Abstract
Despite hundreds of structural MRI studies documenting smaller brain volumes on average in schizophrenia compared to controls, little attention has been paid to group differences in the variability of brain volumes. Examination of variability may help interpret mean group differences in brain volumes and aid in better understanding the heterogeneity of schizophrenia. Variability in 246 MRI studies was meta-analyzed for 13 structures that have shown medium to large mean effect sizes (Cohen’s d≥0.4): intracranial volume, total brain volume, lateral ventricles, third ventricle, total gray matter, frontal gray matter, prefrontal gray matter, temporal gray matter, superior temporal gyrus gray matter, planum temporale, hippocampus, fusiform gyrus, insula; and a control structure, caudate nucleus. No significant differences in variability in cortical/subcortical volumes were detected in schizophrenia relative to controls. In contrast, increased variability was found in schizophrenia compared to controls for intracranial and especially lateral and third ventricle volumes. These findings highlight the need for more attention to ventricles and detailed analyses of brain volume distributions to better elucidate the pathophysiology of schizophrenia.
Keywords: schizophrenia, psychosis, heterogeneity, variability, distribution, brain volume, MRI, neuroimaging, meta-analysis, quantitative review, pathophysiology, clinical neuroscience, cortical volume, subcortical volume, intracranial volume, ventricles
1. Introduction
The title of Eugen Bleuler’s classic text, Dementia Praecox or the Group of Schizophrenias (Bleuler, 1950), highlights the frequent observation that individuals diagnosed with schizophrenia show a large range of behavioral variation. This has led to numerous attempts to define subtypes that may better reflect heterogeneity in the etiology and pathology of schizophrenia. Across behavioral measures that can be assessed in schizophrenia and controls, individuals with schizophrenia often show greater variation than controls, suggesting wider dispersion of important phenotypes in schizophrenia (Tandon, Nasrallah, & Keshavan, 2009), including cognitive functioning, symptoms and illness course (Carpenter, Heinrichs, & Wagman, 1988; Fenton, McGlashan, Victor, & Blyler, 1997; Mahurin, Velligan, & Miller, 1998). Despite repeated observations of increased behavioral variation and numerous investigations linking brain and behavior in schizophrenia, scant attention has been paid to the variation in brain measures within schizophrenia. The study of brain structure arose within the first few decades of conceptualizing schizophrenia as a disorder but only recently have tools become available to examine adequately the volumes of specific brain structures.
Interest in brain structure volume in schizophrenia gained momentum when computed tomography (CT) was first applied to schizophrenia (Johnstone, Crow, Frith, Husband, & Kreel, 1976), generating a considerable literature on primarily the mean but also to a certain extent the variation of overall brain and ventricular volume in schizophrenia. The poor spatial resolution of CT limited observations to gross brain or ventricular volume rather than specific brain structures and measurements of ventricle/brain ratios (VBR) were introduced in attempt to weigh the volume of ventricles against the total brain size. Of the many CT studies reporting increased mean VBR in schizophrenia, only four to our knowledge examined the distribution of VBRs in schizophrenia (Daniel, Goldberg, Gibbons, & Weinberger, 1991; Harvey et al., 1990; Torrey, Bowler, Taylor, & Gottesman, 1994; Vita et al., 2000), although these yielded few clues regarding the distribution of specific brain structure volumes independent of ventricular volumes in schizophrenia. Overall, these studies suggested that ventricle volumes follow a unimodal distribution with somewhat increased variability in schizophrenia compared to controls (Daniel et al., 1991; Harvey et al., 1990; Torrey et al., 1994; Vita et al., 2000).
More recently, starting in the late 1980’s, magnetic resonance imaging (MRI) has been used to study schizophrenia. Despite its capacity to measure brain structure volume more precisely than ever before, examining variation in brain structure volume has been lacking in comparison to the main thrust of examining mean differences. To illustrate, although over 30 meta-analyses conducted on reports of mean volumetric differences between schizophrenia and controls demonstrated reduced mean volume for many brain structures in schizophrenia (Shepherd, Laurens, Matheson, Carr, & Green, 2012), to our knowledge, only one quite recent selective review (Brugger & Howes, 2017), restricted to ten bilateral brain structures and only early course patient studies, has compared variation in brain structure volume between schizophrenia and controls. That review concluded that there was evidence of increased variation in schizophrenia for volumes of the temporal cortex, thalamus, putamen, and third ventricle among first-episode patients. Given that increased duration of illness has been associated with increased reductions in total and prefrontal grey matter (Haijma et al., 2013), variability group differences in brain structure volumes may show different patterns across illness course.
Comparing brain structure volume variation between groups is important because it may help explain the meaning of average group differences in brain structure volume. Observation of greater volumetric variation in brain structure of individuals with schizophrenia compared to controls could suggest heterogeneity in pathological processes that differentially impact brain structure volume across individuals. In contrast, reduced average volumes but equivalence in variability of brain structure volumes between schizophrenia and controls could suggest some process that has a more homogeneous effect across schizophrenia patients, although other alternatives explanations are possible such as increased skewness due to heterogeneous effects that do not increase variability.
Therefore, the aim of this comprehensive quantitative review was to examine the variation of brain structure volume that accompanies the mean decreases in brain structure volume between schizophrenia and controls including both early and later stage patients. To aid in interpreting mean differences, we focused on brain structures that have shown medium to large mean differences in volume in the most comprehensive recent meta-analysis of MRI studies (Haijma et al., 2013). Given the etiological heterogeneity implied by polygenic models and findings (Gottesman & Shields, 1972; Schizophrenia Working Group of the Psychiatric Genomics Consortium, 2014), we hypothesized that mean volume differences observed in schizophrenia would be accompanied by increased variability compared to controls, due to a possible excess of small volumes in schizophrenia arising from heterogeneous causes. We tested this hypothesis in a meta-analysis of 246 studies of thirteen brain structures showing mean volume differences in schizophrenia and a control brain structure showing no mean volume differences in schizophrenia.
2. Method
2.1. Selection of Brain Structures
Of the two most common methods of analyzing structural volume, volumetric analysis and voxel-based morphometry, studies of the former were selected because it provides an index of brain structure volume variation. Here, we focused on 13 structures showing medium or large mean difference between schizophrenia and control groups (Cohen’s d effect size≥0.4) from the latest meta-analysis (Haijma et al., 2013) because these structures may be most likely to show variation differences if there are any to be detected: Intracranial volume, total brain volume, lateral ventricles, third ventricle, total gray matter, frontal lobe gray matter, prefrontal lobe gray matter, temporal lobe gray matter, hippocampus, planum temporale, superior temporal gyrus gray matter, fusiform gyrus, and insula. In addition, given that we did not examine all possible brain structures, we selected one control structure showing no significant mean schizophrenia/control difference in the latest meta-analysis (Haijma et al., 2013) as a comparison: the caudate nucleus. The caudate nucleus was chosen as it was the structure with the closest mean effect size to zero (d= − 0.03) of all the structures reported in this meta-analysis (Haijma et al., 2013). A total of 246 articles were included in this meta-analysis after full-text read (see Figure 1 for flowchart).
Figure 1.
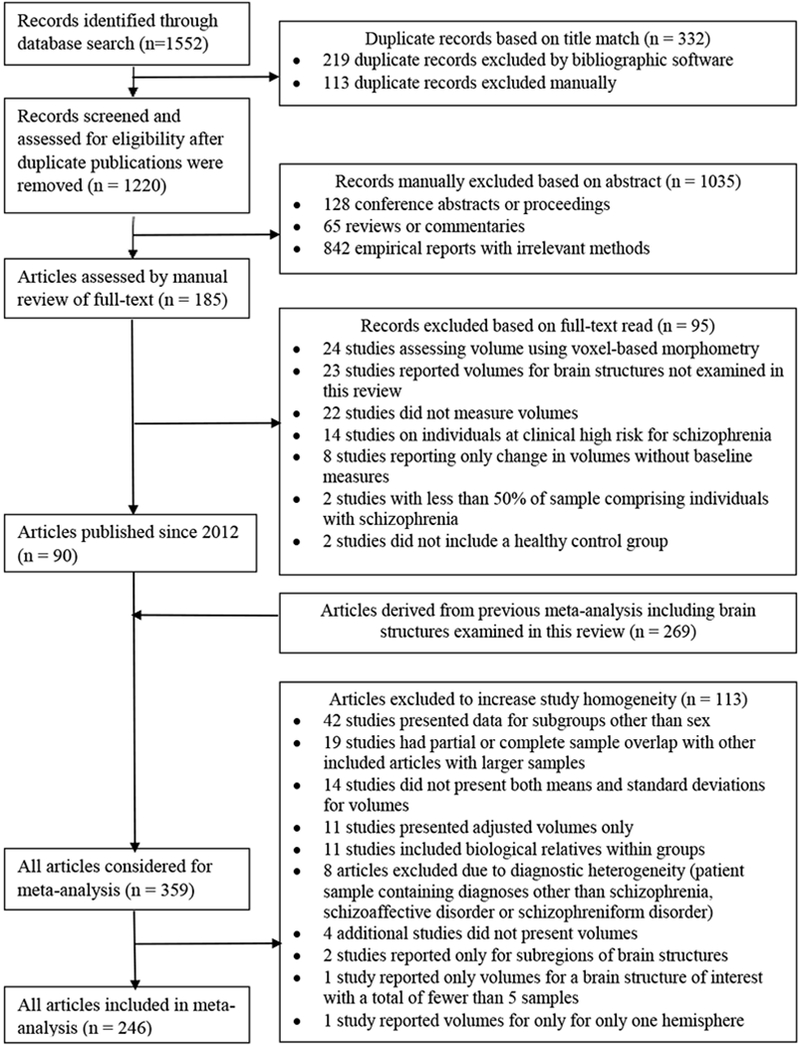
Flowchart depicting systematic review process.
2.2. Inclusion and Exclusion Criteria
Journal articles were screened to meet all the following inclusion criteria:
The full-text article was published in English.
The group sizes for all studies, including all participants in subgroups, comprised at least 10 individuals (a few studies included samples grouped by sex, which reduced the number of individuals in a subgroup to fewer than 10).
The patient sample included only individuals with a primary diagnosis of schizophrenia, schizophreniform disorder, or schizoaffective disorder, based on criteria listed in the Diagnostic and Statistical Manual of Mental Disorders (version III-R or IV) (American Psychiatric Association, 1980, 2000) or International Classification of Diseases (version 9 or 10) (World Health Organization, 1978, 1992).
The comparison group was composed of non-psychotic controls. Some studies screened the control group for all psychiatric diagnoses, whereas many studies did not specify criteria aside from an absence of psychotic diagnoses.
Participants in either group were not related to one another.
Data for structural volumes were presented for the total samples or separately by sex (when data for a structural volume were presented for both the total samples and separately by sex, only effect sizes grouped by sex were included).
Data were reported for the selected brain structures for the overall bilateral structure and/or by hemisphere, without any further subdivision (both bilateral and hemispheric data were included if presented).
Raw volumes (rather than area or thickness) were reported separately for each group for at least one brain structure.
The variance, standard deviation or standard error was reported for each group.
2.3. Search Strategies
A total of 269 articles published between August 1998 and January 2012 were extracted from the bibliography of the latest meta-analysis of mean volume differences between schizophrenia and control groups (Haijma et al., 2013). Following the methods of this meta-analysis of mean group differences (Haijma et al., 2013), the present review included articles published after the last general meta-analysis of brain structure volumes in schizophrenia, which included articles up until 1998 (Wright et al., 2000). In addition, based on their literature search strategy (Haijma et al., 2013), 1552 peer-reviewed journal articles published from January 2012 to September 2015 were also electronically identified using a conjunction of the three free-text search terms, “schizophrenia”, “brain”, “ and “magnetic resonance imaging” or “MRI” in three comprehensive medical journal databases (MEDLINE, PubMed, and EMBASE) and eight leading journal databases that were most relevant to the study topics (American Journal of Psychiatry, JAMA Psychiatry (formerly known as Archives of General Psychiatry prior to July 2012), Biological Psychiatry, NeuroImage, Psychiatry Research, Schizophrenia Bulletin and Schizophrenia Research). When applicable, medical subject heading (MeSH) terms were also included in the search. Duplicate publications were removed using EndNote X7 bibliographic software yielding 1220 articles. A total of 246 articles were included in this meta-analysis after full-text read.
The vast majority of included articles reported cross-sectional structural MRI studies conducted on convenience samples of medicated schizophrenia patients and healthy controls. Brain regions were extracted using automatic segmentation for overall brain structures (intracranial volume and total brain volume) and either semi-automatic or manual segmentation on raw images for specific brain structures. For studies of antipsychotic-naïve patients, articles published before September 1998 that were previously selected for review in the latest meta-analysis of mean differences (Haijma et al., 2013) and met our inclusion criteria were included in addition to studies published after September 1998. Only baseline data from longitudinal studies were included in this review. Furthermore, only hemispheric volumes for the following structures were included as fewer than five samples presenting bilateral volumes met inclusion criteria: superior temporal gyrus gray matter, planum temporale, fusiform gyrus, and insula. All other structures had both bilateral and hemispheric data. Medication dosages were converted to chlorpromazine dose equivalents (Gardner, Murphy, O’Donnell, Centorrino, & Baldessarini, 2010). Because the PANSS total score was the symptom rating with the most observations, it was used as the measure of current symptom severity.
2.4. Data Extraction
The effect sizes extracted from the included articles were entered on two occasions by the first author. Absolute volumes were converted to mm3. When samples were partially overlapping for a structure, only the largest sample for the structure was included. When only standard errors (SE) were provided, standard deviations (s) were calculated for each group using the formula: s = SE × √N, where N represents the number of participants in the group.
2.5. Computation of Effect Sizes
2.5.1. Variability ratio.
To compare the variability of brain structure volumes in schizophrenia and controls, the ratio of schizophrenia and control variability (variability ratio, VR) was calculated for each study. Drawing upon recent work proposing the ratio of standard deviations as an unbiased estimate of group differences in the population variability and its sampling variance, the natural logarithm (ln) of the variability ratio and its sampling variance were calculated according to the following formulas (Nakagawa et al., 2015), where SZ denotes the schizophrenia group, HC the control group, s the standard deviation, and n the sample size:
The variability ratio was derived from an unbiased variability effect size for a single sample, the natural logarithm of the standard deviation and its sampling variance (Nakagawa et al., 2015):
To statistically evaluate the differences in structural volume variability between schizophrenia and controls, meta-analyses were performed of the null hypothesis that the natural log of the variability ratio equals 0 (i.e., the variability ratio is 1).
The ratio of coefficients of variation was also proposed in the same report as an alternative estimate of population variability (Nakagawa et al., 2015). However, the variability ratio was chosen here instead of the ratio of coefficients of variation (group standard deviation divided by group mean) for several reasons. The coefficient of variation divides the variability by the mean in an attempt to adjust for a tendency for means and variability to be positively correlated (i.e., lower means paired with lower variability) perhaps due to floor effects that might reduce variation for groups with lower means because of a truncation of low values. In the current situation, the control group, being the norm, presumably should not have floor effects as studies suggest that brain structure volumes are normally distributed in the general population (Leonard et al., 2008). Thus, for structures for which schizophrenia has reduced means (e.g., most specific brain structures), floor effects if present might reduce their variability compared to controls. However, it is hypothesized that schizophrenia will show increased variability, not decreased and thus any floor effects will not contribute to spurious positive results. In contrast, for structures for which schizophrenia has increased means (e.g., ventricles) floor effects should not reduce or affect their variability. Thus, given reduced means for brain structures, the ratio of coefficients of variation may be inappropriately liberal compared to the variability ratio, whereas given increased means in schizophrenia for ventricles, the ratio of coefficients of variation may be inappropriately conservative. Therefore, the variability ratio was utilized here as it is a more direct, unadjusted measure that is not potentially inappropriately influenced by differences in group means, which are likely present in this situation.
2.5.2. Mean effect size.
To compare mean structural volumes in schizophrenia and controls, the effect size and variability for Glass’ delta (M. L. Smith & Glass, 1977) were computed using the following formulas, where N denotes the number of samples:
Standardizing the mean difference to the control group standard deviation avoids problems in interpreting differences in mean structural volumes when using pooled standard deviations in the context of group differences in variation, as hypothesized in this study. To statistically evaluate the mean differences in structural volumes between schizophrenia and controls, meta-analyses were performed of the null hypothesis that the delta-value equals 0.
2.6. Meta-analyses
Meta-analyses were conducted using STATA (version 14) with a random effects model (a standard and conservative approach), weighting the studies by their inverse variability, and calculating the Dersimonian-Laird effect size. The “metan” and “admetan” subroutines were used to conduct the meta-analysis for each structure and to create graphical depictions of the effect sizes respectively. In addition, the “metanbias” sub-routine was used to examine the possibility of bias, and “metareg” was used to conduct meta-regressions. Although overly conservative given the intercorrelations among brain structures’ volumes, the Bonferroni-adjusted threshold for multiple comparisons was 0.05/31 = 0.0016, based on the number of non-control regions examined.
2.7. Heterogeneity
Given the wide range of recruitment strategies and methods for scanning and defining brain structures, considerable heterogeneity across studies should be expected. To quantify this, we computed two metrics for each meta-analysis: Cochran’s Q (Cochran, 1954) and I2 (Higgins’ Thompson, Deeks, & Altman, 2003). Although no MRI studies to our knowledge have been published that a priori sought to examine if schizophrenia had increased brain volume variability (thus minimizing any potential publication bias), we assessed potential publication bias attributable to small studies with Egger’s regression test (ERT) (Egger, Davey Smith, Schneider, & Minder, 1997), which investigates correlations between effect sizes and sample sizes. A significant ERT may indicate that a result is based upon a biased selection of small studies, although differences in the protocols or populations of smaller studies could also result in larger effect sizes.
2.8. Hemispheric Effects
Hemisphere effects were examined using two methods. First, meta-analyses were conducted for variability ratios of brain structure volumes separately by hemisphere. Secondly, in the absence of appropriate meta-analytic techniques for examining differences between correlated ratios of standard deviations, we also compared left-hemisphere and right-hemisphere variability ratios using one-sample t-tests of the null hypothesis that their difference equaled 0. Specifically, the exponentiated variability ratio for the right hemisphere volume was subtracted from the exponentiated variability ratio for the left hemisphere volume for each sample and a one-sample t-test evaluated whether these hemispheric differences in variability ratios across samples differed significantly from zero. For the hemispheric differences in mean group differences for a structure, a similar strategy was employed in which Glass’ delta for the right hemisphere volume was subtracted from Glass’ delta for the left hemisphere volume for each sample. This one-sample t-test compared whether the hemispheric differences in Glass’ delta across samples differed significantly from zero. Although these one-sample t-tests appropriately account for the pairing of hemispheric volumes within studies, they do not utilize meta-analytic methods and thus do not account for the weighting of the studies nor the increased precision from pooling multiple studies.
2.9. Meta-Regressions
Restricted maximum likelihood (REML) weighted random-effects meta-regressions were performed to examine whether variation in the following demographic characteristics predicted variability group differences in bilateral brain structure volume across studies (given at least five samples):
Ratios of group proportions for sex, handedness and ethnicity.
Ratios of group standard deviations for age, years of education, parental socioeconomic status measured on the Hollingshead Index, intelligence quotient (IQ), height, intracranial volume, and total brain volume.
Standard deviations in the schizophrenia group for clinical variables: age at illness onset, illness duration, antipsychotic medication dosage (in antipsychotic-exposed samples only), and current symptom severity.
In addition, REML weighted random-effects meta-regressions were also performed to examine whether sample means of the following characteristics predicted variability group differences in bilateral brain structure volume across studies (given at least five samples):
Sample mean (averaging the percentages or means of both groups) for: sex, handedness, ethnicity, age, years of education, parental socioeconomic status measured on the Hollingshead Index, IQ, height, intracranial volume, and total brain volume.
Difference in group means for relevant structure volume.
Means in the schizophrenia group for clinical variables: age at illness onset, illness duration, antipsychotic medication dosage (in antipsychotic-exposed samples only), and current symptom severity.
Antipsychotic exposure: 100% antipsychotic-naïve samples vs others
Current substance abuse: explicit exclusion for current substance abuse vs others
Sample recruitment: first admission samples vs others
Scanning parameters: magnetic field strength and slice thickness. There was insufficient variation in slice gap width across studies to conduct meta-regression analyses.
3. Results
3.1. Sample Characteristics
Across all samples, the schizophrenia and control groups included on average 35 participants each. Characteristics of samples included in bilateral structure analyses are shown in Table 1a and samples included in hemispheric analyses are shown in Table 1b. The average group was two-thirds male participants, mostly of European ancestry, and approximately 30 years old. Scanning parameters for the average sample included 1.5T scanners (~80% 1.5T, ~15% 3.0 T), slice thickness approximating 1.6mm, and little to no slice gap (mean width<0.1 mm).
Table 1a.
Characteristics of Samples Included in Bilateral Structure Analyses
| Schizophrenia |
Controls |
|||||
|---|---|---|---|---|---|---|
| Characteristic | N | Mean Across Samples | SD Across Samples | N | Mean Across Samples | SD Across Samples |
| Group Size | 219 | 34.94 | 27.23 | 219 | 36.68 | 31.60 |
| Age | 204 (201) |
30.74 (7.20) |
8.27 (2.97) |
204 (201) |
30.39 (7.15) |
8.53 (3.28) |
| Sex | 216 | 66.74 | 28.60 | 216 | 64.17 | 28.96 |
| Handedness | 138 | 92.76 | 9.42 | 137 | 94.35 | 7.55 |
| Ethnicity | 32 | 70.94 | 26.07 | 32 | 76.03 | 21.84 |
| Education | 90 (89) |
12.42 (2.48) |
1.72 (0.84) |
90 (89) |
14.01 (2.50) |
1.90 (1.12) |
| Socioeconomic Status | 48 (48) |
2.88 (1.02) |
0.57 (0.39) |
47 (47) |
2.62 (0.92) |
0.60 (0.31) |
| Intelligence Quotient | 45 (44) |
97.61 (13.68) |
9.45 (3.51) |
45 (44) |
109.79 (11.70) |
7.34 (2.84) |
| Height | 37 (37) |
170.11 (8.11) |
6.82 (2.16) |
37 (37) |
171.59 (7.69) |
7.09 (2.20) |
| Scanning Parameters | ||||||
| Magnetic Field Strength | ||||||
| 0.5 T | 1 | 0.5% | ||||
| 1.0 T | 5 | 2.3% | ||||
| 1.5 T | 180 | 82.2% | ||||
| 2.0 T | 1 | 0.5% | ||||
| 3.0 T | 20 | 9.1% | ||||
| Slice Thickness | 181 | 1.59 | 0.83 | |||
| Slice Gap Width | 124 | 0.07 | 0.35 | |||
| Intrarater Reliability | 71 | 0.91 | 0.08 | |||
| Interrater Reliability | 31 | 0.92 | 0.07 | |||
| Clinical Characteristics | ||||||
| First-Episode (%) | 63 | 94.53 | 18.10 | |||
| Chronic (%) | 27 | 97.91 | 10.88 | |||
| Inpatient (%) | 10 | 71.94 | 32.77 | |||
| Outpatient (%) | 14 | 78.97 | 33.52 | |||
| Medicated (%) | 82 | 90.66 | 24.16 | |||
| Antipsychotic Dosage | 68 (66) |
468.17 (344.97) |
220.16 (174.51) |
|||
| Illness Onset | 94 (94) |
22.64 (5.47) |
3.79 (1.70) |
|||
| Illness Duration | 131 (129) |
9.65 (6.10) |
7.11 (3.56) |
|||
| Symptom Severity | 51 (51) |
71.52 (16.53) |
15.02 (5.25) |
|||
Note. Group proportions or means within samples are shown with standard deviations enclosed in parentheses where appropriate. N (number of samples reporting a given characteristic), sex (proportion male), handedness (proportion right-handed), ethnicity (proportion European ancestry), education (years of formal education), height (centimeters), socioeconomic status (parental socioeconomic status rated on the Hollingshead Index), antipsychotic dosage (daily dosage in chlorpromazine equivalents only for antipsychotic exposed samples), illness onset (age at schizophrenia onset), symptom severity (Positive and Negative Symptom Scale overall score).
Table 1b.
Characteristics of Samples Included in Hemispheric Structure Analyses
| Schizophrenia |
Controls |
|||||
|---|---|---|---|---|---|---|
| Characteristic | N | Mean Across Samples | SD Across Samples | N | Mean Across Samples | SD Across Samples |
| Group Size | 136 | 32.81 | 29.41 | 136 | 34.88 | 35.50 |
| Age | 123 (121) |
30.90 (7.13) |
8.57 (3.14) |
123 (121) |
30.76 (7.14) |
8.66 (3.32) |
| Sex | 136 | 64.94 | 32.95 | 136 | 62.86 | 32.88 |
| Handedness | 88 | 92.73 | 10.09 | 88 | 93.48 | 9.23 |
| Ethnicity | 18 | 61.55 | 22.02 | 18 | 70.72 | 18.02 |
| Education | 54 (54) |
12.41 (2.53) |
2.01 (1.00) |
54 (54) |
14.13 (2.54) |
2.14 (1.16) |
| Socioeconomic Status | 31 (30) |
2.91 (1.07) |
0.59 (0.44) |
31 (30) |
2.60 (0.93) |
0.65 (0.31) |
| Intelligence Quotient | 21 (21) |
94.14 (13.62) |
9.14 (4.44) |
21 (21) |
107.81 (11.78) |
6.62 (3.20) |
| Height | 28 (28) |
169.19 (8.07) |
6.72 (2.46) |
28 (28) |
169.84 (7.66) |
6.64 (2.73) |
| Scanning Parameters | ||||||
| Magnetic Field Strength | ||||||
| 0.5 T | 1 | 0.7% | ||||
| 1.0 T | 5 | 3.7% | ||||
| 1.5 T | 108 | 79.4% | ||||
| 3.0 T | 15 | 11.0% | ||||
| Slice Thickness | 105 | 1.69 | 1.00 | |||
| Slice Gap Width | 78 | 0.07 | 0.34 | |||
| Intrarater Reliability | 68 | 0.90 | 0.08 | |||
| Interrater Reliability | 36 | 0.93 | 0.04 | |||
| Clinical Characteristics | ||||||
| First-Episode (%) | 36 | 95.85 | 15.30 | |||
| Chronic (%) | 11 | 94.24 | 19.10 | |||
| Inpatient (%) | 10 | 75.93 | 36.40 | |||
| Outpatient (%) | 13 | 80.04 | 35.71 | |||
| Medicated (%) | 46 | 93.04 | 16.41 | |||
| Antipsychotic Dosage | 48 (46) |
536.81 (437.69) |
206.44 (199.18) |
|||
| Illness Onset | 57 (57) |
22.65 (5.33) |
3.27 (1.95) |
|||
| Illness Duration | 83 (81) |
9.41 (5.87) |
7.84 (3.86) |
|||
| Symptom Severity | 21 (21) |
74.09 (16.62) |
11.98 (5.96) |
|||
Note. Group proportions or means within samples are shown with standard deviations enclosed in parentheses where appropriate. N (number of samples reporting a given characteristic), sex (proportion male), handedness (proportion right-handed), ethnicity (proportion European ancestry), education (years of formal education), height (centimeters), socioeconomic status (parental socioeconomic status rated on the Hollingshead Index), antipsychotic dosage (daily dosage in chlorpromazine equivalents only for antipsychotic exposed samples), illness onset (age at schizophrenia onset), symptom severity (Positive and Negative Symptom Scale overall score).
3.2. Mean Group Differences in Brain Structure Volumes
Ventricle volumes showed the largest mean effect sizes of all examined structures (Supplemental Table 1): individuals with schizophrenia showed enlargement of the lateral ventricles (d=0.443, p<.001) and third ventricle (d=0.518, p<.001). As also expected, individuals with schizophrenia showed as well smaller average global structural volumes than controls: intracranial volume (d=−0.121, p<.001), total brain volume (d=−0.246, p<.001), and gray matter volume (d=−0.377, p<.001). Similarly, individuals with schizophrenia showed smaller average gray matter volumes than controls for the frontal lobe (d=−0.313, p=.003), prefrontal lobe (d=−0.400, p<.001), temporal lobe (d=−1.093, p=.029), and superior temporal gyrus (left hemisphere d=−0.572 and right hemisphere d=−0.903, ps<.001). Average hippocampal volume was also smaller in schizophrenia compared to controls (d=−0.492, p=<0.001), as were fusiform gyrus (left hemisphere d=−0.600 and right hemisphere d=−0.449, ps<.005), planum temporale (left hemisphere d=−0.775 and right hemisphere d=−0.349, ps<.043), and left insula (d=−0.459, p=.045); right insula volume was non-significantly smaller in schizophrenia. As expected, the control region, the caudate nucleus, on average did not differ significantly between schizophrenia and controls (d=−0.182, p=.107). Mean effect sizes for brain structures appeared similar between right and left hemispheres (Supplemental Table 1) and no significant differences were found between hemispheres in mean group volume differences (Supplemental Table 2).
3.3. Variability Group Differences in Brain Structure Volumes
Overall variability group differences in brain structure volumes are summarized in Table 2 (variability ratios for each individual sample are presented for bilateral, left, and right hemisphere structures in Supplemental Tables 3a, 3b, and 3c). Variability group differences in brain structure volumes were greatest for the ventricles: compared to controls, individuals with schizophrenia showed 8.7% greater variability in lateral ventricle volumes (VR=1.087, p=.002) and 14.1% greater variability in third ventricle volumes (VR=1.141, p<.001). Variability group differences for lateral ventricle volumes also did not differ significantly between hemispheres (see Table 3), and effect sizes for hemispheric lateral ventricle volumes were even somewhat larger than those found for bilateral ventricle volumes (left hemisphere VR=1.128 and right hemisphere VR=1.141, ps<.010). Significant variability group differences were also found for intracranial volume, which was 2.8% more variable in schizophrenia than controls (VR=1.028, p=.002). Using a perhaps overly conservative (given intercorrelations among brain structure volumes) Bonferroni adjustment for multiple testing (alpha=0.0016), the only significant finding was increased variability in third ventricle volume in schizophrenia compared to healthy controls. Forestplots for variability group differences in intracranial and ventricle volumes are presented in Supplemental Figures 1–4.
Table 2.
Summary of Meta-Analyses Comparing Variability of Brain Structure Volumes in Schizophrenia and Controls
| Number of Samples (Studies) | Combined Sample Size |
Variability Ratio |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Brain Structure | Hemisphere | Patients | Controls | Effect Size | Effect Size 95% CI | Effect Size p-value | Cochran’s Q (p-value) | I2 | ERT (p-value) | |
| Intracranial Volume | 125 (111) |
4515 | 4752 | 1.028 | (1.010/1.046) | 0.002 | 2094.17 (<0.001) |
94.1 | 0.843 (0.128) |
|
| Total Brain Volume | Bilateral | 85 (76) |
2830 | 3046 | 1.002 | (0.968/1.037) | 0.909 | 3212.57 (<0.001) |
97.4 | 0.740 (0.517) |
| Left | 11 (8) |
280 | 249 | 1.009 | (0.915/1.112) | 0.863 | 142.94 (<0.001) |
93.0 | −1.344 (0.602) |
|
| Right | 11 (8) |
280 | 249 | 1.030 | (0.955/1.110) | 0.449 | 83.63 (<0.001) |
88.0 | −1.748 (0.367) |
|
| Total Gray Matter Volume | Bilateral | 69 (63) |
2617 | 2737 | 1.024 | (0.993/1.055) | 0.128 | 2001.74 (<0.001) |
96.6 | −1.771 (0.110) |
| Left | 5 (4) |
238 | 236 | 1.045 | (0.967/1.129) | 0.271 | 65.36 (<0.001) |
93.9 | −0.943 (0.872) |
|
| Right | 5 (4) |
238 | 236 | 1.038 | (0.968/1.113) | 0.290 | 52.46 (<0.001) |
92.4 | 0.063 (0.990) |
|
| Lateral Ventricle | Bilateral | 14 (13) |
695 | 681 | 1.087 | (1.030/1.146) | 0.002 | 373.97 (<0.001) |
96.5 | −3.164 (0.143) |
| Left | 20 (16) |
839 | 852 | 1.128 | (1.043/1.219) | 0.003 | 1186.50 (<0.001) |
98.4 | −1.005 (0.720) |
|
| Right | 20 (16) |
839 | 852 | 1.141 | (1.032/1.261) | 0.010 | 1982.10 (<0.001) |
99.0 | 1.502 (0.678) |
|
| Third Ventricle | 17 (16) |
760 | 710 | 1.141 | (1.092/1.193) | <0.001 | 295.67 (<0.001) |
94.6 | 1.734 (0.259) |
|
| GM Frontal Lobe | Bilateral | 6 (5) |
206 | 259 | 1.056 | (0.969/1.151) | 0.212 | 77.42 (<0.001) |
93.5 | −3.794 (0.369) |
| Left | 8 (5) |
199 | 253 | 1.112 | (0.996/1.242) | 0.059 | 110.68 (<0.001) |
93.7 | −4.055 (0.407) |
|
| Right | 8 (5) |
199 | 253 | 1.146 | (0.987/1.331) | 0.074 | 207.76 (<0.001) |
96.6 | −3.416 (0.617) |
|
| GM Prefrontal Lobe | Bilateral | 7 (6) |
319 | 308 | 1.037 | (0.982/1.095) | 0.193 | 34.94 (<0.001) |
82.8 | 0.755 (0.580) |
| Left | 7 (7) |
182 | 192 | 1.079 | (0.954/1.220) | 0.224 | 100.96 (<0.001) |
94.1 | −1.739 (0.657) |
|
| Right | 7 (7) |
182 | 192 | 0.913 | (0.803/1.037) | 0.161 | 109.01 (<0.001) |
94.5 | −7.427* (0.016) |
|
| GM Temporal Lobe | Bilateral | 7 (6) |
206 | 253 | 0.944 | (0.805/1.107) | 0.476 | 267.25 (<0.001) |
97.8 | 8.876 (0.217) |
| Left | 9 (7) |
234 | 269 | 1.030 | (0.914/1.160) | 0.631 | 164.07 (<0.001) |
95.1 | −0.733 (0.896) |
|
| Right | 9 (7) |
234 | 269 | 1.034 | (0.944/1.132) | 0.473 | 94.27 (<0.001) |
91.5 | 0.877 (0.837) |
|
| GM Superior Temporal Gyrus | Left | 9 (8) |
330 | 386 | 0.946 | (0.876/1.022) | 0.162 | 165.38 (<0.001) |
95.2 | 0,455 (0.886) |
| Right | 9 (8) |
330 | 386 | 1.013 | (0.925/1.111) | 0.774 | 233.51 (<0.001) |
96.6 | −0.085 (0.982) |
|
| Hippocampus | Bilateral | 10 (10) |
416 | 459 | 1.012 | (0.976/1.049) | 0.527 | 44.71 (<0.001) |
79.9 | 0.191 (0.865) |
| Left | 66 (57) |
2345 | 2558 | 1.001 | (0.976/1.027) | 0.928 | 1204.03 (<0.001) |
94.6 | 0.141 (0.850) |
|
| Right | 66 (57) |
2345 | 2558 | 1.021 | (0.988/1.054) | 0.216 | 2080.11 (<0.001) |
96.9 | 0.906 (0.353) |
|
| Fusiform Gyrus | Left | 5 (4) |
193 | 191 | 0.949 | (0.827/1.088) | 0.450 | 80.16 (<0.001) |
95.0 | −2.157 (0.567) |
| Right | 5 (4) |
193 | 191 | 0.954 | (0.886/1.027) | 0.214 | 22.26 (<0.001) |
82.0 | −1.826 (0.329) |
|
| Planum Temporale | Left | 13 (13) |
415 | 379 | 0.969 | (0.904/1.038) | 0.372 | 169.61 (<0.001) |
92.9 | 2.199 (0.329) |
| Right | 13 (13) |
415 | 379 | 0.948 | (0.895/1.004) | 0.067 | 112.30 (<0.001) |
89.3 | 2.047 (0.261) |
|
| Insula | Left | 5 (4) |
111 | 101 | 0.928 | (0.838/1.028) | 0.152 | 21.23 (<0.001) |
81.2 | −2.562 (0.585) |
| Right | 5 (4) |
111 | 101 | 1.003 | (0.887/1.133) | 0.963 | 30.55 (<0.001) |
86.9 | 8.233* (0.044) |
|
| Caudate Nucleus | Bilateral | 10 (9) |
323 | 404 | 1.035 | (0.905/1.184) | 0.613 | 546.57 (<0.001) |
98.4 | −4.366 (0.521) |
| Left | 22 (20) |
825 | 891 | 0.928 | (0.838/1.028) | 0.152 | 21.23 (<0.001) |
81.2 | −0.325 (0.793) |
|
| Right | 22 (20) |
825 | 891 | 1.026 | (0.995/1.058) | 0.104 | 166.60 (<0.001) |
87.4 | 1.065 (0.243) |
|
Note. CI: confidence interval; ERT: Egger’s Regression Test statistic. Variability ratios were natural log transformed for meta-analysis and are shown here exponentiated for ease of interpretation.
Table 3.
Summary of T-Tests Comparing Group Differences in Variability for Brain Structure Volume by Hemisphere
| Laterality in Brain Structure | Number of Samples | Difference | t | p-value |
|---|---|---|---|---|
| Total Brain Volume | 11 | −0.012 | −0.120 | 0.907 |
| Total Gray Matter Volume | 5 | 0.006 | 0.105 | 0.921 |
| Lateral Ventricles | 20 | −0.034 | −0.463 | 0.649 |
| Gray Matter Frontal Lobe | 8 | −0.052 | −0.498 | 0.634 |
| Gray Matter Prefrontal Lobe | 7 | 0.177 | 1.547 | 0.173 |
| Gray Matter Temporal Lobe | 9 | −0.020 | −0.199 | 0.847 |
| Gray Matter Superior Temporal Gyrus | 9 | −0.067 | −1.533 | 0.164 |
| Hippocampus | 66 | −0.030 | −1.089 | 0.280 |
| Fusiform Gyrus | 5 | 0.004 | 0.088 | 0.934 |
| Planum Temporale | 13 | 0.025 | 0.480 | 0.640 |
| Insula | 5 | −0.092 | −0.981 | 0.382 |
| Caudate Nucleus | 22 | −0.003 | −0.187 | 0.853 |
Note. One-sample t-test conducted on difference in exponentiated ratios of group standard deviations between left hemisphere and right hemisphere. Positive values indicate that left hemisphere volume shows larger group difference in variation than right hemisphere volume.
In contrast, variability in global brain tissue structures was not significantly different in schizophrenia and controls, as suggested by the small, non-significant effect sizes for total brain volume (VR=1.002, p=.909) and total gray matter volume (VR=1.024, p=.128). Similarly, gray matter volumes of the frontal lobe, prefrontal lobe, temporal lobe and superior temporal gyrus and volumes of the hippocampus, fusiform gyrus, planum temporale, insula and the control caudate region did not differ significantly in variability between schizophrenia than controls. Variability group differences did not differ significantly by hemisphere for any of these brain structure volumes (see Table 3).
3.4. Heterogeneity
Cochran’s Q tests suggested significant heterogeneity in variability group differences across all brain structures examined (see Table 2). The proportion of heterogeneity in variability group differences across studies that was not attributable to chance, as indicated by the I2 statistic, approximated 79 to 99% across all studies. Addressing the potential effects of publication bias, the results of Egger’s regression tests indicated that small sample sizes were unlikely to contribute to larger variability group differences for any brain structure except for gray matter volume of the right prefrontal lobe and right insula volume.
3.5. Meta-Regressions
Given that variability group differences appeared uniform across hemispheres based on the results of separate meta-analyses by hemisphere and the nonsignificant one-sample t-tests of hemispheric differences across all brain structure volumes, heterogeneity was investigated in variability group differences of bilateral structures.
Results of meta-regressions first examined whether sample differences in variation in demographic, scanning and clinical characteristics accounted for some of the heterogeneity across samples in variability group differences for bilateral brain structure volumes (see Supplemental Table 4a-j). Focusing on those structures that had group differences in variability, increased variability group difference for intracranial volume was significantly predicted by greater variation in schizophrenia symptom severity and greater group difference in variability in lateral ventricle volume was predicted by deceased right handedness in patients vs controls; otherwise, variability group differences in intracranial volume and ventricle volumes were not significantly predicted by variation in sample characteristics. Meta-regressions also examined if average sample demographic, scanning and clinical characteristics accounted for some of the heterogeneity across samples in variability group differences for bilateral brain structure volumes (see Supplemental Table 5a-j). Increased variability group difference in intracranial volume was predicted by increased mean antipsychotic dosage in antipsychotic-exposed schizophrenia samples and by non-first episode status. Increased lateral ventricle group differences in variability was significantly predicted by antipsychotic exposure; otherwise, intracranial volume and ventricle volumes were not significantly predicted by mean sample characteristics. Meta-regressions were also conducted examining the relationship between mean group difference and variability ratio (see Supplemental Table 5a-j). These analyses indicated that mean group differences were positively correlated with variability ratios for volumes of the lateral ventricles and third ventricle.
Similar meta-regression results for brain structures that did not show significant overall group differences in variation in schizophrenia compared to controls are presented in Supplemental Tables 4a-j, 5a-j.
Overall, these analyses found few sample characteristics that predicted variability group differences in brain structure volumes and given the number of meta-regressions and often small number of studies, those few significant results should be interpreted with caution.
4. Discussion
Using stringent, conservative study selection and data aggregation criteria, we comprehensively review the magnitude of variation in brain structure volumes in schizophrenia, including early and late stages, measured using MRI from 246 studies across 14 brain structures. Overall, our results highlight increased variation in intracranial (+2.8%), and lateral (+8.7%) and third (+14.1%) ventricles in schizophrenia compared to healthy controls. In contrast, volumes of 11 other brain structures did not differ significantly in variability between schizophrenia and controls (Table 2). Using a conservative Bonferroni adjustment for multiple corrections (alpha=0.0016), the increased variability in third ventricle volume in schizophrenia compared to healthy controls remained significant. These results were consistent across hemispheres and all (except as expected the control structure) showed the mean reduction in brain volume expected based on prior meta-analyses (Haijma et al., 2013). Results from a recent smaller meta-analysis restricted to first-episode patients (Brugger & Howes, 2017) generally fit with these observations, also finding significantly increased variability in schizophrenia for lateral and third ventricles and non-significant differences for frontal lobe gray matter, hippocampus, and caudate nucleus based on variability ratios, although analyses of coefficients of variation produced some different results. In contrast, that review reported significantly increased variability for total temporal lobe volume whereas we did not for our measure of temporal lobe gray matter volume (p=.476), perhaps due to duration of illness effects or differences between gray and white matter. We cannot compare results for other structures as that review did not examine intracranial volume, total brain volume, total gray matter volume, prefrontal gray matter, superior temporal gyrus gray matter, fusiform gyrus, planum temporale, insula, or any hemispheric structures. In addition, the current review did not include the amygdala, anterior cingulate cortex, putamen, or thalamus because they had not shown robust mean volume decreases (Cohen’s d effect size>0.4) in the most recent meta-analysis of mean volume differences in schizophrenia (Haijma et al., 2013). Beyond including patients from early and later stages of illness, which over doubled the number of studies included here, the current review also employed more conservative methods, using only data from unadjusted raw volumes without combining structural volumes across subregions, hemispheres, subgroups, or gray and white matter based on uncertain statistical assumptions.
The heterogeneity analyses suggest that, on the whole, the findings are not consistently explained by key demographic, scanning, and clinical characteristics. Possible exceptions include: Recruitment/episode analyses indicated increased variability differences for intracranial volume in non-first admission samples vs first admission samples; other findings concern antipsychotic medications, such that although antipsychotic exposed samples did not differ significantly from naive samples, among antipsychotic exposed patients, increased mean antipsychotic dosage was associated with increased variability group differences in intracranial volume. Antipsychotic exposed samples also showed greater group differences in variability for lateral ventricles compared to naive samples. Taken together, these results suggest that antipsychotic levels may somehow be associated with greater variability in intracranial and ventricle volume in schizophrenia, although given the small number of antipsychotic naïve studies and the large number of meta-regressions, such results need to be interpreted cautiously.
Interestingly, larger mean group differences were associated with larger variability group differences for lateral and third ventricle volumes (and also for gray matter volume of the temporal lobe), suggesting that increased mean shifts in the distribution were accompanied by greater variability in ventricle volumes.
How confident can we be in our findings based on methodological considerations? The significantly increased variability in schizophrenia for intracranial and lateral and third ventricle volumes is unlikely to be attributable to publication bias and they were also statistically well-powered (participant Ns=9267, 1376 and 1470, respectively). Likewise, group differences in variability or mean demographic, sampling or clinical characteristics did not appear to account clearly for these positive results. On the other hand, the non-significant findings for several of the other brain structures do not seem to be due to low power, as sample sizes for total brain, total gray matter, and bilateral hippocampal volumes were quite large (participant Ns 5876, 5354, and 4903, respectively), although sample sizes for other non-significant structures were smaller and ranged between approximately 450 to 750, with a low outlier of 212 (insula). Of the structures with non-significant results, the majority (72%, 21/29) had variability ratios of 1.0 (truncated to 1 decimal place) (indicating no difference), eight (28%) had variability ratios less than 1.0 (indicating decreased schizophrenia variation) and only 2 (7%) had variability ratios greater than 1.0, suggesting that in most cases, non-significant effect sizes were indeed small or non-existent. Interestingly, there were no significant findings of decreased variation in schizophrenia compared to controls. It is also possible that the non-significant results for brain structure volumes are due to being measured less reliably than intracranial and ventricular volumes. However, other large, presumably well-measured structures, such as total brain and total gray matter volumes, showed low non-significant variability ratios (1.002 and 1.024 respectively). Intracranial and ventricular volume may also have shown significantly increased variability because they represent the aggregated effects of many individual structures, each of which has only a small non-significant effect-size. Although plausible, again the non-significant results for total brain and total gray matter volumes suggest that this may not be the entire story.
First, how might the findings of no significant differences in variability between schizophrenia patients and controls arise for ten of the brain structures, especially given the reduced mean volumes of schizophrenia patients? Although it can be difficult to interpret null findings, the negative results for total brain and total gray matter volume and the other eight individual brain structures warrant attempts at explanation. Such a pattern of results (mean difference but no variability difference) is consistent with the simple situation in which every schizophrenia patient’s brain structure volume is reduced by a constant amount across patients, thus reducing the mean but not affecting the variability. While consistent with the observations, such a hypothesis seems very unlikely given what we know about the multifactorial polygenic nature of schizophrenia etiology, although iatrogenic effects (e.g., medication) might act in this fashion (Weinberger & Radulescu, 2016).
In contrast, many other scenarios predict some variability difference in schizophrenia. For example, variability may decline with reduced means due to floor effects, although it is possible that this effect was not statistically significant here because the reduction in mean volumes (mean effect size usually less than 0.5 control standard deviations) was too small to confront the lower biological bound for brain volumes. Likewise, beginning with a normal distribution in controls (Leonard et al., 2008) and increasing the frequency in schizophrenia of some brain volume reducing causes (e.g., schizophrenia genetic risk variants that pleiotropically also reduce brain volume) can also reduce both variability and mean while increasing positive skewness (i.e., a skew-normal distribution). In contrast, heterogeneity hypotheses in which schizophrenia brain volumes reflect a mixture of multiple distributions due to differing pathologies would usually predict increased variation compared to controls. Given such plausible hypotheses, the apparent absence of variability differences was unexpected. Analysis of individual participant data and the specifics of the distributions (e.g., shape, skewness, kurtosis, mixture) in both schizophrenia and control populations are needed to understand further these unexpected findings of apparently equivalent variability.
In contrast to these negative results for specific brain structures, robust findings of increased variability in schizophrenia were found for the “non-brain” structures of intracranial volume and especially for lateral and third ventricles. Although it was a relatively small effect (1.028) for intracranial volume, given the young age at which the cranium usually ceases development (Matsumae et al., 1996; Sgouros, Goldin, Hockley, Wake, & Natarajan, 1999), such results are consistent with the possibility that at least some schizophrenia causes have effects early in life. How should we interpret the significant findings of increased ventricular variability in schizophrenia, which were the largest observed here (variability ratios ranged from 1.087 to 1.141)? Reduced variability may be associated with reduced means in the presence of floor and the absence of ceiling effects. In this particular situation however, the control group, being the norm, presumably should not have floor effects as brain structure volumes are normally distributed in the general population (Leonard et al., 2008). Thus, for structures like the ventricles for which schizophrenia has increased means, floor effects should not reduce and certainly not increase their variability. Potential ceiling effects likewise might reduce variability in schizophrenia but not increase them. Furthermore, the mean effect size increases in ventricular volumes are approximately 0.5 control standard deviations, which are generally similar to the mean reductions in volume of many of the specific brain regions discussed above. If a 0.5 effect size reduction is hypothesized to be too small to affect the variability of the specific brain structures, it is not clear why a similar mean effect size increase would not have the same null effect for the ventricles. These points suggest that the increased variability in ventricles in schizophrenia is not spurious and instead that some other factors are operating with ventricles, with one possibility being that ventricle volumes reflect a mixture of distributions. Although often considered as only reflecting the lack of volume of other more specific brain structures, it may therefore be that ventricular volume also reflects other causes that are specific to ventricles alone and are not shared with effects on specific brain structures. Ventricular volume was by necessity the focus of considerable early research using CT scans but has received less attention (Elkis, Friedman, Wise, & Meltzer, 1995; Torrey et al., 1994; van Horn & McManus, 1992) with the advent of MRI’s ability to measure volumes more accurately. These results suggest renewed attention be paid to ventricular volume.
In contrast, variability group differences were non-significant for brain tissue structures. Of these non-significant results, the largest effect size trends may suggest potentially increased variability in schizophrenia for total frontal lobe gray matter volume in the hemispheric analyses (left variability ratio 1.112, p=.059 and right 1.146, p=.074). While tentative, these findings suggest that among specific brain structures, frontal gray matter volume may be the most likely to demonstrate increased variability in schizophrenia. Although tentative, such findings are particularly interesting in light of cognitive, neural and pathophysiological abnormalities associated with the prefrontal cortex in schizophrenia (Weinberger et al., 2001).
This study consolidates reports of MRI-measured variation in brain volumes in schizophrenia conducted over the past two decades and as a result large numbers of subjects contributed to the analysis of most brain structure volumes. Furthermore, a wide range of relevant demographic, clinical, and scanning variables were explored as possible contributors to the heterogeneity across studies. Still, the findings of this review should be interpreted in the light of some limitations. Following the methods of the most recent comprehensive meta-analysis of mean group differences (Haijma et al., 2013), this review only encompassed studies published since 1998. Our conclusions for certain brain structures are constrained by the small number and size of some samples included. We decided a priori to examine only the volumes of those brain structures showing at least a medium mean effect size; other brain structures may show different results. We also decided that one control region with a mean effect size of approximately zero was sufficient for interpretability, although we acknowledge the possibility that other similar structures may show other patterns of variability group differences. The large number of meta-regressions also increases the likelihood of inflated alpha error for these heterogeneity analyses. In addition, because this meta-analysis relied upon cross-sectional designs, we cannot provide any information concerning developmental aspects of brain volume variability.
As far as we are aware, this is the first meta-analysis of MRI studies of brain structure variation across all illness stages in schizophrenia and the most comprehensive. We analyzed data for 14 brain structures from 246 studies and found no significant differences in variability in cortical and subcortical brain structures volumes in schizophrenia relative to controls, consistent across a wide range of demographic, clinical and neuroimaging characteristics. In contrast, robust increased variability was found in schizophrenia compared to controls for intracranial and ventricular volumes.
Overall, these findings present a proof of concept for interrogating the meaning of mean group differences in biological features for schizophrenia and controls. Although this study does not completely resolve the meaning of mean group differences in structural brain volumes, raises important questions and suggests multiple directions for further research. Broadly, this study suggests that variability of brain structure volumes in schizophrenia merits further characterization. In particular, these findings highlight the need for more detailed analyses of MRI brain volume distributions based on raw data to determine their shape and mixture, with skew and kurtosis for distributions of brain volumes evaluated within and between groups. Furthermore, we recommend examining not only whether means of key demographic, scanning, and clinical variables may contribute to variability in brain structure volumes, but also whether group differences in the variability of these predictors may contribute to this variability. The heterogeneity in these findings further suggests the utility of examining distributional differences in brain structure volumes associated with antipsychotic medication dosage, to further inform the effects of medication on brain structure volumes in schizophrenia. Ultimately, resolving the shape of the underlying distribution and the fit of multiple distributions necessitates analyses conducted on individual-level data rather than group-level data. These results also recommend renewed attention to the etiology and development of brain ventricles in schizophrenia, and to examine whether these processes arise specifically in schizophrenia or are found in other psychiatric disorders.
Supplementary Material
Highlights.
Cortical and subcortical volumes are equally variable in schizophrenia and controls
Intracranial and ventricle volumes are more variable in schizophrenia than controls
Variance group differences consistent across demographic and clinical variables
Acknowledgements
This work was supported by the Doctoral Foreign Study Award from the Canadian Institutes of Health Research to SSK and the NIMH collaborative R01 grant [MH60722] to MPG. We thank Satish Iyengar, Ph.D., Aidan Wright, Ph.D., and Shaun Eack, Ph.D. for statistical consultation and discussion. Earlier versions were presented in October 2016 at the 30th annual meeting of the Society for Research in Psychopathology and in February 2017 at the International Imaging Genetics Conference.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
*References marked with an asterisk indicate studies included in the meta-analysis.
- Ahmed M, Cannon DM, Scanlon C, Holleran L, Schmidt H, McFarland J, … McDonald C (2015). Progressive Brain Atrophy and Cortical Thinning in Schizophrenia after Commencing Clozapine Treatment. Neuropsychopharmacology, 40(10), 2409–2417. doi: 10.1038/npp.2015.90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altshuler LL, Bartzokis G, Grieder T, Curran J, Jimenez T, Leight K, … Mintz J (2000). An MRI study of temporal lobe structures in men with bipolar disorder or schizophrenia. Biol Psychiatry, 48(2), 147–162. doi: 10.1016/s0006-3223(00)00836-2 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (1980). Diagnostic and statistical manual of mental disorders (DSM-III): American Psychiatric Publishing.
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders - text revision (DSM-IV-TR): American Psychiatric Publishing.
- Ananth H, Popescu I, Critchley HD, Good CD, Frackowiak RS, & Dolan RJ (2002). Cortical and subcortical gray matter abnormalities in schizophrenia determined through structural magnetic resonance imaging with optimized volumetric voxel-based morphometry. Am J Psychiatry, 159(9), 1497–1505. doi: 10.1176/appi.ajp.159.9.1497 [DOI] [PubMed] [Google Scholar]
- Anderson JE, Wible CG, McCarley RW, Jakab M, Kasai K, & Shenton ME (2002). An MRI study of temporal lobe abnormalities and negative symptoms in chronic schizophrenia. Schizophr Res, 58(2-3), 123–134. doi: 10.1016/s0920-9964(01)00372-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreone N, Tansella M, Cerini R, Rambaldelli G, Versace A, Marrella G, … Brambilla P (2007). Cerebral atrophy and white matter disruption in chronic schizophrenia. Eur Arch Psychiatry Clin Neurosci, 257(1), 3–11. doi: 10.1007/s00406-006-0675-1 [DOI] [PubMed] [Google Scholar]
- Baare WF, Hulshoff Pol HE, Hijman R, Mali WP, Viergever MA, & Kahn RS (1999). Volumetric analysis of frontal lobe regions in schizophrenia: relation to cognitive function and symptomatology. Biol Psychiatry, 45(12), 1597–1605. doi: 10.1016/s0006-3223(98)00266-2 [DOI] [PubMed] [Google Scholar]
- Bagary MS, Foong J, Maier M, duBoulay G, Barker GJ, Miller DH, & Ron MA (2002). A magnetization transfer analysis of the thalamus in schizophrenia. J Neuropsychiatry Clin Neurosci, 14(4), 443–448. doi: 10.1176/jnp.14.4.443 [DOI] [PubMed] [Google Scholar]
- Baiano M, Perlini C, Rambaldelli G, Cerini R, Dusi N, Bellani M, … Brambilla P (2008). Decreased entorhinal cortex volumes in schizophrenia. Schizophr Res, 102(1-3), 171–180. doi: 10.1016/j.schres.2007.11.035 [DOI] [PubMed] [Google Scholar]
- Balevich EC, Haznedar MM, Wang E, Newmark RE, Bloom R, Schneiderman JS, … Hazlett EA (2015). Corpus callosum size and diffusion tensor anisotropy in adolescents and adults with schizophrenia. Psychiatry Res, 231(3), 244–251. doi: 10.1016/j.pscychresns.2014.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballmaier M, Schlagenhauf F, Toga AW, Gallinat J, Koslowski M, Zoli M, … Heinz A (2008). Regional patterns and clinical correlates of basal ganglia morphology in non-medicated schizophrenia. Schizophr Res, 106(2-3), 140–147. doi: 10.1016/j.schres.2008.08.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballmaier M, Toga AW, Siddarth P, Blanton RE, Levitt JG, Lee M, & Caplan R (2004). Thought disorder and nucleus accumbens in childhood: a structural MRI study. Psychiatry Res, 130(1), 43–55. doi: 10.1016/j.pscychresns.2003.10.001 [DOI] [PubMed] [Google Scholar]
- Berge D, Carmona S, Rovira M, Bulbena A, Salgado P, & Vilarroya O (2011). Gray matter volume deficits and correlation with insight and negative symptoms in first-psychotic-episode subjects. Acta Psychiatr Scand, 123(6), 431–439. doi: 10.1111/j.1600-0447.2010.01635.x [DOI] [PubMed] [Google Scholar]
- Bleuler E (1950). Dementia praecox or the group of schizophrenias. [PubMed]
- Boonstra G, van Haren NE, Schnack HG, Cahn W, Burger H, Boersma M, … Kahn RS (2011). Brain volume changes after withdrawal of atypical antipsychotics in patients with first-episode schizophrenia. J Clin Psychopharmacol, 31(2), 146–153. doi: 10.1097/JCP.0b013e31820e3f58 [DOI] [PubMed] [Google Scholar]
- Boos HBM, Cahn W, van Haren NEM, Derks EM, Brouwer RM, Schnack HG, … Kahn RS (2012). Focal and global brain measurements in siblings of patients with schizophrenia. Schizophr Bull, 38(4), 814–825. doi: 10.1093/schbul/sbq147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bossu P, Piras F, Palladino I, Iorio M, Salani F, Ciaramella A, … Spalletta G (2015). Hippocampal volume and depressive symptoms are linked to serum IL-18 in schizophrenia. Neurol Neuroimmunol Neuroinflamm, 2(4), e111. doi: 10.1212/nxi.0000000000000111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bottmer C, Bachmann S, Pantel J, Essig M, Amann M, Schad LR, … Schroder J (2005). Reduced cerebellar volume and neurological soft signs in first-episode schizophrenia. Psychiatry Res, 140(3), 239–250. doi: 10.1016/j.pscychresns.2005.02.011 [DOI] [PubMed] [Google Scholar]
- Brown GG, Lee JS, Strigo IA, Caligiuri MP, Meloy MJ, & Lohr J (2011). Voxel-based morphometry of patients with schizophrenia or bipolar I disorder: A matched control study. Psychiatry Res, 194(2), 149–156. doi: 10.1016/j.pscychresns.2011.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brugger SP, & Howes OD (2017). Heterogeneity and homogeneity of regional brain structure in schizophrenia: a meta-analysis. JAMA Psychiatry, 74(11), 1104–1111. doi: 10.1001/jamapsychiatry.2017.2663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant NL, Buchanan RW, Vladar K, Breier A, & Rothman M (1999). Gender differences in temporal lobe structures of patients with schizophrenia: a volumetric MRI study. Am J Psychiatry, 156(4), 603–609. doi: 10.1176/ajp.156.4.603 [DOI] [PubMed] [Google Scholar]
- Cahn W, Hulshoff Pol HE, Bongers M, Schnack HG, Mandl RC, Van Haren NE, … Kahn RS (2002). Brain morphology in antipsychotic-naive schizophrenia: A study of multiple brain structures. Br J Psychiatry Suppl, 43(43), s66–72. doi: 10.1192/bjp.181.43.s66 [DOI] [PubMed] [Google Scholar]
- Cancel A, Comte M, Truillet R, Boukezzi S, Rousseau PF, Zendjidjian XY, … Fakra E (2015). Childhood neglect predicts disorganization in schizophrenia through grey matter decrease in dorsolateral prefrontal cortex. Acta Psychiatr Scand. doi: 10.1111/acps.12455 [DOI] [PubMed] [Google Scholar]
- Cannon TD, van Erp TGM, Huttunen M, Lönnqvist J, Salonen O, Valanne L, … Yan M (1998). Regional gray matter, white matter, and cerebrospinal fluid distributions in schizophrenic patients, their siblings, and controls. Arch Gen Psychiatry, 55(12), 1084. doi: 10.1001/archpsyc.55.12.1084 [DOI] [PubMed] [Google Scholar]
- Carpenter WT Jr., Heinrichs DW, & Wagman AM (1988). Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry, 145(5), 578–583. doi: 10.1176/ajp.145.5.578 [DOI] [PubMed] [Google Scholar]
- Chen Z, Deng W, Gong Q, Huang C, Jiang L, Li M, … Li T (2014). Extensive brain structural network abnormality in first-episode treatment-naive patients with schizophrenia: morphometrical and covariation study. Psychol Med, 44(12), 2489–2501. doi: 10.1017/s003329171300319x [DOI] [PubMed] [Google Scholar]
- Choi JS, Kang DH, Kim JJ, Ha TH, Roh KS, Youn T, & Kwon JS (2005). Decreased caudal anterior cingulate gyrus volume and positive symptoms in schizophrenia. Psychiatry Res, 139(3), 239–247. doi: 10.1016/j.pscychresns.2004.05.008 [DOI] [PubMed] [Google Scholar]
- Chua SE, Cheung C, Cheung V, Tsang JT, Chen EY, Wong JC, … McAlonan GM (2007). Cerebral grey, white matter and CSF in never-medicated, first-episode schizophrenia. Schizophr Res, 89(1-3), 12–21. doi: 10.1016/j.schres.2006.09.009 [DOI] [PubMed] [Google Scholar]
- Chua SE, Lam IWS, Tai KS, Cheung C, Tang WN, Chen EYH, … McKenna PJ (2003). Brain morphological abnormality in schizophrenia is independent of country of origin. Acta Psychiatr Scand, 108(4), 269–275. doi: 10.1034/j.1600-0447.2003.00134.x [DOI] [PubMed] [Google Scholar]
- Cochran WG (1954). The combination of estimates from different experiments. Biometrics, 10(1), 101. doi: 10.2307/3001666 [DOI] [Google Scholar]
- Collinson SL, Mackay CE, James AC, Quested DJ, Phillips T, Roberts N, & Crow TJ (2003). Brain volume, asymmetry and intellectual impairment in relation to sex in early-onset schizophrenia. Br J Psychiatry, 183(2), 114–120. doi: 10.1192/bjp.183.2.114 [DOI] [PubMed] [Google Scholar]
- Crespo-Facorro B, Kim J, Andreasen NC, O’Leary DS, & Magnotta V (2000). Regional frontal abnormalities in schizophrenia: a quantitative gray matter volume and cortical surface size study. Biol Psychiatry, 48(2), 110–119. doi: 10.1016/s0006-2332(00)00238-9 [DOI] [PubMed] [Google Scholar]
- Crespo-Facorro B, Kim JJ, Chemerinski E, Magnotta V, Andreasen NC, & Nopoulos P (2004). Morphometry of the superior temporal plane in schizophrenia: Relationship to clinical correlates. J Neuropsychiatry Clin Neurosci, 16(3), 284–294. doi: 10.1176/jnp.16.3.284 [DOI] [PubMed] [Google Scholar]
- Csernansky JG, Joshi S, Wang L, Haller JW, Gado M, Miller JP, … Miller MI (1998). Hippocampal morphometry in schizophrenia by high dimensional brain mapping. Proc Natl Acad Sci U S A, 95(19), 11406–11411. doi: 10.1073/pnas.95.19.11406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniel DG, Goldberg TE, Gibbons RD, & Weinberger DR (1991). Lack of a bimodal distribution of ventricular size in schizophrenia: A Gaussian mixture analysis of 1056 cases and controls. Biol Psychiatry, 30(9), 887–903. doi: 10.1016/0006-3223(91)90003-5 [DOI] [PubMed] [Google Scholar]
- Deicken R, Eliaz Y, Chosiad L, Feiwell R, & Rogers L (2002). Magnetic resonance imaging of the thalamus in male patients with schizophrenia. Schizophr Res, 55(2-3), 135–144. doi: 10.1016/s0920-9964(01)00330-9 [DOI] [PubMed] [Google Scholar]
- Deicken RF, Pegues M, & Amend D (1999). Reduced hippocampal N-acetylaspartate without volume loss in schizophrenia. Schizophr Res, 37(3), 217–223. doi: 10.1016/s0920-9964(98)00173-x [DOI] [PubMed] [Google Scholar]
- Deshmukh A, Rosenbloom MJ, De Rosa E, Sullivan EV, & Pfefferbaum A (2005). Regional striatal volume abnormalities in schizophrenia: effects of comorbidity for alcoholism, recency of alcoholic drinking, and antipsychotic medication type. Schizophr Res, 79(2-3), 189–200. doi: 10.1016/j.schres.2005.04.025 [DOI] [PubMed] [Google Scholar]
- Downhill JE, Buchsbaum MS, Hazlett EA, Barth S, Lees Roitman S, Nunn M, … Siever LJ (2001). Temporal lobe volume determined by magnetic resonance imaging in schizotypal personality disorder and schizophrenia. Schizophr Res, 48(2-3), 187–199. doi: 10.1016/s0920-9964(00)00131-6 [DOI] [PubMed] [Google Scholar]
- Duggal HS, Muddasani S, & Keshavan MS (2005). Insular volumes in first-episode schizophrenia: Gender effect. Schizophr Res, 73(1), 113–120. doi: 10.1016/j.schres.2004.08.027 [DOI] [PubMed] [Google Scholar]
- Ebdrup BH, Glenthoj B, Rasmussen H, Aggernaes B, Langkilde AR, Paulson OB, … Baare W (2010). Hippocampal and caudate volume reductions in antipsychotic-naive first-episode schizophrenia. J Psychiatry Neurosci, 35(2), 95–104. doi: 10.1503/jpn.090049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebner F, Tepest R, Dani I, Pfeiffer U, Schulze TG, Rietschel M, … Falkai P (2008). The hippocampus in families with schizophrenia in relation to obstetric complications. SchizophrRes, 104(1-3), 71–78. doi: 10.1016/j.schres.2008.06.007 [DOI] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. doi: 10.1136/bmj.316.7129.469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sayed M, Steen RG, Poe MD, Bethea TC, Gerig G, Lieberman J, & Sikich L (2010). Brain volumes in psychotic youth with schizophrenia and mood disorders. J Psychiatry Neurosci, 35(4), 229–236. doi: 10.1503/jpn.090051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkis H, Friedman L, Wise A, & Meltzer HY (1995). Meta-analyses of studies of ventricular enlargement and cortical sulcal prominence in mood disorders. Comparisons with controls or patients with schizophrenia. Arch Gen Psychiatry, 52(9), 735–746. doi: 10.1001/archpsyc.1995.03950210029008 [DOI] [PubMed] [Google Scholar]
- Exner C, Boucsein K, Degner D, Irle E, & Weniger G (2004). Impaired emotional learning and reduced amygdala size in schizophrenia: a 3-month follow-up. Schizophr Res, 71(2-3), 493–503. doi: 10.1016/j.schres.2004.02.023 [DOI] [PubMed] [Google Scholar]
- Exner C, Nehrkorn B, Martin V, Huber M, Shiratori K, & Rief W (2008). Sex-dependent hippocampal volume reductions in schizophrenia relate to episodic memory deficits. J Neuropsychiatry Clin Neurosci, 20(2), 227–230. doi:10.1176/appi.neuropsych.20.2.227 10.1176/appi.neuropsych.20.2.22710.1176/jnp.2008.20.2.227 [DOI] [PubMed] [Google Scholar]
- Exner C, Weniger G, Schmidt-Samoa C, & Irle E (2006). Reduced size of the pre-supplementary motor cortex and impaired motor sequence learning in first-episode schizophrenia. Schizophr Res, 84(2-3), 386–396. doi: 10.1016/j.schres.2006.03.013 [DOI] [PubMed] [Google Scholar]
- Fannon D, Chitnis X, Doku V, Tennakoon L, O’Ceallaigh S, Soni W, … Sharma T (2000). Features of structural brain abnormality detected in first-episode psychosis. Am J Psychiatry, 157(11), 1829–1834. doi: 10.1176/appi.ajp.157.11.1829 [DOI] [PubMed] [Google Scholar]
- Fenton WS, McGlashan TH, Victor BJ, & Blyler CR (1997). Symptoms, subtype, and suicidality in patients with schizophrenia spectrum disorders. Am J Psychiatry, 154(2), 199–204. doi: 10.1176/ajp.154.2.199 [DOI] [PubMed] [Google Scholar]
- Frederikse M, Lu A, Aylward E, Barta P, Sharma T, & Pearlson G (2000). Sex differences in inferior parietal lobule volume in schizophrenia. Am J Psychiatry, 157(3), 422–427. doi: 10.1176/appi.ajp.157.3.422 [DOI] [PubMed] [Google Scholar]
- Fujiwara H, Hirao K, Namiki C, Yamada M, Shimizu M, Fukuyama H, … Murai T (2007). Anterior cingulate pathology and social cognition in schizophrenia: a study of gray matter, white matter and sulcal morphometry. Neuroimage, 36(4), 1236–1245. doi: 10.1016/j.neuroimage.2007.03.068 [DOI] [PubMed] [Google Scholar]
- Gardner DM, Murphy AL, O’Donnell H, Centorrino F, & Baldessarini RJ (2010). International consensus study of antipsychotic dosing. Am J Psychiatry, 167(6), 686–693. doi: 10.1176/appi.ajp.2009.09060802 [DOI] [PubMed] [Google Scholar]
- Garver DL, Holcomb JA, & Christensen JD (2005). Cerebral cortical gray expansion associated with two second-generation antipsychotics. Biol Psychiatry, 58(1), 62–66. doi: 10.1016/j.biopsych.2005.02.008 [DOI] [PubMed] [Google Scholar]
- Gilbert AR, Rosenberg DR, Harenski K, Spencer S, Sweeney JA, & Keshavan MS (2001). Thalamic volumes in patients with first-episode schizophrenia. Am J Psychiatry, 158(4), 618–624. doi: 10.1176/appi.ajp.158.4.618 [DOI] [PubMed] [Google Scholar]
- Glenthoj A, Glenthoj BY, Mackeprang T, Pagsberg AK, Hemmingsen RP, Jernigan TL, & Baare WF (2007). Basal ganglia volumes in drug-naive first-episode schizophrenia patients before and after short-term treatment with either a typical or an atypical antipsychotic drug. Psychiatry Res, 154(3), 199–208. doi: 10.1016/j.pscychresns.2006.10.002 [DOI] [PubMed] [Google Scholar]
- Goghari VM, Macdonald AW 3rd, & Sponheim SR (2011). Temporal lobe structures and facial emotion recognition in schizophrenia patients and nonpsychotic relatives. Schizophr Bull, 37(6), 1281–1294. doi: 10.1093/schbul/sbq046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gogtay N, Sporn A, Clasen LS, Nugent TF 3rd, Greenstein D, Nicolson R, … Rapoport JL (2004). Comparison of progressive cortical gray matter loss in childhood-onset schizophrenia with that in childhood-onset atypical psychoses. Arch Gen Psychiatry, 61(1), 17–22. doi: 10.1001/archpsyc.61.1.17 [DOI] [PubMed] [Google Scholar]
- Gottesman II, & Shields J (1972). A polygenic theory of schizophrenia. Int J Ment Health, 1(1-2), 107–115. doi: 10.1073/pnas.58.1.199 [DOI] [Google Scholar]
- Gruner P, Christian C, Robinson DG, Sevy S, Gunduz-Bruce H, Napolitano B, … Szeszko PR (2012). Pituitary volume in first-episode schizophrenia. Psychiatry Res, 203(1), 100–102. doi: 10.1016/j.pscychresns.2011.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo W, Hu M, Fan X, Liu F, Wu R, Chen J, … Zhao J (2014). Decreased gray matter volume in the left middle temporal gyrus as a candidate biomarker for schizophrenia: a study of drug naive, first-episode schizophrenia patients and unaffected siblings. Schizophr Res, 159(1), 43–50. doi: 10.1016/j.schres.2014.07.051 [DOI] [PubMed] [Google Scholar]
- Gur RE, Maany V, Mozley PD, Swanson C, Bilker W, & Gur RC (1998). Subcortical MRI volumes in neuroleptic-naive and treated patients with schizophrenia. Am J Psychiatry, 155(12), 1711–1717. doi: 10.1176/ajp.155.12.1711 [DOI] [PubMed] [Google Scholar]
- Gur RE, Turetsky BI, Bilker WB, & Gur RC (1999). Reduced gray matter volume in schizophrenia. Arch Gen Psychiatry, 56(10), 905–911. doi: 10.1001/archpsyc.56.10.905 [DOI] [PubMed] [Google Scholar]
- Gutierrez-Galve L, Chu EM, Leeson VC, Price G, Barnes TR, Joyce EM, & Ron MA (2015). A longitudinal study of cortical changes and their cognitive correlates in patients followed up after first-episode psychosis. Psychol Med, 45(1), 205–216. doi: 10.1017/S0033291714001433 [DOI] [PubMed] [Google Scholar]
- Ha TH, Yoon U, Lee KJ, Shin YW, Lee JM, Kim IY, … Kwon JS (2005). Fractal dimension of cerebral cortical surface in schizophrenia and obsessive-compulsive disorder. Neurosci Lett, 384(1-2), 172–176. doi: 10.1016/j.neulet.2005.04.078 [DOI] [PubMed] [Google Scholar]
- Haijma SV, Van Haren N, Cahn W, Koolschijn PC, Hulshoff Pol HE, & Kahn RS (2013). Brain volumes in schizophrenia: a meta-analysis in over 18 000 subjects. Schizophr Bull, 39(5), 1129–1138. doi: 10.1093/schbul/sbs118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han HJ, Jung WH, Jang JH, Hwang JY, Kim SN, Byun MS, … Kwon JS (2012). Reduced volume in the anterior internal capsule but its maintained correlation with the frontal gray matter in subjects at ultra-high risk for psychosis. Psychiatry Res, 204(2-3), 82–90. doi: 10.1016/j.pscychresns.2012.09.012 [DOI] [PubMed] [Google Scholar]
- Harvey I, Williams M, Toone BK, Lewis SW, Turner SW, & McGuffin P (1990). The ventricular-brain ratio (VBR) in functional psychoses: The relationship of lateral ventricular and total intracranial area. Psychol Med, 20(1), 55–62. doi: 10.1017/S0033291700013222Published [DOI] [PubMed] [Google Scholar]
- Hasan A, Kremer L, Gruber O, Schneider-Axmann T, Guse B, Reith W, … Wobrock T (2011). Planum temporale asymmetry to the right hemisphere in first-episode schizophrenia. Psychiatry Res, 193(1), 56–59. doi: 10.1016/j.pscychresns.2011.02.008 [DOI] [PubMed] [Google Scholar]
- Hasan A, Wobrock T, Falkai P, Schneider-Axmann T, Guse B, Backens M, … Scherk H (2014). Hippocampal integrity and neurocognition in first-episode schizophrenia: a multidimensional study. World J Biol Psychiatry, 15(3), 188–199. doi: 10.3109/15622975.2011.620002 [DOI] [PubMed] [Google Scholar]
- Haukvik UK, McNeil T, Nesvag R, Soderman E, Jonsson E, & Agartz I (2010). No effect of obstetric complications on basal ganglia volumes in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry, 34(4), 619–623. doi: 10.1016/j.pnpbp.2010.02.024 [DOI] [PubMed] [Google Scholar]
- Hazlett EA, Buchsbaum MS, Haznedar MM, Newmark R, Goldstein KE, Zelmanova Y, … Siever LJ (2008). Cortical gray and white matter volume in unmedicated schizotypal and schizophrenia patients. Schizophr Res, 101(1-3), 111–123. doi: 10.1016/j.schres.2007.12.472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herold CJ, Lasser MM, Schmid LA, Seidl U, Kong L, Fellhauer I, … Schroder J (2013). Hippocampal volume reduction and autobiographical memory deficits in chronic schizophrenia. Psychiatry Res, 211(3), 189–194. doi: 10.1016/j.pscychresns.2012.04.002 [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, & Altman DG (2003). Measuring inconsistency in meta-analyses. BMJ, 327(7414), 557–560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirayasu Y, McCarley RW, Salisbury DF, Tanaka S, Kwon JS, Frumin M, … Shenton ME (2000). Planum temporale and Heschl gyrus volume reduction in schizophrenia: a magnetic resonance imaging study of first-episode patients. Arch Gen Psychiatry, 57(7), 692–699. doi:10-1001/pubs.Arch Gen Psychiatry-ISSN-0003-990x-57-7-yoa9242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirayasu Y, Tanaka S, Shenton ME, Salisbury DF, DeSantis MA, Levitt JJ, … McCarley RW (2001). Prefrontal gray matter volume reduction in first episode schizophrenia. Cereb Cortex, 11(4), 374–381. doi: 10.1093/cercor/11.4.374 [DOI] [PubMed] [Google Scholar]
- Ho BC, & Magnotta V (2010). Hippocampal volume deficits and shape deformities in young biological relatives of schizophrenia probands. Neuroimage, 49(4), 3385–3393. doi: 10.1016/j.neuroimage.2009.11.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horacek J, Flegr J, Tintera J, Verebova K, Spaniel F, Novak T, … Hoschl C (2012). Latent toxoplasmosis reduces gray matter density in schizophrenia but not in controls: voxel-based-morphometry (VBM) study. World J Biol Psychiatry, 13(7), 501–509. doi: 10.3109/15622975.2011.573809 [DOI] [PubMed] [Google Scholar]
- Horga G, Bernacer J, Dusi N, Entis J, Chu K, Hazlett EA, … Buchsbaum MS (2011). Correlations between ventricular enlargement and gray and white matter volumes of cortex, thalamus, striatum, and internal capsule in schizophrenia. Eur Arch Psychiatry Clin Neurosci, 261(7), 467–476. doi: 10.1007/s00406-011-0202-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houenou J, d’Albis MA, Daban C, Hamdani N, Delavest M, Lepine JP, … Leboyer M (2014). Cytomegalovirus seropositivity and serointensity are associated with hippocampal volume and verbal memory in schizophrenia and bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry, 48, 142–148. doi: 10.1016/j.pnpbp.2013.09.003 [DOI] [PubMed] [Google Scholar]
- Hulshoff Pol HE, Schnack HG, Bertens MG, van Haren NE, van der Tweel I, Staal WG, … Kahn RS (2002). Volume changes in gray matter in patients with schizophrenia. Am J Psychiatry, 159(2), 244–250. doi: 10.1176/appi.ajp.159.2.244 [DOI] [PubMed] [Google Scholar]
- Ichimiya T, Okubo Y, Suhara T, & Sudo Y (2001). Reduced volume of the cerebellar vermis in neuroleptic-naive schizophrenia. Biol Psychiatry, 49(1), 20–27. doi: 10.1016/s0006-3223(00)01081-7 [DOI] [PubMed] [Google Scholar]
- Irle E, Lange C, Ruhleder M, Exner C, Siemerkus J, & Weniger G (2011). Hippocampal size in women but not men with schizophrenia relates to disorder duration. Psychiatry Res, 192(3), 133–139. doi: 10.1016/j.pscychresns.2010.12.009 [DOI] [PubMed] [Google Scholar]
- Iwashiro N, Suga M, Takano Y, Inoue H, Natsubori T, Satomura Y, … Yamasue H (2012). Localized gray matter volume reductions in the pars triangularis of the inferior frontal gyrus in individuals at clinical high-risk for psychosis and first episode for schizophrenia. Schizophr Res, 137(1-3), 124–131. doi: 10.1016/j.schres.2012.02.024 [DOI] [PubMed] [Google Scholar]
- James ACD, Crow TJ, Renowden S, Wardell AMJ, Smith DM, & Anslow P (1999). Is the course of brain development in schizophrenia delayed? Evidence from onsets in adolescence. Schizophr Res, 40(1), 1–10. doi: 10.1016/s0920-9964(99)00042-0 [DOI] [PubMed] [Google Scholar]
- Jang DP, Kim JJ, Chung TS, An SK, Jung YC, Lee JK, … Kim SI (2006). Shape deformation of the insula in schizophrenia. Neuroimage, 32(1), 220–227. doi: 10.1016/j.neuroimage.2006.01.032 [DOI] [PubMed] [Google Scholar]
- Jayakumar PN, Venkatasubramanian G, Gangadhar BN, Janakiramaiah N, & Keshavan MS (2005). Optimized voxel-based morphometry of gray matter volume in first-episode, antipsychotic-naive schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry, 29(4), 587–591. doi: 10.1016/j.pnpbp.2005.01.020 [DOI] [PubMed] [Google Scholar]
- John JP, Burgess PW, Yashavantha BS, Shakeel MK, Halahalli HN, & Jain S (2009). Differential relationship of frontal pole and whole brain volumetric measures with age in neuroleptic-naive schizophrenia and healthy subjects. Schizophr Res, 109(1-3), 148–158. doi: 10.1016/j.schres.2008.12.019 [DOI] [PubMed] [Google Scholar]
- Johnstone EC, Crow TJ, Frith CD, Husband J, & Kreel L (1976). Cerebral ventricular size and cognitive impairment in chronic schizophrenia. Lancet, 2(7992), 924–926. doi: 10.1016/S0140-6736(76)90890-4 [DOI] [PubMed] [Google Scholar]
- Jung WH, Jang JH, Shin NY, Kim SN, Choi CH, An SK, & Kwon JS (2012). Regional brain atrophy and functional disconnection in Broca’s area in individuals at ultra-high risk for psychosis and schizophrenia. PLoS One, 7(12), e51975. doi: 10.1371/journal.pone.0051975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung WH, Kim JS, Jang JH, Choi JS, Jung MH, Park JY, … Kwon JS (2011). Cortical thickness reduction in individuals at ultra-high-risk for psychosis. Schizophr Bull, 37(4), 839–849. doi: 10.1093/schbul/sbp151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmady SV, Venkatasubramanian G, Shivakumar V, Gautham S, Subramaniam A, Jose DA, … Gangadhar BN (2014). Relationship between interleukin-6 gene polymorphism and hippocampal volume in antipsychotic-naïve schizophrenia: Evidence for differential susceptibility? PLoS One, 9(5). doi: 10.1371/journal.pone.0096021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalus P, Buri C, Slotboom J, Gralla J, Remonda L, Dierks T, … Kiefer C (2004). Volumetry and diffusion tensor imaging of hippocampal subregions in schizophrenia. Neuroreport, 15(5), 867–871. doi: 10.1097/00001756-200404090-00027 [DOI] [PubMed] [Google Scholar]
- Kang DH, Kwon KW, Gu BM, Choi JS, Jang JH, & Kwon JS (2008). Structural abnormalities of the right inferior colliculus in schizophrenia. Psychiatry Res, 164(2), 160–165. doi: 10.1016/j.pscychresns.2007.12.023 [DOI] [PubMed] [Google Scholar]
- Kasai K, Shenton ME, Salisbury DF, Onitsuka T, Toner SK, Yurgelun-Todd D, … McCarley RW (2003). Differences and similarities in insular and temporal pole MRI gray matter volume abnormalities in first-episode schizophrenia and affective psychosis. Arch Gen Psychiatry, 60(11), 1069–1077. doi: 10.1001/archpsyc.60.11.1069 [DOI] [PubMed] [Google Scholar]
- Kegeles LS, Shungu DC, Anjilvel S, Chan S, Ellis SP, Xanthopoulos E, … Kaufmann CA (2000). Hippocampal pathology in schizophrenia: magnetic resonance imaging and spectroscopy studies. Psychiatry Res, 98(3), 163–175. doi: 10.1016/s0925-4927(00)00044-5 [DOI] [PubMed] [Google Scholar]
- Keller A, Castellanos FX, Vaituzis AC, Jeffries NO, Giedd JN, & Rapoport JL (2003). Progressive loss of cerebellar volume in childhood-onset schizophrenia. Am J Psychiatry, 160(1), 128–133. doi: 10.1176/appi.ajp.160.1.128 [DOI] [PubMed] [Google Scholar]
- Kemether EM, Buchsbaum MS, Byne W, Hazlett EA, Haznedar M, Brickman AM, … Bloom R (2003). Magnetic resonance imaging of mediodorsal, pulvinar, and centromedian nuclei of the thalamus in patients with schizophrenia. Arch Gen Psychiatry, 60(10), 983–991. doi: 10.1001/archpsyc.60.9.983 [DOI] [PubMed] [Google Scholar]
- Keri S, Szamosi A, Benedek G, & Kelemen O (2012). How does the hippocampal formation mediate memory for stimuli processed by the magnocellular and parvocellular visual pathways? Evidence from the comparison of schizophrenia and amnestic mild cognitive impairment (aMCI). Neuropsychologia, 50(14), 3193–3199. doi: 10.1016/j.neuropsychologia.2012.10.010 [DOI] [PubMed] [Google Scholar]
- Keshavan MS, Haas GL, Kahn CE, Aguilar E, Dick EL, Schooler NR, … Pettegrew JW (1998). Superior temporal gyrus and the course of early schizophrenia: progressive, static, or reversible? J Psychiatr Res, 32(3-4), 161–167. doi: 10.1016/s0022-3956(97)00038-1 [DOI] [PubMed] [Google Scholar]
- Keshavan MS, Rosenberg D, Sweeney JA, & Pettegrew JW (1998). Decreased caudate volume in neuroleptic-naive psychotic patients. Am J Psychiatry, 755(6), 774–778. doi: 10.1176/ajp.155.6.774 [DOI] [PubMed] [Google Scholar]
- Kim JJ, Kim DJ, Kim TG, Seok JH, Chun JW, Oh MK, & Park HJ (2007). Volumetric abnormalities in connectivity-based subregions of the thalamus in patients with chronic schizophrenia. Schizophr Res, 97(1-3), 226–235. doi: 10.1016/j.schres.2007.09.007 [DOI] [PubMed] [Google Scholar]
- Kim JJ, Youn T, Lee JM, Kim IY, Kim SI, & Kwon JS (2003b). Morphometric abnormality of the insula in schizophrenia: a comparison with obsessive-compulsive disorder and normal control using MRI. Schizophr Res, 60(2-3), 191–198. doi: 10.1016/s0920-9964(02)00306-7 [DOI] [PubMed] [Google Scholar]
- Klar AA, Ballmaier M, Leopold K, Hake I, Schaefer M, Bruhl R, … Gallinat J (2010). Interaction of hippocampal volume and N-acetylaspartate concentration deficits in schizophrenia: a combined MRI and 1H-MRS study. Neuroimage, 53(1), 51–57. doi: 10.1016/j.neuroimage.2010.06.006 [DOI] [PubMed] [Google Scholar]
- Koo MS, Levitt JJ, Salisbury DF, Nakamura M, Shenton ME, & McCarley RW (2008). A cross-sectional and longitudinal magnetic resonance imaging study of cingulate gyrus gray matter volume abnormalities in first-episode schizophrenia and first-episode affective psychosis. Arch Gen Psychiatry, 65(7), 746–760. doi: 10.1001/archpsyc.65.7.746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koolschijn PC, van Haren NE, Cahn W, Schnack HG, Janssen J, Klumpers F, … Kahn RS (2010). Hippocampal volume change in schizophrenia. J Clin Psychiatry, 71(6), 737–744. doi: 10.4088/JCP.08m04574yel [DOI] [PubMed] [Google Scholar]
- Kumra S, Ashtari M, Wu J, Hongwanishkul D, White T, Cervellione K, … Szeszko PR (2011). Gray matter volume deficits are associated with motor and attentional impairments in adolescents with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry, 35(4), 939–943. doi: 10.1016/j.pnpbp.2011.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumra S, Giedd JN, Vaituzis AC, Jacobsen LK, McKenna K, Bedwell J, … Rapoport JL (2000). Childhood-onset psychotic disorders: magnetic resonance imaging of volumetric differences in brain structure. Am J Psychiatry, 157(9), 1467–1474. doi: 10.1176/appi.ajp.157.9.1467 [DOI] [PubMed] [Google Scholar]
- Kuroki N, Kubicki M, Nestor PG, Salisbury DF, Park HJ, Levitt JJ, … Shenton ME (2006). Fornix integrity and hippocampal volume in male schizophrenic patients. Biol Psychiatry, 60(1), 22–31. doi: 10.1016/j.biopsych.2005.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon JS, McCarley RW, Hirayasu Y, Anderson JE, Fischer IA, Kikinis R, … Shenton ME (1999). Left planum temporale volume reduction in schizophrenia. Arch Gen Psychiatry, 56(2), 142–148. doi: 10.1001/archpsyc.56.2.142 [DOI] [PubMed] [Google Scholar]
- Kwon JS, Shin YW, Kim CW, Kim YI, Youn T, Han MH, … Kim JJ (2003). Similarity and disparity of obsessive-compulsive disorder and schizophrenia in MR volumetric abnormalities of the hippocampus-amygdala complex. J Neurol Neurosurg Psychiatry, 74(7), 962–964. doi: 10.1136/jnnp.74.7.962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacerda AL, Hardan AY, Yorbik O, Vemulapalli M, Prasad KM, & Keshavan MS (2007). Morphology of the orbitofrontal cortex in first-episode schizophrenia: relationship with negative symptomatology. Prog Neuropsychopharmacol Biol Psychiatry, 31(2), 510–516. doi: 10.1016/j.pnpbp.2006.11.022 [DOI] [PubMed] [Google Scholar]
- Lang DJ, Khorram B, Goghari VM, Kopala LC, Vandorpe RA, Rui Q, … Honer WG (2006). Reduced anterior internal capsule and thalamic volumes in first-episode psychosis. Schizophr Res, 87(1-3), 89–99. doi: 10.1016/j.schres.2006.05.002 [DOI] [PubMed] [Google Scholar]
- Lappin JM, Morgan C, Chalavi S, Morgan KD, Reinders AA, Fearon P, … Dazzan P (2014). Bilateral hippocampal increase following first-episode psychosis is associated with good clinical, functional and cognitive outcomes. Psychol Med, 44(6), 1279–1291. doi: 10.1017/s0033291713001712 [DOI] [PubMed] [Google Scholar]
- Lawrie SM, Whalley HC, Abukmeil SS, Kestelman JN, Donnelly L, Miller P, … Johnstone EC (2001). Brain structure, genetic liability, and psychotic symptoms in subjects at high risk of developing schizophrenia. Biol Psychiatry, 49(10), 811–823. doi:Doi 10.1016/S0006-3223(00)01117-3 [DOI] [PubMed] [Google Scholar]
- Lawyer G, Nesvag R, Varnas K, Frigessi A, & Agartz I (2008). Investigating possible subtypes of schizophrenia patients and controls based on brain cortical thickness. Psychiatry Res, 164(3), 254–264. doi: 10.1016/j.pscychresns.2007.12.017 [DOI] [PubMed] [Google Scholar]
- Lee CU, Shenton ME, Salisbury DF, Kasai K, Onitsuka T, Dickey CC, … McCarley RW (2002). Fusiform gyrus volume reduction in first-episode schizophrenia: a magnetic resonance imaging study. Arch Gen Psychiatry, 59(9), 775–781. doi: 10.1001/archpsyc.59.9.775 [DOI] [PubMed] [Google Scholar]
- Leonard CM, Kuldau JM, Breier JI, Zuffante PA, Gautier ER, Heron DC, … DeBose CA (1999). Cumulative effect of anatomical risk factors for schizophrenia: an MRI study. Biol Psychiatry, 46(3), 374–382. doi: 10.1016/s0006-3223(99)00052-9 [DOI] [PubMed] [Google Scholar]
- Leonard CM, Towler S, Welcome S, Halderman LK, Otto R, Eckert MA, & Chiarello C (2008). Size matters: Cerebral volume influences sex differences in neuroanatomy. Cereb Cortex, 18(12), 2920–2931. doi: 10.1093/cercor/bhn052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitt JJ, Alvarado JL, Nestor PG, Rosow L, Pelavin PE, McCarley RW, … Shenton ME (2012). Fractional anisotropy and radial diffusivity: diffusion measures of white matter abnormalities in the anterior limb of the internal capsule in schizophrenia. Schizophr Res, 136(1-3), 55–62. doi: 10.1016/j.schres.2011.09.009 [DOI] [PubMed] [Google Scholar]
- Levitt JJ, Rosow LK, Nestor PG, Pelavin PE, Swisher TM, McCarley RW, & Shenton ME (2013). A volumetric MRI study of limbic, associative and sensorimotor striatal subregions in schizophrenia. Schizophr Res, 145(1-3), 11–19. doi: 10.1016/j.schres.2012.08.032 [DOI] [PubMed] [Google Scholar]
- Liu X, Lai Y, Wang X, Hao C, Chen L, Zhou Z, … Hong N (2014). A combined DTI and structural MRI study in medicated-naive chronic schizophrenia. Magn Reson Imaging, 32(1), 1–8. doi: 10.1016/j.mri.2013.08.004 [DOI] [PubMed] [Google Scholar]
- Mackay CE, Barrick TR, Roberts N, DeLisi LE, Maes F, Vandermeulen D, & Crow TJ (2003). Application of a new image analysis technique to study brain asymmetry in schizophrenia. Psychiatry Res, 124(1), 25–35. doi: 10.1016/s0925-4927(03)00088-x [DOI] [PubMed] [Google Scholar]
- Mahon PB, Eldridge H, Crocker B, Notes L, Gindes H, Postell E, … Barta PE (2012). An MRI study of amygdala in schizophrenia and psychotic bipolar disorder. Schizophr Res, 138(2-3), 188–191. doi: 10.1016/j.schres.2012.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahurin RK, Velligan DI, & Miller AL (1998). Executive-frontal lobe cognitive dysfunction in schizophrenia: A symptom subtype analysis. Psychiatry Res, 79(2), 139–149. doi: 10.1016/S0165-1781(98)00031-6 [DOI] [PubMed] [Google Scholar]
- Malchow B, Hasan A, Schneider-Axmann T, Jatzko A, Gruber O, Schmitt A, … Wobrock T (2013). Effects of cannabis and familial loading on subcortical brain volumes in first-episode schizophrenia. Eur Arch Psychiatry Clin Neurosci, 263 Suppl 2, S155–168. doi: 10.1007/s00406-013-0451-y [DOI] [PubMed] [Google Scholar]
- Maller JJ, Daskalakis ZJ, Thomson RH, Daigle M, Barr MS, & Fitzgerald PB(2012). Hippocampal volumetrics in treatment-resistant depression and schizophrenia: the devil’s in de-tail. Hippocampus, 22(1), 9–16. doi: 10.1002/hipo.20873 [DOI] [PubMed] [Google Scholar]
- Mamah D, Harms MP, Barch D, Styner M, Lieberman JA, & Wang L (2012). Hippocampal shape and volume changes with antipsychotics in early stage psychotic illness. Front Psychiatry, 3, 96. doi: 10.3389/fpsyt.2012.00096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamah D, Wang L, Barch D, de Erausquin GA, Gado M, & Csernansky JG (2007). Structural analysis of the basal ganglia in schizophrenia. Schizophr Res, 59(1-3), 59–71. doi: 10.1016/j.schres.2006.08.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquardt RK, Levitt JG, Blanton RE, Caplan R, Asarnow R, Siddarth P, … Toga AW (2005). Abnormal development of the anterior cingulate in childhood-onset schizophrenia: a preliminary quantitative MRI study. Psychiatry Res, 135(3), 221–233. doi: 10.1016/j.pscychresns.2005.01.001 [DOI] [PubMed] [Google Scholar]
- Mathalon DH, Pfefferbaum A, Lim KO, Rosenbloom MJ, & Sullivan EV (2003). Compounded brain volume deficits in schizophrenia-alcoholism comorbidity. Arch Gen Psychiatry, 60(3), 245–252. doi: 10.1001/archpsyc.60.3.245 [DOI] [PubMed] [Google Scholar]
- Mathew I, Gardin TM, Tandon N, Eack S, Francis AN, Seidman LJ, … Keshavan MS (2014). Medial temporal lobe structures and hippocampal subfields in psychotic disorders: findings from the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP) study. JAMA Psychiatry, 71(7), 769–777. doi: 10.1001/jamapsychiatry.2014.453 [DOI] [PubMed] [Google Scholar]
- Matsui M, Suzuki M, Zhou SY, Takahashi T, Kawasaki Y, Yuuki H, … Kurachi M (2008). The relationship between prefrontal brain volume and characteristics of memory strategy in schizophrenia spectrum disorders. Prog Neuropsychopharmacol Biol Psychiatry, 32(8), 1854–1862. doi: 10.1016/j.pnpbp.2008.08.018 [DOI] [PubMed] [Google Scholar]
- Matsumae M, Kikinis R, Morocz IA, Lorenzo AV, Sandor T, Albert MS, … Jolesz FA (1996). Age-related changes in intracranial compartment volumes in normal adults assessed by magnetic resonance imaging. J Neurosurg, 84(6), 982–991. doi: 10.3171/jns.1996.84.6.0982 [DOI] [PubMed] [Google Scholar]
- Matsumoto H, Simmons A, Williams S, Hadjulis M, Pipe R, Murray R, & Frangou S (2001). Superior temporal gyrus abnormalities in early-onset schizophrenia: similarities and differences with adult-onset schizophrenia. Am J Psychiatry, 158(8), 1299–1304. doi: 10.1176/appi.ajp.158.8.1299 [DOI] [PubMed] [Google Scholar]
- Matsumoto H, Simmons A, Williams S, Pipe R, Murray R, & Frangou S (2001a). Structural magnetic imaging of the hippocampus in early onset schizophrenia. Biol Psychiatry, 49(10), 824–831. doi: 10.1016/S0006-3223(01)01073-3 [DOI] [PubMed] [Google Scholar]
- Meisenzahl EM, Frodl T, Greiner J, Leinsinger G, Maag KP, Heiss D, … Möller HJ (1999). Corpus callosum size in schizophrenia - a magnetic resonance imaging analysis. Eur Arch Psychiatry Clin Neurosci, 249(6), 305–312. doi: 10.1007/s004060050104 [DOI] [PubMed] [Google Scholar]
- Meisenzahl EM, Frodl T, Müller D, Schmitt G, Gallinat J, Zetzsche T, … Hegerl U (2004). Superior temporal gyrus and P300 in schizophrenia: a combined ERP/structural magnetic resonance imaging investigation. J Psychiatr Res, 38(2), 153–162. doi: 10.1016/s0022-3956(03)00078-5 [DOI] [PubMed] [Google Scholar]
- Meisenzahl EM, Frodl T, Zetzsche T, Leinsinger G, Maag K, Hegerl U, … Möller H-J (2002). Investigation of a possible diencephalic pathology in schizophrenia. Psychiatry Res, 115(3), 127–135. doi: 10.1016/s0925-4927(02)00044-6 [DOI] [PubMed] [Google Scholar]
- Meisenzahl EM, Zetzsche T, Preuss U, Frodl T, Leinsinger G, & Moller HJ (2002). Does the definition of borders of the planum temporale influence the results in schizophrenia? Am J Psychiatry, 159(7), 1198–1200. doi: 10.1176/appi.ajp.159.7.1198 [DOI] [PubMed] [Google Scholar]
- Molina V, Sanz J, Sarramea F, Misiego JM, Benito C, & Palomo T (2005). Association between excessive frontal cerebrospinal fluid and illness duration in males but not in females with schizophrenia. Eur Psychiatry, 20(4), 332–338. doi: 10.1016/j.eurpsy.2004.11.015 [DOI] [PubMed] [Google Scholar]
- Morgan KD, Dazzan P, Orr KG, Hutchinson G, Chitnis X, Suckling J, … Murray RM (2007). Grey matter abnormalities in first-episode schizophrenia and affective psychosis. Br J Psychiatry Suppl, 51, s111–116. doi: 10.1192/bjp.191.51.s111 [DOI] [PubMed] [Google Scholar]
- Moriya J, Kakeda S, Abe O, Goto N, Yoshimura R, Hori H, … Korogi Y (2010). Gray and white matter volumetric and diffusion tensor imaging (DTI) analyses in the early stage of first-episode schizophrenia. Schizophr Res, 116(2-3), 196–203. doi: 10.1016/j.schres.2009.10.002 [DOI] [PubMed] [Google Scholar]
- Murakami M, Takao H, Abe O, Yamasue H, Sasaki H, Gonoi W, … Ohtomo K (2011). Cortical thickness, gray matter volume, and white matter anisotropy and diffusivity in schizophrenia. Neuroradiology, 53(11), 859–866. doi: 10.1007/s00234-010-0830-2 [DOI] [PubMed] [Google Scholar]
- Nakagawa S, Poulin R, Mengersen K, Reinhold K, Engqvist L, Lagisz M, & Senior AM (2015). Meta-analysis of variation: ecological and evolutionary applications and beyond. Methods Ecol Evol, 6(2), 143–152. doi: 10.1111/2041-210X.12309 [DOI] [Google Scholar]
- Nakamura K, Takahashi T, Nemoto K, Furuichi A, Nishiyama S, Nakamura Y, … Suzuki M (2013). Gray matter changes in subjects at high risk for developing psychosis and first-episode schizophrenia: a voxel-based structural MRI study. Front Psychiatry, 4, 16. doi: 10.3389/fpsyt.2013.00016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura M, Nestor PG, McCarley RW, Levitt JJ, Hsu L, Kawashima T, … Shenton ME (2007). Altered orbitofrontal sulcogyral pattern in schizophrenia. Brain, 130(Pt 3), 693–707. doi: 10.1093/brain/awm007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura M, Salisbury DF, Hirayasu Y, Bouix S, Pohl KM, Yoshida T, … McCarley RW (2007a). Neocortical gray matter volume in first-episode schizophrenia and first-episode affective psychosis: a cross-sectional and longitudinal MRI study. Biol Psychiatry, 62(7), 773–783. doi: 10.1016/j.biopsych.2007.03.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayan VM, Narr KL, Kumari V, Woods RP, Thompson PM, Toga AW, & Sharma T (2007). Regional cortical thinning in subjects with violent antisocial personality disorder or schizophrenia. Am J Psychiatry, 164(9), 1418–1427. doi: 10.1176/appi.ajp.2007.06101631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narr KL, Bilder RM, Toga AW, Woods RP, Rex DE, Szeszko PR, … Thompson PM (2005). Mapping cortical thickness and gray matter concentration in first episode schizophrenia. Cereb Cortex, 15(6), 708–719. doi: 10.1093/cercor/bhh172 [DOI] [PubMed] [Google Scholar]
- Narr KL, Bilder RM, Woods RP, Thompson PM, Szeszko P, Robinson D, … Toga AW (2006). Regional specificity of cerebrospinal fluid abnormalities in first episode schizophrenia. Psychiatry Res, 146(1), 21–33. doi: 10.1016/j.pscychresns.2005.10.005 [DOI] [PubMed] [Google Scholar]
- Narr KL, Sharma T, Woods RP, Thompson PM, Sowell ER, Rex D, … Toga AW (2003). Increases in regional subarachnoid CSF without apparent cortical gray matter deficits in schizophrenia: modulating effects of sex and age. Am J Psychiatry, 160(12), 2169–2180. doi: 10.1176/appi.ajp.160.12.2169 [DOI] [PubMed] [Google Scholar]
- Narr KL, Thompson PM, Szeszko P, Robinson D, Jang S, Woods RP, … Bilder RM (2004). Regional specificity of hippocampal volume reductions in first-episode schizophrenia. Neuroimage, 21(4), 1563–1575. doi: 10.1016/j.neuroimage.2003.11.011 [DOI] [PubMed] [Google Scholar]
- Nesvag R, Frigessi A, Jonsson EG, & Agartz I (2007). Effects of alcohol consumption and antipsychotic medication on brain morphology in schizophrenia. Schizophr Res, 90(1-3), 52–61. doi: 10.1016/j.schres.2006.11.008 [DOI] [PubMed] [Google Scholar]
- Nguyen AD, Pelavin PE, Shenton ME, Chilakamarri P, McCarley RW, Nestor PG, & Levitt JJ (2011). Olfactory sulcal depth and olfactory bulb volume in patients with schizophrenia: an MRI study. Brain Imaging Behav, 5(4), 252–261. doi: 10.1007/s11682-011-9129-0 [DOI] [PubMed] [Google Scholar]
- Niemann K, Hammers A, Coenen VA, Thron A, & Klosterkotter J (2000). Evidence of a smaller left hippocampus and left temporal horn in both patients with first episode schizophrenia and normal control subjects. Psychiatry Res, 99(2), 93–110. doi: 10.1016/S0925-4927(00)00059-7 [DOI] [PubMed] [Google Scholar]
- Nierenberg J, Salisbury DF, Levitt JJ, David EA, McCarley RW, & Shenton ME (2005). Reduced left angular gyrus volume in first-episode schizophrenia. Am J Psychiatry, 162(8), 1539–1541. doi: 10.1176/appi.ajp.162.8.1539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nopoulos PC, Ceilley JW, Gailis EA, & Andreasen NC (1999). An MRI study of cerebellar vermis morphology in patients with schizophrenia: evidence in support of the cognitive dysmetria concept. Biol Psychiatry, 46(5), 703–711. doi: 10.1016/s0006-3223(99)00093-1 [DOI] [PubMed] [Google Scholar]
- O’Daly OG, Frangou S, Chitnis X, & Shergill SS (2007). Brain structural changes in schizophrenia patients with persistent hallucinations. Psychiatry Res, 156(1), 15–21. doi: 10.1016/j.pscychresns.2007.03.001 [DOI] [PubMed] [Google Scholar]
- Oertel V, Knochel C, Rotarska-Jagiela A, Schonmeyer R, Lindner M, van de Ven V, … Linden DE (2010). Reduced laterality as a trait marker of schizophrenia--evidence from structural and functional neuroimaging. J Neurosci, 30(6), 2289–2299. doi: 10.1523/JNEUROSCI.4575-09.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohtani T, Levitt JJ, Nestor PG, Kawashima T, Asami T, Shenton ME, … McCarley RW (2014). Prefrontal cortex volume deficit in schizophrenia: a new look using 3T MRI with manual parcellation. Schizophr Res, 152(1), 184–190. doi: 10.1016/j.schres.2013.10.026 [DOI] [PubMed] [Google Scholar]
- Okugawa G, Nobuhara K, Takase K, Saito Y, Yoshimura M, & Kinoshita T (2007). Olanzapine increases grey and white matter volumes in the caudate nucleus of patients with schizophrenia. Neuropsychobiology, 55(1), 43–46. doi: 10.1159/000103575 [DOI] [PubMed] [Google Scholar]
- Okugawa G, Tamagaki C, & Agartz I (2007C). Frontal and temporal volume size of grey and white matter in patients with schizophrenia: an MRI parcellation study. Eur Arch Psychiatry Clin Neurosci, 257(5), 304–307. doi: 10.1007/s00406-007-0721-7 [DOI] [PubMed] [Google Scholar]
- Onitsuka T, McCarley RW, Kuroki N, Dickey CC, Kubicki M, Demeo SS, … Shenton ME (2007). Occipital lobe gray matter volume in male patients with chronic schizophrenia: A quantitative MRI study. Schizophr Res, 92(1-3), 197–206. doi: 10.1016/j.schres.2007.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onitsuka T, Shenton ME, Salisbury DF, Dickey CC, Kasai K, Toner SK, … McCarley RW (2004). Middle and inferior temporal gyrus gray matter volume abnormalities in chronic schizophrenia: an MRI study. Am J Psychiatry, 161(9), 1603–1611. doi: 10.1176/appi.ajp.161.9.1603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagsberg AK, Baare WF, Raabjerg Christensen AM, Fagerlund B, Hansen MB, Labianca J, … Hemmingsen RP (2007). Structural brain abnormalities in early onset first-episode psychosis. J Neural Transm (Vienna), 114(4), 489–498. doi: 10.1007/s00702-006-0573-8 [DOI] [PubMed] [Google Scholar]
- Papiol S, Molina V, Desco M, Rosa A, Reig S, Gispert JD, … Fananas L (2005). Ventricular enlargement in schizophrenia is associated with a genetic polymorphism at the interleukin-1 receptor antagonist gene. Neuroimage, 27(4), 1002–1006. doi: 10.1016/j.neuroimage.2005.05.035 [DOI] [PubMed] [Google Scholar]
- Park HY, Hwang JY, Jung WH, Shin NY, Shim G, Jang JH, & Kwon JS (2013). Altered asymmetry of the anterior cingulate cortex in subjects at genetic high risk for psychosis. Schizophr Res, 150(2-3), 512–518. doi: 10.1016/j.schres.2013.08.027 [DOI] [PubMed] [Google Scholar]
- Pinkham A, Penn D, Wangelin B, Perkins D, Gerig G, Gu H, & Lieberman J (2005). Facial emotion perception and fusiform gyrus volume in first episode schizophrenia. Schizophr Res, 79(2-3), 341–343. doi: 10.1016/j.schres.2005.07.012 [DOI] [PubMed] [Google Scholar]
- Pirnia T, Woods RP, Hamilton LS, Lyden H, Joshi SH, Asarnow RF, … Narr KL (2015). Hippocampal dysfunction during declarative memory encoding in schizophrenia and effects of genetic liability. Schizophr Res, 161(2-3), 357–366. doi: 10.1016/j.schres.2014.11.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prestia A, Boccardi M, Galluzzi S, Cavedo E, Adorni A, Soricelli A, … Frisoni G (2011). Hippocampal and amygdalar volume changes in elderly patients with Alzheimer’s disease and schizophrenia. Psychiatry Res, 192(2), 77–83. doi: 10.1016/j.pscychresns.2010.12.015 [DOI] [PubMed] [Google Scholar]
- Pujol N, Penades R, Junque C, Dinov I, Fu CH, Catalan R, … Costafreda SG (2014). Hippocampal abnormalities and age in chronic schizophrenia: morphometric study across the adult lifespan. Br J Psychiatry, 205(5), 369–375. doi: 10.1192/bjp.bp.n3.140384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu A, Tuan TA, Woon PS, Abdul-Rahman MF, Graham S, & Sim K (2010). Hippocampal-cortical structural connectivity disruptions in schizophrenia: an integrated perspective from hippocampal shape, cortical thickness, and integrity of white matter bundles. Neuroimage, 52(4), 1181–1189. doi: 10.1016/j.neuroimage.2010.05.046 [DOI] [PubMed] [Google Scholar]
- Qiu A, Zhong J, Graham S, Chia MY, & Sim K (2009). Combined analyses of thalamic volume, shape and white matter integrity in first-episode schizophrenia. Neuroimage, 47(4), 1163–1171. doi: 10.1016/j.neuroimage.2009.04.027 [DOI] [PubMed] [Google Scholar]
- Radeloff D, Ciaramidaro A, Siniatchkin M, Hainz D, Schlitt S, Weber B, … Freitag CM (2014). Structural alterations of the social brain: a comparison between schizophrenia and autism. PLoS One, 9(9), e106539. doi: 10.1371/journal.pone.0106539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajarethinam R, DeQuardo JR, Miedler J, Arndt S, Kirbat R, A. Brunberg J, & Tandon R (2001). Hippocampus and amygdala in schizophrenia: assessment of the relationship of neuroanatomy to psychopathology. Psychiatry Res, 108(2), 79–87. doi: 10.1016/s0925-4927(01)00120-2 [DOI] [PubMed] [Google Scholar]
- Rametti G, Segarra N, Junque C, Bargallo N, Caldu X, Ibarretxe N, & Bernardo M (2007). Left posterior hippocampal density reduction using VBM and stereological MRI procedures in schizophrenia. Schizophr Res, 96(1-3), 62–71. doi: 10.1016/j.schres.2007.04.034 [DOI] [PubMed] [Google Scholar]
- Rao NP, Kalmady S, Arasappa R, & Venkatasubramanian G (2010). Clinical correlates of thalamus volume deficits in anti-psychotic-naive schizophrenia patients: A 3-Tesla MRI study. Indian J Psychiatry, 52(3), 229–235. doi: 10.4103/0019-5545.70975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razi K, Greene KP, Sakuma M, Ge S, Kushner M, & DeLisi LE (1999). Reduction of the parahippocampal gyrus and the hippocampus in patients with chronic schizophrenia. Br J Psychiatry, 174(6), 512–519. doi: 10.1192/bjp.174.6.512 [DOI] [PubMed] [Google Scholar]
- Reig S, Parellada M, Castro-Fornieles J, Janssen J, Moreno D, Baeza I, … Desco M(2011). Multicenter study of brain volume abnormalities in children and adolescent-onset psychosis. Schizophr Bull, 37(6), 1270–1280. doi: 10.1093/schbul/sbq044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riffkin J, Yucel M, Maruff P, Wood SJ, Soulsby B, Olver J, … Pantelis C (2005). A manual and automated MRI study of anterior cingulate and orbito-frontal cortices, and caudate nucleus in obsessive-compulsive disorder: comparison with healthy controls and patients with schizophrenia. Psychiatry Res, 138(2), 99–113. doi: 10.1016/j.pscychresns.2004.11.007 [DOI] [PubMed] [Google Scholar]
- Rigucci S, Rossi-Espagnet C, Ferracuti S, De Carolis A, Corigliano V, Carducci F, … Comparelli A (2013). Anatomical substrates of cognitive and clinical dimensions in first episode schizophrenia. Acta Psychiatr Scand, 128(4), 261–270. doi: 10.1ll1/acps.12051 [DOI] [PubMed] [Google Scholar]
- Rizos EN, Papathanasiou M, Michalopoulou PG, Mazioti A, Douzenis A, Kastania A, … Lykouras L (2011). Association of serum BDNF levels with hippocampal volumes in first psychotic episode drug-naive schizophrenic patients. Schizophr Res, 129(2-3), 201–204. doi: 10.1016/j.schres.2011.03.011 [DOI] [PubMed] [Google Scholar]
- Rossell SL, Shapleske J, Fukuda R, Woodruff PWR, Simmons A, & David AS (2001). Corpus callosum area and functioning in schizophrenic patients with auditory–verbal hallucinations. Schizophr Res, 50(1-2), 9–17. doi: 10.1016/s0920-9964(00)00070-0 [DOI] [PubMed] [Google Scholar]
- Roy PD, Zipursky RB, Saint-Cyr JA, Bury A, Langevin R, & Seeman MV (1998). Temporal horn enlargement is present in schizophrenia and bipolar disorder. Biol Psychiatry, 44(6), 418–422. doi: 10.1016/S0006-3223(98)00105-X [DOI] [PubMed] [Google Scholar]
- Rupp CI, Fleischhacker WW, Kemmler G, Kremser C, Bilder RM, Mechtcheriakov S, … Hinterhuber H (2005). Olfactory functions and volumetric measures of orbitofrontal and limbic regions in schizophrenia. Schizophr Res, 74(2-3), 149–161. doi: 10.1016/j.schres.2004.07.010 [DOI] [PubMed] [Google Scholar]
- Rusch N, Tebartz van Elst L, Valerius G, Buchert M, Thiel T, Ebert D, … Olbrich HM (2008). Neurochemical and structural correlates of executive dysfunction in schizophrenia. Schizophr Res, 99(1-3), 155–163. doi: 10.1016/j.schres.2007.05.024 [DOI] [PubMed] [Google Scholar]
- Salgado-Pineda P, Baeza I, Perez-Gomez M, Vendrell P, Junque C, Bargallo N, & Bernardo M (2003). Sustained attention impairment correlates to gray matter decreases in first episode neuroleptic-naive schizophrenic patients. Neuroimage, 19(2 Pt 1), 365–375. doi: 10.1016/s1053-8119(03)00094-6 [DOI] [PubMed] [Google Scholar]
- Sallet PC, Elkis H, Alves TM, Oliveira JR, Sassi E, de Castro CC, … Gattaz WF (2003). Rightward cerebral asymmetry in subtypes of schizophrenia according to Leonhard’s classification and to DSM-IV: a structural MRI study. Psychiatry Res, 123(1), 65–79. doi: 10.1016/s0925-4927(03)00020-9 [DOI] [PubMed] [Google Scholar]
- Salokangas RK, Cannon T, Van Erp T, Ilonen T, Taiminen T, Karlsson H, … Hietala J (2002). Structural magnetic resonance imaging in patients with first-episode schizophrenia, psychotic and severe non-psychotic depression and healthy controls. Results of the schizophrenia and affective psychoses (SAP) project. Br J Psychiatry Suppl, 43, s58–65. doi: 10.1192/bjp.181.43.s58 [DOI] [PubMed] [Google Scholar]
- Sanfilipo M, Lafargue T, Rusinek H, Arena L, Loneragan C, Lautin A, … Wolkin A (2000). Volumetric measure of the frontal and temporal lobe regions in schizophrenia: relationship to negative symptoms. Arch Gen Psychiatry, 57(5), 471–480. doi: 10.1001/archpsyc.57.5.471 [DOI] [PubMed] [Google Scholar]
- Sapara A, Cooke M, Fannon D, Francis A, Buchanan RW, Anilkumar AP, … Kumari V (2007). Prefrontal cortex and insight in schizophrenia: a volumetric MRI study. Schizophr Res, 59(1-3), 22–34. doi: 10.1016/j.schres.2006.09.016 [DOI] [PubMed] [Google Scholar]
- Saze T, Hirao K, Namiki C, Fukuyama H, Hayashi T, & Murai T (2007). Insular volume reduction in schizophrenia. Eur Arch Psychiatry Clin Neurosci, 257(8), 473–479. doi: 10.1007/s00406-007-0750-2 [DOI] [PubMed] [Google Scholar]
- Scanlon C, Anderson-Schmidt H, Kilmartin L, McInerney S, Kenney J, McFarland J, … McDonald C (2014). Cortical thinning and caudate abnormalities in first episode psychosis and their association with clinical outcome. Schizophr Res, 159(1), 36–42. doi: 10.1016/j.schres.2014.07.030 [DOI] [PubMed] [Google Scholar]
- Schiffer B, Leygraf N, Muller BW, Scherbaum N, Forsting M, Wiltfang J, … Hodgins S (2013). Structural brain alterations associated with schizophrenia preceded by conduct disorder: a common and distinct subtype of schizophrenia? Schizophr Bull, 39(5), 1115–1128. doi: 10.1093/schbul/sbs115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiffer B, Muller BW, Scherbaum N, Forsting M, Wiltfang J, Leygraf N, & Gizewski ER (2010). Impulsivity-related brain volume deficits in schizophrenia-addiction comorbidity. Brain, 133(10), 3093–3103. doi: 10.1093/brain/awq153 [DOI] [PubMed] [Google Scholar]
- Schizophrenia Working Group of the Psychiatric Genomics Consortium. (2014). Biological insights from 108 schizophrenia-associated genetic loci. Nature, 511(7510), 421–427. doi: 10.1038/nature13595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sgouros S, Goldin JH, Hockley AD, Wake MJ, & Natarajan K (1999). Intracranial volume change in childhood. J Neurosurg, 91(4), 610–616. doi: 10.3171/jns.1999.91.4.0610 [DOI] [PubMed] [Google Scholar]
- Shapleske J, Rossell SL, Simmons A, David AS, & Woodruff PW (2001). Are auditory hallucinations the consequence of abnormal cerebral lateralization? A morphometric MRI study of the sylvian fissure and planum temporale. Biol Psychiatry, 49(8), 685–693. doi: 10.1016/S0006-3223(00)01006-4 [DOI] [PubMed] [Google Scholar]
- Shepherd AM, Laurens KR, Matheson SL, Carr VJ, & Green MJ (2012). Systematic meta-review and quality assessment of the structural brain alterations in schizophrenia. Neurosci Biobehav Rev, 36(4), 1342–1356. doi: 10.1016/j.neubiorev.2011.12.015 [DOI] [PubMed] [Google Scholar]
- Sigmundsson T, Suckling J, Maier M, Williams S, Bullmore E, Greenwood K, … Toone B (2001). Structural abnormalities in frontal, temporal, and limbic regions and interconnecting white matter tracts in schizophrenic patients with prominent negative symptoms. Am J Psychiatry, 158(2), 234–243. doi: 10.1176/appi.ajp.158.2.234 [DOI] [PubMed] [Google Scholar]
- Sim K, DeWitt I, Ditman T, Zalesak M, Greenhouse I, Goff D, … Heckers S (2006). Hippocampal and parahippocampal volumes in schizophrenia: a structural MRI study. Schizophr Bull, 32(2), 332–340. doi: 10.1093/schbul/sbj030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith GN, Lang DJ, Kopala LC, Lapointe JS, Falkai P, & Honer WG (2003). Developmental abnormalities of the hippocampus in first-episode schizophrenia. Biol Psychiatry, 53(7), 555–561. doi: 10.1016/s0006-3223(02)01977-7 [DOI] [PubMed] [Google Scholar]
- Smith MJ, Wang L, Cronenwett W, Goldman MB, Mamah D, Barch DM, & Csernansky JG (2011). Alcohol use disorders contribute to hippocampal and subcortical shape differences in schizophrenia. Schizophr Res, 131(1-3), 174–183. doi: 10.1016/j.schres.2011.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ML, & Glass GV (1977). Meta-analysis of psychotherapy outcome studies. Am Psychol, 32(9), 752–760. doi: 10.1037//0003-066X.32.9.752 [DOI] [PubMed] [Google Scholar]
- Spoletini I, Cherubini A, Banfi G, Rubino IA, Peran P, Caltagirone C, & Spalletta G (2011). Hippocampi, thalami, and accumbens microstructural damage in schizophrenia: a volumetry, diffusivity, and neuropsychological study. Schizophr Bull, 37(1), 118–130. doi: 10.1093/schbul/sbp058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sporn AL, Greenstein DK, Gogtay N, Jeffries NO, Lenane M, Gochman P, … Rapoport JL (2003). Progressive brain volume loss during adolescence in childhood-onset schizophrenia. Am J Psychiatry, 160(12), 2181–2189. doi: 10.1176/appi.ajp.l60.12.2181 [DOI] [PubMed] [Google Scholar]
- Staal WG, Hulshoff Pol HE, Schnack HG, Hoogendoorn ML, Jellema K, & Kahn RS (2000). Structural brain abnormalities in patients with schizophrenia and their healthy siblings. Am J Psychiatry, 157(3), 416–421. doi: 10.1176/appi.ajp.157.3.416 [DOI] [PubMed] [Google Scholar]
- Strasser HC, Lilyestrom J, Ashby ER, Honeycutt NA, Schretlen DJ, Pulver AE, … Pearlson GD (2005). Hippocampal and ventricular volumes in psychotic and nonpsychotic bipolar patients compared with schizophrenia patients and community control subjects: a pilot study. Biol Psychiatry, 57(6), 633–639. doi: 10.1016/j.biopsych.2004.12.009 [DOI] [PubMed] [Google Scholar]
- Suga M, Yamasue H, Abe O, Yamasaki S, Yamada H, Inoue H, … Kasai K (2010). Reduced gray matter volume of Brodmann’s Area 45 is associated with severe psychotic symptoms in patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci, 260(6), 465–473. doi: 10.1007/s00406-009-0094-1 [DOI] [PubMed] [Google Scholar]
- Sumich A, Chitnis XA, Fannon DG, O’Ceallaigh S, Doku VC, Falrowicz A, … Sharma T (2002). Temporal lobe abnormalities in first-episode psychosis. Am J Psychiatry, 159(7), 1232–1235. doi: 10.1176/appi.ajp.159.7.1232 [DOI] [PubMed] [Google Scholar]
- Sun J, Maller JJ, Daskalakis ZJ, Furtado CC, & Fitzgerald PB (2009). Morphology of the corpus callosum in treatment-resistant schizophrenia and major depression. Acta Psychiatr Scand, 120(4), 265–273. doi: 10.1111/j.1600-0447.2009.01389.x [DOI] [PubMed] [Google Scholar]
- Suzuki M, Zhou SY, Takahashi T, Hagino H, Kawasaki Y, Niu L, … Kurachi M (2005). Differential contributions of prefrontal and temporolimbic pathology to mechanisms of psychosis. Brain, 128(Pt 9), 2109–2122. doi: 10.1093/brain/awh554 [DOI] [PubMed] [Google Scholar]
- Szendi I, Kiss M, Racsmany M, Boda K, Cimmer C, Voros E, … Janka Z (2006). Correlations between clinical symptoms, working memory functions and structural brain abnormalities in men with schizophrenia. Psychiatry Res, 147(1), 47–55. doi: 10.1016/j.pscychresns.2005.05.014 [DOI] [PubMed] [Google Scholar]
- Szeszko PR, Goldberg E, Gunduz-Bruce H, Ashtari M, Robinson D, Malhotra AK, … Bilder RM (2003). Smaller anterior hippocampal formation volume in antipsychotic-naive patients with first-episode schizophrenia. Am J Psychiatry, 160(12), 2190–2197. doi: 10.1176/appi.ajp.160.12.2190 [DOI] [PubMed] [Google Scholar]
- Takahashi T, Kido M, Nakamura K, Furuichi A, Zhou SY, Kawasaki Y, … Suzuki M (2012). Longitudinal MRI study of the pituitary volume in chronic schizophrenia: a preliminary report. Psychiatry Res, 202(1), 84–87. doi: 10.1016/j.pscychresns.2011.11.008 [DOI] [PubMed] [Google Scholar]
- Takahashi T, Nakamura K, Ikeda E, Furuichi A, Kido M, Nakamura Y, … Suzuki M (2013). Longitudinal MRI study of the midline brain regions in first-episode schizophrenia. Psychiatry Res, 212(2), 150–153. doi: 10.1016/j.pscychresns.2012.12.001 [DOI] [PubMed] [Google Scholar]
- Takahashi T, Suzuki M, Kawasaki Y, Hagino H, Yamashita I, Nohara S, … Kurachi M (2003). Perigenual cingulate gyrus volume in patients with schizophrenia: A magnetic resonance imaging study. Biol Psychiatry, 53(7), 593–600. doi: 10.1016/s0006-3223(02)01483-x [DOI] [PubMed] [Google Scholar]
- Takahashi T, Suzuki M, Velakoulis D, Lorenzetti V, Soulsby B, Zhou SY, … Pantelis C (2009). Increased pituitary volume in schizophrenia spectrum disorders. Schizophr Res, 108(1-3), 114–121. doi: 10.1016/j.schres.2008.12.016 [DOI] [PubMed] [Google Scholar]
- Takahashi T, Suzuki M, Zhou SY, Hagino H, Tanino R, Kawasaki Y, … Kurachi M (2005). Volumetric MRI study of the short and long insular cortices in schizophrenia spectrum disorders. Psychiatry Res, 138(3), 209–220. doi: 10.1016/j.pscychresns.2005.02.004 [DOI] [PubMed] [Google Scholar]
- Takahashi T, Suzuki M, Zhou SY, Tanino R, Hagino H, Kawasaki Y, … Kurachi M (2006). Morphologic alterations of the parcellated superior temporal gyrus in schizophrenia spectrum. Schizophr Res, 83(2-3), 131–143. doi: 10.1016/j.schres.2006.01.016 [DOI] [PubMed] [Google Scholar]
- Takahashi T, Suzuki M, Zhou SY, Tanino R, Hagino H, Niu L, … Kurachi M (2006). Temporal lobe gray matter in schizophrenia spectrum: a volumetric MRI study of the fusiform gyrus, parahippocampal gyrus, and middle and inferior temporal gyri. Schizophr Res, 87(1-3), 116–126. doi: 10.1016/j.schres.2006.04.023 [DOI] [PubMed] [Google Scholar]
- Takahashi T, Wood SJ, Soulsby B, Kawasaki Y, McGorry PD, Suzuki M, … Pantelis C (2009). An MRI study of the superior temporal subregions in first-episode patients with various psychotic disorders. Schizophr Res, 113(2-3), 158–166. doi: 10.1016/j.schres.2009.06.016 [DOI] [PubMed] [Google Scholar]
- Takahashi T, Wood SJ, Soulsby B, Tanino R, Wong MT, McGorry PD, … Pantelis C (2009). Diagnostic specificity of the insular cortex abnormalities in first-episode psychotic disorders. Prog Neuropsychopharmacol Biol Psychiatry, 33(4), 651–657. doi: 10.1016/j.pnpbp.2009.03.005 [DOI] [PubMed] [Google Scholar]
- Takao H, Abe O, Yamasue H, Aoki S, Kasai K, & Ohtomo K (2010). Cerebral asymmetry in patients with schizophrenia: a voxel-based morphometry (VBM) and diffusion tensor imaging (DTI) study. J Magn Reson Imaging, 31(1), 221–226. doi: 10.1002/jmri.22017 [DOI] [PubMed] [Google Scholar]
- Takase K, Tamagaki C, Okugawa G, Nobuhara K, Minami T, Sugimoto T, … Kinoshita T (2004). Reduced white matter volume of the caudate nucleus in patients with schizophrenia. Neuropsychobiology, 50(4), 296–300. doi: 10.1159/000080956 [DOI] [PubMed] [Google Scholar]
- Takayanagi Y, Gerner G, Takayanagi M, Rao V, Vannorsdall TD, Sawa A, … Cascella NG (2013). Hippocampal volume reduction correlates with apathy in traumatic brain injury, but not schizophrenia. J Neuropsychiatry Clin Neurosci, 25(4), 292–301. doi: 10.1176/appi.neuropsych.12040093 [DOI] [PubMed] [Google Scholar]
- Takayanagi Y, Takahashi T, Orikabe L, Masuda N, Mozue Y, Nakamura K, … Suzuki M(2010). Volume reduction and altered sulco-gyral pattern of the orbitofrontal cortex in first-episode schizophrenia. Schizophr Res, 121(1-3), 55–65. doi: 10.1016/j.schres.2010.05.006 [DOI] [PubMed] [Google Scholar]
- Takayanagi Y, Takahashi T, Orikabe L, Mozue Y, Kawasaki Y, Nakamura K, … Suzuki M (2011). Classification of first-episode schizophrenia patients and healthy subjects by automated MRI measures of regional brain volume and cortical thickness. PLoS One, 6(6), e21047. doi: 10.1371/journal.pone.0021047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamagaki C, Sedvall GC, Jonsson EG, Okugawa G, Hall H, Pauli S, & Agartz I (2005). Altered white matter/gray matter proportions in the striatum of patients with schizophrenia: a volumetric MRI study. Am J Psychiatry, 162(12), 2315–2321. doi: 10.1176/appi.ajp.162.12.2315 [DOI] [PubMed] [Google Scholar]
- Tandon R, Nasrallah HA, & Keshavan MS (2009). Schizophrenia, “just the facts” 4. Clinical features and conceptualization. Schizophr Res, 110(1-3), 1–23. doi: 10.1016/j.schres.2009.03.005 [DOI] [PubMed] [Google Scholar]
- Tanskanen P, Haapea M, Veijola J, Miettunen J, Jarvelin MR, Pyhtinen J, … Isohanni M (2009). Volumes of brain, grey and white matter and cerebrospinal fluid in schizophrenia in the Northern Finland 1966 Birth Cohort: an epidemiological approach to analysis. Psychiatry Res, 174(2), 116–120. doi: 10.1016/j.pscychresns.2009.04.009 [DOI] [PubMed] [Google Scholar]
- Tanskanen P, Veijola JM, Piippo UK, Haapea M, Miettunen JA, Pyhtinen J, … Isohanni MK (2005). Hippocampus and amygdala volumes in schizophrenia and other psychoses in the Northern Finland 1966 birth cohort. Schizophr Res, 75(2-3), 283–294. doi: 10.1016/j.schres.2004.09.022 [DOI] [PubMed] [Google Scholar]
- Tauscher-Wisniewski S, Tauscher J, Christensen BK, Mikulis DJ, & Zipursky RB (2005). Volumetric MRI measurement of caudate nuclei in antipsychotic-naive patients suffering from a first episode of psychosis. J Psychiatr Res, 39(4), 365–370. doi: 10.1016/j.jpsychires.2004.10.001 [DOI] [PubMed] [Google Scholar]
- Taylor JL, Blanton RE, Levitt JG, Caplan R, Nobel D, & Toga AW (2005). Superior temporal gyrus differences in childhood-onset schizophrenia. Schizophr Res, 73(2-3), 235–241. doi: 10.1016/j.schres.2004.07.023 [DOI] [PubMed] [Google Scholar]
- Tepest R, Wang L, Miller MI, Falkai P, & Csernansky JG (2003). Hippocampal deformities in the unaffected siblings of schizophrenia subjects. Biol Psychiatry, 54(11), 1234–1240. doi: 10.1016/s0006-3223(03)00702-9 [DOI] [PubMed] [Google Scholar]
- Thoma RJ, Hanlon FM, Petropoulos H, Miller GA, Moses SN, Smith A, … Canive JM (2008). Schizophrenia diagnosis and anterior hippocampal volume make separate contributions to sensory gating. Psychophysiology, 45(6), 926–935. doi: 10.1111/j.1469-8986.2008.00692.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tijms BM, Sprooten E, Job D, Johnstone EC, Owens DG, Willshaw D, … Lawrie SM (2015). Grey matter networks in people at increased familial risk for schizophrenia. Schizophr Res. doi: 10.1016/j.schres.2015.08.025 [DOI] [PubMed] [Google Scholar]
- Tomelleri L, Jogia J, Perlini C, Bellani M, Ferro A, Rambaldelli G, … Neuroimaging Network of the, E. n. i. (2009). Brain structural changes associated with chronicity and antipsychotic treatment in schizophrenia. Eur Neuropsychopharmacol, 19(12), 835–840. doi: 10.1016/j.euroneuro.2009.07.007 [DOI] [PubMed] [Google Scholar]
- Tordesillas-Gutierrez D, Koutsouleris N, Roiz-Santianez R, Meisenzahl E, Ayesa-Arriola R, Marco de Lucas E, … Crespo-Facorro B (2015). Grey matter volume differences in non-affective psychosis and the effects of age of onset on grey matter volumes: A voxelwise study. Schizophr Res, 164(1-3), 74–82. doi: 10.1016/j.schres.2015.01.032 [DOI] [PubMed] [Google Scholar]
- Torrey EF, Bowler MS, Taylor MS, & Gottesman II (1994). Does schizophrenia change the structure of the brain? In Schizophrenia and Manic-Depressive Disorder: The Biological Roots of Mental Illness as Revealed by the Landmark Study of Identical Twins (pp. 102–115). [Google Scholar]
- Ueda K, Fujiwara H, Miyata J, Hirao K, Saze T, Kawada R, … Murai T (2010). Investigating association of brain volumes with intracranial capacity in schizophrenia. Neuroimage, 49(3), 2503–2508. doi: 10.1016/j.neuroimage.2009.09.006 [DOI] [PubMed] [Google Scholar]
- van Erp TG, Greve DN, Rasmussen J, Turner J, Calhoun VD, Young S, … Fbirn. (2014). A multi-scanner study of subcortical brain volume abnormalities in schizophrenia. Psychiatry Res, 222(1-2), 10–16. doi: 10.1016/j.pscychresns.2014.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Erp TG, Saleh PA, Rosso IM, Huttunen M, Lonnqvist J, Pirkola T, … Cannon TD (2002). Contributions of genetic risk and fetal hypoxia to hippocampal volume in patients with schizophrenia or schizoaffective disorder, their unaffected siblings, and healthy unrelated volunteers. Am J Psychiatry, 159(9), 1514–1520. doi: 10.1176/appi.ajp.159.9.1514 [DOI] [PubMed] [Google Scholar]
- van Horn JD, & McManus IC (1992). Ventricular enlargement in schizophrenia. A meta-analysis of studies of the ventricle:brain ratio (VBR). Br J Psychiatry, 160(5), 687–697. doi: 10.1192/bjp.160.5.687 [DOI] [PubMed] [Google Scholar]
- Venkatasubramanian G (2010). Neuroanatomical correlates of psychopathology in antipsychotic-naive schizophrenia. Indian J Psychiatry, 52(1), 28–36. doi: 10.4103/0019-5545.58892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkatasubramanian G, Gangadhar BN, Jayakumar PN, Janakiramaiah N, & Keshavan MS (2003). Striato-cerebellar abnormalities in never-treated schizophrenia: evidence for neurodevelopmental etiopathogenesis. German J Psychiatry, 6, 1–7. [PMC free article] [PubMed] [Google Scholar]
- Venkatasubramanian G, Jayakumar PN, Gangadhar BN, & Keshavan MS (2008b). Neuroanatomical correlates of neurological soft signs in antipsychotic-naive schizophrenia. Psychiatry Res, 164(3), 215–222. doi: 10.1016/j.pscychresns.2007.12.021 [DOI] [PubMed] [Google Scholar]
- Virupaksha HS, Kalmady SV, Shivakumar V, Arasappa R, Venkatasubramanian G, & Gangadhar BN (2012). Volume and asymmetry abnormalities of insula in antipsychotic-naive schizophrenia: a 3-tesla magnetic resonance imaging study. Indian J Psychol Med, 34(2), 133–139. doi: 10.4103/0253-7176.101778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vita A, Dieci M, Silenzi C, Tenconi F, Giobbio GM, & Invernizzi G (2000). Cerebral ventricular enlargement as a generalized feature of schizophrenia: a distribution analysis on 502 subjects. Schizophr Res, 44(1), 25–34. doi:Doi 10.1016/S0920-9964(99)00134-6 [DOI] [PubMed] [Google Scholar]
- Voets NL, Hough MG, Douaud G, Matthews PM, James A, Winmill L, … Smith S (2008). Evidence for abnormalities of cortical development in adolescent-onset schizophrenia. Neuroimage, 43(4), 665–675. doi: 10.1016/j.neuroimage.2008.08.013 [DOI] [PubMed] [Google Scholar]
- Wang L, Hosakere M, Trein JC, Miller A, Ratnanather JT, Barch DM, … Csernansky JG (2007). Abnormalities of cingulate gyrus neuroanatomy in schizophrenia. Schizophr Res, 93(1-3), 66–78. doi: 10.1016/j.schres.2007.02.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Mamah D, Harms MP, Karnik M, Price JL, Gado MH, … Csernansky JG (2008). Progressive deformation of deep brain nuclei and hippocampal-amygdala formation in schizophrenia. Biol Psychiatry, 64(12), 1060–1068. doi: 10.1016/j.biopsych.2008.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson DR, Anderson JM, Bai F, Barrett SL, McGinnity TM, Mulholland CC, … Cooper SJ (2012). A voxel based morphometry study investigating brain structural changes in first episode psychosis. Behav Brain Res, 227(1), 91–99. doi: 10.1016/j.bbr.2011.10.034 [DOI] [PubMed] [Google Scholar]
- Watson DR, Bai F, Barrett SL, Turkington A, Rushe TM, Mulholland CC, & Cooper SJ (2012). Structural changes in the hippocampus and amygdala at first episode of psychosis. Brain Imaging Behav, 6(1), 49–60. doi: 10.1007/s11682-011-9141-4 [DOI] [PubMed] [Google Scholar]
- Weinberger DR, Egan MF, Bertolino A, Callicott JH, Mattay VS, Lipska BK, … Goldberg TE (2001). Prefrontal neurons and the genetics of schizophrenia. Biol Psychiatry, 56(11), 825–844. doi: 10.1016/S0006-3223(01)01252-5 [DOI] [PubMed] [Google Scholar]
- Weinberger DR, & Radulescu E (2016). Finding the elusive psychiatric “lesion” with 21st-century neuroanatomy: A note of caution. Am J Psychiatry, 173(1), 27–33. doi: 10.1176/appi.ajp.2015.15060753 [DOI] [PubMed] [Google Scholar]
- Weiss AP, Dewitt I, Goff D, Ditman T, & Heckers S (2005). Anterior and posterior hippocampal volumes in schizophrenia. Schizophr Res, 73(1), 103–112. doi: 10.1016/j.schres.2004.05.018 [DOI] [PubMed] [Google Scholar]
- Wible CG, Anderson J, Shenton ME, Kricun A, Hirayasu Y, Tanaka S, … McCarley RW (2001). Prefrontal cortex, negative symptoms, and schizophrenia: an MRI study. Psychiatry Res, 108(2), 65–78. doi: 10.1016/s0925-4927(01)00109-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams LM, Whitford TJ, Gordon E, Gomes L, Brown KJ, & Harris AW (2009). Neural synchrony in patients with a first episode of schizophrenia: Tracking relations with grey matter and symptom profile. J Psychiatry Neurosci, 34(1), 21–29. [PMC free article] [PubMed] [Google Scholar]
- Witthaus H, Mendes U, Brune M, Ozgurdal S, Bohner G, Gudlowski Y, … Juckel G (2010). Hippocampal subdivision and amygdalar volumes in patients in an at-risk mental state for schizophrenia. J Psychiatry Neurosci, 35(1), 33–40. doi: 10.1503/jpn.090013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Womer FY, Wang L, Alpert KI, Smith MJ, Csernansky JG, Barch DM, & Mamah D (2014). Basal ganglia and thalamic morphology in schizophrenia and bipolar disorder. Psychiatry Res, 223(2), 75–83. doi: 10.1016/j.pscychresns.2014.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (1978). International classification of diseases:[9th] ninth revision, basic tabulation list with alphabetic index.
- World Health Organization. (1992). The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines: Geneva: World Health Organization. [Google Scholar]
- Wright IC, Rabe-Hesketh S, Woodruff PW, David AS, Murray RM, & Bullmore ET (2000). Meta-analysis of regional brain volumes in schizophrenia. Am J Psychiatry, 157(1), 16–25. doi: 10.1176/ajp.l57.1.16 [DOI] [PubMed] [Google Scholar]
- Yamasaki S, Yamasue H, Abe O, Yamada H, Iwanami A, Hirayasu Y, … Kasai K (2007). Reduced planum temporale volume and delusional behaviour in patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci, 257(6), 318–324. doi: 10.1007/s00406-007-0723-5 [DOI] [PubMed] [Google Scholar]
- Yamasue H, Iwanami A, Hirayasu Y, Yamada H, Abe O, Kuroki N, … Kasai K (2004). Localized volume reduction in prefrontal, temporolimbic, and paralimbic regions in schizophrenia: an MRI parcellation study. Psychiatry Res, 131(3), 195–207. doi: 10.1016/j.pscychresns.2004.05.004 [DOI] [PubMed] [Google Scholar]
- Yamasue H, Yamada H, Yumoto M, Kamio S, Kudo N, Uetsuki M, … Kasai K (2004). Abnormal association between reduced magnetic mismatch field to speech sounds and smaller left planum temporale volume in schizophrenia. Neuroimage, 22(2), 720–727. doi: 10.1016/j.neuroimage.2004.01.042 [DOI] [PubMed] [Google Scholar]
- Yang Y, Nuechterlein KH, Phillips OR, Gutman B, Kurth F, Dinov I, … Narr KL (2012). Disease and genetic contributions toward local tissue volume disturbances in schizophrenia: a tensor-based morphometry study. Hum Brain Mapp, 33(9), 2081–2091. doi: 10.1002/hbm.21349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo RA, Gangestad SW, Liu J, Ehrlich S, Thoma RJ, Pommy J, … Calhoun VD (2013). The impact of copy number deletions on general cognitive ability and ventricle size in patients with schizophrenia and healthy control subjects. Biol Psychiatry, 73(6), 540–545. doi: 10.1016/j.biopsych.2012.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon U, Lee JM, Koo BB, Shin YW, Lee KJ, Kim IY, … Kim SI (2005). Quantitative analysis of group-specific brain tissue probability map for schizophrenic patients. Neuroimage, 26(2), 502–512. doi: 10.1016/j.neuroimage.2005.01.056 [DOI] [PubMed] [Google Scholar]
- Yoshida T, McCarley RW, Nakamura M, Lee K, Koo MS, Bouix S, … Niznikiewicz MA (2009). A prospective longitudinal volumetric MRI study of superior temporal gyrus gray matter and amygdala-hippocampal complex in chronic schizophrenia. Schizophr Res, 113(1), 84–94. doi: 10.1016/j.schres.2009.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshihara Y, Sugihara G, Matsumoto H, Suckling J, Nishimura K, Toyoda T, … Takei N (2008). Voxel-based structural magnetic resonance imaging (MRI) study of patients with early onset schizophrenia. Ann Gen Psychiatry, 7, 25. doi: 10.1186/1744-859X-7-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yotsutsuji T, Saitoh O, Suzuki M, Hagino H, Mori K, Takahashi T, … Kurachi M (2003). Quantification of lateral ventricular subdivisions in schizophrenia by high-resolution three-dimensional magnetic resonance imaging. Psychiatry Res, 122(1), 1–12. doi: 10.1016/S0925-4927(02)00105-1 [DOI] [PubMed] [Google Scholar]
- Zetzsche T, Preuss U, Frodl T, Watz D, Schmitt G, Koutsouleris N, … Meisenzahl EM (2007). In-vivo topography of structural alterations of the anterior cingulate in patients with schizophrenia: new findings and comparison with the literature. Schizophr Res, 96(1-3), 34–45. doi: 10.1016/j.schres.2007.07.027 [DOI] [PubMed] [Google Scholar]
- Zhou SY, Suzuki M, Hagino H, Takahashi T, Kawasaki Y, Matsui M, … Kurachi M (2005). Volumetric analysis of sulci/gyri-defined in vivo frontal lobe regions in schizophrenia: Precentral gyrus, cingulate gyrus, and prefrontal region. Psychiatry Res, 139(2), 127–139. doi: 10.1016/j.pscychresns.2005.05.005 [DOI] [PubMed] [Google Scholar]
- Zhou SY, Suzuki M, Hagino H, Takahashi T, Kawasaki Y, Nohara S, … Kurachi M (2003). Decreased volume and increased asymmetry of the anterior limb of the internal capsule in patients with schizophrenia. Biol Psychiatry, 54(4), 427–436. doi: 10.1016/s0006-3223(03)00007-6 [DOI] [PubMed] [Google Scholar]
- Zuffante P, Leonard CM, Kuldau JM, Bauer RM, Doty EG, & Bilder RM (2001). Working memory deficits in schizophrenia are not necessarily specific or associated with MRI-based estimates of area 46 volumes. Psychiatry Res, 108(3), 187–209. doi: 10.1016/s0925-4927(01)00124-x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


