Abstract
Introduction
The annual cost of treatment and lost productivity due to chronic pain is estimated to be $635 billion within the USA. Self-management treatments for chronic pain result in lower health care costs and lower utilization of provider-management treatments, such as hospitalization and medication use. The current study sought to identify and characterize patient factors and health conditions associated with chronic pain treatment utilization to inform ways to improve engagement in self-management pain treatment (e.g., applying heat or ice, exercising, or practicing relaxation). This study predicted (1) greater pain intensity and pain interference would be associated with greater utilization of self-management treatments and (2) this association would be moderated by patient factors (gender and age) and health comorbidities (anxiety, trauma, depression, and sleep disturbance).
Materials and Methods
Baseline data from a three-arm clinical trial were collected for 127 Veterans seeking treatment for chronic pain. Veterans were recruited via clinician referral and medical record review at the Veterans Affairs Puget Sound Health Care System, Washington, USA.
Results
Self-management treatments were more utilized than provider-management treatments. Pain intensity and pain interference were not uniquely associated with provider-management or self-management treatment utilization after controlling for demographics and mental health status. Sleep disturbance moderated the relationship between pain interference and provider-management treatment utilization. Depression moderated the relationship between pain intensity and provider-management treatment utilization.
Conclusions
While study conclusions may not generalize to all Veteran populations, findings suggest that Veterans with chronic pain were more likely to seek provider-management treatments when experiencing high-pain interference and high-sleep disturbance. In addition, Veterans were more likely to seek provider-management treatments when experiencing low-pain intensity and high-depression symptoms.
Keywords: Veterans, pain, sleep, depression, functional interference, self-management
INTRODUCTION
Chronic pain affects 47–78% of Veterans presenting to Veterans Health Administration (VHA) clinics.1–4 The annual cost of treatment and lost productivity due to chronic pain is estimated to be $635 billion within the USA, which exceeds any other health condition.5 Within the VHA, Veterans with chronic pain utilize greater outpatient3 and inpatient6 services than Veterans without chronic pain, leading to greater health care costs.
Pain management treatments may be divided into two approaches; those that are administered and managed by a provider and those initiated and managed by the patient.7,8 Provider-management (PM) approaches include more traditional medical treatments such as medications, surgeries, and injections, as well as treatments and services such as massage and psychotherapy. In contrast, self-management (SM) approaches refer to strategies an individual can use on their own to actively cope with or reduce pain and improve functioning, such as using heat or ice, exercising, or practicing relaxation. SM cultivates a patient’s ability to independently manage their symptoms and make subsequent lifestyle changes due to these symptoms,9 emphasizing the patient’s self-efficacy in managing their own health.10 SM treatments for chronic pain have been shown to result in lower health care costs and lower utilization of PM treatments, such as hospitalization11 and medication use.12 SM interventions often involve behavioral components (e.g., heat and ice application, exercise), which are recommended as low-cost, effective options for pain management that, unlike many medications, can be used safely and routinely used over many years.13 Given the potential for high cost, provider burden, lack of sustained improvement, and associated risk of some PM treatments, SM approaches represent alternative or complementary approaches that have demonstrated long-term efficacy.14
Greater pain intensity and greater pain interference are established predictors of treatment seeking from physicians, psychologists, massage therapists, and chiropractors.15 However, their capacity to predict SM treatment utilization is less clear.16 A diverse range of health conditions are frequently comorbid with chronic pain, such as anxiety disorders,17,18 post-traumatic stress disorder (PTSD),19 depression,19,20 and sleep disturbance.21,22 These conditions may also moderate the relationships between pain intensity, pain interference, and pain treatment utilization.23 Demographic and other patient factors also may be associated with PM and SM treatments in the context of chronic pain. For example, while females report a higher incidence of chronic pain than males, treatment seeking among females with chronic pain has been shown to vary as a function of age, with females over 65 years old utilizing fewer pain treatments compared to females less than 65 years of age.2 To date, few studies have examined patient factors associated with treatment utilization among Veterans with chronic pain and whether these characteristics interact with other critical treatment-related factors such as pain intensity and pain interference.
This study aimed to identify and characterize patient factors and health conditions associated with PM and SM treatment utilizations, to inform ways to increase the utilization of SM approaches towards pain management. It was predicted that greater pain intensity and pain interference would be associated with greater PM and SM treatment utilizations as moderated by patient factors (gender and age) and health comorbidities (anxiety, PTSD, depression, and sleep disturbance). We predicted that positive associations between pain-related factors and treatment utilization would be the strongest for Veterans who were female, younger, and endorsed greater symptoms of comorbid health symptoms.
METHODS
Participants and Procedure
Participants were 127 Veterans receiving care at one of two VA Medical Centers in the Pacific Northwest, recruited primarily via clinician referral and focused medical record review. Approximately, 1,288 Veterans were invited by study recruiters to participate, 245 Veterans were screened for eligibility, and 127 were deemed eligible and agreed to participate. Data presented here are extracted from the baseline data of a larger randomized controlled trial who were consecutively recruited and enrolled from October 9, 2015 until January 31, 2017 comparing three behavioral SM interventions (pain education, self-hypnosis training, or mindfulness meditation) for Veterans with chronic pain. Chronic pain was operationalized below to allow sufficient pain severity and persistence to detect treatment-related improvements in the clinical trial. Study inclusion criteria were: Veteran status, age 18 years or older, English proficiency, and presence of self-reported moderate or greater chronic pain, which was operationalized as having pain for at least 3 months with an average intensity of 3 or greater (0–10 scale) over the past week, a worst pain intensity of 5 or greater (0–10 scale) over the past week, and pain experienced at least 75% of the time in the past 3 months. Chronic pain was operationalized in this way to ensure that trial participants’ pain was of sufficient level to warrant intensive SM treatment and allow for measurable improvement in pain intensity.
Exclusion criteria included cognitive impairment measured via a six-item cognitive screener psychometrically derived from the Mini Mental State Exam,24 current or historical (past 5 years) experience of any psychosis or thought disorder, hospitalization (past 5 years) for psychiatric conditions other than suicidality, homicidality, or planned treatment of PTSD, severe or unstable mental health functioning within past 6 months, daily use of greater than 120 mg morphine equivalent dosage medication (cutoff determined by the VA Puget Sound Opioid Safety Review Board), indications of behavioral problems that would be inappropriate in a therapeutic group setting, active suicidal or homicidal ideation or related behaviors presented at time of screening that may interfere with participation, difficulties with telephone communication, and planned life events that may interfere with group participation. All procedures were approved by the University of Washington and VA Puget Sound Health Care System Institutional Review Boards.
Measures
PM and SM Treatment Utilizations
Pain treatment utilization was measured with a self-report checklist in which participants indicated whether (yes/no) they had used 15 different treatments for pain, excluding medications, over the past 3 months. The self-report checklist was developed by a panel of pain treatment experts at the University of Washington for use in the present study and was divided into a seven-item PM subscale and an eight-item SM subscale based on expert consensus (specific items listed in Table I). Items were summed within each subscale for a possible total of seven in the PM category and eight in the SM category. A higher score indicated a greater number of pain treatment strategies utilized from that category in the past 3 months.
TABLE I.
Participant Characteristics
| # (%) | # (%) | ||
|---|---|---|---|
| Gender (n = 127) | PM treatments | ||
| Male | 94 (74.0) | Massage | 45 (35.43) |
| Female | 32 (25.20) | Osteopathic manipulation | 11 (8.66) |
| Transgender | 1 (0.8) | Trigger point injections | 9 (7.09) |
| Race (n = 126) | Spine, joint, or facet injections | 20 (15.87) | |
| African American/Black | 24 (18.9) | Spinal cord stimulation | 5 (3.94) |
| Caucasian/White | 81 (63.8) | Counseling/Talk therapy | 36 (28.35) |
| Asian | 3 (2.4) | Surgery | 7 (5.51) |
| American Indian/Alaska Native | 3 (2.4) | SM treatments | |
| Pacific Islander/Native Hawaiian | 1 (0.8) | Water Therapy/Swimming | 24 (18.90) |
| Multiracial | 9 (7.1) | Another type of exercise | 85 (66.93) |
| Other | 5 (3.9) | Heart or cold to pain location | 98 (77.17) |
| Ethnicity (Hispanic or Latino; n = 122) | 10 (7.9) | TENS | 41 (32.28) |
| Education (n = 127) | Ultrasound | 6 (4.72) | |
| Ninth grade or less | 0 (0.0) | Wearing a brace or corset | 54 (42.52) |
| Grades 10–11 | 0 (0.0) | Pain education/Self-help books | 53 (41.73) |
| High school or general education degree | 9 (7.1) | Relaxation practice | 68 (53.54) |
| Vocational/Technical school | 7 (5.5) | ||
| Some college | 54 (42.5) | ||
| College graduate | 43 (33.9) | ||
| Graduate/Professional school | 14 (11.0) | ||
| Employment status (n = 127) | |||
| Full-time | 28 (22.0) | ||
| Employed part-time | 5 (3.9) | ||
| Attending school/Vocational training full-time | 5 (3.9) | ||
| Attending school/Vocational training part-time | 1 (0.8) | ||
| Retired | 50 (39.4) | ||
| Homemaker | 6 (4.7) | ||
| Unemployed due to pain | 23 (18.1) | ||
| Unemployed due to disability | 47 (37.0) | ||
| Unemployed due to other reasons | 6 (4.7) | ||
| Marital status (n = 127) | |||
| Married | 66 (52.0) | ||
| Separated | 7 (5.5) | ||
| Divorced | 31 (24.4) | ||
| Living with significant other | 9 (7.1) | ||
| Never married | 9 (7.1) | ||
| Widowed | 4 (3.1) | ||
| Military branch (n = 127) | |||
| Air Force | 15 (11.8) | ||
| Army | 71 (55.9) | ||
| Coast Guard | 3 (2.4) | ||
| Marine Corps | 13 (10.2) | ||
| Navy | 30 (23.6) | ||
| Other | 5 (3.9) | ||
Note. Relaxation practice was presented as “Relaxation practice such as deep breathing, self-hypnosis, or listening to audio recordings”; TENS = transcutaneous electrical nerve stimulation.
Pain Intensity
Average pain intensity in the past week was assessed with the Numerical Rating Scale (NRS), which asks respondents to rate their average pain in the past 24 hours, where 0 is “no pain” and 10 is “pain as bad as you can imagine.” The NRS was administered four times within 1 week; each of the four assessment periods was separated by at least 24 hours. The average of the four assessment ratings comprised the average pain intensity in the past week. A composite measure of average pain intensity is more reliable than single rating measures,25 and the NRS specifically demonstrated strong validity26 as a measure of pain intensity and strong reliability with similar pain intensity measures.27
Pain Interference
Pain interference over the past week was measured with the six-item Patient-Reported Outcomes Measurement Information System (PROMIS) Pain Interference Short-Form self-report questionnaire.28 Participants rated the extent to which pain interfered with various functional domains from 1 (not at all) to 5 (very much). A higher score indicated greater pain interference.
Sleep Disturbance
Sleep disturbance over the past week was measured with the eight-item PROMIS Sleep Disturbance self-report questionnaire.28 Participants rated overall “sleep quality” from 5 (very poor) to 1 (very good) and then rated their level of agreement (from 5 (not at all) to 1 (very much)) with statements about their sleep. A higher score indicated greater sleep disturbance. The scale was not designed to diagnose specific sleep disorders or assess sleep quantity or efficiency.
Anxiety Symptoms
Anxiety symptoms over the past week were measured with the eight-item PROMIS Emotional Distress-Anxiety self-report questionnaire.28 Participants rated to what extent they experienced each symptom from 1 (never) to 5 (always). A higher score indicated greater anxiety.
Depression Symptoms
Depression symptoms over the past week were measured with the eight-item PROMIS Emotional Distress-Depression self-report questionnaire.28 Participants rated to what extent they experienced each symptom from 1 (never) to 5 (always). A higher score indicated greater depression symptoms.
PTSD Symptoms
PTSD symptoms over the past month were measured with the 20-item PTSD Checklist for the Diagnostic and Statistical Manual for Mental Disorders, Fifth Edition (PCL-5).29,30 Participants rated to what extent they experienced each symptom from 0 (not at all) to 4 (extremely). A higher score indicated greater PTSD symptoms.29,30
Data Analytic Plan
Missing data analyses in SPSS indicated 0.54% of the data were missing completely at random (MCAR) based on Little’s MCAR test (χ2[3,740] = 3,689.63, p = 0.718). Main effects were calculated in SPSS linear regression with age, gender, pain intensity, pain interference, and all health comorbidities in Table II entered as covariates. Moderation analyses also were conducted in SPSS with bias-corrected bootstrap resampling with 10,000 resamples through Model 1 of the PROCESS macro.31 Pain intensity and pain interference were entered into distinct models for PM and SM treatment utilizations. All hypothesized health moderators were entered into each model, which isolated the distinct effects of each moderator while controlling for the remaining health comorbidities.
TABLE II.
Variable Correlations
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | M(SD) | Study Range | Possible Range | α | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 52.60 (12.07) | 24–79 | |||||||||||
| 2. Intensity | 0.06 | 6.01 (1.66) | 1.50–9.31 | 0–10 | 0.93 | ||||||||
| 3. Interference | 0.05 | 0.38 | 21.21 (5.06) | 8–30 | 6–30 | 0.89 | |||||||
| 4. Anxiety | −0.18 | 0.19 | 0.49 | 19.39 (7.59) | 8–38 | 8–40 | 0.94 | ||||||
| 5. Depression | −0.14 | 0.25 | 0.53 | 0.77 | 16.70 (7.27) | 8–39 | 8–40 | 0.93 | |||||
| 6. PTSD | −0.24 | 0.17 | 0.46 | 0.78 | 0.80 | 33.31 (17.33) | 0–74 | 0–80 | 0.94 | ||||
| 7. Sleep | −0.13 | 0.37 | 0.41 | 0.41 | 0.41 | 0.49 | 28.66 (7.49) | 8–40 | 8–40 | 0.76 | |||
| 8. PM | −0.11 | 0.17 | 0.13 | 0.17 | 0.12 | 0.10 | 0.22 | 1.05 (1.21) | 0–6 | 0–7 | 0.52 | ||
| 9. SM | −0.15 | 0.15 | 0.15 | 0.19 | 0.22 | 0.22 | 0.18 | 0.35 | 3.38 (1.68) | 0–7 | 0–8 | 0.52 | |
Note.Underline = p < 0.05, Underline bold = p < 0.01. Intensity, pain intensity; Interference, pain interference; PM, provider-management treatment utilization; SM, self-management treatment utilization.
RESULTS
Participant characteristics and treatment utilization frequencies are presented in Table I. Variable correlations are presented in Table II. Higher levels of sleep disturbance were associated with greater use of PM treatments at the univariate level, while higher levels of anxiety, depression, PTSD, and sleep disturbance were associated with greater use of SM treatments at the univariate level. SM treatment utilization was greater than PM treatment utilization (Mdif[SD] = 2.32[1.70], t[124] = 15.24, CI95 = 2.02,2.62, p < 0.001), which may reflect greater Veteran willingness to use SM versus PM techniques. Massage was the most frequently endorsed PM treatment (45/127 Veterans), while applying heat or cold on location of pain was the most frequently endorsed SM treatment (98/127 Veterans).
Statistics are reported in Tables III and IV. Findings indicated that pain intensity and pain interference were not significantly associated with PM or SM treatment utilization after controlling for the effects of age, gender, anxiety, depression, PTSD, and sleep disturbance symptoms. Only depression symptoms and sleep disturbance demonstrated significant relationships with PM treatment utilization as supported by significant p-values, significant conditional effects, and confidence intervals.
TABLE III.
Moderation Results for PM Treatment Utilization
| B | SE | t | p(CI95) | Model R2 | |
|---|---|---|---|---|---|
| Main effects | 0.078 | ||||
| Constant | 0.43 | 0.85 | 0.51 | 0.611 (−1.25/2.12) | |
| Age | −0.01 | 0.01 | −1.06 | 0.290 (−0.03/0.01) | |
| Gender | −0.25 | 0.26 | −0.97 | 0.336 (−0.76/0.26) | |
| Pain intensity | 0.07 | 0.08 | 0.88 | 0.379 (−0.08/0.22) | |
| Pain interference | 0.00 | 0.03 | −1.12 | 0.907 (−0.06/0.05) | |
| Anxiety | 0.02 | 0.03 | 0.93 | 0.356 (−0.03/0.08) | |
| Depression | 0.01 | 0.03 | 0.36 | 0.722 (−0.05/0.07) | |
| PTSD | −0.02 | 0.01 | −1.18 | 0.240 (−0.04/0.01) | |
| Sleep | 0.04 | 0.02 | 1.93 | 0.056 (0.00/0.07) | |
| Interaction effects | ∆R2 | ||||
| Pain intensity × age | −0.01 | 0.01 | −1.18 | 0.242 (−0.02/0.00) | 0.012 |
| Pain intensity × gender | 0.18 | 0.16 | 1.13 | 0.260 (−0.13/0.49) | 0.011 |
| Pain intensity × anxiety | −0.02 | 0.01 | −1.62 | 0.108 (−0.03/0.00) | 0.022 |
| Pain intensity × depression | −0.02 | 0.01 | −2.31 | 0.023 (−0.04/0.00) | 0.044 |
| Pain intensity × PTSD | 0.00 | 0.00 | −0.35 | 0.725 (−0.01/0.01) | 0.001 |
| Pain intensity × sleep | 0.01 | 0.01 | 1.44 | 0.153 (0.00/0.03) | 0.018 |
| Pain interference × age | 0.00 | 0.00 | −1.31 | 0.193 (−0.01/0.00) | 0.015 |
| Pain interference × gender | 0.06 | 0.05 | 1.21 | 0.228 (−0.04/0.15) | 0.013 |
| Pain interference × anxiety | 0.00 | 0.00 | 1.08 | 0.281 (0.00/0.01) | 0.010 |
| Pain interference × depression | 0.00 | 0.00 | 1.21 | 0.229 (0.00/0.01) | 0.012 |
| Pain interference × PTSD | 0.00 | 0.00 | 1.73 | 0.087 (0.00/0.01) | 0.025 |
| Pain interference × sleep | 0.01 | 0.00 | 2.03 | 0.044 (0.00/0.01) | 0.034 |
Note. Bold values indicate statistically significant effects. R2 indicates the effect magnitude of the collective model with all covariates included. ∆R2 indicates the magnitude of the interaction effect. All values are rounded, and no significant effects included 0 in the confidence interval (the −0.04/0.00 confidence interval represents −0.0449/−0.0035 without rounding and the 0.00/0.01 confidence interval represents 0.0002/0.0135 without rounding).
TABLE IV.
Moderation Results for SM Treatment Utilization
| B | SE | t | p(CI95) | Model R2 | |
|---|---|---|---|---|---|
| Main effects | 0.091 | ||||
| Constant | 3.60 | 1.19 | 3.04 | 0.003 (1.25/5.95) | |
| Age | −0.02 | 0.01 | −1.51 | 0.133 (−0.05/0.01) | |
| Gender | −0.53 | 0.36 | −1.48 | 0.143 (−1.24/0.18) | |
| Pain intensity | 0.09 | 0.11 | 0.88 | 0.383 (−0.12/0.30) | |
| Pain interference | 0.01 | 0.04 | 0.20 | 0.841 (−0.07/0.09) | |
| Anxiety | −0.01 | 0.04 | −0.36 | 0.719 (−0.09/0.06) | |
| Depression | 0.03 | 0.04 | 0.66 | 0.512 (−0.05/0.11) | |
| PTSD | 0.01 | 0.02 | 0.40 | 0.690 (−0.03/0.04) | |
| Sleep | 0.01 | 0.03 | 0.49 | 0.623 (−0.04/0.06) | |
| Interaction effects | ∆R2 | ||||
| Pain intensity × age | 0.00 | 0.01 | 0.23 | 0.819 (−0.01/0.02) | 0.000 |
| Pain intensity × gender | −0.01 | 0.22 | −0.06 | 0.953 (−0.45/0.43) | 0.000 |
| Pain intensity × anxiety | −0.01 | 0.01 | −0.64 | 0.524 (−0.03/0.02) | 0.004 |
| Pain intensity × depression | −0.01 | 0.02 | −0.95 | 0.342 (−0.04/0.02) | 0.008 |
| Pain intensity × PTSD | 0.00 | 0.01 | 0.06 | 0.956 (−0.01/0.01) | 0.000 |
| Pain intensity × sleep | 0.02 | 0.01 | 1.79 | 0.076 (0.00/0.05) | 0.026 |
| Pain interference × age | 0.00 | 0.00 | 0.24 | 0.810 (0.00/0.01) | 0.001 |
| Pain interference × gender | −0.03 | 0.07 | −0.47 | 0.639 (−0.17/0.10) | 0.002 |
| Pain interference × anxiety | 0.00 | 0.00 | 0.72 | 0.474 (−0.01/0.01) | 0.000 |
| Pain interference × depression | 0.00 | 0.01 | 0.09 | 0.926 (−0.01/0.01) | 0.000 |
| Pain interference × PTSD | 0.00 | 0.00 | 0.77 | 0.440 (0.00/0.01) | 0.001 |
| Pain interference × sleep | 0.01 | 0.00 | 1.88 | 0.063 (0.00/0.02) | 0.029 |
Note. R2 indicates the effect magnitude of the collective model with all covariates included. ∆R2 indicates the magnitude of the interaction effect.
Pain Intensity
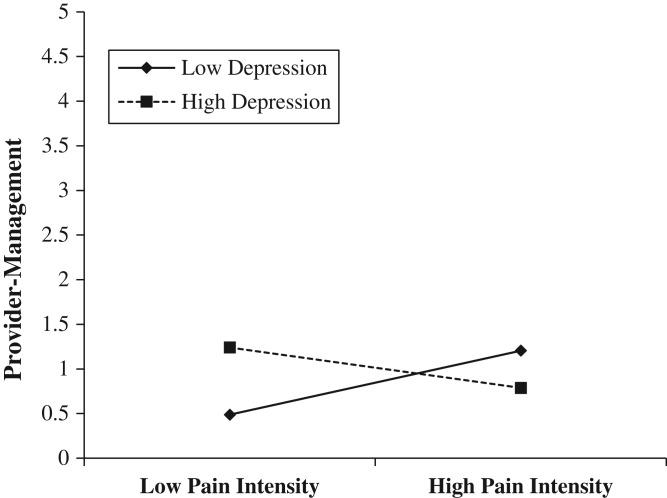
Veterans with high-pain intensity reported comparable PM treatment utilization regardless of depression symptom severity, but Veterans with low-pain intensity and high-depression symptoms reported significantly greater PM treatment utilization compared with Veterans with low-pain intensity and low-depression symptoms (Fig. 1).
FIGURE 1.
Depression moderates the relationship between pain intensity and PM treatment utilization.
Pain Interference
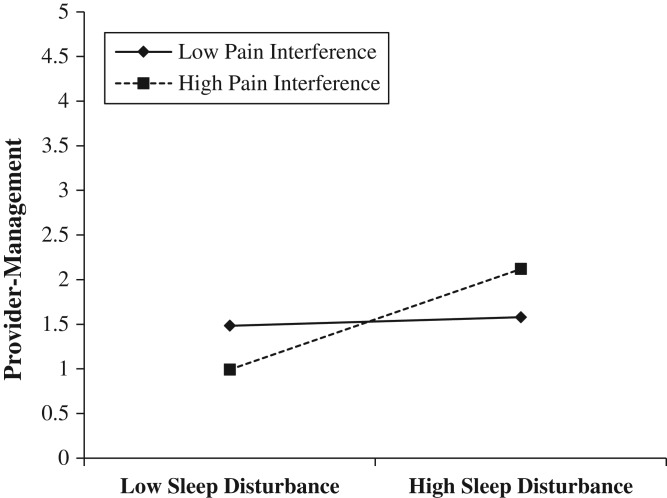
Veterans with low-pain interference reported comparable PM treatment utilization regardless of their level of sleep disturbance, but Veterans with high-pain interference and high-sleep disturbance reported significantly greater PM treatment utilization compared with Veterans with high-pain interference and low-sleep disturbance (Fig. 2).
FIGURE 2.
Pain interference moderates the relationship between sleep disturbance and PM treatment utilization.
Interaction Effects
The Johnson–Neyman technique32 was conducted to determine the conditional effects of the pain intensity × depression and pain interference × sleep disturbance. This technique examines the full variance of the moderation effect and determines regions of significance for conditional effects. For the moderation of pain intensity and PM treatment utilization, less pain intensity was significantly associated with greater PM treatment utilization when depression symptoms were reported as less than 11.10 (depression M[SD] = 16.70[7.27]). For the moderation of pain interference and PM, greater sleep disturbance was significantly associated with greater PM when pain interference was reported as greater than 21.26 (pain interference M[SD] = 21.21[5.06]).
DISCUSSION
High comorbidity between chronic pain and mental health is associated with substantial costs to the VA health care system.3,6 Given the potential costs of PM treatment utilization compared with SM treatment utilization,11,12,14 identifying modifiable factors associated with PM and SM treatment utilization has important clinical implications to inform ways to motivate greater SM treatment utilization. Results indicated significant relationships between pain intensity, pain interference, sleep disturbance, and psychological symptoms. Within this complex presentation, depression symptoms and sleep disturbance specifically emerged as significant moderators of the associations between pain intensity, pain interference, and PM treatment utilization. Veterans with chronic pain were more likely to seek PM treatments when experiencing (a) high-pain interference and high-sleep disturbance as well as (b) low-pain intensity and high-depression symptoms.
Consistent with prior research,17–21 findings identified strong associations between chronic pain and psychological comorbidities. Positive correlations were found between pain intensity, anxiety, depression, and sleep disturbance. Positive correlations also were found between pain interference and anxiety, depression, PTSD symptoms, and sleep disturbance. These overlapping conditions confer particular vulnerability, as each condition worsens pain outcomes, functioning, and interferes with treatment. Research has identified anxiety as a barrier to treatment utilization,33,34 and worse pain outcomes have been reported when underlying depression symptoms go undiagnosed and untreated.35 Conversely, treatment of comorbid sleep problems improves pain outcomes,36 and treatments targeting improved mood may concurrently improve pain and sleep.37,38 Thus, mental health treatments have the potential to instigate meaningful improvements in pain management.
Research has identified that higher pain intensity predicts increased PM treatment utilization.15 When additionally considering depression severity, results showed that in the context of high-depression symptoms, Veterans with low-pain intensity were also significantly more likely to have used PM treatments in the preceding 3 months; recent utilization of PM treatment for those with high-pain intensity did not vary as a function of depression symptoms. Thus, findings indicate in the context of significant depression symptoms, even low-pain intensity is likely to be associated with seeking PM treatments.
Additionally, pain interference interacted with sleep disturbance, with Veterans reporting both high-pain interference and high-sleep disturbance more likely to report higher levels of utilization of PM treatments in the past 3 months. PM treatment utilization for Veterans with low-pain interference was not associated with the degree of sleep disturbance. While not possible to disentangle from the present correlational data, future studies should examine whether Veterans might more readily pursue PM treatments to help reduce sleep disturbance, which may lead to greater utilization of PM pain treatments.
The interactions of sleep disturbance with pain intensity and pain interference associated with SM treatment utilization trended toward significance, but interpretations were not elaborated due to the lack of statistical significance. We suspect that a larger sample size may have detected a statistically and clinically significant impact of sleep disturbance as a comorbidity in the relationships between pain intensity, pain interference, and SM treatment utilization. Given the significant interactions of depression and sleep disturbance associated with PM treatment utilization, changes in depression and sleep appear to impact PM utilization more than SM utilization. Overall, chronic pain × comorbidity interaction effects contributed more to R2 changes for the PM treatment utilization model compared with the SM treatment utilization model.
Limitations
This study was limited by the cross-sectional nature of the data, which precluded the examination of longitudinal predictors of treatment utilization over time and understanding of potential directions of influence. Additionally, data collected to assess treatment utilization over the past 3 months were collected with an unvalidated measure, which may have been biased by retrospective recall. Although the measure included a variety of commonly used treatment and SM strategies, it did not include an exhaustive list of available strategies or assess degree of treatment compliance for each strategy. Treatment utilization in this study captured heterogeneous categories and did not include the quantity of treatment utilization, only the presence or absence. Finally, this study sampled Veterans already scheduled to begin SM treatments (recruitment described above), so results are likely biased toward Veterans already open to SM treatment options and may not generalize to all Veterans with chronic pain.
CONCLUSIONS
Findings broaden existing literature to Veterans seeking pain SM interventions in several ways, with recognition that study conclusions may not generalize to all Veteran populations. First, findings provide patient demographic and health characteristics on an ongoing investigation on the efficacy of SM group interventions. Second, our single time-point moderation results inform clinical care by suggesting that depression symptoms and sleep disturbance may interact with pain intensity and functional interference to influence Veteran willingness to engage in certain types of pain management strategies. Strategies that improve depressed mood and sleep quality may be particularly pertinent to further develop for this population, and clinicians may be alerted to monitor mood and sleep changes. Also notable was the finding that a few SM strategies were used by most participants (i.e., heat or cold on location of pain, relaxation practice, and another type of exercise), suggesting openness to such treatments, at least among patients willing to participate in a behavioral clinical trial. This study emphasizes the importance of evaluating and treating mood and sleep in individuals as important aspects of chronic pain management. It also suggests some conceptual support for the burden of adversity hypothesis; that increased treatment utilization is associated with higher levels of comorbid symptoms.
Funding
Hypnosis and Meditation for Pain Management in Veterans: Efficacy and Mechanisms. (Jensen & Williams). NIH; National Center for Complementary and Integrative Health. Grant #: 1R01AT008336-01.
Previous presentation
A version of these analyses was presented as a poster presentation at the Association for Cognitive and Behavioral Therapies in November of 2017 in San Diego, CA, USA.
References
- 1. Gironda RJ, Clark ME, Massengale JP, Walker RL: Pain among veterans of operations enduring freedom and Iraqi freedom. Pain Med 2006; 7(4): 339–43. [DOI] [PubMed] [Google Scholar]
- 2. Haskell SG, Heapy A, Reid MC, Papas RK, Kerns RD: The prevalence and age-related characteristics of pain in a sample of women veterans receiving primary care. J Women’s Health 2006; 15(7): 862–9. [DOI] [PubMed] [Google Scholar]
- 3. Kerns RD, Otis J, Rosenberg R, Reid MC: Veterans’ reports of pain and associations with ratings of health, health-risk behaviors, affective distress, and use of the healthcare system. J Rehabil Res Dev 2003; 40(5): 371–80. [DOI] [PubMed] [Google Scholar]
- 4. Lew HL, Otis JD, Tun C, et al. : Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OIF/OEF veterans: polytrauma clinical triad. J Rehabil Res Dev 2009; 46(6): 697–702. [DOI] [PubMed] [Google Scholar]
- 5. Gaskin DJ, Richard P: The economic costs of pain in the United States. J Pain 2012; 13(8): 715–24. [DOI] [PubMed] [Google Scholar]
- 6. Caldeiro RM, Malte CA, Calsyn DA, et al. : The association of persistent pain with out‐patient addiction treatment outcomes and service utilization. Addiction 2008; 103(12): 1996–2005. [DOI] [PubMed] [Google Scholar]
- 7. Chou R, Qaseem A, Snow V, et al. : Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007; 147(7): 478–91. [DOI] [PubMed] [Google Scholar]
- 8. Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH: Collaborative management of chronic illness. Ann Intern Med 1997; 127(12): 1097–102. [DOI] [PubMed] [Google Scholar]
- 9. Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J: Self-management approaches for people with chronic conditions: a review. Patient Educ Couns 2002; 48(2): 177–87. [DOI] [PubMed] [Google Scholar]
- 10. Dorflinger L, Kerns RD, Auerbach SM: Providers’ roles in enhancing patients’ adherence to pain self management. Transl Behav Med 2012; 3(1): 39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lorig KR, Sobel DS, Stewart AL, et al. : Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care 1999; 1: 5–14. [DOI] [PubMed] [Google Scholar]
- 12. Gottlieb H, Alperson BL, Schwartz AH, Beck C, Kee S: Self-management for medication reduction in chronic low back pain. Arch Phys Med Rehabil 1988; 69(6): 442–8. [PubMed] [Google Scholar]
- 13. Department of Defense, Department of Veterans Affairs : VA/DoD clinical practice guideline for opioid therapy for chronic pain. 2017; Available at https://www.healthquality.va.gov/guidelines/Pain/cot/VADoDOTCPGPatientSummary022717.pdf; accessed August 8, 2018.
- 14. Goeppinger J, Armstrong B, Schwartz T, Ensley D, Brady TJ: Self‐management education for persons with arthritis: managing comorbidity and eliminating health disparities. Arthritis Care Res 2007; 57(6): 1081–8. [DOI] [PubMed] [Google Scholar]
- 15. Côté P, Cassidy JD, Carroll L: The treatment of neck and low back pain: who seeks care? Who goes where? Med Care 2001; 1: 956–67. [DOI] [PubMed] [Google Scholar]
- 16. Kerns RD, Rosenberg R: Predicting responses to self-management treatments for chronic pain: application of the pain stages of change model. Pain 2000; 84(1): 49–55. [DOI] [PubMed] [Google Scholar]
- 17. Asmundson GJ, Katz J: Understanding the co‐occurrence of anxiety disorders and chronic pain: state‐of‐the‐art. Depress Anxiety 2009; 26(10): 888–901. [DOI] [PubMed] [Google Scholar]
- 18. Kuch K, Cox BJ, Woszczyna CB, Swinson RP, Shulman I: Chronic pain in panic disorder. J Behav Ther Exp Psychiatry 1991; 22(4): 255–9. [DOI] [PubMed] [Google Scholar]
- 19. Morasco BJ, Lovejoy TI, Lu M, et al. : The relationship between PTSD and chronic pain: mediating role of coping strategies and depression. Pain 2013; 154(4): 609–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Arola HM, Nicholls E, Mallen C, Thomas E: Self‐reported pain interference and symptoms of anxiety and depression in community‐dwelling older adults: Can a temporal relationship be determined? Eur J Pain 2010; 14(9): 966–71. [DOI] [PubMed] [Google Scholar]
- 21. Menefee LA, Cohen MJ, Anderson WR, et al. : Sleep disturbance and nonmalignant chronic pain: a comprehensive review of the literature. Pain Med 2000; 1(2): 156–72. [DOI] [PubMed] [Google Scholar]
- 22. Morin CM, Gibson D, Wade J: Self-reported sleep and mood disturbance in chronic pain patients. Clin J Pain 1998; 14(4): 311–4. [DOI] [PubMed] [Google Scholar]
- 23. Helmer DA, Chandler HK, Quigley KS, et al. : Chronic widespread pain, mental health, and physical role function in OEF/OIF veterans. Pain Med 2009; 10(7): 1174–82. [DOI] [PubMed] [Google Scholar]
- 24. Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC: Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care 2002; 1: 771–81. [DOI] [PubMed] [Google Scholar]
- 25. Jensen MP, Turner JA, Romano JM: What is the maximum number of levels needed in pain intensity measurement? Pain 1994; 58(3): 387–92. [DOI] [PubMed] [Google Scholar]
- 26. Jensen MP: Measurement of pain In: Bonica’s Management of Pain, Ed 4, pp 251–70. Edited by Fishman SM, Ballantyne JC, Rathmell JP. Media, PA, Williams & Wilkins, 2010. [Google Scholar]
- 27. Dworkin RH, Turk DC, Farrar JT, et al. : Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005; 113(1): 9–19. [DOI] [PubMed] [Google Scholar]
- 28. Cella D, Riley W, Stone A, et al. : The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol 2010; 63(11): 1179–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Weathers FW, Litz BT, Keane TM, et al. : The PTSD checklist for DSM-5 (PCL-5). 2013; Available at www.ptsd.va.gov; accessed August 8, 2018.
- 30. Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL: The posttraumatic stress disorder checklist for DSM‐5 (PCL‐5): Development and initial psychometric evaluation. J Trauma Stress 2015; 28(6): 489–98. [DOI] [PubMed] [Google Scholar]
- 31. Hayes AF: Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY, Guilford Press, 2013. [Google Scholar]
- 32. Hayes AF, Matthes J: Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behav Res Methods 2009; 41: 924–36. [DOI] [PubMed] [Google Scholar]
- 33. Gordon SM, Dionne RA, Snyder J: Dental fear and anxiety as a barrier to accessing oral health care among patients with special health care needs. Spec Care Dentist 1998; 18(2): 88–92. [DOI] [PubMed] [Google Scholar]
- 34. Kushner MG, Sher KJ: The relation of treatment fearfulness and psychological service utilization: an overview. Prof Psychol Res Pr 1991; 22(3): 196. [Google Scholar]
- 35. Shmuely Y, Baumgarten M, Rovner B, Berlin J: Predictors of improvement in health-related quality of life among elderly patients with depression. Int Psychogeriatr 2001; 13(1): 63–73. [DOI] [PubMed] [Google Scholar]
- 36. Khalid I, Roehrs TA, Hudgel DW, Roth T: Continuous positive airway pressure in severe obstructive sleep apnea reduces pain sensitivity. Sleep 2011; 34(12): 1687–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. O’brien EM, Waxenberg LB, Atchison JW: Negative mood mediates the effect of poor sleep on pain among chronic pain patients. Clin J Pain 2010; 26(4): 310–9. [DOI] [PubMed] [Google Scholar]
- 38. Schrimpf M, Liegl G, Boeckle M, et al. : The effect of sleep deprivation on pain perception in healthy subjects: a meta-analysis. Sleep Med 2015; 16(11): 1313–20. [DOI] [PubMed] [Google Scholar]