Abstract
Purpose
Heritable thoracic aortic disease (HTAD) can result from null variants in MYLK, which encodes myosin light chain kinase (MLCK). Data on which MYLK missense variants are pathogenic and information to guide aortic disease management are limited.
Methods
Clinical data from 33 cases with MYLK pathogenic variants were analyzed (5 null and 2 missense variants) and the effect of missense variants on kinase activity was assessed.
Results
Twenty-three individuals (39%) experienced an aortic event (defined as aneurysm repair or dissection); the majority of these events were aortic dissections (87%). Aortic diameters were minimally enlarged at the time of dissection in many cases. Time to aortic event curves showed missense mutation carriers have earlier onset aortic events than null mutation carriers. A MYLK missense variant segregated with aortic disease over five generations but only marginally decreases MLCK kinase activity, and functional assays fail to identify all pathogenic variants in MYLK.
Conclusions
These data further define aortic phenotype associated with MYLK pathogenic variants. Given minimal aortic enlargement prior to dissection, an alternative approach to guide the timing of aortic repair is proposed based the probability of a dissection at a given age.
Keywords: MYLK, hereditary thoracic aortic disease, acute aortic dissection, myosin light chain kinase, thoracic aortic surgery
INTRODUCTION
Investigation of the genetic basis of thoracic aortic aneurysms and dissections has yielded an increased understanding of the underlying genetic changes that are associated with significantly increased risk for thoracic aortic aneurysms and dissections. Much of the current literature describes syndromic causes of heritable thoracic aortic disease (HTAD), including Marfan syndrome, Loeys-Dietz syndrome and vascular Ehlers-Danlos syndrome. In recent years, mutations of HTAD genes that cause aortic disease with no other syndromic findings have been identified, such as ACTA2 mutations, which are responsible for up to 20% of families with non-syndromic HTAD, 1,2 and mutations of MYLK, PRKG1, and MYH11 3–5
MYLK encodes the Ca2+/calmodulin-dependent myosin light chain kinase (MLCK), which phosphorylates the regulatory light chain to initiate contraction in smooth muscle cells. Using a candidate gene approach, MYLK pathogenic variants were identified in non-syndromic HTAD families. Segregation analyses confirmed that variants leading to MYLK haploinsufficiency caused HTAD, and functional analyses indicated that a missense variant in the calmodulin binding domain decreased MLCK kinase activity by 85% and therefore most likely disease-causing.4 Further support that haploinsufficiency could cause disease came from studies of an inducible, smooth muscle specific Mylk knock-out mouse model.6 In the aorta, knock out of half of the MLCK led to 40% inhibition of RLC phosphorylation and aortic contractile response. These results indicate that MLCK levels limit contraction of aortic SMCs and therefore provide insight into why haploinsufficiency of MYLK leads to thoracic aortic disease.
More recently, case reports have described individuals and families with pathogenic variants in MYLK segregating with aortic disease.7–9 Aortic measurements in mutation carriers prior to dissection were within normal limits in almost all individuals. In two cases with type B dissections, hypertension was noted, as were the presence of features associated with syndromic causes of thoracic aortic aneurysms and dissections. However, due to the limited number of affected individuals, the clinical phenotype associated with MYLK mutations has not been clearly defined. With the addition of MYLK to commercial genetic testing panels, detection of individuals with pathogenic mutations is becoming more frequent. However, the lack of phenotypic data poses a challenge to clinicians when determining aortic surveillance and timing of surgical repair of the aorta. This report aims to provide additional information on the thoracic aortic disease phenotype associated with MYLK mutations, provide gene-specific management recommendations to guide clinical care, and present functional data for new MYLK missense variants.
METHODS AND MATERIALS
This study was approved by the Institutional Review Board at the University of Texas Health Science Center in Houston and de-identified data was provided by other centers after institutional review board approval. Informed consent was obtained from all study participants. MYLK variants were identified in our research facility (2 families), through diagnostic laboratories (4 families) and in published reports.8 Sixty individuals from seven unrelated families were studied. Cases who tested positive for a pathogenic or likely pathogenic variant, obligate carriers and family members who are affected with aortic disease with a 50% chance of carrying the variant were included in the analysis.
Phenotypic data, including demographics, diagnosis of aortic event (defined as aortic dissection or surgical repair of an aortic aneurysm), age at event, and aortic measurements prior to or at the time of event, were collected from medical records. Aortic measurements were taken at large, academic institutions and provided by the cardiologists. Aortic dissections were classified as a type A or type B dissection using the Stanford criteria. Type A dissections originate in the ascending thoracic aorta; type B dissections originate in the descending aorta. Individuals were classified as having “sudden death” if they died suddenly prior to hospitalization and no autopsy was conducted. These individuals were considered unknown phenotype and not included in risk estimates. Previously reported families were contacted to update phenotypic data. Collaborators from outside the United States provided clinical data using a standard data collection form. Church parish records were used to confirm family history and age of death for family famIT-001.
The families with MYLK (NM_053025.3) variants p.Arg1480*(c.4438C>T), p.Ser1091*(c.3272_3273delCA) and p.Ser1759P (c.5275T>C) were previously described 4;8. Two variants identified by commercial genetic testing laboratories, p.Thr1096Glnfs*38 (c.3285delG), and p.Glu1066Aspfs*10 (c.3196delG), are frameshifts and lead to a premature stop codon and haploinsufficiency. A gross deletion of coding exon 18 to the 3’UTR end of MYLK, also identified by a commercial testing laboratory, is predicted to cause haploinsufficiency. The MYLK p.Tyr1575His (c.4723T>C) missense variant was identified by whole exome sequencing and confirmed using Sanger sequencing in a research laboratory using previously described methods.9
MYLK kinase activity assay
Three missense variants in MYLK were assessed for functional effects: p.Gly1317Cys (c.3949G>T), p.Cys1384Gly (c.4150T>G), and p.Tyr1575His (c.4723T>C). Wildtype and mutant MYLK plasmids were constructed using site-directed mutagenesis and the recombinant proteins expressed in transfected cell lines. The mutagenesis and expression of myosin light chain kinase, along with activity and calmodulin activation assays were performed using previously published methods.4 The recombinant proteins were purified by affinity chromatography, and the kinase activity (Vmax) and binding to CaM (KCaM) were determined.
Statistical Analysis
Statistical analysis was done using the STATA software program [Version 12.1]. Categorical variables were presented as count and percentage. Age was summarized as median and interquartile range (25%ile- 75%ile). Wilcoxon rank-sum test was used to compare median ages between groups. The Kaplan Meier method was used to produce survival curves using age at aortic event or last follow up in the absence of aortic event to determine cumulative risk. Log-rank test was used to compare failure functions. Five individuals, considered obligate carriers, died suddenly with no prior history of aortic disease. These individuals were not included in the analysis.
A LOD score was calculated for famIT-001, which carries variant p.Tyr1575His, in which there was one generation between the shared common ancestors and the individuals in the pedigree (Figure 1). These individuals in the first two generations were included in the analysis and designated as unknown for phenotype and genotype data. A two-point LOD score was calculated using Superlink-Online (http://bioinfo.cs.technion.ac.il/superlink-online/index-working2.shtml)10 was calculated for the reconstructed pedigree using an autosomal dominant model with the reduced penetrance 0.9. The disease frequency was set to 0.0001, and the causal allele frequency was set to 0.00001.
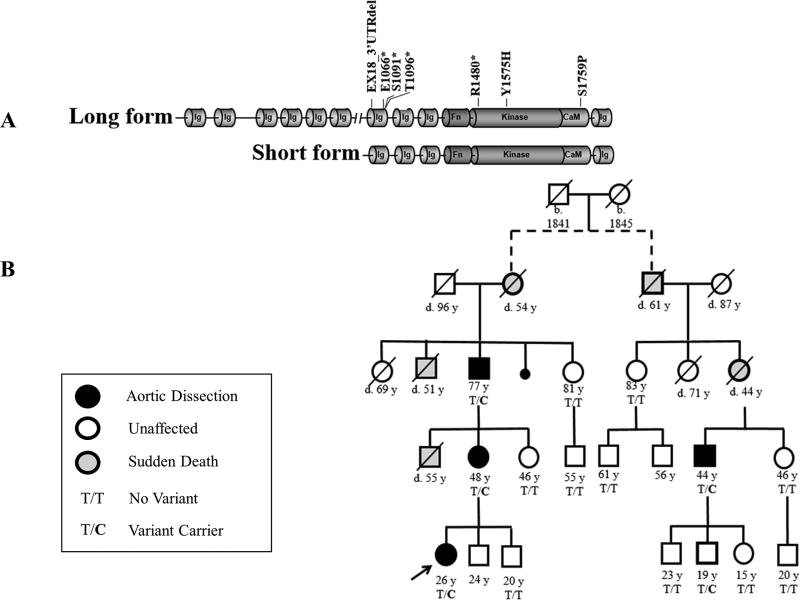
Figure 1. Pathogenic MYLK variants and segregation of variant p.Tyr1575His in famIT-001.
A. A schematic depiction of the long and short form of myosin light chain kinase (MLCK) shows the location of the MYLK pathogenic variants included in these studies. All variants are located in the short form of MLCK, which is the only form expressed in the thoracic aorta. Carriers of the variants depicted here were included in the phenotypic analysis. B. The pedigree depicts a multi-generational family with two distant arms affected with thoracic aortic disease. Church parish records were used to confirm common ancestry. Circles represent females, squares represent males. A line through the individual indicates that they are deceased and the legend provides information about the phenotype associated with shaded symbols. T/C is used to denote the pathogenic variant genotype and T/T is used to denote the WT genotype.
RESULTS
This study evaluated the aortic disease phenotype associated with seven pathogenic MYLK variants identified in unrelated families. Two pathogenic variants, p.Arg1480* and p.Ser1759Pro, were previously described in TAA400 and TAA026, respectively, and showed segregation with disease in family members.4 Since publication, one individual in TAA026, a 33 year old male known to carry the p.Ser1759Pro variant, has undergone prophylactic repair for an ascending aortic aneurysm. Previously published functional assays of the p.Ser1759Pro variant demonstrated an 85% loss of myosin light chain kinase activity.
In addition to the published families, five pathogenic or likely pathogenic variants from additional families were included in this study (Figure 1A). The first variant, p.Tyr1575His, was detected in a large Italian family using whole exome sequencing (famIT-001; Figure 1B); no other pathogenic variants were detected in other HTAD genes. This variant was not found in the Exome Aggregation Consortium (ExAC) database, has a CADD score of 24.3, is highly conserved, and is predicted to be damaging by PolyPhen2. The variant was detected in four affected family members and one young, unaffected male, and segregated through distant branches of the family with a LOD score of 4.0. The relationship between the two arms of the family could be traced through church parish records, with one generation between the proband’s generation and the shared common ancestors. Three individuals who died suddenly of unknown causes were obligate carriers. Affected individuals presented with type A aortic dissections at 26 to 77 years of age.
MYLK variant p.Thr1096Glnfs*38 was detected in TAA795 and predicted to lead to nonsense mediated decay and haploinsufficiency. The variant was detected after the proband experienced a type B dissection at the age of 56 and underwent thoracic endovascular aneurysm repair (TEVAR). On post-op day 5, he experienced a retrograde type A dissection and succumbed to complications related to his dissection. Prior to his retrograde dissection, his ascending aorta measured 3.7 cm (z-score = 0.98). At the time of surgery, his aortic tissue was noted to be thin and friable. There were no other affected family members. Eight family members, ages 25–62 years, also carry the variant and four of them, have undergone imaging and no aortic enlargement was noted.
A genomic deletion from coding exon 18 to the 3’UTR region, leading to haploinsufficiency, was detected in a 46-year-old female who presented with a type A dissection. At the time of dissection, the patient’s ascending aorta measured 4.7cm and the aortic root measured 3.3 cm. Two additional family members, ages 12 and 73 years, have the variant and have no had aortic events. The 12-year-old has had normal imaging of his entire aorta and the 73 year old has not had imaging.
Additional data from a published family with a MYLK null variant (p.S1091*) were obtained, including current status (history of aortic event/no aortic event), age at aortic event or last follow up without an event, and thoracic aortic diameters.8 The variant segregated with aortic events in five affected individuals, all of whom presented with type A dissections from 23 to 75 years of age; three resulted in death. Ascending aortic diameters at the time of dissection for the two surviving individuals were 4.7 cm and 4.8 cm. A sixth individual in this family with the variants chose to undergo prophylactic repair of his aorta at the age of 64 years after learning that his ascending aorta measured 4.1 cm.
Finally, an individual from famFRA-003 with a null variant (p.Glu1066Asnfs*10) was included. This is a 45-year-old female who had a type A dissection extending to her iliac bifurcation. At the time of the dissection, her aortic root measured 3.2 × 3.4 cm and the ascending aorta measured 3.9 cm. She had no family history of aortic dissection or vascular disease.
Two additional variants of uncertain significance were identified in French individuals, p.Gly1317Cys (famFRA-001) and p.Cys1384Gly (famFRA-002). The variants are in the kinase domain of the protein, are highly conserved, predicted to be damaging by PolyPhen and have CADD scores of 23 and 34, respectively. These variants had insufficient data to support pathogenicity (see enzymatic assay results below) and therefore, the clinical data on these families were not included in the phenotypic analyses.
Analyses of aortic disease presentation in individuals with MYLK pathogenic variants
Only individuals with MYLK pathogenic variants were included for these analyses (Table 1). Nearly half were female (n=27) and all were of European descent. The mean age of the study population who are still living was 49 years (SD 21). The majority of study participants had variants leading to haploinsufficiency.
Table 1.
Demographic characteristics and MYLK variants of cases with and without aortic events.
| Variable | All (n=55) | With Aortic Events (n=23) |
Without Aortic Events (n=32) |
|---|---|---|---|
| Mean Age at last follow up (SD), yrs | 49 (21) | 53 (16) | 44 (21) |
| Mean age of death (SD), yrs | 67 (21) | 69 (14) | 55 (0)β |
| Sex | |||
| Men | 28 (51%) | 14 (47%) | 14 (53%) |
| Women | 27 (49%) | 9 (30%) | 18 (70%) |
| MYLK Mutations | |||
| p.S1759P | 7 (13%) | 4 (57%) | 3 (43%) |
| p.Y1575H | 5 (9%) | 4 (80%) | 1 (20%) |
| p.R1480* | 16 (29%) | 6 (38%) | 10 (62%) |
| p.T1096Qfs*38 | 9 (15%) | 1 (11%) | 8 (89%) |
| p.S1091* | 14 (25%) | 6 (43%) | 8 (57%) |
| p.E1066Nfs*10 | 1 (2%) | 1 (100%) | 0 |
| EX18_3'UTRdel | 3 (5%) | 1 (33%) | 2 (67%) |
100% of participants were European or European-American
Five individuals reported as sudden death with no autopsy report to confirm or deny aortic disease, were not included in this table
The mean is based on one individual who died as a result of cancer at the age of 55
Twenty-three individuals (38%) had experienced an aortic event, defined as aortic dissection or thoracic aortic repair (Table 2). Median age at aortic event was 48 years (IQR 42–70). Of these aortic events, 87% (20/23) were thoracic aortic dissections. Type A dissections were the most common (17/20, 85%), followed by type B dissection (3/20, 15%). Surgical repair of an aortic aneurysm was the presenting aortic event in 13% of individuals (3/23). The median age at the time of type A dissection was 48 years (IQR 44–70).
Table 2.
Disease Presentation of MYLK Mutation Carriers
| Variable | Frequency | Median age of onset in years (IQR) |
|---|---|---|
| Aortic event | 38% (23/60) | 48 (28) |
| Aortic dissection | 87% (20/23) | 51 (27.5) |
| Type A | 85% (17/20) | 48 (26) |
| Type B | 15% (3/20) | 56 (62) |
| Aneurysm repair | 13% (3/23) | 42 (31) |
| Without aortic event | 53% (32/60) | 39.5 (36.5) |
| Sudden death | 8% (5/60) | 61 (16) |
Aortic measurements (aortic root and/or ascending aorta) were available for 12 participants who experienced aortic events (Supplemental Table 1 and 2). In two individuals, ascending aortic measurements taken prior to aortic event were 3.9 cm and 5 cm with no mention of aortic root dilatation. Relevant to these data is the fact that studies indicate that the ascending aorta enlarges with a type A dissection, whereas the aortic root does not.11 Aortic root measurements at the time of dissection were normal in two cases (3.2 and 3.3 cm) but enlarged in one case (5.2 cm). Thus, the median aortic root diameter at the time of a type A dissection was 3.3 cm (IQR 2.0). The ascending aortic measurements in 5 individuals at the time of dissection were between 3.8 cm and 4.8 cm. One individual was noted to have progressive enlargement of his aortic root after repair of his ascending aortic dissection, and he underwent repair when it reached 4.8 cm. The median ascending aortic diameter in type A dissection was 4.25 (IQR 0.8). Of participants with no history of aortic event, 15 had aortic root and ascending aortic measurements available, and only one individual has an enlarged aorta, a 77 year old male null variant carrier with a 4.3 cm aortic root and 3.7 cm ascending aorta (Supplemental Table 2). Two of the individuals with type B dissections experienced complications, specifically paralysis and retrograde type A dissection and had no aortic root or ascending enlargement. Information on hypertension was available for 10 individuals with aortic dissections, and 50% were diagnosed with hypertension prior to their aortic event.
It is notable that 17 women known to carry pathogenic variants had a total of 48 pregnancies. Of the seven women who had aortic events, one woman, a 26 year old, had an aortic dissection associated with pregnancy (post-partum).
To determine if the type of MYLK pathogenic variant affected age at first aortic event, we assessed the median age of onset for null variant carriers, which 55.5 years (IQR = 27) versus 42 years (IQR = 15) in missense variant carriers (p=0.14). The median age at aortic event for MYLK mutation carriers was also not significantly different between males and females (p=0.97).
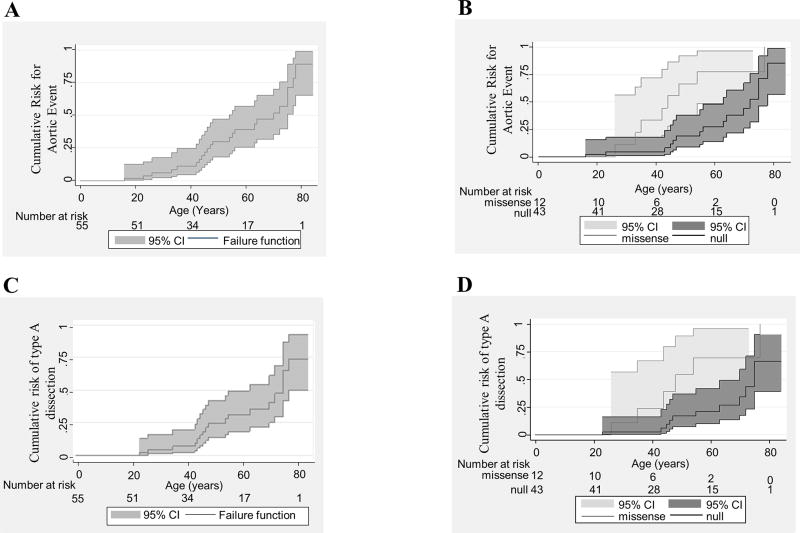
To further explore the variability of age of onset based on mutation type, Kaplan Meier analysis was done. For the entire MYLK population, the cumulative probability of aortic event showed the risk at 84 years of age to be 89% (95% CI 65, 99; Figure 2A) and 50% cumulative risk at the age of 70 years. Cumulative risk of aortic event in males and females showed no significant difference (chi2(1) = 0.51, p = 0.47;). However, stratification by type of mutation (missense vs. null) showed the probability of aortic event at an earlier age was significantly higher among missense mutation carriers ( , p = 0.01; Figure 2B). The same analyses restricted to just type A dissections showed similar results (Figure 2C and D).
Figure 2. Kaplan Meier Survival Analysis.
A. Kaplan Meier failure function evaluating cumulative risk of aortic event in persons with variants in MYLK. Individuals who died suddenly with no prior history of aortic event were not included in the analysis. B. Kaplan Meier curve demonstrating the significant difference in age of onset amongst individuals with missense mutations vs. null variants. Persons with missense variants in MYLK presented approximately 10 years earlier than those with null variants. C. Kaplan Meier failure function evaluating cumulative risk of type A aortic dissection in persons with MYLK variants. D. Kaplan Meier curve demonstrating significant difference in age of onset for type A dissection in individuals with missense versus null variants.
Myosin light chain kinase functional assays
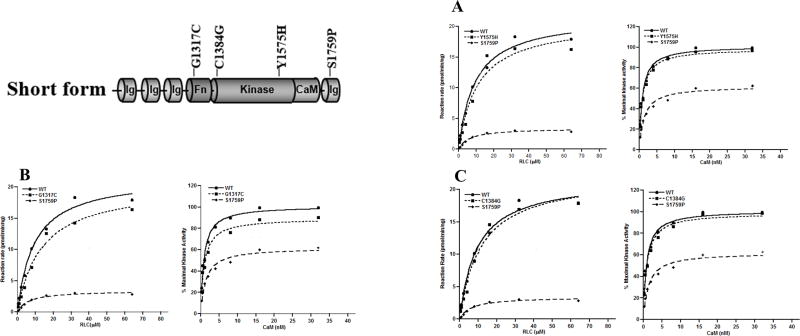
To determine if the missense variants disrupted MLCK kinase activity or activation of kinase activity with calmodulin binding, assays were completed on p.Tyr1575His, p.Gly1317Cys and p.Cys1384Gly (Figure 3). Surprisingly, p.Tyr1575His in famIT-001 showed only a 2% decrease in the kinase activity when compared to wild type kinase (p = 0.0004; Figure 3A). The p.Gly1317Cys mutant showed a 10% reduction in kinase activity and a 40% increase in CaM concentration was required for half-maximal activation (Figure 3B). Variant p.Cys1384Gly only showed a 2% decrease in kinase activity (Figure 3C). Based on these in vitro assays, none of these variants would be expected to decrease enzymatic activity to the extent of a previously reported mutation (p. Ser1759Pro). Therefore, we have classified only p.Tyr1575His as pathogenic based on segregation of the variant with aortic disease in the family and not on disruption of MLCK enzymatic function.
Figure 3. Functional assays of missense variants in MYLK.
The kinase activity and CaM activation of recombinant wild-type (WT) and mutant MLCK were assessed, and the results are shown along with previously published data on a variant shown to decrease MLCK activity, p.Ser1759Pro.4 The rate of 32P incorporation into the regulatory light chair (RLC) was measured. The maximal activities of WT MLCK (circle), variant MLCK (square), and Ser1759Pro MLCK (diamond) were obtained at different RLC concentrations. The three variants which were assessed: Tyr1575His (A), Gly1317Cys (B), and Cys1384Gly (C). The relative percentage of maximal kinase activity was plotted as a function of CaM concentration. The data points represented the mean ± standard error of three or more determinations. The data were fit to the Michaelis-Menten equation for estimation of the Vmax values and KCaM value.
DISCUSSION
Individuals with MYLK mutations present a unique challenge in terms of aortic disease management because a subset have minimal enlargement of the aortic root or ascending aorta at the time of a type A aortic dissection. Based on the data presented here, both the root and ascending aorta can enlarge in individuals with MYLK pathogenic variants. Therefore, imaging of the ascending aorta and aortic root should be part of disease management and both segments of the aorta should be repaired at the time of aortic surgery, even if the segment is not enlarged. After repair of a dissected ascending aorta, the aortic root can enlarge, therefore, imaging should be done to monitor the size of the aortic root. This study also determined that missense variants lead to higher risk and are likely to have an earlier onset of aortic events, specifically type A dissections, when compared to null variants. Interestingly, this finding is similar to COL3A1 variants in individuals with vascular Ehlers Danlos syndrome; null mutations carriers tend to present with a milder phenotype and vascular disease onset 10–15 years later than missense mutation carriers.12 MYLK mutation carriers have later onset and lower penetrance of aortic disease when compared to other HTAD genes, like TGFBR1, and TGFBR214.
Given that there may be no aortic enlargement prior to type A dissections, surgical intervention cannot be based solely on the diameter of the aorta. As more data becomes available, we propose adapting an alternate surgical timing model for cases with mutations in the MYLK gene, similar to that used for hereditary cancer populations. In individuals with BRCA1 or BRCA2 mutations, surgical recommendations are determined by the age at which the risk for breast or ovarian cancer increases significantly. For example, guidelines from the National Comprehensive Cancer Network recommend that women with BRCA1 mutations consider prophylactic bilateral salpingo-oophorectomy surgery between the ages of 35–40 years, or older if they have not finished having children, to reduce the risk of ovarian cancer 13. Similarly, individuals with mutations in MYLK should consider surgery based on the age at which risk for dissection increases significantly and not solely based on aortic diameter. Based on our data, individuals with haploinsufficiency variants are a minimal risk for a type A dissection before the age of 40 years; data are limited for missense variants but onset of type A dissection is earlier in these cases. Physicians and surgeons should consider discussing prophylactic surgical repair of the ascending aorta and aortic root to prevent dissections with their patients based both on underlying mutation and the age at which the risk for dissection increases. Given the variability of surgical outcomes between institutions, we recommend that carriers of pathogenic variants in MYLK consider surgery at a tertiary care center with experience in surgical management of hereditary aortic disease in order to minimize risk of unfavorable outcomes. Blood pressure should be well controlled and treatment with β-adrenergic blocking agents be considered even in the absence of hypertension.
The MYLK p.Tyr1575His variant segregates with disease in distantly related branches of family IT-001 with a LOD score of 4 and is absent in the ExAC database, and therefore is classified as a pathogenic variant. It was surprising that functional assays of this variant showed only a minimal decrease in kinase activity, most likely not sufficient to cause disease. These findings emphasize the fact that established functional assays do not always correlate with the pathogenicity of variants. In the long form of MLCK, which is responsible for RLC phosphorylation in non-muscle cells, the cellular localization and regulation of MLCK is dependent on phosphorylation of tyrosines in the unique N-terminal domain of the protein15,16. Therefore, future studies to determine how MYLK p.Tyr1575His predisposes to disease should focus on whether phosphorylation of this tyrosine plays a role in kinase activation in smooth muscle cells. Finally, the difference in the Kaplan Meier time to aortic event curves between missense and haploinsufficiency MYLK variants raises the possibility that missense MYLK pathogenic variants lead to a dominant negative effect that disrupts protein function to a greater degree than null variants. Further functional analyses of co-expressed wildtype and mutant MLCK proteins will be necessary to determine whether missense variants can disrupt the function of the wildtype protein.
Type B aortic dissection cause life-threatening complications in 25% of cases, including malperfusion leading to paraplegia, periaortic hematoma, and hemorrhagic pleural effusion17. Interestingly, amongst this study population of cases with MYLK pathogenic variants, all individuals with type B dissections experienced life-threatening complications, including retrograde dissection with TEVAR placement and rupture of the descending aorta. It is also interesting to note that two individuals undergoing surgery of the descending aorta were noted to have fragile aortic tissue.
It is important to note that these recommendations are based on data from a small population of mutation carriers and represent patients who presented for genetic evaluation due to early onset of aortic dissection or family history of aortic disease. Thus, these cases may reflect the more severe end of the disease spectrum in carriers of MYLK variants. Skewing of early data on the phenotype associated with novel genes towards more severe phenotypes occurs, including the early publications on disease presentation in patients with mutations in TGFBR1, TGFBR2, BRCA1 or BRCA2.14,18,19 However, the information provided by these cases provides valuable insight into the presentation of the disease and can be used to inform decision-making in terms of timing of aortic surgical repair.
In summary, these data define the aortic disease presentation associated with MYLK mutation, both in terms of aortic disease risk associated with different types of mutations and the associated aortic presentations and complications. Our data suggest that the size of the aorta may not be a useful marker of risk of dissection since many of the individuals in this study dissection at small aortic diameters. Additional markers of aortic instability should be taken into account in decisions concerning the timing of aortic repair, including probability of aortic dissections based on the patient’s age and type of mutation. Studies involving a larger cohort of patients with MYLK variants are needed to improve the precision of these risk estimates and confirm earlier dissections for all missense pathogenic variants. Furthermore, the present data indicate that additional studies are needed to determine why MYLK heterozygous missense variants with essentially normal disrupt kinase activity can nevertheless cause disease.
Supplementary Material
Acknowledgments
The authors are grateful to the patients and families for their participation in this study.
SOURCES OF FUNDING
The following provided funding for this study: National Institutes for Health (RO1 HL62594 and P01HL110869-01), the John Ritter Research Foundation, Genetic Aortic Disorders Association of Canada, and the Temerty Family Fund (all to D.M.M.).
Footnotes
DISCLOSURES
Tami Johnston and Christian Antolik are employed by a commercial testing laboratory, Ambry Genetics.
References
- 1.Guo DC, Pannu H, Papke CL, et al. Mutations in smooth muscle alpha-actin(ACTA2) lead to thoracic aortic aneurysms and dissections. Nat Genet. 2007;39:1488–93. doi: 10.1038/ng.2007.6. [DOI] [PubMed] [Google Scholar]
- 2.Disabella E, Grasso M, Gambarin FI, et al. Risk of dissection in thoracic aneurysms associated with mutations of smooth muscle alpha-actin 2(ACTA2) Heart. 2011;97(4):321–6. doi: 10.1136/hrt.2010.204388. [DOI] [PubMed] [Google Scholar]
- 3.Guo DC, Regalado E, Casteel DE, et al. Recurrent Gain-of-Function Mutation in PRKG1 Causes Thoracic Aortic Aneurysms and Acute Aortic Dissections. Am J Hum Genet. 2013;93:398–404. doi: 10.1016/j.ajhg.2013.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang L, Guo DC, Cao J, et al. Mutations in Myosin light chain kinase cause familial aortic dissections. Am J Hum Genet. 2010;87:701–7. doi: 10.1016/j.ajhg.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pannu H, Tran-Fadulu V, Papke CL, et al. MYH11 mutations result in a distinct vascular pathology driven by insulin-like growth factor 1 and angiotensin II. Hum Mol Genet. 2007;16:3453–62. doi: 10.1093/hmg/ddm201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gao N, Huang J, He W, et al. Signaling through myosin light chain kinase in smooth muscles. J Biol Chem. 2013;288:7596–605. doi: 10.1074/jbc.M112.427112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luyckx I, Proost D, Hendriks JM, et al. Two novel MYLK nonsense mutations causing thoracic aortic aneurysms/dissections in patients without apparent family history. Clin Genet. 2017 doi: 10.1111/cge.13000. [DOI] [PubMed] [Google Scholar]
- 8.Hannuksela M, Stattin EL, Klar J, et al. A novel variant in MYLK causes thoracic aortic dissections: genotypic and phenotypic description. BMC Med Genet. 2016;17:61. doi: 10.1186/s12881-016-0326-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ziganshin BA, Bailey AE, Coons C, et al. Routine Genetic Testing for Thoracic Aortic Aneurysm and Dissection in a Clinical Setting. Ann Thorac Surg. 2015;100:1604–11. doi: 10.1016/j.athoracsur.2015.04.106. [DOI] [PubMed] [Google Scholar]
- 10.Silberstein M, Tzemach A, Dovgolevsky N, et al. Online system for faster multipoint linkage analysis via parallel execution on thousands of personal computers. Am J Hum Genet. 2006;78:922–35. doi: 10.1086/504158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rylski B, Blanke P, Beyersdorf F, et al. How does the ascending aorta geometry change when it dissects? J Am Coll Cardiol. 2014;63:1311–9. doi: 10.1016/j.jacc.2013.12.028. [DOI] [PubMed] [Google Scholar]
- 12.Leistritz DF, Pepin MG, Schwarze U, et al. COL3A1 haploinsufficiency results in a variety of Ehlers-Danlos syndrome type IV with delayed onset of complications and longer life expectancy. Genet Med. 2011;13:717–22. doi: 10.1097/GIM.0b013e3182180c89. [DOI] [PubMed] [Google Scholar]
- 13.National Comprehensive Cancer Network. NCCN Guidelines Version 2.2017: BRCA-Related Breast and/or Ovarian Syndrome. 2017 [Google Scholar]
- 14.Jondeau G, Ropers J, Reglado E, et al. International Registry of Patients Carrying TGFBR1 or TGFBR2 Mutations: Results of the MAC(Montalcino Aortic Consortium) Circ Cardiovasc Genet. 2016;9:548–48. doi: 10.1161/CIRCGENETICS.116.001485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang T, Brown M, Kelly G, et al. Myosin light chain kinase(MYLK) coding polymorphisms modulate human lung endothelial cell barrier responses via altered tyrosine phosphorylation, spatial localization and lamellipodial protrusions. Puml Cir. 2018 doi: 10.1177/2045894018764171. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dudek SM, Chiang ET, Camp SM, et al. Abl tyrosine kinase phosphorylates nonmuscle Myosin light chain kinase to regulate endothelial barrier function. Mol Biol Cell. 2010;21:4042–56. doi: 10.1091/mbc.E09-10-0876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel AY, Eagle KA, Vaishnava P. Acute type B aortic dissection: insights from the International Registry of Acute Aortic Dissection. Ann Cardiothorac Surg. 2014;3:368–74. doi: 10.3978/j.issn.2225-319X.2014.07.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Loeys BL, Schwarze U, Holm T, et al. Aneurysm syndromes caused by mutations in the TGF-beta receptor. N Engl J Med. 2006;355:788–98. doi: 10.1056/NEJMoa055695. [DOI] [PubMed] [Google Scholar]
- 19.Narod S, Lynch H, Conway T, et al. Increasing incidence of breast cancer in family with BRCA1 mutation. Lancet. 1993;341:1101–2. doi: 10.1016/0140-6736(93)92468-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.