Abstract
Background
Evidence of an association between exposure to domestic violence and abuse (DVA) and use of emergency contraception (EC) is lacking in the UK.
Aim
To quantify the association between exposure to DVA and consultations for EC in general practice.
Design and setting
Nested case-control study in UK general practice.
Method
Using the Clinical Practice Research Datalink, the authors identified all women all women aged 15–49 years registered with a GP between 1 January 2011 and 31 December 2016. Cases with consultations for EC (n = 43 570) were each matched on age and GP against four controls with no consultations for EC (n = 174 280). The authors calculated odds ratios (ORs) and 95% confidence intervals (CIs) for the association between exposure to DVA in the previous year and consultations for EC. Covariates included age, ethnicity, socioeconomic status, pregnancy, children, alcohol misuse, and depression.
Results
Women exposed to DVA were 2.06 times more likely to have a consultation for EC than unexposed women (95% CI = 1.64 to 2.61). Women aged 25–39 years with exposure to DVA were 2.8 times more likely to have a consultation for EC, compared with unexposed women (95% CI = 2.08 to 3.75). The authors found some evidence of an independent effect of exposure to DVA on the number of consultations for EC (OR 1.48, 95% CI = 0.99 to 2.21).
Conclusion
A request for EC in general practice can indicate possible exposure to DVA. Primary care consultation for EC is a relevant context for identifying and responding to DVA as recommended by the World Health Organization and National Institute for Health and Care Excellence guidelines. DVA training for providers of EC should include this new evidence.
Keywords: contraception, domestic violence, emergency contraception, general practice, intimate partner violence, postcoital, primary health care
INTRODUCTION
Domestic violence and abuse (DVA) encompass ‘any incident or pattern of incidents of controlling, coercive, threatening behaviour, violence or abuse between those aged 16 or over who are, or have been, intimate partners or family members’.1 Although experienced across the sexes, health consequences of DVA are reported as being worse among women, mainly impacting on their mental and reproductive health.2 Two systematic reviews have found an association between exposure to DVA and reduction in use of regular contraception.3,4 The authors’ recent systematic review found some evidence for a positive association between exposure to DVA and use of emergency contraception (EC).5 However, none of these reviews included UK studies.
The negative impact of DVA on health results in higher presentation of women exposed to DVA among healthcare service users compared with general populations. Between 7 and 17% of female patients in general practice reported experiencing DVA in the previous year.6–8 National and international health organisations identify primary care providers as an important point of contact for victims of DVA and survivors.9–12 Patients perceive healthcare professionals as being well placed to enquire about DVA and respond to disclosure.13 World Health Organization (WHO)12 and National Institute for Health and Care Excellence (NICE)11 guidelines recommend a case-finding or clinical enquiry approach to DVA identification, prompted by clinical conditions associated with DVA. Recommended initial response to disclosure should follow the WHO LIVES principles: Listen, Inquire about needs and concerns, Validate, Enhance safety, provide Support.14 A number of DVA resources for healthcare professionals are available in the UK,15–18 including the Identification and Referral to Improve Safety (IRIS) model — a training, support, and referral programme for general practice19–22 and sexual health services,23,24 currently implemented across 30 administrative areas. None of the existing DVA training sources includes presentation for EC as a condition associated with DVA that should trigger clinical enquiry. As the association between DVA and use of EC can be influenced by the country context, such as access to EC,25,26 it is important to obtain the UK evidence to inform national clinical guidance and training resources on DVA. New evidence will inform clinicians’ decision making on DVA clinical enquiry, and potentially lead to more women with experience of DVA accessing evidence-based interventions.
How this fits in
Professional awareness of clinical associations of domestic violence and abuse (DVA) is a first step towards the evidence-based healthcare response recommended by the World Health Organization and National Institute for Health and Care Excellence. This study’s findings fill the gap in evidence from UK primary care on the association between exposure to DVA and increased use of emergency contraception (EC). This study found that a request for EC in general practice can indicate possible exposure to DVA. A consultation for EC is an appropriate context for asking about DVA, responding supportively, and offering referral to specialist DVA services.
This study aimed to fill a gap in the UK-based evidence by quantifying the association between exposure to DVA and general practice consultation for EC. The primary objective was to estimate the association between exposure to DVA and consultations for EC. The secondary objective was to estimate whether there is an association between exposure to DVA and having multiple consultations for EC. The authors hypothesised that exposure to DVA is associated with an increase in EC consultations.
METHOD
Study design
The authors conducted a nested case-control study in the Clinical Practice Research Datalink (CPRD), which contains anonymised electronic primary care records for approximately 17 million patients registered at 718 participating general practices in the UK.27 Patients registered during any time period and meeting quality criteria monitored by the CPRD (about 15 million) are considered broadly representative of the UK population with regards to age, sex, and ethnicity. The time from the date when practice data were considered to meet CPRD standards for quality and completeness is defined as the period of up-to-standard (UTS) registration. CPRD data are recorded by general practice clinicians using version 2 Read codes, a hierarchical clinical classification system containing >96 000 codes.28 Prescriptions are automatically recorded with a product name and British National Formulary code.
The authors used CPRD data on patient demographics, consultations (medical codes), and prescriptions (product codes) recorded by clinicians as part of their usual medical practice. For each variable, one researcher ran searches and compiled a draft list of Read and drug codes,29 which was revised by two academic GPs and cross-referenced with comparable code lists from the online clinical codes repository30 and the authors’ previous studies,19 leading to the final version of codes for data extraction (further details are available from the authors on request).
Participants
The authors identified female patients aged 15–49 years (the WHO definition of reproductive age)31 with any period of registration at a general practice between 1 January 2011 and 31 December 2016. From this cohort, the authors identified all women with at least one record of EC consultation within the study period (cases). The date of the first EC consultation was defined as the case’s index date (or index consultation).
Each case was matched on age (year of birth ± 2 years) and general practice, with up to four controls who had no record of EC consultation within the study period and were randomly selected from the study population. Controls inherited the index date of their matched case. All patients were required to have at least 1 complete year of UTS medical history before their index date.
Potential controls were excluded if they had any indication that they would not have been eligible for, or needed, EC. The full list of inclusion and exclusion criteria, with justification, is available from the authors on request.
Variables
Exposure and outcomes
Primary outcome (an index consultation for EC) was the first occasion on which any EC Read or drug code from the authors’ list was entered in the patient medical record. Secondary outcome (multiple consultation for EC) was defined as having more than one consultation for EC, occurring >1 week apart and within 12 months after the index consultation (to increase the likelihood that records relate to separate events occurring within a relatively short time period).
Exposure to DVA was defined as the first retrospective record of any CPRD code for DVA within 12 months before the index consultation for EC, to meet the UK Home Office definition of DVA and allow an adequate window for exposure to affect the outcome (further details are available from the authors on request.
Covariates
The authors extracted CPRD and linkage data on known factors that affect women’s use of contraception.4 CPRD covariates included age (year of birth) and history of alcohol abuse (Read codes for any records of alcoholism, alcohol dependency, or alcohol induced disease since the age of 15 years), or depression (Read and drug codes for any records of depression or depressive episode within 2 years before the index date)30 (further details are available from the authors on request).
Other covariates were extracted from datasets linked to CPRD. Information about patient ethnicity (white, black, Asian, mixed, other) was obtained via linkage to the Hospital Episode Statistics (HES) dataset. Socioeconomic status (quintiles of Indices of Multiple Deprivation [IMD]) was identified via linkage to the 2015 English IMD32 (2011 lower layer super output area [LSOA] boundaries). Information about number of pregnancies was obtained from the CPRD pregnancy register, which contains details about all pregnancies identified in the CPRD using an algorithm developed to identify and maximise the use of records relating to the timing and duration of pregnancy, the type of pregnancy outcome (live birth, stillbirth, or pregnancy loss), and additional features pertaining to the pregnancy. The authors identified the number of children for each woman using the CPRD mother–baby link, which contains data on mother–baby pairings, linked using an algorithm that matches live births to maternal records in the CPRD. No restrictions relating to use of data from UTS time only within a practice are imposed, and therefore may include children born before the practice became UTS and those who initially registered at a different practice after birth, but subsequently joined the current practice.
Statistical analysis
Statistical analyses were performed using STATA version 15. The authors used univariable and multivariable conditional logistic regression models to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for the association between record for DVA exposure and consultations for EC. The choice of analysis allowed the authors to take into account matched sets of cases and controls, among whom unmeasured confounders are assumed equal.
Multiple imputation for missing ethnicity or socioeconomic status was not performed, as the necessary data to inform the imputation were not available. The authors conducted an analysis of all subjects, excluding ethnicity and socioeconomic status from the model, and an analysis of complete cases adjusting for all covariates.
Secondary analysis used univariable and multivariable logistic regression to model the association between exposure to DVA and multiple consultations for EC among cases.
RESULTS
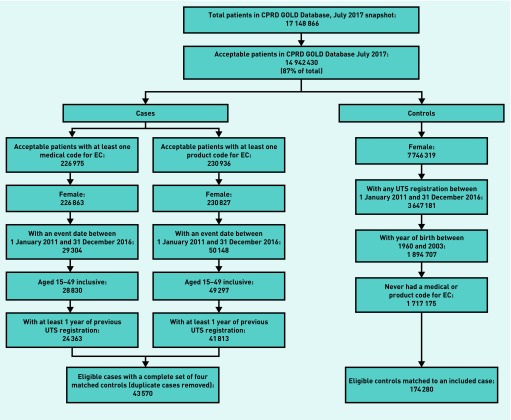
The authors identified 43 570 eligible cases and 174 280 matched controls (Figure 1).
Figure 1.
Flow diagram reporting numbers of patients at each stage of the study.
CPRD = Clinical Practice Research Datalink.
EC = emergency contraception. UTS = up to standard.
Cases and controls were similar in terms of age, ethnicity, and socioeconomic status (Table 1). Cases tended to have had more pregnancies and to have more children, and were more likely to have a history of depressive episodes.
Table 1.
Demographic and patient characteristics of women who had a consultation for emergency contraception (cases), and women who did not have a consultation for emergency contraception (controls)
| Variable | Cases, n (%) | Controls, n (%) | |
|---|---|---|---|
| Previous 12 months’ experience of domestic violence and abusea | No | 43 418 (99.65) | 174 108 (99.90) |
| Yes | 152 (0.35) | 172 (0.10) | |
|
| |||
| Mean age, years (standard deviation) | 28.46 (8.29) | 28.46 (8.41) | |
|
| |||
| Age categories, years | 15–24 | 15 844 (36.36) | 63 510 (36.44) |
| 25–39 | 22 545 (51.74) | 89 410 (51.30) | |
| 40–49 | 5181 (11.89) | 21 360 (12.26) | |
|
| |||
| Ethnicity | White | 17 986 (41.28) | 56 450 (32.39) |
| Black | 1001 (2.30) | 2033 (1.17) | |
| Asian | 1065 (2.44) | 3848 (2.21) | |
| Mixed | 389 (0.89) | 800 (0.46) | |
| Other | 354 (0.81) | 1370 (0.79) | |
| Missing | 22 775 (52.27) | 109 779 (62.99) | |
|
| |||
| Socioeconomic status (quintiles of level of deprivation) | Least deprived: 1 | 4419 (10.14) | 19 991 (11.47) |
| 2 | 4665 (10.71) | 19 795 (11.36) | |
| 3 | 5140 (11.80) | 20 252 (11.62) | |
| 4 | 5437 (12.48) | 19 813 (11.37) | |
| Most deprived: 5 | 5615 (12.89) | 18 959 (10.88) | |
| missing | 18 294 (41.99) | 75 470 (43.30) | |
|
| |||
| Pregnancies, n | 0 | 15 617 (35.84) | 105 190 (60.36) |
| 1 | 7209 (16.55) | 24 178 (13.87) | |
| ≥2 | 20 744 (47.61) | 44 912 (25.77) | |
|
| |||
| Children, n | 0 | 25 426 (58.36) | 133 040 (76.34) |
| 1 | 10 623 (24.38) | 25 472 (14.62) | |
| ≥2 | 7521 (17.26) | 15 768 (9.05) | |
|
| |||
| History of alcohol misuse since age 15a | No | 43 180 (99.10) | 173 621 (99.62) |
| Yes | 390 (0.90) | 659 (0.38) | |
|
| |||
| History of depression/depressive episode within 2 yearsa | No | 39 174 (89.91) | 166 101 (95.31) |
| Yes | 4396 (10.09) | 8179 (4.69) | |
Before the index date.
In the year before the index date, 0.35% of cases and 0.10% of controls had one or more record of DVA (Table 1). Compared with women with no record of DVA, women who had experienced DVA within the year before their index date were more than three times likely to have had one or more consultations for EC (OR 3.59, 95% CI = 2.88 to 4.47) (Table 2).
Table 2.
Association of domestic violence and abuse and other covariates with having a consultation for emergency contraception, univariable analysis
| Variable | All subjects (n = 217 850) | Cases with complete data (n = 22 135) | |||
|---|---|---|---|---|---|
|
|
|
||||
| OR (95% CI) | P-value | OR (95% CI) | P-value | ||
| Previous 12 months’ experience of domestic violence and abusea | No | 1.00 | 1.00 | ||
| Yes | 3.59 (2.88 to 4.47) | <0.000 | 3.37 (1.95 to 5.81) | <0.000 | |
|
| |||||
| Age categories, years | 15–24 | 0.98 (0.92 to 1.04) | 0.415 | 0.93 (0.75 to 1.16) | 0.527 |
| 25–39 | 1.00 | 1.00 | |||
| 40–49 | 0.78 (0.72 to 0.85) | <0.000 | 0.84 (0.69 to 1.04) | 0.109 | |
|
| |||||
| Ethnicity | White | 1.00 | 1.00 | ||
| Black | 1.60 (1.46 to 1.73) | <0.000 | 1.42 (1.17 to 1.71) | <0.000 | |
| Asian | 0.87 (0.81 to 0.94) | <0.000 | 0.87 (0.74 to 1.03) | 0.099 | |
| Mixed | 1.51 (1.33 to 1.71) | <0.000 | 1.42 (1.07 to 1.90) | 0.017 | |
| Other | 0.81 (0.71 to 0.91) | <0.000 | 0.61 (0.45 to 0.82) | 0.001 | |
| Missing | 0.37 (0.36 to 0.38) | <0.000 | |||
|
| |||||
| Socioeconomic status (quintiles of level of deprivation) | Least deprived: 1 | 1.00 | 1.00 | ||
| 2 | 1.14 (1.09 to 1.20) | <0.000 | 1.07 (0.94 to 1.21) | 0.314 | |
| 3 | 1.30 (1.23 to 1.36) | <0.000 | 1.29 (1.14 to 1.47) | <0.000 | |
| 4 | 1.49 (1.41 to 1.57) | <0.000 | 1.36 (1.20 to 1.55) | <0.000 | |
| Most deprived: 5 | 1.74 (1.64 to 1.84) | <0.000 | 1.66 (1.45 to 1.91) | <0.000 | |
| Unknown | 0.36 (0.32 to 0.41) | <0.000 | |||
|
| |||||
| Pregnancies, n | 0 | 1.00 | 1.00 | ||
| 1 | 2.93 (2.83 to 3.04) | <0.000 | 2.23 (1.98 to 2.52) | <0.000 | |
| ≥2 | 5.56 (5.39 to 5.74) | <0.000 | 4.39 (3.95 to 4.88) | <0.000 | |
|
| |||||
| Children, n | 0 | 1.00 | 1.00 | ||
| 1 | 2.63 (2.55 to 2.71) | <0.000 | 1.82 (1.68 to 1.97) | <0.000 | |
| ≥2 | 3.27 (3.15 to 3.38) | <0.000 | 2.18 (1.99 to 2.39) | <0.000 | |
|
| |||||
| History of alcohol misuse since age 15a | No | 1.00 | 1.00 | ||
| Yes | 2.40 (2.11 to 2.72) | <0.000 | 2.58 (1.83 to 3.64) | <0.000 | |
|
| |||||
| History of depression/depressive episode within 2 yearsa | No | 1.00 | 1.00 | ||
| Yes | 2.32 (2.24 to 2.42) | <0.000 | 1.98 (1.77 to 2.22) | <0.000 | |
Before index date.
When included individually, potential confounding factors changed odds ratios for exposure to DVA by percentages ranging from 0.8% to 38.2%, with number of pregnancies producing the largest change. After adjusting for all covariates, women who had been exposed to DVA were two times more likely to have a consultation for EC than women with no experience of DVA (OR 2.06, 95% CI = 1.64 to 2.61) (Table 3).
Table 3.
Association of domestic violence and abuse with having a consultation for emergency contraception, multivariable conditional logistic regressions models
| Model | All subjects (n = 217 850) | Cases with complete data (n = 22 135) | |||
|---|---|---|---|---|---|
|
|
|
||||
| Adjusted OR (95% CI) | P-value | Adjusted OR (95% CI) | P-value | ||
| Previous 12 months DVAa | 3.59 (2.88 to 4.47) | <0.000 | 3.37 (1.95 to 5.81) | <0.000 | |
|
| |||||
| Previous 12 months DVAa and age categories | 3.59 (2.88 to 4.47) | <0.000 | 3.38 (1.96 to 5.84) | <0.000 | |
|
| |||||
| Previous 12 months DVAa and ethnicity | 3.43 (1.99 to 5.94) | <0.000 | |||
|
| |||||
| Previous 12 months DVAa and socioeconomic status | 3.29 (1.90 to 5.70) | <0.000 | |||
|
| |||||
| Previous 12 months DVAa and number of pregnancies | 2.22 (1.76 to 2.80) | <0.000 | 2.76 (1.57 to 4.85) | <0.000 | |
|
| |||||
| Previous 12 months DVAa and number of children | 2.85 (2.27 to 3.58) | <0.000 | 3.23 (1.85 to 5.61) | <0.000 | |
|
| |||||
| Previous 12 months DVAa and record of alcohol abuseb | 3.54 (2.84 to 4.41) | <0.000 | 3.20 (1.84 to 5.54) | <0.000 | |
|
| |||||
| Previous 12 months DVAa and record of depression/depressive episodec | 3.28 (2.63 to 4.10) | <0.000 | 3.12 (1.80 to 5.42) | <0.000 | |
|
| |||||
| Full model | 2.06 (1.64 to 2.61) | <0.000 | 2.53 (1.43 to 4.47) | 0.001 | |
|
| |||||
| Full model and previous 12 months DVAa multiplied by age interaction | 15–24 years | 1.25 (0.82 to 1.93) | 0.290 | ||
| 25–39 years | 2.78 (2.08 to 3.75) | <0.000 | |||
| 40–49 years | 1.23 (0.51 to 3.02) | 0.643 | |||
Before index date.
Since age 15, before index date.
Within 2 years before index date. DVA = domestic violence and abuse. OR = odds ratio.
There was a positive interaction between exposure to DVA and age, with the odds of EC consultation being 2.8 times greater among women aged 25–39 years with exposure to DVA, compared with those without such exposure (OR 2.78, 95% CI = 2.08 to 3.75) (Table 3).
When restricted to women with complete data for all covariates, the overall pattern of results was similar to the main analysis, that is, women who had been exposed to DVA were more than twice as likely to have a consultation for EC than women with no experience of DVA (Tables 2 and 3).
In the 12 months following their index date, 12.8% of cases had multiple consultations for EC. Demographic and patient characteristics were similar between cases who had a single consultation and cases who had multiple consultations for EC (Table 4).
Table 4.
Demographic and patient characteristics of cases who had multiple consultations for emergency contraception and women who had a single consultation for emergency contraception
| Variable | Cases with a single consultation, n (%) | Cases with multiple consultations, n (%) | |
|---|---|---|---|
| Previous 12 months domestic violence and abusea | No | 37 869 (99.68) | 5549 (99.46) |
| Yes | 122 (0.32) | 30 (0.54) | |
|
| |||
| Age categories, years | 15–24 | 13 693 (36.04) | 2151 (38.56) |
| 25–39 | 19 616 (51.63) | 2929 (52.50) | |
| 40–49 | 4682 (12.32) | 499 (8.94) | |
|
| |||
| Pregnancies, n | 0 | 13 927 (36.66) | 1690 (30.29) |
| 1 | 6204 (16.33) | 1005 (18.01) | |
| ≥2 | 17 860 (47.01) | 2884 (51.69) | |
|
| |||
| Children, n | 0 | 22 266 (58.61) | 3160 (56.64) |
| 1 | 9140 (24.06) | 1483 (26.58) | |
| ≥2 | 6585 (17.33) | 936 (16.78) | |
|
| |||
| History of alcohol misuse since age 15a | No | 37 822 (99.56) | 5550 (99.48) |
| Yes | 169 (0.44) | 29 (0.52) | |
|
| |||
| History of depression/depressive episode within 2 yearsa | No | 34 261 (90.18) | 4913 (88.06) |
| Yes | 3730 (9.82) | 666 (11.94) | |
Before the index date.
In the 12 months before their index date, 0.32% of cases with a single consultation for EC had one or more record of DVA, compared with 0.54% of cases with multiple consultations for EC (Table 4). Compared with women with no record of DVA, women who had experienced DVA within the 12 months before their index date were 1.7 times more likely to have had multiple consultations for EC (OR 1.68, 95% CI = 1.12 to 2.50) (Table 5).
Table 5.
Association of domestic violence and abuse and other covariates with having multiple consultations for emergency contraception, univariable analysis
| Variable | OR (95% CI) | P-value | |
|---|---|---|---|
| Previous 12 months domestic violence and abusea | No | 1.00 | |
| Yes | 1.68 (1.12 to 2.50) | 0.011 | |
|
| |||
| Age categories, years | 15–24 | 1.05 (0.99 to 1.12) | 0.096 |
| 25–39 | 1.00 | ||
| 40–49 | 0.71 (0.65 to 0.79) | 0.000 | |
|
| |||
| Pregnancies, n | 0 | 1.00 | |
| 1 | 1.33 (1.23 to 1.45) | 0.000 | |
| ≥2 | 1.33 (1.25 to 1.42) | 0.000 | |
|
| |||
| Children, n | 0 | 1.00 | |
| 1 | 1.14 (1.07 to 1.22) | 0.000 | |
| ≥2 | 1.00 (0.93 to 1.08) | 0.969 | |
|
| |||
| History of alcohol abuse within 2 yearsa | No | 1.00 | |
| Yes | 1.17 (0.79 to 1.74) | 0.437 | |
|
| |||
| History of depression/depressive episode within 2 yearsa | No | 1.00 | |
| Yes | 1.25 (1.14 to 1.36) | 0.000 | |
Before the index date. OR = odds ratio.
The addition of potential confounding factors to the model individually produced little change in odds ratios for exposure to DVA. When adjusted for all covariates, there was some evidence of an independent effect of exposure to DVA on the number of consultations for EC (OR 1.48, 95% CI = 0.99 to 2.21) (Table 6).
Table 6.
Association of domestic violence and abuse with having multiple consultations for emergency contraception, multivariable logistic regressions models
| Model | Adjusted OR (95% CI) | P-value | |
|---|---|---|---|
| Previous 12 months DVAa | 1.68 (1.12 to 2.50) | 0.011 | |
| Previous 12 months DVAa and age categories | 1.65 (1.11 to 2.46) | 0.014 | |
| Previous 12 months DVAa and number of pregnancies | 1.57 (1.05 to 2.34) | 0.028 | |
| Previous 12 months DVAa and number of children | 1.66 (1.11 to 2.48) | 0.013 | |
| Previous 12 months DVAa and record of alcohol abuseb | 1.67 (1.12 to 2.50) | 0.012 | |
| Previous 12 months DVAa and record of | 1.65 (1.11 to 2.47) | 0.014 | |
| depression/depressive episodec | |||
| Full model | 1.48 (0.99 to 2.21) | 0.058 | |
| Full model and previous 12 months DVAa multiplied by age interaction | 15–24 | 0.96 (0.43 to 2.17) | 0.923 |
| 25–39 | 1.67 (1.03 to 2.70) | 0.038 | |
| 40–49 | 3.44 (0.67 to 17.81) | 0.140 |
Before index date.
Since age 15, before index date.
Within 2 years before index date. DVA = domestic violence and abuse. OR = odds ratio.
The positive interaction between exposure to DVA and age remained, with the odds of having multiple consultations for EC being 1.7 times greater among women aged 25–39 years with exposure to DVA, compared to those without such exposure (OR 1.67, 95% CI = 1.03 to 2.70) (Table 6).
DISCUSSION
Summary
In this nested case-control study of UK general practice data, after adjusting for covariates, women with exposure to DVA within the past 12 months were two times more likely to have had at least one consultation for EC, compared with women with no exposure to DVA. There was also some evidence that, after adjusting for covariates, women with exposure to DVA within the past 12 months were >1.5 times more likely to have had multiple consultations for EC, compared with women without such exposure.
Strengths and limitations
The main strengths of this study are the coverage and quality of the CPRD data, and the representativeness of included cases. CPRD data are entered by clinicians during routine consultations in general practice, rather than for research purposes. As practice-based prescribing is generally electronic, prescriptions for EC will automatically be captured by GP software systems, leading to good ascertainment of cases. In addition, data quality for patients and practices are monitored by CPRD internal processes for validity and completeness, and active patients (as are included in this study) are generally representative of the UK population in terms of age and sex.27
This study’s main limitation is the under-recording of DVA in electronic medical records, which could attenuate the association between exposure to DVA and consultations for EC. The first UK study on DVA in primary care found an 83% under-recording of DVA exposure when comparing rates in electronic medical records with patient’s self-reported rates.33 Another study found that, although multiple Read codes exist for DVA, recording practices vary considerably across UK general practice.34 Additionally, there is a potential misclassification of controls, due to the increasing availability of EC from varied providers during the past 10 years.35 Though the authors’ cases sought EC through general practice, the controls could either have not used EC (true controls) or obtained it elsewhere (misclassified controls). The authors also did not adjust their models for misuse of substances other than alcohol, known to be associated with DVA.36 Their findings are also restricted to consultations for EC provided by clinicians in general practice. Data from other sources of EC provision, such as sexual and reproductive health services and community pharmacies, could not be linked to CPRD due to regulatory, technical, and logistical reasons. The authors estimate that they have captured around 30% of the total provision of EC.37 Considering these limitations, the authors anticipate that the true association between DVA and EC is higher than the results they have presented here.
Comparison with existing literature
This study supports the recent systematic review of cross-sectional studies that found some evidence for an association between exposure to DVA and increased use of EC.5 The two main reasons for seeking EC are women’s fear that the contraceptive method they used would not work, and women’s fear of unintended pregnancy after unprotected intercourse.38 A recent meta-analysis suggested a causal relationship between exposure to DVA and reduction in women’s use of regular contraception.4 The authors can further speculate that, due to the reduction in use of regular contraception, women exposed to DVA are more likely to have unprotected intercourse and therefore might need more EC compared with women unexposed to DVA. Another mechanism connecting DVA and unprotected intercourse is reproductive coercion — a pattern of male behaviour aimed at controlling women’s reproductive outcomes through birth control sabotage or pregnancy coercion.39,40
The authors’ findings are in line with the US study on the effect of DVA on contraceptive patterns, though their effect estimates are much smaller.41 Fantasia et al analysed medical records from four family planning clinics and found that exposure to DVA in the previous 12 months was associated with a 6.5-fold increase in use of EC (95% CI = 3.8 to 9.3).41 Several factors could contribute to the difference in the effect size: study settings, national differences in the provision of EC, and methods of identifying and recording exposure, outcome, and confounding variables.
The authors found some evidence that women exposed to DVA can seek EC from GPs on multiple occasions. This suggests women exposed to DVA may use EC instead of regular contraceptive methods, which they cannot access because of reproductive coercion, coercive control, or economic abuse. This is in line with the US survey in five family planning clinics which showed that women who had experienced DVA and reproductive coercion were two times more likely to report multiple use of EC in the previous 3 months (OR 2.40, 95% CI = 1.41 to 4.09).42 Reproductive coercion was not captured in the present study, which could have resulted in the smaller effect estimate. However, the authors considered the temporality of the exposure versus outcome, which was not possible in the US study.42
Implications for research and practice
Future studies should use data linkage from core providers of EC (general practice, sexual and reproductive health services, and pharmacies) to analyse the total provision of EC.
DVA interventions for primary care (for example, IRIS in the UK) should be updated to include new evidence on the association between exposure to DVA and increased use of EC. All providers of EC should be aware that a request for EC can indicate possible exposure to DVA. A consultation for EC in general practice is an appropriate context for asking about DVA and responding to disclosure in line with the WHO LIVES14 principles.
Acknowledgments
The authors wish to thank academic clinical fellows Claire Hawcroft and Kate Pitt for revising CPRD code lists.
Funding
This research was funded by the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care West (NIHR CLAHRC West) at University Hospitals Bristol NHS Foundation Trust. Natalia Lewis was supported by NIHR CLAHRC North Thames at Bart’s Health NHS Trust, and Avon Primary Care Research Collaborative. Gene Feder and Natalia Lewis were supported for this study by the NIHR Biomedical Research Centre at University Hospitals Bristol NHS Foundation Trust and the University of Bristol. The views expressed in this article are those of the authors and not necessarily those of the NHS, NIHR, or the Department of Health and Social Care.
Ethical approval
Protocol for this study was approved by the Independent Scientific Advisory Committee (ISAC) for MHRA Database Research (ref. 16_293, 1 March 2017).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Contributors
Joni Jackson and Natalia V Lewis are joint first authors.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1. Gov.UK Domestic violence and abuse, how to get help. 2018 https://www.gov.uk/domestic-violence-and-abuse (accessed 22 Oct 2018) [Google Scholar]
- 2.Feder G, MacMillan HL. Intimate partner violence. In: Goldman L, Schafer AI, editors. Goldman’s Cecil medicine. 25th edn. Philadelphia, PA: Elsevier Saunders; 2016. pp. 1629–1635. [Google Scholar]
- 3.Bergmann JN, Stockman JK. How does intimate partner violence affect condom and oral contraceptive use in the United States? A systematic review of the literature. Contraception. 2015;91(6):438–455. doi: 10.1016/j.contraception.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maxwell L, Devries K, Zionts D, et al. Estimating the effect of intimate partner violence on women’s use of contraception: a systematic review and meta-analysis. PLoS One. 2015;10(2):e0118234. doi: 10.1371/journal.pone.0118234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lewis NV, Moore THM, Feder GS, et al. Use of emergency contraception among women with experience of domestic violence and abuse: a systematic review. BMC Womens Health. 2018;18(1):156. doi: 10.1186/s12905-018-0652-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feder G, Ramsay J, Dunne D, et al. How far does screening women for domestic (partner) violence in different health care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria. Health Technol Assess. 2010;13(16):iii–iv. xi–xiii, 1–113, 137–347. doi: 10.3310/hta13160. [DOI] [PubMed] [Google Scholar]
- 7.Hegarty KL, Bush R. Prevalence and associations of partner abuse in women attending general practice: a cross-sectional survey. Aust N Z J Public Health. 2002;26(5):437–442. doi: 10.1111/j.1467-842x.2002.tb00344.x. [DOI] [PubMed] [Google Scholar]
- 8.Lokhmatkina NV, Kuznetsova OY, Feder GS. Prevalence and associations of partner abuse in women attending Russian general practice. Fam Pract. 2010;27(6):625–631. doi: 10.1093/fampra/cmq044. [DOI] [PubMed] [Google Scholar]
- 9.Royal Australian College of General Practitioners . Abuse and violence: working with our patients in general practice. 4th edn. Melbourne: RACGP; 2014. [Google Scholar]
- 10.Garcia-Moreno C, Hegarty K, d’Oliveira AFL, et al. The health systems response to violence against women. Lancet. 2015;385(9977):1567–1579. doi: 10.1016/S0140-6736(14)61837-7. [DOI] [PubMed] [Google Scholar]
- 11.National Institute for Health and Care Excellence . Domestic violence and abuse: how social care, health services, and those they work with can respond effectively. London: NICE; 2014. PH50. [Google Scholar]
- 12.World Health Organization . Responding to intimate partner violence and sexual violence against women: WHO clinical and policy guidelines. Geneva: WHO; 2013. [PubMed] [Google Scholar]
- 13.Feder GS, Hutson M, Ramsay J, Taket AR. Women exposed to intimate partner violence: expectations and experiences when they encounter health care professionals: a meta-analysis of qualitative studies. Arch Intern Med. 2006;166(1):22–37. doi: 10.1001/archinte.166.1.22. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization . Health care for women subjected to intimate partner violence or sexual violence. A clinical handbook: field testing version. Geneva: WHO; 2014. http://www.who.int/reproductivehealth/publications/violence/vaw-clinical-handbook/en/ (accessed 23 Oct 2018). [Google Scholar]
- 15.Centre for Academic Primary Care, University of Bristol RESPONDS training pack. 2015 http://www.bristol.ac.uk/primaryhealthcare/researchthemes/responds/training-pack/ (accessed 23 Oct 2018) [Google Scholar]
- 16.Department of Health and Social Care . Responding to domestic abuse: a resource for health professionals. DHSC; 2017. https://www.gov.uk/government/publications/domestic-abuse-a-resource-for-health-professionals (accessed 23 Oct 2018) [Google Scholar]
- 17.Royal College of General Practitioners Domestic violence. 2018. http://www.rcgp.org.uk/clinical-and-research/resources/a-to-z-clinical-resources/domestic-violence.aspx (accessed 23 Oct 2018).
- 18.Szilassy E, Das J, Drinkwater J, et al. Researching Education to Strengthen Primary care ON Domestic violence & Safeguarding (RESPONDS). Final report for the Department of Health, Policy Research Programme Project. Bristol: University of Bristol; 2015. [Google Scholar]
- 19.Feder G, Davies RA, Baird K, et al. Identification and Referral to Improve Safety (IRIS) of women experiencing domestic violence with a primary care training and support programme: a cluster randomised controlled trial. Lancet. 2011;378(9805):1788–1795. doi: 10.1016/S0140-6736(11)61179-3. [DOI] [PubMed] [Google Scholar]
- 20.Yeung H, Chowdhury N, Malpass A, Feder GS. Responding to domestic violence in general practice: a qualitative study on perceptions and experiences. Int J Family Med. 2012;2012:960523. doi: 10.1155/2012/960523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malpass A, Sales K, Johnson M, et al. Women’s experiences of referral to a domestic violence advocate in UK primary care settings: a service-user collaborative study. Br J Gen Pract. 2014. . [DOI] [PMC free article] [PubMed]
- 22.Devine A, Spencer A, Eldridge S, et al. Cost-effectiveness of Identification and Referral to Improve Safety (IRIS), a domestic violence training and support programme for primary care: a modelling study based on a randomised controlled trial. BMJ Open. 2012;2(3):e001008. doi: 10.1136/bmjopen-2012-001008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horwood J, Morden A, Bailey JE, et al. Assessing for domestic violence in sexual health environments: a qualitative study. Sex Transm Infect. 2018;94(2):88–92. doi: 10.1136/sextrans-2017-053322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sohal AH, Pathak N, Blake S, et al. Improving the healthcare response to domestic violence and abuse in sexual health clinics: feasibility study of a training, support and referral intervention. Sex Transm Infect. 2018;94(2):83–87. doi: 10.1136/sextrans-2016-052866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Westley E, Kapp N, Palermo T, Bleck J. A review of global access to emergency contraception. Int J Gynaecol Obstet. 2013;123(1):4–6. doi: 10.1016/j.ijgo.2013.04.019. [DOI] [PubMed] [Google Scholar]
- 26.Westley E, Schwarz EB. Emergency contraception: global challenges, new opportunities. Contraception. 2012;85(5):429–431. doi: 10.1016/j.contraception.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 27.Herrett E, Gallagher AM, Bhaskaran K, et al. Data resource profile: Clinical Practice Research Datalink (CPRD) Int J Epidemiol. 2015;44(3):827–836. doi: 10.1093/ije/dyv098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chisholm J. The Read clinical classification. BMJ. 1990;300(6732):1092. doi: 10.1136/bmj.300.6732.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dave S, Petersen I. Creating medical and drug code lists to identify cases in primary care databases. Pharmacoepidemiol Drug Saf. 2009;18(8):704–707. doi: 10.1002/pds.1770. [DOI] [PubMed] [Google Scholar]
- 30.Springate DA, Kontopantelis E, Ashcroft DM, et al. ClinicalCodes: an online clinical codes repository to improve the validity and reproducibility of research using electronic medical records. PLoS One. 2014;9(6):e99825. doi: 10.1371/journal.pone.0099825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization . Reproductive health indicators: guidelines for their generation, interpretation and analysis for global monitoring. Geneva: WHO; 2006. [Google Scholar]
- 32.Ministry of Housing, Communities and Local Government . The English indices of deprivation, 2015. MHCLG; 2015. [Google Scholar]
- 33.Richardson J, Coid J, Petruckevitch A, et al. Identifying domestic violence: cross-sectional study in primary care. BMJ. 2002;324(7332):274. doi: 10.1136/bmj.324.7332.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Drinkwater J, Stanley N, Szilassy E, et al. Juggling confidentiality and safety: a qualitative study of how general practice clinicians document domestic violence in families with children. Br J Gen Pract. 2017. . [DOI] [PMC free article] [PubMed]
- 35.FSRH CEU clinical guidance. Emergency contraception. London: FSRH RCOG; 2017. Faculty of Sexual and Reproductive Healthcare of the Royal College of Obstetricians and Gynaecologists. https://www.fsrh.org/documents/ceu-clinical-guidance-emergency-contraception-march-2017/ (accessed 23 Oct 2018) [Google Scholar]
- 36.Bacchus LJ, Ranganathan M, Watts C, Devries K. Recent intimate partner violence against women and health: a systematic review and meta-analysis of cohort studies. BMJ Open. 2018;8(7):e019995. doi: 10.1136/bmjopen-2017-019995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Office for National Statistics . Contraception and sexual health 2008–9 Opinions Survey Report No. 41. A report on research using the National Statistics Opinions Survey produced on behalf of the NHS Information Centre for health and social care. Newport: ONS; 2009. [Google Scholar]
- 38.Daniels K, Jones J, Abma J. Use of emergency contraception among women aged 15–44: United States, 2006–2010. NCHS Data Brief. 2013;(112):1–8. [PubMed] [Google Scholar]
- 39.Grace KT, Anderson JC. Reproductive coercion: a systematic review. Trauma Violence Abuse. 2018;19(4):371–390. doi: 10.1177/1524838016663935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miller E, Jordan B, Levenson R, Silverman JG. Reproductive coercion: connecting the dots between partner violence and unintended pregnancy. Contraception. 2010;81(6):457–459. doi: 10.1016/j.contraception.2010.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fantasia HC, Sutherland MA, Fontenot HB, Lee-St John TJ. Chronicity of partner violence, contraceptive patterns and pregnancy risk. Contraception. 2012;86(5):530–535. doi: 10.1016/j.contraception.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 42.Kazmerski T, McCauley HL, Jones K, et al. Use of reproductive and sexual health services among female family planning clinic clients exposed to partner violence and reproductive coercion. Mατερν Child Health J. 2015;19(7):1490–1496. doi: 10.1007/s10995-014-1653-2. [DOI] [PMC free article] [PubMed] [Google Scholar]