Abstract
Benign Paroxysmal Positional Vertigo (BPPV) is the most common cause in patients with vertigo (Pereira et al. in Braz J Otorhinolaryngol (Impr) 76(6):704–708, 2010; Dix and Hallpike in Ann Otol Rhinol Laryngol 6:987–1016, 1952). Posterior Semicircular Canal BPPV (PSCBPPV) has more incidence and prevalence then Lateral, and Anterior Semicircular Canal BPPV (Alghwiri et al. in Arch Phys Med Rehabil 93:1822–1831, 2012). Quality of life (QoL) is significantly impaired by vertigo (Sargent et al. in Otol Neurotol 22:205–209, 2001; World Health Organization in International classification of functioning, disability and health, World Health Organization, Geneva, 2001). To study the effect and compare Epley, Semont maneuvers and Brandt–Daroff Exercise on QoL in patients with PSCBPPV. 90 individuals with unilateral PSCBPPV were selected based on positive Dix–Hallpike test. 3 groups Epley, Semont, and Brandt–Daroff were formed and 30 individuals were selected in each group randomly. Dix–Hallpike test and Vestibular Activities and Participation (VAP) Scale based on International Classification of Functioning were administered before and after Epley, Semont maneuvers, and Brandt–Daroff Exercise to fulfill the aim. VAP Scale results revealed significant difference between pre and post treatment score in all 3 groups, suggestive of positive effect on QoL in patients with PSCBPPV. Improvements in VAP Score between 3 groups were compared and significant difference was observed. Dix–Hallpike test results revealed that 90, 73.33, and 50% patients improved in Epely, Semont, and Brandt–Daroff group respectively. Epely maneuver found to be the best choice and then Semont and Brandt–Daroff should be least preferred in treatment of patients with PSCBPPV.
Keywords: Posterior Semicircular Canal Benign Positional Vertigo (PSCBPPV), Vestibular Activities and Participation (VAP) Scale, Dix–Hallpike, Epley maneuver, Semont maneuver, Brandt–Daroff Exercise
Introduction
Benign paroxysmal positional vertigo (BPPV) is one of the most common causes in patients with vertigo of vestibular disorders [6, 11]. BPPV may be characterized by the symptom rotating dizziness caused by sudden changes in the position of the head, such as lying down on one or both sides, looking right or left side [6, 18].
BPPV may be divided into 3 types based on canal involvement Posterior, Horizontal, and Anterior Semicircular Canal BPPV [1]. Out of 3 Posterior Canal BPPV (PSCBPPV) is most common almost 80%, Lateral Canal BPPV is about 20%, and Anterior Canal BPPV is very rare as it is self-treated due to gravity [1]. Pathophysiology may be explained with two currents: cupulolithiasis and canallithiasis [2]. In cupulolithiasis, degenerated otoconia in the utricle adhere to the cupula of the semicircular canal, making it denser than the surrounding endolymph, and thus more susceptible to the effects of gravity. The canalithiasis theory contends that degenerated otoconia do not adhere to the cupula, but remain floating in the endolymph of the posterior canal [2]. In both theories, head movements cause the fragments to move, which stimulates the cupula of semicircular canal inappropriately and excites the ampullary nerve, resulting in vertigo.
The etiology of BPPV may involve cranial trauma, metabolic diseases, hormone dysfunction, and other conditions; in most cases, however, BPPV is idiopathic [6, 18].
The diagnosis and treatment of BPPV can significantly improve the quality of life (QoL) in patients with BPPV [9, 20]. Dix–Hallpike test is gold standard in diagnosing PSCBPPV [18]. Qol can be assessed by various scales [20].
There are several approaches to treat BPPV, such as vestibular habituation exercises, vestibular sedatives, destructive surgeries, and repositioning maneuvers. Maneuvers have been more widely adopted than the former methods. Epley, Semont maneuvers and Brandt–Daroff Exercise are used for treatment of Posterior Canal BPPV [6, 8, 16].
Subjects and Methods
Aim of present research was to study the effect and compare Epley, Semont maneuvers and Brandt–Daroff Exercise on Quality of Life in patients with PSCBPPV. Total 90 individuals were included in this study with unilateral posterior canal BPPV based on positive Dix–Hallpike test. 3 groups Epely, Semont, and Brandt–Daroff were formed and 30 individuals were selected randomly in each group. Dix–Hallpike test and Vestibular Activities and Participation (VAP) Scale based on International Classification of Functioning (ICF), Disability and Health were administered pre and post treatment to evaluate efficacy and results of 3 groups were compared to find which treatment provides better quality of life in patients with PSCBPPV.
Dix–Hallpike was administered using standard protocol, M-glasses were used to reveal the nystagmus and avoid visual fixation. In Dix–Hallpike positional test examiner moves the patient’s head to cause movement of the endolymph, thereby moving the cupula of the posterior semicircular canal. In this maneuver, patients were seated with the head rotated laterally about 45° (right or left, depending on which side is to be tested) on examination table. The examiner holds the patient’s head and rapidly moves the patient into supine position with the head extended backwards about 30°. The patient stays in this position with eyes open and nystagmus is observed. All patients had shown up beating counter clockwise torsional nystagmus confirming the diagnosis that it is posterior canal BPPV [18].
After confirmation of PSCBPPV Vestibular Activities and Participation (VAP) scale was administered. VAP includes domains like attention, daily routine, psychological demands, travelling, job, recreation, and socialization. VAP was developed by Alghwiri in 2012 in English [3]. VAP was adopted in Indian context and translated in Hindi with prior permission from author and reverse translation was done as WHO and authors recommendation. Questions were asked by the clinician and the rating was done on each task. Total score was obtained by calculating the average score without considering NA (not applicable) none = 0, Mild = 1, Moderate = 2, Severe = 3, Unable to do = 4, Maximum Score = 136, Minimum Score = 0 [3].
On completion of pre-treatment evaluation Epley and Semont maneuvers were administered using standard protocol. In the Epley maneuver, the patient was seated on examination table and head was rotated 45° toward affected side and quickly moved patient in supine position with head extended 30° causing movement of debris, inducing an attack. Then patient’s head was rotated 45° towards unaffected side, then trunk was rotated towards unaffected side in such a way that patient’s nose will be pointing towards floor, causing further movement of the debris downward toward the exit to the canal, resulting in more vertigo and nystagmus. Each position should be maintained for 2 min or at least until the provoked vertigo and nystagmus subsides. The final uprighting of the patient causes the debris to enter the utricle [7].
In Semont maneuver patient was seated on examination table with legs hanging then head was rotated 45° horizontally toward the unaffected ear. After that patient was tilted 105° so that patient was lying on the side of the affected ear with patient’s head hanging and nose pointed upward. Patient remains in this position for around 3 min—allowing debris to move to the apex of the ear canal. Then patient was moved quickly from the seated position, holding patient’s head in place, until patient was lying on the side of the unaffected ear with patient’s nose pointed to the ground. Patient remains in this position for 3 min allowing the debris to move toward the exit of the ear canal. Then patient was moved slowly back to the seated position. The debris should fall into the utricle of the canal, where it will no longer cause vertigo sensations [13, 17, 19].
Brandt–Daroff exercise were performed using standard method, in which the patient is in the sitting position on examination table, the patient moves into the lying position on the affected side on the shoulder, with the head angled upward with about 45°. The patient stays in this for 30 s and then goes back to the sitting position, looks forward, and remains in this position for 30 s as well. The patient repeats the same procedure for the other side, too. The patient performs this maneuver 5–10 times, thrice a day [14].
Patients who refuse to give written consent and patients did not come for follow-up were excluded from study. Patients who were on medication were excluded from study and no medication was prescribed to the patients during this study. Dix–Hallpike was administered immediately after maneuvers, if nystagmus persisted maneuver was repeated till the nystagmus disappeared or intensity was decreased, maximum thrice maneuver was repeated and results were documented. After 7 days again VAP scale was administered and results were documented. For Brandt–Daroff group exercise was given for 7 days and Dix–Hallpike was administered after 7 days of exercise. VAP scale was administered after 15 days of exercise. Results were tabulated and Statistical analysis was done using SPSS.
Results
Descriptive Statistics
All patients gave written consent. 17 patients excluded from study as they did not come for follow up. Total 90 cases included in the present study comprised 31 (35%) male and 59 (65%) female patients. The age of the patients ranged from 31 to 70 years, with the mean age being 49.96 ± 13.96 years and maximum number of patients being in the age group of 41 to 50 years. 57(63.33%) patients had Right PSCBPPV and 33(36.66%) patients had Left PSCBPPV.
VAP Scale Scores Pre and Post Treatment
VAP scores pre and post-treatment were compared using paired t test for Epley, Semont maneuver and Brandt–Daroff Exercise. VAP mean score pre and post Epley were 2.32 with SD 0.17 and 0.64 with SD 0.61 respectively. Paired t-test shows highly significant difference between VAP scores pre and post Epley maneuver with P value 0.0002 (Table 1).
Table 1.
Mean VAP scores, SD, and P value within 3 groups
| Group | Mean VAP score | SD | P value paired t test | Results |
|---|---|---|---|---|
| Epely pre-treatment | 2.32 | 0.17 | 0.0002 | Highly significant |
| Epely post-treatment | 0.64 | 0.61 | ||
| Semont pre-treatment | 2.42 | 0.20 | 0.00054 | Highly significant |
| Semont post-treatment | 0.992 | 0.83 | ||
| Brandt–Daroff pre-treatment | 2.27 | 0.17 | 0.0026 | Significant |
| Brandt–Daroff post-treatment | 1.41 | 0.88 |
VAP mean score pre and post Semont were 2.42 with SD 0.20 and 0.99 with SD 0.83 respectively. Paired t-test shows highly significant difference between VAP scores pre and post Semont maneuver with P value 0.0005 (Table 1).
VAP mean score pre and post Brandt–Daroff were 2.27 with SD 0.17 and 1.41 with SD 0.88 respectively. Paired t-test shows significant difference between VAP scores pre and post Brandt–Daroff with P value 0.0002 (Table 1).
Comparison of Improvement on VAP Results Between 3 Groups
Improvement was calculated by subtracting post-treatment VAP score from pre-treatment VAP scores in all 3 groups i.e. Epley, Semont, and Brandt–Daroff group. Improvement was compared between groups with one way ANOVA, statistically significant difference was found between 3 groups (Table 2).
Table 2.
Mean improvement of VAP scores and P value between 3 groups
| Group | Mean improvement of VAP scores | Pvalue one-way ANOVA |
|---|---|---|
| Epley | 1.68 | 0.000597 |
| Semont | 1.43 | |
| Brandt–Daroff | 0.86 |
Dix–Hallpike Results
Dix–Hallpike was administered pre and post Epley, Semont maneuvers, and Brandt–Daroff Exercise. All patients had counter clockwise up beating trosional nystagmus before treatment. No nystagmus after treatment on Dix–Hallpike test recorded as improvement. 27 out of 30 (90%) patients improved with Epley maneuver, 22 out of 30 (73.33%) patients improved with Semont maneuver, and 15 out of 30 (50%) patients improved with Brandt–Daroff Exercise (Fig. 1).
Fig. 1.
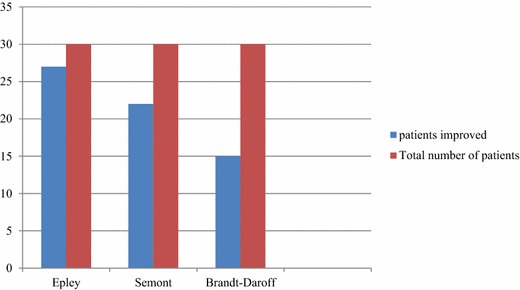
Dix–Hallpike results pre and post maneuvers
Discussion
BPPV generally observed in older age group individuals, however it may be observed in early age with head trauma. Present study observed that mean age of patients with PSCBPPV was 50 years which is in correlation with previous studies [11, 15]. In present study gender distribution revealed that females were 65% however previous studies showed that female is to male ratio is higher which is 75–85% [15, 20].
A significant difference was found between pre and post-treatment mean VAP scores in Epley, Semont maneuvers, and Brandt–Daroff Exercise group. This reveals that all 3 methods had positive effect on quality of life in patients with Posterior Canal BPPV. To find which method is better, improvement in VAP scores were compared and significant difference was found among 3 groups. Maximum improvement mean score was observed in Epely group than Semont and least improvement mean score was observed in Brandt–Daroff group. This finding was consistent with the study done by others assessing quality of life using other scales [15, 20]. There are no studies in best knowledge of authors done until now using VAP scale.
Use of the VAP scale in the study sample revealed that dizziness negatively affected the QoL of patients in all dimensions of daily life. VAP includes domains like attention, daily routine, psychological demands, travelling, job, recreation, and socialization. The functional aspects investigate the effect of dizziness on specific eye, head and body movements, focusing in the subject’s ability to carry out professional, household, social and leisure activities, and his or her independence in performing specific tasks such as walking independently and walking across the house in the dark. The emotional scores of the VAP scale investigate the possibility of dizziness having worsened the QoL of patients and giving rise to frustration, fear of leaving the house unaccompanied, fear of staying alone at home, concerns with the self-image, concentration disorders, feelings of incapacity, changes in family and social relationships, and depression. VAP evaluates participation and limitation of individuals with dizziness in daily activities more extensively than the earlier scale since it is based on ICF model [5].
Nystagmus is induced with Dix–Hallpike test [18]. The nystagmus has a 1–5 s latency time in cases of canalolithiasis, and between 10 and 20 s, in cases of cupulolithiasis [2]. There is discrepancy in treatment method of cupulolithiasis that use of mechanical vibration along with repositioning is more effective than only repositioning. However in present study mechanical vibration was not used and results were comparable with previous studies and findings are consistent with other studies [4, 10, 12]. Dix–Hallpike is gold standard test for diagnosis and to evaluate efficacy of treatment in BPPV. After treatment if no nystagmus is observed, it suggests that dislodged otconia are repositioned in utricle. Results of Dix–Hallpike indicate physiological improvement in patients, and it was observed that 90% patients improved with Epley maneuver, 73.33% patients improved with Semont maneuver, and 50% patients improved with Brandt–Daroff exercises. This finding was consistent with the study done by others [7, 8, 13, 14, 16, 17, 19].
Conclusion
Results of VAP score and Dix–Hallpike correlated with each other. According to results of both tests it was observed that Epley maneuver has produced maximum improvement than Semont maneuver and least improvement was produced by Brandt–Daroff Exercises. It suggests that improvement at physiological level and improvement in all dimensions of quality of life are directly proportional.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Alghwiri AA, Whitney SL, Baker CE, Sparto PJ, Marchetti GF, Rogers JC, et al. The development and validation of the Vestibular Activities and Participation measure. Arch Phys Med Rehabil. 2012;93:1822–1831. doi: 10.1016/j.apmr.2012.03.017. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Otolaryngology—Head and Neck Surgery (2000) Clinical indicators: canalith repositioning. American Academy of Otolaryngology—Head and Neck Surgery, Alexandria. Accessed 23 Nov 2005
- 3.Brandt T, Daroff RB. Physical therapy for benign paroxysmal positional vertigo. Arch Otolaryngol. 1980;106:484–485. doi: 10.1001/archotol.1980.00790320036009. [DOI] [PubMed] [Google Scholar]
- 4.Brandt T, Steddin S. Current view of the mechanism of benign paroxysmal positioning vertigo: cupulolithiasis or canalolithiasis? J Vestib Res Equilib Orientat. 1993;3(4):373–382. [PubMed] [Google Scholar]
- 5.Cohen HS, Kimball KT. Effectiveness of treatments for benign paroxysmal positional vertigo of the posterior canal. Otol Neurotol. 2005;26:1034–1040. doi: 10.1097/01.mao.0000185044.31276.59. [DOI] [PubMed] [Google Scholar]
- 6.Dix R, Hallpike CS. The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Ann Otol Rhinol Laryngol. 1952;6:987–1016. doi: 10.1177/000348945206100403. [DOI] [PubMed] [Google Scholar]
- 7.Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992;107(3):399404. doi: 10.1177/019459989210700310. [DOI] [PubMed] [Google Scholar]
- 8.Gans RE, Harrington-Gans PA. Treatment efficacy of benign paroxysmal positional vertigo (BVVP) with canalith repositioning maneuver and Semont liberatory maneuver in 376 patients. Semin Hear. 2002;23(2):129–142. doi: 10.1055/s-2002-33002. [DOI] [Google Scholar]
- 9.Magliulo G, Bertin S, Ruggieri M, Gagliardi M. Benign paroxysmal positional vertigo and post-treatment quality of life. Eur Arch Otorhinolaryngol. 2005;262:627–630. doi: 10.1007/s00405-004-0784-2. [DOI] [PubMed] [Google Scholar]
- 10.Parnes L, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV) CMAJ. 2003;169(7):681–693. [PMC free article] [PubMed] [Google Scholar]
- 11.Pereira AB, Santos JN, Volpe FM. Effect of Epley’s maneuver on the quality of life of paroxismal positional benign vertigo patients. Braz J Otorhinolaryngol (Impr) 2010;76(6):704–708. doi: 10.1590/S1808-86942010000600006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ruckenstein MJ, Shepard NT. The canalith repositioning procedure with and without mastoid oscillation for the treatment of benign paroxysmal positional vertigo. ORL. 2007;69(5):295. doi: 10.1159/000105265. [DOI] [PubMed] [Google Scholar]
- 13.Ruckenstein MJ, Shepard NT. The canalith repositioning procedure with and without mastoid oscillation for the treatment of benign paroxysmal positional vertigo. ORL J Otorhinolaryngol Relat Spec. 2007;69(5):295–298. doi: 10.1159/000105265. [DOI] [PubMed] [Google Scholar]
- 14.Salvinelli F, Casale M, Trivelli M, D’Ascanioo L, Firrisi L, Lamanna F, et al. Benign paroxysmal positional vertigo: a comparative prospective study on the efficacy of Semonts maneuver and no treatment strategy. Clin Ter. 2003;11:154–157. [PubMed] [Google Scholar]
- 15.Sargent EW, Bankaitis AE, Hollenbeak CS, Currens JW. Mastoid oscillation in canalith repositioning for paroxysmal positional vertigo. Otol Neurotol. 2001;22:205–209. doi: 10.1097/00129492-200103000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Semont A, Freyss G, Vitte E. Curing the BPPV with a liberatory manoeuvre. Adv Otorhinolaryngol. 1988;42:290–293. doi: 10.1159/000416126. [DOI] [PubMed] [Google Scholar]
- 17.Soto Varela A, et al. Benign paroxysmal vertigo: a comparative prospective study of the efficacy of Brandt and Daroff exercises, Semont and Epley manoeuvre. Rev Laryngol Otol Rhinol. 2001;122:179–183. [PubMed] [Google Scholar]
- 18.Soto-Varela A, Santos-Perez S, Rossi-Izquierdo M, Sanchez-Sellero I. Are the three canals equally susceptible to benign paroxysmal positional vertigo? Audiol Neuro-Otol. 2013;18(5):327–334. doi: 10.1159/000354649. [DOI] [PubMed] [Google Scholar]
- 19.Von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007;78:710–715. doi: 10.1136/jnnp.2006.100420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization . International classification of functioning, disability and health. Geneva: World Health Organization; 2001. [Google Scholar]


