Abstract
Background/purpose
Inadequacy to locate the second mesiobuccal canal (MB2) canal leads to the highest probability of endodontic failure in permanent maxillary first molars (PMFMs) and still remains a constant challenge for many clinicians. The aim of this study was to characterize the geometrical features between MB2 and other orifices of examined PMFMs using cone-beam computed tomography images.
Materials and methods
A total of 108 teeth qualified in the cone-beam computed tomography image archives were enrolled in the present study. The intersecting point (T) was determined as the perpendicular line (h, altitude of triangle) projected from the vertex of the MB2 canal orifice to mesiobuccal canal orifice-palatal canal orifice line (MB1-P). We measured the geometric features of PMFMs with the MB2 canal, including the interorifice distances, area, altitude, and the ratio between the canal orifices.
Results
The average interorifice distance was found to be 1.91 ± 0.59 mm for MB1-MB2, 5.73 ± 0.66 mm for MB1-P, and 4.11 ± 0.79 mm for MB2-P, with significant gender difference for MB1-MB2 distance. For the MB1-T distance, a significant difference was found between genders (P = 0.02), with males averaging 1.78 ± 0.07 mm, and females 1.48 ± 0.11 mm. For the MB1-P distance, the majorities of both genders were found in the 20–40% cut-off. A portion of the males exhibited a tendency towards the 40–80% cut-off, while females shifted in the reverse direction towards the 0–20% cut-off.
Conclusion
In clinical scenarios, these anatomical characteristics of the root canals system could be beneficial to locating the MB2 canal.
Keywords: cone-beam computed tomography, maxillary molar, morphology, root canal
Introduction
One of the most common causes of endodontic treatment failure is inadequate diagnosis and treatment planning of the treated tooth, including lack of comprehensive knowledge about the morphological characteristics and their frequent variations of the entire root canal system.1 Therefore, a prerequisite for successful root canal treatment depends on a clinician’s ability to locate, clean, shape, and fill the entire canal system in all dimensions.1
Studies focused on the form, configuration, and number of root canals of maxillary molar teeth have been discussed for decades.2, 3, 4, 5, 6 The permanent maxillary first molars (PMFMs) are teeth that present substantial heterogeneity abnormalities in the root canal system.2, 4, 6, 7 Among these reported abnormalities, the presence of unexpected canals, such as a second mesiobuccal canal (MB2), has drawn much attention in clinical settings and in laboratory investigations.2, 4, 6, 7, 8, 9 Inadequate treatment of MB2 canal leads to the highest probability of endodontic failure in PMFMs and still remains a constant challenge for many clinicians.2, 4, 6, 8, 9, 10
The potential applications of cone-beam computed tomography (CBCT) has gained increasing significance for diagnosis, treatment, and follow-up in the field of endodontics.11, 12 CBCT has the capacity to eliminate superimposition of surrounding structures and generate undistorted three-dimensional images of intricate structures such as teeth and their surrounding tissue from the axial, sagittal, and coronal sections.11, 12 Thus, CBCT has been extensively employed recently to study root and canal morphologic variations in different populations.5, 10, 13, 14, 15, 16, 17, 18, 19, 20, 21
Several studies have used CBCT to investigate the prevalence and morphology of the MB2 canal of PMFMs in various ethnicities.5, 10, 13, 14, 15, 16, 17, 18, 19, 20, 21 However, to our knowledge, limited study has been undertaken to evaluate the geometrical location of the MB2 canal at the orifice level,8, 9, 22 and the relationship between the orifices of mesiobuccal canals (MB1 and MB2), and the palatal canal (P) in PMFMs have yet to be examined in depth.
Considering the lack of detailed information on this topic, the purpose of this study was to characterize the geometrical location and relationships between the MB2 canal and other orifices of examined PMFMs via CBCT images.
Materials and methods
Image acquisition and retrieved
All CBCT images selected in this study were retrieved from Digital Imaging and Communications in Medicine (DICOM) archives possessed by the Department of Dentistry, Tri-Service General Hospital, Taipei, Taiwan. The project and protocol were independently approved by the Institutional Review Board of Tri-Service General Hospital, National Defense Medical Center (TSGHIRB Number 2-105-05-078). CBCT images were taken as part of the dental diagnostic, examination, and/or treatment records from January 2012 to December 2016. Notably, no patients were contacted and no CBCTs were specifically taken for the objectiveness of this project.
Without sacrificing image quality and following the “as low as reasonably achievable” principle, the images were acquired by board-certified radiologists operating a CBCT machine (NewTom 5G; QR, Verona, Italy) with the X-ray tube at an accelerated potential of 110 kV peak, a beam current of 11.94 mA with an automatic adjustment to exposure time according to the area of the scan (about 7 seconds for a full arch).23 The field of view was fixed at 30.5 cm2 × 20.3 cm2 with the resolution and separation of each slice at 0.15 mm. The CBCT scans were saved in DICOM format and this data was encrypted to protect confidentiality.
Inclusion and exclusion criteria of selected images
The inclusion and exclusion criteria were adapted from previous studies with some modification:5, 9 (1) each individual has at least one fully erupted permanent maxillary first and second molar; (2) each investigated tooth has normal position and alignment; and (3) each investigated tooth has the apex fully formed. Images were excluded if they contained: (1) previous root canal fillings, posts, or fixed prosthesis restoration; (2) unclear or incomplete image due to scattering, or beam-hardening artifacts; (3) pathological lesions, calcification or evident root resorption attached with analyzed tooth; or (4) evidence of previous radiectomy or periapical surgery.
Morphologic analysis
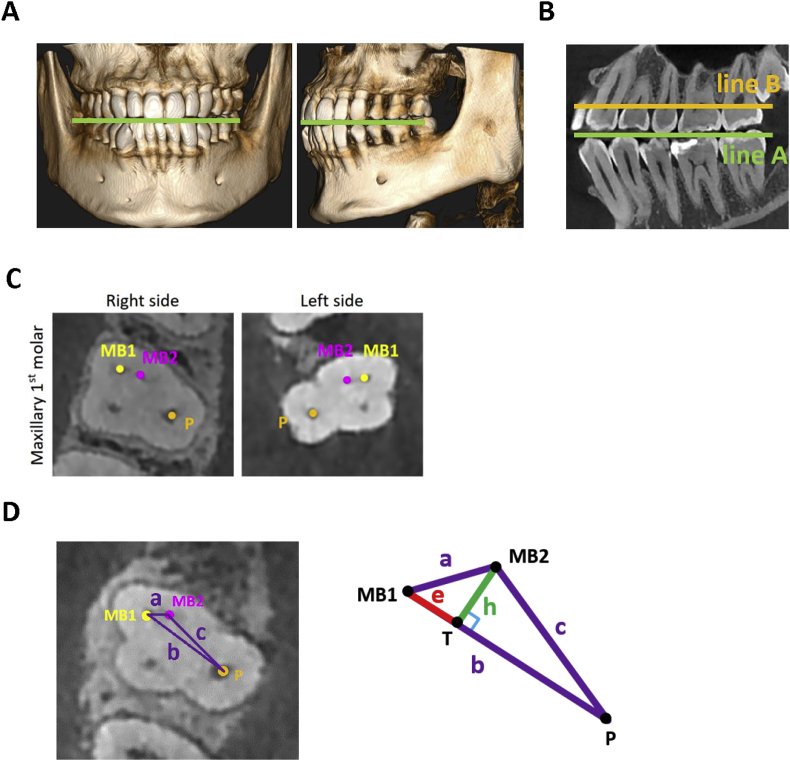
Of the 380 initially examined CBCT images, 255 qualified images of PMFMs were analyzed in detail using ImplantMax software (HiAim Biomedical Technology, Taipei, Taiwan). All qualified images were reoriented so that the maxilla was bilaterally symmetrical and the occlusal plane, either in frontal or sagittal view, was parallel to the ground (Figure 1A). The long axis of the investigated molar (indicated as a green line) was adjusted to be perpendicular to the ground floor. Afterwards, two horizontal lines were drawn with line A parallel to the inferior border of the cementoenamel junction, and line B to indicate the pulp chamber floor (Figure 1B).9 An image of chamber floor was arbitrarily designated as the first 2D slice on which all orifices were present (Figure 1C) and a series of images were evaluated at the level of the root canal orifice by axial sections. The horizontal distance between the center of identified orifices was measured on the orifice level (after identifying the MB2 canal; Figure 1C).
Figure 1.
Schematic description of the steps of image orientation and illustration of the measurement parameters. (A) Skull orientation and region of interest from coronal and lateral view; (B) after the tooth orientation (the long axis of the tooth shown as the green line), a slice was selected and determined as reference line A and line B, of which line A is defined as a horizontal line parallel to the inferior border of the cementoenamel junction, and line B is defined as another parallel horizontal line immediately adjacent to pulp chamber floor; (C) cross-section of cone-beam computed tomography image of the each orifice of the maxillary first with a second mesiobuccal canal (MB2); (D) illustrations of geometric parameters of right permanent maxillary first molars. The interorifice distance (a, b, c), altitude of triangle (h), and MB1-T distance (e) were measured. The distance in the lines drawn between the points was measured in mm. P = palatal canal; T = the intersecting point.
Geometric measurements
For the interorifice distances (IODs), straight lines were projected in PMFMs with the MB2 canal, joining different points: MB1 to MB2, MB1-MB2 line (a); MB1 to P, MB1-P line (b, base of triangle); MB2 to P, MB2-P line (c; Figure 1D).
To calculate the area of the surface bounded by the central points of each orifice, the area of the triangle can be calculated using Heron's formula:
where a, b, and c are the lengths of the three sides of the triangle and s is the semiperimeter of the triangle defined by
To determine the geometric location of the MB2 canal in relation to the MB1 canal and the P canal at the orifice level, a fourth line (MB2-T) was drawn from the vertex where the MB2 canal orifice is perpendicular to the MB1-P line. Following a previously described protocol,8, 9, 24 the intersecting point was determined as point T, and the perpendicular line, MB2-T line, is the altitude (h) of the triangle. The distance between the intersecting point T to MB1 (e) was also determined (Figure 1D). The distances of the lines drawn between the orifices and points were measured in millimeters.
The following information was evaluated for PMFMs with MB2 canal:
(1) the distances (a, b, c) and perimeter (s) between the MB1, P, and MB2 root canal orifices; (2) the area of triangle (A) formed by the MB1, P, and MB2 root canal orifices; (3) measurements of the triangle's h and h to b ratio (h/b ratio); where 100% denotes close proximity to the P canal; and (4) the distance of MB1-T (e), and the MB1-T (e) to b ratio (e/b ratio).
Data acquisition and validation
All images were displayed on a 19-inch LCD monitor (ChiMei, Innolux Corporation, Tainan, Taiwan) with a 1920 × 1080 pixel resolution. All reoriented images were inspected in a dimly lit environment by two calibrated examiners (C.-C. Su, and Y.-C. Wu). After calibration, the two examiners separately evaluated the images, and any disagreement in the interpretation of images was discussed until a consensus was reached. To assure data reliability, the intraexaminer and interexaminer calibration were performed for nominal and continuous variables to assess data reliability based on the anatomic diagnosis of CBCT images by evaluation of 20 randomly selected images. The intraexaminer and interexaminer analysis was performed before the disagreements among examiners were discussed and resolved.25 The kappa statistic values were 0.967 and 0.958 for intraobserver and interobserver agreement, respectively. The measurement errors, intraclass correlation coefficient, and Cronbach α values were also performed to check the reliability of intraobservations and interobservations for continuous variables measurement.
Statistical analysis
Descriptive statistics were expressed as mean values and standard deviations (mean ± standard deviation), frequencies, or percentages, as appropriate to each measurement calculated. To compare the mean values of continuous variables (i.e., distances), a one-way analysis of variance test and a Fisher exact test were performed to examine differences in the variables. All statistical analysis was performed using a statistical package SPSS for Windows (Version 22.0; SPSS, Inc., Chicago, IL, USA). The level of statistical significance was set at P < 0.05.
Results
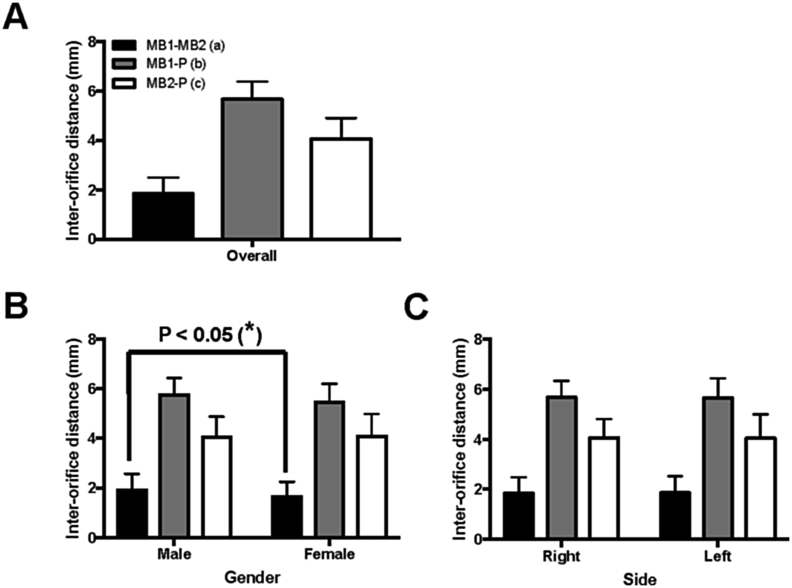
Of the total 108 teeth surveyed, 80 were from males (74.1%) and 28 were from females (25.9%). In this batch, 57 were from the right side (52.8%) and 51 from the left side (47.2%). The average IODs were found to be 1.91 ± 0.59 mm for MB1-MB2 (a), 5.73 ± 0.66 mm for MB1-P (b), and 4.11 ± 0.79 mm for MB2-P (c) (Figure 2A). The average IODs in males were 1.98 ± 0.60 mm, 5.80 ± 0.64 mm, and 4.11 ± 0.77 mm for MB1-MB2 (a), MB1-P (b), and MB2-P (c), respectively (Figure 2B). For females, the average IODs were 1.71 ± 0.54 mm, 5.52 ± 0.69 mm, and 4.13 ± 0.85 mm for MB1-MB2 (a), MB1-P (b), and MB2-P (c), respectively (Figure 2C). No significant differences were found between males and females (Figure 2B) and right or left side (Figure 2C), except for the MB1-MB2 (a) distance between males and females (P < 0.05, Figure 2B).
Figure 2.
The distribution of interorifice distances (IODs) of MB1-MB2 (a), MB1-P (b), and MB2-P (c) in permanent maxillary first molars (PMFMs). (A) The distribution of IODs of all investigated molar teeth; (B) the distribution of IODs of PMFMs with MB2 canal between males and females; (C) the distribution of IODs of PMFMs with MB2 canal between right and left. Bars and lines show the mean ± standard deviation. Statistical analyses were performed with one-way analysis of variance and the level of statistical significance was set at P < 0.05.
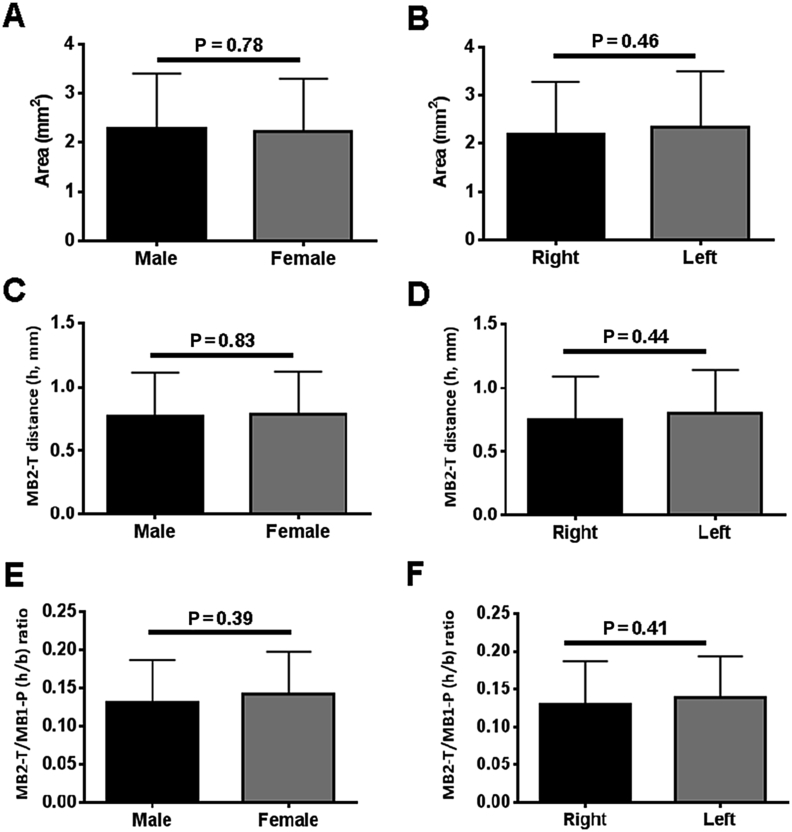
The average area of the triangle (A, in mm2) was found to be 2.28 ± 0.13 mm2 in males, 2.21 ± 0.20 mm2 in females, with no significant differences (P = 0.78, Figure 3A). The average area of the triangle (A, in mm2) for the right side was 2.19 ± 0.14 mm2 while the left side was 2.35 ± 0.16 mm2, with no significant differences (P = 0.46, Figure 3B).
Figure 3.
Comparison of gender and side differences of the area of triangle, length of MB2-T , and MB2-T/MB1-P ratio. (A, B) Analysis of area of triangle in (A) males and females; (B) right and left. (C, D) Analysis of length of MB2-T in (C) males and female; (D) right and left. (E, F) Analysis of MB2-T/MB1-P ratio in (E) males and females; (F) right and left. Bars and lines show the mean ± standard deviation. Statistical analyses were performed and the level of statistical significance was set at P < 0.05.
For the h of the triangle (in mm), no significant differences were found between gender (P = 0.83, Figure 3C) or side (P = 0.44, Figure 3D). For the MB2-T/MB1-P (h/b) ratio, no significant differences were found between gender (P = 0.39, Figure 3E) or side (P = 0.41, Figure 3F). Regarding the percentile cut-off of the h/b ratio (Table 1), there were also no significant differences found between gender (P = 0.32) or side (P = 0.38, Table 1).
Table 1.
The percentile cutoffs for the altitude to base ratio (h/b ratio) of permanent maxillary first molars with MB2 canal in gender (male vs. female) and side (right vs. left).
| h/b ratio (%) | 0–20 (%) | 20–40 (%) | 40–60 (%) | 60–80 (%) | 80–100 (%) | P |
|---|---|---|---|---|---|---|
| Gender, n (%) | 0.32 | |||||
| Male (n = 80) | 72 (90%) | 8 (10%) | 0 | 0 | 0 | |
| Female (n = 28) | 23 (82.1%) | 5 (17.9%) | 0 | 0 | 0 | |
| Side, n (%) | 0.38 | |||||
| Right (n = 57) | 52 (91.2%) | 5 (8.8%) | 0 | 0 | 0 | |
| Left (n = 51) | 43 (84.3%) | 8 (15.7%) | 0 | 0 | 0 | |
The level of statistical significance was set at P < 0.05.
MB2 = second mesiobuccal canal.
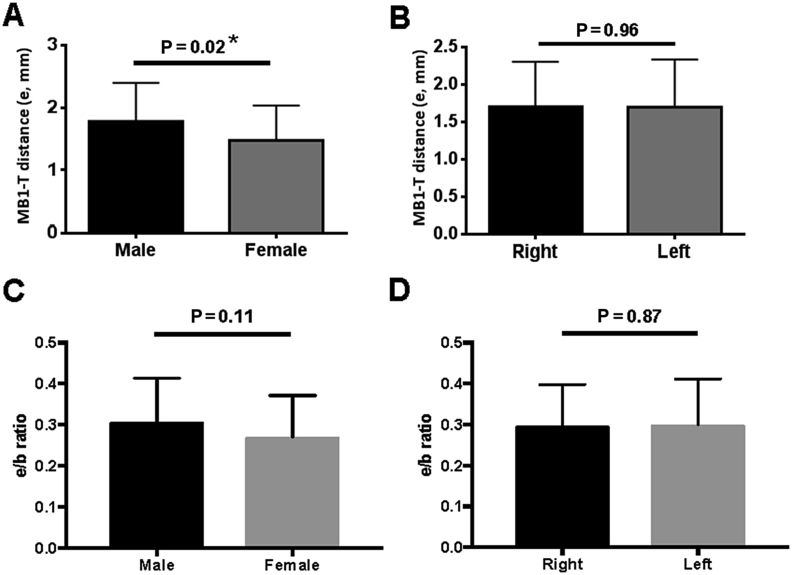
For the MB1-T distance (e, in mm), the average MB1-T distance was 1.70 ± 0.61 mm. A significant difference was found between genders (P = 0.02), with males averaging 1.78 ± 0.07 mm, longer on average than females at 1.48 ± 0.11 mm (Figure 4A).
Figure 4.
Analysis of area of MB-1-T distance (e, mm) between (A) males and females, and (B) right versus left, and distribution of MB1-T/MB1-P (e/b) ratio between (C) males and females, and (D) right versus left. Bars and lines show the mean ± standard deviation. Statistical analyses were performed and the level of statistical significance was set at P < 0.05. *, < 0.05.
A significant gender difference was found (P = 0.03) in the percentile cut-off, with the majority of both genders found in the 20–40% cut-off (Table 2). A portion of males exhibited prevalence towards 40–80% cutoff, with 17.5% and 1.3% found in the 40–60% and 60–80% cut-offs, respectively (Table 2). On the contrary, almost a third of females shifted in the reverse direction, towards the 0–20% cut-off (32.1%). These results suggest that MB2 orifices appear with greater frequency towards P orifices in males than females. Additionally, left orifices also had a tendency towards P canals, but with no significant differences (P = 0.75, Table 2). No significant differences were found between gender (P = 0.11) or site (P = 0.87, Figure 4B) for MB1-T/MB1-P (e/b) ratio.
Table 2.
The percentile cutoffs for the MB1-T (e) to base ratio (e/b ratio) of permanent maxillary first molars with MB2 canal in gender (male vs. female) and side (right vs. left).
| e/b ratio | 0–20 (%) | 20–40 (%) | 40–60 (%) | 60–80 (%) | 80–100 (%) | P |
|---|---|---|---|---|---|---|
| Gender, n (%) | 0.03* | |||||
| Male (n = 80) | 10 (12.5%) | 55 (68.7%) | 14 (17.5%) | 1 (1.3%) | 0 | |
| Female (n = 28) | 9 (32.1%) | 16 (57.1%) | 3 (10.8%) | 0 | 0 | |
| Side, n (%) | 0.75 | |||||
| Right (n = 57) | 9 (15.8%) | 38 (66.7%) | 10 (17.5%) | 0 | 0 | |
| Left (n = 51) | 10 (19.6) | 33 (64.7%) | 7 (13.7%) | 1 (2.0) | 0 | |
The level of statistical significance was set at P < 0.05. * P < 0.05.
MB1 = first mesiobuccal canal; MB2 = second mesiobuccal canal.
Discussion
To the best of our knowledge, this is the first study to provide a detailed description of the geometric relationships between the orifices of mesiobuccal canals (MB1 and MB2), and the P canal in PMFMs. The present study shows significant gender differences in the location of the MB2 canal orifice in PMFMs through analyzing CBCT images. Moreover, the results revealed a higher frequency of PMFMS MB2 canal orifice to appear in close proximity of the P canal orifice in males over females. These findings also highlight CBCT as a highly useful tool in aiding clinicians towards locating the orifice of MB2 canals in PMFM, through noninvasive exploration and identification of canal orifices in the intricate root canal anatomy of maxillary molar teeth. Our results provide clinical value in identifying the location of MB2 canals.
Although periapical radiography is most commonly used in clinics, various noninvasive imaging technologies such as CBCT have been introduced to investigate root and canal details. The fidelity of CBCT imaging and measurements is shown to be highly accurate, and comparable with staining and clearing techniques used to study extracted teeth in vitro.3, 4, 7, 11, 12, 26 Currently, increasing numbers of studies have extensively employed CBCT imaging to detect the presence of the MB2 canal in PMFMs.8, 9, 10 Although limiting factors, such as the presence of metallic posts or root canal fillings (i.e., gutta-percha, AH 26 sealer), can interfere with the image quality of CBCT, these images can still provide highly precise three-dimensional information regarding the morphological characteristics of a complex root and root canal system. In determining a MB2 canal of maxillary molars in three dimensions, CBCT images have demonstrated superior accuracy to conventional periapical films.7, 10, 21, 26 Other advanced diagnostic modalities such as dental loupes,27 and dental microscopes,28, 29 have also been applied as noninvasive approaches in assessing the presence of an MB2 canal of maxillary molars. However, these microsurgical devices alone are insufficient at locating the MB2 canal in every case.30 A recent prospective clinical study demonstrated that the use of the dental operating microscope in conjunction with selective troughing and CBCT imaging allowed clinicians to locate only 90% (maxillary first molars) of MB2 canals, suggesting the effectiveness of CBCT to be limited.10 These findings promote the importance of utilizing multiple diagnostic tools when attempting to locate the MB2 canal. Clinicians should familiarize themselves with magnification equipment and new diagnostic imaging technology, such as CBCT scanning, to provide themselves with detailed information of anatomic variations for endodontic treatment.
To better determine the optimal access pathway to canal orifices in clinical practice, we measured the distances between each orifice in PMFMs (Figure 2A). Several studies have indicated PMFMs with MB2 canal as one of the most complicated to negotiate during root canal treatment.10, 31, 32 Inability to recognize, locate, and treat MB2 canals adequately in maxillary molars may result in the persistence of intracanal microorganisms colonization, which leads to long term treatment failure.10, 31, 32 Although the prevalence and factors affecting the negotiability of the MB2 in PMFMs have been discussed for decades,22, 24, 29, 33, 34, 35 there is little research about the geometric location of the MB2 canal in PMFMs. The geometric location of the MB2 canal has only been reported using in vitro studies,22, 24, 34, 35, 36 however, limited results revealed the efficiency of CBCT on MB2 canal location maxillary molars in vivo.8, 9 Our study intends to expand the knowledge of the geometric relationship between the MB2 canal and other orifices of PMFMs at the orifice level. In this study, we observed that the MB2 canal was located 1.70 ± 0.61 mm palatally and 1.91 ± 0.59 mm mesially to the MB1 canal in the PMFMs (Figure 2A). Additionally, a significant gender difference was found in MB1-MB2 (a) distance (P < 0.05, Figure 2B). Using the same technique, Betancourt et al8 found it to be 1.25 ± 0.34 mm palatally and 2.69 ± 0.49 mm mesially to the MB1 canal. Gorduysus et al24 determined the location of the MB2 canal in 45 extracted maxillary molars and found these measurements, 1.65 ± 0.72 mm palatally and 1.81 ± 0.38 mm mesially to the MB1 canal, in a combined study of first and second molars. In summary, the MB2 orifice always appears in a mesial and P direction in reference to the MB1 orifice.
In this study, males have a significantly longer MB1-T (e) distance than females (1.78 ± 0.07 mm vs. 1.48 ± 0.11 mm, Figure 4A); however, the distance may also be influenced by external crown size and morphology. Therefore, the MB1-T/MB1-P (e/b) ratio was established to determine the geometric location of the MB2 canal on orifice level properly. Through direct inspection, an MB2 canal orifice located close to the MB orifice in the buccolingual direction, and slightly mesial to the line between the MB and P canal orifices, is the most frequently observed morphology in clinical practice.37 Our study is the first to determine the percentile cut-off between MB1-T/MB1-P (e/b) ratio, observing males to have a disposition of MB2 canals closer to the P canal orifice compared with females (Table 2). These results remarked that the location of the MB2 canal varied not only in relation to the main mesiobuccal canal, but also another reference point, the P canal orifice.
Our data provides the geometric location of the MB2 canal at the orifice level, which may indicate that the enlargement of the access preparation or modification of access shape for molars with an MB2 canal is necessary. From a clinical point of view, these findings are relevant to the design of cavity access; a tooth with an MB2 canal would require a more rhomboidal access preparation as opposed to the classic triangular shape.37 Consequently, a modified access preparation would allow for easier positioning of instruments and filling materials. Further studies should be conducted to investigate the exact anatomic coordination between each orifice and its impact on access preparation and external crown morphology.
In conclusion, the clinical significance of the results presents critical information on the geometric features of PMFMs with an MB2 canal at the orifice level via CBCT images. In clinical scenarios, the anatomical characteristics of these root canal systems could be beneficial in locating the MB2 canal, influencing the design of cavity access and the effectiveness of endodontic debridement.
Conflicts of interest
The authors declare no conflicts of interest related to this study.
Acknowledgments
This work was supported by research grants from the Tri-Service General Hospital, Taipei, Taiwan (TSGH-C104-165, TSGH-C105-030, MAB-105-100). The authors appreciate Mr. Yu-Feng Lin (Hi-Aim Biomedical Technology Inc.), Ms. Yi-Shing Lin, and Ms. Li-Chin Yu (Tri-Service General Hospital) for their help in CBCT taking and imaging processing, and Ms. Jing-Shu Huang and Mr. Shao-Wen Tou (School of Public Health, National Defense Medical Center) for their valuable contribution in statistical analysis and consultation. We also thank Ms. Katherine Shao-Tzu Chang (School of Dentistry, National Defense Medical Center) for her help in manuscript editing. The founders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Hammad M., Qualtrough A., Silikas N. Evaluation of root canal obturation: a three-dimensional in vitro study. J Endod. 2009;35:541–544. doi: 10.1016/j.joen.2008.12.021. [DOI] [PubMed] [Google Scholar]
- 2.Spagnuolo G., Ametrano G., D'Anto V. Microcomputed tomography analysis of mesiobuccal orifices and major apical foramen in first maxillary molars. Open Dent J. 2012;6:118–125. doi: 10.2174/1874210601206010118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Han X., Yang H., Li G., Yang L., Tian C., Wang Y. A study of the distobuccal root canal orifice of the maxillary second molars in Chinese individuals evaluated by cone-beam computed tomography. J Appl Oral Sci. 2012;20:563–567. doi: 10.1590/S1678-77572012000500012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corbella S., Del Fabbro M., Tsesis I., Taschieri S. Computerized tomography technique for the investigation of the maxillary first molar mesiobuccal root. Int J Dent. 2013;2013:614898. doi: 10.1155/2013/614898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tian X.M., Yang X.W., Qian L., Wei B., Gong Y. Analysis of the root and canal morphologies in maxillary first and second molars in a Chinese population using cone-beam computed tomography. J Endod. 2016;42:696–701. doi: 10.1016/j.joen.2016.01.017. [DOI] [PubMed] [Google Scholar]
- 6.Cleghorn B.M., Christie W.H., Dong C.C. Root and root canal morphology of the human permanent maxillary first molar: a literature review. J Endod. 2006;32:813–821. doi: 10.1016/j.joen.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 7.Mirmohammadi H., Mahdi L., Partovi P., Khademi A., Shemesh H., Hassan B. Accuracy of cone-beam computed tomography in the detection of a second mesiobuccal root canal in endodontically treated teeth: an ex vivo study. J Endod. 2015;41:1678–1681. doi: 10.1016/j.joen.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 8.Betancourt P., Navarro P., Munoz G., Fuentes R. Prevalence and location of the secondary mesiobuccal canal in 1,100 maxillary molars using cone beam computed tomography. BMC Med Imaging. 2016;16:66. doi: 10.1186/s12880-016-0168-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Betancourt P., Navarro P., Cantin M., Fuentes R. Cone-beam computed tomography study of prevalence and location of MB2 canal in the mesiobuccal root of the maxillary second molar. Int J Clin Exp Med. 2015;8:9128–9134. [PMC free article] [PubMed] [Google Scholar]
- 10.Parker J., Mol A., Rivera E.M., Tawil P. CBCT uses in clinical endodontics: the effect of CBCT on the ability to locate MB2 canals in maxillary molars. Int Endod J. 2016 Dec 15 doi: 10.1111/iej.12736. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Rosen E., Taschieri S., Del Fabbro M., Beitlitum I., Tsesis I. The diagnostic efficacy of cone-beam computed tomography in endodontics: a systematic review and analysis by a hierarchical model of efficacy. J Endod. 2015;41:1008–1014. doi: 10.1016/j.joen.2015.02.021. [DOI] [PubMed] [Google Scholar]
- 12.Patel S., Durack C., Abella F., Shemesh H., Roig M., Lemberg K. Cone beam computed tomography in Endodontics–a review. Int Endod J. 2015;48:3–15. doi: 10.1111/iej.12270. [DOI] [PubMed] [Google Scholar]
- 13.Sert S., Bayirli G.S. Evaluation of the root canal configurations of the mandibular and maxillary permanent teeth by gender in the Turkish population. J Endod. 2004;30:391–398. doi: 10.1097/00004770-200406000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Guo J., Vahidnia A., Sedghizadeh P., Enciso R. Evaluation of root and canal morphology of maxillary permanent first molars in a North American population by cone-beam computed tomography. J Endod. 2014;40:635–639. doi: 10.1016/j.joen.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 15.Zheng Q.H., Wang Y., Zhou X.D., Wang Q., Zheng G.N., Huang D.M. A cone-beam computed tomography study of maxillary first permanent molar root and canal morphology in a Chinese population. J Endod. 2010;36:1480–1484. doi: 10.1016/j.joen.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 16.Pattanshetti N., Gaidhane M., Al Kandari A.M. Root and canal morphology of the mesiobuccal and distal roots of permanent first molars in a Kuwait population–a clinical study. Int Endod J. 2008;41:755–762. doi: 10.1111/j.1365-2591.2008.01427.x. [DOI] [PubMed] [Google Scholar]
- 17.Kim Y., Lee S.J., Woo J. Morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a Korean population: variations in the number of roots and canals and the incidence of fusion. J Endod. 2012;38:1063–1068. doi: 10.1016/j.joen.2012.04.025. [DOI] [PubMed] [Google Scholar]
- 18.Lee J.H., Kim K.D., Lee J.K. Mesiobuccal root canal anatomy of Korean maxillary first and second molars by cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:785–791. doi: 10.1016/j.tripleo.2010.11.026. [DOI] [PubMed] [Google Scholar]
- 19.Silva E.J., Nejaim Y., Silva A.I., Haiter-Neto F., Zaia A.A., Cohenca N. Evaluation of root canal configuration of maxillary molars in a Brazilian population using cone-beam computed tomographic imaging: an in vivo study. J Endod. 2014;40:173–176. doi: 10.1016/j.joen.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 20.Plotino G., Tocci L., Grande N.M. Symmetry of root and root canal morphology of maxillary and mandibular molars in a white population: a cone-beam computed tomography study in vivo. J Endod. 2013;39:1545–1548. doi: 10.1016/j.joen.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 21.Zhang R., Yang H., Yu X., Wang H., Hu T., Dummer P.M. Use of CBCT to identify the morphology of maxillary permanent molar teeth in a Chinese subpopulation. Int Endod J. 2011;44:162–169. doi: 10.1111/j.1365-2591.2010.01826.x. [DOI] [PubMed] [Google Scholar]
- 22.Tuncer A.K., Haznedaroglu F., Sert S. The location and accessibility of the second mesiobuccal canal in maxillary first molar. Eur J Dent. 2010;4:12–16. [PMC free article] [PubMed] [Google Scholar]
- 23.Sung C.E., Cochran D.L., Cheng W.C. Preoperative assessment of labial bone perforation for virtual immediate implant surgery in the maxillary esthetic zone: a computer simulation study. J Am Dent Assoc. 2015;146:808–819. doi: 10.1016/j.adaj.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 24.Gorduysus M.O., Gorduysus M., Friedman S. Operating microscope improves negotiation of second mesiobuccal canals in maxillary molars. J Endod. 2001;27:683–686. doi: 10.1097/00004770-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Landis J.R., Koch G.G. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33:363–374. [PubMed] [Google Scholar]
- 26.Vizzotto M.B., Silveira P.F., Arus N.A., Montagner F., Gomes B.P., da Silveira H.E. CBCT for the assessment of second mesiobuccal (MB2) canals in maxillary molar teeth: effect of voxel size and presence of root filling. Int Endod J. 2013;46:870–876. doi: 10.1111/iej.12075. [DOI] [PubMed] [Google Scholar]
- 27.Hasan M., Raza Khan F. Determination of frequency of the second mesiobuccal canal in the permanent maxillary first molar teeth with magnification loupes (× 3.5) Int J Biomed Sci. 2014;10:201–207. [PMC free article] [PubMed] [Google Scholar]
- 28.Das S., Warhadpande M.M., Redij S.A., Jibhkate N.G., Sabir H. Frequency of second mesiobuccal canal in permanent maxillary first molars using the operating microscope and selective dentin removal: a clinical study. Contemp Clin Dent. 2015;6:74–78. doi: 10.4103/0976-237X.149296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yoshioka T., Kikuchi I., Fukumoto Y., Kobayashi C., Suda H. Detection of the second mesiobuccal canal in mesiobuccal roots of maxillary molar teeth ex vivo. Int Endod J. 2005;38:124–128. doi: 10.1111/j.1365-2591.2004.00918.x. [DOI] [PubMed] [Google Scholar]
- 30.Stropko J.J. Canal morphology of maxillary molars: clinical observations of canal configurations. J Endod. 1999;25:446–450. doi: 10.1016/S0099-2399(99)80276-3. [DOI] [PubMed] [Google Scholar]
- 31.Wolcott J., Ishley D., Kennedy W., Johnson S., Minnich S. Clinical investigation of second mesiobuccal canals in endodontically treated and retreated maxillary molars. J Endod. 2002;28:477–479. doi: 10.1097/00004770-200206000-00016. [DOI] [PubMed] [Google Scholar]
- 32.Wolcott J., Ishley D., Kennedy W., Johnson S., Minnich S., Meyers J.A. 5 yr clinical investigation of second mesiobuccal canals in endodontically treated and retreated maxillary molars. J Endod. 2005;31:262–264. doi: 10.1097/01.don.0000140581.38492.8b. [DOI] [PubMed] [Google Scholar]
- 33.Ibarrola J.L., Knowles K.I., Ludlow M.O., McKinley I.B., Jr. Factors affecting the negotiability of second mesiobuccal canals in maxillary molars. J Endod. 1997;23:236–238. doi: 10.1016/S0099-2399(97)80054-4. [DOI] [PubMed] [Google Scholar]
- 34.Peeters H.H., Suardita K., Setijanto D. Prevalence of a second canal in the mesiobuccal root of permanent maxillary first molars from an Indonesian population. J Oral Sci. 2011;53:489–494. doi: 10.2334/josnusd.53.489. [DOI] [PubMed] [Google Scholar]
- 35.Degerness R., Bowles W. Anatomic determination of the mesiobuccal root resection level in maxillary molars. J Endod. 2008;34:1182–1186. doi: 10.1016/j.joen.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 36.Zhang C.F., Ding R.Y., Yin X.Z., Zhao B.H., Lin Q.G. Location and negotiation of second mesiobuccal canals in maxillary molars. Zhonghua Kou Qiang Yi Xue Za Zhi. 2003;38:86–88. [PubMed] [Google Scholar]
- 37.Weller R.N., Hartwell G.R. The impact of improved access and searching techniques on detection of the mesiolingual canal in maxillary molars. J Endod. 1989;15:82–83. doi: 10.1016/s0099-2399(89)80114-1. [DOI] [PubMed] [Google Scholar]