Abstract
Introduction
South Africa has a wide distribution of scorpion species, yet limited data are available regarding the incidence and severity of scorpion envenomation. The aim of this study was to analyse South African epidemiological data of scorpion stings and envenomation as reported to the Tygerberg Poisons Information Centre (TPIC).
Methods
A retrospective analysis was conducted of scorpion-related telephonic consultations to the TPIC over a ten year period (1 January 2005 to 31 December 2014). Data were entered onto a Microsoft Excel® spreadsheet and descriptive statistics are presented for all variables. Associations with severity of envenomation are presented as odds ratios (OR) with 95% confidence intervals (95%CI).
Results
During the study period 52,163 consultations were processed by the TPIC of which 740 (1.4%) cases involved scorpion stings. Of these, 146 (19.7%) cases were deemed serious envenomations. Antivenom was recommended to be administered in 131 (90%) of these cases. Healthcare professionals made most calls (63%), but were less likely to phone for non-serious cases (OR 0.16; 95%CI 0.09 to 0.29). The Western Cape Province had the highest incidence of calls (6.9 scorpion-related calls/100 000 people). Adults (>20 years) were victims in 71.4% of cases, and were more likely to experience less serious stings (OR 0.57; 95%CI 0.37 to 0.86). The TPIC was consulted within six hours of the sting occurring in 356 (48.1%) cases with a significant association to less severity (OR 3.51; 95%CI 1.9 to 6.3). Only 2% (15) of the scorpions were available for identification.
Conclusion
The incidence of severe scorpionism to the TPIC was low. Care should be taken when children are involved and when calls are received more than six hours after the sting. TPIC consultants as well as healthcare professionals working in semi-arid regions should be aware of these high risk populations.
Keywords: Scorpion sting, Scorpionism, Envenomation, Epidemiology, Poisons centre, South Africa
African relevance
-
•
Scorpion stings in Africa can develop into a severe medical emergency, especially in young children.
-
•
Prevention measures are needed in Africa to reduce morbidity rates from these poisonous scorpions.
-
•
Healthcare professionals in Africa should know about the benefits and risks of antivenom.
-
•
African healthcare professionals should know how and where to contact a poisons centre for guidance.
Introduction
Scorpion sting may cause life-threatening envenoming. There are almost 2000 scorpion species known in the world, but the venom of only about 50 (<3%) species is dangerous to humans [1]. Most of the scorpions that cause serious envenoming belong to the Buthidae family, which includes scorpions from the genera Leiurus in the Near and Middle East, Androctonus and Buthus in North Africa, Tityus in South America, Centruroides in North and Central America, Mesobuthus in Asia and Parabuthus in southern Africa [2].
South Africa is home to about 130 scorpion species. These all belong to the dangerous Buthidae and the relatively harmless Scorpionidae, Bothriuridae, and Ischnuridae families [3]. The Buthidae family have characteristic thin pincers and thick tails (metasoma), and is represented by seven genera of which the Parabuthus is medically the most important. Approximately 22 Parabuthus species are distributed throughout southern Africa [4], of which only two (Parabuthus granulatus and Parabuthus transvaalicus) cause serious envenomations [5]. The remainder of the scorpion species are relatively harmless to humans, although they can inflict quite a painful sting [6].
Identification of a scorpion is difficult and can often only be done by an expert. The P. transvaalicus is overall black and the P granulatus’ colour can range from orange to blackish brown with pale legs [3]. Both species are large in size, up to a 150 mm long (Fig. 1).
Fig. 1.
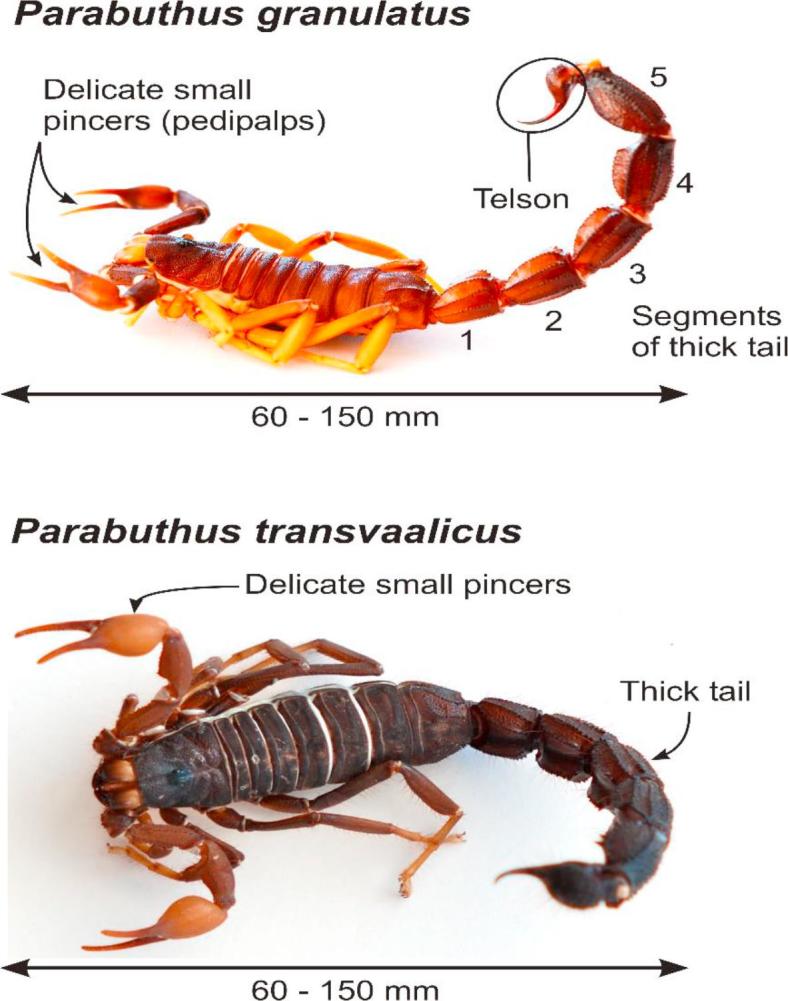
General morphology of Parabuthus granulatus and P. transvaalicus. (Photos courtesy of Dr Gerbus Muller).
Since identification of scorpions is challenging and not always possible it becomes important for the treating physician to be guided by the symptoms and signs of the patient to assess the severity of the envenomation. The clinical manifestations of scorpion envenomation appear to be mainly due to the activation of the peripheral nervous system, e.g. somatic and autoimmune nerves.
Inadequate data are available regarding the incidence and severity of scorpion envenoming in southern Africa. The aim of this study was to analyse South African epidemiological data of scorpion stings and envenomation as reported to the Tygerberg Poisons Information Centre (TPIC).
Methods
A retrospective analysis was conducted on data with regard to scorpion sting as telephonically managed by the TPIC over a ten year period (1 January 2005 to 31 December 2014). This study was approved by the Health Research Ethics Committee of the University of Stellenbosch (Ref: N 17/05/054).
The TPIC is a specialist service provided by the Tygerberg Academic Hospital, a tertiary hospital of the Western Cape province of South Africa, and the Division of Clinical Pharmacology in the Faculty of Medicine and Health Sciences, Stellenbosch University. The TPIC provides a free 24/7 poison information service to health care workers and members of the public throughout South Africa. During the study period acute poisoning consultations were telephonically managed via a nationally advertised dedicated emergency number. Poisoning enquiries were dealt with by pharmacists, medical scientists and medical doctors and were manually recorded on a standard consultation form. Information included date and time; geographical area; patient’s age and gender; time since exposure; severity of the sting and the recommendation for antivenom administration. Severity grading was performed according to the European Association of Poisons Centers and Clinical Toxicologists Poisoning Severity Score (PSS) [7]. The score categorise severity as none (PSS = 0), minor (PSS = 1), moderate (PSS = 2), severe (PSS = 3), and fatal (PSS = 4). The severity score was allocated at the time of the call and a PSS ≥ 2 was deemed a serious envenomation.
All consultation calls relating to scorpion sting were included. Multiple calls about the same victim were managed as one entry. In the event of incomplete consultation forms, the cases were not excluded entirely; instead, the specific missing variable was indicated as unknown for the relevant analysis.
Collected data were entered onto a standard Microsoft Excel® spreadsheet. Descriptive statistics are presented for all variables. Sting severity were compared with age, gender, type of caller, and time since exposure to determine any associations. Age and time since exposure were collected as categorical data and were dichotomized for the analysis. Effect size is presented as odds ratios (OR) with 95% confidence intervals (95%CI); calculated using standard formulae.
Results
During the study period 52,163 telephonic consultations were managed, of which 740 (1.4%) involved scorpion stings; 725 cases (98.0%) involved humans and 15 cases (2.0 %) involved animals. Serious envenomation occurred in 146 (19.7%) cases with a mean occurrence of 11.8 per year (PSS unknown n = 112). Antivenom administration was recommended in 131 (89.7%) of the serious cases and the only fatality occurred in a dog.
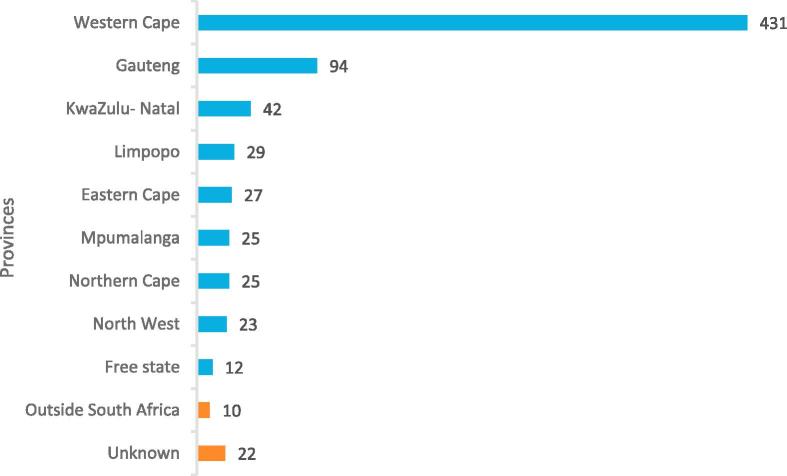
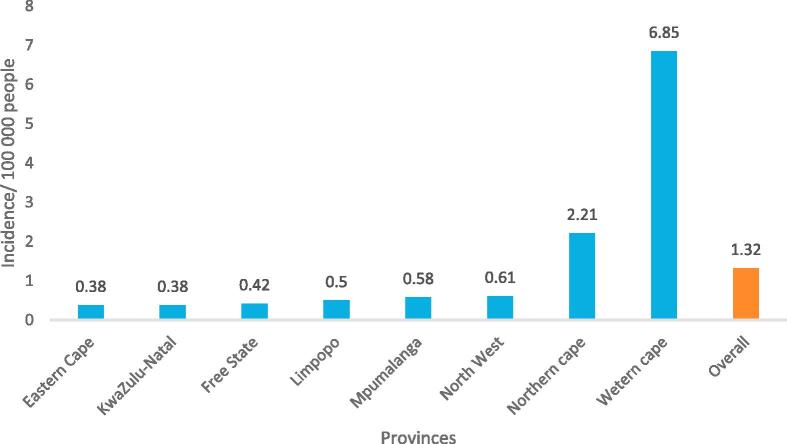
Most of the calls were from healthcare professionals (n = 466, 63%), 250 (34%) from the general public and in 24 cases the caller was not identified. Healthcare professionals were less likely to phone for non-serious cases (OR 0.16, 95%CI 0.09 to 0.29). The majority of calls originated from the Western Cape (n = 431, 58.2%) and Gauteng (n = 94, 12.7%) provinces (Fig. 2), although the most calls per population originated from the Western Cape (6.9 stings/100 000 people) and the Northern Cape (2.1 stings/100 000 people) provinces (Fig. 3) [8].
Fig. 2.
Geographical distribution of the number of scorpion sting calls received by the Tygerberg Poisons Information Centre over a 10 year period.
Fig. 3.
Incidence of scorpion sting calls per 100 000 population as recorded by the Tygerberg Poisons Information Centre over a 10 year period (excluding location unknown (n = 22) and outside South Africa (n = 10) [7].
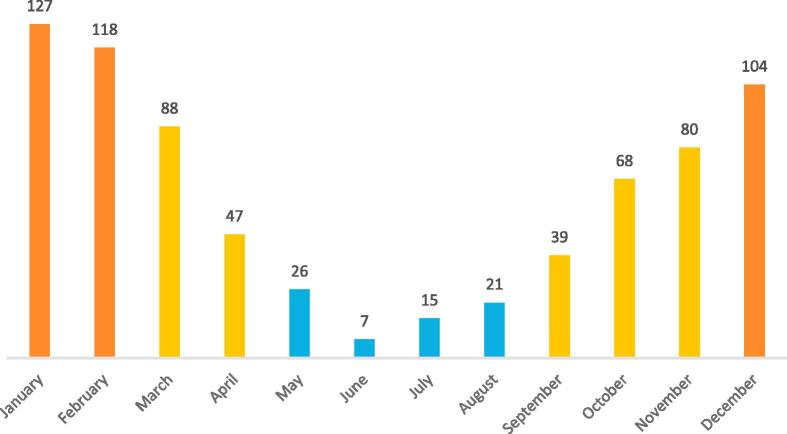
A slight male pre-dominance existed in suspected victims (393/725, 54.2%; animals exclude n = 15; gender not indicated n = 40). No significant difference were found between the severity of the sting and gender (OR 0.82, 95%CI 0.56 to 1.2). Most stings occurred in adults (>20 years of age) (518/725, 71.4%; animals exclude n = 15; unknown n = 32), although adults were more likely to experience less serious stings than younger patients (OR 0.57, 95%CI 0.37 to 0.86). Scorpion stings mainly occurred in the warmer summer months, from October to March, with a peak in January (n = 127, 17.2%) and February (n = 118, 15.9%) (Fig. 4).
Fig. 4.
Monthly distribution of calls related to scorpion stings as reported to the Tygerberg Poisons Information Centre over 10 years (orange, Summer; yellow, Spring and Autumn; blue, Winter).
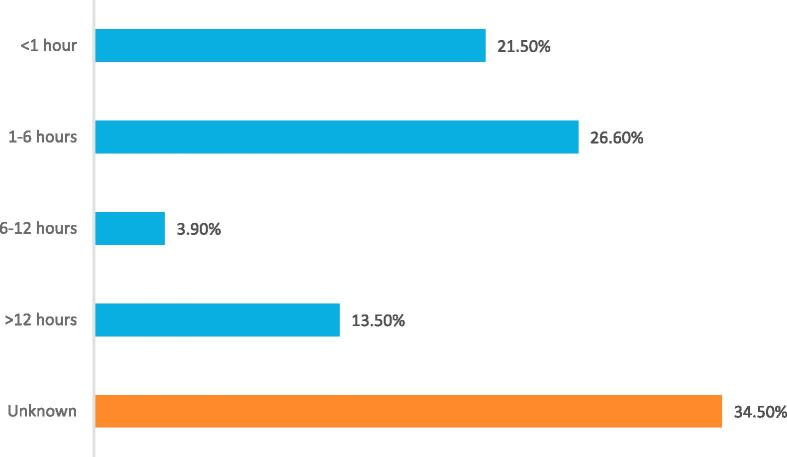
In 356 (48.1%) scorpion sting consultations a call to the TPIC was made within six hours of the scorpion sting occurring (Fig. 5), with a significant association to less severity (OR 3.51, 95%CI 1.9 to 6.3).
Fig. 5.
Time intervals for contacting the Tygerberg Poisons Information Centre after the scorpion sting occurred.
Identification of the relevant scorpion was done in only 15 (2%) cases by positive morphological examination.
Discussion
This study describes previously unknown epidemiological data regarding scorpion envenomation in calls made to a South African poisons information centre. Most stings were reported during the warmer summer months, October to March, with the Western Cape and Northern Cape provinces having the highest incidence of calls. Positive morphological identification of the scorpion species involved was low (2%). The majority of victims (65%) reported no or only minor symptoms such as local pain.
The incidence of scorpion sting reported to the TPIC is low. Less than 2% of calls made to the TPIC involved scorpion stings and this result is in accord with reports from other countries’ PICs [9], [10], [11]. However one PIC study from Morocco, a country known for a high incidence of scorpion envenomation, reported that 73% of their calls related to scorpion stings [12].
Most venomous scorpions in South Africa prefer deserts or semi-arid regions. In this study the Western Cape and the Northern Cape provinces had the highest incidence of scorpion sting per 100 000 people as well as the highest number of serious cases (Fig. 2, Fig. 3). This finding is in support of Muller, who previously described that all 42 serious scorpion envenomations over a 5-year period occurred in the Western and Northern Cape provinces [4].
The correct identification of scorpions to species level is notoriously difficult; in our study only 15 scorpion specimen were identified. Symptoms and signs of systemic envenomation includes general paraesthesia, hyperaesthesia, dysphagia, increased salivation, involuntary movements, tremors, hypertension, tachycardia and respiratory failure. These clinical manifestations have been described in the literature [1], [2], [4], [5], [6], [13]. In our study a P. granulatus or P. transvaalicus sting were often identified by the typical symptoms the victim presented with. Antivenom administration was recommended in patients with systemic toxicity. A study performed in mice indicated the LD50 of P. granulatus to be 1.56 mg/kg, close to that of the Centruroides noxius, a highly venomous species found in North America (LD50 = 1.19 mg/kg), and three times more toxic than the venom of the P. transvaalicus (LD50 = 4.25 mg/kg) [14]. The venom from P. transvaalicusis is locally used for the production of antivenom. It has been recommended that a specific antivenom against P. granulatus should be produced and evaluated [6].
The severity of most scorpion-related cases were mild (65%) with only localized pain. Globally, most scorpion stings cause localised pain, whereas only an estimated 10% of stings result in serious systemic envenomation [2]. In our study 20% of the cases were classified as serious, whereas a Zimbabwean study reported 15.4% of scorpion sting cases as severe [5].
There are several limitations to our study. Most importantly, this is a retrospective study with inherent risks of error since it used data from an existing database and from manually recorded data. Data entered might be incomplete, imprecise or invalid, resulting in information bias. Incomplete data might influence the results in either direction. However, this possible effect was limited by indicating the specific missing variable as unknown and not excluding the entire case. It is also known that poisons centre utilization is associated with poisons centre awareness [15]. This could also apply to our result where most calls were received from the Western Cape region, which hosts two of the three poisons centres in South Africa. Lastly, enquiries to a poisons centre do not reflect the true incidence of poisoning in the community, but rather reflect a need for information. A possible approach to compensate for this shortcoming in the future is to utilize data from all South African poisons information centres along with actual hospital admissions [16].
Conclusion
The incidence of severe scorpionism to the TPIC was low. Care should be taken when children are involved and when calls are received more than six hours after the sting. TPIC consultants as well as healthcare professionals working in semi-arid regions should be aware of these high risk populations.
Dissemination of results
Results were shared in Tygerberg hospital’s newsletter.
Authors’ contributions
Authors contributed as follows to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: CM contributed 30%; DVH contributed 25%; GM and DS contributed 15% each; HR, CW, and CDP contributed 5% each. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Conflict of Interest
The authors declare no conflicts of interest.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.afjem.2018.12.003.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Santos M.S., Silva C.G., Silva Neto B., Grangeiro Júnior C.R., Lopes V.H., Teixeira Júnior A.G. Clinical and epidemiological aspects of scorpionism in the world: a systematic review. WILDERNESS Environ Med. 2016;27:504–518. doi: 10.1016/j.wem.2016.08.003. http://www.sciencedirect.com/science/article/pii/S1080603216302149 Available from. [DOI] [PubMed] [Google Scholar]
- 2.Isbister G.K., Bawaskar H.S. Scorpion Envenomation. N Engl J Med. 2014;371(5):457–463. doi: 10.1056/NEJMra1401108. Available from: http://www.nejm.org/doi/abs/10.1056/NEJMra1401108. [DOI] [PubMed] [Google Scholar]
- 3.Leeming J. Scorpions of Southern Africa. Jeane Hromnik, editor. Cape Town: Struik Nature; 2003. 1–87 p. Available from: http://www.scorpions.co.za/portfolio-item/scorpions-southern-africa/.
- 4.Muller G.J. Scorpionism in South Africa. A report of 42 serious scorpion envenomations. SAMJ. 1993;83:405–411. [PubMed] [Google Scholar]
- 5.Bergman NJ. Scorpion sting in Zimbabwe. SAMJ. 87(2); 163–167. [PubMed]
- 6.Muller GJ, Modler H, Wium C, Veale D. Scorpion sting in southern Africa: diagnosis and management. Continuing Medical Education. 2012;30:356–361 p. Available from: http://www.cmej.org.za/index.php/cmej/article/view/2545/2580.
- 7.Persson H.E., Sjöberg G.K., Haines J.A., Pronczuk de Garbino J. Poisoning Severity Score. Grading of acute poisoning. J Toxicol Clin Toxicol. 1998;36(3):205–213. doi: 10.3109/15563659809028940. [DOI] [PubMed] [Google Scholar]
- 8.Statistical release P0302 Mid-year population estimates. 2016 Available from: https://www.statssa.gov.za/publications/P0302/P03022016.pdf.
- 9.Mowry JB, Spyker DA, Brooks DE, McMillan N, Schauben JL. 2014 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32nd Annual Report. Clin Toxicology, 2015; 53(10):962–1147. Available from: http://www.tandfonline.com/doi/full/10.3109/15563650.2015.1102927. [DOI] [PubMed]
- 10.Srivastava A, Peshin SS, Kaleekal T, Gupta SK. An epidemiological study of poisoning cases reported to the National Poisons Information Centre, All India Institute of Medical Sciences, New Delhi. 2005; 279–85. [DOI] [PubMed]
- 11.Cesaretli Y., Ozkan O. Scorpion stings in Turkey: epidemiological and clinical aspects between the years 1995 and 2004. Rev Inst Med Trop Sao Paulo. 2010;52:215–220. doi: 10.1590/s0036-46652010000400010. [DOI] [PubMed] [Google Scholar]
- 12.Rhalem N., Aghandous R., Chaoui H., Eloufir R., Badrane N. Role of the Poison Control Centre of Morocco in the Improvement of Public Health. ASIA PACIFIC J Med Toxicol. 2013;2(3):82–86. [Google Scholar]
- 13.Dawn Rossiter, Marc Blockman KB et al, editor. South African Medicines Formulary 12th ed. Cape Town; 2016. 618-620 Available from: http://www.medicalbooks.co.za/product_info.php/products_id/9400.
- 14.Fourie C. Comparison of the Relative Toxicities of some medically important Parabuthus scorpion species in Southern Africa. Stellenbosch University; 1998. Available from: carinem@sun.ac.za.
- 15.Marks C.J., van Hoving D.J. A 3-year survey of acute poisoning exposures in infants reported in telephone calls made to the Tygerberg poison information centre, South Africa. South African J Child Heal. 2016;10(1):43–46. Available from: http://scholar.sun.ac.za/handle/10019.1/100011. [Google Scholar]
- 16.Marks CJ. Acute poisonings : a comparative study of hospital admissions versus poison centre consultations 2001. Available from: http://scholar.sun.ac.za/handle/10019.1/13/browse?value=Marks%2C+C.+J&type=author.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.