Abstract
To demonstrate the affection of skull base by mucormycosis in an immunocompetent individual. Mucormycosis is an opportunistic infection principally seen in immunocompromised individuals, but recently being increasingly recognized in otherwise healthy individuals. Skull base involvement secondary to otogenic nidus, mimicking otitis media was rarely reported. A 34 year-old male, an otherwise healthy patient presented with facial nerve palsy followed by trismus, neck swelling and neck stiffness. Radical mastoidectomy with tympanoplasty and Facial nerve decompression along with Endoscopic guided debridement of sinuses and pterygopalatine fossa followed by medical treatment for 14 weeks. Facial nerve functioning, dry ear canal and relief from other symptoms. Surgical debridement and post op Anti fungal treatment improved the facial nerve function to House brackmann grade-II and also provided relief from trismus and stiffness and improved the overall general condition of the patient. Mucor is a saprophytic organism, which can cause extensive progression, regardless of the immune status. To the best of our knowledge, this is one of the very few rare cases that have been reported in the context of skull base mucormycosis in immunocompetent individuals. Surgical debridement followed by anti fungal therapy continues to remain the mainstay of treatment.
Keywords: Mucormycosis, Immunocompetent, Otitis media, Pterygopalatine fossa
Introduction
Mucormycosis refers to a group of disorders caused by fungi belonging to the order Mucorales. Paultauf first described it in 1885. It causes five major forms of infection: Rhinoorbitocerebral, pulmonary, disseminated, cutaneous and gastrointestinal. Apart from these, there are some minor forms including temporal bone and skull base involvement. Mucormycosis involving the skull base is a rare presentation, especially in an immunocompetent patient, with only few cases being reported. Our case is unique in its presentation of an immunocompetent patient, with extensive involvement of middle ear and mastoid, later progressively invading the skull base and prevertebral region. It illustrates a clinical picture mimicking otitis media, and thus creating a diagnostic as well as a therapeutic dilemma.
Case Vignette
A 34 year-old male patient presented to the out patient department with complaints of left ear discharge, facial nerve palsy, hearing loss, trismus, neck swelling and stiffness. The patient reported that he underwent canal wall down mastoidectomy a month before in another hospital, after which he developed trismus, neck swelling and stiffness along with persistent ear discharge, which was sent for culture sensitivity. Ultrasound guided aspiration of neck swelling was done and the collection was also sent for culture and sensitivity test. Routine investigations like blood glucose and tests for viral markers were performed which ruled out immunocompromised state. The CT scans of Temporal bones and paranasal sinuses showed sphenoid sinusitis extending to pterygopalatine fossa (Fig. 1) and soft tissue opacity in left middle ear and mastoid (Fig. 2). Contrast enhanced CT neck (Fig. 3) revealed multiple intra and inter muscular abscesses in the extensor muscles of the neck along with lytic lesions in the occipital bone and atlas with an associated soft tissue component along the base of the skull and prevertebral region at C1 vertebra. Further to these, the culture and sensitivity test revealed the presence of zygomycetes species. Considering the above results, the patient was planned for Left Radical mastoidectomy, Facial nerve decompression and endoscopic guided debridement of the bilateral ethmoid, sphenoid sinuses, and pterygopalatine fossa. During the surgery, necrotic debris was surgically debrided in the involved sinuses, pterygopalatine fossa, temporal bone and around the facial nerve in mastoid surgery. Postoperatively, the patient was given Injection Amphotericin B 250 mg iv for 6 weeks followed by Posaconazole syrup 10 mL bd for 2 months.
Fig. 1.
CT paranasal sinuses showing opacity involving sphenoid sinuses
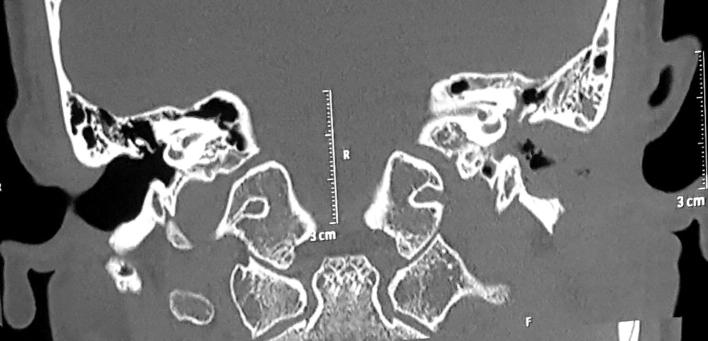
Fig. 2.
CT temporal bones showing soft tissue density noted filling the middle ear cavity and mastoid air cells
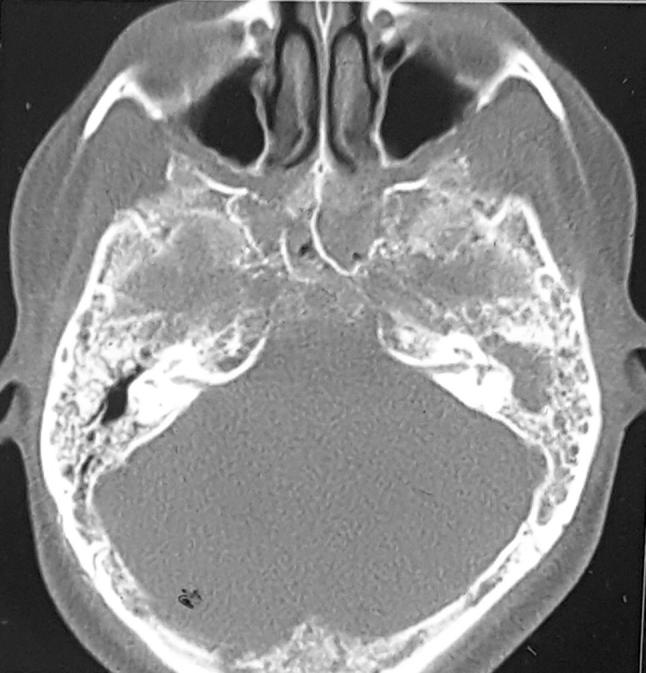
Fig. 3.

CT neck showing diffuse cellulitis involving left parapharyngeal space, left carotid space and submandibular space
Two months post the surgery; a nasal swab was obtained from the patient. Though Zygomycetes species was not detected, the tests were positive for MRSA. For treating this condition, Linezolid was prescribed to the patient at a dose of 600 mg twice daily for 2 months. After 6 months, the patient was asymptomatic and facial nerve function improved to house Brackmann grade-II.
Discussion
Mucormycosis encompasses a group of disorders caused by the genera in the order Mucorales with Rhizopus being the most common causative organism followed by Mucor and Absidia. These organisms are ubiquitous in nature and release a large number of spores, thus inhalation is the mode of spread. Mucormycosis is angio-invasive and causes infarction and necrosis of the host tissues. It is characterized by extension of infection through perivascular channels causing vasculitis, thrombosis, and infarcts, which precede bony destruction. The histopathological analysis shows fibro-collagenous tissue with granulomas, necrotic foci with aseptate irregular fungal hyphae with right angle branching. The necrotic bone demonstrates necrotic osseous trabeculae mixed with osteoclast cells. Imaging studies denote hyper dense material in the affected region. MRI, more specifically T1 is sensitive to minor pathologic abnormalities in the skull base, showing the high signal intensity of skull base marrow fat [1].
Mucormycosis can affect any organ in the body, devitalizing the tissues and results in widespread dissemination. Rhino-orbito-cerebral mucormycosis is the most common form and extensive forms predominantly occur in the immunocompromised individuals. Mucormycosis affecting cranial bones is rare, mainly seen in skull base [2] and considered following the failure of antibacterial therapy. On our review of the literature, we have noticed that these cases have been reported in a very few numbers in the immunocompetent individuals. In 1995, Fortum et al. described an unusual case of bilateral rhino orbital mucormycosis of posttraumatic origin in a previously healthy man [3]. Later, Buhl MR et al. reported extensive zygomycosis in a 38-year-old pregnant woman which involved temporal bones. There was no evidence of any other underlying immune deficiency except that of pregnancy [4]. A more widespread involvement of cavernous sinus, temporal fossa, and petrous bone with Internal carotid artery pseudoaneurysm was reported by Alvernia et al. in a 38-year-old man presented with a history of a headache, diplopia, and Trigeminal (V) nerve involvement [5]. In all these cases, initial symptoms are of rhinological and cerebral in origin with a paucity of otological features and no evidence of facial nerve involvement, whereas, our patient presented with features mimicking chronic otitis media with facial nerve palsy, which was highly misleading. Later, histopathological examination revealed aseptate hyphae, which helped us in arriving at a diagnosis.
Treatment of mucormycosis is multimodal and involves a combination of surgical debridement, antifungal therapy, and elimination of predisposing factors. Surgical debridement is required prior to medical therapy as blood vessel thrombosis and tissue necrosis results in poor penetration of antifungal agents to the site of infection. Antifungal therapy in the form of liposomal Amphotericin-B 10–15 mg/kg/day is the most effective treatment with improved survival rate. Posaconazole is reserved as salvage therapy for patient refractory to treatment [6]. Other adjunctive treatments include deferasirox, colistin [7], hyperbaric oxygen therapy and pro-inflammatory cytokines such as Interferon-gamma and Granulocyte-macrophage colony stimulating factor which enhance the ability of granulocytes [8]. In addition to the standard treatment above, our patient required facial nerve decompression along its tympanic and mastoid segments in view of facial nerve palsy. Further to this, prolonged therapy was required because of the involvement of skull base. Additionally, a regular follow up at 2 and 6-months interval showed a remarkable improvement in the symptomatology and the general condition of the patient.
Conclusion
Owing to high morbidity and mortality of mucormycosis, a comprehensive and efficient multidisciplinary approach must be executed. Early diagnosis by means of histopathological examination along with a high-index of suspicion plays a crucial role in avoiding delay of treatment. Surgical debridement followed by antifungals like amphotericin B continues to remain the mainstay of treatment, regardless of the immune status. The characteristics and outcome of these patients are better than those occurring in patients with the immune-compromised conditions. Whenever the clinical features and histopathology are suggestive of mucormycosis, the absence of predisposing factors should not be used to exclude this dreadful disease.
Compliance with Ethical Standards
Conflict of interest
There are no commercial of financial conflicts of interest. There are no funding sources for the underlying scientific work.
Contributor Information
N. Vishnu Swaroop Reddy, Email: vishnureddyn@hotmail.com
Raja Sekharam Natti, Email: drnrsekharam@gmail.com.
T. Radha, Email: radhatirumala97@gmail.com
Manoj Sharma, Email: dr.sharmamanoj@yahoo.com.
Murali Chintham, Email: drmuralikondaiah91@gmail.com.
References
- 1.Chan LL, Singh S, Jones D, Diaz EM, Jr, Ginsberg LE. Imaging of mucormycosis skull base osteomyelitis. AJNR Am J Neuroradiol. 2000;21(5):828–831. [PMC free article] [PubMed] [Google Scholar]
- 2.Devireddy SK, Kumar RVK, Gali R, Kanubaddy SR, Dasari MR, Akheel M. Mucormycotic skull base osteomyelitis: a case report. J Oral Maxillofac Surg Med Pathol. 2014;26(3):336–339. doi: 10.1016/j.ajoms.2013.01.006. [DOI] [Google Scholar]
- 3.Forton J, Cobo J, Caiqal J Post-traumatic cranial mucormycosis in an immunocompetent patient. J Oral Maxillofac Surg 53:1099–1102. t9952 [DOI] [PubMed]
- 4.Buhl MR, Joseph TP, Snelling BE, Buhl L. Temporofacial zygomycosis in a pregnant woman. Infection. 1992;20(4):230–232. doi: 10.1007/BF02033066. [DOI] [PubMed] [Google Scholar]
- 5.Alvernia JE, Patel RN, Cai DZ, Dang N, Anderson DW, Melgar M. A successful combined endovascular and surgical treatment of a cranial base mucormycosis with an associated internal carotid artery pseudoaneurysm. Neurosurgery. 2009;65(4):733–740. doi: 10.1227/01.NEU.0000351773.74034.5E. [DOI] [PubMed] [Google Scholar]
- 6.Greenberg RN, Mullane K, van Burik JA, et al. Posaconazole as salvage therapy for zygomycosis. Antimicrob Agents Chemother. 2006;50:126–133. doi: 10.1128/AAC.50.1.126-133.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ben-Ami R, Lewis RE, Tarrand J, et al. Antifungal activity of colistin against Mucorales species in vitro and in a murine model of Rhizopus oryzae pulmonary infection. Antimicrob Agents Chemother. 2010;54:484–490. doi: 10.1128/AAC.00956-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gil-Lamaignere C, Simitsopoulou M, Roilides E, et al. Interferon-gamma and granulocyte-macrophage-colony-stimulating factor augment the activity of polymorphonuclear leukocytes against medically important Zygomycetes. J Infect Dis. 2005;191:1180–1187. doi: 10.1086/428503. [DOI] [PubMed] [Google Scholar]