Abstract
SUMMARY – Previous findings on peripartum anxiety are inconsistent in respect to the prevalence and course of peripartum anxiety with comorbidity of depression. Our aim was threefold: (1) to examine the course of elevated anxiety during pregnancy, immediately after childbirth, and six weeks postpartum; (2) to establish comorbidity of postpartum anxiety and postpartum depression (PPD); and (3) to examine predictors of anxiety 6 weeks postpartum. A sample of women (N=272) who were below the cut-off score for clinical depression during pregnancy were assessed in the third trimester of pregnancy, then 2 days and 6 weeks postpartum. Questionnaires on anxiety, pregnancy specific distress, stress, coping styles, social support, and depression were administered at each assessment. Obstetric data were collected from the participants’ medical records. The estimated rate of high anxiety was 35% during pregnancy, 17% immediately after childbirth, and 20% six weeks postpartum, showing a decrease in anxiety levels after childbirth. Comorbidity of anxiety and PPD was 75%. Trait anxiety and early postpartum state anxiety are significant predictors of postpartum anxiety. Anxiety is a common peripartum psychological disturbance. Anxiety symptoms overlap with PPD, but not completely, indicating that screening for postpartum mental difficulties should include both depression and anxiety.
Key words: Anxiety; Pregnancy, predictors; Depression; Depressive disorder; Depression, postpartum; Comorbidity; Prognosis; Risk factors; Surveys and questionnaires; Medical records
Introduction
Even though extensive research on postpartum depression (PPD) over the last few decades has given some insightful findings about anxiety, anxiety during pregnancy and postpartum has been relatively neglected. PPD differs from depression not related to childbirth in that the anxiety symptoms are more often present in PPD (1, 2), and in that anxiety disorders are more prevalent than depression in the postpartum period (3). Also, the proportion of anxious women who do not report symptoms of PPD is higher than the proportion of PPD women who report symptoms of anxiety (4). Approximately 30% of primiparous women report symptoms of depression, anxiety and/or stress, but of these only one in three women is identified when screening solely for depression (5).
Anxiety in pregnancy has many adverse effects, both for maternal mental health and for the birth outcome, while also being a risk factor for PPD (6-8). Anxiety and stress during pregnancy are related to fetal heart rate and motor activity (9, 10), preterm delivery (11, 12), and infant behavior (13, 14). Postpartum anxiety is related to lower maternal self-confidence (15), and can have long-term negative consequences leading to delayed mental development in children (16). Although these findings emphasize the importance of anxiety during pregnancy and postpartum, studies on peripartal anxiety have been relatively neglected compared to studies on PPD and their results are often inconsistent. Findings on anxiety prevalence, predictors, course from pregnancy to postpartum, and comorbidity of PPD will be summarized here. Although anxiety may refer to different concepts (17), in this study the term ‘anxiety disorder’ is used when a clinical interview against specific criteria was applied; ‘state anxiety’ or ‘level of anxiety symptoms’ is used when anxiety as a transitory emotion and general state of nervousness, uneasiness and worry was assessed by self-report measures; finally, ‘trait anxiety’ refers to a disposition to perceive different situations as threatening and stressful and therefore to experience an increased level of state anxiety.
Prevalence and course of anxiety during pregnancy and postpartum
Literature review suggests the prevalence of anxiety disorders in postpartum women to be the same as the prevalence of anxiety disorders in women in general (5%-12%). However, due to methodological issues such as low participation of mothers with obstetric and neonatal problems, these figures could be even higher, around 20%-25% (18). Some studies established a 20%-25% prevalence of anxiety disorders during pregnancy (4, 8, 19) and 15%-20% in the postpartum period (4, 20). When the level of general anxiety symptoms was taken into account, high anxiety levels were present in 25%-33% of women during pregnancy (4, 21), 17%-22% in the early postpartum period (22, 23), and 15%-33% in the late postpartum period (4, 22, 24). Paul et al. (23) found a very low percentage of parturient women with high anxiety levels in the late postpartum period; approximately 6% of women had high anxiety levels at 2 weeks, 2 months or 6 months after chidlbirth. However, this study included only women who breastfed during their stay at maternity ward and intended to breastfeed at home, and the anxiety levels could be higher in women who could not or did not want to breastfeed.
Data on stability of state anxiety levels during pregnancy and postpartum are inconsistent. Most studies found the level of anxiety to be lower after childbirth than during pregnancy (25-27), but some suggested the postpartum anxiety level to be the same as during pregnancy (4), or even higher (28), although the latter measured trait anxiety, and not state anxiety. Therefore, the course of state anxiety from pregnancy to postpartum is not clear and is yet to be described.
Comorbidity of anxiety and postpartum depression
A strong relationship between postpartum anxiety and PPD has been established (29, 30). About 25% to 50% of women with some anxiety disorder also show symptoms of PPD two months after childbirth (3). Two in three women suffering from depression during the first 7 postpartum months have a comorbid anxiety disorder (4). Contrary to these findings, Muzik et al. (31) indicate that comorbidity of PPD and anxiety is low, but that anxiety disorders are as common as depression. It is difficult to determine the exact comorbidity of anxiety and depression, as most studies that examined both PPD and anxiety did not provide these data (for example, Heron et al. (26)), while some examined comorbidity only in women with PPD or elevated depressive symptoms (32, 33).
Predictors of postpartum state anxiety
Numerous studies were conducted in order to identify predictors of PPD, while predictors of postpartum anxiety were rarely addressed, and when they were, the studies focused on specific anxiety disorders such as general anxiety disorder (34) or post-traumatic stress disorder (35). General anxiety symptoms were mostly measured only as predictors of PPD (6, 7, 36), implying that anxiety is important only as an antecedent of PPD, but not per se. In a few studies where postpartum anxiety was used as a criterion variable, only anxiety during pregnancy and basic demographic variables were usually considered as possible predictors (examples in Wenzel et al. (3), Heron et al. (26)).
Previous findings indicate that postpartum anxiety is related to anxiety and other psychological disorders present before pregnancy (19, 37), anxiety during pregnancy (4, 26), anxiety in the early postpartum period (22), and maternity blues (15). A recent study by Farr et al. (24) showed that a higher number of stressful life events during pregnancy was a risk factor for postpartum anxiety. However, the study was retrospective and stressful events during pregnancy were assessed postpartum, so that cognitive bias due to the current mental health difficulties cannot be excluded. Van Bussel et al. (27) showed that depressive coping style was a significant predictor of postpartum anxiety, but as the actual stress level was not assessed, the role of both stress and coping styles for postpartum anxiety was not clear. Low levels of perceived social support are related to postpartum anxiety levels (38), and poor relationship adjustment is a significant predictor of higher postpartum anxiety (39).
Of obstetric variables, history of artificial abortion (40) and unwanted pregnancy (41) are significant predictors of postpartum anxiety. Mode of delivery (cesarean section or assisted vaginal delivery) is related to anxiety immediately after childbirth (23, 40), but not to anxiety 6 weeks postpartum (40).
Previous studies on predictors of postpartum anxiety were focused mainly on just one set of variables as potential predictors. In rare comprehensive studies that measured peripartum anxiety prospectively and comprised different psychological predictors of anxiety, obstetric variables were neglected. Furthermore, anxiety during pregnancy as a predictor of postpartum anxiety was measured by general anxiety questionnaires (4, 26), although pregnancy specific anxiety and general anxiety share less than one-quarter of the total variance (42, 43), indicating that these constructs are somewhat different. Pregnant women are concerned about health and medical problems, childbirth and the baby’s health, weight and body image, emotions and relationships, and socioeconomic issues (42, 44), and these aspects should also be assesed in order to grasp the full range of anxiety and distress in pregnant women.
To fill in the gap in previous studies, it is necesary to conduct a prospective study on postpartum anxiety that will look at demographic, obstetric, and psychological variables (general and pregnancy specific anxiety, stress, coping, and social support), during pregnancy and in the early postpartum period, as predictors of postpartum anxiety. Furthermore, as previous studies measured anxiety in the longer postpartum period (three months after childbirth or more) or in specific samples (e.g., women with unwanted pregnancy only), it is difficult to determine the relationship between anxiety and PPD in the period when PPD is assessed most commonly (i.e. 6 weeks postpartum). Our aim was threefold: (1) to examine the prevalence and course of elevated state anxiety during pregnancy, in the early and late postpartum period; (2) to establish comorbidity of postpartum state anxiety and PPD; and (3) to examine predictors of state anxiety 6 weeks postpartum.
Subjects and Methods
Participants
Pregnant women older than 18 years, in the third trimester of pregnancy were invited to participate in the study conducted as part of a larger prospective study on PPD (45). Women with a history of psychiatric disorders or treatment, and who scored above the cut-off for clinical depression on the Beck Depression Inventory (46) during pregnancy were excluded (n=13) in order to measure the new-onset PPD. Based on these criteria, 375 pregnant women were eligible to participate in the study. In the early postpartum period, 326 (86.9%) women gave birth at the University Department and filled out all the questionnaires. Out of these, 272 (83.4%) women filled out questionnaires 6 weeks postpartum. Complete description of the sample recruitment and attrition is provided elsewhere (47).
Women in the final sample (N=272) had the mean (±SD) age of 29.5±4.4 years, 98.2% were married or cohabiting, 85.3% lived in urban areas, and 74.3% reported an average socioeconomic status. Participants equally graduated from high school (48.6%) and university (50.7%). Previous depressiveness that was neither diagnosed nor treated was reported by 9.2%, and family history of psychiatric disorders was present in 9.2% of participants.
The mean gestational age at assessment during pregnancy was 35.5±3.1 weeks. Considering parity, 59.2% were primiparae, 31.3% secundiparae, and 9.5% triparae/quadriparae. The majority of participants had vaginal delivery (79.8%). The mean age of infants at the last assessment was 6.5±1.2 weeks. The feeding methods at that time were as follows: breastfeeding (62.5%), bottle-feeding (12.5%), and a combination of the two methods (25%).
Measures
Demographic questionnaire comprised questions on age, marital status, socioeconomic status, place of living, maternal and paternal education level and employment, psychiatric disorders and treatment, previous depressiveness (with answer options: 0 = no; 1 = yes, shorter than 2 weeks; 2 = yes, longer than 2 weeks, but neither diagnosed nor treated), maternal perception of the course of pregnancy, and whether the pregnancy was wanted. After delivery, several questions on the course of delivery, health of the newborn, and feeding methods were included.
Previous medical conditions, obstetric data on parity, previous abortions, hospitalization during pregnancy, delivery mode, duration of delivery, as well as the newborn’s Apgar score and neonatal complications were collected from medical records.
The State-Trait Anxiety Inventory (STAI) (48) was used as a measure of state (STAI-S) and trait (STAI-T) anxiety. The cut-off score for elevated anxiety in pregnant women is 40 or more with sensitivity of 81.0% and specificity of 79.8% for both STAI-S and STAI-T (4). STAI has been translated and validated for use in Croatia (48). As STAI-T measures a dispositional trait, it was administered only during pregnancy, while STAI-S was administered at all three assessments. The Cronbach’s α in the current study was α=0.94 for STAI-S at all three assessments, and α=0.90 for STAI-T.
The Pregnancy Concerns Scale (PCS) (49) is a self-report measure of specific distress, concerns and worries during pregnancy, constructed in accordance with pregnancy specific anxiety findings (21, 42-44). PCS is a list of 16 worries and concerns covering four domains: (1) concerns about fetal health (sample item ‘worry if the baby will be born healthy’); (2) concerns about own health and fear of childbirth (sample item ‘fear of childbirth’); (3) concerns about own appearance (sample item ‘fear of gaining weight’); and (4) socioeconomic and relationship issues (sample item ‘worry about relationship with partner’). The participant estimates her concerns about specific issues during the previous month on a 4-point scale from 0 (not bothered at all) to 3 (bothered by that a lot). Four previously described factors were extracted by factor analysis, but all items were saturated by one factor, so the score was calculated as total sum of all items. The internal consistency Cronbach’s α of the total scale and split-half coefficient were 0.80 and 0.85, respectively. PCS is a reliable and valid scale with satisfactory convergent and discriminant validity.
The Perceived Stress Scale (PSS) (50) is a 10-item scale measuring three major components of stress in general, i.e. how much a person perceives life as unpredictable, uncontrollable or overwhelming (51) on a 5-point scale, where higher numbers indicate a higher level of stress. PPS was translated and validated for use in Croatia (52). It was administered during pregnancy and in the early postpartum period, with Cronbach’s α of 0.81 and 0.85, respectively.
The COPE Inventory (53) measures dispositional ways of coping with stress on three subscales: problem-focused coping, emotion-focused coping, and avoidance. The scale has been translated into Croatian, and a brief version of 15 items has been validated (54). The brief COPE was validated in pregnant and postpartum women and was further shortened to 13 items (55). Given that COPE is a dispositional measure, it was administered only during pregnancy with Cronbach’s α of 0.68, 0.72, and 0.65 for problem-focused, emotion-focused, and avoidance coping, respectively.
The Perceived Partner Support scale (PPS) (55) is a 5-item scale measuring global relationship satisfaction, reliance and confidence in one’s partner, emotional support and instrumental partner support on a 5-point rating scale. A higher total score indicates higher perceived partner support. It was administered during pregnancy and in the early postpartum period, with Cronbach’s α of 0.74 and 0.82, respectively.
The Social Support Appraisals scale (SS-A) (56) is a composite of three subscales that measure the perceived social support provided by family, friends and others in general. It has been translated into Croatian and validated (57). The subscales measuring perceived support from family and friends were administered during pregnancy and in the early postpartum period. Cronbach’s α for the family support subscale during pregnancy and early postpartum was 0.91 and 0.93, respectively, and for the support from friends subscale during pregnancy and early postpartum 0.88 and 0.90, respectively.
Beck Depression Inventory, validated for use in Croatia (BDI) (46), was used to assess depression during pregnancy in order to exclude depressed pregnant women, so that new-onset PPD could be measured. It is a 21-item depression scale with a cut-off score for clinical depression of 29 or more. The internal consistency of BDI in the current study was α=0.80.
Edinburgh Postnatal Depression Scale (EPDS) (58) is a 10-item depression scale. Given that BDI items assess several somatic symptoms that are normal in puerperium (59), the EPDS was used to assess depression 6 weeks postpartum. Each item is rated on a 4-point scale (range 0-3), giving a maximum score of 30. The internal consistency Cronbach’s α in the original study was α=0.88 and a cut-off score for probable depression of 12/13 (58). The EPDS has been translated into Croatian and validated against DSM-IV criteria, with a sensitivity of 77.3% and specificity of 82.4% at the cut-off score of 8/9 (47). Cronbach’s α in the current study was 0.86.
Procedure
The study was conducted as part of a larger prospective study on PPD at University Department of Obstetrics and Gynecology, Sestre milosrdnice University Hospital Center in Zagreb (45). The study encompassed three assessments: in the third trimester of pregnancy at prenatal clinic (T1); in the early postpartum period (two days after vaginal birth or three days after cesarean section) at the maternity ward (T2); and 6 weeks postpartum by postal questionnaires (T3).
The study was approved by the Croatian Ministry of Science, Education and Sports. Before the administration of questionnaires, the participants were informed about the study and signed an informed consent form. As the study was prospective, anonymity could not be provided, but the participants were assured that confidentiality would be preserved.
Statistical analysis
Initial data screening revealed that the levels of anxiety were normally distributed, but perceived social support was negatively skewed. As various transformations did not normalize the skewed data, Spearman rank correlation analysis was performed to test the correlations of demographic, obstetric and psychological variables with anxiety levels. The repeated measures ANOVA was conducted on the anxiety levels to examine changes in the anxiety levels through pregnancy and postpartum. The hierarchical regression analysis was conducted to examine which variables predicted the state anxiety level 6 weeks postpartum. Given that predictors do not need to be normally distributed to conduct regression analysis (60) and all other criteria for regression were met, the regression analysis was performed on non-transformed data. The Statistical Package for Social Sciences, version 20.0 (IBM Corp., Armonk, NY, USA) was used. In all analyses, the level of significance was set at p<0.05.
Results
Prevalence and course of anxiety during pregnancy and postpartum
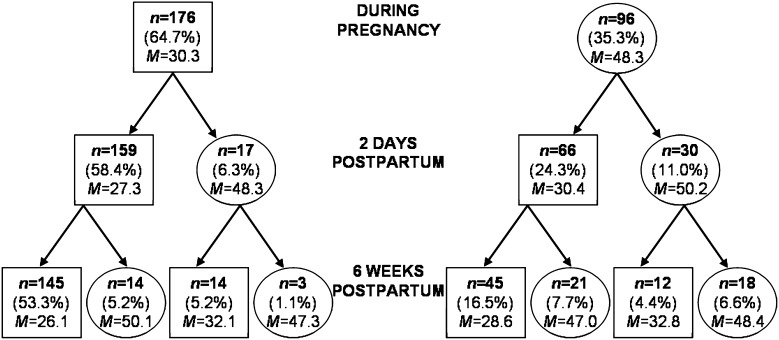
The longitudinal pattern of elevated levels of anxiety (defined as the STAI-S score of 40 or more) from pregnancy to 6 weeks postpartum is presented in Figure 1. One in three women (35.3%) had elevated anxiety during pregnancy, 17.3% were anxious in the early postpartum period (i.e. 6.3% + 11.0%) and 20.6% were anxious in the late postpartum period, (i.e. 5.2% + 1.1% + 7.7% + 6.6%). Approximately half of the participants reported high anxiety on at least one assessment (46.7%). Of the women who were anxious during pregnancy, 31.3% were anxious in the early postpartum (i.e. 30/96*100) and 18.8% were anxious on both postpartum assessments (i.e. 18/96*100). Of the women who were anxious in the early postpartum, 44.7% were also anxious in the late postpartum (i.e. 21/47*100). Finally, of the women who were anxious in the late postpartum, only 25% were completely new cases (i.e. 14/56*100) and 75% reported anxiety during pregnancy and/or in the early postpartum.
Fig. 1.
Flow chart of the State-Trait Anxiety Inventory as a measure of state anxiety (STAI-S) scores from pregnancy to 6 weeks postpartum. At each time point, the sample is divided into groups of women who scored below the cut-off for anxiety (square) and those who scored above the cut-off (round). In each cell, numbers represent the number of participants in the subsample, percent of the total sample (N=272), and mean STAI-S score for the subsample (the data presented were obtained in the current study, however, the flow chart was made on the model presented in Heron et al. (26)).
There was a significant decrease in the number of women with elevated anxiety from pregnancy to postpartum (χ2(2)=27.13, p<0.001), but without further change from 2 days postpartum to 6 weeks postpartum (χ2(1)=0.766, p>0.05). Similarly, anxiety levels significantly decreased over time (F(2, 542)=35.12, p<0.001). Post hoc Bonferroni test showed that anxiety decreased significantly from pregnancy (36.65±10.75) to immediately after childbirth (31.86±10.42), and then remained stable until 6 weeks postpartum (31.69±10.29).
Comorbidity of anxiety and postpartum depression
The results showed that anxiety and depressive symptoms 6 weeks postpartum were related (rs=0.55, p<0.01). In this sample, 22.4% of women had elevated depressive symptoms (i.e. 61/272) (results previously reported) (61). Of the women reporting anxiety symptoms, 75.0% also reported comorbid depressive symptoms (i.e. 42/56). Of the women reporting depressive symptoms, 68.9% reported anxiety symptoms as well (i.e. 42/61).
Correlates of anxiety levels 6 weeks postpartum
Demographic and obstetric variables did not show clinically significant correlations with anxiety levels (Table 1). However, partner employment status, previous depressiveness (neither diagnosed nor treated) (Table 1) and unwanted pregnancy (Table 2) were in low but statistically significant correlation with anxiety and were therefore controlled for in subsequent regression analysis.
Table 1. Spearman rank correlations of demographic and obstetric variables with STAI-S measured 6 weeks postpartum (N=272).
| STAI-S 6 weeks postpartum |
|
|---|---|
| Demographic variable | |
| Maternal age | -0.09 |
| Maternal education level | 0.05 |
| Maternal employmenta | -0.11 |
| Marital statusb | 0.04 |
| Partner’s education level | 0.04 |
| Partner’s employmenta | -0.13* |
| Socioeconomic status | -0.08 |
| Previous depressivenessc | 0.22** |
| Obstetric variable | |
| Parity | 0.03 |
| History of artificial abortiona | 0.04 |
| History of spontaneous abortiona | 0.05 |
| Delivery moded | 0.04 |
| Delivery duration (h) | 0.11 |
| Neonatal complicationsa | 0.06 |
| Feeding methode | 0.05 |
*p<0.05; **p<0.01; a1 = yes, 0 = no; bmarital status: 1 = married or cohabiting, 0 = single or separated; cprevious depressiveness: 0 = no, 1 = yes, shorter than 2 weeks, 2 = yes, longer than 2 weeks, but not diagnosed or treated; ddelivery mode: 0 = vaginal, 1 = cesarean section; efeeding method: 1 = exclusive breastfeeding, 2 = breastfeeding and bottle-feeding, 3 = exclusive bottle-feeding; STAI-S = State-Trait Anxiety Inventory as a measure of state anxiety
Table 2. Spearman rank correlations of psychological variables measured during pregnancy (T1) and two days after childbirth (T2) with STAI-S measured 6 weeks postpartum (T3) (N=272).
| Psychological variable | Correlations of T1 variables with STAI-S at T3 | Correlations of T2 variables with STAI-S at T3 |
|---|---|---|
| Unwanted pregnancya | -0.17** | - |
| STAI-S | 0.45** | 0.54** |
| STAI-T | 0.46** | - |
| PCS | 0.25** | - |
| PSS | 0.38** | 0.43** |
| COPE: problem-focused coping | -0.12* | - |
| COPE: emotion-focused coping | -0.04 | - |
| COPE: avoidance | 0.24** | - |
| PPS: support from partner | -0.23** | -0.27** |
| SS-A: support from family | -0.20** | -0.23** |
| SS-A: support from friends | -0.18** | -0.21** |
*p<0.05; **p<0.01; aunwanted pregnancy: 0 = unwanted, 1 = wanted pregnancy; STAI-S = State-Trait Anxiety Inventory as a measure of state anxiety; STAI-T = State-Trait Anxiety Inventory as a measure of trait anxiety; PCS = Pregnancy Concerns Scale; PSS = Perceived Stress Scale; PPS = Perceived Partner Support; SS-A = Social Support Appraisals
All psychological variables, both during pregnancy and in the early puerperium, were related to anxiety levels 6 weeks postpartum, except for the emotion-focused coping (Table 2). A higher level of postpartum anxiety was present in women who had a higher level of trait anxiety, state anxiety, pregnancy specific anxiety, higher levels of stress, lower levels of problem-focused coping and higher levels of avoidance coping. Postpartum anxiety also showed significant negative, albeit low correlations with perceived social support from their partner, family and friends, both during pregnancy and immediately after childbirth.
Prediction of anxiety levels 6 weeks postpartum
Hierarchical regression analysis was conducted with STAI-S 6 weeks postpartum as the outcome variable. Demographic variables were entered in the first step, pregnancy variables in the second step, and variables from the early postpartum period in the third step. Using the empirically driven approach, only variables that correlated significantly with the STAI-S were entered into regression analysis. The final model was significant and explained 34.9% of the total STAI-S variance (Table 3). Demographic variables accounted for 6.0% of STAI-S variance, with partner employment status and previous depressiveness as significant predictors. Pregnancy variables accounted for additional 20.9% of variance, with trait and state anxiety as significant predictors. Finally, the early postpartum variables explained the additional 8.0% of STAI-S variance, with state anxiety being a significant predictor. Overall, in the final step, only trait anxiety and early postpartum state anxiety were found to be significant predictors of postpartum anxiety.
Table 3. Summary of hierarchical multiple regression analysis predicting levels of state anxiety (STAI-S) score 6 weeks postpartum (N=272).
| Predictor | b | SE b | β | ΔR2 |
|---|---|---|---|---|
| Step 1: Demographic variables | ||||
| Constant | 34.45 | 2.43 | ΔR2=0.06*** | |
| Partner’s employment statusa | -5.09 | 2.39 | -0.13* | |
| Previous depressivenessb | 3.15 | 0.94 | 0.20** | |
| Step 2: Pregnancy variables | ||||
| Constant | 23.05 | 9.58 | ||
| Partner’s employment statusa | -1.57 | 2.32 | -0.04 | |
| Previous depressivenessb | 0.14 | 0.95 | 0.01 | |
| Unwanted pregnancyc | -1.30 | 1.69 | -0.04 | ΔR2=0.21*** R2=0.27*** |
| STAI-S | 0.17 | 0.07 | 0.17* | |
| STAI-T | 0.31 | 0.12 | 0.24** | |
| PCS | 0.17 | 0.11 | 0.10 | |
| PSS | 0.08 | 0.14 | 0.05 | |
| COPE – problem-focused | 0.33 | 0.19 | 0.10 | |
| COPE – avoidance | -0.11 | 0.28 | -0.02 | |
| PPS partner | -0.18 | 0.26 | -0.04 | |
| SS-A family | -0.15 | 0.20 | -0.05 | |
| SS-A friends | -0.34 | 0.18 | -0.11 | |
| Step 3: Early postpartum variables | ||||
| Constant | 22.80 | 9.71 | ||
| Partner’s employment statusa | -1.84 | 2.26 | -0.05 | |
| Previous depressivenessb | 0.70 | 0.92 | 0.04 | |
| Unwanted pregnancyc | -1.82 | 1.63 | -0.06 | |
| STAI-S | 0.08 | 0.07 | 0.08 | |
| STAI-T | 0.25 | 0.11 | 0.19* | |
| PCS | 0.11 | 0.11 | 0.06 | |
| PSS | 0.02 | 0.15 | 0.01 | |
| COPE – problem-focused | 0.35 | 0.19 | 0.11 | |
| COPE – avoidance | -0.11 | 0.27 | -0.02 | |
| PPS partner | 0.04 | 0.36 | 0.01 | |
| SS-A family | -0.01 | 0.27 | -0.00 | |
| SS-A friends | -0.20 | 0.24 | -0.07 | |
| STAI-S | 0.30 | 0.06 | 0.31** | ΔR2=0.08*** R2=0.35*** |
| PSS | 0.04 | 0.14 | 0.02 | |
| PPS partner | -0.51 | 0.38 | -0.11 | |
| SS-A family | -0.03 | 0.27 | -0.01 | |
| SS-A friends | -0.08 | 0.23 | -0.03 | |
| F(17, 254)=8.01*** | ||||
*p<0.05; **p<0.01; ***p<0.001; employment statusa: 1 = yes, 0 = no; history of depressivenessb: 0 = no, 1 = yes, shorter than 2 weeks, 2 = yes, longer than 2 weeks; unwanted pregnancyc: 0 = unwanted, 1 = wanted pregnancy; STAI-S = State-Trait Anxiety Inventory as a measure of state anxiety; STAI-T = State-Trait Anxiety Inventory as a measure of trait anxiety; PCS = Pregnancy Concerns Scale; PSS = Perceived Stress Scale; PPS = Perceived Partner Support; SS-A = Social Support Appraisals
Discussion
Prevalence and course of anxiety during pregnancy and postpartum
The prevalence of elevated anxiety (score on STAI-S of 40 or more) during pregnancy, in the early postpartum and late postpartum periods was 35.3%, 17.3%, and 20.6%, respectively. The prevalence of anxiety measured by self-report scales during pregnancy is consistent with 33% prevalence obtained in the Australian sample (4), but somewhat higher than the 25% prevalence in the Canadian sample of pregnant women (21). The prevalence of elevated anxiety was significantly lower in the postpartum period, but higher than the 6% established by Paul et al. (23). However, the latter study included only women who breastfed, while our sample also included women who bottle-fed their infants. In the immediate and late postpartum periods, one in five women had elevated anxiety, which is consistent with other studies (22, 24).
One in three women who were anxious during pregnancy continued to be anxious in the early postpartum and one in two women who were anxious in the early postpartum continued to be anxious in the late postpartum. Also, of the anxious women during pregnancy, only one in five women reported anxiety at both postpartum assessments, meaning that these women experienced transient anxiety in the peripartum period. However, finding that half of the participants reported anxiety on at least one assessment implies that it is a prominent aspect of psychological distress in the peripartum. Also, the majority (75%) of the women who were anxious in the late postpartum also reported anxiety previously, a finding consistent with Heron et al. (26), showing that anxiety in the peripartum period should be given full attention.
We found the mean anxiety levels during pregnancy to be quite high, close to the cut-off score for severe anxiety (4). The anxiety level decreased immediately after childbirth, but there was no further decrement to the late postpartum period. The fact that anxiety levels in postpartum were lower than anxiety levels during pregnancy is consistent with earlier findings (25, 26). This decrease may be due to different worries and concerns in pregnancy and after childbirth. As mentioned in the Introduction section, anxiety during pregnancy includes fear of childbirth and worry about fetal health (21, 43), which both are alleviated after childbirth (62).
Comorbidity of postpartum anxiety and depression
Both anxiety and depressive symptoms were equally present in postpartum (20.6% and 22.4%, respectively), even showing high comorbidity. Three in four anxious women suffered from comorbid depressive symptoms, and two in three depressed women suffered from comorbid anxiety symptoms. These findings imply that anxiety and depression are related in the postpartum period, similarly to previous findings in peripartum population (29, 30) and general population (63). Also, anxiety was a prominent aspect of PPD, as pointed out in previous studies (1, 2). However, 25% of the anxious women who did not suffer from depression would have been overlooked, if only screening for PPD had been performed. Therefore, screening for postpartum mental health difficulties should be extended to include other symptoms, rather than focus on depression exclusively (64). Even if anxious women screen positive on depression scales, they will probably be misdiagnosed as depressed, leading to inappropriate therapy (65).
Predictors of postpartum anxiety
Of the various demographic, obstetric and psychological variables, only trait and early postpartum state anxiety were significant predictors of anxiety levels 6 weeks postpartum. When pregnancy variables were entered in the hierarchical regression analysis (step 2), pregnancy state anxiety was predictive of postpartum anxiety, consistently with previous findings (4, 26). However, when early postpartum variables were entered in the next step, pregnancy state anxiety was no longer a significant predictor, but the early postpartum anxiety was, similarly to the findings reported by Dennis et al. (22). As reported by Heron et al. (26), the shorter the time interval between measurements, the stronger is the relation of anxiety levels, which could explain why only early postpartum anxiety was a significant predictor.
State anxiety is general and may not reflect all worries of pregnant women. Although various general anxiety scales have been validated for the peripartum population (66), some pregnancy specific measures assessing different worries and concerns related to pregnancy may be more appropriate (11, 67, 68). Pregnancy specific distress was related to postpartum anxiety in this study, but it was not a significant predictor of postpartum anxiety, while state anxiety was. It is possible that pregnancy related anxiety has short-term effects on adverse outcomes during pregnancy and childbirth, rather than longer-term effects extending to the postpartum period. The findings that pregnancy specific anxiety and stress are more related to risky health behaviors during pregnancy (e.g., alcohol consumption (69)) and adverse neonatal outcomes (70) than general anxiety and stress, are in accordance with this notion.
To summarize, only trait and early postpartum state anxiety were significant predictors of state anxiety 6 weeks postpartum. Explanation for this could lie in the fact that pregnancy variables were all related to the early postpartum state anxiety (results not presented), which in turn was in the highest correlation with 6-week postpartum anxiety, and therefore the only significant predictor. These findings suggest that focusing on trait and state anxiety in the early postpartum period could be a promising way to develop screening programs for postpartum anxiety, similar as proposed by Dennis et al. (22). Screening in the early postpartum period should be followed by interventions to ease up the transition to parenthood. Many programs for such interventions have already been developed with specific guidelines (71, 72).
Limitations
Several limitations of this study should be considered. Firstly, anxiety and depression were measured by a self-report scale, and not diagnosed by interview. As self-report scales give higher figures of anxiety prevalence than clinical interview (4), the high prevalence of increased anxiety in this study should be interpreted with care. Secondly, the cut-off score for STAI (40 or more) was chosen to enable comparison with previous studies in which it had been used. However, this cut-off was not validated for the Croatian population of postpartum women against clinical interview, so future validation studies are needed. On the other hand, the cut-off score for EPDS was validated against clinical interview and showed the anxiety prevalence by EPDS to be almost three times higher than the prevalence by interview (46). Finally, only women without a history of psychiatric disorders participated in the study, and there was an attrition of women who were unemployed and less educated, as described previously (44). Therefore, the final sample could have been biased, and a somewhat higher prevalence of anxiety might be expected if other inclusion criteria were applied.
Conclusion
Increased anxiety during pregnancy and in the postpartum period is highly prevalent. Despite the decrease of anxiety levels after childbirth, one in five women is highly anxious postpartum. Anxiety and PPD overlap, but as one in four anxious women is not depressed, the screening for postpartum mental health difficulties should include both depression and anxiety. Given that state anxiety in the early postpartum period was a significant predictor of late postpartum anxiety, it might be appropriate to screen for postpartum anxiety immediately after childbirth.
Acknowledgment
This study was carried out as part of a research project Postpartum Depression – Risk Factors, Early Detection, and Therapy, supported by the Croatian Ministry of Science, Education and Sports (grant number 134-0000000-2421).
References
- 1.Hendrick V, Altshuler L, Strouse T, Grosser S. Postpartum and nonpostpartum depression: differences in presentation and response to pharmacologic treatment. Depress Anxiety. 2000;11(2):66–72. [DOI] [PubMed] [Google Scholar]
- 2.Jolley SN, Betrus P. Comparing postpartum depression and major depressive disorder: issues in assessment. Issues Ment Health Nurs. 2007;28:765–80. 10.1080/01612840701413590 [DOI] [PubMed] [Google Scholar]
- 3.Wenzel A, Haugen EN, Jackson LC, Brendle JR. Anxiety symptoms and disorders at eight weeks postpartum. J Anxiety Disord. 2005;19:295–311. 10.1016/j.janxdis.2004.04.001 [DOI] [PubMed] [Google Scholar]
- 4.Grant KA, McMahon C, Austin MP. Maternal anxiety during the transition to parenthood: a prospective study. J Affect Disord. 2008;108:101–11. 10.1016/j.jad.2007.10.002 [DOI] [PubMed] [Google Scholar]
- 5.Miller RL, Pallant JF, Negri LM. Anxiety and stress in the postpartum: is there more to postnatal distress than depression. BMC Psychiatry. 2006;6:12. 10.1186/1471-244X-6-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alipour Z, Lamyian M, Hajizadeh E. Anxiety and fear of childbirth as predictors of postnatal depression in nulliparous women. Women Birth. 2012;25(3):e37–43. 10.1016/j.wombi.2011.09.002 [DOI] [PubMed] [Google Scholar]
- 7.Austin MP, Tully L, Parker G. Examining the relationship between antenatal anxiety and postnatal depression. J Affect Disord. 2007;101(1-3):169–74. 10.1016/j.jad.2006.11.015 [DOI] [PubMed] [Google Scholar]
- 8.Sutter-Dallay AL, Giaconne-Marcesche V, Glatigny-Dallay E, Verdoux H. Women with anxiety disorders during pregnancy are at increased risk of intense postnatal depressive symptoms: a prospective survey of the MATQUID cohort. Eur Psychiatry. 2004;19:459–63. 10.1016/j.eurpsy.2004.09.025 [DOI] [PubMed] [Google Scholar]
- 9.DiPietro JA, Costigan KA, Gurewitsch ED. Fetal response to induced maternal stress. Early Hum Dev. 2003;74:125–38. 10.1016/j.earlhumdev.2003.07.001 [DOI] [PubMed] [Google Scholar]
- 10.Monk C, Myers MM, Sloan RP, Ellman LM, Fifer WP. Effects of women’s stress-elicited physiological activity and chronic anxiety on fetal heart rate. J Dev Behav Pediatr. 2003;24(1):32–8. 10.1097/00004703-200302000-00008 [DOI] [PubMed] [Google Scholar]
- 11.Alderdice F, Lynn F, Lobel M. A review and psychometric evaluation of pregnancy-specific stress measures. J Psychosom Obstet Gynaecol. 2012;33(2):62–77. 10.3109/0167482X.2012.673040 [DOI] [PubMed] [Google Scholar]
- 12.Mancuso RA, Dunkel Schetter C, Rini CM, Roesch SC, Hobel CJ. Maternal prenatal anxiety and corticotropin-releasing hormone associated with timing of delivery. Psychosom Med. 2004;66:762–9. 10.1097/01.psy.0000138284.70670.d5 [DOI] [PubMed] [Google Scholar]
- 13.Davis EP, Snidman N, Wadhwa PD, Glynn LM, Schetter CD, Sandman CA. Prenatal maternal anxiety and depression predict negative behavioral reactivity in infancy. Infancy. 2004;6(3):319–31. 10.1207/s15327078in0603_1 [DOI] [Google Scholar]
- 14.Huizink AC, De Medina PR, Mulder EJH, Visser GHA, Buitelaar JK. Psychological measures of prenatal stress as predictors of infant temperament. J Am Acad Child Adolesc Psychiatry. 2002;41:1078–85. 10.1097/00004583-200209000-00008 [DOI] [PubMed] [Google Scholar]
- 15.Reck C, Noe D, Gerstenlauer J, Stehle E. Effects of postpartum anxiety disorders and depression on maternal self-confidence. Infant Behav Dev. 2012;35(2):264–72. 10.1016/j.infbeh.2011.12.005 [DOI] [PubMed] [Google Scholar]
- 16.Ali NS, Mahmud S, Khan A, Ali B. Impact of postpartum anxiety and depression on child’s mental development from two peri-urban communities of Karachi, Pakistan: a quasi-experimental study. BMC Psychiatry. 2013;13:274. 10.1186/1471-244X-13-274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Endler NS, Kocovski NL. State and trait anxiety revisited. J Anxiety Disord. 2001;15:231–45. 10.1016/S0887-6185(01)00060-3 [DOI] [PubMed] [Google Scholar]
- 18.Lonstein JS. Regulation of anxiety during the postpartum period. Front Neuroendocrinol. 2007;28:115–41. 10.1016/j.yfrne.2007.05.002 [DOI] [PubMed] [Google Scholar]
- 19.Giardinelli L, Innocenti A, Benni L, Stefanini MC, Lino G, Lunardi C, et al. Depression and anxiety in perinatal period: prevalence and risk factors in an Italian sample. Arch Womens Ment Health. 2012;15:21–30. 10.1007/s00737-011-0249-8 [DOI] [PubMed] [Google Scholar]
- 20.Coates AO, Schaefer CA, Alexander JL. Detection of postpartum depression and anxiety in a large health plan. J Behav Health Serv Res. 2004;31(2):117–33. 10.1007/BF02287376 [DOI] [PubMed] [Google Scholar]
- 21.Doyle-Waters MMR. Anxiety scale for pregnancy: development and validation [master thesis]. Vancouver, Canada: The University of British Columbia, 1994. [Google Scholar]
- 22.Dennis CL, Coghlan M, Vigod S. Can we identify mothers at-risk for postpartum anxiety in the immediate postpartum period using the state-trait anxiety inventory? J Affect Disord. 2013;150(3):1217–20. 10.1016/j.jad.2013.05.049 [DOI] [PubMed] [Google Scholar]
- 23.Paul IM, Downs DS, Schaefer EW, Beiler JS, Weisman CS. Postpartum anxiety and maternal-infant health outcomes. Pediatrics. 2013;131(4):e1218–24. 10.1542/peds.2012-2147 [DOI] [PubMed] [Google Scholar]
- 24.Farr SL, Dietz PM, O’Hara MW, Burley K, Ko JY. Postpartum anxiety and comorbid depression in a population-based sample of women. J Womens Health (Larchmt). 2014;23(2):120–8. 10.1089/jwh.2013.4438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Figueiredo B, Conde A. Anxiety and depression symptoms in women and men from early pregnancy to 3 months postpartum: parity differences and effects. J Affect Disord. 2011;132:146–57. 10.1016/j.jad.2011.02.007 [DOI] [PubMed] [Google Scholar]
- 26.Heron J, O’Connor TG, Evans J, Golding J, Glover V, ALSPAC Study Team. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affect Disord. 204;8(1):65-73. http://dx.doi.org/ 10.1016/j.jad.2003.08.004 [DOI] [PubMed]
- 27.van Bussel JCH, Spitz B, Demyttenaere K. Anxiety in pregnant and postpartum women. An exploratory study of the role of maternal orientations. J Affect Disord. 2009;114:232–42. 10.1016/j.jad.2008.07.018 [DOI] [PubMed] [Google Scholar]
- 28.Skouteris H, Wertheim EH, Rallis S, Milgrom J, Paxton SJ. Depression and anxiety through pregnancy and the early postpartum: an examination of prospective relationships. J Affect Disord. 2009;113:303–8. 10.1016/j.jad.2008.06.002 [DOI] [PubMed] [Google Scholar]
- 29.Correia LL, Linhares MBM. Maternal anxiety in the pre- and postnatal period: a literature review. Rev Lat Am Enfermagem. 2007;15(4):677–83. 10.1590/S0104-11692007000400024 [DOI] [PubMed] [Google Scholar]
- 30.Stuart S, Couser G, Schilder K, O’Hara M, Gorman L. Postpartum anxiety and depression: onset and comorbidity in a community sample. J Nerv Ment Dis. 1998;186(7):420–4. 10.1097/00005053-199807000-00006 [DOI] [PubMed] [Google Scholar]
- 31.Muzik M, Klier CM, Rosenblum KL, Holzinger A, Umek W, Katschnig H. Are commonly used self-report inventories suitable for screening postpartum depression and anxiety disorders? Acta Psychiatr Scand. 2000;102:71–3. 10.1034/j.1600-0447.2000.102001071.x [DOI] [PubMed] [Google Scholar]
- 32.Wenzel A, Gorman LL, O’Hara MW, Stuart S. The occurrence of panic and obsessive compulsive symptoms in women with postpartum dysphoria: a prospective study. Arch Women Ment Health. 2001;4:5–12. 10.1007/s007370170002 [DOI] [Google Scholar]
- 33.Wisner KL, Peindl KS, Gigliotti T, Hanusa BH. Obsessions and compulsions in women with postpartum depression. J Clin Psychiatry. 1999;60(3):176–80. 10.4088/JCP.v60n0305 [DOI] [PubMed] [Google Scholar]
- 34.Buist A, Gotman N, Yonkers KA. Generalized anxiety disorder: course and risk factors in pregnancy. J Affect Disord. 2011;131:277–83. 10.1016/j.jad.2011.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Olde E, editor. Childbirth-Related Posttraumatic Stress: A Prospective Longitudinal Study on Risk Factors. Wageningen: Ponsen & Looijen BV, 2006. [Google Scholar]
- 36.Teissedre F, Chabol H. Postnatal depression: a study of the predictive effects of postnatal anxiety. Ir J Psychol Med. 2003;20(4):111–4. 10.1017/S0790966700007898 [DOI] [PubMed] [Google Scholar]
- 37.Matthey S, Barnett B, Howie P, Kavanagh DJ. Diagnosing postpartum depression in mothers and fathers: whatever happened to anxiety? J Affect Disord. 2003;74(2):139–47. 10.1016/S0165-0327(02)00012-5 [DOI] [PubMed] [Google Scholar]
- 38.Aktan NM. Social support and anxiety in pregnant and postpartum women: a secondary analysis. Clin Nurs Res. 2012;21(2):183–94. 10.1177/1054773811426350 [DOI] [PubMed] [Google Scholar]
- 39.Whisman MA, Davila J, Goodman SH. Relationship adjustment, depression, and anxiety during pregnancy and the postpartum period. J Fam Psychol. 2011;25(3):375–83. 10.1037/a0023790 [DOI] [PubMed] [Google Scholar]
- 40.Fatoye FO, Oladimeji BY, Adeyemi AB. Difficult delivery and some related selected factors as predictors of early postpartum psychological symptoms among Nigerian women. J Psychosom Res. 2006;60:299–301. 10.1016/j.jpsychores.2005.04.012 [DOI] [PubMed] [Google Scholar]
- 41.Najman JM, Morrison J, Williams G, Andersen M, Keeping JD. The mental health of women 6 months after they give birth to an unwanted baby: a longitudinal study. Soc Sci Med. 1991;32(3):241–7. 10.1016/0277-9536(91)90100-Q [DOI] [PubMed] [Google Scholar]
- 42.Green JM, Kafetsios K, Statham HE, Snowdon CM. Factor structure, validity and reliability of the Cambridge Worry Scale in a pregnant population. J Health Psychol. 2003;8(6):753–64. 10.1177/13591053030086008 [DOI] [PubMed] [Google Scholar]
- 43.Huizink AC, De Medina PR, Mulder EJH, Visser GHA, Buitelaar JK. Is pregnancy anxiety a relatively distinctive syndrome? Early Hum Dev. 2004;79(2):81–91. 10.1016/j.earlhumdev.2004.04.014 [DOI] [PubMed] [Google Scholar]
- 44.Alderdice F, Lynn F. Factor structure of Prenatal Distress Questionnaire. Midwifery. 2011;27:553–59. 10.1016/j.midw.2010.05.003 [DOI] [PubMed] [Google Scholar]
- 45.Nakić Radoš S, Herman R, Tadinac M. Is the predictability of new-onset postpartum depression better during pregnancy or in the early postpartum period? A prospective study in Croatian women. Health Care Women Int. 2016;37(1):23–44. 10.1080/07399332.2014.992522 [DOI] [PubMed] [Google Scholar]
- 46.Beck AT, Steer RA, Brown GK. BDI-II, Beck Depression Inventory: Manual. 2nd ed. Jastrebarsko: Naklada Slap; 2008. (in Croatian) [Google Scholar]
- 47.Nakić Radoš S, Tadinac M, Herman R. Validation study of the Croatian version of the Edinburgh Postnatal Depression Scale (EPDS). Suvrem Psihol. 2013;16(2):203–18. [Google Scholar]
- 48.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Jastrebarsko: Naklada Slap, 2000. (in Croatian)
- 49.Nakić Radoš S, Tadinac M, Herman R. Development and validation of Pregnancy Concerns Scale. Klin Psihol. 2015;8(2):151–66. [in Croatian] [Google Scholar]
- 50.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- 51.Lazarus RS, Folkman S. Stress, Appraisal and Coping. New York: Springer, 1984. [Google Scholar]
- 52.Hudek-Knežević J, Kardum I, Lesić R. Effects of perceived stress and coping strategies on physical symptoms. Drus Istraz (Zagreb). 1999;8(4):543–61. [in Croatian] [Google Scholar]
- 53.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56:267–83. 10.1037/0022-3514.56.2.267 [DOI] [PubMed] [Google Scholar]
- 54.Hudek-Knežević J, Krapić N, Kardum I. Burnout in dispositional context: the role of personality traits, social support and coping styles. Rev Psychol. 2006;13(2):65–73. [Google Scholar]
- 55.Nakić S. Predictors of postpartum depression. Dissertation; Zagreb, Croatia: University of Zagreb; 2011. (in Croatian) [Google Scholar]
- 56.Vaux A, Phillips J, Holly L, Thompson B, Williams D, Stewart D. The social support appraisals (SS-A) scale: studies of reliability and validity. Am J Community Psychol. 1986;14(2):195–219. 10.1007/BF00911821 [DOI] [Google Scholar]
- 57.Hudek-Knežević J. Coping with stressful situations of conflict between professional and family role. Dissertation]. Zagreb, Croatia: University of Zagreb; 1994. (in Croatian) [Google Scholar]
- 58.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–6. 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- 59.Noble RE. Depression in women. Metabolism. 2005;54(5):49–52. 10.1016/j.metabol.2005.01.014 [DOI] [PubMed] [Google Scholar]
- 60.Field A. Discovering statistics using SPSS. 3rd ed. London: Sage, 2009. [Google Scholar]
- 61.Nakić Radoš S, Tadinac M, Herman R. Prevalence of depression during pregnancy and postpartum in a sample of Croatian women. Klin Psihol. 2013;6(1-2):79–93. [Google Scholar]
- 62.Fenwick J, Gamble J, Nathan E, Bayes S, Hauck Y. Pre- and postpartum levels of childbirth fear and the relationship to birth outcomes in a cohort of Australian women. J Clin Nurs. 2009;18:667–77. 10.1111/j.1365-2702.2008.02568.x [DOI] [PubMed] [Google Scholar]
- 63.Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annu Rev Psychol. 1998;49:377–412. 10.1146/annurev.psych.49.1.377 [DOI] [PubMed] [Google Scholar]
- 64.Marrs CR, Durette RT, Ferraro DP, Cross CL. Dimensions of postpartum psychiatric distress: preliminary evidence for broadening clinical scope. J Affect Disord. 2009;115:100–11. 10.1016/j.jad.2008.08.012 [DOI] [PubMed] [Google Scholar]
- 65.Rowe HJ, Fisher JRW, Loh WM. The Edinburgh Postnatal Depression Scale detects but does not distinguish anxiety disorders from depression in mothers of infants. Arch Womens Ment Health. 2008;11:103–8. 10.1007/s00737-008-0003-z [DOI] [PubMed] [Google Scholar]
- 66.Meades R, Ayers S. Anxiety measures validated in perinatal populations: a systematic review. J Affect Disord. 2011;133:1–15. 10.1016/j.jad.2010.10.009 [DOI] [PubMed] [Google Scholar]
- 67.DiPietro JA, Christensen AL, Costigan KA. The pregnancy experience scale – brief version. J Psychosom Obstet Gynaecol. 2008;29(4):262–7. 10.1080/01674820802546220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yali AM, Lobel M. Stress-resistance resources and coping in pregnancy. Anxiety Stress Coping. 2002;15(3):289–309. 10.1080/1061580021000020743 [DOI] [Google Scholar]
- 69.Arch JJ. Pregnancy-specific anxiety: which women are highest and what are the alcohol-related risks? Compr Psychiatry. 2013;54(3):217–28. 10.1016/j.comppsych.2012.07.010 [DOI] [PubMed] [Google Scholar]
- 70.Lobel M, Cannella DL, Graham JE, DeVincent C, Schneider J, Meyer BA. Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychol. 2008;27(5):604–15. 10.1037/a0013242 [DOI] [PubMed] [Google Scholar]
- 71.Fisher JR, Wynter K, Rowe H. Innovative psycho-educational program to prevent common postpartum mental disorders in primiparous women: a before and after controlled study. BMC Public Health. 2010;10:432–453. 10.1186/1471-2458-10-432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Petch J, Halford WK. Psycho-education to enhance couples’ transition to parenthood. Clin Psychol Rev. 2008;28:1125–37. 10.1016/j.cpr.2008.03.005 [DOI] [PubMed] [Google Scholar]