Abstract
Malnutrition in all its forms has risen on global and national agendas in recent years because of the recognition of its magnitude and its consequences for a wide range of human, social, and economic outcomes. Although the WHO, national governments, and other organizations have endorsed targets and identified appropriate policies, programs, and interventions, a major challenge lies in implementing these with the scale and quality needed to achieve population impact. This paper presents an approach to implementation science in nutrition (ISN) that builds upon concepts developed in other policy domains and addresses critical gaps in linking knowledge to effective action. ISN is defined here as an interdisciplinary body of theory, knowledge, frameworks, tools, and approaches whose purpose is to strengthen implementation quality and impact. It includes a wide range of methods and approaches to identify and address implementation bottlenecks; means to identify, evaluate, and scale up implementation innovations; and strategies to enhance the utilization of existing knowledge, tools, and frameworks based on the evolving science of implementation. The ISN framework recognizes that quality implementation requires alignment across 5 domains: the intervention, policy, or innovation being implemented; the implementing organization(s); the enabling environment of policies and stakeholders; the individuals, households, and communities of interest; and the strategies and decision processes used at various stages of the implementation process. The success of aligning these domains through implementation research requires a culture of inquiry, evaluation, learning, and response among program implementers; an action-oriented mission among the research partners; continuity of funding for implementation research; and resolving inherent tensions between program implementation and research. The Society for Implementation Science in Nutrition is a recently established membership society to advance the science and practice of nutrition implementation at various scales and in varied contexts.
Keywords: implementation science, policies, programs, interventions, effectiveness, impact, research, knowledge utilization, collaboration, capacity
Introduction
Malnutrition in all its forms has risen on global and national agendas in recent years because of the recognition of its magnitude and its consequences for a wide range of human, social, and economic outcomes (1, 2). The Scaling Up Nutrition Movement, the resolutions and targets from the World Health Assembly, and the placement of nutrition targets within the Sustainable Development Goals are among the many examples of this increased attention (3–6). Despite this unprecedented attention, and the availability of a number of evidence-based interventions (7), the Global Nutrition Report (6) observed that only about one-third of countries are on track for achieving the global stunting target, roughly one-half are on track for the wasting and exclusive breastfeeding targets, and virtually none are on track for anemia in reproductive-aged women and adult overweight and obesity. There are also extreme variations in the national coverage and prevalence of key recommended practices to improve nutrition across countries, which masks even greater inequities at subnational levels (8). This demonstrates the persistent and significant gaps between global targets and actual achievements.
These observations highlight the profound challenge of translating the current evidence base and collective will into effective and sustainable actions that result in impact at scale. It is not enough to know that a nutrition intervention is efficacious; it is also necessary to know how to identify barriers, build upon strengths, and address weaknesses in actions in real-world conditions. The growing recognition of the critical importance of addressing the “implementation gap” has stimulated interest in developing and applying implementation science (IS) in nutrition (ISN).
The purpose of this article is to describe an approach to ISN that builds upon concepts developed in other policy domains and addresses critical gaps in linking knowledge to effective action. In the next section, we describe key concepts, frameworks, and principles for ISN drawn from earlier literature, followed by a series of brief case studies illustrating the various purposes and forms of implementation research (IR). We conclude with a discussion of immediate and longer-term strategies and priorities for advancing this emerging field of science and practice.
Concepts, Frameworks, and Principles for ISN
The rationale for developing and applying ISN is the same as that found in many other problem areas and policy domains: namely, to close the gap between what is known about efficacious interventions and what is actually achieved in practice. This gap is seen, for example, in health care (9), public health (10, 11), education (12), and public policy, broadly (13, 14). The literature from these other policy domains provides helpful conceptual foundations and principles for ISN, including the need to recognize: 1) the wide range of “objects” that must be implemented to improve population nutrition (e.g., nutrition-specific interventions, sectoral or multisectoral policies, and innovative practices and delivery mechanisms); 2) the wide range of factors, decisions and processes that can affect the quality and impact of implementation (e.g., political support, financing, organizational capacities and community receptivity); 3) the diverse forms of knowledge (and methods to generate it) that are required to enhance implementation quality (e.g., capacity assessments, formative research, operations research, quality improvement schemes and effectiveness trials); 4) the need to support access to and utilization of new and existing implementation knowledge by policymakers, planners, and implementers (e.g., via technical assistance, knowledge brokering and practical tools and guidelines); and 5) the need for researchers and implementers to collaborate at many points in the research cycle when planning and generating new implementation knowledge, such as in setting research priorities, advocating for IR funding, designing studies, interpreting findings, and applying findings. Text Box 1 illustrates some of the models and mechanisms being used to facilitate such collaboration in the case of NIH-related initiatives.
TEXT BOX 1 INNOVATIVE COMMUNICATION AND COLLABORATION PLATFORMS FOR IS IN GLOBAL HEALTH: EXPERIENCE FROM NIH
Premised on the idea that support for IS alone will have limited impact unless coupled with concerted efforts to bring researchers together with policymakers and program implementers, the Center for Global Health Studies (CGHS) at the Fogarty International Center, NIH has been experimenting with curating and hosting innovative platforms that enhance communication and catalyze collaboration among funded IS researchers, policymakers, and program implementers to promote a cross-fertilization of ideas, insights, and experiences. The first “platform” experiment CGHS undertook was the NIH President's Emergency Plan for AIDS Relief preventing mother-to-child transmission (PEPFAR PMTCT) Implementation Science Alliance (the Alliance) https://www.fic.nih.gov/About/center-global-health-studies/Pages/pmtct-prevent-mother-child-transmission-hiv.aspx. The Alliance was launched as a kind of “living laboratory” and provided an important opportunity to explore:
how to build, strengthen, and nurture interactions between researchers and those who utilize research evidence;
whether this type of model can catalyze positive results for implementation and global health; and
the potential to catalyze new collaborations, increase IS capacity, and seed important sustainable activities to address the implementation challenges related to prevention of mother-to-child transmission of HIV.
Building on the Alliance's successes, CGHS has initiated and continues to host 3 additional similar networks aimed at addressing intractable implementation challenges related to global health:
the Learning Collaborative for Implementation Science in Global Brain Disorders (https://www.fic.nih.gov/About/center-global-health-studies/Pages/learning-collaborative-implementation-science-global-brain-disorders.aspx);
the Clean Cooking Implementation Science Network (https://www.fic.nih.gov/About/Staff/Policy-Planning-Evaluation/Pages/clean-cooking-implementation-science-network.aspx); and
the Adolescent HIV Prevention and Treatment Implementation Science Alliance (AHISA) (https://www.fic.nih.gov/About/center-global-health-studies/Pages/adolescent-hiv-prevention-treatment-implementation-science-alliance.aspx).
Although each is slightly different, all of these initiatives implicitly value the importance of supporting shared learning among stakeholders and that providing a platform for enhanced interaction between researchers, decision-makers, and program implementers can catalyze positive results for IS and global health.
These principles highlight that IS must acknowledge the larger system of factors that affect implementation, knowledge production, and knowledge utilization if it is to fulfill its promise to improve the quality and impact of implementation. More empirical research by itself, even if it focuses on implementation issues, will not be sufficient. This is the difference between IS (as an integrated set of principles and activities) and IR (as a subset of activities devoted to generating new empirical knowledge). These concepts and principles are integrated into the definitions and frameworks for ISN below.
A definition and frameworks for implementation
Implementation involves “systematic and planned efforts within a system (or organization) to introduce and institutionalize a policy, plan, program, intervention, guideline, innovation, or practice and ensure its intended effects and impacts.”
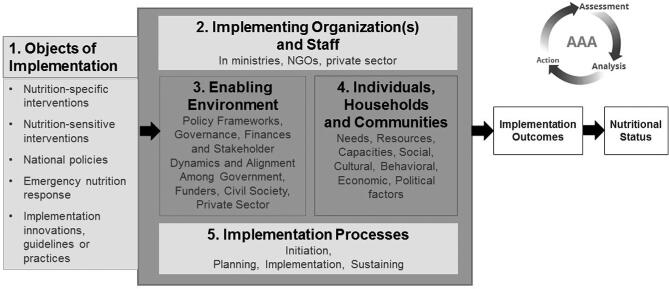
This definition acknowledges the many different objects of implementation noted above (e.g., “pills, policies, programs and practices”) and underscores the need not only to introduce these into organizations or communities, but also to ensure they have the intended effects and impacts and can sustain them. Doing so requires the ability to identify, assess, and address the wide range of factors that can compromise quality, effectiveness, and sustainability. A number of frameworks have been developed to guide such work, including, for example, 1 for micronutrient interventions (15), another for breastfeeding (16), and another for nutrition-specific and nutrition-sensitive interventions (17). This in in addition to the 61 frameworks in the literature outside nutrition (18). There are many common elements across these frameworks, including staff and organizational capacities, governance, contextual factors, financing and planning, implementation, and evaluation processes. Given the considerable diversity of interventions, policies, and practices in nutrition, and of implementation settings and organizations, we developed a generic framework adapted from an earlier literature review (19), which provides a robust frame of reference deemed useful across most applications (Figure 1). This framework calls attention to the characteristics, capacities, and dynamics of factors within and among 5 domains:
The object of implementation (e.g., a supplement compared with a multisectoral program) and their varied requirements for high-quality implementation;
The implementing organizations and staff [e.g., nongovernmental organizations (NGOs), ministries of health or agriculture, private sector entities];
The broader enabling environment, including policy frameworks, governance, and a diverse range of stakeholders;
Individuals, households, communities and community actors; and
Implementation processes (from initiation through sustaining).
FIGURE 1.
Five domains whose characteristics, capacities, dynamics, and fit affect implementation quality. NGO, nongovernmental organization. Adapted from reference 19.
These 5 domains can be used to guide implementation planning and to identify the need for various forms of IR before and during implementation in an iterative manner. This is suggested by the Triple A Cycle (Assessment, Analysis, and Action) in the figure.
These 5 domains are presented in Figure 1 in their simplest form, analogous to the simple presentation of the “food, health, care” framework for the determinants of malnutrition (20). Their utility for some purposes lies precisely in their simplicity. However, just as each of the “food, health and care” determinants of malnutrition fails to reveal the large number of factors and the complexity underlying each of them, Figure 1 also fails to reveal important details and complexity underlying each of the 5 domains. Supplemental Figure 1 illustrates this greater complexity based on an adaptation of the 37 factors identified in earlier literature review (19). This more detailed framework is a summary of current knowledge concerning the wide range of factors that might affect implementation, to varying extents in various settings, that researchers, evaluators, and consultants can draw upon when discussing and planning implementation and IR. It can be adapted to different project, program, and policy contexts, and is likely to be updated or modified over time based on IR and experience.
A definition and classification of IR
With the above framework in mind, IR is defined as “a variety of methods of assessment, inquiry and formal research whose purpose is to systematically assess, build on strengths and address potential weaknesses within and between each of the five domains that affect implementation.”
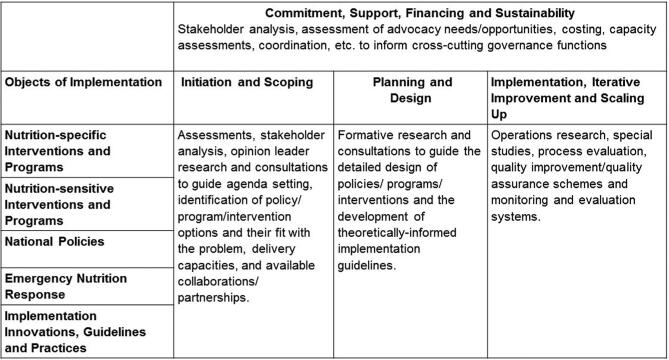
As depicted in Figure 1 and Supplemental Figure 1, Domain 5 refers to implementation processes that can be classified into 4 broad, overlapping and often iterative “phases” of implementation:
Initiation and Scoping, including identification of policy/program/intervention options and their fit with the problem, delivery platforms, and capacities, available collaborations or partnerships, and available resources.
Planning and Design, which involves making adaptations to evidence-based and/or promising interventions, along with detailed decisions regarding inputs, activities, and implementation strategies.
Implementation, Iterative Improvement, and Scaling Up, which includes the roll out, expansion, and full implementation phases. It is during these phases that many unanticipated design or implementation problems arise. These must be assessed and addressed early on and at various stages of implementation, adaptation, and scale-up, and various methods exist to support these assessments (e.g., operations research, special studies, rapid assessments, process evaluations, and routine monitoring).
Governance, Commitment, Stakeholder Dynamics, Financing, and Sustainability, which are processes pertaining to the enabling environment and are relevant throughout each of the other 3 phases rather than during a distinct phase.
IR can take many forms, depending on which of the 5 domains or 4 phases of implementation is the focus of concern. For instance, IR could take the form of rigorous evaluations of pilot or larger-scale implementation trials, with or without comparison groups, and with or without randomization at household or community level—depending on the decisions it is intended to inform. In the case of IR, such trials would assess aspects such as the acceptability, feasibility, effectiveness, cost, and implementation challenges under real-world conditions, rather than evaluating the efficacy of technical nutrition interventions under controlled conditions. Formal IR trials generally involve long time horizons (months to years), and they address only certain types of implementation questions, yet they are an important and underfunded form of IR.
A broader family of methods is needed to “assess and address” the wide range of weaknesses (and strengths) in real-time implementation, in relation to the 5 domains and 4 phases. As shown in Figure 2, the potential methods include stakeholder analysis, opinion leader research, formative research, rapid assessments, operations research, special studies, process evaluation, costing studies, Delphi studies, and various forms of quality improvement or quality assurance. In other words, IR is an umbrella term that is defined by its various purposes (i.e., to inform specific implementation-relevant decisions and processes). It is flexible and eclectic in its methods. Supplemental Figure 2 provides examples of published IR in each of the cells of the IR classification scheme. There are many more examples in the files and gray literature of in-country researchers, NGOs, donors, and government agencies, but many are not yet easily located and retrievable.
FIGURE 2.
Illustration of the diverse forms of assessments, inquiries, and research before and during implementation.
An integrated framework for IS
The frameworks and classification system described here are deliberately comprehensive in order to be useful in a wide range of applications and settings. However, they also highlight an important practical dilemma: given the complexity of implementation, the many possible weaknesses in the 5 domains, and the fact that implementers cannot wait for “research findings” on all of these, it is not feasible to systematically assess and address all potential weaknesses in all of the 5 domains during all phases of the implementation process. A practical solution to this dilemma is to conceptualize and define IS in such a way that it offers additional strategies (beyond new empirical inquiries) for addressing implementation weaknesses. Thus, IS (or “the science of implementation”) is defined here as “an interdisciplinary body of theory, knowledge, frameworks, tools and approaches whose purpose is to strengthen implementation quality and impact.” As with any science, it represents a cumulative and accumulating body of knowledge. This definition helps resolve the practical dilemma for the following reasons:
A great deal is already known about implementation, such that many of the most common mistakes could be prevented by applying current implementation (and management) knowledge rather than undertaking new investigations;
Much of this current knowledge has already been packaged by NGOs, UN agencies, and other organizations into practical tools, frameworks, and guidelines that can be adapted and used in a variety of settings;
Many of the “implementation gaps” lie in knowledge utilization, rather than knowledge production, as can be seen in the broader literature pertinent to IS;
Thus, an urgent need in nutrition implementation is to close the knowledge sharing and utilization gap by making existing practical tools, frameworks, and guidelines more readily accessible through various forms of capacity building, technical assistance, coaching, knowledge brokering, and dissemination.
The foregoing considerations emphasize the fact that IS includes, but is not limited to, new empirical investigations as a means to improve implementation. It also includes the application of frameworks, guidelines, and tools from the emergent and cumulative science of implementation, which can provide more immediate, practical, and efficient ways to address many of the weaknesses in the 5 domains.
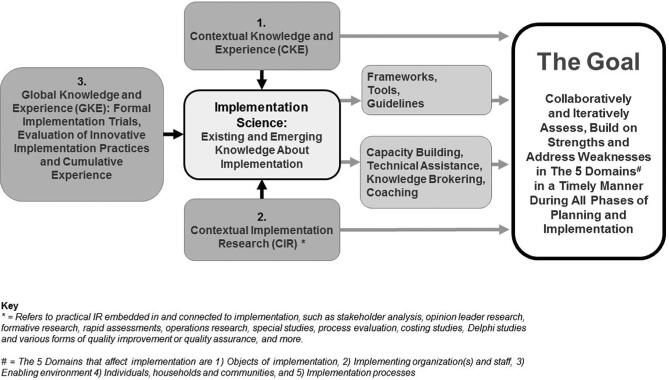
Figure 3 brings together the concepts presented in this paper into a single picture depicting key elements of the theory and practice of ISN. The shared goal is to “Assess, build on strengths and address weaknesses, in varied domains, in a timely manner, during all phases of implementation.” The framework shows that this goal can be pursued by drawing upon existing and emerging knowledge about implementation (“the science of implementation”), with attention to 3 broad and complementary categories of knowledge:
Global Knowledge and Experience (GKE): The most immediate and practical way to assess and address implementation issues in an entire system is to draw upon existing and emerging knowledge on the science of implementation. A great deal of such knowledge exists (conveniently packaged into frameworks, tools, and guidelines, as noted above) but it typically is underutilized because it is widely dispersed, and planners and implementers typically do not have the time, means, or incentives to locate, adapt, and apply it. For this reason, efforts are needed to curate this large body of knowledge products, and strategies are needed to facilitate its access and utilization through knowledge brokering (21), and tailored capacity building, technical assistance, and coaching (22, 23). The development and evaluation of such strategies are a high-priority topic for future IR (24, 25). The GKE category also includes the (often tacit) knowledge and experience of practitioners who have confronted similar implementation challenges in other settings and often have found practical solutions. This can be shared through traditional in-person exchanges (conferences, etc.) as well as through virtual means [e.g., communities of practice (26), among others]. Finally, the GKE category includes the findings from formal and rigorous trials and evaluations of interventions at scale, innovative implementation practices (e.g., for training, supervision, reporting, performance-based incentives, etc.), and other forms of research that may have broad applicability across countries and contexts.
Contextual Implementation Research (CIR): Although GKE can address many implementation tasks and challenges, there is typically also a need for various forms of practical, timely, empirical inquiries and assessments in a specific country or programmatic context, to identify or clarify the weaknesses, strengths, and bottlenecks in various domains and phases, and to adapt interventions to local contexts during the planning phase. The most common example is formative research to assist the design and implementation of interventions, but as noted, CIR involves a much wider range of purposes and methods (e.g., operations research, special studies, rapid assessments, etc.). One of the challenges in CIR is to define “acceptable methodological rigor” that will generate trustworthy results in a given case but also will meet the needs and timetables of decision-makers. In most cases, it is inappropriate to adopt the high standards of evidence used in conventional (efficacy) research, which seeks to clarify causal relations under tightly controlled conditions and operates on different time horizons.
Contextual Knowledge and Experience (CKE): CKE refers to the often tacit knowledge and experience of planners, implementers, and others who possess intimate knowledge of contextual features that can have profound implications for the performance and prospects for a policy, program, intervention, or innovation. This includes, for instance, knowledge of: stakeholder relations, histories, and dynamics; capacity strengths and weaknesses in various organizations or districts; what has or has not worked, where, when, how, why; what is actually happening (or not) in a program or district at the present time; how to navigate formal and informal administrative procedures; who may have influence with whom; etc. CKE plays a vital role in many aspects of implementation, such as adapting actions, innovations, and implementation strategies to the context; rapidly identifying bottlenecks; designing and interpreting CIR, generating and sustaining organizational or political support, and so on. CKE is such a ubiquitous element in the entire planning and implementation process that it can be taken for granted, yet there are important reasons to recognize its presence and its potential strengths and weaknesses. Specifically, its tacit and subjective nature may cause it to be dismissed or undervalued as opinion or anecdotal; if accepted uncritically, it can lead to faulty decisions, just as with other forms of knowledge; and efforts to systematize and codify it can transform it into explicit rather than tacit knowledge, thereby allowing it to play a greater role in the existing and emerging science of implementation. A wide range of strategies exist for stress-testing, systematizing, and strengthening CKE, such as triangulation, participatory procedures, pile sorting, concept mapping, and Delphi studies, among others (27–32). An important contribution in this regard is the Program Reporting Standards recently developed by WHO that aim to capture program implementation experience more systematically and accurately (33).
FIGURE 3.
An integrated framework for implementation science in nutrition.
Implications of the framework
Although elements of the ISN framework may seem intuitive, its implications are profound and call into question many conventional practices in research and implementation. For example, the framework and its associated principles caution against the following common practices or tendencies: 1) generating new knowledge through field research while neglecting the utilization of existing knowledge, tools, and frameworks from the existing science of implementation; 2) “privileging” scientific knowledge while overlooking the value of contextual, experiential, and tacit knowledge; 3) emphasizing rigorous trials while neglecting the diverse methods for contextual inquiries; 4) emphasizing research on certain objects of implementation (such as nutrition-specific interventions) and neglecting others (such as nutrition-sensitive actions, national multisectoral agendas, and implementation innovations); 5) conducting research on field-level implementation processes while neglecting the problems and bottlenecks at the other 3 stages in the implementation cycle; 6) strengthening capacity of implementing organizations and staff (through training) while neglecting critical bottlenecks in the other 4 domains; and 7) failing to establish effective linkages and collaborations when planning, conducting, and applying the findings from IR. In short, the ISN suggests a need for significant changes in the norms and conventions in research and implementation communities, as well as in the organizations that fund and govern them.
Illustrations of IR in Nutrition
IR is defined by its objectives and not by the type of methods or study designs. The following examples are illustrative of IR during different phases (Figure 2) and do not constitute a definitive review of approaches and methodologies. The first example highlights the application of IR to support initiation and scoping to move from policy to program design and implementation. The second example describes the process of making the results of IR accessible to inform feasible program planning and adaptation; it is also an example of “bridging” between investigators and program implementers to facilitate knowledge mobilization. The third example illustrates a long-term and emergent program of IR to improve program design and delivery at scale. The final example illustrates the application of IR to support multiple phases, including initiation and scoping, planning and design, and iterative improvement.
Moving from policy to program in Mozambique: Testing the feasibility of implementation delivery platforms
In response to the high prevalence of malnutrition in the country, the Ministry of Health of Mozambique developed in 2010 a comprehensive action plan (34), detailing policy related to a number of nutrition interventions. Within the context of counseling to improve infant and young child feeding practices (IYCF), and aligned with recent WHO guidance (35), the government recommended the inclusion of micronutrient powders (MNP). Many development partners work closely with the Ministry of Health, and a few were asked to pilot MNPs as part of IYCF programs across different regions of the country. In 2 districts of Sofala Province, Global Alliance for Improved Nutrition, Save the Children, and Population Services International supported the Ministry of Health to pilot a model using a voucher distribution system (representing an Innovation as the Object of Implementation in Domain 1 of Figure 1). A formative evaluation was conducted by the Global Alliance for Improved Nutrition (GAIN) and Division of Nutrition, Physical Activity, and Obesity, CDC, to assess the viability of a model to deliver MNP and motivate adherence to recommendations regarding its use. Mothers of children 6–23 mo of age were provided with IYCF counseling, as part of ongoing Ministry of Health and Save the Children programs, and vouchers that could be redeemed for MNPs at community vendors of Population Services International's existing sales platform (to increase accessibility and alleviate burden on the public health system). The evaluation assessed elements of implementing organizations (Domain 2) and of the individuals, households, and communities (Domain 4). For example, the delivery of the vouchers for MNPs was affected by factors in the organizations themselves as well as their staff at multiple levels, and the redemption, acceptance, and utilization were affected (positively and negatively) by numerous factors at the individual, household, and community level (36). The evidence generated here, together with other delivery models being tested by other partners across the country, will inform potential for scale-up nationally.
Resolving implementation challenges with micronutrient powders and counseling in Bangladesh
Since 2010, Bangladesh Rural Advancement Committee (BRAC) has included MNPs in the package of goods sold by Shasthya Shebikas—community volunteers trained to provide counseling related to good IYCF practices and several other health and nutrition-related messages. This case study highlights the use of a collaborative model that recognized the critical role of generating rigorous evidence on diverse elements of implementation, but also ensured that the questions asked and the proposed responses to address implementation challenges were feasible and acceptable to program implementers.
The Shasthya Shebikas are unpaid by the program but earn a small income from providing services such as identification of pregnancy, prenatal, and postnatal services, as well as from the sales of the goods in their package, and may receive incentives if they meet BRAC program sales targets. During the first phase, the program was implemented across 61 districts (Bangladesh has 64 districts), in collaboration with GAIN and with funding from the Bill & Melinda Gates Foundation; this phase had a rigorous process and impact evaluation. The evaluation revealed high acceptance of the MNPs but low coverage and utilization; less emphasis on counseling on IYCF; several challenges related to the product itself (supply gaps and challenges in forecasting supply needs); and challenges related to the reliance on the Shasthya Shebikas and the frequency with which they visited the households (37). Despite these challenges, the program was perceived to have a high potential for impact (38), and funding was obtained from the Children's Investment Fund Foundation to adapt the program to focus more attention to optimal IYCF, including MNP as part of the package in 27 districts and 6 urban slums with a high risk of malnutrition. BRAC and The International Center for Diarrheal Disease Research, Bangladesh, worked with Children's Investment Fund Foundation and GAIN to prioritize IR questions, identify appropriate study approaches to address them (including, for example, bottle-neck analyses and in-depth qualitative interviews to identify barriers and opportunities for improved implementation, and testing a revised model of delivery in a small randomized trial), interpret results, and identify feasible program modifications for implementation and for further testing. GAIN (and international NGO) served as the coordinator and knowledge broker, ensuring that the needs of each of the program partners are met. The program evaluation is now testing a number of the adaptations made as a result of the IR, including: strengthened training and job aids for all workers; the implementation of a standardized behavior change strategy in collaboration with Social Marketing Company and building on the IYCF Strategy of the Ministry of Health and Family Welfare, Government of Bangladesh; smooth supply procurement and management; and a number of new initiatives to improve program implementation suggested by research at various stages. The results of these evaluations will be available in late 2018.
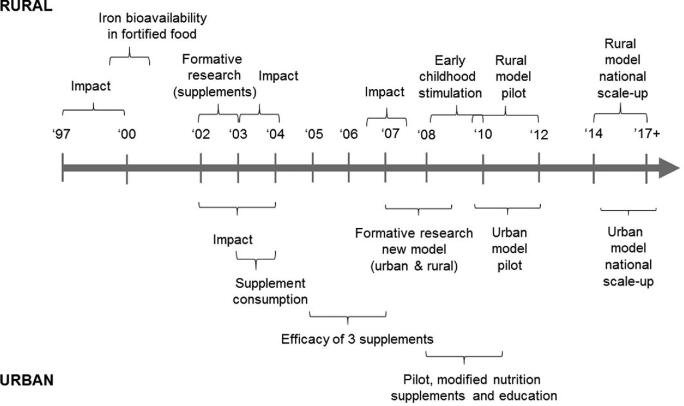
Long-term investments in IR to strengthen program design and implementation: The case of Mexico's social protection program
In 1997, Mexico piloted at small scale (∼100,000 households) a social protection program (then named “Progresa”) that included cash transfers, the receipt of which was conditional on a number of “coresponsibilities,” including attending preventive health care and health and nutrition education sessions. Fortified complementary foods (for children 6–23 mo of age, and those 2–4 y of age with malnutrition) and a supplementary food for pregnant and lactating women were among the services provided. The pilot program was found to be highly effective in rigorous impact evaluation (39, 40) and, as a result, was gradually scaled up and has now formed the cornerstone of Mexican social protection for nearly 20 y (the name was changed to Oportunidades for some years and is now Prospera). Despite continued positive impacts (41, 42), there were a few challenges related to 1) the design and implementation of the many components of the complex program (43, 44); 2) diversity in the prevalence and determinants of nutrition problems across regions and subgroups of the population as the program rolled out nationally, including the obesity epidemic (45); and 3) the growing body of evidence nationally and globally on potential interventions to address these challenges. Over 20 y, a series of IR studies were carried out (Figure 4) involving close collaboration among the National Institute of Public Health Mexico, the program itself (including the evaluation unit), the Inter-American Development Bank, and the World Bank, which provided loan and grant funds to the Government of Mexico for the program, and the Secretary of Health (who implemented the nutrition component) (46). Over the years, the diverse studies touched on all elements of implementation, including but not limited to: constraints in the coordination mechanisms across the multiple sectors involved in the program; staff knowledge, skills, time, and other constraints and motivations of staff; acceptance, constraints and factors that favored program utilization broadly and the nutrition components specifically; and testing alternative packages of interventions to address malnutrition, among others. The results of this body of work culminated in the redesign of the nutrition component of the program. Three key areas of change included 1) the types of supplements provided—ensuring that they met both biological criteria (i.e., responded to the nutritional issues in the population), and acceptance criteria to ensure high potential to be used as intended, tested in a rigorous randomized trial before implementing (47–50); 2) an overhaul of the communications and interpersonal counseling component, designed based on formative research results and pilot-tested; and 3) working closely with the Secretary of Health, a redesign of the training and supervision strategy within the health system. The changes were pilot-tested at a small scale, and based on results (51, 52), now rolled out at national scale. Other novel program modifications, for example the addition of an existing early childhood stimulation program to the package of interventions, were tested in a large randomized trial (53) and have not been implemented as such but have highlighted and increased attention to early childhood stimulation. In the context of the 20th anniversary of the program, lessons learned from the evaluation and IR are being consolidated and will be shared nationally and internationally over the coming year(s).
FIGURE 4.
Selected implementation research studies conducted to support the Prospera Social Protection Program, Mexico. Unpublished data, reproduced with permission from Lynnette Neufeld.
Highlighting challenges in delivery of essential nutrition interventions across the continuum of care to support nutrition strategy in Odisha: An example of initiation and scoping
The state of Odisha in eastern India is characterized by high levels of undernutrition and poverty, but a strong commitment to the social sector, and positive changes over time in the scale-up of multiple interventions (54). Starting in 2011, a team of researchers from the International Food Policy Research Institute (IFPRI), under the Partnerships and Opportunities to Strengthen and Harmonize Actions for Nutrition in India (POSHAN) initiative (55), began work on examining the scope and scale of the reach of nutrition-specific interventions in India. Focusing on a few states, including Odisha, the POSHAN team engaged in research and policy engagement that assessed the national policy frameworks for intervention delivery (56), program experiences with delivering essential nutrition interventions (57), and state-specific research to examine the coverage and reach of interventions across the continuum of care (58). The research team also simultaneously designed a study aimed at understanding and examining the issue of “intersectoral convergence,” honing in on issues of convergence between frontline workers in 2 national programs run by 2 different ministries—the Integrated Child Development Services and the National Rural Health Mission. The results of the research highlighted that 1) on aspects of intervention coverage and delivery, support for IYCF counseling was most limited; and 2) part of the challenge was the lack of role clarity among frontline workers in the 2 national programs and the limited ownership of interventions such as counseling by both national programs. Intersectoral convergence itself was stronger in Odisha, where program managers at all levels shared a commitment to reducing infant mortality, conducted joint reviews, and issued joint government orders, among other actions, to support frontline implementation (59). Challenges identified in relation to IYCF counseling scaling up, even in an overall supportive environment, included limited investments in training and the absence of monitoring indicators for counseling. Since 2012, the IFPRI team continued to collaborate and engage with the government of Odisha and supported their investments in nutrition through widespread sharing of research findings along with stakeholder convening to synthesize and interpret new data on nutrition in Odisha (through state and district nutrition profiles) and disseminate findings from an analysis of the factors that had supported nutrition policy efforts in Odisha over the last 2 decades. IFPRI's engagement continued with the Odisha government's working group on nutrition, which contributed to the Odisha Nutrition Action Plan (60) and specifically recognized the need to strengthen program activities to ensure full scale implementation of all nutrition-specific interventions, support complementary feeding counseling and support, and engage frontline workers in the Integrated Child Development Services and the National Rural Health Mission more effectively around provision of core interventions across the continuum of care. Looking forward, the IFPRI/POSHAN research team is building a continuing engagement with Odisha to strengthen the evidence base on implementation of nutrition interventions, including analyses of survey data on intervention coverage, estimations of the costs of scaling up, and possible IR studies on delivery of interventions across the continuum of care, especially for interventions such as counseling and support for behavior change.
Success factors for IR in nutrition
In reviewing the case studies and other experiences of IR efforts in nutrition, 3 facilitating factors stand out:
A culture of evaluation and inquiry among program implementers and an action-oriented mission and orientation among the research partners. These distinctive norms and practices, among program staff and researchers alike, are critical to ensure that joint planning and communication throughout the process are prioritized and respected. Including a third-party individual or organization to foster the knowledge mobilization, or to act as knowledge broker, can help bridge the gap between research and programs, and facilitate an explicit process to foster a sense of ownership and commitment on both sides.
Continuity of funding and commitment to programmatic improvement. Although many IR studies identify and address specific design and implementation constraints and opportunities, they often identify additional challenges along the way. Implementation is a dynamic process, and the situations in which programs are implemented change. Prioritizing budgetary allocations for an ongoing agenda of program improvement and supportive research, and fostering the commitment, and mechanisms to permit that, is vital to ensure that longstanding programs can continue to be responsive to context and the ever-evolving evidence base in nutrition. Other challenges come from the fact that many programs (especially those supported by international donors) have a fixed time frame (of, say, 4—5 y) and disappear once funding terminates. Some of these programs may have identified implementation challenges, tested solutions, and generated significant relevant learning, but far too often this learning remains within the individuals and institutions that supported implementation and fails to be shared more broadly because program implementers usually have to move quickly from 1 program to the next as funding cycles evolve. This is where collaboration between researchers and program implementers is particularly valuable, because researchers may be more inclined to organize and disseminate findings from ISN to national and international networks of practitioners, government representatives, United Nations agencies, and researchers.
Resolving inherent tensions between program implementation and research: The areas of tension between programs and research are well documented and involve several elements: time and decision-making processes (61) as well as differing priorities, expectations, incentives and perceptions, and trade-offs between implementation constraints and evaluation rigor (62). Programs have been described as chronophobic and research as chronophilic, terms that capture the classic tension between programmatic stakeholders that are anxious to act and research that takes time to collect, analyze, and synthesize. Although this is often the case, there are also often programmatic constraints (in design and/or limitations) that can slow the process of adaptation in response to IR. This can be mitigated somewhat by establishing effective communication and collaboration linkages, as discussed earlier. These linkages can help ensure recommendations are grounded in contextual realities and are actionable. Joint ownership and the role of the knowledge broker to facilitate understanding and managing the challenges related to the decision-making process are critical.
Concluding Comments: Ways Forward in Developing IS in Nutrition
The success factors noted above, together with the earlier IS literature, point to the need for changes in nutrition research and nutrition-implementing communities if global and national goals and targets are to be achieved. Researchers, research organizations, and their funders must develop the capacity and commitment to support research agendas and methods that better meet the needs of implementers; implementing organizations and their funders must develop the capacity and commitment to embrace IR as a core component of their policy, program, and funding portfolios; and both sectors must develop the capacity for and practice of effective communication and collaboration. The Society for Implementation Science in Nutrition (SISN) was formed in 2016 as a means to catalyze and support these goals and changes (63) including some immediate priorities (Text Box 2). SISN is a membership society (that includes researchers, implementers, and other stakeholders), but the changes indicated above clearly will require a much larger effort. The formation of IS networks, alliances, or chapters at country level would be a strategically important approach for creating linkages among researchers, implementers, policymakers, and funders at precisely the level where they are most needed.
TEXT BOX 2 SOME IMMEDIATE PRIORITIES FOR DEVELOPING AND PROMOTING IS IN NUTRITION
Implementation science curriculum development
Guidance on IS research methods
Funded opportunities for short- and medium-term IS capacity development
Collections of case studies of IS in nutrition
Small grants programs for IR on specific topics or in specific countries or programs
A curated set of tools to strengthen a variety of implementation decisions and process
Analysis and description of the distinctive requirements for various objects of implementation
Experience-based guidance on mechanisms for creating effective linkages between researchers, implementers, and policymakers
Guidance for deploying innovative mechanisms for technical assistance, knowledge brokering, and coaching to facilitate evidence uptake
Supplementary Material
Acknowledgments
We thank the Interim Secretariat (Jean-Pierre Habicht, Jessica Johnston, Rolf Klemm, Klaus Kraemer, Eva Monterrosa, and Gretel Pelto) and the Founding Members who initiated the creation of the Society as well as the financial and staff support provided by Sight and Life. We also thank Kesso Gabrielle van Zutphen for the skillful editorial assistance in preparing an earlier version of this paper. The authors’ responsibilities were as follows—DP: carried out much of the drafting and integration of input; LN, RS: provided additional content for some of the brief case studies based on presentations in an ASN Symposium on IS organized by SISN; and all authors: read and approved the final manuscript.
Notes
Society for Implementation Science in Nutrition, address to be provided
The Society for Implementation Science in Nutrition (SISN) did not receive any specific funding for the production of this paper, nor for the ASN symposium in 2017 upon which it is based. Three of the authors (DP, LN, RS) presented at that symposium, and the travel expenses for RS were paid by SISN. SISN receives unrestricted funding from Sight and Life, a humanitarian think-tank of Royal DSM, which is a purpose-led global science-based company in Nutrition, Health and Sustainable Living. SISN is a 501(c)(3) nonprofit membership organization: https://www.implementnutrition.org/
Author disclosures: The authors have no conflicts of interest. The views expressed here are those of the authors and not their employers.
Supplemental Figures 1 and 2 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/cdn/.
This paper is the product of multiple rounds of drafting and discussion among SISN Board Members in the course of forming SISN, developing its strategic plan and disseminating its core concepts through presentations and webinars.
Abbreviations used: BRAC, Bangladesh Rural Advancement Committee; CGHS, Center for Global Health Studies; CIR, Contextual Implementation Research; CKE, Contextual Knowledge and Experience; GAIN; Global Alliance for Improved Nutrition; GKE, Global Knowledge and Experience; IFPRI, International Food Policy Research Institute; IR, implementation research; IS, implementation science; ISN, implementation science in nutrition; IYCF, infant and young child feeding practices; MNP, micronutrient powder; NGOs, nongovernmental organizations; POSHAN, Partnerships and Opportunities to Strengthen and Harmonize Actions for Nutrition in India; SISN, Society for Implementation Science in Nutrition.
References
- 1. Gakidou E, Afshin A, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abdulle AM, Abera SF, Aboyans V et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet North Am Ed 2017;390:1345–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Bank Repositioning nutrition as central to development: A strategy for large scale action. Washington, DC: The World Bank; 2006. [Google Scholar]
- 3. Scaling Up Nutrition Scaling up nutrition movement [Internet]. 2018[cited 2018 April 7]; Available from: http://scalingupnutrition.org/. [Google Scholar]
- 4. Organization WH Global action plan for the prevention and control of noncommunicable diseases 2013–2020. 2013. [Google Scholar]
- 5. World Health Organization Nutrition: Maternal, infant and young child nutrition: Draft comprehensive implementation plan. Geneva: World Health Organization; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Initiatives D. Global nutrition report 2017: Nourishing the SDGs. Bristol, UK: Development Initiatives; 2017. [Google Scholar]
- 7. Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, Haider BA, Kirkwood B, Morris SS, Sachdev H. What works? Interventions for maternal and child undernutrition and survival. Lancet North Am Ed 2008;371:417–40. [DOI] [PubMed] [Google Scholar]
- 8. Bhutta ZA. Nutrition: How will the next ‘Decade of Nutrition’ be different from the past one? Nat Rev Gastroenterol Hepatol 2016;13:441–2. [DOI] [PubMed] [Google Scholar]
- 9. Glasgow RE, Vinson C, Chambers D, Khoury MJ, Kaplan RM, Hunter C. National Institutes of Health approaches to dissemination and implementation science: current and future directions. Am J Public Health 2012;102:1274–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Peters D, Tran N, Adam T. Implementation research in health: A practical guide. Geneva, Switzerland: Alliance for Health Policy and Systems Research, World Health Organization; 2013. [Google Scholar]
- 11. Schackman BR. Implementation science for the prevention and treatment of HIV/AIDS. J Acquir Immune Defic Syndr 2010;55:S27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. Implementation research: A synthesis of the literature. Tampa, FL: National Implementation Research Network; 2005. [Google Scholar]
- 13. National Research Council Using science as evidence in public policy. Washington, DC: National Academies Press; 2012. [Google Scholar]
- 14. Nilsen P, Stahl C, Roback K, Cairney P. Never the twain shall meet? A comparison of implementation science and policy implementation research. Implement Sci 2013;8:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Menon P, Covic NM, Harrigan PB, Horton SE, Kazi NM, Lamstein S, Neufeld L, Oakley E, Pelletier D. Strengthening implementation and utilization of nutrition interventions through research: A framework and research agenda. Ann N Y Acad Sci 2014;1332:39–59. [DOI] [PubMed] [Google Scholar]
- 16. Perez-Escamilla R, Curry L, Minhas D, Taylor L, Bradley E. Scaling up of breastfeeding promotion programs in low- and middle-income countries: The “breastfeeding gear” model. Adv Nutr 2012;3:790–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gillespie S, Menon P, Kennedy AL. Scaling up impact on nutrition: what will it take? Adv Nutr Int Rev J 2015;6:440–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tabak R, Khoong E, Chambers D, Brownson R. Bridging research and practice: Models for dissemination and implementation research. Am J Prev Med 2012;43:337–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement Sci 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. UNICEF Strategy for improved nutrition of children and women in developing countries UNICEF policy review. New York: UNICEF; 1991. [DOI] [PubMed] [Google Scholar]
- 21. Glegg SM, Hoens A. Role domains of knowledge brokering: A model for the health care setting. J Neurol Phys Ther 2016;40:115–23. [DOI] [PubMed] [Google Scholar]
- 22. Wandersman A, Chien VH, Katz J. Toward an evidence-based system for innovation support for implementing innovations with quality: Tools, training, technical assistance, and quality assurance/quality improvement. Am J Community Psychol 2012;50:445–59. [DOI] [PubMed] [Google Scholar]
- 23. Nadeem E, Gleacher A, Beidas RS. Consultation as an implementation strategy for evidence-based practices across multiple contexts: Unpacking the black box. Admin Policy Mental Health Mental Health Serv Res 2013;40:439–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chew S, Armstrong N, Martin G. Institutionalising knowledge brokering as a sustainable knowledge translation solution in healthcare: How can it work in practice? Evid Policy 2013;9. [Google Scholar]
- 25. Ward VL, House AO, Hamer S. Knowledge brokering: Exploring the process of transferring knowledge into action. BMC Health Serv Res 2009;9:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Li LC, Grimshaw JM, Nielsen C, Judd M, Coyte PC, Graham ID. Use of communities of practice in business and health care sectors: A systematic review. Implement Sci 2009;4:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Watt AM, Hiller JE, Braunack-Mayer AJ, Moss JR, Buchan H, Wale J, Riitano DE, Hodgetts K, Street JM, Elshaug AG. The ASTUTE Health study protocol: Deliberative stakeholder engagements to inform implementation approaches to healthcare disinvestment. Implement Sci 2012;7:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Leshabari SC, Koniz-Booher P, Åstrøm AN, de Paoli MM, Moland KM. Translating global recommendations on HIV and infant feeding to the local context: The development of culturally sensitive counselling tools in the Kilimanjaro Region, Tanzania. Implement Sci 2006;1:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cabassa LJ, Gomes AP, Meyreles Q, Capitelli L, Younge R, Dragatsi D, Alvarez J, Manrique Y, Lewis-Fernández R. Using the collaborative intervention planning framework to adapt a health-care manager intervention to a new population and provider group to improve the health of people with serious mental illness. Implement Sci 2014;9:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tso P, Culyer AJ, Brouwers M, Dobrow MJ. Developing a decision aid to guide public sector health policy decisions: A study protocol. Implement Sci 2011;6:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Becerril-Montekio V, Alcalde-Rabanal J, Darney BG, Orozco-Nuñez E. Using systematized tacit knowledge to prioritize implementation challenges in existing maternal health programs: Implications for the post MDG era. Health Policy Plan 2016;31:1031–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Waltz TJ, Powell BJ, Matthieu MM, Chinman MJ, Smith JL, Proctor EK, Damschroder LJ, Kirchner JE. Innovative methods for using expert panels in identifying implementation strategies and obtaining recommendations for their use. Implement Sci 2015;10:A44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Koek I, Monclair M, Anastasi E, ten Hoope-Bender P, Higgs E, Obregon R. Doing what we do, better: Improving our work through systematic program reporting. Global Health Sci Pract 2018;6:257–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Government of the Republic of Mozambique Multisectorial plan for chronic malnutrition reduction in Mozambique 2011–2014. Maputo: Government of the Republic of Mozambique; 2010. [Google Scholar]
- 35. World Health Organization Use of multiple micronutrient powders for point-of-use fortification of foods consumed by infants and young children aged 6–23 months and children aged 2–12 years—guideline. Geneva: World Health Organization; 2016. [PubMed] [Google Scholar]
- 36. Vossenaar M, Kjaer K, Vettersand J, Possolo E, Pelto G Jefferds ME Norte A dos Santos Dias K Osman N Gonzalez W et al. Mixed methods formative evaluation identifies and explains caregiver bypassing of vouchers in micronutrient powder trial in Sofala Province, Mozambique. Maternal and Child Nutrition 2019(in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rawat R, Saha K, Kennedy A, Ruel M, Menon P. Sale of micronutrient powders (MNPs) by frontline workers (FLWs) enables high reach, but low uptake limits impact on anemia and iron status: A cluster randomized study in Bangladesh. FASEB J 2015;29:391.6. [Google Scholar]
- 38. Afsana K, Haque MR, Sobhan S, Shahin SA. BRAC's experience in scaling-up MNP in Bangladesh. Asia Pac J Clin Nutr 2014;23:377–84. [DOI] [PubMed] [Google Scholar]
- 39. Rivera JA, Sotres-Alvarez D, Habicht JP, Shamah T, Villalpando S. Impact of the Mexican program for education, health, and nutrition (Progresa) on rates of growth and anemia in infants and young children: A randomized effectiveness study. JAMA 2004;291:2563–70. [DOI] [PubMed] [Google Scholar]
- 40. Fernald LC, Gertler PJ, Neufeld LM. Role of cash in conditional cash transfer programmes for child health, growth, and development: An analysis of Mexico's Oportunidades. Lancet 2008;371:828–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Leroy JL, Garcia-Guerra A, Garcia R, Dominguez C, Rivera J, Neufeld LM. The Oportunidades program increases the linear growth of children enrolled at young ages in urban Mexico. J Nutr 2008;138:793–8. [DOI] [PubMed] [Google Scholar]
- 42. Fernald LC, Gertler PJ, Neufeld LM. 10-year effect of Oportunidades, Mexico's conditional cash transfer programme, on child growth, cognition, language, and behaviour: A longitudinal follow-up study. Lancet 2009;374:1997–2005. [DOI] [PubMed] [Google Scholar]
- 43. Neufeld LM, Steta Cn, Rivera J, Martinez Valle A, Grados R, Uriega S, López VH. Evaluation for program decision making: A case study of the oportunidades program in Mexico. J Nutr 2011;141:2076–83. [DOI] [PubMed] [Google Scholar]
- 44. Bonvecchio A, Pelto G, Escalante E, Monterrubio E, Habicht J, Nava F, Villanueva M, Safdie M, Rivera J. Maternal knowledge and use of a micronutrient supplement was improved with a programmatically feasible intervention in Mexico. J Nutr 2007;137:440. [DOI] [PubMed] [Google Scholar]
- 45. Neufeld LM, M-RF, Fernández-Gaxiola CA. The Nutritional status of children under 2 and their mothers. In: External evaluation of Oportunidades 2008. 1997–2007: 10 years of intervention in rural areas. México City: Secretaría de Desarrollo Social Coordinación Nacional del Programa de Desarrollo Humano Oportunidades; 2008. [Google Scholar]
- 46. Neufeld LM, Steta C, Rivera J, Valle AM, Grados R, Uriega S, López VH. Evaluation for program decision making: A case study of the oportunidades program in Mexico. J Nutr 2011;141:2076–83. [DOI] [PubMed] [Google Scholar]
- 47. Neufeld LM, Dominguez CP, Guerra AG, Feregrino RG, Cabrera AH. Effect of three supplements with identical micronutrient content on length and weight of Mexican children. FASEB J 2008;22:44.1. [Google Scholar]
- 48. Aburto NJ, Ramirez-Zea M, Neufeld LM, Flores-Ayala R. The effect of nutritional supplementation on physical activity and exploratory behavior of Mexican infants aged 8–12 months. Eur J Clin Nutr 2010;64:644–51. [DOI] [PubMed] [Google Scholar]
- 49. Flores L, Théodore F, Bonvecchio A, Blanco I, Neufeld LM. Acceptability of three supplements with identical micronutrient content in Mexican children. FASEB J 2008;22:677.2–.2. [Google Scholar]
- 50. Young SL, Blanco I, Hernandez-Cordero S, Pelto GH, Neufeld LM. Organoleptic properties, ease of use, and perceived health effects are determinants of acceptability of micronutrient supplements among poor Mexican women. J Nutr 2010;140:605–11. [DOI] [PubMed] [Google Scholar]
- 51. Garcia-Guerra A, Neufeld LM, Quezada AD, Fernandez-Gaiola AC, Hernandez-Cabrera A, Bonvecchio A, Lozada AL, Rivera J. The Integrated Strategy for Attention in Nutrition (EsIAN) reduces the prevalence of anemia in children 6 to 59 months in the context of a conditional cash-transfer program in Mexico. 2015. [Google Scholar]
- 52. Fernandez-Gaxiola AC, Garcia-Guerra A, Neufeld LM, Quezada-Sanchez AD, Hernandez-Cabrera A, Bonvecchio A, Lozada AL, Rivera J. An integrated strategy for attention in nutrition (EsIAN) increases physicians’ and nurses’ nutrition knowledge and perceptions in Mexico. 2015.
- 53. Fernald LC, Kagawa R, Knauer HA, Schnaas L, Guerra AG, Neufeld LM. Promoting child development through group-based parent support within a cash transfer program: Experimental effects on children's outcomes. Dev Psychol 2017;53:222. [DOI] [PubMed] [Google Scholar]
- 54. Kohli N, Avula R, van den Bold M, Becker E, Nisbett N, Haddad L, Menon P. What will it take to accelerate improvements in nutrition outcomes in Odisha? Learning from the past. Global Food Security 2017;12:38–48. [Google Scholar]
- 55. POSHAN POSHAN [Internet]. 2015. [cited 2017 August 25]; Available from: http://poshan.ifpri.info. [Google Scholar]
- 56. Vir S, Sreenath KC, Bose V, Chauhan K, Mathur S, Menon P. National policies and strategic plans to tackle undernutrition in India: A review. In: 2. PRN, editor New Delhi, India: International Food Policy Research Institute; 2014. [Google Scholar]
- 57. Avula R, Kadyala S, Singh K, Menon P. The operational evidence base for delivering direct nutrition interventions in India: A desk review. In: 01299 IFPRIDP, editor Washington, DC; 2013. [Google Scholar]
- 58. Avula R, Kim SS, Chakrabarti S, Tyagi P, Kohli N, Menon P. Delivering for nutrition in Odisha: Insights from a study on the state of essential nutrition interventions. POSHAN Report No. 7 New Dehli, India: International Food Policy Research Institute; 2015. [Google Scholar]
- 59. Kim SS, Avula R, Ved R, Kohli N, Singh K, van den Bold M, Kadiyala S, Menon P. Understanding the role of intersectoral convergence in the delivery of essential maternal and child nutrition interventions in Odisha, India: A qualitative study. BMC Public Health 2017;17:161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. The Telegraph Goal to make children grow—State ties up with Azim Premji for kids’ nutrition plan [internet]. 2016. [cited 2017 August 25]; Available from: https://www.telegraphindia.com/1161223/jsp/odisha/story_126236.jsp. [Google Scholar]
- 61. Frenk J. Balancing relevance and excellence: organizational responses to link research with decision making. Soc Sci Med 1992;35:1397–404. [DOI] [PubMed] [Google Scholar]
- 62. Leroy JL, Olney DK, Ruel MT. Evaluating nutrition-sensitive programs: challenges, methods, and opportunities. In: Covic NH, Hendriks SL, editors. Achieving a nutrition revolution for Africa: The road to healthier diets and optimal nutrition. Washington, DC: International Food Policy Research Institute; 2016. p. 130–46. [Google Scholar]
- 63. SISN Society for Implementation Science in Nutrition. [cited July 2, 2018]; Available from: https://www.implementnutrition.org/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.