ERCP is the gold standard method for biliary drainage. Alternative methods such as the percutaneous transhepatic biliary drainage (PTBD) or surgery have a higher rate of complications.
Hepaticogastrostomy under EUS (EUS-HGS) drainage was developed in 2001 as an additional alternative to PTBD and ERCP.[1,2,3,4]
In this case, we report hepaticogastrostomy for a patient who has undergone a gastric bypass surgery to treat obesity with a new stent design.
A 64-year-old female patient with a history of gastric bypass with esophagojejunal anastomosis and with 6 months of progressive weight loss, abdominal pain, anorexia, jaundice, and asthenia was sent to our medical center [Figure 1].
Figure 1.

Pancreatic mass on CT scan
A 50-mm mass with infiltration of the mesenteric artery and vein was observed in the pancreatic head on computed tomography; this was associated with the dilatation of the main pancreatic and the common bile ducts. EUS-guided fine-needle aspiration performed in a left lateral position with intubation (22G needle, Cook medical) suggested a diagnosis of pancreatic adenocarcinoma
Drainage by hepaticogastrostomy [Video 1] was performed at the level of the gastric stump in a supine position. Segment III was punctured and a partially covered 10-cm HANARO stent, designed by MI tech in association with Dr. Poincloux, was inserted. The patient was discharged after one night of hospitalization and received chemotherapy after 15 days (four cycles of Folfirinox) [Figures 2‑4].
Figure 2.

CT scan after EUS-HGS
Figure 4.
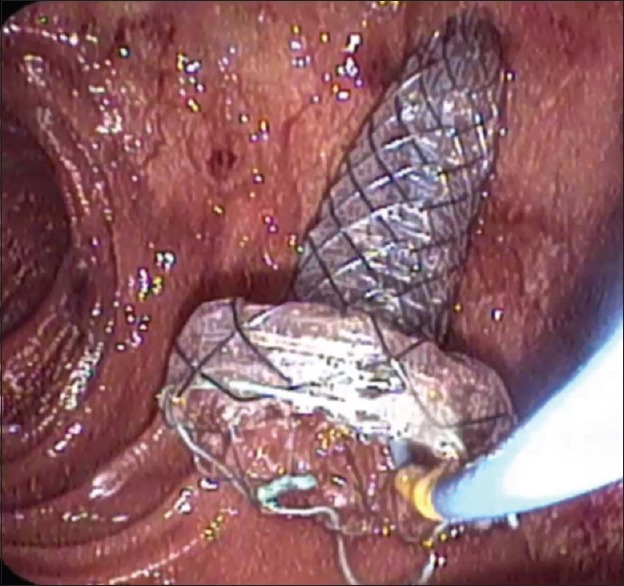
Endoscopic view of the proximal part of the stent
Figure 3.
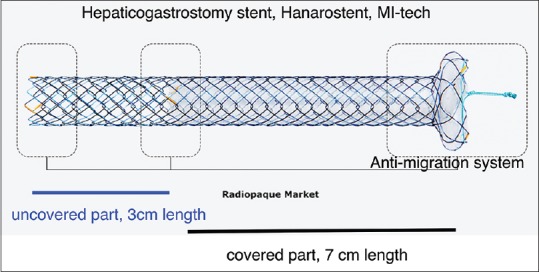
Description of the MI-tech stent
DISCUSSION
Patients with altered anatomy represent a challenge for biliary drainage. Deep enteroscopy-assisted ERCP for Roux-en-Y gastric bypass surgery has a success rate of 63%, and it depends on the length of the Roux limb.[5] Gastric bypass surgery with excluded stomach is a new challenge for biliary drainage. ERCP through a gastrostomy into the excluded stomach could allow success in 60% of cases.[6]
Another drainage technique in two steps with the creation of a transgastric fistula first to access the papilla with a duodenoscope has recently been described.[7]
In our case, drainage with EUS-HGS represents a new indication of EUS-HGS (not yet described after gastric bypass surgery) and has the advantage of involving only one step. The design of this new stent with a long covered portion (7 cm) and a flap to avoid migration probably facilitates drainage.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has provided her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
Laurent Poincloux who participated in the design of the stent has no financial disclosure to declare. There are no other conflicts of interest.
Video Available on: www.eusjournal.com
REFERENCES
- 1.Giovannini M, Moutardier V, Pesenti C, et al. Endoscopic ultrasoundguided bilioduodenal anastomosis: A new technique for biliary drainage. Endoscopy. 2001;33:898–900. doi: 10.1055/s-2001-17324. [DOI] [PubMed] [Google Scholar]
- 2.Bories E, Pesenti C, Caillol F, et al. Transgastric endoscopic ultrasonographyguided biliary drainage: Results of a pilot study. Endoscopy. 2007;39:287–91. doi: 10.1055/s-2007-966212. [DOI] [PubMed] [Google Scholar]
- 3.Poincloux L, Rouquette O, Buc E, et al. Endoscopic ultrasoundguided biliary drainage after failed ERCP: Cumulative experience of 101 procedures at a single center. Endoscopy. 2015;47:794–801. doi: 10.1055/s-0034-1391988. [DOI] [PubMed] [Google Scholar]
- 4.Ratone JP, Caillol F, Bories E, et al. Hepatogastrostomy by EUS for malignant afferent loop obstruction after duodenopancreatectomy. Endosc Ultrasound. 2015;4:250–2. doi: 10.4103/2303-9027.163017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah RJ, Smolkin M, Yen R, et al. A multicenter, U.S. experience of singleballoon, doubleballoon, and rotational overtubeassisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video) Gastrointest Endosc. 2013;77:593–600. doi: 10.1016/j.gie.2012.10.015. [DOI] [PubMed] [Google Scholar]
- 6.Kedia P, Tyberg A, Kumta NA, et al. EUSdirected transgastric ERCP for rouxenY gastric bypass anatomy: A minimally invasive approach. Gastrointest Endosc. 2015;82:560–5. doi: 10.1016/j.gie.2015.03.1913. [DOI] [PubMed] [Google Scholar]
- 7.Ngamruengphong S, Nieto J, Kunda R, et al. Endoscopic ultrasoundguided creation of a transgastric fistula for the management of hepatobiliary disease in patients with RouxenY gastric bypass. Endoscopy. 2017;49:549–52. doi: 10.1055/s-0043-105072. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


