Abstract
Background:
Intra-articular injection is an important technique for treating rheumatoid arthritis and osteoarthritis of the knee. However, medication is often inaccurately injected outside of the joint. We devised an intra-articular injection method in which the needle is inserted into the suprapatellar bursa while the patient maintains isometric contraction of the quadriceps. This isometric contraction method is based on the concept that isometric contraction of the quadriceps induces contraction of the articularis genus muscle, thus expanding the lumen of the suprapatellar bursa.
Methods:
Intra-articular injections were performed on 150 osteoarthritic knees without effusion. The knees were alternately assigned to the isometric quadriceps method group (75 knees) and non-activated quadriceps method group (75 knees). Prior to joint injection, the anterior-posterior dimension of each suprapatellar bursa was measured to ascertain its expansion. The isometric quadriceps method was performed with the quadriceps and the articularis genus muscle maintained in a contracted state. The non-activated quadriceps method was performed in a relaxed state. Ultrasound guidance was not used for either method. Subsequently, an ultrasonic probe was used only to confirm whether the intra-articular injections were successful. We compared the accuracy of injections performed between the 2 groups.
Results:
Suprapatellar expansion was significantly larger (p < 0.001) using the isometric quadriceps method (2.1 ± 1.4 mm [range, 0 to 5 mm]) than using the non-activated quadriceps method (0.8 ± 0.7 mm [range, 0 to 2 mm]). The percentage of accurate intra-articular injections was significantly higher (p = 0.0287) using the isometric quadriceps method (93%) compared with the non-activated quadriceps method (80%).
Conclusions:
In comparison with the non-activated quadriceps method, the isometric quadriceps method led to a larger expansion of the suprapatellar bursa, which should lead to more accurate intra-articular injections. The isometric quadriceps method is effective in reducing inaccurate injections into the synovium or surrounding fatty tissues.
Clinical Relevance:
Putting force on the quadriceps muscle increases the success rate of intra-articular injection of the knee. The results of this study could provide a clinically relevant injection technique for future treatment.
The treatment of knee osteoarthritis and rheumatoid arthritis can involve intra-articular injections of corticosteroids, hyaluronic acid, or other drugs. However, it has been reported that, in some cases, medication is mistakenly injected into the surrounding synovium, suprapatellar fat pad, or prefemoral fat pad1-3. Patients receiving inaccurate injections can report extreme pain. In such cases, it is possible that the injection was not into the suprapatellar bursa but rather into the synovial tissue, which has many nerve endings4,5.
The risk of extra-articular injections rises in patients with an abundance of subcutaneous fat and little effusion6, which makes it difficult for physicians to sense whether the needle has penetrated the suprapatellar bursa. To prevent pain associated with extra-articular injections7 and to ensure that an injected drug is effective, a reliable method to inject into the joint should be established. Ultrasound guidance is considered to be the best method to ensure that the needle tip is placed accurately8-12. However, ultrasound equipment is not available in many medical facilities. Thus, an accurate method for administering blind intra-articular injections (injections without ultrasound guidance) would be desirable. A literature search of previous studies indicated that various approaches have been attempted13-19. Many of these involve changing the position of the knee and anatomical landmarks8,9.
We believe that using the isometric quadriceps contraction method, which focuses on the expansion of the suprapatellar bursa by inducing isometric contraction of the quadriceps and the articularis genus muscle (Video 1), would enable greater accuracy in delivering intra-articular injections to patients with arthritis without effusion.
Video 1.
Ultrasonography showing the suprapatellar bursa and injection technique for the isometric quadriceps contraction method.
In this study, we compared the expansion of the suprapatellar bursa and the accuracy rate of intra-articular injections between the isometric quadriceps contraction method and the non-activated quadriceps method.
Materials and Methods
One hundred and fifty knees that underwent intra-articular injection for the initial treatment of knee osteoarthritis without effusion in our outpatient department between December 2016 and June 2017 were enrolled. Knees with osteoarthritis severity rated as Kellgren and Lawrence grades I to III were included. Subjects with a knee mobility range that restricted extension by ≥10° were excluded. Sonographic examination was performed to check synovial fluid retention. Patients with a >2-mm anterior-posterior dimension of the suprapatellar bursa when in the supine position with the knees naturally extended were excluded. After exclusion, the 150 knees were alternately assigned to the isometric quadriceps contraction group or the non-activated quadriceps group as a controlled clinical trial using quasi-randomization (Fig. 1).
Fig. 1.
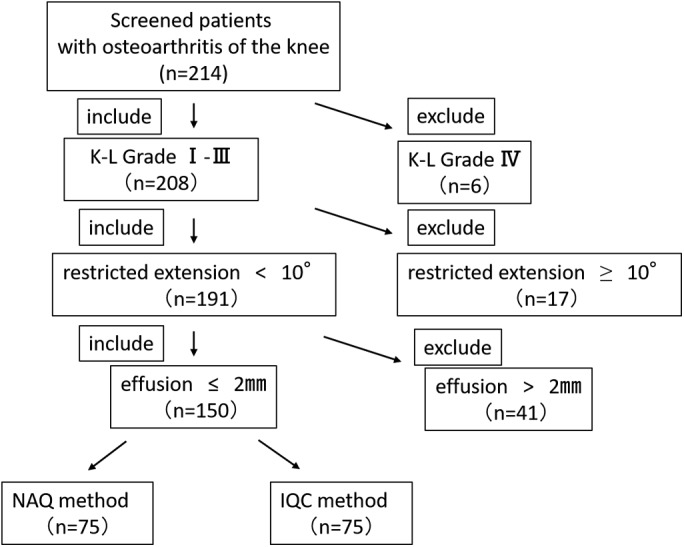
Eligibility criteria and flowchart. K-L = Kellgren and Lawrence, NAQ = non-activated quadriceps, and IQC = isometric quadriceps contraction.
We determined the sample size as follows. Based on previous studies14-19, sample size was calculated assuming that the treatment success rate of the isometric quadriceps contraction method was 95%, and that of the non-activated quadriceps method was 75% (because of the difficult conditions, the anterior-posterior dimension was ≤2 mm); the detection power was 90%; and the significance was set at an equal 2-sided level of p < 0.05. As a result, the required number of cases was 75 per group, and the target number of cases was a total of 150 in both groups.
The isometric quadriceps contraction method was performed on 75 knees in 17 male patients and 58 female patients with a mean age (and standard deviation) of 72.7 ± 8.3 years. The non-activated quadriceps method was performed on 75 knees in 14 male patients and 61 female patients with a mean age of 74.4 ± 6.6 years. Prior to the study, we obtained the approval of the institutional review board. Subjects were provided an explanation of the purpose of the study and methods, and their consent was received.
The ultrasound equipment used was a HI VISION Avius with an EUP-L75 linear probe (5.0 to 8.0 MHz) (Hitachi).
Ultrasound Observation of the Suprapatellar Bursa and Anterior-Posterior Dimension Measurements
All patients in both groups (150 knees) were told to relax the muscles surrounding the knees, the injection condition used in the non-activated quadriceps method (Fig. 2-A). The anterior-posterior dimension of the suprapatellar bursa on the longitudinal axis along the midline of the quadriceps tendon was measured by the same orthopaedic surgeon. The measurement site was the point proximal to the suprapatellar fat pad, which is the area with the smallest amount of soft tissue between the suprapatellar bursa and the quadriceps (Fig. 3-A).
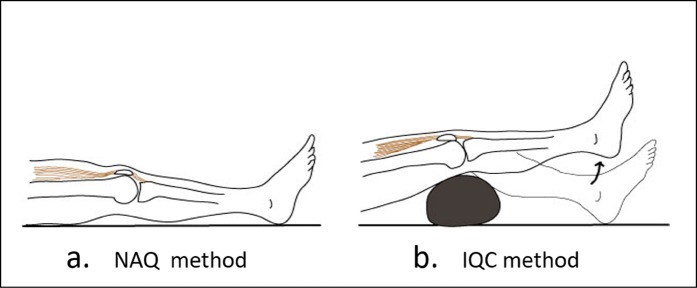
Fig. 2.
Fig. 2-A The non-activated quadriceps (NAQ) method. Subjects lie down in the supine position and relax the muscles surrounding the knees. Fig. 2-B The isometric quadriceps contraction (IQC) method. Subjects lie down with the knees at an angle of approximately 25° on a pillow. Subsequently, the knees are kept fully extended by firmly contracting the quadriceps muscle.
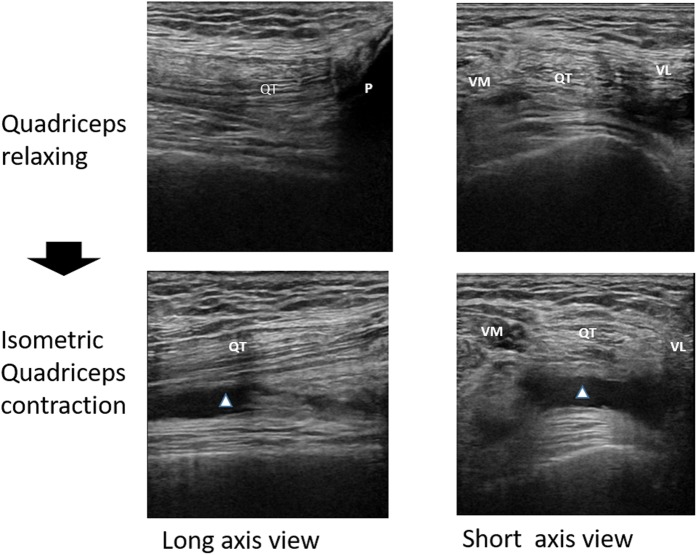
Fig. 3.
Ultrasonography assessments of the suprapatellar bursa (SPB) expansion on the non-activated quadriceps (NAQ) method (Fig. 3-A) and the isometric quadriceps contraction (IQC) method (Fig. 3-B). The anterior-posterior dimension of the SPB (bar marked by arrow) was measured vertically to the femoral bone. The target point for the needle to successfully enter the SPB is this measurement point immediately proximal to the suprapatellar fat pad (SPF). The SPB expands maximally in the anterior-posterior plane at this point, which is an area with relatively little obstruction.
Next, the patients were instructed to place the knees at an angle of approximately 25° on a pillow and were then instructed to extend the knees, as follows: “Please extend your knee firmly and keep your heel off the bed.” Subsequently, we touched the quadriceps and said, “Please contract this muscle firmly.” There were no subjects who could not follow these instructions. This is the position used in the isometric quadriceps contraction method (Fig. 2-B). After manually confirming that the quadriceps muscle was in a state of isometric contraction with the knee extended and the heel off the surface of the bed, the anterior-posterior dimension was measured again (Fig. 3-B). The 2 anterior-posterior dimensions were then compared.
We also validated the reliability of ultrasonographic measurements of the anterior-posterior dimensions. To assess the intraobserver reliability, the surgeon of this study measured 6 healthy knees on 3 days at 1-week intervals. Three measurements were done on each day, and the mean values on the 3 days were compared. For interobserver reliability, 4 examiners measured 4 healthy knees each, 3 times per knee. The measurement order was randomly assigned. Reliability was assessed by calculating intraclass correlation coefficients.
Statistical analysis was performed using SAS 9.4 (SAS Institute). Significant differences were determined using the Mann-Whitney U test (p < 0.05).
Intra-Articular Injection Method and Accuracy Measurement
The skin was pierced at a point on the lateral side of the quadriceps tendon approximately 1 cm proximal to the superior margin of the patella. The needle tip was angled toward the suprapatellar bursa without ultrasound guidance. It was stopped when the surgeon sensed that the needle had pierced the synovial membrane of the suprapatellar bursa (Video 1). The target point for the needle was the measurement site of the anterior-posterior dimension, which is an area with relatively little obstruction (Fig. 3). Once the drug solution was injected, an ultrasound probe was used parallel to the needle to capture its image and confirm whether the solution diffused within the joint. A 25-G needle and 1% hyaluronic acid (low molecular weight, approximately 900 kDa) solution at a dose of 2.5 mL/injection (Artz [purified sodium hyaluronate]; Seikagaku) were employed.
We performed this procedure for both the non-activated quadriceps method and the isometric quadriceps contraction method. Prior to extending the knee, the skin puncture point was confirmed, because it becomes difficult to palpate the margin of the patella because of isometric contraction of the quadriceps. The percentages of accurate intra-articular injections within the 2 groups were compared. Statistical analysis was performed with the Fisher exact test using SAS 9.4.
Results
There were no significant differences (p < 0.05) with regard to sex, age, or side between the isometric quadriceps contraction group and the non-activated quadriceps group (Table I). We found that the anterior-posterior dimension in the isometric quadriceps contraction method was significantly greater (p < 0.001) than that in the non-activated quadriceps method (Table II). Also, the success probability of the isometric quadriceps contraction method was higher than that of the non-activated quadriceps method (Table III).
TABLE I.
Differences Between the 2 Groups
| Isometric Quadriceps Contraction Group (N = 75) | Non-Activated Quadriceps Group (N = 75) | P Value | |
| Sex* | 0.687 | ||
| Male | 17 (22.7%) | 14 (18.7%) | |
| Female | 58 (77.3%) | 61 (81.3%) | |
| Age† (yr) | 72.7 ± 8.3 | 74.4 ± 6.6 | 0.174 |
| Side* | 0.512 | ||
| Left | 32 (42.7%) | 37 (49.3%) | |
| Right | 43 (57.3%) | 38 (50.7%) |
The values are given as the number of patients, with the percentage in parentheses. The p value was determined with use of the chi-square test.
The values are given as the mean and the standard deviation. The mean difference in years, with the 95% confidence interval, is −1.25 (−3.53 to 1.02). The p value was determined with use of the t test.
TABLE II.
Expansion of the Suprapatellar Bursa According to Injection Technique
| Method | Anterior-Posterior Dimension* † |
| Isometric quadriceps contraction | 2.1 ± 1.4 (2.0 [0 to 5]) |
| Non-activated quadriceps | 0.8 ± 0.7 (1.0 [0 to 2]) |
The values are given as the mean and the standard deviation, in millimeters, with the median in parentheses and the range in brackets.
Significantly different at p < 0.001, determined with use of the Mann-Whitney U test.
TABLE III.
Comparison of Intra-Articular Injection Accuracies*
| Method | Total No. | No. with Success | Success Rate |
| Isometric quadriceps contraction | 75 | 70 | 93.3% |
| Non-activated quadriceps | 75 | 60 | 80% |
The p value between the 2 groups, determined with use of the Fisher test, was p = 0.0287.
When performing the isometric contraction method, the intraclass correlation coefficients of the sonographic measurements were 0.999 for intraobserver reliability and 0.935 for interobserver reliability (Tables IV and V). High reliability was thus obtained for both intraobserver and interobserver correlations.
TABLE IV.
Intraobserver Reliability of Ultrasonographic Measurement of the Anterior-Posterior Dimension of the Suprapatellar Pouch*
| Subject No. | First Day† | Second Day† | Third Day† |
| 1 | 3.73 | 3.70 | 3.86 |
| 2 | 3.60 | 3.63 | 3.63 |
| 3 | 1.93 | 2.07 | 2.00 |
| 4 | 1.60 | 1.70 | 1.63 |
| 5 | 2.53 | 2.70 | 2.67 |
| 6 | 4.60 | 4.47 | 4.60 |
The intraclass correlation coefficient was 0.999 (95% confidence interval, 0.995 to 1.000).
The value is given as the mean value of 3 measurements, in millimeters.
TABLE V.
Interobserver Reliability of Ultrasonographic Measurement of the Anterior-Posterior Dimension of the Suprapatellar Pouch*
| Subject No. | Observer 1† | Observer 2† | Observer 3† | Observer 4† |
| 1 | 3.68 | 3.83 | 3.78 | 3.78 |
| 2 | 3.50 | 3.25 | 3.60 | 3.53 |
| 3 | 4.85 | 4.35 | 4.23 | 4.70 |
| 4 | 3.20 | 3.95 | 3.75 | 3.83 |
The intraclass correlation coefficient was 0.935 (95% confidence interval, 0.711 to 0.995).
The value is given as the mean value of 3 measurements, in millimeters.
Discussion
The results of this study indicate that the suprapatellar bursa is likely to expand during isometric quadriceps contraction, improving the probability of successful intra-articular injections.
We believe that the isometric quadriceps contraction method is therapeutically effective and could reduce the risk of injection pain due to inaccurate injections into the synovial membrane, which has a large number of nerve endings4,6,7.
There are many reports providing evidence for the validity of ultrasound in detecting structural pathology20-22, and good agreement between ultrasonography and magnetic resonance imaging (MRI) in visualizing effusion and synovial hypertrophy with knee osteoarthritis has been shown23. The reliability in this current study, as shown by intraclass correlation coefficients, was also very high. Thus, ultrasound measurement is effective for evaluating the expansion of the suprapatellar bursa, which occurs as discussed below.
The quadriceps tendon becomes tense under isometric contraction; therefore, the space between the tendon and the femoral bone increases. The articularis genus muscle synchronously contracts with the quadriceps and lifts the suprapatellar bursa to a proximal position, preventing it from being entrapped in the patellofemoral joint24-28. Thus, the suprapatellar bursa can expand in this space under the quadriceps tendon. In addition, when subjects contract the quadriceps muscle, the patella is lifted to the proximal position. Tension on the patellar tendon and the patellar retinaculum moves the Hoffa fat pad toward the femoral condyles and intercondylar space, reducing the lumen of the tibiofemoral joint and patellofemoral joint. This moves the joint fluid to the suprapatellar bursa20,28.
Next we will look into difficult cases, such as obese patients. A large amount of subcutaneous fat makes it difficult to predict the distance that the needle must travel to reach the suprapatellar bursa. In such cases, accidental injection into the wrong tissues, such as the quadriceps tendon, suprapatellar fat pad, and prefemoral fat pad, may occur. There is also a risk of extra-articular injections when it is difficult for the physician to detect when the needle has pierced the suprapatellar bursa synovium.
The expansion of the suprapatellar bursa enables accurate injections even for individuals with a large amount of subcutaneous fat. The articularis genus muscle pulls the suprapatellar bursa up, which puts the synovium under tension25-29 and therefore makes it easier to determine when the needle tip has pierced it. As a result, the probability of successfully administering an intra-articular injection increases, and, conversely, the risk of administering an inaccurate injection is reduced.
When synovial fluid is present under the vastus lateralis and vastus medialis muscles30, movement of the fluid can be detected by palpation. Clinically, when patients have a large amount of synovial fluid, fluid can be aspirated without any special treatment. However, for patients with only a small amount of synovial fluid, the fluid was manually gathered into the suprapatellar bursa prior to performing aspirations.
This accumulation is difficult in cases in which the anterior-posterior dimension of the suprapatellar bursa is ≤2 mm. For subjects with little synovial fluid, isometric contraction of the quadriceps proved effective for concentrating the synovial fluid of the tibiofemoral joint and the patellofemoral joint into the suprapatellar bursa (Fig. 4).
Fig. 4.
The isometric contraction of the quadriceps was effective for concentrating the synovial fluid of the tibiofemoral joint and patellofemoral joint into the suprapatellar bursa (arrowhead). QT = quadriceps tendon, P = patella, VM = vastus medialis, and VL = vastus lateralis.
On the basis of this mechanism, we believe that the isometric quadriceps contraction method can be utilized to reduce the risk of accidental injection into the fat pads surrounding the suprapatellar bursa and into the quadriceps tendon.
Maricar et al. gathered data from 23 previous studies with regard to the accuracy of intra-articular injections administered via various approaches14. According to their systematic review, the superolateral patellar approach without ultrasonography had a higher success rate (87%) than the medial midpatellar approach (64%) and the anterolateral joint line approach (70%). In their systematic review, Hermans et al. reported that the superolateral patellar approach resulted in the highest pooled accuracy of 91%15. These systematic reviews included patients in whom a substantial amount of synovial fluid was present. In our current study, the superolateral patellar approach was performed only for subjects with a suprapatellar bursa anterior-posterior dimension of ≤2 mm (minimal synovial fluid accumulation), which means that conditions were more difficult. Nevertheless, the results indicated that isometric contraction of the quadriceps led to a high success rate of 93.3%.
Lockman reported that confirmation by palpation was difficult for obese patients and other patients with a thick layer of subcutaneous fat; as a result, he developed an approach that used the apex of the patella and the femur as anatomical landmarks6. However, we could not find any previous studies of methods in which patients were directed to consciously contract the quadriceps and articularis genus muscles. The isometric quadriceps contraction method in the present study is a type of superolateral patellar approach, which was reported by Maricar et al. to have the highest success rate.
Park et al. reported that the success rate of intra-articular injections using the superolateral patellar approach was 83.7% without ultrasound guidance and 96.0% with ultrasound guidance11. The accuracy of the isometric quadriceps contraction method is near that of the ultrasound guidance method.
Ultrasound equipment is not always available. As a result, many physicians perform intra-articular injections without ultrasonography. When physicians rely only on the sense of touch, there are many subjects for whom it is difficult to ascertain whether the needle has entered the suprapatellar bursa. The use of the isometric quadriceps contraction technique allows for more accurate and successful intra-articular injections even for these subjects without using sonography.
One limitation of this study was that it was not an ideal randomized controlled trial; because of the quasi-randomization, randomness was not guaranteed. However, the background factors showed no bias between the 2 groups (Table I), and double-blinding was not applicable in this study because we compared the methods of injection. In light of the methodology and relatively small sample size of this current study, further studies with randomization and a larger sample size are needed.
In conclusion, the isometric quadriceps contraction method can expand the suprapatellar bursa and improve the accuracy of intra-articular injections. We believe that this method is a highly useful injection technique for knees with osteoarthritis without effusion.
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, Wada Orthopaedic Clinic, Hirakata, Japan, and the Department of Orthopaedic Surgery, Kashiba Asahigaoka Hospital, Kashiba, Japan
Disclosure: There was no source of external funding for this study. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A73).
References
- 1.Jones A, Regan M, Ledingham J, Pattrick M, Manhire A, Doherty M. Importance of placement of intra-articular steroid injections. BMJ. 1993. November 20;307(6915):1329-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glattes RC, Spindler KP, Blanchard GM, Rohmiller MT, McCarty EC, Block J. A simple, accurate method to confirm placement of intra-articular knee injection. Am J Sports Med. 2004. June;32(4):1029-31. [DOI] [PubMed] [Google Scholar]
- 3.Jackson DW, Evans NA, Thomas BM. Accuracy of needle placement into the intra-articular space of the knee. J Bone Joint Surg Am. 2002. September;84(9):1522-7. [DOI] [PubMed] [Google Scholar]
- 4.Wojtys EM, Beaman DN, Glover RA, Janda D. Innervation of the human knee joint by substance-P fibers. Arthroscopy. 1990;6(4):254-63. [DOI] [PubMed] [Google Scholar]
- 5.Konttinen YT, Tiainen VM, Gomez-Barrena E, Hukkanen M, Salo J. Innervation of the joint and role of neuropeptides. Ann N Y Acad Sci. 2006. June;1069:149-54. [DOI] [PubMed] [Google Scholar]
- 6.Lockman LE. Practice tips. Knee joint injections and aspirations: the triangle technique. Can Fam Physician. 2006. November;52(11):1403-4. [PMC free article] [PubMed] [Google Scholar]
- 7.Salaffi F, Ciapetti A, Carotti M. The sources of pain in osteoarthritis: a pathophysiological review. Reumatismo. 2014. June 6;66(1):57-71. [DOI] [PubMed] [Google Scholar]
- 8.Wiler JL, Costantino TG, Filippone L, Satz W. Comparison of ultrasound-guided and standard landmark techniques for knee arthrocentesis. J Emerg Med. 2010. July;39(1):76-82. Epub 2008 Dec 5. [DOI] [PubMed] [Google Scholar]
- 9.Bum Park Y, Ah Choi W, Kim YK, Chul Lee S, Hae Lee J. Accuracy of blind versus ultrasound-guided suprapatellar bursal injection. J Clin Ultrasound. 2012. January;40(1):20-5. Epub 2011 Oct 28. [DOI] [PubMed] [Google Scholar]
- 10.Lueders DR, Smith J, Sellon JL. Ultrasound-guided knee procedures. Phys Med Rehabil Clin N Am. 2016. August;27(3):631-48. [DOI] [PubMed] [Google Scholar]
- 11.Park Y, Lee SC, Nam HS, Lee J, Nam SH. Comparison of sonographically guided intra-articular injections at 3 different sites of the knee. J Ultrasound Med. 2011. December;30(12):1669-76. [DOI] [PubMed] [Google Scholar]
- 12.Sibbitt WL, Jr, Kettwich LG, Band PA, Chavez-Chiang NR, DeLea SL, Haseler LJ, Bankhurst AD. Does ultrasound guidance improve the outcomes of arthrocentesis and corticosteroid injection of the knee? Scand J Rheumatol. 2012. February;41(1):66-72. Epub 2011 Nov 21. [DOI] [PubMed] [Google Scholar]
- 13.Im SH, Lee SC, Park YB, Cho SR, Kim JC. Feasibility of sonography for intra-articular injections in the knee through a medial patellar portal. J Ultrasound Med. 2009. November;28(11):1465-70. [DOI] [PubMed] [Google Scholar]
- 14.Maricar N, Parkes MJ, Callaghan MJ, Felson DT, O’Neill TW. Where and how to inject the knee—a systematic review. Semin Arthritis Rheum. 2013. October;43(2):195-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hermans J, Bierma-Zeinstra SM, Bos PK, Verhaar JA, Reijman M. The most accurate approach for intra-articular needle placement in the knee joint: a systematic review. Semin Arthritis Rheum. 2011. October;41(2):106-15. [DOI] [PubMed] [Google Scholar]
- 16.Toda Y, Tsukimura N. A comparison of intra-articular hyaluronan injection accuracy rates between three approaches based on radiographic severity of knee osteoarthritis. Osteoarthritis Cartilage. 2008. September;16(9):980-5. Epub 2008 Mar 12. [DOI] [PubMed] [Google Scholar]
- 17.Lopes RV, Furtado RNV, Parmigiani L, Rosenfeld A, Fernandes ARC, Natour J. Accuracy of intra-articular injections in peripheral joints performed blindly in patients with rheumatoid arthritis. Rheumatology (Oxford). 2008. December;47(12):1792-4. Epub 2008 Sep 27. [DOI] [PubMed] [Google Scholar]
- 18.Luc M, Pham T, Chagnaud C, Lafforgue P, Legré V. Placement of intra-articular injection verified by the backflow technique. Osteoarthritis Cartilage. 2006. July;14(7):714-6. Epub 2006 Apr 18. [DOI] [PubMed] [Google Scholar]
- 19.Esenyel C, Demirhan M, Esenyel M, Sonmez M, Kahraman S, Senel B, Ozdes T. Comparison of four different intra-articular injection sites in the knee: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2007. May;15(5):573-7. Epub 2006 Dec 6. [DOI] [PubMed] [Google Scholar]
- 20.Bevers K, Zweers MC, van den Ende CH, Martens HA, Mahler E, Bijlsma JW, Wakefield RJ, van den Hoogen FH, den Broeder AA. Ultrasonographic analysis in knee osteoarthritis: evaluation of inter-observer reliability. Clin Exp Rheumatol. 2012. Sep-Oct;30(5):673-8. Epub 2012 Oct 17. [PubMed] [Google Scholar]
- 21.Ishida Y, Carroll JF, Pollock ML, Graves JE, Leggett SH. Reliability of B-mode ultrasound for the measurement of body fat and muscle thickness. Am J Hum Biol. 1992;4(4):511-20. [DOI] [PubMed] [Google Scholar]
- 22.Kwah LK, Pinto RZ, Diong J, Herbert RD. Reliability and validity of ultrasound measurements of muscle fascicle length and pennation in humans: a systematic review. J Appl Physiol (1985). 2013. March 15;114(6):761-9. Epub 2013 Jan 10. [DOI] [PubMed] [Google Scholar]
- 23.Tarhan S, Unlu Z. Magnetic resonance imaging and ultrasonographic evaluation of the patients with knee osteoarthritis: a comparative study. Clin Rheumatol. 2003. September;22(3):181-8. [DOI] [PubMed] [Google Scholar]
- 24.Kimura K, Takahashi Y. M. articularis genus. Observations on arrangement and consideration of function. Surg Radiol Anat. 1987;9(3):231-9. [DOI] [PubMed] [Google Scholar]
- 25.Woodley SJ, Latimer CP, Meikle GR, Stringer MD. Articularis genus: an anatomic and MRI study in cadavers. J Bone Joint Surg Am. 2012. January 4;94(1):59-67. [DOI] [PubMed] [Google Scholar]
- 26.Toscano AE, Arruda de Moraes SR, Da Silva Almeida KS. The articular muscle of the knee: morphology and disposition. Int J Morphol. 2004;22(4):303-6. [Google Scholar]
- 27.Sakuma E, Sasaki Y, Yamada N, Wada I, Soji T. Morphological characteristics of the deep layer of articularis genus muscle. Folia Morphol (Warsz). 2014. August;73(3):309-13. [DOI] [PubMed] [Google Scholar]
- 28.Bianchi S, Zamorai MP. US guided interventional procedures. In: Bianchi S, Martinoli C, editors. Ultrasound of the musculoskeletal system. 1st ed. Berlin: Springer; 2007. p 891. [Google Scholar]
- 29.Grob K, Gilbey H, Manestar M, Ackland T, Kuster MS. The anatomy of the articularis genus muscle and its relation to the extensor apparatus of the knee. JBJS Open Access. 2017;2(4):e0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hirsch G, O’Neill T, Kitas G, Klocke R. Distribution of effusion in knee arthritis as measured by high-resolution ultrasound. Clin Rheumatol. 2012. August;31(8):1243-6. Epub 2012 Apr 24. [DOI] [PubMed] [Google Scholar]