Abstract
SUMMARY – Recent developments in the diagnosis and treatment of chronic lymphocytic leukemia (B-CLL) have led to change of approach in clinical practice. New treatments have been approved based on the results of randomized multicenter trials for first line and for salvage therapy, and the results of numerous ongoing clinical trials are permanently providing new answers and further refining of therapeutic strategies. This is paralleled by substantial increase in understanding the disease genetics due to major advances in the next generation sequencing (NGS) technology. We define current position of the Croatian Cooperative Group for Hematologic Disease on diagnosis and treatment of CLL in the transition from chemo-immunotherapy paradigm into a new one that is based on new diagnostic stratification and unprecedented therapeutic results of B-cell receptor inhibitors (BRI) and Bcl-2 antagonists. This is a rapidly evolving field as a great number of ongoing clinical trials constantly accumulate and provide new knowledge. We believe that novel therapy research including genomic diagnosis is likely to offer new options that will eventually lead to time limited therapies without chemotherapy and more effective clinical care for B-CLL based on individualized precision medicine.
Key words: Chronic lymphocytic leukemia, Practice guidelines as topic, Precision medicine, Croatia, KROHEM*
Introduction and definition
In recent years, dramatic change in therapeutic landscape led to unprecedented therapeutic results that were translated to clinical practice, and after years of slow to modest progress in the field of B-cell chronic lymphocytic leukemia (B-CLL), the American Society of Clinical Oncology (ASCO) named transformation of CLL treatment Cancer Advance of the Year for 2015 (1). New treatments were approved based on the results of randomized multicenter trials for first line and for salvage therapy, and the results of numerous ongoing clinical trials are permanently providing new answers and further refining of therapeutic strategies. This is paralleled by substantial increase in understanding the disease genetics owing to major advances in the next generation sequencing (NGS) technology (2, 3). All these have led to change of the until now predominant paradigm based on chemo-immunotherapy (CIT) to a new one (4, 5).
Definition. B-cell chronic lymphocytic leukemia and related disorders (monoclonal B-lymphocytosis (MBL) and small lymphocytic lymphoma (SLL)) are defined by the presence of clonal mature B-lymphocytes with typical immunophenotype in peripheral blood, bone marrow and lymphoid organs (WHO, iwCLL) (6, 7) representing one nosologic entity. Today, it is considered that these entities are different manifestations of the same disease. MBL is most prevalent and is considered as an early stage of malignancy progressing to CLL/SLL in 1%-2% of cases per year. SLL accounts for less than 10% of overt malignancy, and for this reason B-CLL is most commonly used to represent both variants (CLL/SLL) (6, 8-17).
Epidemiology. B-CLL is the most common type of leukemia in Western countries. The incidence is estimated to more than 6 per 100,000 people annually. The median age at diagnosis is growing globally, so that now exceeds 70 years. It should be noted that the age at treatment initiation is several years older than the age at diagnosis, depending on the duration of observation without treatment. The disease is nearly twice as common in men (18-22). The incidence and prevalence of MBL is much higher, depends on sensitivity of the methods used, and is estimated to involve up to 12% of the population aged over 40 years (23, 24).
Diagnostic procedure
The diagnostic process can be conditionally divided into several sections (steps, phases) with respect to different objectives to be achieved. In Table 1, the basis for decision is specified, along with the main criteria for classification and the possible categories to which the classification in this section should lead.
Table 1. Steps and aims in diagnostic process that leads to definition of therapeutic goal and strategy.
| STEPS AND AIMS | BASIS FOR DECISION | CRITERIA | TARGETED CATEGORIES OF CLASSIFICATION | |
|---|---|---|---|---|
| 1 | Disease detection; Patient – hematologist contact |
• Lymphocytosis (70%-80%) and/or • Lymph nodes/spleen enlargement (20%-30%) |
• PE and hematology lab | |
| 2 | Diagnosis and differential diagnosis | • B-cell clone of typical B-CLL phenotype (in PB and/or BM and/or LN) • Other lymphoproliferative disease with lymphocytosis |
• Morphology + characteristic immuno-phenoptype with quantifications • Difference in phenotype and/or morphology |
• CLL (73%) • SLL (7%) • MBL • B (15%): FL, MCL, MZL, PLL, HCL • T (5%): PLL, TLLO, Sezary, LGL |
| 3 | Disease extent assessment | • Clinical and lab (hematology) assessment | • Rai, • Binet, • TTM |
• 0, I, II, III, IV • A, B, C • Continuous parameter of the size and distribution of tumor mass |
| 4 | Classification in prognostic groups | • PFs @ dg | • Prognostic markers (CD38 and ZAP), FISH(4), • Prognostic indices, • Mutation status of IgHV genes |
• Good prognosis • Poor prognosis |
| 5 | Indications for therapy | • Quantitative threshold criteria • Dynamic criteria • Qualitative criteria |
• Anemia, thrombocytopenia, organomegaly, lymphocytosis • Trend of tumor load increase (DT), progressive cytopenias • Presence of symptoms |
• Early, stable, asymptomatic disease = observation only • Any other = indication for therapy |
| 6 | Immediate pre-treatment evaluation and comorbidity & general condition assessment | • Clinical and laboratory assessment | • Updating and completing work-up • CIRS |
• Fit • Unfit |
| 7 | Individualization of therapy Therapy aim and strategy definition |
• B-CLL related factors • Patient related factors |
• Difference in advancement and progressiveness, p53 • General condition and comorbidity |
Stratification (2x2): • High risk/Low risk • Fit/Unfit (frail) |
Comment: the table shows diagnostic steps. Steps 1-4 are made in single visit. Each step is different with respect to aim, decision criteria, and the extent of work-up. Last column describes classification categories proposed. Only about 10% of patients have indication for therapy at diagnosis. Others are followed-up repeatedly until the criteria for therapy are reached (step 5). The scope of work-up is different in each step, pretreatment evaluation being most complete, aiming to provide all the necessary elements for patient stratification and definition of therapeutic goal. The overall goal of diagnostic process is to enable individualization of therapy, definition of therapeutic aim and strategy, by implementing general principles to each individual case.
Setting suspicion and patient referral to hematologist
The most common finding leading to suspicion of B-CLL is absolute lymphocytosis in routine blood examination (70%-80%), and less frequently (20%-30%) the finding of organomegaly (swollen lymph nodes and/or spleen) or symptoms associated with CLL.
Diagnosis and differential diagnosis
It is mandatory to make the diagnosis of typical B-CLL on the basis of morphology and flow cytometry in peripheral blood sample and to distinguish it from other entities in the CLL syndrome. For the diagnosis of B-CLL phenotype (typical phenotype), the following is required: restriction of sIg light-chain expression of low intensity, CD5+, CD19+, CD20low, CD23+ (25). Basic hematologic clinical findings and blood count allow for quantification of the tumor mass in peripheral blood and lymphoid organs, which enables classification of entities that meet the diagnostic criteria for:
B-CLL (presence in the blood of more than 5x109/L clonal cells), or
SLL (less than 5x109/L clonal cells in the blood and clonal lymphadenopathy greater than 1.5 cm), and
MBL (less than 5x109/L clonal cells in the blood and no clonal lymphadenopathy or symptoms).
So, a different size of the tumor mass between B-CLL and MBL is critical and tumor distribution is critical for distinction between B-CLL and SLL.
It is evident that for the diagnosis of disease type, a very small number of tests could be considered sufficient because if the result is positive in peripheral blood (PB), it is not necessary to analyze bone marrow (BM) or lymph nodes (LN), although these tests have their place in further diagnostic work-up. For the diagnosis of SLL, it is recommended to make lymph node biopsy to establish the diagnosis, and radiological assessment (ultrasound (US) or computed tomography (CT)) of the neck, thorax, abdomen and pelvis can be useful to distinguish between MBL and SLL.
Other B-cell malignancies that can be accompanied by increased lymphoid cell counts in the blood should be taken in consideration in differential diagnosis. Distinction to CLL is usually made by flow cytometry assessed immune phenotype. The majority are B-cell malignancies such as follicular lymphoma (FL), mantle cell lymphoma (MCL), marginal zone lymphoma (MZL), prolymphocytic leukemia (PLL) and hairy cell leukemia (HCL), which all together represent less than 15% of all lymphoid appearing leukocytoses, and less than 5% express T-cell lineage marker variants.
It should be remembered that this type of disorder classification based only on the immune phenotype is not using morphological, cytogenetic, molecular, or other characteristics of the diseases that today show significant association with prognosis.
Evaluation of the stage/extent of the disease
After the diagnosis, the next step is evaluation of the disease stage or extent. It is based on clinical and hematologic evaluation, under the criteria shown in Table 2. Clinical stages represent a simple tool for clinical assessment of the disease extent. The basis of these systems is the assumption that the disease is gradually progressing and expanding. Therefore, the patients who have advanced disease have a higher tumor load and more extensive disease (26-28).
Table 2. Clinical stages and TTM.
| Rai stages | |||
|---|---|---|---|
| STAGE | DESCRIPTION | RISK | |
| 0 | Lymphocytosis, in peripheral blood >15x109/L and >40% in bone marrow | Low | |
| I | Stage 0 with enlarged lymph node (nodes) | Intermediate | |
| II | Stage 0-I with splenomegaly, hepatomegaly or both | Intermediate | |
| III* | Stage 0-II with hemoglobin <110 g/L | High | |
| IV* | Stage 0-III with platelets <100x109/L | High | |
| * immune cytopenias do not fit in this stage definition | |||
| Binet stages | |||
| STAGE | DESCRIPTION | RISK | |
| A | Hemoglobin ≥100 g/L and platelets ≥100x109/L and <3 involved regions** | Low | |
| B | Hemoglobin ≥100g/L and platelets ≥100x109/L and ≥3 involved regions | Intermediate | |
| C* | Hemoglobin <100g/L and/or platelets <100x109/L and any number of involved regions | High | |
| ** immune cytopenias do not fit in this stage definition ** the five lymphoid areas comprise uni- or bilateral cervical, axillary and inguinal lymphoid, hepatomegaly and splenomegaly | |||
| TTM-score | |||
| COMPARTMENT | REPRESENTATIVE | SIZE | RISK |
| TM1 - BM and PB | Lymphocyte count (peripheral blood) | 9 Low | |
| TM2 - Ly nodes | Diameter of largest palpable node | cm | 9-15 Intermed |
| TM3 - spleen | Palpable spleen (below left costal margin) | cm | >15 High |
| TTM | TM1+TM2+TM3 | Continuous variable | |
| |ly| = absolute number of lymphocytes; TTM = Total Tumor Mass score Note: if the largest lymph node is found by imaging (US or CT), those values should be used for TM2 | |||
| Tumor Mass Distribution (TD) is calculated as quantitative parameter according to formula: TD = . Doubling Time of TTM (DT) is calculated as quantitative parameter according to formula: DT =, where TTMbeg is the size of TTM at the beginning of period M: TTMend is TTM size at the end of period M; M is interval between TTMbeg and TTMend in months. M should be at least 3 months. Electronic calculator available online at: http://www.krohem.hr | |||
The clinical stages according to Rai and Binet assess tumor size by simple parameters, which estimate the size of the tumor mass (without precise quantification of the affected compartments), along with the parameters for the assessment of bone marrow failure. In doing so, the greatest prognostic power contribution has the failure of bone marrow. Note that it is not a direct but an indirect sign of tumor size. Their prognostic power is relatively weak if the failure of the bone marrow is excluded.
The estimation of the size of the Total Tumor Mass (TTM) is different in that it quantitatively evaluates tumor mass in 3 major cell compartments, regardless of bone marrow failure (Table 2). Quantitative character enables unbiased monitoring of disease progression and is a very convenient tool for the assessment of therapeutic response (see later). In addition, in most patients who have both peripheral blood and lymphoid organs affected, it is possible to determine the type of distribution of the tumor mass by comparing leukemic (TM1) and lymphoid organ (TM2 +TM3) compartments (29). This feature of TTM system enables to estimate the dynamics of disease progression and response to therapy and redistribution (see later) (30).
Prognostic factors at diagnosis and predictors of response
Analyses of prognostic factors performed in the era when therapy had little effect on clinical course identified a number of clinical or laboratory factors (31), describing broadly the natural course of the disease. Prognostic factors that can be determined immediately at diagnosis are primarily related to the additional characterization of the tumor itself. Some of them do not change during evolution of the disease, such as the mutational status of IgVH genes that generally discriminate between more benign and more malignant disease (32-34), and it is currently suggested to become minimal standard initial evaluation (31). Until now, these were rarely used in routine clinical practice and other tests showing high correlation with mutational status are used instead, such as CD38 and ZAP-70 by flow cytometry and immunohistochemistry, with the higher value found to correlate with poorer prognosis (35-44). The usefulness of these surrogate factors is still controversial. In contrast, cytogenetic and molecular tests (FISH) to determine del (11q22-23), +12; del (13q14), del (17p13) (45) showed a strong independent prognostic effect and usually change (progress) over time. Also, finding certain mutations (including TP53, SF3B1, NOTCH1, etc.) (46, 47) can complement these findings. These tests are good predictors of response in the chemo-immunotherapy era and have proven to be useful to stratify patients into groups that react differently to certain drugs (4, 48). Since they may change during the course of disease, testing must be performed just before each new line of therapy. All these tests that further characterize neoplastic clone cells are technically demanding and expensive, but relatively inexpensive compared to drugs, and for those validated the cost and effort are justified. Predictive factors seem to change or even lose their predictive power with novel treatments. Likewise, failure to new treatments will require discovery of new predictors.
On the other hand, a number of additional factors more related to patient’s state also have a strong prognostic power, so a number of different parameters is often used, and multivariate analyses are performed to study their impact on prognosis (49).
Because of the above, we distinguish three types of factors, given the causal relationship with B-CLL. First, those that are associated with B-CLL clonal neoplastic diseases (size distribution, growth rate of tumors, mutational status, CD38, ZAP-70, FISH) may be used as predictors of response to therapy, etc. (28, 32, 33, 45, 50-52). Also, numerous other characteristics such as blood chemistry (serum beta2 microglobulin, sCD23 and serum thymidine kinase (53-55)), clonogenic (56), kinetic, and computer assisted cell imaging have been shown to be related to prognosis (57, 58); second, those that are associated with organ failure (mixed groups, they may be due to both very underlying neoplastic diseases and to consequences of associated diseases, such as anemia, thrombocytopenia, the etiology of which should be carefully evaluated); and third, those factors that are associated with the patient but not directly with the neoplasm (age, gender, performance status, comorbidity), that correlate with fitness and the ability to tolerate aggressive treatments (40, 59-62).
On the basis of strong independent predictors, composite prognostic indices are calculated (63-65), most recently the CLL International Prognostic Index (IPI) (66). They show very good prognostic power with respect to the length of survival in the chemo-immunotherapy (CIT) era, but much less so with new treatments. Also, one should be careful using them to stratify patients for treatment that is adapted to risk because a composite index usually consists of the factors that belong to each of the three above mentioned groups.
With new, more effective therapies, the prognostic landscape changes. Most of the important predictors in the CIT era lose their power, and new ones are yet to be identified (4, 48).
Indications for treatment/the criteria for therapy initiation
The criteria for active disease that warrant initiation of treatment are based on iwCLL criteria, and are amended with TTM (Table 3). The decision should be based solely on the assessment of parameters that are associated with neoplastic B-CLL clone (6). For parameters that may be unrelated to the neoplasm, it is necessary to carefully evaluate the extent to which the parameters are associated with neoplastic clone (e.g., fever, anemia, etc.). Criterion parameters can be classified into three distinct types:
Table 3. Criteria for active (progressive/symptomatic) disease.
| CRITERION | THRESHOLD | DYNAMICS | QUALITATIVE | COMMENT | |
|---|---|---|---|---|---|
| 1 | Hemoglobin | <100 g/L | Trend (worsening) | The level of anemia that is used in determining clinical stages according to Rai and Binet. | |
| 2 | Platelets | <100x109/L | Trend (worsening) |
The level of thrombocytopenia that is used in determining clinical stages according to Rai and Binet. | |
| 3 | High tumor mass | TTM >15 | TTM DT <12 mo | Below 9 is not a sufficient criterion, between 9 and 15 is a ‘gray zone’, above 15 is an indication present. Lymphocyte count in itself is not a sufficient criterion, except for extreme cases (TTM >15 = lymphocytes >225x109/L) |
|
| 4 | Massive splenomegaly | >6 cm below LCM or US >20 cm |
(progressive) | Pain | Usually they are combined, but not necessarily. Dynamic parameters involved in TTM |
| 5 | Massive lymph nodes | >10 cm | (progressive) | Pain | Usually they are combined, but not necessarily. Dynamic parameters involved in TTM |
| 6 | Threat to organ function | Clinical judgment | For example, compressive symptoms | ||
| 7 | B symptoms defined as any one or more of the disease-related symptoms or signs: | Unintentional weight loss >10%/6 months; or Significant fatigue (ECOG PS 2 or worse); or Fever >38 oC for 2 or more weeks without evidence of infection; or Night sweats for more than 1 month without evidence of infection |
Usually they are combined, but not necessarily. The proposed system has long been used, particularly in lymphomas, and is well validated. The presence of B-symptoms is an important and indisputable element of therapeutic indications. It suffices that one is present, but there may be several present simultaneously. | ||
| 8 | Autoimmune anemia or thrombocytopenia | Poorly responsive to standard therapy | Standard therapy does not imply anticancer drugs, but includes corticoids |
Hypogammaglobulinemia, monoclonal or oligoclonal paraproteinemia, or absolute lymphocyte count do not by themselves constitute an indication for therapy. It is out of 8 groups of criteria theoretically possible to identify 11 individual indications based on exceeding a threshold, 3 dynamic evaluation of continuous quantitative parameters, where individual trends can be compared and thereby gain additional derived criteria, and 4 qualitative assessments. Although in principle the presence of at least one indication is sufficient, we should avoid making decisions on an isolated indication. It is clear that a larger number of indications further reinforces the decision to begin treatment. It is possible to decide that the patient needs to document the presence of at least two or more of the above indications for active (progressive/symptomatic) disease. The indication for treatment (according to KROHEM guidance) should be documented in patient records!
Quantitative parameters for which threshold consensus is defined, which is considered to justify treatment initiation, such as anemia, defined by a certain level of hemoglobin, thrombocytopenia defined by platelet count, organomegaly defined by the size of spleen or lymph nodes.
Monitoring data to enable assessment of trends, for example, progressive cytopenia, progressive lymphadenopathy and/or splenomegaly, increased leukocyte count or TTM values (see the previous section). It should be emphasized that only measurement of dynamic parameters can directly evaluate progression of the disease, as opposed to the a priori estimate of a possible evolution described in the previous section (see Prognostic features at diagnosis section). Here, however, we should point out certain difficulties and ambiguities in quantitative measurement of the dynamic parameters, especially in the early stages of the disease. This imprecision in a priori definition of the criteria for progressiveness, despite a very attractive concept, often leads to decision delay until the moment when it reaches the absolute value of the threshold that is set up as described above.
Qualitative criteria of the occurrence of symptoms threatening organ damage and the like, considered to be the result of neoplastic disease activity.
Today, we seek to combine threshold criteria with dynamic criteria (see Table 7). Note that a number of criteria, the criteria of threshold, dynamics and qualitative changes may be used. Although it is sufficient to indicate treatment by the presence of only one of the stipulated criteria, it is important that this criterion is compelling, and the presence of multiple criteria makes decision certainly easier. It especially holds for dynamic criteria, so it is good to compare the growth trend of the tumor mass with the trends of deepening anemia and/or thrombocytopenia. The indication for treatment (according to KROHEM guidance) should be documented in patient records.
Table 7. Treatment of relapsed/refractory CLL (KROHEM v1 2017).
| Relapse | % a | Molecular cytogenetics | % | General condition | % | Salvage treatment | ||
|---|---|---|---|---|---|---|---|---|
| Standard b,c | Extended / Maintenance | |||||||
| Early (<2 years) Refractory disease (<1 year) |
30 | No del(17p) / TP53mut | 22 | Fit | 7 | Ibrutinib (1) Idelalisib + R (1) Venetoclax (1)c HDMP + R Ofa |
FCR d B+R d F + A e |
→AlloSCT →antiCD20 g |
| Unfit | 15 | B + R Chl + antiCD20 d |
→antiCD20 g | |||||
| Del(17p) / TP53mut | 8 | Fit & Unfit |
8 | Ibrutinib (1) Idelalisib + R (1) Venetoclax (1)f HDMP + R A e ± R |
→AlloSCT (fit) →antiCD20 g |
|||
| Late (>2 years) | 70 | 70 | Fit & Unfit |
Repeat first line (or choose from above) | ||||
The guidelines for salvage treatment are more complex than in first-line treatment. It should take into consideration additional criteria depending on the type of treatment in first line, and on the observed duration of response. Clinical trials are highly recommended for all subsets and we strongly believe that they improve the level of care.
a Projected percentages of early and late relapses are based on Dubrava University Hospital data for 2015 and 2016. Percentages of unfit patients and patients with del(17p) tend to increase. Fit patients = less than 65 years of age and with CIRS score less than 6. Younger patients with CIRS score of 6 and more and patients aged 65 years or more qualify as unfit;
b Standard treatments are in order of preference, but for each individual patient should be based on integration of clinical data and patient preference. All treatments are 2A according to NCCN consensus, treatments with higher grade or lower grade are marked;
c In patients who are unsuitable for or have failed a B-cell receptor pathway inhibitor and chemo-immunotherapy;
d If not in 1st line;
e Alemtuzumab is withdrawn from market, but can be obtained free of charge from producer upon request;
fIn patients who are unsuitable for or have failed a B-cell receptor pathway inhibitor;
g Ofatumumab is found to significantly prolong PFS in responsive patients in second or third response to chemo-immunotherapy, approved by FDA.
FCR (fludarabine, cyclophosphamide and R); B = bendamustine; Chl = chlorambucil; R = rituximab; Obi = obinutuzumab; Ofa = ofatumumab; A = alemtuzumab; Allo SCT = allogeneic stem cell transplantation; HDMP (high dose methylprednisolone); antiCD20 (ofatumumab or obinutuzumab or rituximab).
The schedule of activities and assessments
Table 4 shows the general scheme of tests that are used in pretreatment work-up, in therapy monitoring, and after therapy. Of the newly diagnosed CLL patients, about 10% require therapy immediately, so the pretreatment work-up is done immediately at diagnosis and visits 1-3 are completed without delay. Other patients (90% of all diagnosed) are observed after diagnosis at periodic visits until meeting the criteria for initiation of treatment. At that point, complete pretreatment work-up is performed. About 30% of all diagnosed patients never reach the criteria for initiation of treatment, while about 60% of all diagnosed patients reach the criteria, but in different periods, from several months to more than 10 years.
Table 4. General schedule of investigations before, during and after therapy.
| Visits?→ | 1 | 2* | 3 | 4** | 5 | (2’→3’) (4’,5’) | |
|---|---|---|---|---|---|---|---|
| Investigations ↓ |
@ dg | Monitoring to meet criteria for treatment | Pre-th work-up | Th monitoring | EOT evaluation | After therapy repeat 2’-5’ before new line (3’) |
|
| a | History/PE | + | + | + | + | + | + |
| b | Hematology | + | + | + | + | + | + |
| c | TTM/stage | + | + | + | + | + | + |
| d | Flow cytometry | + | + | + | + | ||
| e | FISH CLL(4)/ Molecular |
+b | + | + | |||
| f | Cyto/Histo | +b | + | + | + | ||
| i | Imaging | + | + | + | |||
| j | Otherclin ind | + | + | + | + | + | + |
| k | Research b | + | + | + | + | + | + |
*Monitoring protocol frequency varies depending on clinical condition from several weeks to several months, or even one year if the situation is stable, without change. However, in the emergence of new circumstances, it is necessary to check-up early; **these repetitive visits depend on treatment applied. For novel agents with at present unlimited duration, these visits should enable detection of treatment failure; bpreferred but not required tests.
It is possible to distinguish several specific clinical questions that need to be answered in stipulated visits and require different extent of investigations. These questions are answered in the following visits: (1) diagnosis, differential diagnosis, evaluation of the extent of disease, and preferably but not mandatory, assessment of prognostic groups that require investigations (a-f). At this time, it is recommended to evaluate general health profile (j); (2) repetitive visits monitoring clinical and hematologic parameters that serve as criteria for initiation of treatment, based on simple parameters (investigations a, b, c, j). The time between the visits may vary from weeks to months; (3) immediate pre-therapeutic work-up provides definite classification of the disease, definitive assessment of prognostic parameters, as well as the general state of the patient, and any associated illnesses including infection status. For this reason, this visit should be most complete, enabling stratification and providing baseline parameters for treatment; (4) these repetitive visits to monitor the course of therapy should be tailored according to the needs of respective therapy; and (5) end of therapy (EOT) visit should enable evaluation of the response achieved. After that, for CIT that is time limited, monitoring visits without therapy (2’) are repeated again and in case of the need for a new line of therapy, repeat visits 3’, 4’ and 5’ are scheduled. The situation is different for novel agents since this treatment is at present unlimited and visits 4 should enable detection of treatment failure.
Therapy individualization – defining goals and strategies, and stratifying patients
At the end of diagnostic procedure described above, there is a need to make decision on therapy, which will reflect individualization of the respective patient. Decision is based on the integration of the factors related to the neoplasm on the one hand and the factors related to the patient on the other hand. According to new circumstances and new emerging paradigm because of the lack of curative treatment, initial therapy should maximize efficacy while minimizing overall toxicity. The overall approach is essentially based on clinical judgment and the expertise.
In general, we are comparing two risks: the risk of disease and the risk of treatment. It is clear that the risk of treatment should be reasonably lower than the risk of disease.
The risk of disease. Some treatments have been shown to be inefficient in some disease subsets. However, novel treatments are also active in those subsets, which will diminish the importance of stratification according to FISH and TP53, which was necessary until now. Nevertheless, since CIT has proved very effective in some subsets of patients and contraindicated in others, the classification according to risk should remain until head-to-head comparisons resolve pending questions.
The risk of therapy, i.e. tolerance (or acute treatment toxicity) is highly dependent on the general condition of the patient and the presence of associated diseases, which is often associated (though not exclusively) with the patient’s age. However, treatments with new B-cell receptor inhibitors (BRI) have much better toxicity profile that diminishes the importance of stratification according to fitness, which was necessary in the chemo-immunotherapy based paradigm. Nevertheless, for the same reason as described above, this stratification should remain for CIT. Since CIT is not indicated in patients with del(17p)/TP53 mutation, the distinction between fit and unfit becomes irrelevant.
A patient is classified as capable (fit, Go Go) when there is a low comorbidity score (e.g., CIRS-G <6). Although age does not enter in the calculation of CIRS-G, it is known that age is a very important factor and it should be taken into account. It is common to impose an age limit for stratification in therapeutic groups. Today, the limit is set at 65 years. Patients aged over 65 can be considered capable for receiving aggressive therapy if in excellent health, without substantial comorbidity.
On the basis of the two above-mentioned principles, patients are today stratified into three strata with respect to antineoplastic therapy: (1) without the p53 gene deletion with good general condition (capable for aggressive, fludarabin based CIT therapy) – (LOW RISK + FIT), (2) without the p53 gene deletions with poor general condition (incapable for aggressive therapy) – (LOW RISK + UNFIT), and (3) deletion of (17p)/TP 53 mutation (HIGH RISK + FIT/UNFIT). For those patients, no further division according to fitness is necessary, since the new approved treatments are well tolerated (16, 17, 67, 68). In other words, these strata may in principle represent the combination of risk (high correlation with TP53 abnormality) and age (high correlation with fitness). However, for the reasons stipulated above, the chronologic age cut-off should not be rigid, so as to allow elderly patients in good health to enjoy the benefit of more aggressive treatment, and vice versa, to spare younger patients with comorbidity of unwarranted therapy associated risks.
The stratification is used for guidelines and reflects general principles, but for each patient, treatment plan should be individualized and set up after careful clinical evaluation, also taking into account patients’ preferences.
Therapeutic procedure
Therapeutic recommendations based on evidence/clinical trials
The treatment for B-CLL consists of antineoplastic therapy and supportive measures. Antineoplastic measures consist traditionally of chemotherapy, therapeutic antibodies, radiotherapy, stem cell transplantation methods, and recently novel agents that include B-cell receptor signal transduction inhibitors (BRI) and bcl-2 antagonists. In these guidelines, the recommendations are based on phase 3 clinical trials, in some cases on evidence from earlier phase trials, and on the approved agents and therapies in Croatia. Combination therapy is generally more efficient than monotherapy.
Choice of antineoplastic treatment options – new therapeutic paradigm
Because this disease is generally not curable, occurs in elderly population, and often progresses slowly, it is most often treated in a conservative fashion. In asymptomatic patients, treatment may be deferred until the patient becomes symptomatic as the disease progresses (69). This concept is still valid and the treatment outside clinical trials is recommended only for patients that fulfill the indications described. Since the rate of progression may vary from patient to patient, with long periods of stability and sometimes spontaneous regressions, frequent and careful observation is required to monitor the clinical course (5). At present, about 30% live without symptoms and never need therapy. Others will progress sooner or later, and will meet the criteria for therapy introduction.
The new, very effective treatments have recently dramatically changed the therapeutic landscape and led to change in the current CIT based paradigm into a new one. In comparison to therapies available to date, the new treatments show markedly improved efficacy and considerably better tolerance. This has an impact on all aspects of patient management and choice of treatment options. This also goes for deferring therapy, but at present there are no data to support early treatment. Current and future clinical trials that include novel agents in this setting may change this current concept. For patients in whom the criteria for therapy initiation are met, the general principle in the new paradigm is that (because no curative therapy has yet been found) initial therapy should maximize efficacy with improvement of overall survival (OS), while introducing the least overall toxicity, both short term and long term. Standard chemotherapeutic agents induce not only cytopenias and sometimes fatal infections (acute treatment toxicity) but also mutational damage to the genome that can manifest as more aggressive and refractory phenotypes upon relapse and can induce second malignancies. For this reason, avoiding chemotherapeutic agents upfront, when possible, is a new paradigm of sequencing therapy for CLL (5). Major changes are explained in Figure 1.
Fig. 1.
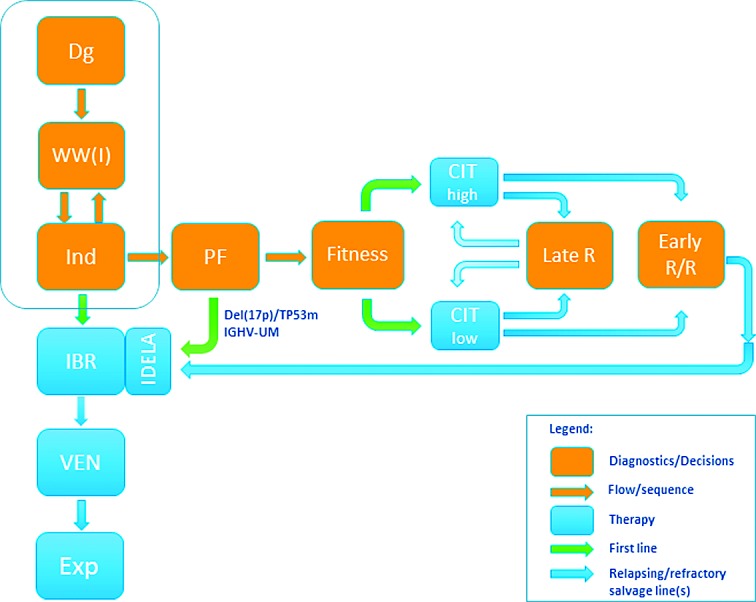
Flow chart describing B-CLL diagnosis and treatment 2017 paradigm shift. This chart shows diagnostics based decision steps (orange rectangles) and their sequence (orange arrows), currently approved therapies by EMA (in 2/2017) (blue rectangles), as well as the sequence for first-line treatment (green arrows) and salvage treatment lines (blue arrows). The minority of patients (about 10%) present with indication for treatment at diagnosis, while the majority are observed until the criteria for treatment are met. This part (framed) did not change. When the indication is present, B-CLL patients are eligible for first-line treatment. In this part, major changes have occurred because of recent approval of new options. Ibrutinib monotherapy is approved as continuous treatment of undetermined duration or until progression or unmanageable toxicity for all patient strata because of favorable efficacy/tolerance ratio in disease control. This is a new approved option, so that ibrutinib could be used to start the new path. In case of progression or toxicity, patients qualify for second-line treatment (approved option is venetoclax). If this fails, the patient is eligible for experimental treatments (combinations of novel agents with immunotherapy, allogeneic stem cell transplantation, CAR-T cell therapy, and the like). Theoretically, all of these could be done without further diagnostics and stratification, while avoiding chemotherapy. However, head-to-head comparison data between novel agents and chemo-immunotherapy (CIT) are still lacking. CIT, although associated with higher short- and long-term toxicities, has proved to be highly effective in achieving long, durable remissions and perhaps even a cure in some patient subsets. It was therefore in the CIT era essential to identify those who would respond, and a number of predicting factors have emerged in this setting. The NGS has revealed that intratumoral heterogeneity and genomic changes can be used for better CIT response prediction. Most important for CIT clinical use are two predictors, del(17p)/TP53mut and IGHV mutation status. The former can identify patient subset in which chemotherapy is ineffective and even contraindicated because of inducing adverse clonal evolution, and the latter can identify disease type, where patients with unmutated IGHV poorly respond to CIT and even if they respond, the response is short and clones that are more resistant emerge. Both predictors are considered standard minimum for stratification. If adverse features are present, the patients should be treated with ibrutinib or idelalisib in first line. Others may continue towards CIT that is tailored according to age and comorbidities. Fit patients qualify for FCR, unfit for Clb+Obi or like, and patients ‘in-between’ for BR. If they relapse late, the CIT may be repeated, tailored to current fitness, while early relapsed/refractory patients qualify for BRI or venetoclax salvage. At present, baseline stratification based on genetically defined risk, as well as on age and comorbidities to tailor treatment intensity is still needed for CIT, although fitness is currently not important for novel agents. The current CIT based paradigm (shown horizontally) is losing importance and the new paradigm (shown vertically) is likely to take over. However, it will require identification of new important predictors along the new path, since the majority of predictors identified for CIT lose their power in the new setting. As data accumulate, new predictors will emerge for this setting. High throughput NGS has begun to identify new predictors for targeted therapy response, as well as new predictors of failure at molecular level, as treatment proceeds. All this may eventually lead to a new upfront stratification for risk adapted precision medicine therapy in B-CLL. The ongoing trials and head-to-head comparison of novel agents and their combinations with immunotherapy versus CIT are under way. They will hopefully resolve current dilemmas. Novel therapy research including genomic diagnostics is likely to offer new options that will eventually lead to time limited therapies, without chemotherapy. Dg = diagnosis; WW(I) = watch and wait (investigate); Ind = indications for treatment; PF = predictive factors; Late R = late relapse; Early R/R = early relapsing or refractory; IBR = ibrutinib; IDELA = idelalisib; VEN = venetoclax; Exp = experimental treatment; CIT = chemo-immunotherapy
However, in the absence of head-to-head randomized trials to assess efficacy/tolerance ratio between novel therapies and best CIT for fit patients, in this subset CIT should not be abandoned. Also, the access and availability of new treatments will need some time, and the current cost of novel treatment may be out of reach for insurers.
Treatment options and current labels for approved antineoplastic medications
Observation. For patients who do not fulfill the criteria for starting therapy, the treatment is observation. Although it is in contrast to general oncologic tendency to treat patients with neoplasms as soon as possible, no data exist to suggest any harm in deferring therapy in those patients. Since the rate of progression may vary, frequent and careful observation is required to monitor the clinical course.
Ibrutinib. Ibrutinib is a selective irreversible inhibitor of Bruton tyrosine kinase, a signaling molecule located upstream in the B-cell receptor-signaling cascade. Label: IMBRUVICA as a single agent is indicated for the treatment of adult patients with previously untreated CLL; IMBRUVICA as a single agent or in combination with bendamustine and rituximab (BR) is indicated for the treatment of adult patients with CLL who have received at least one prior therapy (70). Those indications have been approved based on the randomized phase 3 studies RESONATE-2 (PCYC-1115-CA), RESONATE and HELIOS (71-73).
Idelalisib. Idelalisib is an oral inhibitor of the delta isoform of phosphatidylinositol 3-kinase, which is located in the B-cell receptor-signaling cascade. Label: ZYDELIG is indicated in combination with an anti-CD20 monoclonal antibody (rituximab or ofatumumab) for the treatment of adult patients with CLL who have received at least one prior therapy, or as first-line treatment in the presence of 17p deletion or TP53 mutation in patients who are not eligible for any other therapies (74). Approval is based on randomized, double-blind, phase 3 study (75) and phase 2 study (76).
Rituximab. Rituximab is a murine anti-CD20 monoclonal antibody. Label: MABTHERA is indicated in combination with chemotherapy for the treatment of patients with previously untreated and relapsed/refractory CLL (77). Approval was based on randomized phase 3 studies with fludarabine and cyclophosphamide (FCR) (78, 79), bendamustine (BR) (80, 81), and chlorambucil (82, 83).
Obinutuzumab. Obinutuzumab is a human anti-CD20 monoclonal antibody. Label: GAZYVARO in combination with chlorambucil is indicated for the treatment of adult patients with previously untreated CLL and with comorbidities making them unsuitable for full-dose fludarabine based therapy (84). Approval is based on a randomized phase 3 study (82).
Ofatumumab. Ofatumumab is a human anti-CD20 monoclonal antibody. Label: ARZERRA is used in previously untreated patients who cannot be treated with fludarabine; in these patients, it is used together with chlorambucil or bendamustine (other cancer medicines); in patients whose disease has not responded to previous treatment (known as refractory disease) with fludarabine and a medicine called alemtuzumab; and in patients whose disease has come back after previous treatment (known as relapsed disease). In these patients, ARZERRA is used together with fludarabine and cyclophosphamide (85). Approval is based on a randomized phase 3 study in combination with chlorambucil COMPLEMENT-1 (86).
Alemtuzumab. Alemtuzumab, a monoclonal antibody directed at CD52. The drug was withdrawn for CLL indication by the producer because of commercial reasons. However, the company can offer the drug on request for compassionate use free of charge. Label: (EMA EPAR 2011 authorization withdrawn). MABCAMPATH is used to treat patients with B-cell CLL for whom treatment combinations including fludarabine are not appropriate (87). Approval was based on randomized clinical trials and showed activity in TP53 mutation (88-90).
Venetoclax. Venetoclax is a highly selective inhibitor of Bd2. Label: VENCLYXTO monotherapy is indicated for the treatment of CLL in the presence of 17p deletion or TP53 mutation in adult patients who are unsuitable for or have failed a B-cell receptor pathway inhibitor. Venclyxto monotherapy is indicated for the treatment of CLL in the absence of 17p deletion or TP53 mutation in adult patients who have failed both chemo-immunotherapy and B-cell receptor pathway inhibitor (91). Approval is based on a phase 1 escalation study (92) and phase 2 study (93).
Oral alkylating agents with or without corticosteroids. Chlorambucil was used for the treatment of CLL for more than 60 years. Label: LEUKERAN is indicated for the treatment of CLL (94). Although the role of chlorambucil has considerably diminished, regulators paradoxically still accept drugs for registration on the basis of phase 3 trials, which use chlorambucil in very low doses as comparator (89, 95, 96), while claiming at the same time that the therapeutic success of such therapies is extremely modest. Thus, low doses are still considered standard therapy, although it was shown that medium and especially high doses had significantly greater effectiveness (97-100). A meta-analysis of six trials of immediate versus deferred therapy with chlorambucil showed no difference in OS at 10 years (69).
Purine analogs. Fludarabine is a purine analog, one of a group of chemotherapy drugs known as anti metabolites. They stop cells making and repairing DNA. Cancer cells need to make and repair DNA in order to grow and multiply. Label: Fludarabine (gen) is used in the treatment of B-cell CLL in patients with sufficient healthy blood cell production. First treatment for CLL with this medicine should only be started in patients with advanced disease having disease related symptoms or evidence of disease progression (101). Approval is based on a phase 3 randomized study (95). This drug is also used in combination therapies (see below).
Bendamustine. Bendamustine is a cytotoxic agent with bifunctional properties of an alkylator and a purine analog. Label: bendamustine (gen) is used as monotherapy or in combinations with other drugs for treatment of CLL in cases when combination chemotherapy containing fludarabine is not appropriate (102). Approval is based on a randomized phase 3 trial for monotherapy (103) and for combinations on phase 2 trials in previously treated (80) and untreated patients (81).
Combination therapy
Fludarabine based combinations include FCR, FCOfa, FR, and FC. Fludarabine plus cyclophosphamide plus rituximab has proved very effective in those patients who can tolerate the treatment. For this reason, in the last 10 years, FCR has become the gold standard of CIT for fit patients (78). Long-term results have confirmed overall efficacy and a subset of long-term responders defined by genomic risk groups has emerged (104-106). Although no head-to-head comparisons have yet been completed in line with the new paradigm, the indication is narrowed to a subset of fit patients with hypermutated IVGH in whom the likelihood of very long remission may outweigh the concerns of chemotherapy toxicity.
Bendamustine combinations are used in those patients in whom fludarabine cannot be tolerated. In head-to-head comparison to FCR, BR combination was found inferior (107).
Combination therapy without anti-CD20 monoclonal antibodies. For FC, CVP and CHOP, a meta-analysis of ten trials compared combination chemotherapy (before the availability of rituximab) with chlorambucil alone and showed no difference in OS at 5 years (69).
Combination with novel agents. It is likely that combinations of BRI and Bcl2 inhibitors with anti-CD20 antibodies will be the basis in the era of the new emerging paradigm. At present, only ibrutinib + bendamustine + rituximab and idelalisib + anti-CD20 monoclonal antibodies are approved.
Bone marrow and peripheral stem cell transplantations. Although this modality is considered the only option for cure, it is still under clinical evaluation, especially in the context of novel agents and new emerging paradigm (108, 109).
The overall therapeutic effect is a consequence of total therapeutic interventions, including antineoplastic and supportive measures that are particularly important.
Criteria for evaluation of response to therapy
Table 5 shows the criteria for assessment of therapeutic effect. The criteria generally used the same grounds, based on the estimation of the tumor mass parameters in different compartments on the one hand, and the parameters for the assessment of myelopoiesis on the other hand. The criteria are somewhat different in the current NCI/iwCLL criteria (6, 13) and the criteria described below (IGCI, EORTC) (97-99, 110, 111).
Table 5. Definition of response to treatment (NCI updated guidelines, Blood 2008).
| PARAMETER | CR1 | PR (1) | PD (1) | |
|---|---|---|---|---|
| NCI / IWCLL | Group A | |||
| Lymphadenopathy (2) | There is none >1.5 cm | Decrease ≥50% | Increase ≥50% | |
| Hepatomegaly | No | Decrease ≥50% | Increase ≥50% | |
| Splenomegaly | No | Decrease ≥50% | Increase ≥50% | |
| Lymphocytosis in blood | <4x109/L | Decrease ≥50% from baseline | Increase ≥50% from baseline | |
| Bone marrow (3) | Normocellular, <30% lymphocytes, No B-lymphoid nodules. Hypocellular marrow defines CRi. |
50% reduction of marrow infiltration or B lymphoid nodules. | ||
| Group B | ||||
| Platelets | >100x109/L | >100x109/L or increase ≥50% from baseline | Reduction by ≥50% from baseline as a result of CLL | |
| Hemoglobin | >110 g/L | >110 g/L or increase ≥50% from baseline | Reduction by >2 g/dL from baseline as a result of CLL | |
| Neutrophils (3) | >1.5x109/L | >1.5x109/L or >50% improvement from baseline | ||
| TTM* (EORTC/IGCI/ KROHEM) |
TTM | TTM <2 (lymphocytosis <4x109/L, no lymphadenopathy, no organomegaly) | TTM decrease ≥50% and TTM<9 | TTM increase ≥25% |
| BM function (Plt, Hb, Neutro): same as NCI/IWCLL (group B) | ||||
Group A criteria define tumor mass, group B criteria define hematopoietic system (or bone marrow) function.
1 CR (complete remission): all criteria must be present, and patients must be without general symptoms associated with CLL; PR (partial remission): at least two criteria in group A plus one in group B must be present; SD (stable disease) is the absence of progressive disease (PD) if at least PR is not reached; PD (progressive disease): at least one criterion from group A or B must be present.
2 The sum of the products of multiple lymph nodes (as evaluated by CT in clinical trials or by physical examination in general practice).
3 These parameters are irrelevant for certain types of responses.
To monitor the dynamics of the disease (both progression and response to therapy), TTM score (described in clinical stage) is very convenient because it is the only clinical system that is based on a continuous, quantitative parameter that is easy to apply and validated in thousands of patients in various international clinical trials. To estimate the doubling time (DT), it is more reliable than just the number of lymphocytes because it can compensate for changes in the distribution of the tumor mass occurrence after the administration of corticosteroids or TKIs, when there may be an increase in the number of leukocytes while reducing the nodes or spleen. For this reason, the NCI/iwCLL criteria have recently been amended, but are still suboptimal for monitoring disease response (23, 112), while the TTM scoring system is much better for measuring redistribution of clonal cells among compartments (30, 113).
When assessing the response to therapy, complete remission (CR) is assessed equally in the TTM and NCI based criteria, but TTM shows the advantage in assessing partial remission (PR) by comparing total tumor mass before and after treatment, so it is possible to set a minimum threshold for minimal remission (MR), e.g., reduction by >25%, partial remission (PR) >50%, and very good PR >75% and more. Likewise, the TTM based criteria are more accurate and without bias on estimating stable disease (SD) and progressive disease (PD). The continuous quantitative character of TTM size allows for comparison of trends between the criterion group A (TTM) and group B (function of residual normal hematopoiesis). It is possible to evaluate the beneficial antineoplastic effect of therapy independently of the toxic effect on hematopoiesis.
Minimal residual disease (MRD) is an important end point, and should reflect no measurable disease in the body. However, MRD testing should be standardized and the sample source well defined. By doing this, we should avoid reports of MRD negative patients with persistent significant organomegaly. Those cases in fact have ‘clean’ blood but sometimes may not fulfill common criteria for partial remission, and the term MRD without specification is misleading.
Antineoplastic therapy – current treatment options
There are several treatment options. Therapeutic recommendations summary for first-line treatment and for salvage treatment in major therapeutic stratification groups are shown in respective tables.
Management of patients with no accepted criteria for therapy
If the patient is not showing any signs of active/progressive/symptomatic disease, the antineoplastic therapy is not recommended, but the patient is monitored and reviewed without therapy. Thus ‘Watch and Wait’ should be transformed to ‘Watch and Investigate’ (W&I). This view is based on the evidence collected in randomized trials during the 1980s, when it was shown that chlorambucil based treatment did not contribute to longer survival, moreover, despite the relative ease of controlling symptoms and achieving clinical remission, overall survival was marginally worse (97, 110, 114). Until now, there are no data indicating that harm is due to deferring therapy in asymptomatic, stable disease. However, trials that are under way, which include novel agents and/or combinations, may change this concept, but it will take time since those trials require prolonged follow up.
While for these patients antineoplastic medication is not recommended, standard care should include infection prophylaxis such as annual flu and pneumococcal every 5 years, and in case of infection early treatment.
Initial treatment (first-line treatment)
The first-line treatment relates to previously untreated patients. All patients in standard care must have clinical indication for treatment initiation (i.e. must fulfill the criteria stipulated above). Recommendation depends on the risk associated with B-CLL (High or Low) and patient general condition (Fit or Unfit) (Table 6, Fig. 1). Each stratum will be discussed separately.
Table 6. First-line treatment of CLL (KROHEM v1 2017).
| Stage | % a | Molecular cytogenetics | % b | General condition | % b | First-line treatment |
|---|---|---|---|---|---|---|
| Standard c | ||||||
| Asymptomatic; Binet: A-B ; Rai 0-II; TTM<9 (15) |
33 | Irrelevant | Irrelevant | Nothing (W&I) | ||
| Binet C, Rai III-IV; TTM>15; or symptomatic disease (indication for treatment met) |
67 | No del(17p) /TP53 mut | 93 | Fit | 32 | FCR (1)d B + R e Ibrutinib (1) |
| Unfit | 61 | Chl + Obi (1) Chl + R Chl + Ofa B + R Ibrutinib (1) |
||||
| del(17p)/ TP53 mut |
7 | Irrelevant | 7 | Ibrutinib Idelalisib + R HDMP+R A f |
Clinical trials are highly recommended for all subsets and we strongly believe that they improve the level of care.
a Projected percentages are based on compiled data from Western countries and Croatia.
b Percentages of patients with distinct general condition and molecular genetics groups refer to treated patients. Fit patients are less than 65 years of age and with CIRS score less than 6. Younger patients with CIRS score of 6 and more and patients aged 65 years or more (regardless of CIRS score) qualify as unfit.
c Standard treatments are in order of preference, all are 2A or less according to NCCN consensus, treatments with higher grade are marked (1).
d In patients with hypermutated IGHV and no 11q.
e For less fit patients.
f Alemtuzumab is withdrawn from market, but can be obtained free of charge from producer upon request.
FCR (fludarabine, cyclophosphamide and rituximab); B = bendamustine; Chl = chlorambucil; R = rituximab; Obi = obinutuzumab; Ofa = ofatumumab; A = alemtuzumab; HDMP (high dose methylprednisolone).
Initial treatment for patients with no del(17p/TP53 mutation that are fit (LOW RISK + FIT)
As a rule, the patients in this stratum (about one-third of first-line treatment) are younger than 65. Therapeutic goal is to be set high, to achieve complete, durable remission, prolong survival, and perhaps even offer a possible cure.
FCR (fludarabine, cyclophosphamide, rituximab) is recommended as a standard initial therapy for previously untreated fit patients outside clinical trials (78). According to the DCLLSG CLL8 protocol, 6 cycles at intervals of 28 days if the patients tolerate the treatment well, and after EOT, no further treatment is anticipated, only follow up visits. Long-term follow up identified a subset of patients in whom long and durable response was achieved (105, 106, 115). Those patients had mutated IGHV, no 11q and were aged <65. Other patients may respond, but they tend to relapse soon. For this reason, for fit patients aged <65, mutated IGHV and no 11q (nor del(17p)/TP mutation) who fulfill the criteria for treatment, FCR is the treatment of choice. In others, according to the new paradigm, it is suggested to avoid chemotherapy, especially FC.
In patients who are unsuitable for fludarabine therapy, bendamustine + rituximab (BR) can be tried. It seems to be both less toxic and less effective.
Ibrutinib is also approved for this indication. According to the new paradigm, BRI may replace CIT but at present, there are no data of randomized trials to support it. Head-to-head comparison of FCR or BR with ibrutinib is under way and is likely to resolve this question.
Initial treatment for patients with no del(17p)/TP53 abnormality that are unfit (LOW RISK+UNFIT)
The majority of patients (more than 60% of treated in first line) belong to this group. As a rule, the patients are older than 65, with comorbidity, and therefore not capable to tolerate aggressive CIT therapeutic approach; thus, it is necessary to modify therapeutic goal and choose remission or stabilization of disease with a well-preserved quality of life.
We recommend chlorambucil plus one of the anti-CD20 antibodies as a standard (82, 83, 86, 116). Best results have been published with chlorambucil + obinutuzumab.
Also, BR is an option of chemo-immunotherapy for patients with appropriate fitness.
Ibrutinib is also approved for this indication because of excellent results in this patient subset. According to the new paradigm, BRI may replace CIT but at present, there are no direct data to support it. Head-to-head comparison of ibrutinib + obinutuzumab with chlorambucil + obinotuzumab is under way and is likely to resolve this question.
Initial treatment for fit/unfit patients with del(17p)/TP53 mutation (HIGH RISK + FIT/UNFIT)
In this stratum, we expect less than 7% of all patients treated in first line. CIT is contraindicated in this subset, since the TP53 mutated clone is not responding and CIT may enhance unfavorable clonal selection and is therefore harmful. We recommend for both fit and unfit the induction with ibrutinib or idelalisib plus rituximab. Ibrutinib appears superior to idelalisib in all settings as first choice BRI (117-119). In selected cases, this therapy can be followed by elective AlloSCT. HDMP plus rituximab (120, 121) or alemtuzumab (122) should be used if BCI therapy is unavailable.
Treatment for relapsed/refractory CLL
This relates to previously treated patients. Again, they should fulfill the criteria for retreatment, essentially the same as described above. For this reason, time to progression (measured as PFS) is distinct from time to next treatment (TTNT). The situation in this setting is much more complex, since in addition to four major therapeutic strata, special attention should be paid to previous treatment(s) (type of treatment, number of treatment lines, the period that has elapsed from previous treatment, etc.). In principle, with the exception of very late relapses, the patients require more therapy to achieve less response.
Since the vast majority (>90%) of all CLL first-line treated patients have no TP53 abnormality, their treatment allocation was essentially dependent on their general condition (Fit or Unfit). Thus, the fit patients receive more aggressive treatment aiming at MRD negativity (hopefully eradication of the disease), while the unfit patients receive less aggressive treatment that is less likely to achieve MRD negativity and consequently the therapeutic aim is less ambitious.
The relapse is, therefore, primarily linked to the first-line therapeutic stratum. It is an indicator of respective therapy failure. In principle, the longer the period to relapse, the more effective first-line treatment was.
General principles of therapeutic strategies in relapsing/refractory patients are shown in Table 7 and Figure 1. The relapsing patient in early relapse is considered refractory and requires change of therapy. If the treatment results in remission of long duration, it is reasonable to try the same treatment that has proved effective again in the relapse.
For this reason, relapses will be described as a function of first-line stratification therapeutic failures. However, in all patients in relapse, TP53 status should be checked (before each new line of therapy) to assess whether the risk grade has changed in comparison to front-line stratification. Most of the patients currently relapsing early were in first line treated by CIT adjusted to fitness status. Occasionally, some patients in first relapse were in first line treated by chemotherapy (chlorambucil, fluradabine alone or in combination with cyclophosphamide).
Patients relapsing from the LOW RISK + FIT stratum
Patients relapsing early are considered refractory and should be treated with ibrutinib, or idelalisib plus rituximab.
If the anti BCR drugs cannot be provided, the current options include BR, HDMP+R, FA, other chemo-immunotherapy, ofatumumab and alloSCT.
Patients relapsing late who have not acquired TP53 abnormality remain fit enough for fludarabine-based treatment, and those with a clinical indication for treatment may receive FCR, provided that they have mutated IGHV, no TP53 or 11q (108, 123). If the patient at the time of relapse changes to unfit stratum, the relapse treatment described in respective section applies.
Patients relapsing from the LOW RISK + UNFIT stratum
Over 50% of all treated patients belong to this group. In this group, less aggressive treatment was applied in front line because these patients are not likely to tolerate FCR. The response obtained is less likely MRD negative and relapses are expected in a wide range from early (less than 24 months) or late (more than 24 months).
In case of early relapse, patient is considered refractory to given treatment and ibrutinib or idelalisib + rituximab is recommended. Less benefit can be expected from BR or chlorambucil + antiCD20 or HDMP + R. In selected responsive cases, ofatumumab maintenance is applied.
In case of late relapse, the patients relapsing after chlorambucil can be retreated with chlorambucil + anti-CD20 monoclonal antibody (116). This therapy may be repeated several times (in function of achieved duration) until the duration of remission is shortened to 2 years, after which it is justified to go to the second-line therapy (ibrutinib or idelalisib+R).
Patients relapsing from the HIGH RISK + FIT/UNFIT stratum
These patients are at a particularly high risk. If the patients did not receive BRI treatment, those drugs are recommended. If the patients relapse on BRI drugs, venetoclax or alternative BRI is indicated. If those are not available, HDMP + R or alemtuzumab ± R can be tried.
If the fit patients were not previously allo transplanted, reinduction should be considered with different combinations (including ofatumumab) and if successful, proceed to transplantation.
In selected responsive cases, ofatumumab maintenance may be considered (124).
Consolidation/Maintenance therapy
It has been observed that MRD negative remission is associated with prolonged progression free survival both in previously untreated (125) and relapsed (126) patients. This has led to studies of additional treatment in patients with residual disease post therapy. In line with the new paradigm, although chlorambucil maintenance can prolong survival (127), maintenance treatment should be chemotherapy free. Ofatumumab in selective responsive patients was shown to prolong PFS but not OS (128), and is approved for this indication by FDA. Other anti-CD20 antibodies, although approved in some other B-cell malignancies (129), are not yet approved in B-CLL by regulators. Lenalidomide was also shown to improve PFS, but is not yet approved by regulators (130, 131).
As described earlier, BRI therapies are given for a prolonged period to maintain the response as distinct from chemo-immunotherapy. Early (months) period of treatment is characterized by marked tumor mass redistribution, so that monitoring should be adjusted accordingly (see section on response criteria).
The role of allogeneic transplantation
The indication for allogeneic SCT is currently changing in line with excellent results of BRI and venetoclax. Current indications include poor responders to BRI and Bcl-2 antagonist, and appearance of Richter syndrome (109).
The role of radiotherapy
Radiotherapy can provide effective palliation in cases with symptomatic bulky lymphadenopathy and should be offered to patients in which chemo-immunotherapy has been ineffective or is contraindicated. Low doses of external beam radiotherapy (2x2 Gy) can be highly effective in this situation and a higher dose (30 Gy in 2-3 Gy fractions) may be required in patients with transformed aggressive disease or those known to have a TP53 abnormality (132).
Treatment of SLL
The biological similarities between SLL and CLL are so close that a similar response to treatment could be expected. This is supported by the MDACC single centre retrospective study (133). Indications for and choices of treatment are the same as for CLL. Rare patients in whom SLL is diagnosed following biopsy of an enlarged lymph node in the absence of detectable disease at any other site may be offered local radiotherapy with curative intent.
Risk of other diseases
Infections
The risk of infections is related to progressive defect both in antibody- and cell-mediated immunity. In addition, therapy may worsen immune impairment, particularly fludarabine and anti-CD20 antibodies, but also B-cell receptor inhibitors. For this reason, infections represent a frequent cause of morbidity and mortality in CLL. Infections are typically bacterial and should be treated early. For those who have repeated infection and require repeated antibiotics, immunoglobulin replacement therapy should be considered. Prophylactic vaccination is advised, but live vaccine should be avoided.
Autoimmune complications
Autoimmune complications are common in CLL, occurring in 10%-20% of patients (134). They almost exclusively target blood cells, most commonly red blood cells. Hemolytic anemia (AIHA) is predominant and immune thrombocytopenia (ITP) is 4-5 times less common. A bone marrow aspirate is usually required to confirm the diagnosis of autoimmune cytopenia.
AIHA or ITP should be treated before deciding whether therapy for CLL is needed. First-line therapy is prednisolone. Second-line therapies for patients intolerant of or refractory to steroids include cyclosporine, intravenous immunoglobulin (ITP), thrombopoietin mimetic agents (ITP), CVP, low-dose cyclophosphamide, rituximab, alemtuzumab and splenectomy (135). CLL treatment may be initiated to control recurrent or refractory AIHA/ITP. Rituximab-containing regimens are recommended in patients who do not have a TP53 abnormality. If AIHA/ITP develops during CLL treatment, the same regimen should be used again in this patient with extreme caution and only if no effective alternative is available. Autoimmune neutropenia usually responds to GCSF.
Prolymphocytic transformation
B-cell prolymphocytic transformation is diagnosed in progressive organomegaly and lymphocytosis with increase of prolymphocytes >55% and is treated as aggressive CLL. It occurs rarely in <1% of cases.
Richter syndrome
Richter syndrome is CLL transformation to aggressive lymphoma, usually DLBCL or Hodgkin like. LN biopsy is mandatory for diagnosis, PET may be helpful. It occurs in 2%-7% of patients. While novel agents are under investigation, CIT is still the recommended approach. Depending on the histologic subtype of lymphomatous transformation, patients who are suitable for intensive therapy should receive regimens currently employed for either primary diffuse large B cell lymphoma (Richter syndrome) or Hodgkin’s lymphoma. Younger patients who achieve good response are candidates for allogeneic stem cell transplantation.
Check point inhibitor pembrolizumab showed activity in RS, but not in CLL (136-138).
Myelodysplastic syndrome and acute leukemia
Although MDS and AML are uncommon in CLL, the rate of therapy related to fluadarabine based CIT is about 5% and much higher after autologous stem cell transplantation. The response to therapy is poor. Whether novel agents that do not induce genotoxic stress to stem cells reduce the incidence of this serious complication is currently under evaluation.
Supportive therapy
Supportive therapy plays an important role in management and is carried out in accordance with the generally accepted good clinical practice (16, 17).
Table 8 shows the basic characteristics of supportive therapy in B-CLL. This covers the area of vaccination, anti-infective prophylaxis, respiratory recurrent infections requiring IV antibiotics and hospitalization, immunoglobulin replacement therapy, blood transfusions, and tumor lysis.
Table 8. Supportive therapy in patients with B-CLL.
| PROBLEM | RECOMMENDATIONS | |
|---|---|---|
| 1 | Vaccination | • Annual vaccination against influenza. Care must be taken of the fact that the recovery of B-cell system after anti CD20 antibody therapy lasts for about 9 months, so that the response to vaccination in this period is inadequate. • Pneumococcal vaccine every 5 years • Avoid all live vaccines, including Zoster |
| 2 | Anti-infective prophylaxis | • For patients receiving purine analogs and/or alemtuzumab, and in period after that the following prophylaxis is recommended: ✓ Herpes viruses (acyclovir) ✓ PCP (sulfamethoxazole/trimethoprim) • Special attention in patients receiving alemtuzumab should be paid to the problem of CMV reactivation. Although there is no common position in the literature, most reports recommend that prophylactic ganciclovir is prescribed if viremia present. The viral load levels must be monitored every few weeks. • For patients receiving anti CD20 antibody and BRI and positive for HBV, HCV consult GE/infectologist for antiviral prophylaxis. |
| 3 | Respiratory infections requiring IV antibiotics and hospitalization | • Apply appropriate antibiotic therapy. • Determine serum IgG, and if the value is less than 5 g/L: ✓ Apply monthly IVIG 0.3-0.5 g/kg ✓ Adjust the dose so that the value is maintained above 5 g/L |
| 4 | Immunoglobulin replacement therapy | • Should be considered as a means of reducing the incidence of bacterial infections in patients with a low serum IgG level who have experienced previous major or recurrent minor bacterial infections despite optimal antibacterial prophylaxis. • The goal should be to reduce the incidence of infection and the immunoglobulin dose should be adjusted accordingly. • Patients should be reviewed regularly to evaluate the effectiveness of immunoglobulin replacement therapy and whether there is a continuing need for treatment. • Patients who develop serious and/or recurrent infections despite antimicrobial prophylaxis and immunoglobulin replacement should be managed in conjunction with a microbiologist, infectious disease specialist, and/or immunologist. |
| 5 | Blood transfusion | • The use of irradiated blood products should be considered in the following situations: indefinitely in patients treated with a purine analog, following bendamustine until more evidence emerges about the risk of transfusion-associated graft versus host disease, following alemtuzumab and for 3 months post conditioning with chemotherapy or immunotherapy (6 months after total body irradiation) for patients undergoing autologous transplantation. |
| 6 | Tumor lysis | • Venetoclax can cause severe tumor lysis syndrome. Special precautions and ramp-up therapy should be followed strictly. |
Extended version and updates can be found on KROHEM website: http://www.krohem.hr/Documents/AMENDMENT%20KROHEM%20CLL%20GUIDELINES%20v1.%202016%20%20ENGL.pdf
References
- 1.Masters GA, Krilov L, Bailey HH, Brose MS, Burstein H, Diller LR, et al. Clinical Cancer Advances 2015: Annual Report on Progress against Cancer from the American Society of Clinical Oncology. J Clin Oncol. 2015;33(7):786–809. 10.1200/JCO.2014.59.9746 [DOI] [PubMed] [Google Scholar]
- 2.Rossi D, Gaidano G. The clinical implications of gene mutations in chronic lymphocytic leukaemia. Br J Cancer. 2016;114(8):849–54. 10.1038/bjc.2016.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guièze R, Robbe P, Clifford R, de Guibert S, Pereira B, Timbs A, et al. Presence of multiple recurrent mutations confers poor trial outcome of relapsed/refractory CLL. Blood. 2015;126(18):2110–7. 10.1182/blood-2015-05-647578 [DOI] [PubMed] [Google Scholar]
- 4.Kipps TJ, Stevenson FK, Wu CJ, Croce CM, Packham G, Wierda WG, et al. Chronic lymphocytic leukaemia. Nat Rev Dis Primers. 2017;3:16096. 10.1038/nrdp.2016.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.PDQ. Chronic Lymphocytic Leukemia Treatment (PDQ(R)): Health Professional Version Bethesda (MD)2017 [cited 2017-2-22]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26389470.
- 6.Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Dohner H, et al. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood. 2008;111(12):5446–56. 10.1182/blood-2007-06-093906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375–90. 10.1182/blood-2016-01-643569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gibson SE, Swerdlow SH, Ferry JA, Surti U, Dal Cin P, Harris NL, et al. Reassessment of small lymphocytic lymphoma in the era of monoclonal B-cell lymphocytosis. Haematologica. 2011;96(8):1144–52. 10.3324/haematol.2011.042333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Campo E, Swerdlow SH, Harris NL, Pileri S, Stein H, Jaffe ES. The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications. Blood. 2011;117(19):5019–32. 10.1182/blood-2011-01-293050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rawstron AC, Bennett FL, O’Connor SJ, Kwok M, Fenton JA, Plummer M, et al. Monoclonal B-cell lymphocytosis and chronic lymphocytic leukemia. N Engl J Med. 2008;359(6):575–83. 10.1056/NEJMoa075290 [DOI] [PubMed] [Google Scholar]
- 11.Jaksic B. Sindrom kronične limfocitne leukemije. In: Vrhovac BJ, Reiner Z, Vucelic B, eds. Interna medicina. Zagreb: Ljevak d.o.o.; 2008. p. 1006-13. [Google Scholar]
- 12.Cheson BD, Bennett J, Grever M, Kay N, Keating M, O’Brien S, et al. National Cancer Institute-sponsored Working Group guidelines for chronic lymphocytic leukemia: revised guidelines for diagnosis and treatment. Blood. 1996;87(12):4990–7. [PubMed] [Google Scholar]
- 13.Marti G, Zenger V. The natural history of CLL: historical perspective. In: Faguet G, ed. Chronic Lymphocytic Leukemia Molecular Genetics, Biology, Diagnosis, and Management. New York: Humana Press; 2004. p. 3-56. [Google Scholar]
- 14.Marti GE, Rawstron AC, Ghia P, Hillmen P, Houlston RS, Kay N, et al. Diagnostic criteria for monoclonal B-cell lymphocytosis. Br J Haematol. 2005;130(3):325–32. 10.1111/j.1365-2141.2005.05550.x [DOI] [PubMed] [Google Scholar]
- 15.Fung SS, Hillier KL, Leger CS, Sandhu I, Vickars LM, Galbraith PF, et al. Clinical progression and outcome of patients with monoclonal B-cell lymphocytosis. Leuk Lymphoma. 2007;48(6):1087–91. 10.1080/10428190701321277 [DOI] [PubMed] [Google Scholar]
- 16.Zelenetz AD, Gordon LI, Wierda WG, et al. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma. V2.2017-21 February 2017 [2017 Mar 1]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/cll.pdf
- 17.Oscier D, Dearden C, Erem E, Fegan C, Follows G, Hillmen P, et al. Guidelines on the diagnosis, investigation and management of chronic lymphocytic leukaemia. Br J Haematol. 2012;159:541–64. 10.1111/bjh.12067 [DOI] [PubMed] [Google Scholar]
- 18.Surveillance E, Results E. (SEER) Program [Internet]. NCI. 2017 [cited 2017 Feb 22]. Available from: http://seer.cancer.gov/statfacts/html/clyl.html.
- 19.HMNR. Haematological Malignancy Research Network (HMRN). Epidemiology & Cancer Statistics Group at the University of York; 2017 [2017 Feb 22]. Available from: http://www.hmrn.org/statistics/incidence.
- 20.Jaksic B, Vitale B, Hauptmann E, Planinc-Peraica A, Ostojic S, Kusec R. The roles of age and sex in the prognosis of chronic leukaemias. A study of 373 cases. Br J Cancer. 1991;64(2):345–8. 10.1038/bjc.1991.303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cartwright RA, Bird CC, Darwin CM, O’Brien C, Richards ID, Roberts B, et al. Chronic lymphocytic leukaemia: case control epidemiological study in Yorkshire. Br J Cancer. 1987;56(1):79–82. 10.1038/bjc.1987.158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Novak I, Jaksic O, Kulis T, Batinjan K. Incidence and mortality trends of leukemia and lymphoma in Croatia, 1988-2009. Croat Med J. 2012;53(2):115–23. 10.3325/cmj.2012.53.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nieto WG, Almeida J, Romero A, Teodosio C, Lopez A, Henriques AF, et al. Increased frequency (12%) of circulating chronic lymphocytic leukemia-like B-cell clones in healthy subjects using a highly sensitive multicolor flow cytometry approach. Blood. 2009;114(1):33–7. 10.1182/blood-2009-01-197368 [DOI] [PubMed] [Google Scholar]
- 24.Strati P, Shanafelt TD. Monoclonal B-cell lymphocytosis and early-stage chronic lymphocytic leukemia: diagnosis, natural history, and risk stratification. Blood. 2015;126(4):454–62. 10.1182/blood-2015-02-585059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rawstron AC, Kreuzer KA, Soosapilla A, Spacek M, Gambell P, McIver-Brown N, et al. Reproducible diagnosis of chronic lymphocytic leukemia (CLL) by flow cytometry: an European Research Initiative on CLL (ERIC) & European Society for Clinical Cell Analysis (ESCCA) Harmonisation Project. Cytometry B Clin Cytom. 2018;94(1):121–8. 10.1002/cyto.b.21595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rai KR, Sawitsky A, Cronkite EP, Chanana AD, Levy RN, Pasternack BS. Clinical staging of chronic lymphocytic leukemia. Blood. 1975;46(2):219–34. [DOI] [PubMed] [Google Scholar]
- 27.Binet JL, Auquier A, Dighiero G, Chastang C, Piguet H, Goasguen J, et al. A new prognostic classification of chronic lymphocytic leukemia derived from a multivariate survival analysis. Cancer. 1981;48(1):198–206. [DOI] [PubMed] [Google Scholar]
- 28.Jaksic B, Vitale B. Total tumour mass score (TTM): a new parameter in chronic lymphocyte leukaemia. Br J Haematol. 1981;49(3):405–13. 10.1111/j.1365-2141.1981.tb07243.x [DOI] [PubMed] [Google Scholar]
- 29.Jaksic O, Vrhovac R, Kusec R, Kardum MM, Pandzic-Jaksic V, Kardum-Skelin I, et al. Clinical tumor cell distribution pattern is a prognostically relevant parameter in patients with B-cell chronic lymphocytic leukemia. Haematologica. 2001;86(8):827–36. [PubMed] [Google Scholar]
- 30.Jaksic O, Vitale B, Jaksic B. An old and simple solution for a new problem - more on clinical staging and evaluation of response in B-cell chronic lymphocytic leukaemia in the era of new therapies. Br J Haematol. 2014;165(5):737–40. 10.1111/bjh.12793 [DOI] [PubMed] [Google Scholar]
- 31.Parikh SA, Shanafelt TD. Prognostic factors and risk stratification in chronic lymphocytic leukemia. Semin Oncol. 2016;43(2):233–40. 10.1053/j.seminoncol.2016.02.009 [DOI] [PubMed] [Google Scholar]
- 32.Damle RN, Wasil T, Fais F, Ghiotto F, Valetto A, Allen SL, et al. Ig V gene mutation status and CD38 expression as novel prognostic indicators in chronic lymphocytic leukemia. Blood. 1999;94(6):1840–7. [PubMed] [Google Scholar]
- 33.Hamblin TJ, Davis Z, Gardiner A, Oscier DG, Stevenson FK. Unmutated Ig V(H) genes are associated with a more aggressive form of chronic lymphocytic leukemia. Blood. 1999;94(6):1848–54. [PubMed] [Google Scholar]
- 34.Hamblin TJ, Orchard JA, Ibbotson RE, Davis Z, Thomas PW, Stevenson FK, et al. CD38 expression and immunoglobulin variable region mutations are independent prognostic variables in chronic lymphocytic leukemia, but CD38 expression may vary during the course of the disease. Blood. 2002;99(3):1023–9. 10.1182/blood.V99.3.1023 [DOI] [PubMed] [Google Scholar]
- 35.Jaksic O, Paro MM, Kardum Skelin I, Kusec R, Pejsa V, Jaksic B. CD38 on B-cell chronic lymphocytic leukemia cells has higher expression in lymph nodes than in peripheral blood or bone marrow. Blood. 2004;103(5):1968–9. 10.1182/blood-2003-11-3890 [DOI] [PubMed] [Google Scholar]
- 36.Jaksic O, Gizdic B, Veic T, et al. ZAP-70 has higher expression in lymph nodes and bone marrow compared to peripheral blood in B-cell chronic lymphocytic leukemia. Haematologica 2009;94 Suppl 2:S367 (Meeting Abstract: 0913).
- 37.Korac P, Ajdukovic R, Kardum Paro MM, Jaksic B, Dominis M. Immunohistochemical analysis of ZAP-70 expression in chronic lymphocytic leukemia. J Mol Histol. 2009;40(1):81–6. 10.1007/s10735-009-9213-6 [DOI] [PubMed] [Google Scholar]
- 38.Crespo M, Bosch F, Villamor N, Bellosillo B, Colomer D, Rozman M, et al. ZAP-70 expression as a surrogate for immunoglobulin-variable-region mutations in chronic lymphocytic leukemia. N Engl J Med. 2003;348(18):1764–75. 10.1056/NEJMoa023143 [DOI] [PubMed] [Google Scholar]
- 39.Letestu R, Rawstron A, Ghia P, Villamor N, Boeckx N, Boettcher S, et al. Evaluation of ZAP-70 expression by flow cytometry in chronic lymphocytic leukemia: a multicentric international harmonization process. Cytometry B Clin Cytom. 2006;70(4):309–14. 10.1002/cyto.b.20132 [DOI] [PubMed] [Google Scholar]
- 40.Rassenti LZ, Jain S, Keating MJ, Wierda WG, Grever MR, Byrd JC, et al. Relative value of ZAP-70, CD38, and immunoglobulin mutation status in predicting aggressive disease in chronic lymphocytic leukemia. Blood. 2008;112(5):1923–30. 10.1182/blood-2007-05-092882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hallek M. Prognostic factors in chronic lymphocytic leukemia. Ann Oncol. 2008;19 Suppl 4:iv51–3. 10.1093/annonc/mdn196 [DOI] [PubMed] [Google Scholar]
- 42.Bergmann M, Eichhorst B, Busch R, et al. Prospective evaluation of prognostic parameters in early stage chronic lymphocytic leukemia (CLL): results of the CLL1-protocol of the German CLL Study Group (GCLLSG) [abstract] Blood. 2007;110:625. [Google Scholar]
- 43.Kardum-Skelin I, Planinc-Peraica A, Ostojic Kolonic S, Radic-Kristo D, Milas M, Vrhovac R, et al. Clinical and laboratory prognostic parameters for leukemic types of chronic lymphoproliferative diseases. Acta Med Croatica. 2008;62(4):351–64. [in Croatian] [PubMed] [Google Scholar]
- 44.Deaglio S, Vaisitti T, Aydin S, Bergui L, D’Arena G, Bonello L, et al. CD38 and ZAP-70 are functionally linked and mark CLL cells with high migratory potential. Blood. 2007;110(12):4012–21. 10.1182/blood-2007-06-094029 [DOI] [PubMed] [Google Scholar]
- 45.Döhner H, Stilgenbauer S, Benner A, et al. Genomic aberrations and survival in chronic lymphocytic leukemia. N Engl J Med. 2000;343(26):1910–6. 10.1056/NEJM200012283432602 [DOI] [PubMed] [Google Scholar]
- 46.Strefford JC. The genomic landscape of chronic lymphocytic leukaemia: biological and clinical implications. Br J Haematol. 2015;169(1):14–31. 10.1111/bjh.13254 [DOI] [PubMed] [Google Scholar]
- 47.Arruga F, Gizdic B, Serra S, Vaisitti T, Ciardullo C, Coscia M, et al. Functional impact of NOTCH1 mutations in chronic lymphocytic leukemia. Leukemia. 2014;28(5):1060–70. 10.1038/leu.2013.319 [DOI] [PubMed] [Google Scholar]
- 48.Eichhorst B, Hallek M. Prognostication of chronic lymphocytic leukemia in the era of new agents. Hematology (Am Soc Hematol Educ Program). 2016;2016(1):149–55. 10.1182/asheducation-2016.1.149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shanafelt TD, Jenkins G, Call TG, Zent CS, Slager S, Bowen DA, et al. Validation of a new prognostic index for patients with chronic lymphocytic leukemia. Cancer. 2009;115(2):363–72. 10.1002/cncr.24004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baliakas P, Mattsson M, Stamatopoulos K, Rosenquist R. Prognostic indices in chronic lymphocytic leukaemia: where do we stand how do we proceed? J Intern Med. 2016;279(4):347–57. 10.1111/joim.12455 [DOI] [PubMed] [Google Scholar]
- 51.Molica S, Alberti A. Prognostic value of the lymphocyte doubling time in chronic lymphocytic leukemia. Cancer. 1987;60(11):2712–6. [DOI] [PubMed] [Google Scholar]
- 52.Dicker F, Herholz H, Schnittger S, Nakao A, Patten N, Wu L, et al. The detection of TP53 mutations in chronic lymphocytic leukemia independently predicts rapid disease progression and is highly correlated with a complex aberrant karyotype. Leukemia. 2009;23(1):117–24. 10.1038/leu.2008.274 [DOI] [PubMed] [Google Scholar]
- 53.Hallek M, Wanders L, Ostwald M, Busch R, Senekowitsch R, Stern S, et al. Serum beta(2)-microglobulin and serum thymidine kinase are independent predictors of progression-free survival in chronic lymphocytic leukemia and immunocytoma. Leuk Lymphoma. 1996;22(5-6):439–47. 10.3109/10428199609054782 [DOI] [PubMed] [Google Scholar]
- 54.Gentile M, Cutrona G, Neri A, Molica S, Ferrarini M, Morabito F. Predictive value of beta2-microglobulin (beta2-m) levels in chronic lymphocytic leukemia since Binet A stages. Haematologica. 2009;94(6):887–8. 10.3324/haematol.2009.005561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jaksic O, Kusec R, Kardum MM, Kusec V, Jaksic B. Tumor mass assessment in CLL. Distinction between sCD23 and beta-2 microglobulin. Blood. 1998;92(10 Suppl 1):S265B-B.
- 56.Pejsa V, Kusec R, Petrovecki M, Jaksic O, Jaksic B, Boranic M. Bone marrow and peripheral blood hematopoietic reserve in patients with B-cell chronic lymphocytic leukemia. Haematologica. 2003;88(12):1429–31. [PubMed] [Google Scholar]
- 57.Kardum-Skelin I, Jaksic O, Kolonic SO, Vrhovac R, Fabijanic I, Jelic-Puskaric B, et al. New parameters of diploid histogram of image DNA cytometry and newly characterized types of nucleolar organizer region structures in defining the proliferative-kinetic index in chronic leukemic lymphoproliferative disorders. Anal Quant Cytol Histol. 2009;31(5):313–23. [PubMed] [Google Scholar]
- 58.Kardum-Skelin I, Puskaric BJ, Radic-Kristo D, Jaksic O, Kardum M, Jaksic B. Multimodal image analysis of chronic leukemic lymphoproliferative disorders and the hypothesis of “single” and “multiple” programmed stops in the development of typical and atypical forms of leukemias and lymphomas. Coll Antropol. 2010;34(2):367–76. [PubMed] [Google Scholar]
- 59.Hallek M. Physiologic evaluation in the elderly prior to treatment with chemotherapy. Clin Adv Hematol Oncol. 2007;5(8):620–1. [PubMed] [Google Scholar]
- 60.Extermann M, Overcash J, Lyman GH, Parr J, Balducci L. Comorbidity and functional status are independent in older cancer patients. J Clin Oncol. 1998;16(4):1582–7. 10.1200/JCO.1998.16.4.1582 [DOI] [PubMed] [Google Scholar]
- 61.Cramer P, Hallek M. Prognostic factors in chronic lymphocytic leukemia - what do we need to know? Nat Rev Clin Oncol. 2011;8(1):38–47. 10.1038/nrclinonc.2010.167 [DOI] [PubMed] [Google Scholar]
- 62.Van Bockstaele F, Verhasselt B, Philippe J. Prognostic markers in chronic lymphocytic leukemia: a comprehensive review. Blood Rev. 2009;23(1):25–47. 10.1016/j.blre.2008.05.003 [DOI] [PubMed] [Google Scholar]
- 63.Wierda WG, O’Brien S, Wang X, Faderl S, Ferrajoli A, Do KA, et al. Characteristics associated with important clinical end points in patients with chronic lymphocytic leukemia at initial treatment. J Clin Oncol. 2009;27(10):1637–43. 10.1200/JCO.2008.18.1701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tam CS, Seymour JF. A new prognostic score for CLL. Blood. 2014;124(1):1–2. 10.1182/blood-2014-05-575407 [DOI] [PubMed] [Google Scholar]
- 65.Pflug N, Bahlo J, Shanafelt TD, Eichhorst BF, Bergmann MA, Elter T, et al. Development of a comprehensive prognostic index for patients with chronic lymphocytic leukemia. Blood. 2014;124(1):49–62. 10.1182/blood-2014-02-556399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.International CLLIPIwg An international prognostic index for patients with chronic lymphocytic leukaemia (CLL-IPI): a meta-analysis of individual patient data. Lancet Oncol. 2016;17(6):779–90. 10.1016/S1470-2045(16)30029-8 [DOI] [PubMed] [Google Scholar]
- 67.Hallek M. State-of-the-art treatment of chronic lymphocytic leukemia. Hematology (Am Soc Hematol Educ Program). 2009:440–9. 10.1182/asheducation-2009.1.440 [DOI] [PubMed] [Google Scholar]
- 68.Gribben JG. How I treat CLL up front. Blood. 2010;115(2):187–97. 10.1182/blood-2009-08-207126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.CLL Trialists’ Collaborative Group Chemotherapeutic options in chronic lymphocytic leukemia: a meta-analysis of the randomized trials. CLL Trialists’ Collaborative Group. J Natl Cancer Inst. 1999;91(10):861–8. 10.1093/jnci/91.10.861 [DOI] [PubMed] [Google Scholar]
- 70.Imbruvica EMA. EPAR - summary for the public [updated 2016-10-6; cited 2017 2017-2-22]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/003791/WC500177778.pdf.
- 71.Burger JA, Tedeschi A, Barr PM, Robak T, Owen C, Ghia P, et al. Ibrutinib as initial therapy for patients with chronic lymphocytic leukemia. N Engl J Med. 2015;373(25):2425–37. 10.1056/NEJMoa1509388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Byrd JC, Brown JR, O’Brien S, Barrientos JC, Kay NE, Reddy NM, et al. Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med. 2014;371(3):213–23. 10.1056/NEJMoa1400376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chanan-Khan A, Cramer P, Demirkan F, Fraser G, Silva RS, Grosicki S, et al. Ibrutinib combined with bendamustine and rituximab compared with placebo, bendamustine, and rituximab for previously treated chronic lymphocytic leukaemia or small lymphocytic lymphoma (HELIOS): a randomised, double-blind, phase 3 study. Lancet Oncol. 2016;17(2):200–11. 10.1016/S1470-2045(15)00465-9 [DOI] [PubMed] [Google Scholar]
- 74.Zydelig EMA. EPAR - summary for the public: EMA; [updated 2016-11-142017-2-22]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/003843/WC500175380.pdf.
- 75.Furman RR, Sharman JP, Coutre SE, Cheson BD, Pagel JM, Hillmen P, et al. Idelalisib and rituximab in relapsed chronic lymphocytic leukemia. N Engl J Med. 2014;370(11):997–1007. 10.1056/NEJMoa1315226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.O’Brien SM, Lamanna N, Kipps TJ, Flinn I, Zelenetz AD, Burger JA, et al. A phase 2 study of idelalisib plus rituximab in treatment-naive older patients with chronic lymphocytic leukemia. Blood. 2015;126(25):2686–94. 10.1182/blood-2015-03-630947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mabthera EMA. EPAR - summary for the public: EMA; [updated 2016-8-2; cited 2017 2017-2-22]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/000165/WC500025815.pdf.
- 78.Hallek M, Fischer K, Fingerle-Rowson G, Fink AM, Busch R, Mayer J, et al. Addition of rituximab to fludarabine and cyclophosphamide in patients with chronic lymphocytic leukaemia: a randomised, open-label, phase 3 trial. Lancet. 2010;376(9747):1164–74. 10.1016/S0140-6736(10)61381-5 [DOI] [PubMed] [Google Scholar]
- 79.Robak T, Dmoszynska A, Solal-Celigny P, Warzocha K, Loscertales J, Catalano J, et al. Rituximab plus fludarabine and cyclophosphamide prolongs progression-free survival compared with fludarabine and cyclophosphamide alone in previously treated chronic lymphocytic leukemia. J Clin Oncol. 2010;28(10):1756–65. 10.1200/JCO.2009.26.4556 [DOI] [PubMed] [Google Scholar]
- 80.Fischer K, Cramer P, Busch R, Bottcher S, Bahlo J, Schubert J, et al. Bendamustine in combination with rituximab for previously untreated patients with chronic lymphocytic leukemia: a multicenter phase II trial of the German Chronic Lymphocytic Leukemia Study Group. J Clin Oncol. 2012;30(26):3209–16. 10.1200/JCO.2011.39.2688 [DOI] [PubMed] [Google Scholar]
- 81.Fischer K, Cramer P, Busch R, Stilgenbauer S, Bahlo J, Schweighofer CD, et al. Bendamustine combined with rituximab in patients with relapsed and/or refractory chronic lymphocytic leukemia: a multicenter phase II trial of the German Chronic Lymphocytic Leukemia Study Group. J Clin Oncol. 2011;29(26):3559–66. 10.1200/JCO.2010.33.8061 [DOI] [PubMed] [Google Scholar]
- 82.Goede V, Fischer K, Busch R, Engelke A, Eichhorst B, Wendtner CM, et al. Obinutuzumab plus chlorambucil in patients with CLL and coexisting conditions. N Engl J Med. 2014;370(12):1101–10. 10.1056/NEJMoa1313984 [DOI] [PubMed] [Google Scholar]
- 83.Hillmen P, Gribben JG, Follows GA, Milligan D, Sayala HA, Moreton P, et al. Rituximab plus chlorambucil as first-line treatment for chronic lymphocytic leukemia: final analysis of an open-label phase II study. J Clin Oncol. 2014;32(12):1236–41. 10.1200/JCO.2013.49.6547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gazyvaro EMA. EPAR - summary for the public [2017-2-22]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/002799/WC500171597.pdf.
- 85.Arzerra EMA. EPAR - summary for the public [updated 2017-2-82017-2-22]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/001131/WC500093092.pdf.
- 86.Hillmen P, Robak T, Janssens A, Babu KG, Kloczko J, Grosicki S, et al. Chlorambucil plus ofatumumab versus chlorambucil alone in previously untreated patients with chronic lymphocytic leukaemia (COMPLEMENT 1): a randomised, multicentre, open-label phase 3 trial. Lancet. 2015;385(9980):1873–83. 10.1016/S0140-6736(15)60027-7 [DOI] [PubMed] [Google Scholar]
- 87.EMA. MABCAMPATH: EPAR - summary for the public [updated 2012-8-152017-2-22]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/000353/WC500025261.pdf.
- 88.Elter T, Gercheva-Kyuchukova L, Pylylpenko H, Robak T, Jaksic B, Rekhtman G, et al. Fludarabine plus alemtuzumab versus fludarabine alone in patients with previously treated chronic lymphocytic leukaemia: a randomised phase 3 trial. Lancet Oncol. 2011;12(13):1204–13. 10.1016/S1470-2045(11)70242-X [DOI] [PubMed] [Google Scholar]
- 89.Hillmen P, Skotnicki AB, Robak T, Jaksic B, Dmoszynska A, Wu J, et al. Alemtuzumab compared with chlorambucil as first-line therapy for chronic lymphocytic leukemia. J Clin Oncol. 2007;25(35):5616–23. 10.1200/JCO.2007.12.9098 [DOI] [PubMed] [Google Scholar]
- 90.Pettitt AR, Jackson R, Carruthers S, Dodd J, Dodd S, Oates M, et al. Alemtuzumab in combination with methylprednisolone is a highly effective induction regimen for patients with chronic lymphocytic leukemia and deletion of TP53: final results of the National Cancer Research Institute CLL206 trial. J Clin Oncol. 2012;30(14):1647–55. 10.1200/JCO.2011.35.9695 [DOI] [PubMed] [Google Scholar]
- 91.Venclyxto EMA. EPAR - summary for the public [updated 2016-12-212017-2-22]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/004106/WC500218803.pdf.
- 92.Roberts AW, Davids MS, Pagel JM, Kahl BS, Puvvada SD, Gerecitano JF, et al. Targeting BCL2 with venetoclax in relapsed chronic lymphocytic leukemia. N Engl J Med. 2016;374(4):311–22. 10.1056/NEJMoa1513257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Stilgenbauer S, Eichhorst B, Schetelig J, Coutre S, Seymour JF, Munir T, et al. Venetoclax in relapsed or refractory chronic lymphocytic leukaemia with 17p deletion: a multicentre, open-label, phase 2 study. Lancet Oncol. 2016;17(6):768–78. 10.1016/S1470-2045(16)30019-5 [DOI] [PubMed] [Google Scholar]
- 94.FDA. Leukeran [updated 20032017-2-22]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2003/10669slr028_leukeran_lbl.pdf.
- 95.Rai KR, Peterson BL, Appelbaum FR, Kolitz J, Elias L, Shepherd L, et al. Fludarabine compared with chlorambucil as primary therapy for chronic lymphocytic leukemia. N Engl J Med. 2000;343(24):1750–7. 10.1056/NEJM200012143432402 [DOI] [PubMed] [Google Scholar]
- 96.Knauf WU, Lissichkov T, Aldaoud A, Herbrecht R, Liberati AM, Loscertales J, et al. bendamustine versus chlorambucil in treatment-naive patients with b-cell chronic lymphocytic leukemia (B-CLL): results of an international phase III study. ASH Annual Meeting Abstracts; November 16, 2007. p. 2043. [Google Scholar]
- 97.Jaksic B, Brugiatelli M. High dose continuous chlorambucil vs intermittent chlorambucil plus prednisone for treatment of B-CLL - IGCI CLL-01 trial. Nouv Rev Fr Hematol. 1988;30(5-6):437–42. [PubMed] [Google Scholar]
- 98.Jaksic B, Brugiatelli M, Krc I, Losonczi H, Holowiecki J, Planinc-Peraica A, et al. High dose chlorambucil versus Binet’s modified cyclophosphamide, doxorubicin, vincristine, and prednisone regimen in the treatment of patients with advanced B-cell chronic lymphocytic leukemia. Results of an international multicenter randomized trial. International Society for Chemo-Immunotherapy, Vienna. Cancer. 1997;79(11):2107–14. [DOI] [PubMed] [Google Scholar]
- 99.Jaksic B, Brugiatelli M, Suciu S, et al Randomized phase II study in untreated B-cell chronic lymphocytic leukemia (B-CLL) comparing fludarabine (FAMP) vs. high dose continuous chlorambucil (HD-CLB). Blood. 1998;92:103A (Meeting Abstract:421).
- 100.Catovsky D, Richards S, Matutes E, et al. Fludarabine plus cyclophosphamide improves response and progression-free survival in chronic lymphocytic leukemia. A report from the LRF CLL4 trial. Lancet. 2007;370:230–9. 10.1016/S0140-6736(07)61125-8 [DOI] [PubMed] [Google Scholar]
- 101.HALMED. Fludarabin [updated 2013-10-312017-2-22]. Available from: http://www.halmed.hr/en/Lijekovi/Baza-lijekova/Fludarabin-Pliva-25-mgml-koncentrat-za-otopinu-za-injekciju-ili-infuziju/10171/.
- 102.HALMED. Bendamustin [updated 2016-1-212017-2-22]. Available from: http://www.halmed.hr/en/Lijekovi/Baza-lijekova/Bendamustin-PharmaS-25-mgml-prascaronak-za-koncentrat-za-otopinu-za-infuziju/12264/.
- 103.Knauf WU, Lissichkov T, Aldaoud A, Liberati A, Loscertales J, Herbrecht R, et al. Phase III randomized study of bendamustine compared with chlorambucil in previously untreated patients with chronic lymphocytic leukemia. J Clin Oncol. 2009;27(26):4378–84. 10.1200/JCO.2008.20.8389 [DOI] [PubMed] [Google Scholar]
- 104.Fischer K, Bahlo J, Fink AM, Goede V, Herling CD, Cramer P, et al. Long-term remissions after FCR chemoimmunotherapy in previously untreated patients with CLL: updated results of the CLL8 trial. Blood. 2016;127(2):208–15. 10.1182/blood-2015-06-651125 [DOI] [PubMed] [Google Scholar]
- 105.Woyach JA, Johnson AJ. Targeted therapies in CLL: mechanisms of resistance and strategies for management. Blood. 2015;126(4):471–7. 10.1182/blood-2015-03-585075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Thompson PA, Tam CS, O’Brien SM, Wierda WG, Stingo F, Plunkett W, et al. Fludarabine, cyclophosphamide, and rituximab treatment achieves long-term disease-free survival in IGHV-mutated chronic lymphocytic leukemia. Blood. 2016;127(3):303–9. 10.1182/blood-2015-09-667675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Eichhorst B, Fink AM, Bahlo J, Busch R, Kovacs G, Maurer C, et al. First-line chemoimmunotherapy with bendamustine and rituximab versus fludarabine, cyclophosphamide, and rituximab in patients with advanced chronic lymphocytic leukaemia (CLL10): an international, open-label, randomised, phase 3, non-inferiority trial. Lancet Oncol. 2016;17(7):928–42. 10.1016/S1470-2045(16)30051-1 [DOI] [PubMed] [Google Scholar]
- 108.Barrientos JC. Sequencing of chronic lymphocytic leukemia therapies. Hematology (Am Soc Hematol Educ Program). 2016;2016(1):128–36. 10.1182/asheducation-2016.1.128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Dreger P, Schetelig J, Andersen N, Corradini P, van Gelder M, Gribben J, et al. Managing high-risk CLL during transition to a new treatment era: stem cell transplantation or novel agents? Blood. 2014;124(26):3841–9. 10.1182/blood-2014-07-586826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jaksic B, Brugiatelli M, Jaksic O, et al. More intensive treatment significantly improves survival in young patients with advanced CLL. Meta-analysis of IGCI CLL-01 and CLL-02 trials after 10 years of follow-up. Blood. 1999;94:311B (Meeting Abstract:4617).
- 111.EORTC CLL-01 protocol. A randomized phase II trial of high-dose chlorambucil vs. fludarabine in patients with advanced B-chronic lymphocytic leukemia. EORTC Leukemia Cooperative Group. Hematol Cell Ther. 1999;41(3):127–36. [PubMed] [Google Scholar]
- 112.Cheson BD, Byrd JC, Rai KR, Kay NE, O’Brien SM, Flinn IW, et al. Novel targeted agents and the need to refine clinical end points in chronic lymphocytic leukemia. J Clin Oncol. 2012;30(23):2820–2. 10.1200/JCO.2012.43.3748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Jaksic O, Kinda SB, Aurer I, Carzavec D, Rogulj IM, Haris V, et al. Redistribution pattern and assessment of early response to ibrutinib in CLL by total tumor mass score (TTM) - KROHEM CLL2 study. Haematologica. 2016;101:723. [Google Scholar]
- 114.Dighiero G, Maloum K, Desablens B, Cazin B, Navarro M, Leblay R, et al. Chlorambucil in indolent chronic lymphocytic leukemia. N Engl J Med. 1998;338(21):1506–14. 10.1056/NEJM199805213382104 [DOI] [PubMed] [Google Scholar]
- 115.Fischer K, Bahlo J, Fink AM, Goede V, Herling CD, Cramer P, et al. Long-term remissions after FCR chemoimmunotherapy in previously untreated patients with CLL: updated results of the CLL8 trial. Blood. 2016;127(2):208–15. 10.1182/blood-2015-06-651125 [DOI] [PubMed] [Google Scholar]
- 116.Basic-Kinda S, Aurer I, Hude I, Ostojic-Kolonic S, Pejsa V, Radman I, et al. Rituximab plus continuous or intermittent high-dose chlorambucil for previously untreated CLL: dose, but not schedule, matters. A retrospective study of KROHEM, Croatian cooperative group for hematological diseases. Leuk Lymphoma. 2015;56:32–3. 10.3109/10428194.2015.1080893 [DOI] [Google Scholar]
- 117.Sorensen S, Wildgust M, Sengupta N, Trambitas C, Diels J, van Sanden S, et al. Indirect treatment comparisons of ibrutinib versus physician’s choice and idelalisib plus ofatumumab in patients with previously treated chronic lymphocytic leukemia. Clin Ther. 2017;39(1):178–89.e5. 10.1016/j.clinthera.2016.12.001 [DOI] [PubMed] [Google Scholar]
- 118.Mato AR, Nabhan C, Barr PM, Ujjani CS, Hill BT, Lamanna N, et al. Outcomes of CLL patients treated with sequential kinase inhibitor therapy: a real world experience. Blood. 2016;128(18):2199–205. 10.1182/blood-2016-05-716977 [DOI] [PubMed] [Google Scholar]
- 119.Mato AR, Hill BT, Lamanna N, Barr PM, Ujjani CS, Brander DM, et al. Optimal sequencing of ibrutinib, idelalisib, and venetoclax in CLL: results from a large multi-center study of 683 US-patients: ASH; 2016 [2017-2-22]. Available from: https://ash.confex.com/ash/2016/webprogram/Paper93270.html. [DOI] [PubMed]
- 120.Castro JE, James DF, Sandoval-Sus JD, Jain S, Bole J, Rassenti L, et al. Rituximab in combination with high-dose methylprednisolone for the treatment of chronic lymphocytic leukemia. Leukemia. 2009;23(10):1779–89. 10.1038/leu.2009.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Dungarwalla M, Evans SO, Riley U, Catovsky D, Dearden CE, Matutes E. High dose methylprednisolone and rituximab is an effective therapy in advanced refractory chronic lymphocytic leukemia resistant to fludarabine therapy. Haematologica. 2008;93(3):475–6. 10.3324/haematol.11903 [DOI] [PubMed] [Google Scholar]
- 122.Jain N, O’Brien S. Initial treatment of CLL: integrating biology and functional status. Blood. 2015;126(4):463–70. 10.1182/blood-2015-04-585067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Badoux XC, Keating MJ, Wang X, O’Brien SM, Ferrajoli A, Faderl S, et al. Cyclophosphamide, fludarabine, alemtuzumab, and rituximab as salvage therapy for heavily pretreated patients with chronic lymphocytic leukemia. Blood. 2011;118(8):2085–93. 10.1182/blood-2011-03-341032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Fiegl M, Falkner F, Steurer M, Zojer N, Hopfinger G, Haslbauer F, et al. Successful alemtuzumab retreatment in progressive B-cell chronic lymphocytic leukemia: a multicenter survey in 30 patients. Ann Hematol. 2011;90(9):1083–91. 10.1007/s00277-011-1192-5 [DOI] [PubMed] [Google Scholar]
- 125.Bosch F, Ferrer A, Villamor N, Gonzalez M, Briones J, Gonzalez-Barca E, et al. Fludarabine, cyclophosphamide, and mitoxantrone as initial therapy of chronic lymphocytic leukemia: high response rate and disease eradication. Clin Cancer Res. 2008;14(1):155–61. 10.1158/1078-0432.CCR-07-1371 [DOI] [PubMed] [Google Scholar]
- 126.Moreton P, Kennedy B, Lucas G, Leach M, Rassam SM, Haynes A, et al. Eradication of minimal residual disease in B-cell chronic lymphocytic leukemia after alemtuzumab therapy is associated with prolonged survival. J Clin Oncol. 2005;23(13):2971–9. 10.1200/JCO.2005.04.021 [DOI] [PubMed] [Google Scholar]
- 127.Jaksic B, Brugiatelli M, Stelitano C, Morabito F, Callea V, Jaksic O, et al. Chlorambucil maintenance significantly improves survival in B-cell chronic lymphocytic leukemia (CLL): meta-analysis of IGCI CLL trials. Blood. 1997;90(10):2362. [Google Scholar]
- 128.van Oers MHJ, Kuliczkowski K, Smolej L, Petrini M, Offner F, Grosicki S, et al. Ofatumumab maintenance versus observation in relapsed chronic lymphocytic leukaemia (PROLONG): an open-label, multicentre, randomised phase 3 study. Lancet Oncol. 2015;16(13):1370–9. 10.1016/S1470-2045(15)00143-6 [DOI] [PubMed] [Google Scholar]
- 129.Milunović V, Patekar MB, Jakubac KM, Rogulj IM, Radic-Kristo D, Planinc-Peraica A, et al. Rituximab maintenance strategy in advanced follicular lymphoma: facts and controversies. Acta Clin Croat. 2017;56(1):143–56. 10.20471/acc.2017.56.01.20 [DOI] [PubMed] [Google Scholar]
- 130.Fink AM, Bahlo J, Robrecht S, Al-Sawaf O, Aldaoud A, Hebart H, et al. Lenalidomide maintenance after front line therapy substantially prolongs progression free survival in high risk CLL: interim results of a phase 3 study (CLL M1 study of the German CLL Study Group 2016 [2017-3-1]. Available from: https://ash.confex.com/ash/2016/webprogram/Paper89160.html.
- 131.Results of the phase 3 study of lenalidomide versus placebo as maintenance therapy following second-line treatment for patients with chronic lymphocytic leukemia (the CONTINUUM Trial) [Internet]. 2016 [cited 2017-3-1]. Available from: https://ash.confex.com/ash/2016/webprogram/Paper93104.html.
- 132.Lowry L, Smith P, Qian W, Falk S, Benstead K, Illidge T, et al. Reduced dose radiotherapy for local control in non-Hodgkin lymphoma: a randomised phase III trial. Radiother Oncol. 2011;100(1):86–92. 10.1016/j.radonc.2011.05.013 [DOI] [PubMed] [Google Scholar]
- 133.Tsimberidou AM, Wen S, O’Brien S, McLaughlin P, Wierda WG, Ferrajoli A, et al. Assessment of chronic lymphocytic leukemia and small lymphocytic lymphoma by absolute lymphocyte counts in 2,126 patients: 20 years of experience at the University of Texas M.D. Anderson Cancer Center. J Clin Oncol. 2007;25(29):4648–56. 10.1200/JCO.2006.09.4508 [DOI] [PubMed] [Google Scholar]
- 134.Hodgson K, Ferrer G, Montserrat E, Moreno C. Chronic lymphocytic leukemia and autoimmunity: a systematic review. Haematologica. 2011;96(5):752–61. 10.3324/haematol.2010.036152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zent CS, Kay NE. Autoimmune complications in chronic lymphocytic leukaemia (CLL). Best Pract Res Clin Haematol. 2010;23(1):47–59. 10.1016/j.beha.2010.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Brusa D, Serra S, Coscia M, Rossi D, D’Arena G, Laurenti L, et al. The PD-1/PD-L1 axis contributes to T-cell dysfunction in chronic lymphocytic leukemia. Haematologica. 2013;98(6):953–63. 10.3324/haematol.2012.077537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Hude I, Sasse S, Engert A, Brockelmann PJ. The emerging role of immune checkpoint inhibition in malignant lymphoma. Haematologica. 2017;102(1):30–42. 10.3324/haematol.2016.150656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ding W, Le Rademacher J, et al. Paper: PD-1 Blockade with pembrolizumab in relapsed CLL including Richterâ ™s Transformation: an updated report from a phase 2 trial (MC1485) 2016. Available from: https://ash.confex.com/ash/2016/webprogram/Paper95426.html.


