off at 10.5 ng/mL (sensitivity 75%; specificity ≈ 96%). Values > 10.5 ng/mL could hence be defined as pathological. Thus, we dichotomized both cytokines and performed a K–M analysis, with respect to the entire follow-up period, to evaluate the cumulative risk of coronary events. For both the log-rank p reached a high statistical significance (log-rank p = 0.001 and log-rank p = 0.000, respectively) (Fig. 2—lower panel).
Table 3.
Characteristics of the study population, according to the occurrence or not of overall new PCI (for restenosis and de novo IHD) (n = 54)
| Parameter | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|
| Overall new PCI | p | OR [95% CI] | p | ||
| Yes (n = 8) | No (n = 46) | ||||
| Age (years), median [IQR] | 59.5 [58–60.7] | 60.5 [57.7–63] | 0.590 | ||
| Sex, no. (%) | 0.380 | ||||
| M | 6 (75) | 40 (87) | |||
| F | 2 (25) | 6 (13) | |||
| BMI, kg/m2, median [IQR] | 26.7 [24.8–28.8] | 27 [25.8–28] | 1.000 | ||
| Blood pressure (mmHg), median [IQR] | |||||
| Systolic | 125 [120–130] | 130 [120–136.2] | 0.296 | ||
| Diastolic | 80 [72.5–80] | 80 [70–80] | 0.574 | ||
| Hypertension, no. (%) | 1 (14) | 14 (30) | 0.296 | ||
| Smoke, no. (%) | 7 (88) | 36 (78) | 0.549 | ||
| Cholesterol (mg/dL), median [IQR] | |||||
| Total | 173.5 [147.5–209.7] | 172.5 [146.2–189] | 0.658 | ||
| HDL | 44 [34.2–64.5] | 42 [35–51] | 0.590 | ||
| LDL | 107.5 [86–123.7] | 105 [70.2–119.7] | 0.765 | ||
| Triglycerides (mg/dL), median [IQR] | 127.5 [117.2–157.7] | 127 [102.7–151.5] | 0.495 | ||
| Glycemia (mg/dL), median [IQR] | |||||
| Baseline | 95.5 [86.2–97.7] | 86.5 [79.7–89.2] | 0.015 | 0.643 [0.389–1.064] | 0.086 |
| 2 h | 132 [116–136.7] | 102.5 [93–121.2] | |||
| Glycated hemoglobin (%), median [IQR] | 5.6 [5.5–5.7] | 5.2 [5–5.4] | 0.001 | ||
| Insulin (µU/mL), median [IQR] | 9.8 [9.1–10.1] | 3.5 [2.8–4.3] | 0.000 | 0.008 [0.000–1.183] | 0.058 |
| HOMA IR, median [IQR] | 2.23 [2.1–2.5] | 0.74 [0.57–0.94] | 0.000 | 1.5*1011 [2.593–8.68 * 1021] | 0.042 |
| Creatinine (mg/dL), median [IQR] | 1 [0.85–1.1] | 1 [0.87–1.1] | 0.971 | ||
| Hemoglobin (mg/dL), median [IQR] | 14.2 [13.2–14.8] | 14.3 [13.3–15.3] | 0.495 | ||
| Adiponectin (µg/mL), median [IQR] | 8 [6.5–8.7] | 12 [10–14] | 0.000 | 0.206 [0.053–0.796] | 0.022 |
| Resistin (ng/mL), median [IQR] | 13 [6–15] | 6 [4–8] | 0.013 | ||
| TNF-alpha (ng/mL), median [IQR] | 13 [7.5–20.7] | 8 [7–10] | 0.073 | ||
| Follow-up duration (months), median [IQR] | 31 [25.7–33.7] | 29 [13.5–34] | 0.558 | ||
| Death, no. (%) | |||||
| Cardiovascular/other causes | 0 (−)/− | 0 (−)/1 (2) | 0.674 | ||
Discussion
It is well known that coronary artery disease progresses more rapidly in diabetic subjects. In particular insulin treated diabetes is an independent and strong predictor of late and repeat coronary revascularization [24]. Intriguingly, in the general population treated with PCI, insulin resistance promoted the “late catch-up phenomenon”, a restenosis due to continuous neointimal growth during long-term follow-up, after first generation DES implantation [25]. Indeed, the Casale Monferrato study suggested that, insulin resistance was associated to natriuretic peptides serum levels, with lower circulating levels in insulin-resistance non diabetic people, and higher values in the upper spectrum of metabolic abnormalities, such as diabetes with the metabolic syndrome [26]. These findings seem indirectly to be confirmed by the observation that in patients undergoing elective PCI, pioglitazone, an insulin-sensitizer drugs, improved cardiometabolic profiles. In particular, pioglitazone increased adiponectin and reduced plasma levels of natriuretic peptides [27]. Therefore, growing evidences indicate that adiposity and impaired glycemia levels importantly contribute to IHD even in non-diabetic individuals [28]. To date, visceral as well as epicardial adiposity are related to ischemic heart diseases through secretion of adipokines and pro-inflammatory factors from adipocytes [29]. Actually, the role of adipokines on IHD in NGT subjects is still not well-known. In a previous cross-sectional study, both number of stenosed coronary arteries and coronary damage score were found independently associated to fasting and post load insulin and HOMA in NGT subjects [7]. Moreover, the present study refers to a longitudinal analysis on non-obese NGT patients submitted to PCI. In this setting, we observed that metabolic and inflammatory factors are significantly related to relapse of new PCI, due to both restenosis and de novo stenosis. Restenosis constitutes an important limitation after stent implantation, but its pathogenesis is not yet fully understood. Several studies showed increased HOMA-IR levels as an important prognostic indicator in non-diabetic patients who underwent PCI [30–32]. Free survival from IHD in non-diabetic patients treated with primary PCI is significantly correlated with plasma glucose levels at admission [33], and elevated glucose levels on admission are associated with an adverse prognosis in patients with STEMI treated with PCI [34]. On the other hand, the metabolic milieu and, above all, IR and cytokines levels are strongly influenced by the adrenergic stress and inflammatory status occurring during an ACS. Therefore, glucose tolerance, IR and cytokines levels during ACS are not representative of their status before and a few days after an ACS. These last conditions could similarly impact the CV outcome in subjects with IHD (Additional file 3: Table S2).
In non-diabetic patients, neointimal tissue proliferation after stent implantation is greater in IGT patients than in NGT patients at 6 months of follow-up. Moreover, higher insulin and HOMA levels are suggested as the best predictors of restenosis [35]. More recently, insulin resistance was associated with in-stent restenosis in no diabetic patients undergoing coronary DES implantation at long-term angiographic follow-up [36]. Some reports investigated the significance of serum adiponectin levels in predicting clinical outcomes after PCI. These studies demonstrated that, in male patients with acute myocardial infarction (AMI), adiponectin blood concentration was independently predictive of AMI during a 1-year follow-up after primary PCI [21]. Originally, our study suggests that pre-procedural lower expression of adiponectin may be an independent predictor of major cardiovascular events after PCI. In particular, patients with significantly lower pre-procedural adiponectin serum levels had higher rate of AMI than those with higher levels. Univariate analysis suggests that risk of restenosis in patients with NGT was significantly associated with higher levels of insulin and HOMA-IR. Moreover, higher TNF-alpha levels revealed significantly associated with the development of restenosis, and the same occurred in the case of lower values of adiponectin. However, only adiponectin levels appear independently associated with the occurrence of restenosis at the multivariate analysis. This last finding is most likely due to the small sample size of our population. Overall new PCI (restenosis and de novo IHD) emerged significantly associated with higher levels of insulin and HOMA-IR, whilst higher levels of resistin were significantly associated with the development of coronary events, and the same in the case of lower adiponectin values. At the multivariate analysis, HOMA IR and adiponectin levels revealed independently associated. Our findings are consistent with An et al. who found IR as an independent predictor of atherosclerosis plaque progression in patients with IHD, both in DM and non-DM patients [37]. Since adiponectin has insulin-sensitizing, anti-inflammatory and anti-atherogenic properties, low plasma levels of adiponectin can be therefore independent predictors of IHD, and platelet activation in carotid atherosclerosis both in diabetic and non-diabetic subjects [38–41]. In addition, excessive inflammatory coronary responses may be related to a lack of this adipocytokine [19, 42, 43]. Moreover, adiponectin revealed as a potential biological marker for restenosis in T2DM patients and, in this sense, it has been tried to find a possible cut-off (plasma adiponectin levels ≥ 6.0 µg/mL) associated with a lower risk of restenosis both in diabetic and non-diabetic subjects [44]. In the general population, none cut-off has been found yet. However, it has been recently demonstrated an association between lowest adiponectin serum levels and an increased risk of restenosis due to endothelium functions impairment [45]. Actually, no data is available in NGT people about resistin role on atherosclerosis development. To date, only few studies show that resistin levels are correlated with cardiovascular death in patients with documented IHD, i.e. unstable angina and myocardial infarction [19]. Intriguingly, it was demonstrated that resistin levels are associated with increased restenosis rates in diabetic patients with IHD after successful coronary stenting [46]. Indeed, pre-procedural serum resistin concentrations were higher in the restenosis group rather than in the patients without restenosis [46]. This association was found in the general population too. Originally, our data, included in a Kaplan–Meier analysis, showed a statistically significant association between pathological values of the cytokines and a higher risk of overall new PCI in NGT. Finally, results from our study are also useful to remark how the use optimal medical therapy, including potent antiplatelet agents, should be implemented in patients undergoing PCI as they have proven to be of benefit regardless of concomitant risk factors or glycemic/diabetic status [47].
Study limitations
This study presents several limitations. First of all, we have to mention the small sample size of our population, which affects the results of the multivariate analysis. To date, this might be particularly evident for what concerns HOMA-IR index, which loses of significance at the multivariate analysis. Actually, the sample size might be justified by the difficult to find higher numbers of patients NGT subjects who underwent coronary revascularization by PCI for IHD. Another study limitation is the short duration of 2.5 years of follow-up. This might be a limiting factor to assess at longer follow up duration the important clinical effects of the present study analysis. On the other hand, the overall assessment of new PCI seems to strengthen our results and confirm previous cross-sectional studies in NGT subjects.
Conclusions
In conclusion, our findings strongly support the role of IR and cytokine in progression of any stage of IHD also in people without a metabolic disease (diabetes or prediabetes) as NGT subjects. Future studies are needed to analyze more in depth and on larger populations the role of adipokines and IR on IHD progression in non-diabetic people. In particular, a pharmacological treatment of this metabolic and inflammatory milieu should be studied in order to try to improve the CV outcomes of these large setting of patients.
Additional files
Additional file 1: Figure S1. Definition of the best cut-off level of ROC curves respectively for adiponectin (a), resistin (b) and TNF-alpha (c), according to the risk of restenosis. (Central panel) Definition of the best cut-off level of ROC curves respectively for adiponectin (a), resistin (b) and TNF-alpha (c), according to the risk of new stenosis. (Lower panel) Definition of the best cut-off level of ROC curves respectively for adiponectin (a), resistin (b) and TNF-alpha (c), according to the risk of any coronary event.
Additional file 2: Table S1. Characteristics of the study population, according to the occurrence or not of PCI for de novo IHD (n = 51).
Additional file 3: Table S2. Adiponectin and HOMA-IR values for the patients who experimented restenosis.
Authors’ contributions
Conception and design: FCS, Analysis and interpretation of the data: FCS, PCP, MD, FF. Drafting of the article: FCS, PCP. Critical revision for important intellectual content: FCS, PCP, RM, PC, CS, LP, FF, GE, TS, LEA. Provision of study materials or patients: FCS, FP, FF, Statistical expertise: PCP. Collection and assembly of data: PCP, PC, FF, RG, LR, FG. Obtaining of funding: FCS. Administrative, technical, or logistic support: PC, FP, FF, GE. Final approval of the article: FCS, PCP, RM, PC, CS, LP, FF, GE, RG, FG, LR, TS, MD, LEA. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The authors declare that the data supporting the findings of this study are available within the article and its additional files.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study protocol was approved by the Ethical Committee of University of Campania (No = 189/2015). All subjects gave written informed consent to participate to the study.
Funding
University founding source supported the study. It had no role in study’s design, conduct, and reporting.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- CVD
cardiovascular disease
- IR
insulin resistance
- IHD
ischemic heart disease
- NGT
normal glucose tolerance
- PAI-1
plasminogen activator inhibitor type 1
- PCI
percutaneous coronary intervention
- OGTT
oral glucose tolerance test
- T2DM
type 2 diabetes mellitus
- DM
diabetes mellitus
- ACS
Acute Coronary Syndrome
- AFG
altered fasting glycaemia
- IGF
impaired glucose tolerance
- DES
drug eluting stent
- IQR
interquartile range
- K–M
Kaplan–Meier
- HbA1c
glycated hemoglobin
- AMI
acute myocardial infarction
Contributor Information
Ferdinando Carlo Sasso, Phone: +39 081 566 5010, Email: ferdinandocarlo.sasso@unicampania.it.
Pia Clara Pafundi, Email: piaclara.pafundi@unicampania.it.
Raffaele Marfella, Email: raffaele.marfella@unicampania.it.
Paolo Calabrò, Email: paolo.calabro@unicampania.it.
Federico Piscione, Email: fpiscione@unisa.it.
Fulvio Furbatto, Email: ffurbatto@hotmail.com.
Giovanni Esposito, Email: giovanni.esposito2@unina.it.
Raffaele Galiero, Email: raffaele_ga@outlook.it.
Felice Gragnano, Email: felice.gragnano@unicampania.it.
Luca Rinaldi, Email: luca.rinaldi@unicampania.it.
Teresa Salvatore, Email: teresa.salvatore@unicampania.it.
Michele D’Amico, Email: michele.damico@unicampania.it.
Luigi Elio Adinolfi, Email: luigielio.adinolfi@unicampania.it.
Celestino Sardu, Email: celestino.sardu@unicampania.it.
References
- 1.Yazdanyar A, Newman AB. The burden of cardiovascular disease in the elderly: morbidity, mortality, and costs. Clin Geriatr Med. 2009;25(4):563–577. doi: 10.1016/j.cger.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reaven G. Insulin resistance and coronary heart disease in nondiabetic individuals. Arterioscler Thromb Vasc Biol. 2012;32(8):1754–1759. doi: 10.1161/ATVBAHA.111.241885. [DOI] [PubMed] [Google Scholar]
- 3.Salazar MR, Carbajal HA, Espeche WG, Aizpurúa M, LeivaSisnieguez CE, LeivaSisnieguez BC, Stavile RN, March CE, Reaven GM. Insulin resistance: the linchpin between prediabetes and cardiovascular disease. Diab Vasc Dis Res. 2016;13(2):157–163. doi: 10.1177/1479164115610057. [DOI] [PubMed] [Google Scholar]
- 4.Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):122. doi: 10.1186/s12933-018-0762-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marfella R, Sardu C, Balestrieri ML, Siniscalchi M, Minicucci F, Signoriello G, Calabrò P, Mauro C, Pieretti G, Coppola A, Nicoletti G, Rizzo MR, Paolisso G, Barbieri M. Effects of incretin treatment on cardiovascular outcomes in diabetic STEMI-patients with culprit obstructive and multivessel non obstructive-coronary-stenosis. Diabetol Metab Syndr. 2018;3(10):1. doi: 10.1186/s13098-017-0304-3.eCollection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marfella R, Sardu C, Calabrò P, Siniscalchi M, Minicucci F, Signoriello G, Balestrieri ML, Mauro C, Rizzo MR, Paolisso G, Barbieri M. Non-ST-elevation myocardial infarction outcomes in patients with type 2 diabetes with non-obstructive coronary artery stenosis: effects of incretin treatment. Diabetes Obes Metab. 2018;20(3):723–729. doi: 10.1111/dom.13122. [DOI] [PubMed] [Google Scholar]
- 7.Sasso FC, Carbonara O, Nasti R, Campana B, Marfella R, Torella M, Nappi G, Torella R, Cozzolino D. Glucose metabolism and coronary heart disease in patients with normal glucose tolerance. JAMA. 2004;291(15):1857–1863. doi: 10.1001/jama.291.15.1857. [DOI] [PubMed] [Google Scholar]
- 8.Lin JD, Chang JB, Wu CZ, Pei D, Hsieh CH, Hsieh AT, Chen YL, Hsu CH, Liu CC. Identification of insulin resistance in subjects with normal glucose tolerance. Ann Acad Med Singapore. 2014;43(2):113–119. [PubMed] [Google Scholar]
- 9.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 10.Bao X, Borné Y, Johnson L, Muhammad IF, Persson M, Niu K, Engström G. Comparing the inflammatory profiles for incidence of diabetes mellitus and cardiovascular diseases: a prospective study exploring the ‘common soil’ hypothesis. Cardiovasc Diabetol. 2018;17(1):87. doi: 10.1186/s12933-018-0733-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352(16):1685–1695. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- 12.Lee SH, Ha JW, Kim JS, Choi EY, Park S, Kang SM, Choi D, Jang Y, Chung N. Plasma adiponectin and resistin levels as predictors of mortality in patients with acute myocardial infarction: data from infarction prognosis study registry. Coron Artery Dis. 2009;20(1):33–39. doi: 10.1097/MCA.0b013e328318ecb0. [DOI] [PubMed] [Google Scholar]
- 13.De Carvalho MH, Colaço AL, Fortes ZB. Cytokines, endothelial dysfunction, and insulin resistance. Arq Bras Endocrinol Metabol. 2006;50(2):304–312. doi: 10.1590/S0004-27302006000200016. [DOI] [PubMed] [Google Scholar]
- 14.Sardu C, Pieretti G, D’Onofrio N, Ciccarelli F, Paolisso P, Passavanti MB, Marfella R, Cioffi M, Mone P, Dalise AM, Ferraraccio F, Panarese I, Gambardella A, Passariello N, Rizzo MR, Balestrieri ML, Nicoletti G, Barbieri M. Inflammatory cytokines and SIRT1 levels in subcutaneous abdominal fat: relationship with cardiac performance in overweight pre-diabetics patients. Front Physiol. 2018;9:1030. doi: 10.3389/fphys.2018.01030.eCollection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beltowski J, Jamroz-Wiśniewska A, Widomska S. Adiponectin and its role in cardiovascular diseases. Cardiovasc Hematol Disord: Drug Targets. 2008;8(1):7–46. doi: 10.2174/187152908783884920. [DOI] [PubMed] [Google Scholar]
- 16.Yaturu S, Daberry RP, Rains J, Jain S. Resistin and adiponectin levels in subjects with coronary artery disease and type 2 diabetes. Cytokine. 2006;34(3–4):219–223. doi: 10.1016/j.cyto.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 17.Pischon T, Girman CJ, Hotamisligil GS, Rifai N, Hu FB, Rimm EB. Plasma adiponectin levels and risk of myocardial infarction in men. JAMA. 2004;291(14):1730–1737. doi: 10.1001/jama.291.14.1730. [DOI] [PubMed] [Google Scholar]
- 18.Knudson JD, Dick GM, Tune JD. Adipokines and coronary vasomotor dysfunction. Exp Biol Med (Maywood). 2007;232(6):727–736. [PubMed] [Google Scholar]
- 19.Shioji K, Moriwaki S, Takeuchi Y, Uegaito T, Mutsuo S, Matsuda M. Relationship of serum adiponectin level to adverse cardiovascular events in patients who undergo percutaneous coronary intervention. Circ J. 2007;71(5):675–680. doi: 10.1253/circj.71.675. [DOI] [PubMed] [Google Scholar]
- 20.Takagi T, Akasaka T, Yamamuro A, Honda Y, Hozumi T, Morioka S, Yoshida K. Impact of insulin resistance on neointimal tissue proliferation after coronary stent implantation: intravascular ultrasound studies. J Diabetes Complications. 2002;16(1):50–55. doi: 10.1016/S1056-8727(01)00190-8. [DOI] [PubMed] [Google Scholar]
- 21.Piatti P, Di Mario C, Monti LD, Fragasso G, Sgura F, Caumo A, Setola E, Lucotti P, Galluccio E, Ronchi C, Origgi A, Zavaroni I, Margonato A, Colombo A. Association of insulin resistance, hyperleptinemia, and impaired nitric oxide release with in-stent restenosis in patients undergoing coronary stenting. Circulation. 2003;108(17):2074–2081. doi: 10.1161/01.cir.0000095272.67948.17. [DOI] [PubMed] [Google Scholar]
- 22.Smith SC, Jr, Dove JT, Jacobs AK, Kennedy JW, Kereiakes D, Kern MJ, Kuntz RE, Popma JJ, Schaff HV, Williams DO, Gibbons RJ, Alpert JP, Eagle KA, Faxon DP, Fuster V, Gardner TJ, Gregoratos G, Russell RO, Smith SC, American Heart Association Task Force on Practice Guidelines Committee to Revise the 1993 Guidelines for Percutaneous Transluminal Coronary Angioplasty ACC/AHA guidelines of percutaneous coronary interventions (revision of the 1993 PTCA guidelines)-executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (committee to revise the 1993 guidelines for percutaneous transluminal coronary angioplasty) J Am Coll Cardiol. 2001;37:2215–2239. doi: 10.1016/S0735-1097(01)01344-4. [DOI] [PubMed] [Google Scholar]
- 23.Ellis SG, Vandormael MG, Cowley MJ, Di Sciascio G, Deligonul U, Topol EJ, Bulle TM. Coronary morphologic and clinical determinants of procedural outcome with angioplasty for multivessel coronary disease. Implications for patient selection. Multivessel Angioplasty Prognosis Study Group. Circulation. 1990;82(4):1193–1202. doi: 10.1161/01.cir.82.4.1193. [DOI] [PubMed] [Google Scholar]
- 24.Orbach A, Halon DA, Jaffe R, Rubinshtein R, Karkabi B, Flugelman MY, Zafrir B. Impact of diabetes and early revascularization on the need for late and repeat procedures. Cardiovasc Diabetol. 2018;17(1):25. doi: 10.1186/s12933-018-0669-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Komatsu T, Komatsu S, Nakamura H, Kuroyanagi T, Fujikake A, Hisauchi I, Sakuma M, Nakahara S, Sakai Y, Taguchi I. Insulin resistance as a predictor of the late catch-up phenomenon after drug-eluting stent implantation. Circ J. 2016;80(3):657–662. doi: 10.1253/circj.CJ-15-1012. [DOI] [PubMed] [Google Scholar]
- 26.Baldassarre S, Fragapani S, Panero A, Fedele D, Pinach S, Lucchiari M, Vitale AR, Mengozzi G, Gruden G, Bruno G. NT-proBNP in insulin-resistance mediated conditions: overweight/obesity, metabolic syndrome and diabetes. The population-based Casale Monferrato Study. Cardiovasc Diabetol. 2017;16(1):119. doi: 10.1186/s12933-017-0601-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tanaka A, Komukai S, Shibata Y, Yokoi H, Iwasaki Y, Kawasaki T, Horiuchi K, Nakao K, Ueno T, Nakashima H, Tamashiro M, Hikichi Y, Shimomura M, Tago M, Toyoda S, Inoue T, Kawaguchi A, Node K, Pioglitazone Reduce Inflammation and Restenosis with and without Drug Eluting Stent (PRIDE) Study Investigators Effect of pioglitazone on cardiometabolic profiles and safety in patients with type 2 diabetes undergoing percutaneous coronary artery intervention: a prospective, multicenter, randomized trial. Heart Vessels. 2018;33(9):965–977. doi: 10.1007/s00380-018-1143-3. [DOI] [PubMed] [Google Scholar]
- 28.Levitan EB, Song Y, Ford ES, Liu S. Is nondiabetic hyperglycemia a risk factor for cardiovascular disease? A meta-analysis of prospective studies. Arch Intern Med. 2004;164(19):2147–2155. doi: 10.1001/archinte.164.19.2147. [DOI] [PubMed] [Google Scholar]
- 29.González N, Moreno-Villegas Z, González-Bris A, Egido J, Lorenzo Ó. Regulation of visceral and epicardial adipose tissue for preventing cardiovascular injuries associated to obesity and diabetes. Cardiovasc Diabetol. 2017;16(1):44. doi: 10.1186/s12933-017-0528-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yun KH, Jeong MH, Kim KH, Hong YJ, Park HW, Kim JH, Ahn YK, Cho JG, Park JC, Kim NH, Oh SK, Jeong JW, Kang JC. The effect of insulin resistance on prognosis of non-diabetic patients who underwent percutaneous coronary intervention. J Korean Med Sci. 2006;21(2):212–216. doi: 10.3346/jkms.2006.21.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Muhlestein JB, Anderson JL, Horne BD, Lavasani F, Allen Maycock CA, Bair TL, Pearson RR, Carlquist JF, Intermountain Heart Collaborative Study Group Effect of fasting glucose levels on mortality rate in patients with and without diabetes mellitus and coronary artery disease undergoing percutaneous coronary intervention. Am Heart J. 2003;146(2):351–358. doi: 10.1016/s0002-8703(03)00235-7. [DOI] [PubMed] [Google Scholar]
- 32.Gasior M, Pres D, Stasik-Pres G, Lech P, Gierlotka M, Hawranek M, Wilczek K, Szyguła-Jurkiewicz B, Lekston A, Kalarus Z, Strojek K, Gumprecht J, Poloński L. Effect of blood glucose levels on prognosis in acute myocardial infarction in patients with and without diabetes, undergoing percutaneous coronary intervention. Cardiol J. 2008;15(5):422–430. [PubMed] [Google Scholar]
- 33.Corrada E, Cappelleri A, Belli G, Genovese S, Barbaro C, Gasparini G, Pagnotta P, Rossi M, Zavalloni D, Presbitero P. Admission glycemia and markers of inflammation are independent outcome predictors in primary PCI in non-diabetic patients. Minerva Cardioangiol. 2008;56(5):445–452. [PubMed] [Google Scholar]
- 34.Gasior M, Stasik-Pres G, Pres D, Lech P, Gierlotka M, Lekston A, Hawranek M, Tajstra M, Kalarus Z, Poloński L. Relationship between blood glucose on admission and prognosis in patients with acute myocardial infarction treated with percutaneous coronary intervention. Kardiol Pol. 2007;65(9):1031–1038. [PubMed] [Google Scholar]
- 35.Piestrzeniewicz K. Value of blood adipose tissue hormones concentration-adiponectin, resistin and leptin in the prediction of major adverse cardiac events (MACE) in 1-year follow-up after primary percutaneous coronary intervention in ST-segment elevation acute myocardial infarction. Neuro Endocrinol Lett. 2008;29(4):581–588. [PubMed] [Google Scholar]
- 36.Zhao LP, Xu WT, Wang L, Li H, Shao CL, Gu HB, Chan SP, Xu HF, Yang XJ. Influence of insulin resistance on in-stent restenosis in patients undergoing coronary drug-eluting stent implantation after long-term angiographic follow-up. Coron Artery Dis. 2015;26(1):5–10. doi: 10.1097/MCA.0000000000000170. [DOI] [PubMed] [Google Scholar]
- 37.An X, Yu D, Zhang R, Zhu J, Du R, Shi Y, Xiong X. Insulin resistance predicts progression of de novo atherosclerotic plaques in patients with coronary heart disease: a one-year follow-up study. Cardiovasc Diabetol. 2012;11:71. doi: 10.1186/1475-2840-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pilz S, Mangge H, Wellnitz B, Seelhorst U, Winkelmann BR, Tiran B, Boehm BO, März W. Adiponectin and mortality in patients undergoing coronary angiography. J Clin Endocrinol Metab. 2006;91(11):4277–4286. doi: 10.1210/jc.2006-0836. [DOI] [PubMed] [Google Scholar]
- 39.Laughlin GA, Barrett-Connor E, May S, Langenberg C. Association of adiponectin with coronary heart disease and mortality. Am J Epidemiol. 2007;165(2):164–174. doi: 10.1093/aje/kwk001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Menon V, Li L, Wang X, Greene T, Balakrishnan V, Madero M, Pereira AA, Beck GJ, Kusek JW, Collins AJ, Levey AS, Sarnak MJ. Adiponectin and mortality in patients with chronic kidney disease. J Am Soc Nephrol. 2006;17(9):2599–2606. doi: 10.1681/asn.2006040331. [DOI] [PubMed] [Google Scholar]
- 41.Kistorp C, Faber J, Galatius S, Gustafsson F, Frystyk J, Flyvbjerg A, Hildebrandt P. Plasma adiponectin, body mass index, and mortality in patients with chronic heart failure. Circulation. 2005;112(12):1756–1762. doi: 10.1161/circulationaha.104.530972. [DOI] [PubMed] [Google Scholar]
- 42.Tapan S, Dogru T, Tasci I, Ercin CN, Erbil MK. Adiponectin levels in patients undergoing coronary stenting. Clin Biochem. 2009;42(6):544–545. doi: 10.1016/j.clinbiochem.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 43.Baysan O, Yokusoglu M, Bugan B. Is low adiponectin levels more sensitive predictor of in-stent restenosis: new questions and challenges. Int J Cardiol. 2010;144(2):236. doi: 10.1016/j.ijcard.2008.12.203. [DOI] [PubMed] [Google Scholar]
- 44.Mito T, Miura S, Iwata A, Morii J, Sugihara M, Ike A, Mori K, Kawamura A, Nishikawa H, Zhang B, Saku K. Determination of the cut-off plasma adiponectin level associated with a lower risk of restenosis in patients with stable angina. Coron Artery Dis. 2011;22(7):451–457. doi: 10.1097/MCA.0b013e3283495d43. [DOI] [PubMed] [Google Scholar]
- 45.Li TD, Zeng ZH. Adiponectin as a potential therapeutic target for the treatment of restenosis. Biomed Pharmacother. 2018;101:798–804. doi: 10.1016/j.biopha.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 46.On YK, Park HK, Hyon MS, Jeon ES. Serum resistin as a biological marker for coronary artery disease and restenosis in type 2 diabetic patients. Circulation. 2007;71(6):868–873. doi: 10.1253/circj.71.868. [DOI] [PubMed] [Google Scholar]
- 47.Conrotto F, Bertaina M, Raposeiras-Roubin S, Kinnaird T, Ariza-Solé A, Manzano-Fernández S, Templin C, Velicki L, Xanthopoulou I, Cerrato E, Rognoni A, Boccuzzi G, Omedè P, Montabone A, Taha S, Durante A, Gili S, Magnani G, Autelli M, Grosso A, Flores Blanco P, Garay A, Quadri G, Varbella F, CaneiroQueija B, Cobas Paz R, Cespón Fernández M, Muñoz Pousa I, Gallo D, Morbiducci U, Dominguez-Rodriguez A, Valdés M, Cequier A, Alexopoulos D, Iñiguez-Romo A, Gaita F, Abu-Assi E, D’Ascenzo F. Prasugrel or ticagrelor in patients with acute coronary syndrome and diabetes: a propensity matched substudy of RENAMI. Eur Heart J Acute Cardiovasc Care. 2018;1:2048872618802783. doi: 10.1177/20488726188027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1. Definition of the best cut-off level of ROC curves respectively for adiponectin (a), resistin (b) and TNF-alpha (c), according to the risk of restenosis. (Central panel) Definition of the best cut-off level of ROC curves respectively for adiponectin (a), resistin (b) and TNF-alpha (c), according to the risk of new stenosis. (Lower panel) Definition of the best cut-off level of ROC curves respectively for adiponectin (a), resistin (b) and TNF-alpha (c), according to the risk of any coronary event.
Additional file 2: Table S1. Characteristics of the study population, according to the occurrence or not of PCI for de novo IHD (n = 51).
Additional file 3: Table S2. Adiponectin and HOMA-IR values for the patients who experimented restenosis.
Data Availability Statement
The authors declare that the data supporting the findings of this study are available within the article and its additional files.