Abstract
Aims/Introduction
On April 14 and 16 2016, the Kumamoto area was severely damaged by several massive magnitude 7 class earthquakes.
Materials and Methods
To examine the effects of these earthquakes on glycemic control and stress factors, glycated hemoglobin, glycated albumin, other biochemical parameters, a self‐administered lifestyle‐associated questionnaire and disaster‐associated stress scores were analyzed. A total of 557 patients with diabetes were enrolled, and data were collected at 13 months before to 13 months after the earthquakes.
Results
In patients with type 1 diabetes and specific types of diabetes due to other causes, glycemic control was not altered during the observational period. This glycemic stability in type 1 diabetes might result from self‐management of insulin doses. In patients with type 2 diabetes, glycated hemoglobin decreased by 0.11% (from 7.33 to 7.22%) at 1–2 months after the earthquakes, and increased thereafter. The reduction of glycated hemoglobin after 1–2 months in type 2 diabetes was associated with ‘early restoration of lifelines’ and ‘sufficient sleep.’ The glycemic deterioration at a later stage was related to ‘shortage of antidiabetic agents,’ ‘insufficient amount of food,’ ‘largely destroyed houses’ and ‘changes in working environments.’ Disaster‐associated stress levels were positively correlated with ‘age,’ ‘delayed restoration of lifelines,’ ‘self‐management of antidiabetic agents’ and ‘increased amount of physical activity/exercise,’ and negatively associated with ‘early restoration of lifelines’ and ‘sufficient sleep.’
Conclusions
Glycemic control, associated factors and stress levels are altered in chronological order. Post‐disaster diabetic medical care must consider these corresponding points in accordance with the time‐period.
Keywords: Diabetes, Earthquake, Glycemic control
Introduction
In April 2016, the Kumamoto area located on the island of Kyushu, southwest Japan, was severely damaged by several massive earthquakes. A magnitude (M) 7.3 on the Richter scale mainshock occurred on April 16 2016, close to the epicenter of an M 6.5 foreshock that occurred approximately 28 h earlier (Figure 1)1. These two huge earthquake sequences generated severe shaking, and caused extensive destruction in central Kyushu. The earthquakes caused 50 casualties, and >7,000 buildings were severely damaged. The epicenters of the two major earthquakes were located in the western part of the Mashiki Town, and Kumamoto University Hospital is mapped approximately 10 km west from the epicenters (Figure 1).
Figure 1.
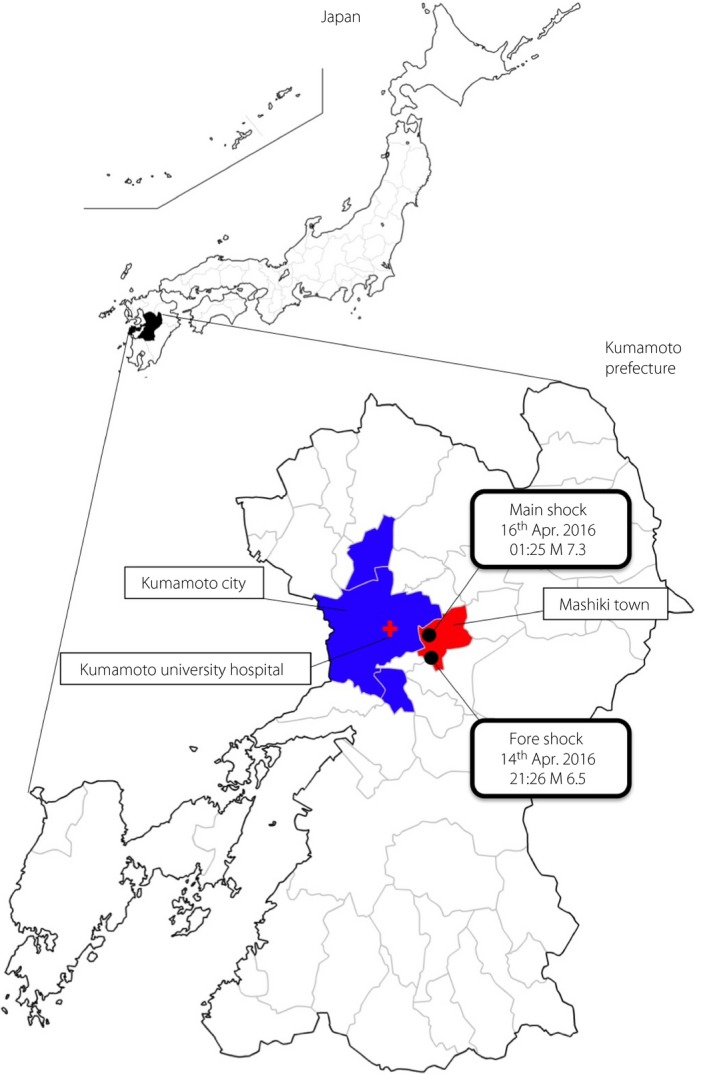
The geographical location of Kumamoto University Hospital and the epicenters. Closed circles indicate the epicenters. A cross sign indicates the location of Kumamoto University Hospital approximately 10 km west of the epicenters.
Previous reports have shown that, after a natural disaster, glycemic control in patients with diabetes deteriorates2, 3, 4, 5, 6, 7, 8, 9. Such worsening of glycemic control can be explained by inadequate food intake6, 9. It has also been proposed that post‐disaster glycemic control alterations vary among individual patients7. Glycemic control in patients with diabetes after the 1995 Hanshin‐Awaji earthquake in Japan significantly deteriorated in the Kobe area, but not in the Osaka area3. In 2011, the Great East Japan Earthquake struck the Tohoku area in Japan, and glycated hemoglobin (HbA1c) in patients with type 1 diabetes involved in the earthquake became 0.26% higher, indicating that patients with a lower insulin secretory capacity might be more vulnerable to stressful conditions7. The stressful conditions provoked by prolonged aftershocks, long‐term shelter life and/or spending nights in a car were problematic after the Kumamoto earthquakes. To identify the association between lifestyle alterations, stress levels and glycemic changes in patients with diabetes affected by the Kumamoto earthquakes, we examined the alterations in metabolic parameters, physical examinations and biochemical data. In addition, we carried out questionnaire surveys of the study participants regarding earthquake‐related damage and post‐earthquake lifestyle alterations, as well as identifying traumatic stress scores using the Impact of Event Scale‐Revised (IES‐R).
Methods
Study population
The present study was approved by the ethics committee of Kumamoto University Hospital (Ethics No. 1170), and was carried out in line with the ethical rules of the Declaration of Helsinki in 1995. The observational research was registered with an approved International Committee of Medical Journal Editors clinical trial registry, University Medical Hospital Information Network (ID: UMIN000024757), and the date of registration is 8 November 2016. We carefully obtained informed consent as well as questionnaire responses from individual patients attending doctors for their mental burden. As a result, there were no rejections in the participation of this study, and no problems associated with mental burden.
To identify potential association markers, we collected data on several metabolic parameters, including glycemic control indexes, such as HbA1c, glycated albumin (GA) and random plasma glucose, from 727 outpatients with diabetes who had been regularly followed up at Kumamoto University Hospital, Kumamoto, Japan. To minimize other possible influential factors, exclusion criteria were specified as follows: thyroid dysfunction (71 patients), active hepatic disease (22 patients), pregnancy (excluded at recruitment), taking medication that affects glucose levels (excluded at recruitment), regular follow‐up period of <12 months (73 patients) and living outside Kumamoto prefecture at the time of the earthquakes (four patients). After a total of 170 exclusions, 557 patients were considered to be eligible for the analysis.
Study design
We examined the parameters in these patients 1–2, 3–4, 6–7 and 12–13 months before, and 1–2, 3–4, 6–7 and 12–13 months after the 2016 Kumamoto earthquakes. We carried out a questionnaire survey of the study participants regarding earthquake‐related damage and post‐earthquake lifestyle alterations. Post‐traumatic mental stress levels were assessed using the IES‐R score10.
Laboratory and physical examinations
Observational acquisition of data, such as the type of diabetes, diabetes history, bodyweight, systolic and diastolic blood pressure, heart rate, and biochemical parameters including random blood glucose, HbA1c, GA, immune reactive insulin, C‐peptide, urinary albumin excretion, aspartate transaminase, alanine transaminase, lactate dehydrogenase, blood urea nitrogen, creatinine, estimated glomerular filtration rate, uric acid, low‐density lipoprotein cholesterol, high‐density lipoprotein cholesterol, triglyceride, total cholesterol, white blood cells, red blood cells, hemoglobin, platelets and hematocrit was carried out.
Statistical analysis
Continuous variables were expressed as average ± standard deviation, and categorical variables were expressed as percentages. Pre‐ and post‐glycemic control were assessed by mixed model statistics.
Results
Baseline characteristics of eligible participants in the study
The baseline characteristics of the participants in the present study are shown in Table 1. A total of 55 patients with type 1 diabetes, 449 with type 2 diabetes and 53 with specific types of diabetes due to other causes (Others) were enrolled and their data collected. The mean age of type 2 diabetes patients (63.4 ± 11.9 years) was significantly higher than that of type 1 diabetes patients (51.2 ± 16.4 years) or Others (59.3 ± 12.7 years). The sex ratio was comparable among groups. The duration of diabetes history was shorter in Others (9.1 ± 7.2 years) than that in type 1 diabetes patients (20.0 ± 9.8 years) or type 2 diabetes (14.6 ± 9.5 years). The mean HbA1c in type 1 diabetes patients (8.23 ± 1.54%) was significantly higher than that of type 2 diabetes (7.26 ± 1.07%) or Others (7.08 ± 1.28%). The baseline physical examinations, such as blood pressure and heart rate, were indistinguishable among the groups. The prevalence of diabetic nephropathy was significantly higher in type 2 diabetes patients (35.6%) than in type 1 diabetes patients (28.2%) or Others (22.5%). The presence of retinopathy and neuropathy was not different among the groups. In terms of medications, oral hypoglycemic agents were predominantly prescribed for type 2 diabetes patients (81.6%). The ratio of insulin treatment in type 1 diabetes patients was the highest at 98.6%, compared with 33.8 and 59.6% in type 2 diabetes patients and Others, respectively.
Table 1.
Clinical characteristics of 557 participants before the earthquakes
| Type 1 diabetes | Type 2 diabetes | Others | |
|---|---|---|---|
| n | 55 | 449 | 53 |
| Age (years) | 51.2 ± 16.4 | 63.4 ± 11.9‡ | 59.3 ± 12.7 |
| Male/female | 20/35 | 239/210 | 20/33 |
| BMI | 22.2 ± 3.7 | 25.4 ± 4.8 | 23.9 ± 4.8 |
| Diabetes history (years) | 20.0 ± 9.8 | 14.6 ± 9.5 | 9.1 ± 7.2** |
| Blood glucose (mg/dL) | 177.4 ± 72.3 | 150.9 ± 47.3 | 135.4 ± 49.9 |
| HbA1c (%) | 8.23 ± 1.54* | 7.26 ± 1.07 | 7.08 ± 1.28 |
| GA (%) | 26.6 ± 7.3 | 18.6 ± 3.8 | 19.4 ± 6.7 |
| SBP (mmHg) | 121.0 ± 16.5 | 128.6 ± 17.1 | 124.9 ± 16.0 |
| DBP (mmHg) | 67.5 ± 13.2 | 72.6 ± 11.8 | 72.8 ± 11.8 |
| HR (b.p.m) | 76.8 ± 12.0 | 77.7 ± 12.2 | 79.2 ± 13.4 |
| Retinopathy | 36.60% | 29.40% | 20.50% |
| Nephropathy | 28.20% | 35.6%§ | 22.50% |
| Neuropathy | 34.30% | 34.20% | 20.30% |
| OHA | 15.50% | 81.6%‡ | 55.40% |
| Insulin | 98.6%† | 33.80% | 59.5%†† |
| GLP‐1RA | 0% | 10.0%‡ | 5.40% |
Data are presented as means or ratio (%). The Fisher's exact test with Bonferroni correction were carried out. *P = 0.002 type 1 diabetes vs type 2 diabetes. † P < 0.001 type 1 diabetes vs type 2 diabetes or specific types of diabetes due to other causes (Others). ‡ P < 0.001 type 2 diabetes vs type 1 diabetes or Others. § P = 0.037 type 2 diabetes vs Others. **P < 0.001 Others vs type 1 diabetes or type 2 diabetes. †† P < 0.001 Others vs type 2 diabetes. DBP, diastolic blood pressure; GA, glycated albumin; GLP‐1RA, glucagon like peptide‐1 receptor agonist; HbA1c, glycated hemoglobin; HR, heart rate; OHA, oral hypoglycemic agents; SBP, systolic blood pressure.
Comparison of pre‐ and post‐earthquake glycemic parameters
Physical examinations, such as bodyweight, systolic blood pressure, diastolic blood pressure and heart rate, were not altered during the observational period. Blood glucose levels at random sampling were not significantly altered after the earthquakes compared with those before the earthquakes in all types of diabetes (type 1 diabetes 181.2 ± 66.3 mg/dL, type 2 diabetes 148.9 ± 45.0 mg/dL, Others 142.9 ± 62.1 mg/dL at 1–2 months after the earthquakes). In type 1 diabetes patients and Others, HbA1c and GA levels during the study period were unchanged. In type 2 diabetes patients, HbA1c first declined by 0.11% (from 7.33 to 7.22%) at 1–2 months after the earthquakes compared with that before the earthquakes, and increased at 3–4, 6–7 and 12–13 months after the earthquakes. GA levels showed a similar trend in type 2 diabetes patients (Figure 2). As >80% of the patients in the present study had type 2 diabetes, the trend in HbA1c alterations in across all participants was quite similar to that seen in type 2 diabetes patients (Figure 2). The correlation between delta bodyweight and delta HbA1c was not significant (P = 0.089) in the present study. There were no significant alterations in other biochemical parameters (data no shown).
Figure 2.
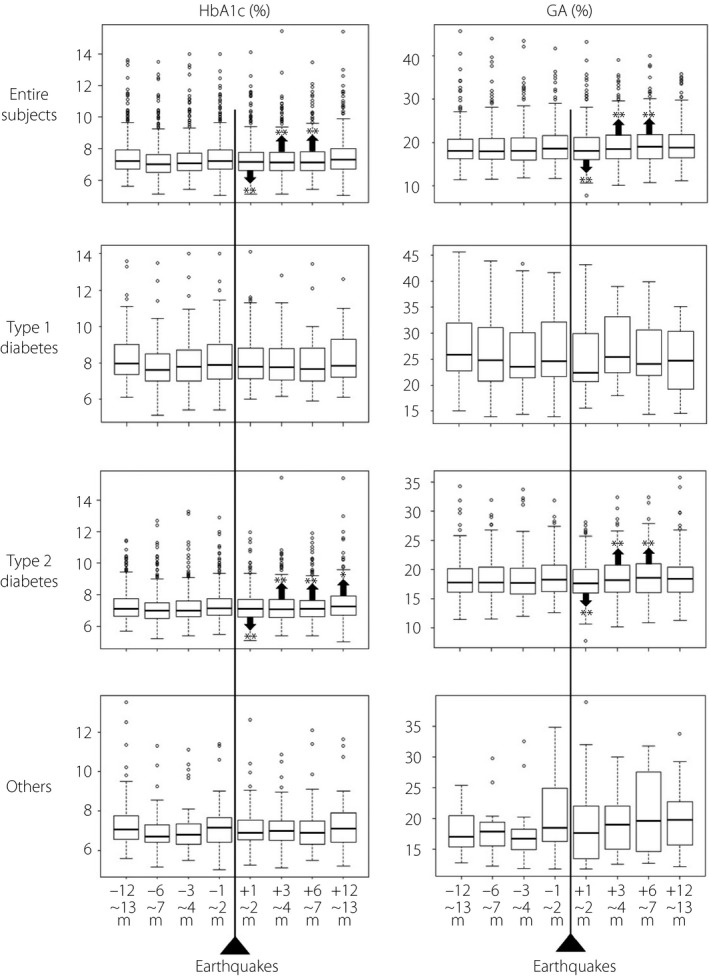
Chronological alterations in glycated hemoglobin (HbA1c) and glycated albumin (GA) in all patients, type 1 diabetes patients, type 2 diabetes patients and patients with diabetes due to other causes (Others). The median, first and third quartiles of HbA1c and GA are expressed in a box plot. The statistical analysis was carried out using a mixed model. *P < 0.05, **P < 0.01 compared with the corresponding values before the earthquake.
Results of the self‐administered lifestyle‐associated questionnaire at 1 month after the earthquakes
All eligible study participants were living in the Kumamoto area at the time of the earthquakes.
The results of the life management component of the questionnaire are shown in Table 2.
Table 2.
Results of self‐administered lifestyle‐associated questionnaire at 1 month after the earthquakes (life management)
| Total, % | Type 1 diabetes, % | Type 2 diabetes, % | Others, % | |
|---|---|---|---|---|
| 1) Evacuation after foreshock | ||||
| In shelters | 4.69 | 5.56 | 4.91 | 1.92 |
| In their cars | 10.65 | 14.81 | 10.49 | 7.69 |
| 1) Shelter use after mainshock | 26.13 | 28.30 | 26.74 | 18.87 |
| 11.73 days | 13.72 days | 8.90 days | ||
| 1) Spend nights in their cars after mainshock | 47.46 | 54.55 | 47.07 | 43.40 |
| 5.17 days | 6.57 days | 5.91 days | ||
| 2) House damage | ||||
| No damage | 38.38 | 45.45 | 34.90 | 60.38 |
| Partially damaged | 43.60 | 30.91 | 46.53* | 32.08 |
| Half destroyed | 10.27 | 14.55 | 10.51 | 3.77 |
| Largely destroyed | 4.32 | 7.27 | 4.25 | 1.89 |
| Totally destroyed | 3.42 | 1.82 | 3.80 | 1.89 |
| 3) Lifelines | ||||
| Recovered within 1 week | 55.27 | 59.26 | 54.92 | 54.00 |
| Recovered in 1–2 weeks | 24.58 | 20.37 | 24.49 | 30.00 |
| Recovered in 2–4 weeks | 14.60 | 18.52 | 14.42 | 12.00 |
| Recovered more than 4 weeks | 5.55 | 1.85 | 6.18 | 4.00 |
| 4) Food supply | ||||
| As usual | 46.95 | 36.54 | 48.75 | 42.00 |
| Insufficient | 9.06 | 11.54 | 8.88 | 8.00 |
| Unbalanaced | 37.34 | 50.00 | 35.31 | 42.00 |
| NA | 6.65 | 1.92 | 7.06 | 8.00 |
| 5) Water supply | ||||
| Sufficient | 83.84 | 90.91 | 82.41 | 88.68 |
| Insufficient | 16.16 | 9.09 | 17.59 | 11.32 |
| 6) The amount of physical activity/exercise | ||||
| No change | 53.60 | 50.91 | 53.90 | 53.85 |
| Reduced | 36.69 | 34.55 | 37.42 | 32.69 |
| Increased | 9.71 | 14.55 | 8.69 | 13.46 |
| 7) The amount of sleep | ||||
| Sufficient | 23.15 | 12.73 | 24.66 | 21.15 |
| Fair enough | 35.80 | 32.73 | 34.75 | 48.08 |
| Not enough | 31.83 | 43.64 | 31.61 | 21.15 |
| Insomnia | 9.22 | 10.91 | 8.97 | 9.62 |
| 8) Changes in family environment | ||||
| Yes | 13.79 | 14.81 | 14.19 | 9.43 |
| No | 86.21 | 85.19 | 85.81 | 90.57 |
| 9) Changes in their working environment | ||||
| Yes | 18.25 | 18.87 | 18.01 | 19.61 |
| No | 81.75 | 81.13 | 79.95 | 80.39 |
| 10) Changes in a family member's working environment | ||||
| Yes | 16.11 | 9.09 | 17.78 | 9.62 |
| No | 83.89 | 90.91 | 82.22 | 90.38 |
| 11) Bereavement | 3.64 | 3.64 | 4.07 | 0.00 |
Data are expressed as ratio (%) unless otherwise indicated. *P = 0.037 vs type 1 diabetes. NA, not available, Others, specific types of diabetes due to other causes.
Evacuation
After the foreshock, 4.69% of the patients were evacuated to shelters nearby and 10.65% of those were staying in their cars at the time of the mainshock that occurred at 01.25 hours on 16 April. After the mainshock, the percentage of patients staying in shelters or spending nights in their cars became 26.14 and 47.46%, respectively. The average period of shelter use was 11.73 days for type 1 diabetes patients, 13.72 days for type 2 diabetes patients and 8.90 days for Others. The average period of time staying in their car was 5.17 days for type 1 diabetes patients, 6.57 days for type 2 diabetes patients and 5.19 days for Others.
House damage
More than 60% of the patients experienced house damage, ranging from partially damaged to totally destroyed. In particular, the ratio of ‘partially damaged’ for type 2 diabetes patients was significantly higher than that of type 1 diabetes patients (P = 0.037).
Lifelines
More than 50% of the patients experienced lifeline recovery within 1 week; however, 20% of the patients suffered from disruption of lifelines for >2 weeks.
Food supply during the first month after the earthquakes
More than 50% of the patients struggled to access the appropriate amount and right balance of food. In particular, unbalanced meals were observed in 37.34% (n = 202) of all patients.
Water supply
Approximately 20% of the patients experienced a shortage of water supply.
Amount of physical activity/exercise during the first month after the earthquakes
Approximately 50% of the patients reported that the amount of physical activity/exercise did not change. One‐third of the patients experienced a reduced amount of physical activity/exercise. These results were consistent with the data that the number of patients with type 1 diabetes who reduced their insulin doses (20.00%) was higher than those who increased their insulin doses (7.27%).
Amount of sleep during the first month after the earthquakes
Three‐quarters of the patients experienced some kind of sleep disturbance.
Changes in family environment
A total of 76 patients (13.8%) experienced changes in their family environment.
Changes in working environment
A total of 98 patients (18.2%) experienced changes in their working environment.
Changes in family members’ working environments
A total of 87 patients (16.11%) experienced changes in a family member's working environment.
Bereavement
A total of 20 patients (3.64%) experienced bereavement.
The results of the medical care management component of the questionnaire are shown in Table 3.
Table 3.
Results of self‐administered lifestyle associated questionnaire at 1 month after the earthquakes (medical care management)
| Total, % | Type 1 diabetes, % | Type 2 diabetes, % | Others, % | |
|---|---|---|---|---|
| 12) The insufficiency of antidiabetic agents | 5.60 | 7.27 | 5.09 | 8.16 |
| 13) Irregular visits to the hospital | 42.89 | 35.14 | 43.35 | 48.15 |
| 13) How many days prescriptions at 1st visit | 36.71 days | 42.96 days | 37.64 days | |
| 13) Prescriptions from other hospitals | 2.11 | 2.70 | 1.90 | 3.70 |
| 14) Glucose monitoring | ||||
| Lost personal SMBG device | 3.21 | 10.26 | 2.57 | 2.50 |
| Insufficiency of SMBG sensor | 5.56 | 15.38* | 4.11 | 10.00 |
| Insufficiency of SMBG lancet | 3.63 | 5.13 | 3.08 | 7.50 |
| Insufficiency of replenishing glucose | 2.14 | 10.26† | 1.29 | 2.50 |
| Insufficiency of cotton swab | 3.42 | 5.13 | 2.57 | 10.00 |
| Use of different SMBG device | 1.12 | 1.82 | 1.16 | 0.00 |
| Reductions in the frequency of glucose monitoring | 5.79 | 9.09 | 5.09 | 8.33 |
| Increases in the frequency of glucose monitoring | 2.43 | 7.27 | 2.08 | 0.00 |
| No glucose monitoring | 8.04 | 10.91 | 7.64 | 8.33 |
| Increased incidence of hypoglycemia | 2.62 | 7.27 | 2.08 | 2.08 |
| Decreased incidence of hypoglycemia | 1.50 | 7.27 | 0.93 | 0.00 |
| Reuse of insulin injection needles | 1.68 | 7.27‡ | 1.16 | 0.00 |
| Insulin dose reduction in insulin users | 3.55 | 20.00§ | 4.30 | 3.10 |
| Insulin dose increase in insulin users | 1.68 | 7.27 | 2.10 | 0.00 |
| 15) Remedy | ||||
| No alterarions | 89.34 | 75.93¶ , †† | 90.87 | 90.38 |
| Cessation on self‐judgment | 2.21 | 0.00 | 2.51 | 1.92 |
| Alterations on self‐judgment | 3.49 | 27.27¶ , †† | 0.68 | 1.92 |
| Alterations on consulting a doctor | 5.51 | 1.85 | 5.94 | 5.77 |
| Lost prescription record book (Okusuri‐techou) | 13.79 | 20.00 | 13.29 | 11.54 |
| 16) The acquisition of medical information | ||||
| Not obtained | 90.33 | 94.44 | 89.38 | 94.12 |
| Obtained | 9.67 | 5.56 | 10.62 | 5.88 |
| 16) The source of the medical information | ||||
| TV/radio | 69.52 | 74.07 | 67.90 | 78.43 |
| Newspapers | 31.78 | 27.78 | 31.18 | 41.18 |
| Cell phones (including e‐mail/SMS) | 20.63 | 31.48 | 20.09 | 13.73 |
| Personal computers | 12.83 | 20.37 | 11.78 | 13.73 |
| Japan Diabetes Society website | 0.37 | 0.00 | 0.23 | 1.96 |
| Medical consultant | 0.56 | 0.00 | 0.69 | 0.00 |
| Others | 9.48 | 9.26 | 9.24 | 11.76 |
Data are expressed as ratio (%) unless otherwise indicated. *P = 0.029 vs type 2 diabetes; † P = 0.016 vs type 2 diabetes; ‡ P = 0.04 vs type 2 diabetes; § P = 0.003 vs type 2 diabetes; ¶ P < 0.001 vs type 2 diabetes; †† P = 0.006 vs specific types of diabetes due to other causes (Others).
Insufficiency of antidiabetic agents
Just 5.6% of the patients complained of an insufficiency of antidiabetic agents. That insufficiency was mainly observed in central (7.0%) and eastern (12.2%) areas of Kumamoto City, but not in Mashiki Town (0%), where the epicenters were located. Just 2.11% of the patients (n = 8) were prescribed antidiabetic agents by other hospitals or at the shelters.
Visit
Regular visits to our hospital were disturbed in the chaotic situation, thus 42.9% of the patients changed their original appointment date, mostly extended. Just 1.9% of the patients with type 2 diabetes visited earlier than their scheduled appointment date.
Self‐monitoring of blood glucose
A total of 15 patients (3.2%) lost their personal self‐monitoring of blood glucose devices. Insufficiency of a glucose‐monitoring sensor was observed in 5.56% (n = 26) in total (15.38% in type 1 diabetes patients [n = 6], 4.11% in type 2 diabetes patients [n = 16] and 10.0% in Others [n = 4]), and was significantly higher in type 1 diabetes patients (P = 0.029) compared with type 2 diabetes patients. In contrast, a shortage of lancets for self‐monitoring of blood glucose was just 3.8% (n = 17) in total. Insufficiency of replenishing glucose was observed in 10.3% (n = 4) in type 1 diabetes patients, 1.3% (n = 5) in type 2 diabetes patients and 2.5% (n = 1) in Others, with a higher incidence in type 1 diabetes patients (P = 0.016). Increased incidence of hypoglycemia was observed in 2.62% of patients (n = 14), and decreased incidence of hypoglycemia was observed in 1.50% of patients (n = 8), without differences among the groups, showing that hypoglycemia was appropriately avoided in the majority of patients. The reuse of insulin injection needles was significantly higher in type 1 diabetes patients (7.27%, n = 4, P = 0.04) compared with that in type 2 diabetes patients (1.16%, n = 5).
When limited to the insulin users, the ratio of patients with type 1 diabetes who reduced their insulin dose was 20.0% (n = 11, P = 0.003 vs type 2 diabetes patients). In type 2 diabetes patients it was 4.3% (n = 6), and in Others it was 3.1% (n = 1). The ratio of patients who increased their insulin dose was 7.27% (n = 4, P = 0.29 vs type 2 diabetes patients) in patients with type 1 diabetes, 2.1% (n = 3) in patients with type 2 diabetes and 0% in Others. According to these results, insulin users with type 1 diabetes successfully managed to control their glycemic control by modulating insulin dosages according to their own judgment.
Remedy
Nearly 90% of the patients did not need to change their treatment regimen. A total of 76 patients (13.79%) lost their prescription record notebook (Okusuri‐techou).
Medical information
It is surprising that >90% of the patients were not able to obtain any kind of medical information at the time of the earthquakes. Medical information was provided mainly by TV/radio (69.52%). Patients with type 1 diabetes showed relatively higher rates of obtaining medical information through cell phones (including e‐mails and/or social network services) and/or personal computers.
IES‐R for post‐traumatic stress disorder scale and associated factors
The present research used the IES‐R) for measuring post‐traumatic stress disorder levels. IES‐R is a self‐administered questionnaire to score the extent of post‐traumatic stress disorder in a wide variety of disasters, identifying stress levels in cross‐sectional studies, observational follow up and screening10. The mean IES‐R score across all patients in the study was 11.75 (11.35 in type 1 diabetes patients, 12.11 in type 2 diabetes patients and 9.18 in Others), without differences among the types of diabetes. The scores were significantly higher in the central (mean 14.73, median 9.00, P < 0.001) and eastern (mean 13.66, median 9.50, P = 0.026) parts of Kumamoto City compared with those in other areas, apart from in Mashiki (mean 22.83, median 14.50, P = 1.00) where the epicenters were located.
Multiple regression analysis was carried out to identify the association between the severity of earthquake damage and IES‐R scores. IES‐R scores were positively correlated with age. IER‐S was negatively correlated with recovery of lifelines within 1 week or no suspension. The longer the recovery of lifelines, the higher the regression coefficient, indicating that the impact on IES‐R was associated with the recovery status of lifelines. IER‐S was also positively correlated with an increased amount of physical activity/exercise, and was negatively correlated with the amount of sleep. IES‐R score was also positively correlated with the location where the patients lived, especially for with those that lived in Mashiki.
The multiple regression analysis was again carried out in type 2 diabetes patients – the majority of the study population (449 / 557 = 80.6%) in this research. The IES‐R score was positively correlated with age. IER‐S was negatively correlated with recovery of lifelines within 1 week or no suspension. A longer lifeline recovery was associated with higher IES‐R scores. The insufficiency of antidiabetic agents was observed only in 5.6% of patients, but IES‐R score was positively correlated with this insufficiency. IER‐S was positively correlated with an increased amount of physical activity/exercise, and was negatively correlated with the amount of sleep.
Glycemic parameters and associated factors
In type 2 diabetes patients, HbA1c and GA first declined at 1–2 months after the earthquakes and increased thereafter (Figure 2). Therefore, multiple regression analysis was carried out to identify the association between the severity of earthquake damage and glycemic parameters in type 2 diabetes patients. At 1–2 months after the earthquakes, HbA1c levels were negatively correlated with lifeline recovery within 2 weeks and sufficient sleep. GA levels were negatively correlated with shelter life and alterations in remedy on consulting a doctor. At 3–4 months after the earthquakes, HbA1c and GA levels were positively correlated with the insufficiency of antidiabetic agents and insufficient food supply. At 6–7 months after the earthquakes, no significant factor was detected in the association of HbA1c levels. GA levels were positively correlated with largely destroyed house damage. At 12–13 months after the earthquakes, HbA1c levels were positively correlated with largely destroyed house damage, the insufficiency of antidiabetic agents and changes in working environment. Increased HbA1c was observed in the patients with type 2 diabetes who experienced largely and totally destroyed houses (+0.243%) compared with that in no damage (+0.044%) at 12–13 months after the earthquakes (P = 0.013). GA levels were positively correlated with largely destroyed house damage, insufficient food supply and changes in working environment.
Discussion
An observational study on glycemic control in patients with diabetes associated with the 2016 Kumamoto Earthquakes was carried out. In type 1 diabetes patients and Others, HbA1c and GA levels during the study period were unchanged. In type 2 diabetes patients, HbA1c levels first declined by 0.11% (from 7.33 to 7.22%) at 1–2 months after the earthquakes and increased thereafter. GA levels showed a similar trend in type 2 diabetes patients.
In Japan, a number of huge earthquakes struck around Kobe in 1995, Chuetsu in 2004 and Tohoku in 2011.
The Great Hanshin‐Awaji Earthquake occurred on 17 January 1995 in Kobe. The magnitude of the earthquake was 7.2, >6,200 people were killed, and 250,000 people lost their houses due to collapse and/or fire. HbA1c levels were aggravated in the Kobe area (+0.20%. M 7.2), but not in the Osaka area (−0.02%. M 4.2)3. Increased HbA1c and high scores for stress levels were evident in patients with diabetes who experienced severe damage to houses and/or whose relatives had been killed or injured3. Other research highlighted that HbA1c in patients with diabetes was elevated from 7.74 to 8.34% (+0.60%), and this was highly correlated with inappropriate diet6.
On 23 October 2004, a major M 6.8 earthquake struck the Chuetsu district of Niigata Prefecture, Japan. In this restricted area, HbA1c in patients with type 1 diabetes had deteriorated at 3 months after the shock (+0.3%), was highest at 5 months (+0.4%) and high HbA1c levels continued until 12 months (+0.3%)5.
In 2011, the Great East Japan Earthquake of M 9.0 struck the Tohoku area of Japan. The impact of the earthquake and subsequent Tsunami resulted in >15,000 casualties and 3,000 missing persons. Tohoku University reported that HbA1c in patients with diabetes was maintained at 1 month (7.3 vs 7.3%), but was significantly decreased at 3 months (−0.1%) after the earthquake8. In contrast, HbA1c in patients with type 1 diabetes became worse with +0.26% (7.81 vs 8.07%), indicating that patients with a lower insulin secretory capacity might be more vulnerable to stressful conditions4. Indeed, fasting C‐peptide levels were significantly lower in the patients with worsened glycemic control7.
In response to the Great East Japan Earthquake 2011, the Japan Diabetes Society published a book titled Diabetes Treatment Manual in the Situation of Disaster in 2014. In this text, it is recommended that a ‘DiaMAT: Diabetes Medical Assistance Team’ should be established in advance. Furthermore, the American Diabetes Association also emphasizes preparedness against disasters11.
However, we did not have such a team at the time of the 2016 Kumamoto earthquakes. Thus, 1 week after the earthquakes we formed a team, named the ‘KDAT: Kumamoto Diabetes medical Assistant Team’ with the cooperation of the Japan Diabetes Society, Japanese Association for Diabetes Education and Care, and Japan Council for Promotion of Countermeasures against Diabetes. For 5 weeks after its establishment, our KDAT team visited 14 shelters mainly in Mashiki, where the damage was the most severe. A total of 229 volunteers contributed to the KDAT activity and provided care for 664 people to help measure blood glucose and blood pressure, and consult on medical problems. We identified 226 people (34.0%) in the shelters who might have had diabetes according to the consultation and/or blood glucose levels. Our team also established a telephone consulting service immediately after the earthquakes. We dealt with 31 consultations over the phone and three e‐mails associated with glucose monitoring, antidiabetic agents, hypoglycemia and so on. The establishment of a DiaMAT and education of the team members in advance are definitely important for an early response to a disaster. In Table 3, >90% of the patients could not appropriately acquire medical information, which was unexpectedly high. There might be a limit to distributing information by a paper‐based medium. First‐line medical team‐led information delivery and push type or bi‐directional communicating applications on their smart phones should be considered.
Our investigation during the Kumamoto earthquake showed that glycemic control in patients with type 1 diabetes was stable; however, that in type 2 diabetes patients decreased by 0.11% at 1–2 months after the earthquake and increased thereafter.
The unaltered glycemic control in type 1 diabetes might be because 27.3% of patients changed their insulin doses based on self‐judgment (20.0% reduced and 7.3% increased). They have communities through social networking services with whom they can discuss insulin doses, food intakes, carbohydrate count and glucose monitoring. This might also have helped to maintain their glucose levels.
In patients with type 2 diabetes, glycemic control unexpectedly decreased at 1–2 months after the earthquakes. This reduction was negatively correlated with prompt recovery of lifelines and sufficient amount of sleep. These two components might contribute to emotional stability (anti‐anxiety) in patients with type 2 diabetes to survive at that time. Indeed, distress, anxiety and/or stress cause glycemic deterioration in patients with diabetes12. This deteriorative reaction can be explained by increased production of cortisol and/or catecholamine13. Insufficient or disturbed sleep and circadian misalignment might have a negative impact on glycemic control in patients with diabetes14.
After 3–4 months or longer, patients with type 2 diabetes showed worsened glycemic control. These deteriorations are positively correlated with the insufficiency of antidiabetic agents, insufficient food supply, largely destroyed houses and changes in working environment, which cannot be controlled by the patients themselves, but are directly associated with their mental and physical stress levels. This result also implies that the stress component during a severe disaster might be dependent on the time after it. Thus, glycemic control, associated factors and stress levels are altered in chronological order, and depend on the severity of the damage and changes in environment.
We propose that the immediate recovery of lifelines and ensuring a sufficient amount of sleep are important effectors to help control blood glucose levels in the early period after a disaster. In the medium term, making arrangements for antidiabetic agents and food supply have to be taken care of. In the long term, public administrations and/or workplaces should consider the situations of affected patients, and propose early counterplans for house reconstruction and/or keeping work environments stable to minimize their stress levels. These long‐term impact factors cannot be managed by patients with diabetes or medical caregivers alone, and have to be tackled by society as a whole. Therefore, it is important to provide a message that we have to take comprehensive care of patients with diabetes affected by a disaster. Post‐disaster diabetic medical care must consider these corresponding points in accordance with the time‐period.
Disclosure
The authors declare no conflict of interest.
Acknowledgments
The authors thank the staff from the Center for Clinical Research (Sonoko Ishihara, Megumi Tamura, Manami Sakurada, Megumi Sakamoto, Takako Tsuda) for their help with carrying out the research. We also thank Tokunori Ikeda, Jun Morinaga and Yoshinori Yamanouchi for helping to collect and assess the data. This research was supported by NPO Blue Circle 2050 (Cooperation No. 4330005009181).
J Diabetes Investig 2019; 10: 521–530
Clinical Trial Registry
University Medical Hospital Information Network
UMIN000024757
References
- 1. Kato A, Nakamura K, Hiyama Y. The 2016 Kumamoto earthquake sequence. Proc Jpn Acad Ser B Phys Biol Sci 2016; 92: 358–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sengul A, Ozer E, Salman S, et al Lessons learnt from influences of the Marmara earthquake on glycemic control and quality of life in people with type 1 diabetes. Endocr J 2004; 51: 407–414. [DOI] [PubMed] [Google Scholar]
- 3. Inui A, Kitaoka H, Majima M, et al Effect of the Kobe earthquake on stress and glycemic control in patients with diabetes mellitus. Arch Intern Med 1998; 158: 274–278. [DOI] [PubMed] [Google Scholar]
- 4. Kamimura M, Hakoda A, Kanno J, et al Glycemic control in type 1 diabetic patients following the Great East Japan Earthquake and Tsunami. J Jpn Diabetes Soc 2014; 57: 16–21 (Japanese). [Google Scholar]
- 5. Kamoi K, Tanaka M, Ikarashi T, et al Effect of the 2004 Mid Niigata Prefecture earthquake on glycemic control in type 1 diabetic patients. Diabetes Res Clin Pract 2006; 74: 141–147. [DOI] [PubMed] [Google Scholar]
- 6. Kirizuka K, Nishizaki H, Kohriyama K, et al Influences of The Great Hanshin‐Awaji Earthquake on glycemic control in diabetic patients. Diabetes Res Clin Pract 1997; 36: 193–196. [DOI] [PubMed] [Google Scholar]
- 7. Tanaka M, Imai J, Satoh M, et al Glycemic control in diabetic patients with impaired endogenous insulin secretory capacity is vulnerable after a natural disaster: study of Great East Japan Earthquake. Diabetes Care 2014; 37: e212–e213. [DOI] [PubMed] [Google Scholar]
- 8. Tanaka M, Imai J, Satoh M, et al Impacts of the Great East Japan Earthquake on diabetic patients. J Diabetes Investig 2015; 6: 577–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Takakura R, Himeno S, Kanayama Y, et al Follow‐up after the Hanshin‐Awaji earthquake: diverse influences on pneumonia, bronchial asthma, peptic ulcer and diabetes mellitus. Intern Med 1997; 36: 87–91. [DOI] [PubMed] [Google Scholar]
- 10. Asukai N, Kato H, Kawamura N, et al Reliability and validity of the Japanese‐language version of the impact of event scale‐revised (IES‐R‐J): four studies of different traumatic events. J Nerv Ment Dis 2002; 190: 175–182. [DOI] [PubMed] [Google Scholar]
- 11. Disaster Response Task Force . American Diabetes Association Statement on Emergency and Disaster Preparedness: a report of the disaster response task force. Diabetes Care 2007; 30: 2395–2398. [DOI] [PubMed] [Google Scholar]
- 12. Tsujii S, Hayashino Y, Ishii H, et al Diabetes distress, but not depressive symptoms, is associated with glycaemic control among Japanese patients with type 2 diabetes: Diabetes Distress and Care Registry at Tenri (DDCRT 1). Diabet Med 2012; 29: 1451–1455. [DOI] [PubMed] [Google Scholar]
- 13. Fukuda S, Morimoto K, Mure K, et al Effect of the Hanshin‐Awaji earthquake on posttraumatic stress, lifestyle changes, and cortisol levels of victims. Arch Environ Health 2000; 55: 121–125. [DOI] [PubMed] [Google Scholar]
- 14. McHill AW, Wright KP Jr. Role of sleep and circadian disruption on energy expenditure and in metabolic predisposition to human obesity and metabolic disease. Obes Rev 2017; 18(Suppl 1): 15–24. [DOI] [PubMed] [Google Scholar]


