Abstract
Experimental and computational studies were performed to elucidate the role of turbulent stresses in mechanical blood damage (hemolysis). A suspension of bovine red blood cells (RBC) was driven through a closed circulating loop by a centrifugal pump. A small capillary tube (inner diameter 1 mm and length 70 mm) was incorporated into the circulating loop via tapered connectors. The suspension of RBCs was diluted with saline to achieve an asymptotic apparent viscosity of 2.0±0.1 cP at 23°C to produce turbulent flow at nominal flow rate and pressure. To study laminar flow at the identical wall shear stresses in the same capillary tube, the apparent viscosity of the RBC suspension was increased to 6.3±0.1 cP (at 23°C) by addition of Dextran-40. Using various combinations of driving pressure and Dextran-mediated adjustments in dynamic viscosity Reynolds numbers ranging from 300 to 5000 were generated, and rates of hemolysis were measured. Pilot studies were performed to verify that the suspension media did not affect mechanical fragility of the RBCs. The results of these bench studies demonstrated that at the same wall shear stress in a capillary tube, the level of hemolysis was significantly greater (p < 0.05) for turbulent flow as compared to laminar flow. This confirmed that turbulent stresses contribute strongly to blood mechanical trauma. Numerical predictions of hemolysis obtained by computational fluid dynamic modeling were in good agreement with these experimental data.
Introduction
The identification of mechanisms of shear-induced blood trauma is essential for all blood-contacting artificial organ design. Numerous investigations over the past several decades have sought to identify the critical shear stress and exposure time related to the produced hemolysis (complete destruction of a fraction of the RBCs in the samples studied). This research has resulted in an assortment of hemolysis thresholds for a variety of experimental setups (1–10). However, the mechanisms of shear blood damage are varied and are not completely identified. Many other parameters in addition to shear stress magnitude and exposure time are relevant to trauma: such as shear exposure history (11), temperature (hypothermia or hyperthermia) (12–13), the concentrations of RBCs and plasma components (14–15), and others. One of the least studied factors is the contribution of turbulence stresses to hemolysis. While blood flow in the human vascular system is mostly laminar, the use of cardiovascular devices frequently introduces significantly disturbed and/or turbulent flows. To date, most of the hemolysis studies examining turbulence involve the use of high velocity turbulent jets in vitro (1, 4, 5). Unfortunately these experiments cannot provide a well-defined shear field. Therefore the relative contribution of turbulent intensity remains poorly characterized.
This paper presents a relatively simple experimental design that independently prescribes the level of shear and turbulence within a capillary tube. Accordingly, it has provided comparative studies of hemolysis in laminar and turbulent flows at the same wall shear stresses and for the same exposure time.
Commensurate computational fluid dynamic analysis is also presented to demonstrate the benefit of incorporating turbulence into a predictive model of hemolysis.
Materials and methods.
Experimental fluids
The fluid media consisted of a suspension of washed bovine red blood cells in saline or 10% dextran solution (Dextran-40, Sigma Chemical Co., St. Louis, MO). Bovine blood obtained from a local slaughterhouse was collected into plastic bags with 10% sodium citrate. Blood was filtered through a sterile non-pyrogenic 40 μm filter (Microaggregate Blood Transfusion Filter, Pall Biomedical, Inc.). Then blood was centrifuged (CR 4–12 Centrifuge, Jouan, Inc., Winchester Virginia) at 3600 rpm for 15 minutes and the plasma and buffy coat containing leukocytes and platelets were aspirated and discarded. RBCs were resuspended in four volumes of standard phosphate buffered saline (PBS, 0.01 M phosphate buffer, 0.0027 M potassium chloride and 0.0137 M sodium chloride, pH 7.4, 290 mOsm/kg, Sigma Chemical Co., St. Louis, Missouri), mixed and centrifuged again. The supernatant was discarded and this procedure was repeated three times. The washed RBCs were resuspended in saline or 10% dextran solution. The hematocrit, measured in a microhematocrit centrifuge (Clay Adams), was adjusted to a standard value of Ht=24.0 ± 0.5%. Gentamicin sulfate (Elkins-Sinn, 40 mg/ml solution, appx. 0.25 ml per 100 ml) was added to the suspension to prevent bacterial growth. The viscosity of the suspension was measured at room temperature (23°C) by a capillary viscometer (Cannon Instrument Company, P.O. Box 16 State College, PA) at the shear rate of about 500 sec−1. Plasma free hemoglobin concentration was measured by spectrophotometer (Spectronic® GENESYSTM5, Spectronic Instruments, Inc., Rochester, NY).
Experimental design and protocol
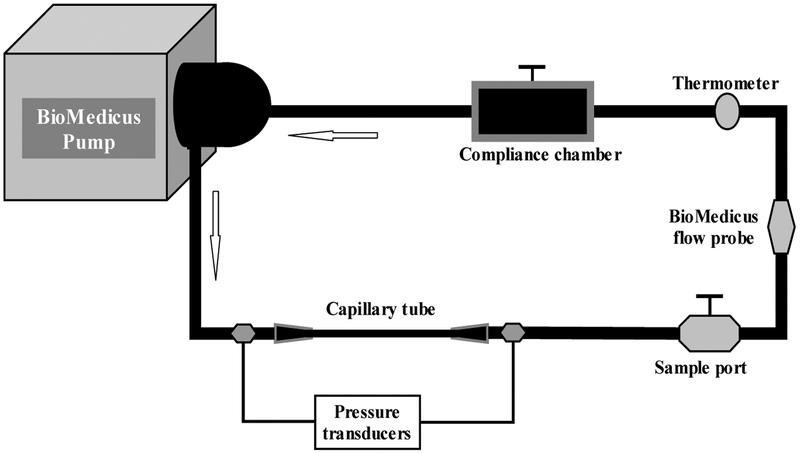
Blood was driven through a closed circulating loop consisting of a centrifugal pump (Bio-Medicus, BP-80), PVC tubing (Tygon), a water bath, a collapsible reservoir and small-caliber glass capillary tube (1 mm diameter, 70 mm length) (Figure 1). The capillary tube was fitted at each end with conically shaped connectors (8 mm length) to minimize entrance and exit effects (Figure 2). A capillary tube was chosen for several reasons: 1) ease of fabrication; 2) reduction of priming volume; and 3) ease of producing a wide range of Reynolds numbers (from laminar to turbulent).
Figure 1.
Schematic of the test-circulating loop.
Figure 2.
Solid model of capillary tube for CFD analysis. The test segment is 1 mm diameter and 70 mm length and is fitted at each end with conically shaped connectors 8 mm length.).
The loop was instrumented with a temperature probe and two Statham type pressure transducers, and flow probe. The temperature was maintained constant by immersing the entire circulating loop within a heated water bath. The differential pressure across the capillary was used to determine the wall shear rate according to the force balance approximated with equation (1):
| (1) |
Here R and L are the radius and length of the capillary tube. This approximation assumes negligible contribution of the connectors to the pressure (see justification below). The flow rate was determined by an in-line ultrasonic flow probe (Transonics, Ithaca, NY).
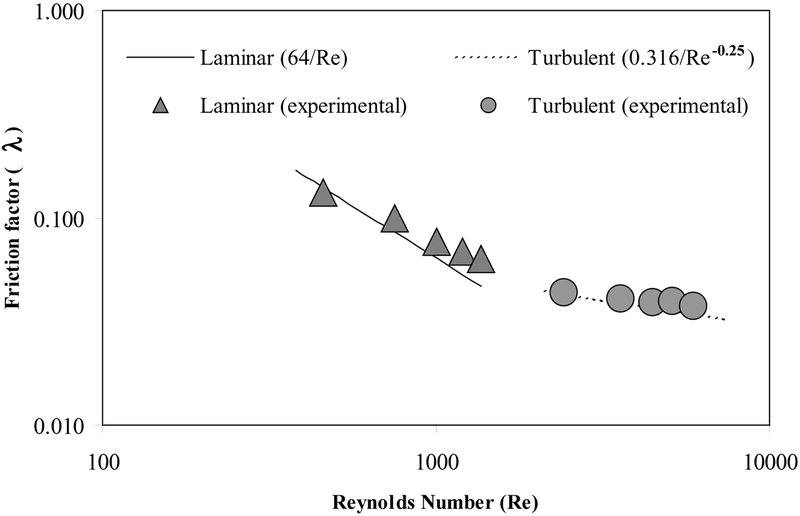
RBC suspensions in saline with viscosity of 2.0±0.1 cP at room temperature of 23°C were used to study transitional and turbulent flow over a range of Reynolds numbers from 2200 to 5100 and wall shear stresses from 100 to 400 Pa (corresponding flow rates from 0.21 to 0.48 L/min). To provide laminar flow at the same range of wall shear stresses in the capillary tube, RBCs were suspended in 10% Dextran-40 solution at the same hematocrit with the resulting viscosity of 6.3±0.1 cP at 23°C. The resulting range of Reynolds numbers for the flow of these suspensions was from 300 to 1300 at the wall shear stresses from 100 to 400 Pa (corresponding to flow rates from 0.09 to 0.29 L/min). To confirm the existence of laminar and turbulent flow, the pipe friction factor (λ) was calculated from the experimental data for both suspension media and compared with the theoretical friction factor for laminar flow
| (2) |
and Blasius friction factor for turbulent flow
| (3) |
Figure 3 shows theoretical and experimental friction factors (λ) plotted versus Reynolds number (Re) over the full range studied. These data demonstrate that, the flow characteristics obtained in this circulation system closely approximate the ideal laminar and turbulent conditions except for the slight increase in λlam within the transitional range (Re =1000–2000).
Figure 3.
Friction factor values obtained in our circulating system for both laminar and turbulent flows compared to theoretical values
A 250 ml sample of RBC suspension was used for each test, which were performed for 90 min. Blood samples were withdrawn every 30 min for measurement of plasma free hemoglobin as indicator of hemolysis. The tests were repeated from 6 to 12 times for each shear stress.
In separate pilot experiments, the mechanical fragility of RBCs suspended in each of the suspension media was measured by using a standard fragility test described previously (16). Briefly, 3 cc of each RBC suspension were placed into identical vacutainers with five 1/8” diameter stainless steel shot added. The vacutainers were agitated on a standard rocker (Thermolyne Speci-Mix, Barnstead/Thermolyne, Dubuque, IA). Liberated plasma free hemoglobin was determined after one hour of rocking and compared with control samples of the same suspensions which were not rocked. These tests were performed to verify that the Dextran does not affect mechanical fragility of RBCs.
Additional pilot studies were performed to evaluate the hemolytic properties of the pump and tubing. RBC suspensions in each of the applied media were driven through the circulating system consisting of the pump and tubing, but without the capillary tube. These studies were conducted at the highest flow rates and highest Re specified by our experimental protocols above.
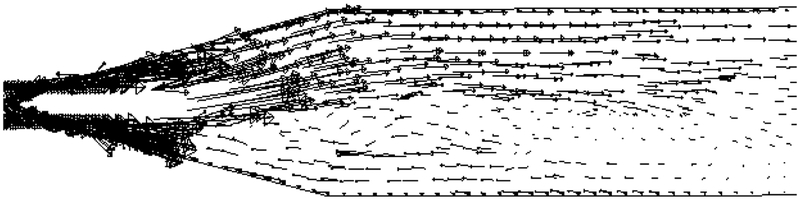
Computational analysis
Computational fluid dynamics (CFD) analyses were performed on the flow field within the capillary tube for all conditions presented above. For the simulation of the turbulent cases, the Reynolds-averaged Navier-Stokes equations were solved for turbulent incompressible flow using a two-equation k-epsilon model for turbulence closure The simulations were preformed using commercial software, CFX 5.3 (AEA Technologies, Inc, Waterloo, Ontario) and Fluent 5.0.4 (Fluent, Inc., Lebanon, NH) on an anisotropic hybrid mesh consisting of 17000 nodes and 41500 cells. These commercial CFD software packages were used to predict detailed fluid dynamics of the capillary tube. Two CFD packages were used in order to resolve the noted pressure drop anomalies (see below). However, both packages predicted similar pressure drop trends. Being available, both sets of CFD results were used to predict hemolysis generation. Blood was modeled as a single-phase homogeneous Newtonian fluid. The assumption of Newtonian behavior of blood was appropriate since shear rates in our test capillary tube were much higher than 500 s−1. Despite the axisymmetry of the capillary tube, a full three-dimensional CFD analysis of the tube was required due to the presence of Coanda flow in the diverging tube outlet. Figure 4 shows an example of a cross-section of the simulated velocity field in the outlet section with the majority of the flow preferentially attached to one side. This flow pattern did not oscillate spatially, but was stable in time.
Figure 4.
A cross-section of the velocity vector field in the diverging outlet section of the capillary tube. Some centerline vectors have been graphically clipped out for clarity purposes.
Using fluid viscosities identical to the experimental measurements, the initial CFD analysis demonstrated a systematic over prediction of the pressure drop for the laminar flows and systematically under-prediction for the turbulent flows. To remedy this, the numerical values of fluid dynamic viscosities were scaled consistent with classical Poiseuille pipe flow relationships to match the measured pressure drops. In particular, the experimental pressure drops were successfully matched by adjusting the numerical fluid viscosity consistent with the equation:
| (4) |
The velocity field and hence the strain rates were not modified. Consequently, the predicted shear stresses were scaled in proportion to the required viscosity adjustment.
A new numerical model of hemolysis (Optimal 1.0, Optimal LLC, Starkville, MS) was coupled with CFD to predict hemolysis generation in the capillary tube. This hemolysis model is based on Lagrangian-Eulerian formulation of cell damage and is unique from the models described in (10, 11, 17 and 18. Shear stress and time exposure are utilized to determine cell lysis probability using a non-linear damage function. Cumulative cell lysis is determined by integration of the cellular damage function over time and space.
Statistical analysis
A two-tailed Student t test for unpaired observations and a two-way analysis of variance (two-way ANOVA) were applied to determine the statistical significance of differences in plasma free hemoglobin obtained in the RBC suspensions exposed to laminar versus turbulent flows at each of the wall shear stress level studied. The data shown in the figures represent mean values ± standard deviation. A value of p < 0.05 was assumed to indicate statistical significance.
Results
No statistically significant difference was found in mechanical fragility of RBCs suspended in either PBS or Dextran-40 medium (Figure 5). Furthermore, the circulating system -- consisting of the pump and tubing, but without the capillary tube -- produced no considerable hemolysis after 90 min of circulating either RBC suspension at all flow conditions applied in the pilot studies specified above. It is worth to note that the flow in the circulating system without capillary tube was never turbulent even at the highest flow rates studied in the system with the capillary tube (Re<1000).
Figure 5.
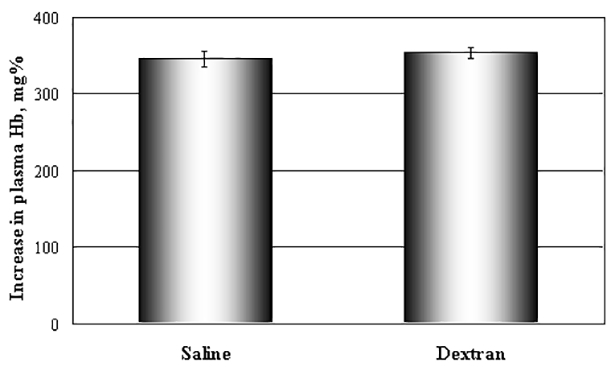
Mechanical fragility of RBCs suspended in either PBS or Dextran-40 medium
Comparison of the pipe friction factors calculated using formulas 2 and 3 and derived from the experimental results confirmed that the contribution of the collector and diffuser to the overall pressure drop of the capillary was negligible: both for laminar (p=0.63) and turbulent (p=0.52) cases.
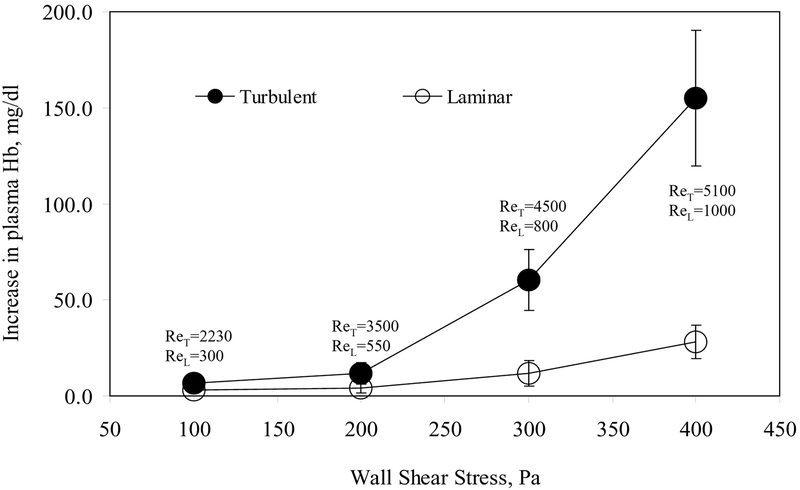
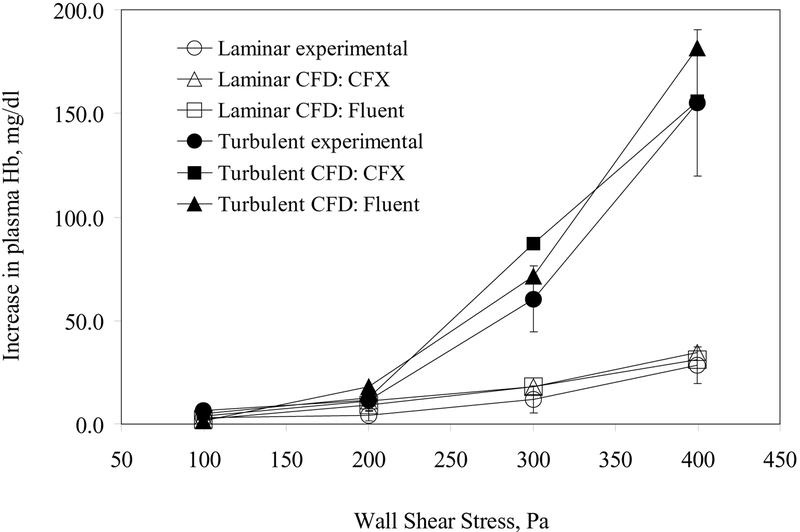
When the capillary tube was present, the hemolysis was found to have linear dependence on time at each shear stress for both laminar and turbulent flow conditions throughout the duration of the experiment. Figure 6 shows experimentally measured hemolysis levels for the RBC suspensions exposed to elevated shear under both laminar and turbulent conditions (see the corresponding Reynolds numbers). The data are presented as mean +/− standard deviation (n=6–12) for each level of wall shear stress. The results demonstrated that the presence of turbulence caused significantly greater hemolysis for the levels of the wall shear stress τw = 200–400 Pa (p<0.05). For both dextran and saline suspensions, hemolysis levels obtained at the laminar (Re = 300) or transitional (Re = 2200) flow conditions corresponding to the lowest wall shear stress (100 Pa) were however not significantly different (p=0.08).
Figure 6.
Increase in plasma free hemoglobin (hemolysis) vs. wall shear stress obtained for the laminar and turbulent flow experiments. Data presented as Mean ± Standard Deviation.
The results of hemolysis prediction with the CFD modeling at these experimental conditions were in good agreement with the measurements reported above (Figure 7). With the viscosity corrections described previously, both CFX and Fluent CFD analyses provided sufficiently accurate flow fields from which numerical hemolysis models could predict these in vitro hemolysis measurements, particularly the relative contribution of turbulence.
Figure 7.
Increase in plasma free hemoglobin vs. wall shear stress: experimental (one test) vs. CFD predictions.
Discussion
Blood trauma has been recognized as one of the major problems of assisted circulation. In fact, the main requirement for improved existing heart-assist devices for destination therapy is the reduction of blood cell damage. The origin of RBC trauma within heart-assist devices and other blood contacting artificial organs may be heterogeneous. Prolonged contact and collision between blood cells and foreign surfaces in regions of flow stasis, cavitation, extremely high shear forces, and elevated Reynolds shear stresses may induce a variety of damage mechanisms: complete mechanical destruction of some erythrocytes (hemolysis), activation of platelets and leukocytes, increased concentrations of inflammatory mediators, complement activation, and unfavorable changes in mechanical properties of erythrocytes (9–10, 19–22). The corresponding clinical complications may include anemia, fatigue, jaundice, hematuria, kidney failure among many others. Mechanical hemolysis can cause hypercoagulation, bleeding, thromboembolism, renal damage, and neurologic dysfunctions (stroke, altered mental status, etc.). By the end of the 19th century, it was already established that hemolysis induces hypercoagulation and intravascular thrombosis (23). Even low levels of hemolysis drastically increase red blood cell aggregation at low shear conditions (24). Additionally, plasma free hemoglobin released from destroyed or overstretched red blood cells may have a detrimental effect on the cardiovascular system producing a strong vasoconstriction due to its ability to bind nitric oxide, an endothelium-derived relaxation factor.
Although heart-assist devices have been in existence for several decades, their designs have been highly reliant upon empirical methods. Modern computational fluid dynamic analysis has the potential to dramatically improve the efficiency and accuracy of the hemodynamic design of these devices (17, 25, 26), provided that the underlying models faithfully represent the physical phenomena. However a comprehensive model for predicting blood damage remains confounded by the uncertain synergistic effect of turbulence. Qian (27–29) and others (1, 4, 5, 30–39) suggested that bulk turbulent stresses may play a more important role than laminar wall shear stresses in mediating hemolysis. However, none of the prior studies has directly compared red blood cell trauma due to turbulent versus laminar stresses in the same flow system at the same wall shear stresses (pressure drop) and at the same exposure time.
Herein was presented a controlled experimental and theoretical study designed to address this ambiguity by maintaining all key independent variables constant with the exception of turbulent intensity. We have demonstrated that the turbulent stresses contribute strongly to blood trauma generating exponential increases of hemolysis at higher Reynolds numbers in turbulent flows. The underlying mechanisms of turbulence-induced trauma are not clear. We may postulate that localized stretching of the RBC’s may be induced by interaction of small (Kolmogorov scale) turbulent eddies. It is also possible that cyclical stretching of the cell membrane may result in fatigue fracture. This is clearly a topic for further investigation.
The data generated from this research contributes to the underlying criteria for design of cardiovascular devices. These data may be used to reduce blood trauma in existing mechanical circulatory devices by correction of hemorheological parameters or flow conditions causing turbulence.
References
- 1.Bernstein EF, Blackshear PL Jr., Keller KH. Factors influencing erythrocyte destruction in artificial organs. Am J Surg 114:126–138, 1967. [DOI] [PubMed] [Google Scholar]
- 2.Indeglia RA, Shea MA, Varco RL, Bernstain EF. Mechanical and biologic considerations in erythrocyte damage. Surgery 62(1):47–55, 1967. [Google Scholar]
- 3.Nevaril CG, Lynch EC, Alfrey CP, Hellums JD. Erythrocyte damage and destruction induced by shearing stress. J Lab & Clin Med 71(5):784–790, 1968. [PubMed] [Google Scholar]
- 4.Leverett LB, Hellums JD, Alfrey CP, Lynch EC. Red blood cell damage by shear stress. Biophysical Journal 12:257–273, 1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blackshear PL. Mechanical hemolysis in flowing blood In: Biomechanics: Its Foundation and Objectives. Edited by Fung YC et al. Englewood Cliffs, N.J., Prentice-Hall, 1972, pp.501–528. [Google Scholar]
- 6.Richardson E. Deformation and Haemolysis in Shear Flow. Proc R Soc Lond A338:129–153, 1974. [Google Scholar]
- 7.Sutera SP. Flow induced trauma to blood cells. Circulation Research 41:2–8, 1977. [DOI] [PubMed] [Google Scholar]
- 8.Blackshear PL and Blackshear GL. Mechanical Hemolysis. In: Handbook of Bioengineering. Edited by Skalak R and Chien S. McGraw-Hill Book Company, 1986, pp.15.1–15.19. [Google Scholar]
- 9.Wurzinger LJ, Opitz R, Eckstein H. Mechanical blood trauma. An overview. Angiology 38:81–97, 1986 [Google Scholar]
- 10.Giersiepen M, Wurzinger LJ, Opitz R, Reul H. Estimation of shear stress-related blood damage in heart valve prostheses - in vitro comparison of 25 aortic valves. Intl J Artificial Organs 13(5):300–306, 1990. [PubMed] [Google Scholar]
- 11.Yeleswarapu KK, Antaki JF, Kameneva MV, and Rajagopal KR. A mathematical model for shear-induced hemolysis. Artificial Organs 19(7):576–582, 1995. [DOI] [PubMed] [Google Scholar]
- 12.Utoh J, and Harasaki H. Damage to erythrocytes from long-term heat stress. Clinical Science 82(1):9–11, 1992. [DOI] [PubMed] [Google Scholar]
- 13.Kameneva MV, Ündar A, Antaki JF, Watach MJ, Calhoon JH, Borovetz HS Decrease in red blood cell deformability due to effects of hypothermia, hemodilution, and mechanical stress - factors related to cardiopulmonary bypass (CPB). ASAIO Journal 45(4):307–310, 1999. [DOI] [PubMed] [Google Scholar]
- 14.Kameneva MV, Antaki JF, Yeleswarapu KK, Watach MJ, and Borovetz HS. Plasma protective effect on red blood cells exposed to mechanical stress. ASAIO Journal 43:M571–M575, 1997. [PubMed] [Google Scholar]
- 15.Müeller MR, Schima H, Engelhardt H, Salat A, Olsen DB, Losert U, and Wolner E. Thoughts and Progress. In Vitro Hematological Testing of Rotary Blood Pumps: Remarks on Standardization and Data Interpretation. Artificial Organs 17:103–110, 1993. [DOI] [PubMed] [Google Scholar]
- 16.Kameneva MV, Watach MJ, Litwak P, Antaki JF, Butler KC, Thomas D, Taylor LP, Borovetz HS, Kormos RL, and Griffith BP. Chronic animal health assessment during axial ventricular assistance: importance of hemorheological parameters. ASAIO Journal 45(3):183–188, 1999. [DOI] [PubMed] [Google Scholar]
- 17.Bludszuweit C Three-dimensional numerical prediction of stress loading of blood particles in a centrifugal pump. Artificial Organs 19(7):590–6, 1995 [DOI] [PubMed] [Google Scholar]
- 18.Fourgeault P, Garon A, Kempenaars, and Mongrain R “Computation of hyperbolic equations for hemolysis rate using finite differences.” Proceedings of 8th Conference of CFD Society, Paper #38, June 2000. [Google Scholar]
- 19.Kormos RL. Borovetz HS. Griffith BP. Hung TC. Rheologic abnormalities in patients with the Jarvik-7 total artificial heart. ASAIO Transactions. 33(3):413–7, 1987. [PubMed] [Google Scholar]
- 20.Borovetz HS. Kormos RL. Griffith BP. Hung TC. Clinical utilization of the artificial heart. Critical Reviews in Biomedical Engineering. 17(2):179–201, 1989. [PubMed] [Google Scholar]
- 21.Hung TC. Butter DB. Yie CL. Kormos RL. Borovetz HS. Griffith BP. Hardesty RL. Effects of long-term Novacor artificial heart support on blood rheology. ASAIO Transactions. 37(3):M312–3, 1991. [PubMed] [Google Scholar]
- 22.Hung TC. Borovetz HS. Kormos RL. Butter DB. Yie CL. Pristas JM. Griffith BP. Hardesty RL. Artificial heart. Hemorrheology and transient ischemic attacks. ASAIO Transactions. 36(3):M132–5, 1990. [PubMed] [Google Scholar]
- 23.Schmidt AA. Zur Blutlehre Leipzig, 1892, p.270. [Google Scholar]
- 24.Seiyama A, Suzuki Y, Tateshi N, and Maeda N. Viscous properties of partially hemolyzed erythrocyte suspension. Biorheology 28:452, 1991. [Google Scholar]
- 25.Antaki JF, Ghattas O, Burgreen GW, He B. Computational flow optimization in rotary blood pump components. Artificial Organs 19(7):608–615, 1995. [DOI] [PubMed] [Google Scholar]
- 26.Burgreen GW, Antaki JF, Wu ZJ, Holmes JA. Computational fluid dynamics as a design tool for rotary blood pumps. Artificial Organs 25(5):336–340, 2001. [DOI] [PubMed] [Google Scholar]
- 27.Qian KX. Haemodynamic approach to reducing thrombosis and haemolysis in an impeller pump. Journal of Biomedical Engineering 12(6):533–5, 1990. [DOI] [PubMed] [Google Scholar]
- 28.Qian KX. New investigations of a pulsatile impeller blood pump. ASAIO Transactions. 36(1):33–5, 1990. [PubMed] [Google Scholar]
- 29.Qian KX, Zeng P, Ru WM, Yuan HY, Feng ZG, Li I. How to produce a pulsatile flow with low haemolysis? Journal of Medical Engineering & Technology 24(5):227–9, 2000. [DOI] [PubMed] [Google Scholar]
- 30.Sallam AM and Hwang NHC. Human red blood cell hemolysis in a turbulent shear flow: contribution of Reynolds shear stress. Biorheology 21:783–797, 1984. [DOI] [PubMed] [Google Scholar]
- 31.Nakahara T and Yoshida F. Mechanical effects on rates of hemolysis. Journal of Biomedical Materials Research 20(3):363–74, 1986 [DOI] [PubMed] [Google Scholar]
- 32.Jones SA. A relationship between Reynolds stresses and viscous dissipation: implications to red cell damage. Annals of Biomedical Engineering 23(1):21–8, 1995 [DOI] [PubMed] [Google Scholar]
- 33.Tamagawa M, Akamatsu T, Saitoh K. Department of Mechanical Engineering, Kyoto University, Japan. Prediction of hemolysis in turbulent shear orifice flow. Artificial Organs 20(6):553–9, 1996 [PubMed] [Google Scholar]
- 34.Grigioni M, Daniele C, D’Avenio G, Barbaro V. A discussion on the threshold limit for hemolysis related to Reynolds shear stress. Journal of Biomechanics 32(10):1107–12, 1999 [DOI] [PubMed] [Google Scholar]
- 35.Grigioni M, Daniele C, D’Avenio G, Barbaro V. Monodimensional estimation of maximum Reynolds shear stress in the downstream flow field of bileaflet valves. Journal of Heart Valve Disease 11(3):392–401, 2002. [PubMed] [Google Scholar]
- 36.Akutsu T, and Modi VJ. Unsteady fluid dynamics of several mechanical prosthetic heart valves using a two component laser Doppler anemometer system. Artificial Organs 21(10):1110–20, 1997 [DOI] [PubMed] [Google Scholar]
- 37.Baldwin JT. Deutsch S. Geselowitz DB. Tarbell JM. Estimation of Reynolds stresses within the Penn State left ventricular assist device. ASAIO Transactions 36(3):M274–8, 1990 [PubMed] [Google Scholar]
- 38.Jarvis P, Tarbell JM, Frangos JA. An in vitro evaluation of an artificial heart. ASAIO Transactions 37(1):27–32, 1991. [DOI] [PubMed] [Google Scholar]
- 39.Baldwin JT, Deutsch S, Geselowitz DB, Tarbell JM. LDA measurements of mean velocity and Reynolds stress fields within an artificial heart ventricle. Journal of Biomechanical Engineering 116(2):190–200, 1994 [DOI] [PubMed] [Google Scholar]