Abstract
Aims/Introduction
The prevalence and risk of vaginal candidiasis before and after initiating sodium–glucose cotransporter 2 (SGLT2) inhibitors, although some clinical trials have been carried out, have not been adequately shown in real‐world practice. We investigated the incidence of vaginal Candida colonization and symptomatic vaginitis, and the clinical risk factors including diabetic microvascular complications.
Materials and Methods
The participants were 114 women with type 2 diabetes who were free of vaginitis symptoms and started SGLT2 inhibitors. Vaginal candidiasis tests through self‐administered swabs were carried out at baseline, 6 and 12 months.
Results
Before starting SGLT2 inhibitors, 17 participants (14.9%) had positive vaginal Candida colonization. Younger age and the presence of microangiopathy were significantly associated with the positive colonization in multivariate analysis. Among all participants, 23 (20.2%, 8 because of vaginitis and 15 for other reasons) discontinued SGLT2 inhibitors before reaching the 6‐month test. Of 65 participants who were negative for Candida at baseline and received the 6‐month test, 24 (36.9%) converted to a positive culture, and multivariate analysis showed older age as an independent risk for developing Candida colonization. There were 18 participants (15.8%) who developed symptomatic vaginitis, and they showed similar characteristics to the 24 participants. Most of those with negative cultures at 6 months showed negative results at 12 months and vice versa.
Conclusions
The rates of developing positive colonization and symptomatic vaginitis after starting SGLT2 inhibitors appear to be higher in real‐world practice than the rates of 31% and 5–10% in clinical trials, respectively. Risk factors of vaginal Candida colonization might be different before and after taking SGLT2 inhibitors.
Keywords: Real‐world practice, Sodium–glucose cotransporter 2 inhibitors, Vaginal candidiasis
Introduction
Patients with type 2 diabetes are at high risk of developing severe microvascular and macrovascular complications, such as cardiovascular disease, end‐stage renal disease and blindness1. These conditions are principally caused by hyperglycemia, and recently new drugs against hyperglycemia have been developed. Among them, sodium–glucose cotransporter 2 (SGLT2) inhibitors are the most recent addition to the therapeutic options available for the treatment of type 2 diabetes. SGLT2 inhibitors reduce rates of hyperglycemia by decreasing renal glucose reabsorption, thereby increasing urinary glucose excretion2. These agents have potential advantages with regard to their weight loss‐promoting effect, low risk of hypoglycemia, reduction in blood pressure, and reduction in cardiovascular and renal events in high‐risk patients3, 4, leading to the increasing popularity and spread of their use for the treatment of type 2 diabetes.
However, SGLT2 inhibitors do have some adverse effects including vaginal candidiasis for women. Generally, vaginal candidiasis is a common genital infection for women, and diabetes is a proven predisposing factor for vaginal candidiasis, along with pregnancy, use of broad‐spectrum antibiotics, high‐estrogen dose oral contraceptives, obesity and drug addiction5, 6, 7. Nevertheless, the prevalence and risk of vaginal Candida colonization and symptomatic vaginitis in women with diabetes remain unclear. There are few longitudinal investigations of vaginal Candida colonization in women with diabetes, whereas yeast colonization is likely a necessary precursor to symptomatic vaginitis. Although clinical trials showed the rate of discontinuing SGLT2 inhibitors and developing vaginitis after starting SGLT2 inhibitors3, 4, 8, 9, 10, 11, the incidence of vaginal Candida colonization and symptomatic vaginitis and risk in terms of clinical features and diabetic microvascular complications have not been adequately investigated in real‐world practice. In the present study, we evaluated the prevalence and risk of Candida colonization in women with diabetes before initiating the SGLT2 inhibitors, and showed the rate of discontinuing SGLT2 inhibitors, the incidence, risk, and time‐course of Candida colonization and symptomatic vaginitis after taking SGLT2 inhibitors in real‐world practice compared with clinical trials.
Methods
Study population
There were approximately 2,200 patients with diabetes who attended the Outpatient Clinic of Jiyugaoka Internal Medicine, Obihiro, Japan, in 2015, in which approximately 200 patients were treated with diet alone, 1,900 patients with antidiabetic tablets and 450 patients with insulin therapy. The following patients were excluded: (i) men; (ii) those with type 1 diabetes; (iii) those who had vaginitis symptoms or a history of recurrent vaginal candidiasis; and (iv) those who did not pass an initial 1‐year treatment for diabetes. Patients with type 2 diabetes who had higher body mass index or glycated hemoglobin (HbA1c) values and had preserved renal function were asked to use SGLT2 inhibitors, but further stringent or specific inclusion criteria were not set. Among the patients, all consecutive female patients with type 2 diabetes who started SGLT2 inhibitors were enrolled. After the advantages and possible adverse effects of SGLT2 inhibitors were explained, a self‐administered vaginal swab was taken at baseline, 6 and 12 months after taking SGLT2 inhibitors to examine vaginal candidiasis associated with SGLT2 inhibitors for clinical and research purposes. There were 147 female patients with type 2 diabetes who started the SGLT2 inhibitors during the period, and 33 patients refused to take a vaginal swab and the remaining 114 patients received the test. They used luseogliflozin (2.5 mg, n = 23), empagliflozin (10 mg, n = 22), tofogliflozin (20 mg, n = 20), canagliflozin (100 mg, n = 18), ipragliflozin (50 mg, n = 18) and dapagliflozin (5 mg, n = 13), and the dose was unchanged during the study period. The study was carried out in a primary care setting. The study was approved by the local ethics committee as #251014, and all participants provided written informed consent. The study was carried out in accordance with the Declaration of Helsinki II.
Measurements and definition
Type 2 diabetes was diagnosed according to the Japan Diabetes Society criteria; that is, fasting blood glucose ≥7.0 mmol/L or casual blood glucose ≥11.1 mmol/L. Body mass index was calculated as the ratio of bodyweight (kg) and height (m) squared. Blood pressure was measured with an appropriately sized cuff in the sitting position using an automated standardized blood pressure device. Non‐fasting blood samples and random urine samples were obtained from each patient. HbA1c (normal range of 4.6–6.2%) was measured by high‐performance liquid chromatography, which was certified by the National Glycohemoglobin Standardization Program, and the International Federation of Clinical Chemistry and Laboratory Medicine‐recommended units (mmol/mol) were also given. Serum and urinary concentrations of creatinine were measured by an enzymatic method. Urinary albumin was measured by a turbidimetric immunoassay. The estimated glomerular filtration rate (eGFR) was calculated using the following equation proposed by the Japanese Society of Nephrology: eGFR (mL/min/1.73 m2) = 194 × (age [years])−0.287 × (serum creatinine [mg/dL])−1.094 × 0.739 (if female). Diabetic retinopathy was diagnosed after pupillary dilation by ophthalmologists. Neuropathy was diagnosed in patients with two or more of three components: (i) the presence of symptoms; (ii) the absence of ankle tendon reflexes; and (iii) abnormal vibration perception threshold scores using a C128 tuning fork, where bilateral spontaneous pain, hypoesthesia or paresthesia of the legs was considered a neuropathic symptom. The urinary albumin excretion was assessed by using the albumin‐to‐creatinine ratio in random spot urine samples, and urinary white blood cells were detected by test strips (Siemens, Tokyo, Japan). Any microangiopathy included the presence of any retinopathy, neuropathy or nephropathy defined as an albumin‐to‐creatinine ratio ≥30 mg/gCr. Menopausal status was collected by an interview.
A self‐administered vaginal swab was collected from the patients and was cultured for Candida. Chromoagar‐Candida (Kanto Kagaku, Tokyo, Japan), which is a chromogenic medium allowing the presumptive identification of Candida albicans, Candida tropicalis and Candida krusei based on the color and shape of the colonies, was used. Other Candida species were identified by Sabouraud dextrose agar with Vitek 2 (Sysmex Biomerieux, Kobe, Japan).
Statistical analysis
The differences in clinical characteristics between the groups were analyzed, in which the significance of differences between groups was assessed by χ2‐tests for categorical variables, and the Student's t‐test for continuous variables. Data were expressed as the mean ± standard deviation if normally distributed. Incidence rates of vaginal Candida colonization and symptomatic vaginitis per 1,000 person‐years and the corresponding 95% confidence interval were calculated. The incidence rate was defined as the number of new cases divided by the total number of person‐years of follow up. The multiple logistic regression analysis to determine the variables associated with positive vaginal Candida colonization at baseline was carried out, with covariates of age, HbA1c, eGFR and microangiopathy that showed significant associations with vaginal candidiasis between the groups. Similarly, the multiple logistic regression analysis to determine the predictors for conversion to positive cultures for vaginal candidiasis after 6 months of taking SGLT2 inhibitors was carried out, with the covariates of model 1 being age and microangiopathy, and model 2 being postmenopause and microangiopathy. Variables that were closely associated; for example, age and postmenopause, were not entered simultaneously to avoid the effect of collinearity in the model. A P‐value of <5% (two‐tailed) was considered significant. All analyses were carried out with the statistical software package SPSS (SPSS Japan, Tokyo, Japan).
Results
Baseline positive cultures for Candida
Among 114 patients with type 2 diabetes who were free of vaginitis symptoms and received a vaginal candidiasis test before starting SGLT2 inhibitors, there were 17 (14.9%) patients who had vaginal cultures positive for Candida. Table 1 shows the clinical characteristics of the patients, and the comparison between those who had positive and negative cultures for Candida. The species detected from the 17 positive patients were C. albicans (n = 9), C. glabrata (n = 3), C. albicans plus C. glabrata (n = 1), C. parapsilosis (n = 3) and C. krusei (n = 1). Thus, the proportion of C. albicans and C. glabrata was 58.8 and 23.5%, respectively. The patients with positive cultures were younger and had significantly higher HbA1c and eGFR values, and microangiopathy than those without Candida growth; otherwise, no significant differences were found. The multiple logistic regression analysis to determine the variables associated with the presence of vaginal Candida colonization at baseline, including age, HbA1c, eGFR and microangiopathy as covariates, showed that age (odds ratio [OR] 0.94, 95% confidence interval [CI] 0.89–0.99/year, P < 0.05) and microangiopathy (OR 4.0, 95% CI 1.1–15.1, P < 0.05) were significantly associated with vaginal Candida colonization.
Table 1.
Clinical characteristics of patients with type 2 diabetes who showed positive and negative cultures for vaginal Candida that were carried out before starting sodium–glucose cotransporter 2 inhibitors
| Total (n = 114) | Cultures for vaginal Candida at baseline | |||
|---|---|---|---|---|
| Positive (n = 17) | Negative (n = 97) | P‐value | ||
| Age (years) | 53.3 ± 11.3 | 46.6 ± 12.6 | 54.4 ± 10.7 | <0.01 |
| Known duration of diabetes (years) | 9.7 ± 7.0 | 7.3 ± 7.4 | 10.1 ± 6.9 | NS |
| Body mass index (kg/m2) | 31.7 ± 6.0 | 33.4 ± 9.1 | 31.4 ± 5.3 | NS |
| HbA1c, % (mmol/mol) | 7.5 ± 1.2 (62 ± 10) | 8.3 ± 1.8 (71 ± 15) | 7.4 ± 1.0 (61 ± 8) | <0.01 |
| Diet alone/tablets/insulin (%) | 9.6/63.2/27.2 | 11.8/76.4/11.8 | 9.3/60.8/29.9 | NS |
| Use of DPP4 inhibitors (%) | 60.5 | 64.7 | 59.8 | NS |
| Use of sulfonylurea (%) | 28.9 | 29.4 | 28.9 | NS |
| Use of metformin (%) | 74.6 | 70.6 | 75.3 | NS |
| Use of pioglitazone (%) | 13.2 | 17.6 | 12.4 | NS |
| Systolic blood pressure (mmHg) | 124 ± 13 | 129 ± 15 | 123 ± 13 | NS |
| Diastolic blood pressure (mmHg) | 72 ± 12 | 75 ± 12 | 72 ± 12 | NS |
| Albuminuria (mg/gCr†) | 13.3 (7.1–31.0) | 29.0 (11.1–115.6) | 12.2 (6.9–27.9) | NS |
| eGFR (mL/min/1.73 m2) | 82.5 ± 22.4 | 92.9 ± 31.2 | 80.1 ± 20.1 | <0.05 |
| Retinopathy (%) | 20.2 | 17.6 | 20.6 | NS |
| Neuropathy (%) | 36.0 | 47.1 | 34.0 | NS |
| Any microangiopathy (%) | 51.8 | 76.5 | 47.4 | <0.05 |
| Postmenopause (%) | 66.7 | 50.0 | 69.1 | NS |
| Positive for urinary WBC (%) | 20.8 | 17.7 | 21.7 | NS |
Total n = 114. †Median and interquartile range are given. eGFR, estimated glomerular filtration rate; HbA1c, glycated hemoglobin; NS, not significant; WBC, white blood cell.
Candida colonization after starting SGLT2 inhibitors
As shown in Figure 1, among 114 patients who started taking SGLT2 inhibitors, eight patients discontinued by themselves due to symptomatic vaginal candidiasis within a month (of whom one had Candida growth at baseline and seven had no Candida growth at baseline), 15 discontinued due to other reasons (i.e., no effect, frequent urination) and 17 refused the 6‐month test; thus, the remaining 74 patients (64.9%) underwent the test at 6 months after taking SGLT2 inhibitors.
Figure 1.
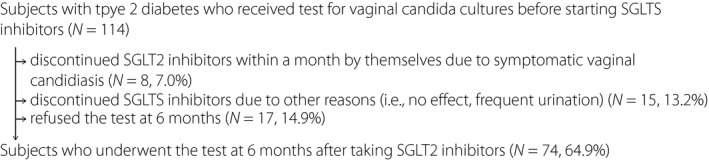
Patient flow chart showing tests for vaginal Candida cultures from baseline before starting sodium–glucose cotransporter 2 (SGLT2) inhibitors to 6 months after taking SGLT2 inhibitors.
Table 2 shows the conversion of vaginal cultures from baseline to 6 months after taking SGLT2 inhibitors. All nine patients who had Candida growth at baseline showed positive cultures at 6 months. Of 65 patients without Candida growth at baseline, 24 (36.9%) converted to positive cultures at 6 months. The species were C. albicans (n = 10), C. glabrata (n = 8), C. albicans plus C. glabrata (n = 2), C. parapsilosis (n = 2), C. glabrata and C. parapsilosis (n = 1), and C. krusei (n = 1). Thus the proportion of C. albicans and C. glabrata was 45.8% and 41.7%, respectively. The incidence rate from negative to positive cultures after 6 months of taking SGLT2 inhibitors was 939.4 (95% CI 797.7–992.6)/1,000 person‐years (78.3/1,000 person‐months). Table 3 shows the comparison of baseline clinical features between those who converted to positive cultures and those who remained negative at 6 months after taking SGLT2 inhibitors. Patients who converted to positive were significantly older, had a higher value of albuminuria at baseline, and had higher rates of neuropathy, any microangiopathy and were postmenopausal. The multiple logistic regression analysis to determine the predictors for conversion, including model 1 of age and microangiopathy, and model 2 of postmenopause and microangiopathy as covariates, showed that age (OR 1.08, 95% CI 1.02–1.14/year, P = 0.005) in model 1, and postmenopause (OR 5.01, 95% CI 1.45–17.31, P = 0.010) in model 2 were significantly associated with the conversion.
Table 2.
Vaginal cultures at baseline and 6 months after taking sodium–glucose cotransporter 2 inhibitors
| At 6 months after taking SGLT2 inhibitors | ||
|---|---|---|
| Negative | Positive | |
| At baseline before taking SGLT2 inhibitors | ||
| Negative n = 65 | 41 (31, 1) | 24 (3, 11) |
| Positive n = 9 | 0 | 9 (1, 2) |
Total n = 74. In parenthesis, the number of negative and positive cultures at 12‐months is given at left and right, respectively. The number of patients is given. SGLT2, sodium–glucose cotransporter 2.
Table 3.
Comparison of clinical features at baseline and 6 months between patients with negative cultures for vaginal Candida at baseline who converted to positive cultures and who remained negative at 6 months after taking sodium–glucose cotransporter 2 inhibitors
| Converted to positive (n = 24) | Remained negative (n = 41) | P‐value | |
|---|---|---|---|
| Age (years) | 57.9 ± 9.2 | 49.9 ± 10.5 | <0.01 |
| Known duration of diabetes (years) | 11.1 ± 7.4 | 8.0 ± 6.8 | NS |
| Body mass index (kg/m2) | 32.3 ± 5.0 | 31.1 ± 5.2 | NS |
| HbA1c, % (mmol/mol) | 7.1 ± 0.8 (58 ± 5) | 7.6 ± 1.2 (57 ± 7) | NS |
| Systolic blood pressure (mmHg) | 120 ± 14 | 123 ± 14 | NS |
| Albuminuria (mg/gCr†) | 16.3 (11.3–31.5) | 8.3 (4.9–21.5) | <0.05 |
| eGFR (mL/min/1.73 m2) | 81.5 ± 22.3 | 84.3 ± 22.0 | NS |
| Retinopathy (%) | 25.0 | 14.6 | NS |
| Neuropathy (%) | 50.0 | 24.4 | <0.05 |
| Any microangiopathy | 62.5 | 36.6 | <0.05 |
| Postmenopause (%) | 87.5 | 53.7 | <0.01 |
| Positive for urinary WBC (%) | 26.1 | 16.2 | NS |
| At 6 months | |||
| Body mass index (kg/m2) | 30.9 ± 5.1 | 29.8 ± 5.1 | NS |
| ΔBMI | −1.4 ± 0.9 | −1.3 ± 1.1 | NS |
| HbA1c (%) | 7.1 ± 0.6 | 7.0 ± 0.8 | NS |
| ΔA1C | −0.01 ± 0.7 | −0.55 ± 1.0 | <0.05 |
†Median and interquartile range are given. BMI, body mass index; eGFR; estimated glomerular filtration rate, HbA1c, glycated hemoglobin; NS, not significant; WBC; white blood cell.
Symptomatic vaginitis after starting SGLT2 inhibitors
Regarding symptomatic vaginitis, of 33 patients with Candida growth at 6 months as shown in Table 2 had vaginitis symptoms. Seven patients were from the 24 who were negative at baseline and three were from the nine who were positive at baseline. Of 10 patients, seven (70.0%) had C. albicans and three (30.0%) had C. glabrata. Including eight patients who discontinued SGLT2 inhibitors due to symptomatic vaginitis within a month, there were 18 (15.8%) patients in total who developed symptomatic vaginitis among the 114 patients who had no symptoms at baseline and started taking SGLT2 inhibitors. This yielded the incidence rate of symptomatic vaginitis after taking SGLT2 inhibitors to be 391.3 (95% CI 250.9–546.3)/1,000 person‐years (32.6/1,000 person‐months). A total of 18 patients had characteristics similar to the 24 patients shown in Table 3, and all vaginitis symptoms were mild in severity.
Results of cultures at 12 months after taking SGLT2 inhibitors
Among the 74 patients who received the test at 6 months, 49 patients continued taking SGLT2 inhibitors for ≥12 months and underwent the test at 12 months, 13 discontinued including five due to the vaginitis symptoms, and 12 did not reach the 12‐month test. The results of cultures at 12 months are shown in parentheses in Table 2. Of 32 patients with negative cultures at 6 months, 31 (96.9%) showed negative results at 12 months. Of 17 patients who had positive cultures at 6 months, 13 (76.5%) showed positive results at 12 months in which 12 were asymptomatic and one was symptomatic. In total, during the period from 6 to 12 months, the rates of developing positive Candida colonization and symptomatic candidiasis were 3.1% (1/32) and 8.1% (6/74), respectively.
Discussion
In the present study, we found that 24 of 65 (36.9%) patients without Candida growth before taking SGLT2 inhibitors converted to positive for Candida culture at 6 months after taking SGLT2 inhibitors, yielding a crude incidence of 939.4/1,000 person‐years (78.3/1,000 person‐months). The risks related to developing positive vaginal colonization were older age, albuminuria, neuropathy and postmenopause. The present study showed the rate of developing symptomatic vaginitis after taking SGLT2 inhibitors to be 15.8%, yielding a crude incidence of 391.3/1,000 person‐years (32.6/1,000 person‐months). These rates of vaginal Candida colonization and symptomatic vaginitis found in real‐world practice appeared to be higher as compared with the findings in clinical trials3, 4, 8, 9, 10, 11, as previous clinical trials showed rates of vaginal Candida colonization to be 31%8, those of symptomatic vaginitis to be 5–10%3, 4, 8, 9, 10, 11 and the incidence of vaginitis to be 52–66/1,000 person‐years10. We found that patients with negative vaginal Candida cultures at 6 months most likely remained negative at 12 months and vice versa. Although vaginal candidiasis was not serious and the effect of antifungal treatment after taking SGLT2 inhibitors was not evaluated, we suggest that careful monitoring and care are important for treatment with SGLT2 inhibitors.
Before starting SGLT2 inhibitors, we found that 14.9% of patients had vaginal cultures positive for Candida. Apart from the use of SGLT2 inhibitors, there are only a few reports in patients with diabetes regarding the prevalence of vaginal Candida colonization, which requires vaginal cultures that are mostly collected through self‐administered swabs5, 8, 9, 10. The prevalence seems to vary according to ethnicity, area and age. Goswami et al.12 from India reported the prevalence of vaginal Candida colonization to be 46% in 78 patients with diabetes, which was significantly higher than 23% in 88 patients without diabetes. The prevalence was higher as compared with the present study, and one reason might be the younger age; that is, a mean age of 32 years. Nyirjesy et al.8 reported the prevalence of vaginal Candida colonization to be 12% in 198 patients with type 2 diabetes at a mean age of 52 years including multiple ethnicities, which was consistent with the present data. The incidence of symptomatic vaginitis was reported to be 21.0/1,000 person‐years in patients with type 2 diabetes, with the risk being 1.81 greater than those without diabetes in the UK General Practice Research Database13. Although the study was not laboratory‐confirmed but interview‐based, this epidemiological study included 125,237 women followed for 1 year, and the incidence was found to be significantly higher in patients with type 2 diabetes of younger age and with higher HbA1c. Consistently, we found that younger age and the presence of microangiopathy were associated with positive culture for Candida at baseline. The inverse age association might be in relation to sexual activity8, 12, 14. The present findings showed that obese women with poorly controlled type 2 diabetes and microangiopathy, which are attributable to elevated eGFR, are characteristics of patients that are likely to have Candida colonization.
The present study showed that the rates of vaginal Candida colonization during the period from the start of SGLT2 inhibitors to 6 months and from 6 to 12 months were 36.9% and 3.1%, respectively, and the corresponding rate of developing symptomatic vaginitis was 15.8% and 8.1%, respectively. We consider that these rates in real‐world practice were high, and the risk of vaginal candidiasis due to SGLT2 inhibitors was high at the initiation phase, which was lowered thereafter.
In the canagliflozin phase 2 trial followed for 12 weeks, the conversion rate of positive colonization was 31%8, which was slightly lower than the present study. We found no predictive effect of baseline HbA1c and body mass index on the conversion to positive, which was consistent with the phase 2 trial. It was also consistent in both the present study and the canagliflozin phase 2 trial that most of the patients with positive Candida cultures at baseline remained positive after taking SGLT2 inhibitors.
The canagliflozin trial found that 16 of 154 patients taking canagliflozin (10.4%) developed vulvovaginal adverse effects8, which might indicate symptomatic vaginitis. Regarding a risk for developing symptomatic vaginitis, the trial indicated that positive baseline culture was a possible risk, in which six out of 16 (37.5%) who had positive baseline culture developed symptomatic vaginitis. However, the rate we found was just 5.9% (1/17). We have no explanation for this difference, and future studies on this issue are required.
Although the phase 2 trial did not investigate diabetic microvascular complications, we found that patients with diabetic microvascular complications are likely susceptible to developing vaginal Candida colonization and symptomatic vaginitis. Factors such as older age, longer duration of diabetes and a higher proportion of postmenopause are in line with having a higher risk for diabetic microvascular complications. The finding that most of those with negative cultures at 6 months showed negative results at 12 months and vice versa might be helpful in considering the need for antifungal therapy.
Importantly, it is likely that the risks of colonization and symptomatic vaginitis are different between before (without) and after taking SGLT2 inhibitors. Younger age for patients before starting SGLT2 inhibitors and older age after starting SGLT2 inhibitors were indicated as an independent risk for Candida colonization in multivariate analysis. Young age, which was a risk factor for Candida growth before SGLT2 inhibitors treatment, might be associated with estrogen‐stimulated glycogen content of the vaginal epithelium, which could serve as an energy source for Candida 6, 14. When elderly patients, despite postmenopausal loss of estrogenic stimulation and decreased glycogen content before SGLT2 inhibitor treatment, are exposed to high urine glucose excretion under a condition accompanied with microvascular impairment due to diabetes, Candida colonization is likely to occur. To explore the relevant indication of SGLT2 inhibitors, and minimize developing vaginal Candida colonization and symptomatic vaginitis, further studies are required.
Although rates of discontinuing SGLT2 inhibitors due to genital mycotic infection were very low in several clinical trials8, 9, 10, 11, the rate in the present study was high; that is, 20.2% (7.0% due to symptomatic vaginitis and 13.2% due to other reasons). In the phase 2 trial followed for 12 weeks, no patients discontinued taking SGLT2 inhibitors8. In the present study, it was a fact that few cases prepared and used antifungal treatment. Furthermore, the higher rate observed in the present study might be explained by the difference of conducting systems between clinical trials and real‐world practice. Although clinical trials remain the most reliable source of clinical evidence and are the gold standard for showing clinical efficacy, the stringent constraints of a clinical trial setting and the selection of patients enrolled might limit the generalizability of clinical trials to routine clinical practice. Other sources of evidence, such as real‐world data, can be used to fill this gap and complement the available clinical trials evidence15.
Regarding Candida species, previous studies have shown that C. albicans is the major cause of symptomatic vaginitis, whereas C. glabrata is less virulent, but increasing8, 16, 17. Consistently, we observed that C. albicans was dominant in symptomatic vaginitis, and C. glabrata was dominant in asymptomatic Candida colonization. The proportion of C. glabrata at baseline was four of 17 (23.5%), which increased to 10 of 24 (41.7%) after taking SGLT2 inhibitors. Future studies are necessary to investigate the species in association with SGLT2 inhibitors and symptomatic vaginitis.
There were some limitations to the present study. We should acknowledge that the number of patients who received the test at baseline and 6 months was rather small, and several patients refused the vaginal swab. We should also acknowledge the lack of a control group. We were unable to collect vaginal cultures from eight patients who discontinued SGLT2 inhibitors within a month, because they discontinued SGLT2 inhibitors by themselves due to vaginitis symptoms. As it is generally considered that the efficacy rates of antifungal treatment are high and follow‐up test‐of‐cure after the completion of treatment is unnecessary18, we did not evaluate the use and effect of antifungal treatment. Despite these issues, we believe that such a real‐world practice study is important in considering whether to initiate SGLT2 inhibitors.
In conclusion, the rate of developing positive vaginal culture for Candida and symptomatic vaginitis after starting SGLT2 inhibitors appears to be rather high in real‐world practice. Risk factors of vaginal Candida colonization appeared to be different before and after taking SGLT2 inhibitors.
Disclosure
The authors declare no conflict of interest.
J Diabetes Investig 2019; 10: 439–445
References
- 1. Brownrigg JR, Hughes CO, Burleigh D, et al Microvascular disease and risk of cardiovascular events among individuals with type 2 diabetes: a population‐level cohort study. Lancet Diabetes Endocrinol 2016; 4: 588–597. [DOI] [PubMed] [Google Scholar]
- 2. Gallo LA, Wright EM, Vallon V. Probing SGLT2 as a therapeutic target for diabetes: basic physiology and consequences. Diab Vasc Dis Res 2015; 12: 78–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zinman B, Wanner C, Lachin JM, et al Empagliflozin, cardiovascular outcomes, and mortality in Type 2 diabetes. N Engl J Med 2015; 373: 2117–2128. [DOI] [PubMed] [Google Scholar]
- 4. Wanner C, Inzucchi SE, Lachin JM, et al Empagliflozin and progression of kidney disease in Type 2 diabetes. N Engl J Med 2016; 375: 323–334. [DOI] [PubMed] [Google Scholar]
- 5. de Leon EM, Jacober SJ, Sobel JD, et al Prevalence and risk factors for vaginal Candida colonization in women with type 1 and type 2 diabetes. BMC Infect Dis 2002; 2: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sobel JD. Vulvovaginal candidosis. Lancet 2007; 369: 1961–1971. [DOI] [PubMed] [Google Scholar]
- 7. Bohannon NJ. Treatment of vulvovaginal candidiasis in patients with diabetes. Diabetes Care 1998; 21: 451–456. [DOI] [PubMed] [Google Scholar]
- 8. Nyirjesy P, Zhao Y, Ways K, et al Evaluation of vulvovaginal symptoms and Candida colonization in women with type 2 diabetes mellitus treated with canagliflozin, a sodium glucose co‐transporter 2 inhibitor. Curr Med Res Opin 2012; 28: 1173–1178. [DOI] [PubMed] [Google Scholar]
- 9. Johnsson KM, Ptaszynska A, Schmitz B, et al Vulvovaginitis and balanitis in patients with diabetes treated with dapagliflozin. J Diabetes Complications 2013; 27: 479–484. [DOI] [PubMed] [Google Scholar]
- 10. Kohler S, Zeller C, Iliev H, et al Safety and tolerability of empagliflozin in patients with Type 2 diabetes: pooled analysis of phase I‐III clinical trials. Adv Ther 2017; 34: 1707–1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nyirjesy P, Sobel JD, Fung A, et al Genital mycotic infections with canagliflozin, a sodium glucose co‐transporter 2 inhibitor, in patients with type 2 diabetes mellitus: a pooled analysis of clinical studies. Curr Med Res Opin 2014; 30: 1109–1119. [DOI] [PubMed] [Google Scholar]
- 12. Goswami R, Dadhwal V, Tejaswi S, et al Species‐specific prevalence of vaginal candidiasis among patients with diabetes mellitus and its relation to their glycaemic status. J Infect 2000; 41: 162–166. [DOI] [PubMed] [Google Scholar]
- 13. Hirji I, Andersson SW, Guo Z, et al Incidence of genital infection among patients with type 2 diabetes in the UK General Practice Research Database. J Diabetes Complications 2012; 26: 501–505. [DOI] [PubMed] [Google Scholar]
- 14. Dennerstein GJ, Ellis DH. Oestrogen, glycogen and vaginal candidiasis. Aust NZ J Obstet Gynaecol 2001; 41: 326–328. [DOI] [PubMed] [Google Scholar]
- 15. Elliott L, Fidler C, Ditchfield A, et al Hypoglycemia event rates: a comparison between real‐world data and randomized controlled trial populations in insulin‐treated diabetes. Diabetes Ther 2016; 7: 45–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gonçalves B, Ferreira C, Alves CT, et al Vulvovaginal candidiasis: epidemiology, microbiology and risk factors. Crit Rev Microbiol 2016; 42: 905–927. [DOI] [PubMed] [Google Scholar]
- 17. Kennedy MA, Sobel JD. Vulvovaginal candidiasis caused by non‐Albicans Candida species: new insights. Curr Infect Dis Rep 2010; 12: 465–470. [DOI] [PubMed] [Google Scholar]
- 18. Nyirjesy P, Sobel JD. Genital mycotic infections in patients with diabetes. Postgrad Med 2013; 125: 33–46. [DOI] [PubMed] [Google Scholar]


