Introduction
In the United States, breastfeeding initiation rates have risen to 80%.1 We report secular trends of breastfeeding initiation and duration by birth weight using nationally representative data from the National Health and Nutrition Examination Survey (NHANES).
Methods
The NHANES is a complex, stratified, multistage probability sample of the US civilian noninstitutionalized population, conducted by the National Center for Health Statistics, Centers for Disease Control and Prevention. The NHANES was approved by the National Center for Health Statistics Research Ethics Review Board.
Using data from 13,859 children ages 0 to 6 years who participated in the NHANES from 1999 to 2014, we constructed birth year cohorts (1997–2000, 2001–2004, 2005– 2008, and 2009–2012) and birth weight categories (<2500 g [low birth weight (LBW)], ≥2500 g). Birth weight and breastfeeding history (ever breastfed or received breast milk) were obtained by proxy interview, most commonly by a parent 2. The unweighted response rate ranged from 77% to 93% 3. Written parental consent was obtained for those younger than 18 years.
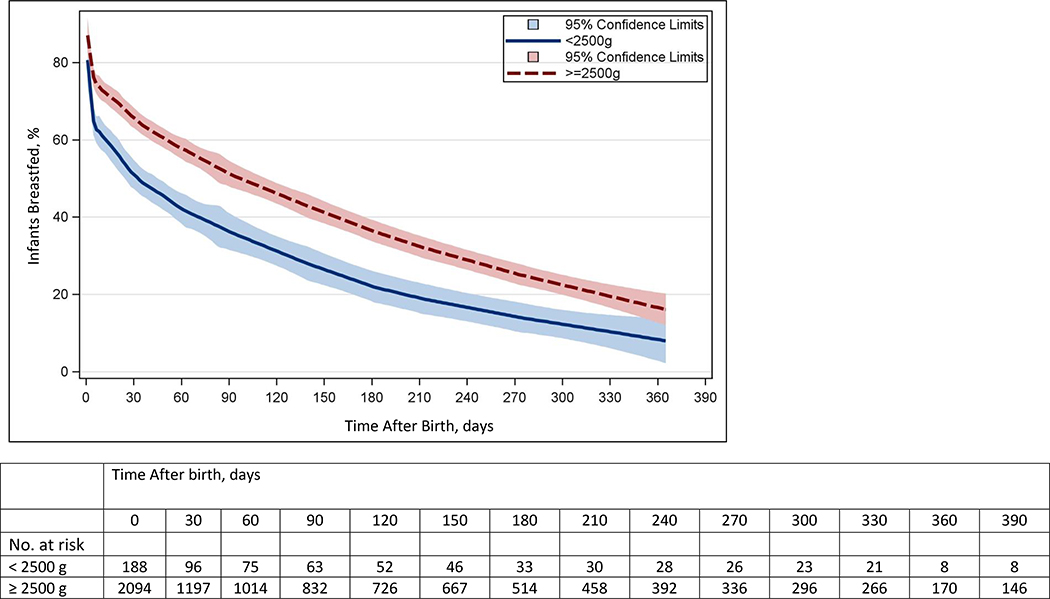
We estimated the proportion of infants ever breastfed (initiated) and those reporting any breastfeeding at 1 month, 4 months, and 6 months by birthweight categories and birth year cohorts. Infants were excluded if they had not attained the age at which breastfeeding was being estimated. Significance was set at α < .05 for adjusted Wald method and orthogonal contrast matrices for linear tests of trends over time. Taylor series linearization was used for variance estimation and 95%CIs were computed by the Wald method. Kaplan-Meier curves and log-rank tests assessed differences in the duration of breastfeeding by birth weight cohort from 2009 to 2012. LOESS smoothed curves and 95% CIs from Kaplan-Meier curves are presented. Infants were censored at the time of interview if they were currently receiving breast milk (12% of respondents, unweighted n = 324). Overall, 8%of infants were LBW (unweighted n = 1279). SAS version 9.3 (SAS Institute) and SUDAAN version 11.0 (RTI International) were used. Survey design variables and interview sample weights, which account for differential probabilities of selection, nonresponse, noncoverage, and sample design, were used to obtain estimates representative of the civilian noninstitutionalized US population.
Results
Among all infants, breastfeeding initiation rates increased from 65.7% (95% CI, 62.4%−69.1%) in 1997–2000 to 76.7% (95% CI, 73.5%−79.8%) (P < .001) in 2009–2012. Over the same period, breastfeeding initiation rates increased from 48.8% (95% CI, 39.6%−57.9%) to 65.4% (95% CI, 55.4%−75.3%) (P = .01) for LBW infants and from 67.4% (95% CI, 64.0%−70.8%) to 77.5% (95% CI, 74.3%−80.8%) (P < .001) for infants weighing 2500 g or more at birth (Table). An increasing secular trend in the percentage of infants still breastfeeding at 1 month (59.7% [95% CI, 56.2%- 63.2%] to 68.7% [95% CI, 65.0–72.4%]; P < .001), 4 months (42.6% [95% CI, 39.3%−46.0%] to 49.6% [95% CI, 45.6%- 53.7%]; P = .005), and 6 months (36.2% [95% CI, 33.0%- 39.5%] to 43.1% [95% CI, 39.3%−47.0%]; P = .002) was observed for infants weighing 2500 g or more. For LBW infants, the increase in the percentage still breastfeeding over time was not significant at any time after birth. This is likely owing to insufficient power arising from the small sample of LBW infants.
Table.
Proportion of Children Ever Breastfed and Breastfed for 1 Month, 4 Months, and 6 Months, by Birth Weight and Birth Year Cohorta
| Breastfeeding, % (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Breastfeeding Status | Total No. | 1997–2000 | 2001–2004 | 2005–2008 | 2009–2012 | P valueb |
| Ever Breastfed | ||||||
| No. | NA | 3480 | 4108 | 3989 | 2282 | NA |
| Total group | 13859 | 65.7 (62.4–69.1) | 67.7 (65.0–70.4) | 72.9 (70.8–75.1) | 76.7 (73.5–79.8) | <0.001 |
| <2500 g | 1279 | 48.8 (39.6–57.9) | 58.0 (49.0–67.0) | 59.5 (52.5–66.4) | 65.4 (55.4–75.3) | 0.01 |
| ≥2500 g | 12580 | 67.4 (64.0–70.8) | 68.6 (65.8–71.4) | 74.1 (72.0–76.2) | 77.5 (74.3–80.8) | <0.001 |
| P valuec | NA | <0.001 | 0.03 | <0.001 | 0.02 | NA |
| At 1 mo | ||||||
| No. | NA | 3444 | 4014 | 3913 | 2222 | NA |
| Total group | 13593 | 58.0 (54.5–61.5) | 58.8 (55.8–61.8) | 64.5 (61.8–67.1) | 67.6 (63.9–71.4) | <0.001 |
| <2500 g | 1276 | 41.1 (31.7–50.4) | 53.5 (44.5–62.6) | 50.4 (43.1–57.7) | 54.0 (45.6–62.3) | 0.07 |
| ≥2500 g | 12317 | 59.7 (56.2–63.2) | 59.2 (56.2–62.3) | 65.7 (62.9–68.4) | 68.7 (65.0–72.4) | <0.001 |
| P valuec | NA | <0.001 | 0.22 | <0.001 | <0.001 | NA |
| At 4 mo | ||||||
| No. | NA | 3300 | 3784 | 3651 | 2009 | NA |
| Total group | 12744 | 41.0 (37.8–44.2) | 42.4 (39.1–45.7) | 46.0 (43.4–48.5) | 48.6 (44.6–52.7) | 0.002 |
| <2500 g | 1199 | 24.6 (17.6–31.5) | 32.5 (24.3–40.7) | 34.8 (27.2–42.3) | 36.1 (26.0–46.2) | 0.05 |
| ≥2500 g | 11545 | 42.6 (39.3–46.0) | 43.3 (39.8–46.8) | 46.9 (44.2–49.6) | 49.6 (45.6–53.7) | 0.005 |
| P valuec | NA | <0.001 | 0.02 | 0.003 | 0.006 | NA |
| At 6 mo | ||||||
| No. | NA | 3186 | 3602 | 3492 | 1867 | NA |
| Total group | 12147 | 34.8 (31.7–37.8) | 34.8 (31.9–37.8) | 40.0 (37.6–42.4) | 42.0 (38.1–45.8) | 0.001 |
| <2500 g | 1150 | 19.7 (13.7–25.8) | 26.6 (18.6–34.6) | 27.5 (20.5–34.5) | 27.7 (18.2–37.2) | 0.16 |
| ≥2500 g | 10997 | 36.2 (33.0–39.5) | 35.6(32.4–38.8) | 41.1 (38.5–43.7) | 43.1 (39.3–47.0) | 0.002 |
| P valuec | NA | <0.001 | 0.04 | <0.001 | <0.001 | NA |
Abbreviations: NA, not applicable.
Data are derived from the National Health and Nutrition Examination Survey, 1999–2014 for birth cohorts above. Birth cohorts 1993–1996 and 2013–2014 are excluded from analysis because the sample sizes did not produce reliable estimates. Sample sizes are unweighted and prevalence estimates are weighted.
Linear test for trend from 1997–2000 to 2009–2012.
Differences between infants <2500 g and infants 2500 g or more were tested using a t statistic with the appropriate df at the P < 0.05 significance level
Within each birth cohort, the percentage of infants initiating breastfeeding and breastfeeding at 1, 4, and 6 months was significantly smaller for LBW infants compared with their heavier counterparts. For example, in 2009–2012, 43.1% of infants (95% CI, 39.3%−47.0%) weighing 2500 g or more were breastfeeding at 6 months compared with 27.7% of LBW infants (95%CI, 18.2%−37.2%) (P < .001). The only exception was among those still breastfeeding at 1 month in 2001–2004; this difference was not statistically significant.
The Figure presents the smoothed Kaplan-Meier curves for the overall duration of breastfeeding in the first year of life by birth weight categories. Infants who never breastfed were censored at time zero. Among infants born in 2009–2012, LBW infants had a 38% (95% CI, 1.17–1.63) increased hazard of discontinuing breastfeeding compared with infants weighing 2500 g or more (P < .001).
Figure:
Kaplan-Meier Curves for Duration of Breastfeeding by Birth Weight
NOTE: Data derived from the National Health and Nutrition Examination Survey2 birth cohort 2009–2012. Estimates derived from PROC KAPLANMEIER and plotted using LOESS. The number at risk is calculated from unweighted data and is therefore not directly comparable with the smoothed LOESS values in the plot.
Discussion
Although breastfeeding rates have increased over the past 2 decades, the percentage of LBW infants ever breastfed and continuing to breastfeed was lower than infants weighing 2500 g or more. These baseline estimates may be used to track current and future public health efforts.
Acknowledgments
Funding Source: This work was performed under employment of the U.S. Federal government and the authors did not receive any outside funding.
Abbreviations:
- NHANES
National Health and Nutrition Examination Survey
- NCHS
National Center for Health Statistics
Footnotes
Disclaimer: The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the National Center for Health Statistics, Centers for Disease Control and Prevention.
Financial Disclosure: The Authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The Authors have no conflicts of interest to disclose.
References
- 1.CDC. Breastfeeding among U.S. children born 2000–2012, CDC National Immunization Survey. Vol 2015 Atlanta, GA: US Department of Health and Human Services, CDC; 2015. [Google Scholar]
- 2.National Center for Health Statistics. National Health and Nutrition Examination Survey: NHANES 2013–2014 Questionnaire Data. http://wwwn.cdc.gov/Nchs/Nhanes/Search/DataPage.aspx?Component=Questionnaire&CycleBeginYear=2013. Accessed Oct 21, 2015.
- 3.National Center for Health Statistics. National Health and Nutrition Examination Survey: NHANES response rates and CPS totals. www.cdc.gov/nchs/nhanes/response_rates_CPS.htm. Accessed Oct 21, 2015.