Abstract
The present study evaluated the flexural properties of a new temporary splint material, G-Fix, for use in dental trauma splints in comparison with other resin materials. Four types of resin materials were considered in the present study: MI Flow II, light-cured composite resin (MI); G-Fix, light-cured resin for splinting teeth (GF); Super-Bond C&B, adhesive resin cement (SB); and Unifast III, self-cured methyl-methacrylate resin (UF). The flexural properties of these four materials were tested according to ISO 4049. The flexural strength significantly increased in the order of UF (64.9 MPa) < SB (76.5 MPa) < GF (94.3 MPa) < MI (161.2 MPa). The elastic modulus significantly increased in the order of UF (2.11 GPa) ≒ SB (2.23 GPa) < GF (2.62 GPa) < MI (7.39 GPa). A splint made of GF may be more flexible than a composite splint, which is categorized as a rigid splint.
Keywords: dental trauma splint, flexural property, G-Fix, resin materials
Introduction
Dental trauma splints (DTSs) are the common therapy for injured teeth. The main roles of DTSs are immobilization of injured teeth in their initial position and protection from re-trauma to support healing, provide patient comfort, and improve function.1, 2, 3, 4, 5 The guidelines for dental trauma management indicate that flexible (nonrigid) splinting assists in healing, and that ideal splints should allow physiologic tooth mobility and injured teeth to experience slight motion.4, 5 There are many types of DTSs, including wire-composite splints, composite splints, titanium trauma splints, and bracket splints. Composite splints are easy to construct and are esthetically pleasing. However, composite splints are rigid and may not be suitable for use as DTSs.3, 6, 7
A new temporary splint material, G-Fix, was released by GC Corporation (Tokyo, Japan). This material is a light-cured flowable resin that is expected to have flexibility because of its phosphate monomer and high-elasticity cross-linking monomer composition. The purpose of the present study is to evaluate the flexural properties of a new temporary splint material, G-Fix, through a three-point flexural test and to compare G-Fix with other resin materials.
Materials and methods
Four types of resin materials were considered in the present study: MI Flow II (MI; GC Corporation), light-cured composite resin; G-Fix (GF; GC Corporation), light-cured resin for splinting teeth; Super-Bond C&B (SB; Sun Medical Co. Ltd., Shiga, Japan), adhesive resin cement; and Unifast III (UF; GC Corporation), self-cured methyl-methacrylate resin.
The flexural properties of these four materials were tested according to ISO 4049. Seven sticks were made for each resin using a stainless-steel split mold (25 mm × 2 mm × 2 mm), which was placed on a polyester film covering a glass slide. SB and UF were mixed according to the manufacturers’ instructions and were placed into stainless-steel molds. MI and GF were directly injected from a syringe into the molds. These resin materials were placed into the molds and were then covered with another polyester film and a glass slide. The materials were then either self-cured (SB and UF) or light cured with Elipar S10 (3M ESPE, MN, USA) (MI and GF). The specimens were stored for 24 hours in distilled water at 37°C before the mechanical tests were conducted. The dimensions of the specimens were measured using a digital caliper. Seven specimens of each material were subjected to the three-point bending flexural strength test using a universal machine (AG-X plus 5 kN; Shimadzu, Kyoto, Japan) at a cross-head speed of 1.0 mm/min. The specimens were positioned on a three-point bending apparatus with a span length of 20.0 mm. The peak breaking stress and the modulus of elasticity were determined from the stress–strain curve using computer software (TREPEZIUMX; Shimadzu) linked to the testing machine.
After testing, the specimen surfaces were coated with gold by an ion coater (IB-3; Eiko, Ibaraki, Japan). The specimens were then observed using a digital microscope (VHX-1000; Keyence, Osaka, Japan).
Data were entered into Microsoft Excel (Microsoft Corporation, Redmond, WA, USA). The results were analyzed by calculating the mean and standard deviation for each resin material. Ekuseru-Toukei 2015 (Social Survey Research Information Co., Ltd., Tokyo, Japan) was used for statistical analysis. Nonparametric tests were used because the data did not exhibit homogeneity of variance (Bartlett’s test, P < 0.05). The Steel–Dwass test was applied to analyze the flexural strengths and elastic moduli of the four resin materials through a multiple-comparison procedure (P < 0.05).
Results
The obtained flexural properties are shown in Table 1. The flexural strengths ranged from 64.9 MPa to 161.2 MPa. The flexural strengths significantly increased in the order of UF < SB < GF < MI (P = 0.014, P = 0.010, P = 0.010, respectively). The elastic modulus ranged from 2.11 GPa to 7.39 GPa. The elastic modulus significantly increased in the order of UF ≒ SB < GF < MI (P = 0.380, P = 0.010, P = 0.010, respectively).
Table 1.
Flexural strengths and elastic moduli of the four materials.
| Materials | Flexural strength (MPa) | Elastic moduli (GPa) |
|---|---|---|
| MI | 161.2 ± 14.5a | 7.39 ± 0.33a |
| GF | 94.3 ± 1.4b | 2.62 ± 0.04b |
| SB | 76.5 ± 5.2c | 2.23 ± 0.14c |
| UF | 64.9 ± 2.6d | 2.11 ± 0.09c |
Data are presented as Mean ± SD values of the flexural strengths and elastic modulus. Different superscript letters indicate a statistically significant difference (P < 0.05). Number of specimens per group = 7. GF = G-Fix; MI = MI Flow II; SB = Super-Bond C&B; SD = standard deviation; UF = Unifast III.
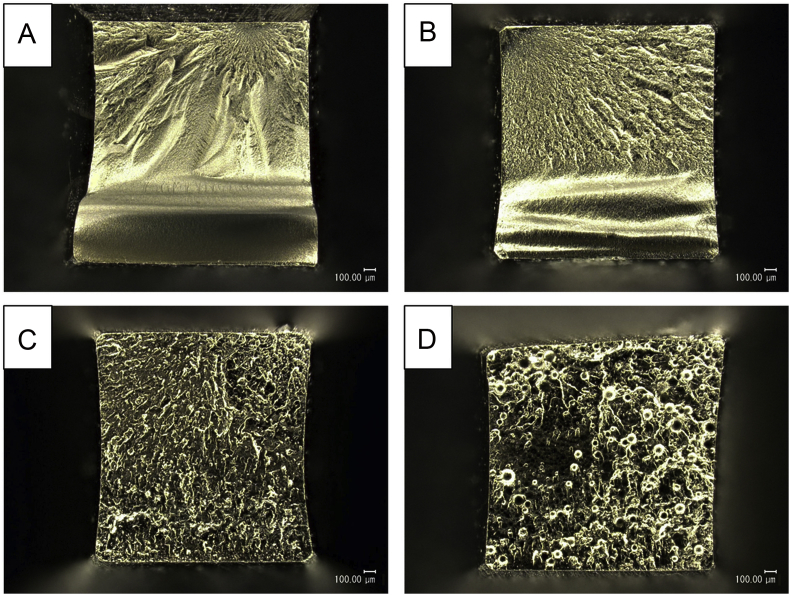
The digital microscope observations of the fracture surfaces are shown in Figure 1. The fracture surface of MI revealed a radial pattern with a fracture origin indicative of a brittle mode of fracture. Although the fracture surface of GF was almost similar to that of MI, GF fracture surface showed characteristic features of both brittle and ductile fracture with dimples. The fracture surface of SB revealed numerous dimples, indicative of a ductile mode of fracture. The surface of UF showed unreacted polymers.
Figure 1.
Digital microscope observations of the fracture surfaces (magnification 100×, bar = 100 μm): (A) MI, (B) GF, (C) SB , and (D) UF. GF = G-Fix; MI = MI Flow II; SB = Super-Bond C&B; UF = Unifast III.
Discussion
The modulus of elasticity is an indicator of the material stiffness, which points to a positive correlation between the modulus of elasticity and material stiffness. Splints that are too rigid are more likely to be developed from materials having high modulus of elasticity, such as composite resins. In the present study, GF exhibited a lower elastic modulus than MI (the composite resin). Based on these results, a splint made of GF may be more flexible than a composite splint, which is categorized as a rigid splint. Since the flexural strength of GF is higher than that of UF or SB, it appears that a splint made of GF may withstand the mechanical stress that a splint made of UF or SB can withstand. Therefore, these findings show the possibility that GF is a suitable material for use as a DTS.
In the present study, flexural strength testing was conducted according to the ISO flexural test. According to previous studies on the flexural properties of SB and UF,8, 9 the flexural strength and elastic modulus of SB were 62.3 MPa and 1.7 GPa, respectively, and the flexural strength and elastic modulus of UF were 68.2 MPa and 2.0 GPa, respectively. In the present study, similar results were obtained for the flexural strengths and elastic moduli of SB and UF, indicating the reliability of the results obtained in the present study.
The present study evaluated the flexural properties of G-Fix in comparison with other resin materials. Evaluation of materials for use in DTSs requires a multifaceted investigation. Further studies are required in order to evaluate splints made of G-Fix in a simulated clinical situation involving dental trauma.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
None.
References
- 1.Oikarinen K. Tooth splinting: a review of the literature and consideration of the versatility of a wire-composite splint. Endod Dent Traumatol. 1990;6:237–250. doi: 10.1111/j.1600-9657.1990.tb00426.x. [DOI] [PubMed] [Google Scholar]
- 2.Berthold C., Holst S., Schmitt J., Goellner M., Petschelt A. An evaluation of the Periotest method as a tool for monitoring tooth mobility in dental traumatology. Dent Traumatol. 2010;26:120–128. doi: 10.1111/j.1600-9657.2009.00860.x. [DOI] [PubMed] [Google Scholar]
- 3.Berthold C., Thaler A., Petschelt A. Rigidity of commonly used dental trauma splints. Dent Traumatol. 2009;25:248–255. doi: 10.1111/j.1600-9657.2008.00683.x. [DOI] [PubMed] [Google Scholar]
- 4.Diangelis A.J., Andreasen J.O., Ebeleseder K.A. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth. Dent Traumatol. 2012;28:2–12. doi: 10.1111/j.1600-9657.2011.01103.x. [DOI] [PubMed] [Google Scholar]
- 5.Andersson L., Andreasen J.O., Day P. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent Traumatol. 2012;28:88–96. doi: 10.1111/j.1600-9657.2012.01125.x. [DOI] [PubMed] [Google Scholar]
- 6.Oikarinen K.S. Splinting of traumatized teeth. In: Andreasen J.O., editor. Textbook and Color Atlas of Traumatic Injuries to the Teeth. 4th ed. Wiley-Blackwell; Oxford: 2007. pp. 842–851. [Google Scholar]
- 7.Mazzoleni S., Meschia G., Cortesi R. In vitro comparison of the flexibility of different splint systems used in dental traumatology. Dent Traumatol. 2010;26:30–36. doi: 10.1111/j.1600-9657.2009.00843.x. [DOI] [PubMed] [Google Scholar]
- 8.Kim Y.K., Park H.S., Kim K.H., Kwon T.Y. Effect of adhesive resin flexibility on enamel fracture during metal bracket debonding: an ex vivo study. Eur J Orthod. 2015;37:550–555. doi: 10.1093/ejo/cju086. [DOI] [PubMed] [Google Scholar]
- 9.Takamizawa T., Barkmeier W.W., Tsujimoto A. Mechanical properties and simulated wear of provisional resin materials. Oper Dent. 2015;40:603–613. doi: 10.2341/14-132-L.1. [DOI] [PubMed] [Google Scholar]