Abstract
Perceived postural stability has been reported to decrease as sway area increases on firm surfaces. However, changes in perceived stability under increasingly challenging conditions (e.g. removal of sensory inputs) and the relationship with sway area are not well characterized. Moreover, whether perceived stability varies as a function of age or history of falls is unknown. Here we investigate how perceived postural stability is related to sway area and whether this relationship varies as a function of age and fall history while vision and proprioceptive information are manipulated. Sway area was measured in 426 participants from the Baltimore Longitudinal Study of Aging while standing with eyes open and eyes closed on the floor and a foam cushion. Participants rated their stability [0 (completely unstable) to 10 (completely stable)] after each condition, and reported whether they had fallen in the past year. Perceived stability was negatively associated with sway area (cm^2) such that individuals who swayed more felt less stable across all conditions (β = −0.53, p < 0.001). Perceived stability decreased with increasing age (β = −0.019, p < 0.001), independent of sway area. Fallers had a greater decline in perceived stability across conditions (F = 2.76, p = 0.042) compared to non-fallers, independent of sway area. Perceived postural stability declined as sway area increased during a multi-sensory balance test. A history of falling negatively impacts perceived postural stability when vision and proprioception are simultaneously challenged. Perceived postural stability may provide additional information useful for identifying individuals at risk of falls.
Keywords: Postural Sway, Perceived Postural Stability, Aging, Falls
Introduction
Individuals with balance problems often report feeling unsteady (Schieppati et al. 1999), although some individuals who report feeling unsteady appear to have normal sway during balance tests (e.g. Persistent Postural Perceptual Dizziness, Mal de Debarquement Syndrome) (Querner et al. 2000; Lewis 2004; Clark et al. 2013). This apparently normal sway may be facilitated by hypervigilance and co-contraction of leg muscles (Dieterich and Staab 2017), which are difficult to quantify in typical clinical settings. Perception of postural stability (i.e. “How stable did you feel?”) has previously been related to sway area during standing, such that as sway area increases, one’s subjective report of steadiness decreases (Schieppati et al. 1999). Sway area has been related to peripheral sensory function (Anson et al. 2017), which may directly influence perception of postural stability (Schieppati et al. 1999; Huffman et al. 2009; Naranjo et al. 2016). This is of particular relevance to older adults who experience age related declines in multiple sensory systems (Black et al. 2008; Ko et al. 2015; Li et al. 2015). Indeed, postural sway has been suggested as an indicator of fall risk in older adults (Baczkowicz et al. 2008; Howcroft et al. 2017).
Falls pose a significant public health risk that increases with age and negatively impacts the health and quality of life for the person who falls (Parry et al. 2014). Older adults with a history of falling often report being unsteady, are afraid/anxious of future falls, and report lower balance confidence (Maki et al. 1991; Delbaere et al. 2009; Parry et al. 2014). Past falls have an adverse effect on risk for future falls via increased fear of falling and changes in activity participation (Allison et al. 2013; Hoang et al. 2017). A history of falls or fear of falling may also bias perception of postural stability via an interaction between multisensory integration, affect, and cognition (Hull et al. 2013; Dieterich and Staab 2017).
It is not clear from previous studies how perception of postural stability is related to sway area when sensory information is systematically manipulated during balance testing. Increased cognitive demand (serial subtraction) does not influence perceived postural stability, but altering the size and shape of the base of support or closing the eyes reduced perceived postural stability (Tarantola et al. 1997; DiDomenico and Nussbaum 2005). Previous work has not included conditions that manipulate somatosensory reliability (such as standing on foam) or conditions where vestibular input would be the primary sensory contribution (such as standing on foam with eyes closed) (Shumway-Cook and Horak 1986; Agrawal et al. 2009). Perceived postural stability is thought to incorporate self-motion with internal representations of points of reference such as gravity or the size of the base of support (Cañal-Bruland et al. 2015), determined in part by sensory input. Given the decline in sensory function and perceptual thresholds with aging, it is important to determine how sensory balance challenges impact the relationship between perceived postural stability and sway area. Additionally, it is not known whether perceived stability differs based on a history of prior falls. Here we report on the relationship between sway area and perceived stability across four balance testing conditions when sensory information is systematically manipulated. We hypothesized that perceived postural stability would decrease as sway area increased as sensory information was systematically manipulated. Additionally, we hypothesized that a history of falling would be associated with a larger change in perceived stability, relative to sway area, as balance tasks became more challenging across conditions.
Methods
The Baltimore Longitudinal Study of Aging (BLSA) is an ongoing prospective cohort study initiated in 1958 and currently conducted by the Intramural Research Program of the National Institute on Aging (IRP-NIA). Subjects are community-dwelling participants aged 20 and older who undergo a standardized array of tests over 3 days every 1-4 years at the Clinical Research Unit of the IRP-NIA in Baltimore, MD. The present analysis includes a cross-sectional sample of all BLSA participants seen between August 2014 and June 2016. During this time period 426 participants underwent postural sway testing and were also queried regarding their perceived postural stability (described below). Participants also completed testing with the Short Physical Performance Battery (n = 421). All participants provided written informed consent. The BLSA study protocol was approved by the National Institute of Environmental Health Sciences Institutional Review Board. Demographic information was collected along with self-reported history of falling in the previous 12 months. A positive history of falling was defined as one or more falls in the previous 12 months. Participants were not eligible to participate in the postural testing if they could not stand and walk unassisted.
Postural Sway and Perceived Stability
Center of mass (COM) sway area was measured using the BalanSens™ inertial measurement units including triaxial accelerometer, triaxial gyroscope, and a triaxial magnetometer (BioSensics LLC, Brookline, MA) placed at the waist and lower leg (Najafi et al. 2010). Body sway was recorded at 100 Hz and the BalanSens proprietary software calculated sway area based on the participants height and weight (Yalla et al. 2014). Each sensor provides quaternions that are converted to Euler angles in three dimensions. The Euler angles are converted to COM displacement using a two-segment model previously described in detail and validated by Najafi and colleagues (Najafi et al. 2010). COM displacement measured with the BalanSens was highly correlated (r = 0.92) with center of pressure displacement (Najafi et al. 2010). Participants stood with feet together and hands on their hips, first on the floor with eyes open (FLEO, condition 1) and then with eyes closed (FLEC, condition 2) and then they stood on a foam cushion (Sunmate, Dynamic Systems, Inc.) of density 72.2 kg/m3 first with eyes open (FOEO, condition 3) and then with eyes closed (FOEC, condition 4). Participants were provided up to three attempts to successfully complete one trial lasting 40 seconds for each condition (Wu et al. 2009; De Nunzio et al. 2014; Anson et al. 2017). Participants were progressed from condition 1 through 4, and in this cohort all participants were able to complete the first 3 conditions and progress to condition 4. Not all participants were able to successfully complete condition 4. After each balance test, participants were asked to rate how stable they felt using an integer scale from 0 (completely unstable) to 10 (perfectly stable) (Schieppati et al. 1999). Eleven point numeric rating scales, such as the one used here, have been widely used to characterize subjective phenomena in research and have high reliability and validity as reported in a recent review (Gries et al. 2017). Participants were excluded from postural sway testing if they required assistance to stand from sitting or to walk to minimize the risk of falling during the balance testing. For each participant, the fitted slope between perceived postural stability and sway area was calculated for all successfully completed balance tests.
Short Physical Performance Battery
Physical performance and mobility was assessed using the Short Physical Performance Battery (SPPB) which consists of standing balance tests, repeated chair stands, and a 6-meter walk. Standing balance was assessed with, participants sequentially standing with their feet side-by-side, in semi-tandem, in full tandem, and then on one leg for 10 seconds each. Each balance task was recorded for 10 seconds whether the participant was successful at maintaining the prescribed position or not. For the chair stands, participants folded their arms across their chest and stand up once from a chair. If successful, they were instructed to stand up and sit down five times as quickly as possible, and the duration was recorded. Gait speed was calculated as the average of two repetitions of a usual pace 6-meter walk with a standing start. Performance scores were based on a previously published scoring system with a maximum score of 12 (Guralnik et al. 1994). Individuals who score less than 10 have a higher risk of developing disability related to mobility and activities of daily living (Guralnik et al. 2000).
Data Analysis
First, a multivariate mixed model regression was used to determine the relationship between perceived stability and sway area across balance conditions accounting for repeated testing within individuals. Perceived stability was modelled as the dependent variable and sway area, age, gender, and history of falling were independent variables. Second, descriptive statistics were calculated for the SPPB and a t-test determined whether fallers and non-fallers differed in their SPPB scores. Third, an ANCOVA was used to determine whether sway area differed across conditions accounting for potential differences between fallers and non-fallers while controlling for perceived postural stability, age, and gender. Sway area was the dependent variable, postural condition and status as a faller were independent variables, and covariates were perceived stability, age, and gender. Last, an ANCOVA was used to determine whether perceived postural stability differed across conditions accounting for potential differences between fallers and non-fallers while controlling for sway area, age, and gender. Perceived postural stability was the dependent variable, postural condition and status as a faller were independent variables, and covariates were sway area, age, and gender. The mixed model, t-test, and ANCOVA analyses were independent questions and main effects and interactions were considered statistically significant at α = 0.05. A corrected α = 0.008 was used for both ANCOVA analyses due to multiple planned post-hoc comparisons.
Results
The mean age of the participants was 72.6 (SD 12.4, range 24-93) and 225 (52.7%) were women. The distribution of participants by decade was as follows: 13 adults under age 40, 17 aged 40-50, 21 aged 50-60, 96 aged 60-70, 148 aged 70-80, 122 aged 80-90, and 10 aged >90. 92 participants (21.5%) reported at least 1 fall in the past year. The mean SPPB score was 11.6 (SD 0.95, range 6-12). There was not a significant difference between fallers and non-fallers on the SPPB (t(1,423) = −0.0685, p = 0.4727). We used a multivariate mixed model regression to understand the contributions of the different factors on perceived postural stability (Table 1). Independent of the other factors, perceived postural stability was negatively correlated with sway area such that as sway area increased perceived postural stability decreased (β = −0.53, p < 0.001). This corresponds to a 0.53 point decrease in perceived postural stability for every 1 cm^2 increase in sway area. Including condition as a covariate in the regression model did not change the significance of the relationship between perceived postural stability and sway area (data not shown). Perceived postural stability also decreased with increasing age (β = −0.019, p < 0.001). This corresponds to a 0.2 point decrease in perceived postural stability for each decade, see Figure 1. The relationship between perceived postural stability and sway area did not differ between fallers and non-fallers (β = −0.17, p = 0.274), see Figure 2.
Table 1.
Multivariate mixed regression model of predictors of perceived stability. β’s represent unstandardized regression coefficients. Significance indicated by *, p’s < 0.001.
| Predictor Variables | β | Standard Error | 95% CI |
|---|---|---|---|
| Age | −0.019* | 0.005 | [−0.03, −0.009] |
| Gender | |||
| Female | Ref | Ref | Ref |
| Male | −0.24 | 0.13 | [−0.49, 0.02] |
| Sway Area (cm^2) | −0.53 * | 0.02 | [−0.57, −0.49] |
| History of Falling | |||
| Non-Fallers | Ref | Ref | Ref |
| Fallers | −0.17 | 0.16 | [−0.48, 0.13] |
| Intercepta | 9.8 | [9.05, 10.7] | |
The intercept would correspond to a male participant without a history of falling, age zero, and with sway area of 0 cm squared and thus is not interpreted.
Figure 1.
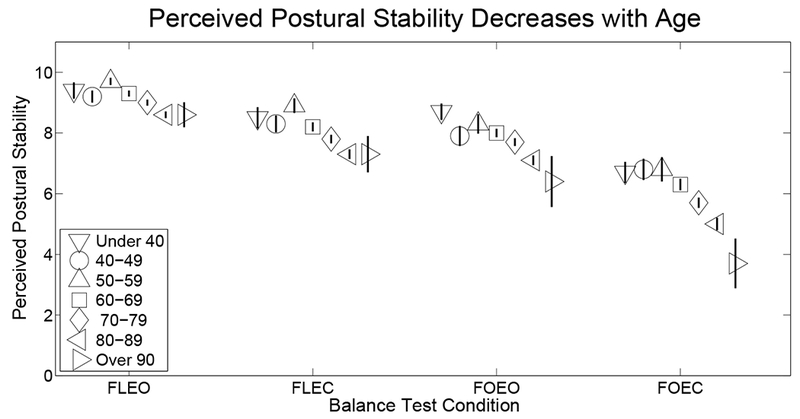
Average perceived postural stability shown for each decade and balance test condition showing the decrease in perceived postural stability with increasing age. Error bars represent standard error of the mean.
Figure 2.
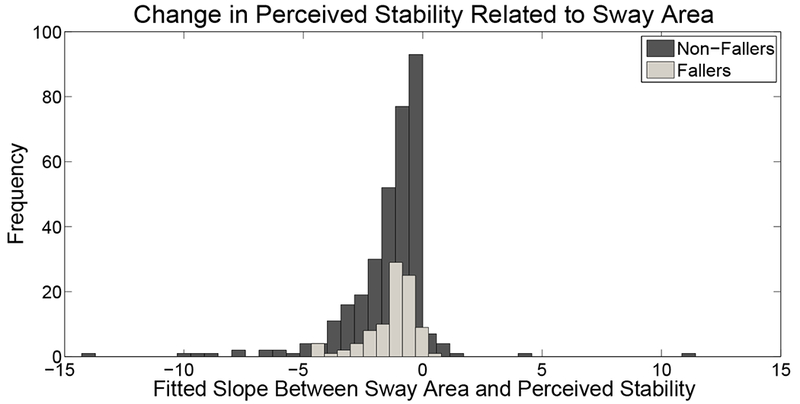
Distribution of the slopes between perceived postural stability and sway area calculated for each participant.
Overall, sway area increased significantly (F(3,1690) = 302.9, p < 0.001) across conditions as the balance tasks became progressively more difficult, and all pairwise comparisons were significant (p’s < 0.004), see Table 2. Perceived postural stability decreased across conditions (F(3,1653) = 190.57, p < 0.001). Perception of postural stability decreased statistically significantly in most but not all pairwise comparisons across conditions as the balance task became progressively more difficult (p’s < 0.004), see Table 2. The exception was the progression from FLEC to FOEO where perceived postural stability was not significantly different between those conditions.
Table 2.
Average [95% CI] COM sway area and perceived postural stability across balance test conditions. Average sway area and perceived postural stability was adjusted for model covariates (age, gender, and either perceived postural stability or sway area).
| FLEO | FLEC | FOEO | FLEC | |
|---|---|---|---|---|
| COM Sway | 0.50 | 0.89* | 1.215 *, ** | 3.24 *, **, † |
| Area (cm^2) | [0.47-0.55] | [0.80-0.97] | [1.11-1.32] | [2.99-3.49] |
| Perceived Postural | 8.91 | 7.73 * | 7.55 * | 5.63 *, **, † |
| Stability | [8.74-9.07] | [7.56-7.89] | [7.39-7.71] | [5.47-5.79] |
indicates significant change relative to FLEO
indicates significant change relative to FLEC,
indicates significant change relative to FOEO.
All significant comparisons p’s < 0.004.
FLEO – floor, eyes open
FLEC – floor, eyes closed
FOEO – foam, eyes open
FOEC – foam, eyes closed
A history of falling was a significant covariate to the relationship between perceived stability and condition after controlling for sway area, age and gender. There was a steeper decline in perceived postural stability across conditions for fallers compared to individuals without falls indicated by an interaction between status as a faller and condition (F(3,1653) = 2.74, p = 0.042), see Figure 3. This steeper decline in perceived stability across conditions was driven by the FOEC condition with fallers reporting significantly lower perceived postural stability (t = −3.69, p = 0.006). History of falling was not a significant covariate to the relationship between sway area and condition (F(1,1653) = 1.65, p = 0.1986 after controlling for perceived stability, age, and gender.
Figure 3.
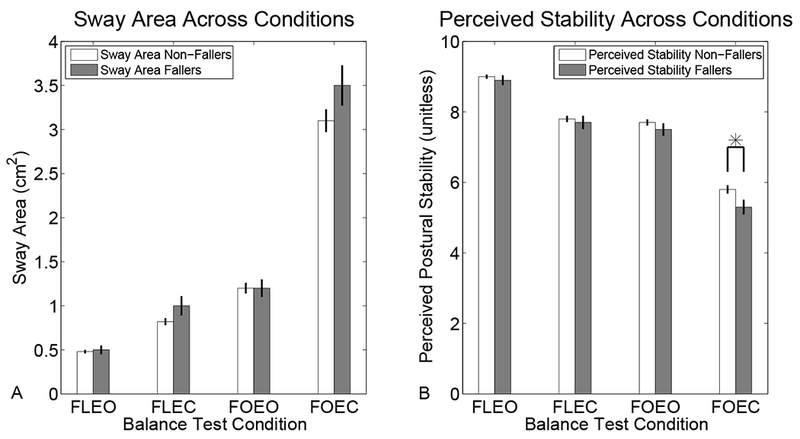
Change in (A) sway area and (B) perceived postural stability across the rank ordered balance test conditions. Lighter bars represent non-fallers and darker bars represent fallers. Error bars represent standard error of the mean. * denotes significant between group difference, note that this group difference was only present for perceived stability and only in the FOEC condition.
Discussion
Perceived postural stability decreased as sway area increased, extending results from prior studies on firm surfaces (Schieppati et al. 1999; DiDomenico and Nussbaum 2005; Murnaghan et al. 2009) to foam surfaces which offer additional sensory challenge. The current results add to prior work by including balance tests which manipulate somatosensory and visual sensory reliability encouraging increased reliance on vestibular inputs (Shumway-Cook and Horak 1986; Cohen et al. 1993). Interestingly, although all sensory manipulations resulted in a decrease in perceived postural stability compared to the FLEO condition, there was not a difference between FLEC and FOEO conditions. Perceived postural stability was equivalently impacted when only one sensory system was challenged regardless of which sensory modality (vision or proprioception) was challenged. In contrast, postural sway in the FOEO condition was significantly greater than during the FLEC condition. Medium and high frequency sway increase when standing on foam with eyes open and closed (Fujimoto et al. 2014; Fujimoto et al. 2015). Higher oscillation frequency may contribute to abnormal perception of stability for individuals who demonstrate elevated leg muscle co-contraction (Blaszczyk et al. 1993; Craig et al. 2017). Perceived stability has also been reported to decline as voluntary oscillation frequency increases (Martin Lorenzo and Vanrenterghem 2015). The difference in sway behavior and perception of postural stability could be explained by differences in multisensory integration.
These results suggest pathways for multisensory integration may differ between perception of postural stability and postural control. Perception of postural stability may depend more on the ability to represent one’s self, independent of the ability to represent external space, which has been shown to remain constant during balance tasks that systematically increase postural sway (Cañal-Bruland et al. 2015). For the balance task presented here, discrete processing of sensory input for perception and postural control may be less relevant since the available sensory input was always congruent with self-motion. However, discrete processing of sensory input for postural control and perception would be useful in more natural environments where optic flow can also result from object motion independent of postural sway (Gibson 1958). This would be particularly relevant in the context of obstacle avoidance, with important implications for multisensory processing during locomotion (Fajen and Warren 2003; Dokka et al. 2015). Alternatively, perceptual processing of self-motion may not be completely distinct from multisensory integration for postural control (Fitzpatrick and McCloskey 1994; Bacsi and Colebatch 2005). Dynamic sensory reweighting for postural control influences the perception of postural orientation between different body segments (Dalton et al. 2017). It remains to be demonstrated whether the relationship between perception of postural stability and postural control is bi-directional as has been reported to exist between motor planning and visual processing of relevant images (Bortoletto et al. 2011). Future studies are needed to investigate whether perceived postural stability directly or indirectly influences postural control.
In addition to the relationship between perceived postural stability and sway area, there was an independent relationship between perceived postural stability and age. As age increased, perceived postural stability decreased by 0.2 points for each decade, independent of sway area. Increased thresholds for detection of self-motion may contribute to the age-related decrease in perceived postural stability observed in this cohort. Older adults’ perception of the onset of a fall is delayed relative to younger adults during temporal order discrimination tasks (what came first: falling or an auditory tone) (Lupo and Barnett-Cowan 2018). Perceived stability may be a construct that is influenced by both sensory integrity and contextual sensory perception. Vestibular perceptual thresholds of self-motion increase with age and higher thresholds were associated with balance problems on FOEC (Bermúdez Rey et al. 2016). Visual motion perception and proprioception thresholds also increase with age (Trick and Silverman 1991; Deshpande et al. 2003). Tremblay et al. previously reported no difference in perceived stability between young and older age groups (Tremblay et al. 2004). However, in contrast to the current study, Tremblay et al excluded anyone with sensory changes or a history of falling thus limiting generalization to only the healthiest older adults. In our cohort there was considerable variability in perceived postural stability that increased with age. Task related anxiety (fear of falling) or cognitive impairments which impact sensory processing could also contribute to the relationship between age and perceived postural stability and future work is needed to identify how affect and cognitive ability impact perceived postural stability.
Clinical Implications
It is interesting to note that several individuals in both the faller and non-faller groups had minimal to no change in perceived postural stability across the balance tasks, despite increase in sway (slopes approximately zero in Figure 2). In contrast, individuals exposed to height-based postural threat report increased instability despite smaller or unchanged sway area (Huffman et al. 2009; Cleworth et al. 2012). The variability in perceptual response to changes in sway across conditions known to modulate postural control further demonstrates that all forms of postural threat are not created equal (Phanthanourak et al. 2016). Being able to match expected perception of self-motion to specific clinical testing conditions may be even more important for individuals with altered perception of self-motion, such as fallers.
Another novel contribution from this work is the characterization of the relationship between fall history and perception of postural stability. Individuals with a history of falling had a more negative change in perceived stability across conditions, driven by their lower perceived stability in the FOEC condition. A past fall could result in a persistent fear or anxiety response which negatively impacts perceived postural stability (Dieterich and Staab 2017). It is possible that the prior fall resulted in hyper-vigilance and the context of the balance testing paradigm increased the stress level of some participants (possibly via perceived threat) leading to a more negative perception of postural stability (Vaegter et al. 2018). Additionally, a prior fall may result in catastrophizing thoughts that bias perception in a negative way (Delbaere et al. 2009). Previous work demonstrated more diffuse cognitive processing for multisensory integration during standing balance in older adults, especially in the frontal-lateral brain region which facilitates attention (Lin et al. 2017). Fallers may allocate more attention to their postural sway during the FOEC balance task than non-fallers. Increased attention combined with hypervigilance could explain the more negative perception of postural stability in the group of fallers observed here. However, it is not clear whether the more negative perception of postural stability associated with a past fall is detrimental to the overall balance ability of the participants, especially since fallers and non-fallers did not differ in their physical performance or mobility as measured by the SPPB. An alternative interpretation is that the individuals with a less negative perception of postural stability over-estimate their stability. The effect of a prior fall may recalibrate perception with reality. In fact, the negative context of a prior fall may enhance processing of vestibular cues for both perception of postural stability and postural control (Preuss et al. 2015). Future studies are needed to determine the mechanisms which contribute to change in perceived postural stability, and to determine whether lack of change reflects a maladaptive perceptual behavior that leads to functional impairments such as falls.
Including measures of perceived postural instability with clinical examinations may offer added value especially since some traditional balance measures are less effective at identifying early changes in balance ability in older adults compared to reported instability (Tanaka et al. 2015). Balance training has beneficial effects on reducing postural sway both within a session (Tarantola et al. 1997), and after repeated training sessions targeting balance training (Rose and Clark 2000). Since the relationship between perception and action may be bi-directional (Bortoletto et al. 2011); it is important not only to ensure that as balance ability improves perception of stability also improves, but also to specifically address enhancing perception of postural stability. Balance confidence is often characterized in studies of balance, and it may be that a global perception of balance confidence mediates the relationship between perception of stability and sway. Perception of postural stability is important to comprehensively evaluate balance ability in the context of rehabilitation.
Limitations
These data are cross-sectional and cannot be used to support causal inferences between the perceived postural stability and sway area. Fall history was determined by retrospective self-report and based on a single fall in the past year. Further, the mechanism linking fall history with steeper decline in perceived stability across balance conditions cannot be identified from this analysis. The population studied here are healthy adults and the relationship between postural sway and perception of postural stability may differ for individuals with more severe balance problems or sensory-motor pathology.
Conclusions
Perceived postural stability decreased as sway area increased across conditions of a multi-sensory balance test. A history of falling negatively impacts perceived postural stability specifically during standing balance testing on foam with eyes closed. Subjective perception of postural stability during balance testing may provide additional information useful for estimating fall risk.
Acknowledgments
Funding: This work was supported in part by the National Institutes of Health [NIDCD K23 DC013056, NIDCD T32 DC000023].
Conflict of Interest
This work was supported in part by the National Institutes of Health: NIDCD K23 DC013056 (YA), NIDCD T32 DC000023 (EA).
Footnotes
Ethical approval: “All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
References
- Agrawal Y, Carey JP, Della Santina CC, et al. (2009) Disorders of balance and vestibular function in US adults. Arch Intern Med 169:938–944. doi: 10.1001/archinternmed.2009.66 [DOI] [PubMed] [Google Scholar]
- Allison LK, Painter JA, Emory A, et al. (2013) Participation Restriction, Not Fear of Falling, Predicts Actual Balance and Mobility Abilities in Rural Community-Dwelling Older Adults. J Geriatr Phys Ther 36:13–23. doi: 10.1519/JPT.0b013e3182493d20 [DOI] [PubMed] [Google Scholar]
- Anson E, Bigelow RT, Swenor B, et al. (2017) Loss of Peripheral Sensory Function Explains Much of the Increase in Postural Sway in Healthy Older Adults. Front Aging Neurosci 9:202. doi: 10.3389/fnagi.2017.00202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacsi AM, Colebatch JG (2005) Evidence for reflex and perceptual vestibular contributions to postural control. Exp Brain Res 160:22–28. doi: 10.1007/s00221-004-1982-2 [DOI] [PubMed] [Google Scholar]
- Baczkowicz D, Szczegielniak J, Proszkowiec M (2008) Relations between postural stability, gait and falls in elderly persons--preliminary report. Ortop Traumatol Rehabil 10:478–485. doi: 872564 [pii] [PubMed] [Google Scholar]
- Bermúdez Rey MC, Clark TK, Wang W, et al. (2016) Vestibular Perceptual Thresholds Increase above the Age of 40. Front Neurol 7:162. doi: 10.3389/fneur.2016.00162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black AA, Wood JM, Lovie-Kitchin JE, Newman BM (2008) Visual impairment and postural sway among older adults with glaucoma. Optom Vis Sci 85:489–97. [DOI] [PubMed] [Google Scholar]
- Blaszczyk JW, Hansen PD, Lowe DL (1993) Postural Sway and Perception of the Upright Stance Stability Borders. Perception 22:1333–1341. doi: 10.1068/p221333 [DOI] [PubMed] [Google Scholar]
- Bortoletto M, Mattingley JB, Cunnington R (2011) Action intentions modulate visual processing during action perception. Neuropsychologia 49:2097–2104. doi: 10.1016/j.neuropsychologia.2011.04.004 [DOI] [PubMed] [Google Scholar]
- Cañal-Bruland R, Aertssen AM, Ham L, Stins J (2015) Size estimates of action-relevant space remain invariant in the face of systematic changes to postural stability and arousal. Conscious Cogn 34:98–103. doi: 10.1016/j.concog.2015.04.006 [DOI] [PubMed] [Google Scholar]
- Clark BC, LePorte A, Clark S, et al. (2013) Effects of persistent Mal de debarquement syndrome on balance, psychological traits, and motor cortex exctiability. J Clin Neurosci 20:446–50. doi: 10.1016/j.jocn.2012.06.004 [DOI] [PubMed] [Google Scholar]
- Cleworth TW, Horslen BC, Carpenter MG (2012) Influence of real and virtual heights on standing balance. Gait Posture 36:172–6. doi: 10.1016/j.gaitpost.2012.02.010 [DOI] [PubMed] [Google Scholar]
- Cohen H, Blatchly CA, Gombash LL (1993) A study of the clinical test of sensory interaction and balance. Phys Ther 73:346–51. [DOI] [PubMed] [Google Scholar]
- Craig CE, Calvert GHM, Doumas M (2017) Effects of the availability of accurate proprioceptive information on older adults’ postural sway and muscle co-contraction. Eur J Neurosci 46:2548–2556. doi: 10.1111/ejn.13703 [DOI] [PubMed] [Google Scholar]
- Dalton BH, Rasman BG, Inglis JT, Blouin JS (2017) The internal representation of head orientation differs for conscious perception and balance control. J Physiol 595:2731–2749. doi: 10.1113/JP272998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Nunzio AM, Zucchella C, Spicciato F, et al. (2014) Biofeedback rehabilitation of posture and weight-bearing distribution in stroke: a center of foot pressure analysis. Funct Neurol 29:127–34. [PMC free article] [PubMed] [Google Scholar]
- Delbaere K, Crombez G, van Haastregt JCM, Vlaeyen JWS (2009) Falls and catastrophic thoughts about falls predict mobility restriction in community-dwelling older people: A structural equation modelling approach. Aging Ment Health 13:587–592. doi: 10.1080/13607860902774444 [DOI] [PubMed] [Google Scholar]
- Deshpande N, Connelly DM, Culham EG, Costigan PA (2003) Reliability and validity of ankle proprioceptive measures. Arch Phys Med Rehabil 84:883–9. [DOI] [PubMed] [Google Scholar]
- DiDomenico A, Nussbaum MA (2005) Interactive effects of mental and postural demands on subjective assessment of mental workload and postural stability. Saf Sci 43:485–495. doi: 10.1016/J.SSCI.2005.08.010 [DOI] [Google Scholar]
- Dieterich M, Staab JP (2017) Functional dizziness: from phobic postural vertigo and chronic subjective dizziness to persistent postural-perceptual dizziness. Curr Opin Neurol 30:107–113. doi: 10.1097/WCO.0000000000000417 [DOI] [PubMed] [Google Scholar]
- Dokka K, DeAngelis GC, Angelaki DE (2015) Multisensory Integration of Visual and Vestibular Signals Improves Heading Discrimination in the Presence of a Moving Object. J Neurosci 35:13599–13607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fajen BR, Warren WH (2003) Behavioral dynamics of steering, obstacle avoidance, and route selection. J Exp Psychol Hum Percept Perform 29:343–62. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick R, McCloskey DI (1994) Proprioceptive, visual and vestibular thresholds for the perception of sway during standing in humans. J Physiol 478:173–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujimoto C, Egami N, Demura S, et al. (2015) The effect of aging on the center-of-pressure power spectrum in foam posturography. Neurosci Lett 585:92–7. doi: 10.1016/j.neulet.2014.11.033 [DOI] [PubMed] [Google Scholar]
- Fujimoto C, Kamogashira T, Kinoshita M, et al. (2014) Power Spectral Analysis of Postural Sway During Foam Posturography in Patients With Peripheral Vestibular Dysfunction. Otol Neurotol 35:e317–e323. doi: 10.1097/MAO.0000000000000554 [DOI] [PubMed] [Google Scholar]
- Gibson JJ (1958) Visually controlled locomotion and visual orientation in animals. Br J Psychol 49:182–194. [DOI] [PubMed] [Google Scholar]
- Gries K, Berry P, Harrington M, et al. (2017) Literature review to assemble the evidence for response scales used in patient-reported outcome measures. J patient-reported outcomes 2:41. doi: 10.1186/s41687-018-0056-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Pieper CF, et al. (2000) Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci 55:M221–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, et al. (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:M85–94. [DOI] [PubMed] [Google Scholar]
- Hoang OTT, Jullamate P, Piphatvanitcha N, Rosenberg E (2017) Factors related to fear of falling among community-dwelling older adults. J Clin Nurs 26:68–76. doi: 10.1111/jocn.13337 [DOI] [PubMed] [Google Scholar]
- Howcroft J, Lemaire ED, Kofman J, McIlroy WE (2017) Elderly fall risk prediction using static posturography. PLoS One 12:e0172398. doi: 10.1371/journal.pone.0172398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JL, Horslen BC, Carpenter MG, Adkin AL (2009) Does increased postural threat lead to more conscious control of posture? Gait Posture 30:528–532. doi: 10.1016/J.GAITPOST.2009.08.001 [DOI] [PubMed] [Google Scholar]
- Hull SL, Kneebone II, Farquharson L (2013) Anxiety, Depression, and Fall-Related Psychological Concerns in Community-Dwelling Older People. Am J Geriatr Psychiatry 21:1287–1291. doi: 10.1016/j.jagp.2013.01.038 [DOI] [PubMed] [Google Scholar]
- Ko S-U, Simonsick E, Deshpande N, Ferrucci L (2015) Sex-specific age associations of ankle proprioception test performance in older adults: results from the Baltimore Longitudinal Study of Aging. Age Ageing 44:485–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis RF (2004) Frequency-specific mal de debarquement. Neurology 63:1983–4. doi: 10.1212/01.WNL.0000144701.94530.6A [DOI] [PubMed] [Google Scholar]
- Li C, Layman AJ, Geary R, et al. (2015) Epidemiology of vestibulo-ocular reflex function: data from the Baltimore Longitudinal Study of Aging. Otol Neurotol 36:267–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C-C, Barker JW, Sparto PJ, et al. (2017) Functional near-infrared spectroscopy (fNIRS) brain imaging of multi-sensory integration during computerized dynamic posturography in middle-aged and older adults. Exp brain Res 235:1247–1256. doi: 10.1007/s00221-017-4893-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupo J, Barnett-Cowan M (2018) Impaired perceived timing of falls in the elderly. Gait Posture 59:40–45. doi: 10.1016/j.gaitpost.2017.09.037 [DOI] [PubMed] [Google Scholar]
- Maki BE, Holliday PJ, Topper AK (1991) Fear of Falling and Postural Performance in the Elderly. J Gerontol 46:M123–M131. doi: 10.1093/geronj/46.4.M123 [DOI] [PubMed] [Google Scholar]
- Martin Lorenzo T, Vanrenterghem J (2015) Effects of increased anterior–posterior voluntary sway frequency on mechanical and perceived postural stability. Hum Mov Sci 39:189–199. doi: 10.1016/j.humov.2014.11.012 [DOI] [PubMed] [Google Scholar]
- Murnaghan CD, Elston B, Mackey DC, Robinovitch SN (2009) Modeling of postural stability borders during heel-toe rocking. Gait Posture 30:161–7. doi: 10.1016/j.gaitpost.2009.03.010 [DOI] [PubMed] [Google Scholar]
- Najafi B, Horn D, Marclay S, et al. (2010) Assessing postural control and postural control strategy in diabetes patients using innovative and wearable technology. J Diabetes Sci Technol 4:780–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naranjo EN, Cleworth TW, Allum JHJ, et al. (2016) Vestibulo-spinal and vestibulo-ocular reflexes are modulated when standing with increased postural threat. J Neurophysiol 115:833–42. [DOI] [PubMed] [Google Scholar]
- Parry SW, Deary V, Finch T, et al. (2014) The STRIDE (Strategies to Increase confidence, InDependence and Energy) study: cognitive behavioural therapy-based intervention to reduce fear of falling in older fallers living in the community - study protocol for a randomised controlled trial. Trials 15:210. doi: 10.1186/1745-6215-15-210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phanthanourak AL, Cleworth TW, Adkin AL, et al. (2016) The threat of a support surface translation affects anticipatory postural control. Gait Posture 50:145–150. doi: 10.1016/j.gaitpost.2016.08.031 [DOI] [PubMed] [Google Scholar]
- Preuss N, Ellis AW, Mast FW (2015) Negative emotional stimuli enhance vestibular processing. Emotion 15:411–5. doi: 10.1037/emo0000092 [DOI] [PubMed] [Google Scholar]
- Querner V, Krafczyk S, Dieterich M, Brandt T (2000) Patients with somatoform phobic postural vertigo: the more difficult the balance task, the better the balance performance. Neurosci Lett 285:21–4. [DOI] [PubMed] [Google Scholar]
- Rose DJ, Clark S (2000) Can the control of bodily orientation be significantly improved in a group of older adults with a history of falls? J Am Geriatr Soc 48:275–82. [DOI] [PubMed] [Google Scholar]
- Schieppati M, Tacchini E, Nardone A, et al. (1999) Subjective perception of body sway. J Neurol Neurosurg Psychiatry 66:313–22. doi: 10.1136/JNNP.66.3.313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shumway-Cook A, Horak FB (1986) Assessing the Influence of Sensory Interaction on Balance. Phys Ther 66:1548–1550. doi: 10.1093/ptj/66.10.1548 [DOI] [PubMed] [Google Scholar]
- Tanaka EH, Santos PF, Reis JG, Rodrigues NC (2015) Is there a relationship between complaints of impaired balance and postural control disorder in community - dwelling elderly women ? A cross-sectional study with the use of posturography. Braz J Phys Ther 19:186–193. doi: 10.1590/bjpt-rbf.2014.0086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarantola J, Nardone A, Tacchini E, Schieppati M (1997) Human stance stability improves with the repetition of the task: effect of foot position and visual condition. Neurosci Lett 228:75–8. [DOI] [PubMed] [Google Scholar]
- Tremblay F, Mireault A-C, Dessureault L, et al. (2004) Postural stabilization from fingertip contact: I. Variations in sway attenuation, perceived stability and contact forces with aging. Exp Brain Res 157:275–85. doi: 10.1007/s00221-004-1830-4 [DOI] [PubMed] [Google Scholar]
- Trick GL, Silverman SE (1991) Visual sensitivity to motion: age-related changes and deficits in senile dementia of the Alzheimer type. Neurology 41:1437–40. [DOI] [PubMed] [Google Scholar]
- Vaegter HB, Andersen TE, Harvold M, et al. (2018) Increased Pain Sensitivity in Accident-related Chronic Pain Patients with Comorbid Posttraumatic Stress. Clin J Pain 34:313–321. doi: 10.1097/AJP.0000000000000543 [DOI] [PubMed] [Google Scholar]
- Wu J, McKay S, Angulo-Barroso R (2009) Center of mass control and multi-segment coordination in children during quiet stance. Exp Brain Res 196:329–339. [DOI] [PubMed] [Google Scholar]
- Yalla SV, Crews RT, Fleischer AE, et al. (2014) An immediate effect of custom-made ankle foot orthoses on postural stability in older adults. Clin Biomech 29:1081–1088. doi: 10.1016/J.CLINBIOMECH.2014.10.007 [DOI] [PubMed] [Google Scholar]


