Abstract
Objective:
Troponin-I (TN-I) levels are elevated following pediatric cardiac surgery with speculation that particular patterns may have prognostic significance. There is lack of procedure-specific data regarding postoperative TN-I levels in infants undergoing cardiac surgery. We hypothesized that TN-I elevation varies with type of surgery and persistent elevation predicts poor prognosis.
Methods:
We prospectively measured serial TN-I levels (preoperatively, 4, 8, 12, 24, and 48 hours postoperatively) in 90 infants (age < 1 year) undergoing cardiac surgery: off cardiopulmonary bypass (CPB) (n = 15), on CPB (n = 43), and on CPB with ventricular incision (CPB with ventricular incision) (n = 32).
Results:
All patients had undetectable baseline TN-I levels. The area under the curve (AUC) of TN-I levels over the 48-hour period was significantly different among the surgical groups (p < 0.002), and highest in patients with CPB with ventricular incision. Generally, TN-I levels peaked by 4 hours after surgery and returned to near-normal levels within 48 hours. A persistent TN-I rise beyond 8 hours after surgery was a strong predictor of postoperative hypoperfusion injury (defined as a composite endpoint of end-organ injury resulting from inadequate perfusion, OR 21.5; p = 0.001) and mortality (30% in those with persistently high TN-I, compared with 3.5% in the remaining patients; p < 0.001), independent of patient age, anatomy/complexity of surgery, and level of postoperative support.
Conclusions:
Our data provide benchmark values for TN-I levels following cardiac surgery in infants. Extent of TN-I elevation correlates with type of surgery. Persistent TN-I elevation beyond 8 hours after surgery is strongly associated with postoperative hypoperfusion injury and mortality.
Introduction:
In the adult population, Troponin levels measured in the blood serum have long been recognized as a marker of myocardial injury. Elevated levels of Troponin-I (TN-I) have been shown to have prognostic value in prediction of morbidity and mortality in critically ill adults, even without previously recognized cardiac symptoms.1 Furthermore, TN-I levels have been validated and are widely used in adult cardiology for non-invasive assessment and screening of perioperative myocardial infarctions.2
Compared to adult hearts, pediatric hearts appear to be more vulnerable to perioperative myocardial damage from ischemia and reperfusion injury.3 In particular, children less than 12 months of age are at highest risk of myocardial injury following cardiac surgery.4 Due to the multitude of factors that can affect clinical status during recovery following congenital heart surgery, evaluation of ongoing myocardial damage is often difficult in the immediate postoperative period. There is currently no standard biochemical marker of myocardial injury after pediatric cardiac surgery.
Previous studies have indicated that serum TN-I levels increase in children after cardiac surgery and can reflect myocardial damage.5–7 It has been speculated that particular patterns of elevation may have prognostic significance.8–11 However, there is lack of procedure-specific data regarding postoperative TN-I levels in infants undergoing cardiac surgery. The aims of this study were: (1) to establish trends in values of postoperative TN-I in infants based on type of cardiac surgery, (2) to identify perioperative factors associated with persistent TN-I elevation, and (3) to evaluate the prognostic value of TN-I with respect to postoperative morbidity and mortality.
Methods
Patients
The Institutional Review Board at Children’s Hospital of Los Angeles (CHLA) approved this study and informed consent was obtained from all patient surrogates. Ninety infants under 12 months of age with a diagnosis of congenital heart disease scheduled to undergo cardiac surgery at CHLA were prospectively enrolled between September 2013 and January 2015. Patients were divided into three groups based on their type of surgery: without cardiopulmonary bypass (off CPB), on bypass (CPB), and on CPB with ventricular incision (defined as need to perform ventriculotomy and resect muscle). Demographic and preoperative clinical information such as patient gender, gestational age, age at surgery, ethnicity, body surface area, primary cardiac diagnosis, presence of associated syndromes, prior cardiac surgeries, history of cardiopulmonary resuscitation, and preoperative cardiac function by echocardiogram were obtained. Additionally, the following postoperative variables were obtained for correlation with TN-I trends: duration of intubation, postoperative cardiac function by echocardiogram, vasoactive inotrope score (VIS) at time of TN-I sample collection, postoperative hypoperfusion injury (used to indicate a composite outcome of end-organ injury resulting from inadequate perfusion and included necrotizing enterocolitis (NEC), neurological injury, renal failure, and pancreatitis), other postoperative complications, need for mechanical circulatory support with extracorporeal membrane oxygenation (ECMO), length of stay in the cardiothoracic intensive care unit (CTICU), length of hospital stay.12
Surgery
In patients who underwent CPB, diastolic arrest was achieved using del Nido cardioplegia solution. Moderate systemic hypothermia (24–32C) was used routinely except for cases of deep hypothermic circulatory arrest (DHCA). Surgical details such as Society of Thoracic Surgeons-European Association for Cardio-Thoracic Surgery (STAT) mortality score, STAT category, duration of CPB, aortic cross-clamping time, need for and duration of DHCA, as well as presence of intraoperative complications were collected.
Sample collection
Blood samples were obtained preoperatively and at 4, 8, 12, 24, and 48 hours postoperatively. All samples were processed within one hour of collection. TN-I levels were measured via fluorescence immunoassay, processed by the CHLA chemistry laboratory. Laboratory personnel performing the assay were blinded to the clinical status of the patients. Of the 450 time points of planned troponin measurement, 436 (97%) measurements were completed and available for analysis. The 14 time points (3%) with missing values were omitted from the trend analyses. Results of laboratory studies drawn concurrently, such as complete metabolic panel, complete blood count, serum lactate and arterial blood gas were also collected.
Statistical analysis
Data were tabulated and analyzed using SAS 9.4. Trends in individual troponin levels were analyzed using mixed linear models and presented as smoothing splines. Area under the curve (AUC), representative of the total release of postoperative TN-I in a 48-hour period, was calculated. Receiver operator characteristic (ROC) curves were constructed to identify cutoff points by Youden’s J statistic analyses to best predict inflection values of TN-I at the various time points (Supplemental Figure 1). Continuous variables are expressed as mean values ± standard deviation. ANOVA was used to compare multiple groups and post-hoc Tukey’s test to determine individual comparisons of significance. Univariate and multiple regression analyses were used to evaluate factors predicting outcomes. Differences were considered statistically significant at p values less than 0.05.
Results
Patients
Of the ninety infants enrolled in the study, mean age was 3.5 months (range 3 days to 12 months), and 48 (53%) were male. Patient demographic and surgical data are provided in Table 1. Fifteen patients underwent surgery off CPB, 43 patients underwent surgery on CPB but did not need a ventricular incision, and 32 patients required surgery on CPB with ventricular incision. Patients who underwent surgery off CPB were significantly younger and, therefore, smaller than the other two groups (Table 1).
Table 1.
Patient demographic and surgical data
| Off CPB (15) | On CPB (43) | CPB with ventricular incision (32) | ||
|---|---|---|---|---|
| Mean ± SD Frequency (%) | Mean ± SD Frequency (%) | Mean ± SD Frequency (%) | P-value | |
| Demographics | ||||
| Male | 9 (60%) | 23 (52%) | 16 (52%) | 0.6 |
| Age at surgery (months) | 1.7±1.5 | 4.2±3.4 | 4.1±4.5 | 0.03* |
| BSA | 0.2±0.1 | 0.3±0.1 | 0.3±0.1 | 0.02* |
| Single ventricle physiology | 7 (47%) | 10 (23%) | 12 (39%) | 0.03† |
| physiology | ||||
| Surgical data | ||||
| CPB time (min) | 0 | 66.4±28.7 | 76.7±34.9 | 0.14 |
| Required DHCA | 0 | 7 (16%) | 13 (42%) | 0.01‡ |
Significant difference between Off CPB group and other groups;
Significant difference between Off CPB and On CPB groups;
Significant difference between On CPB group and CPB with ventricular incision group. BSA, body surface area; CPB, cardiopulmonary bypass; DHCA, deep hypothermic circulatory arrest; SD, standard deviation.
Perioperative Details
There was no significant difference in preoperative renal, neurologic or gastrointestinal function among the three surgical groups. The primary surgical procedure performed in each of the three groups is depicted in Figure 1. There were 16 STAT 1, 21 STAT 2, 11 STAT 3, 30 STAT 4 and 12 STAT 5 procedures. The average CPB time for patients with CPB with ventricular incision was 76.7 minutes, compared with 66.4 minutes in those who did not require ventricular incision (p = 0.14). Patients who underwent procedures off CPB required longer intubation times (p = 0.04) and experienced more hypoperfusion injuries (p = 0.02). Patients who underwent procedures on CPB, on the other hand, fared better with shorter length of stay in CTICU and improved overall survival compared with the other surgical groups (p = 0.03) (Table 2).
Figure 1.
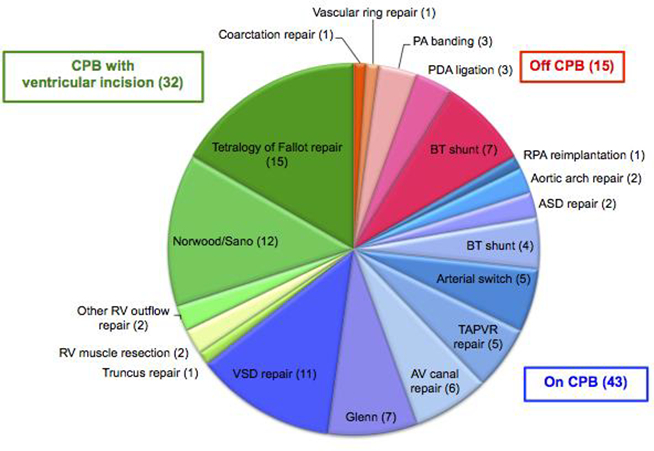
Primary surgical procedures performed among 3 surgical groups. Patients were divided into three groups based on type of surgery: without cardiopulmonary bypass (off CPB) (red hues, n = 15), on bypass (CPB) (blue hues, n = 43), and on bypass with ventricular incision (CPB with ventricular incision) (green hues, n = 32). Primary surgical procedures performed among each group are listed. ASD = atrial septal defect, AV = atrioventricular, BT = Blalock-Taussig, CPB = cardiopulmonary bypass, PA = pulmonary artery, PDA = patent ductus arteriosus, RPA = right pulmonary artery, RV = right ventricle, TAPVR = total anomalous pulmonary venous return, VSD = ventricular septal defect
Table 2.
Patient postoperative data
| Off CPB | On CPB | CPB with ventricular incision | ||
|---|---|---|---|---|
| Mean ± SD Frequency (%) | Mean ± SD Frequency (%) | Mean ± SD Frequency (%) | P-value | |
| Postoperative course | ||||
| Peak lactate level (mg/dl) | 18.3±9.1 | 29.1±19.1 | 35.5±25.5 | 0.12 |
| Peak VIS | 9.9±8.1 | 13.1±6.4 | 15±4.3 | 0.03* |
| Length of intubation (days) | 8.9±10.6 | 3.8±5.4 | 4.7±5.6 | 0.04* |
| ECMO requirement | 1 (7%) | 0 (0%) | 2 (6%) | 0.4 |
| Hypoperfusion injury CTICU (days) | 4 (27%) | 3 (7%) | 4 (13%) | 0.02† |
| Discharge from | 6±4.1 | 5.2±4.8 | 7.4±6.1 | 0.03§ |
| Died | 2 (13%) | 0 (0%) | 4 (13%) | 0.03‡ |
Significant difference between Off CPB group and other groups;
Significant difference between Off CPB and On CPB groups;
Significant difference between On CPB group and CPB with ventricular incision group;
Significant difference between On CPB group and other groups. CPB, cardiopulmonary bypass; CTICU, cardiothoracic intensive care unit; ECMO, extracorporeal membrane oxygenation; SD, standard deviation. CPB, cardiopulmonary bypass; TN-I, Troponin-I.
Surgery and TN-I trends
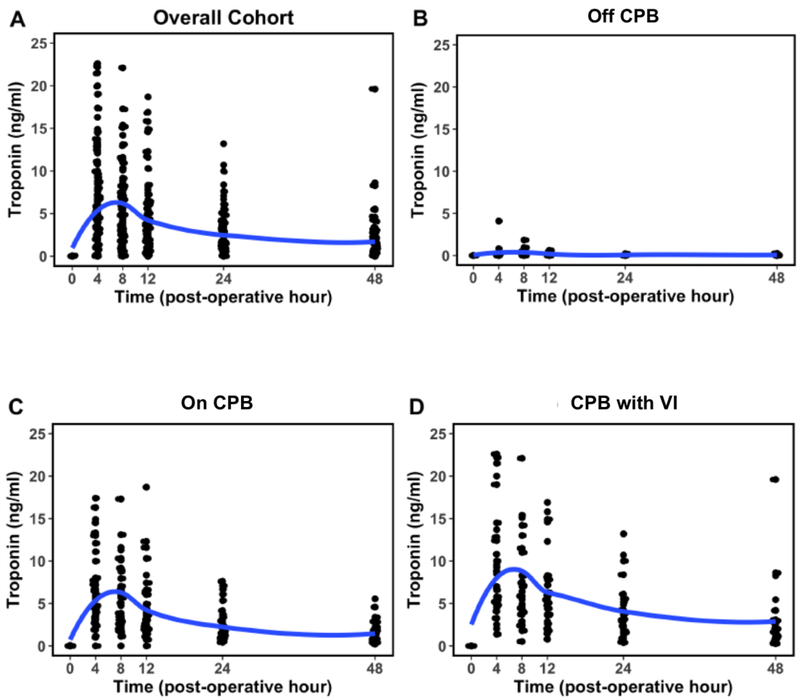
All preoperative TN-I concentrations were within normal limits, less than 0.07 ng/mL. In the majority of patients, postoperative TN-I levels peaked by 4 hours after surgery and returned to near-normal levels by 48 hours (Figure 2, Table 3). Specifically, 56 (62%) patients experienced measured peak TN-I levels at 4 hours after surgery, 17 (19%) had TN-I peak levels at 8 hours, and 13 (14%) experienced continued rise of TN-I beyond 8 hours surgery. Four (4%) patients experienced no TN-I leak.
Figure 2.
Postoperative TN-I trends among different surgical groups Measured troponin levels over a 48-hour postoperative period is shown for the entire cohort (A) and for the three subgroups (B-D) as smoothed splines of individual values. Troponin was lowest in the Off cardiopulmonary bypass (CPB) group, and highest in the CPB with ventricular incision (VI) group.
Table 3.
Trends in values of postoperative TN-I values based on type of surgery
| Surgical group | Postoperative hour | Mean TN-I(ng/mL) | Median TN-I(ng/mL) | TN-I Range(ng/mL) | Standard Deviation |
|---|---|---|---|---|---|
| Off CPB (n=10) | 0 | 0 | 0 | 0 – 0 | 0 |
| 4 | 0.16 | 0.07 | 0 – 0.82 | 0.25 | |
| 8 | 0.23 | 0.1 | 0 – 0.95 | 0.32 | |
| 12 | 0.15 | 0.085 | 0 – 0.61 | 0.19 | |
| 24 | 0.06 | 0.055 | 0 – 0.16 | 0.06 | |
| 48 | 0.06 | 0.025 | 0 – 0.19 | 0.06 | |
| CPB (n=42) | 0 | 0 | 0 | 0 – 0 | 0 |
| 4 | 5.9 | 4.7 | 0 – 16.3 | 3.95 | |
| 8 | 4.9 | 3.6 | 0 – 11.6 | 3.05 | |
| 12 | 3.7 | 2.82 | 0 – 12.3 | 2.72 | |
| 24 | 2.0 | 1.36 | 0.42 – 7.1 | 1.56 | |
| 48 | 1.3 | 0.84 | 0.22 – 5.55 | 1.1 | |
| CPB with ventricular incision (n=25) | 0 | 0 | 0 | 0– 0 | 0 |
| 4 | 10 | 9.03 | 1.37 – 26 | 6.95 | |
| 8 | 7.3 | 6.4 | 0.52 – 22.1 | 5 | |
| 12 | 5.7 | 5.05 | 0.79 – 15.8 | 4 | |
| 24 | 4 | 3.435 | 0.39 – 13.2 | 3.1 | |
| 48 | 2.2 | 1.72 | 0.27 – 8.27 | 1.85 | |
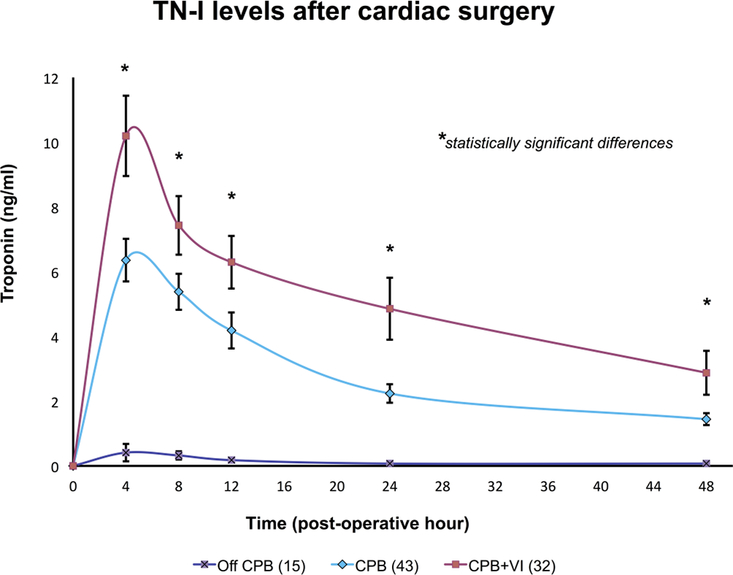
The AUC of TN-I levels over the 48-hour period was significantly different among the three surgical groups, with minimal elevation detected in patients who underwent surgery off CPB, and the highest rise in patients with CPB with ventricular incision (p < 0.002) (Figure 3). The AUC of TN-I also increased with longer CPB time (r2 = 0.28, p < 0.0001). Interestingly, for those who underwent DHCA, a negative correlation was observed between postoperative TN-I AUC and DHCA time (r2 = 0.43, p < 0.002). There was no correlation between STAT category and peak TN-1 levels (p=0.48) or TN-I AUC (p=0.39).
Figure 3.
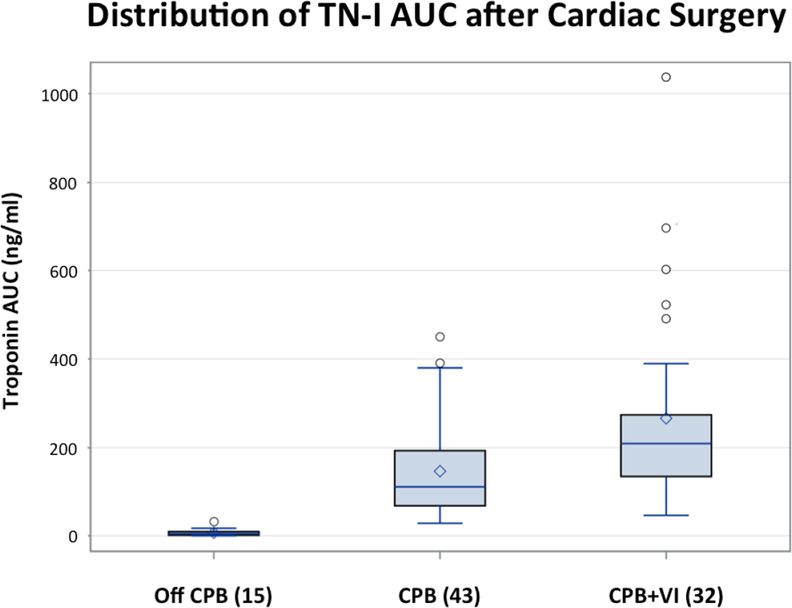
Postoperative TN-I AUC among different surgical groups The area under the curve (AUC) of TN-I levels over a 48-hour postoperative period was significantly different among the three surgical groups. The AUC was lowest in the Off CPB group, and highest in the CPB with ventricular incision group. Other abbreviations as in Figure 1.
TN-I trends and clinical outcomes
Whereas we observed a general trend in individual TN-I levels at the different timepoints (Table 3, Figure 2), there was significant overlap between the TN-I levels at different time-points between different patients in the various groups. Consequently, the peak TN-I level or the actual value of TN-I at any single time point did not correlate with the outcomes evaluated. However, among the three surgical groups, a higher AUC of TN-I correlated with prolonged CTICU stay (p = 0.006) and increased mortality (p < 0.0001). We believe that because AUC is retrospectively calculated over a 48-hour time-period, its clinical use as a predictor of outcomes is limited.
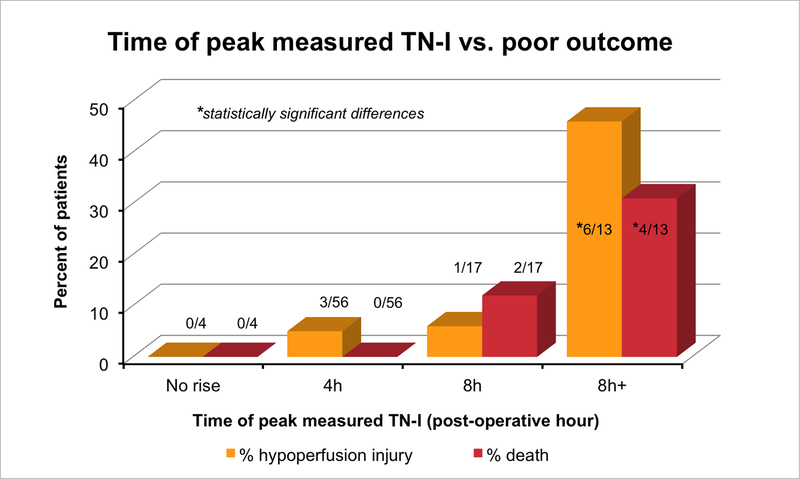
We found that the timing of TN-I peak was clinically significant. With intent to identify a clinically relevant prospective tool, we therefore further pursued the significance of persistent elevation of TN-I at 8h after surgery in our subsequent analyses. Whereas 93% of patients had detectable TN-I levels 8h post-operatively, only 13 patients continued to experience persistent TN-I rise beyond 8h after surgery. Of these 13 patients, 6 (46%) had postoperative hypoperfusion injuries (Figure 4) – NEC in 3 (23%), neurological insult in 2 (15%), renal failure requiring peritoneal dialysis in 2 (15%), and pancreatitis in 1 (8%). Such organ-specific hypoperfusion injuries occurred in only 5% of the remaining cohort who experienced typical postoperative TN-I decline pattern (p < 0.001). To assess the usefulness of absolute TN-I values at various time-points in predicting hypoperfusion injuries, we generated individual ROC curves of TN-I levels at the different time-points (Supp Fig 1). There was no significant TN-I cut-off value that predicted hypoperfusion injury at any of the time-points analyzed. A troponin level of 8.44 at 12h was the only value that had a trend towards significance (p=0.1, AUC 0.53).
Figure 4.
Distribution of negative outcomes based on peak measured TN-I. A persistent TN-I rise beyond 8 hours after surgery is significantly associated with postoperative hypoperfusion injury and mortality, independent of patient age, ventricular anatomy, complexity of surgery, and level of postoperative support. Examples of hypoperfusion injuries include necrotizing enterocolitis (NEC), neurological injury, renal failure, and pancreatitis. Abbreviations as in Figure 2.
Overall, mortality was 30% in patients who had persistent TN-I elevation beyond 8h after surgery, compared with only 3.5% in the remaining patients (p < 0.001). Persistent TN-I elevation beyond 8 hours also correlated with higher postoperative creatinine level (p = 0.03), longer intubation time (p < 0.0001), and increased length of CTICU stay (p < 0.0001). There was no correlation, however, between persistent TN-I elevation beyond 8 hours and need for ECMO support (p=0.1), and we did not find correlation between TN-I trend and other markers of hemodynamic assessment such as lactate levels, VIS, or ventricular function measured by echocardiogram. Because DHCA had a negative association with troponin levels, we evaluated DHCA patients as a separate sub-group. Of the 20 DHCA patients, 4 (20%) had persistent TN-I elevation beyond 8h. One of these 4 patients had hypoperfusion injury and one died. There was no significant difference in the outcomes of patients with and without persistent troponin elevation within the DHCA sub-group, likely due to small number of events. In addition, no association was observed when the analysis was performed with the three surgical groups considered separately, or when patients were classified based on single or two-ventricle anatomy in any of the surgical groups. Given the particular heterogeneity in the off CPB group, we further analyzed these patients based on single- (n=7) vs. two-ventricle (n=8) physiology. The only significant differences in TN-I levels were at 12h (0.3 + 0.2 vs. 0.1 + 0.1ng/ml, p = 0.04) and 48h (0.1 + 0.1 vs. 0.03 + 0.05 ng/ml, p = 0.03). There was one death in each of the sub-groups (p=0.8) and 3 of the 4 hypoperfusion injuries were seen in the single ventricle group (43% vs. 13%, p=0.2). Two patients with single-ventricle physiology (29%) had persistent elevation of TN-I beyond 8 hours after surgery compared to none in the two-ventricle group (p=0.2). None of the correlations was statistically significant, again likely due to small numbers. After adjusting in a multiple regression analysis for gestational age, age at surgery, ventricular anatomy, STAT category, duration of bypass and level of postoperative support required, persistent elevation of TN-I beyond 8 hours after surgery was strongly and independently predictive of hypoperfusion injury (OR 12.1 (2.2–67.4), p=0.005) and death (OR 16, CI 1.8–84.6; p=0.006) among the entire cohort of infants undergoing congenital heart surgery.
Discussion
Pediatric patients with congenital heart disease comprise a particularly vulnerable surgical population. They often require immediate medical attention in the neonatal period for clinical stabilization prior to surgical correction or palliation. In particular, congenital heart defects that result in ventricular pressure- and volume-overload may result in abnormal cardiac function or myocardial derangement even before surgery. Patients with such conditions may be particularly susceptible to sustained myocardial injury from ischemia, direct surgical manipulation, and postoperative reperfusion.
In the past decade, many biomarkers have been studied in both the adult and pediatric cardiac population for potential use in surgical prognostication.13–15 Post-surgical cardiac function in the congenital heart patient, however, is often difficult to objectively assess, hence making evaluation of potential biomarkers particularly challenging in this population, and more relevant. Congenital defects resulting in single ventricle physiology, ventricular hypertrophy, dilation, or abnormal postoperative septal motion also hamper accurate assessment of cardiac function by routine imaging modalities such as echocardiography. Thus, in patients with congenital heart disease, identification of a postoperative biomarker that may consistently predict outcome is a challenging but particularly valuable venture. Standardization of such a biomarker for specific types of cardiac surgeries is an important consideration.
Troponin-I is a protein specific to the myocardium as part of the tropomyosin complex. It has previously been shown to be a promising biomarker in assessment of myocardial damage in children and infants, with virtually no cross-reactivity with skeletal muscle.4, 6, 8, 9 Unlike Troponin-T (TN-T), TN-I does not appear to be significantly affected by renal function, and is thus ideal for assessment of myocardial damage particularly post-cardiac surgery when cardiopulmonary bypass and hemodynamic fluctuations may transiently affect end-organ function.6 In comparison with proteins such as TN-T, CK-MB, and BNP, TN-I is has improved specificity for myocardial damage, it rises and normalizes quickly after surgery, and has a relatively narrow normal range.16, 17
Previous studies have indicated that infants tend to have higher troponin leak following myocardial damage when compared with older children, and for this reason we narrowed the scope of our cohort to infants younger than 1 year of age.18 The two major intraoperative factors that correlated with increased postoperative TN-I levels were: (1) the use and duration of CPB, and (2) the requirement of ventricular incision during surgery (Figure 2). Under ideal circumstances, one would like to establish expected range of post-operative, time-varying troponin levels for every specific procedure. Such an exercise would require prospective evaluation of a large number of patients standardized based on underlying diagnosis and/or primary procedure. We view our study more as hypothesis-generating and as a proof-of-concept that troponin levels may have value broadly as a biomarker in all congenital heart surgical patients, not just in an intuitive subset such as those undergoing coronary manipulation during an arterial switch operation, for example. To that end, we prospectively enrolled all patients undergoing cardiac surgery and arbitrarily divided them into three surgical groups (off CPB, on CPB, and on CPB with ventricular incision). We acknowledge that this stratification artificially groups patients with widely different physiologies into the same category. We pursued multiple sub-group analyses in an attempt to account for this heterogeneity. First, we evaluated the effects of surgical complexity, and found that STAT score or category of the surgical procedure did not correlate with peak troponin levels, troponin AUC, individual troponin levels at any of the time points or with persistent troponin elevation beyond 8h. STAT category was also not associated with hypoperfusion state. We then categorized patients in the off-CPB group, the group with greatest heterogeneity, into single and two-ventricle patients. This analysis showed, as expected, that single ventricle patients had a trend towards greater troponin elevation. However, the predictive effect of troponin persisted after accounting for underlying ventricular anatomy. Lastly, we analyzed patients with DHCA separately, given that we found a negative correlation between use of DHCA and extent of postoperative TN-I rise. Specifically, there were 20 patients in our cohort who required DHCA as part of their surgery (5 repairs of total anomalous pulmonary venous connection, 3 aortic arch reconstructions, and 12 Norwood/Sano). While our study cannot definitively address the reasons for this finding, we speculate that the deep hypothermia may have myocardial protective effects. Future studies will be required to specifically address some of these findings and to further evaluate focused sub-groups of patients.
There have been conflicting reports of whether peak TN-I levels are associated with poor surgical outcomes.9, 18, 19 Our study did not reveal significant correlation between peak TN-I level and outcomes. In addition, individual TN-I levels varied widely at each time point even within the individual surgical groups, such that no particular TN-I level could be reliably used to predict poor clinical outcome. Despite this variability in absolute levels, we found that measured TN-I levels generally peaked at 4 hours after surgery and tapered slowly thereafter. This is consistent with previous reports and indicates that troponin leak from myocardium following cardiac surgery does not typically persist longer than this period.4, 7 In fact, we found that persistent TN-I elevation beyond 8 hours after surgery is strongly and independently predictive of impending hypoperfusion injury and death (Figure 4). We interpret the persistent elevation in TN-I as a marker for persistent myocardial damage and, consequently, myocardial dysfunction. We speculate that such an altered hemodynamic state predisposes the child to end-organ hypoperfusion sequelae such as NEC and neurologic injury. Another possibility is that TN-I elevation is a marker of overall clinical instability, independent of myocardial dysfunction, such that patients with higher TN-I levels were more critically ill and had systemic hypoperfusion. These results need to be interpreted with the limitation that in this study, post-operative monitoring was carried out according to routine clinical practices and not specifically protocolized.
The patients who underwent surgery off CPB comprise a particularly high-risk population. These patients required a longer postoperative intubation time (p=0.04) and experienced more hypoperfusion injuries (p=0.02) than the rest of our cohort (Table 2). They were also were significantly younger (1.7 months, compared with 4.2 months in the other two groups; p=0.03), and truly represented a neonatal (rather than infant) surgical population (Table 1). The relatively high morbidity and mortality in the off CPB group is likely a reflection of the particularly fragile physiology of the young patients in this group. After accounting for these known confounders, continued TN-I elevation beyond 8h still predicted poor outcomes.
Our findings provide early convincing evidence that there is value to following trends in TN-I levels following cardiac surgery. No one measure, clinical or biochemical, can in isolation determine the approach to care for a post-operative pediatric cardiac patient. That said, TN-I levels serve as another valuable tool in the armamentarium of the treating clinician. We believe that the most beneficial application of TN-I levels would be to guide clinical therapy in a patient who does not demonstrate expected postoperative recovery, or to tilt the balance in a patient with otherwise incongruent clinical and/or biochemical parameters. Our goal was to identify the most impactful way to prospectively utilize TN-I levels in clinical care. Whereas TN-I AUC correlated with adverse outcomes, this would only be relevant after all measurements became available, in our case 48h post-op, thereby limiting its utility. As a more immediate measure, we show that identification of persistent TN-I elevation beyond 8 hours after surgery predicts higher likelihood of organ-specific hypoperfusion injury and death. This would suggest that the addition of 8 and 12h measures of TN-I, at bare minimum, can be used effectively along with other traditional parameters to identify the patient at increased risk for postoperative morbidity and mortality. Such information would guide clinical care, such as more judicious weaning of cardiac and/or respiratory support and an aggressive search for organ-specific hypoperfusion. Future studies will need to address whether clinical intervention to augment cardiac support in children with persistent TN-I elevation can prevent or reverse these hypoperfusion injuries.
Conclusions
In infants undergoing cardiac surgery, higher postoperative TN-I levels correlate with surgical complexity. Typically, TN-I levels peak at 4 hours after surgery and taper slowly thereafter. Persistent TN-I elevation beyond 8 hours after surgery is strongly predictive of hypoperfusion injury and death, regardless of patient age, ventricular anatomy, or type of cardiac surgery. Thus, for patients noted to have this pattern of persistent elevation, closer clinical monitoring for systemic hypoperfusion is strongly advised, as well as perhaps appropriate modifications in management strategies.
In conclusion, TN-I trends have important value in postoperative prognostication. Our data provide trends in values for TN-I levels following different types of cardiac surgery in infants, as well as their utility in identifying patients at particular risk for postoperative morbidity and mortality.
Supplementary Material
Central Picture.
Distribution of negative outcomes based on peak measured TN-I after cardiac surgery.
Central Message:
After infant heart surgery, extent of troponin elevation correlates with complexity of surgery, and persistent elevation beyond 8 hours after surgery is strongly predictive of postoperative morbidity.
Perspective Statement:
Post-surgical heart function in infants with congenital heart disease may be difficult to assess, and hence identification of a reliable biomarker is particularly valuable in this population. Our data provide benchmark values for TN-I following different types of infant cardiac surgeries. Persistent elevation of TN-I beyond 8 hours after surgery is strongly predictive of morbidity and mortality.
Acknowledgments
Funding Source: This work was supported in part by the Southern California Clinical and Translational Science Institute, National Institute of Health/National Center for Research Resources/National Center for Advancing Translational Sciences (NIH/NCRR/NCATS) [UL1TR000130 to GK and SRK] and by NHLBI Grant K08HL121191 to SRK.
Glossary of Abbreviations:
- AUC
Area under the curve
- CPB
Cardiopulmonary bypass
- CTICU
Cardiothoracic intensive care unit
- DHCA
Deep hypothermic circulatory arrest
- ECMO
Extracorporeal membrane oxygenation
- NEC
Necrotizing enterocolitis
- TN-I
Troponin-I
- VIS
Vasoactive inotrope score
Footnotes
Conflict of Interest Statement: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Guest TM, Ramanathan AV, Tuteur PG, Schechtman KB, Ladenson JH and Jaffe AS. Myocardial injury in critically ill patients. A frequently unrecognized complication. JAMA. 1995;273:1945–9. [PubMed] [Google Scholar]
- 2.Adams JE, Sicard GA, Allen BT, Bridwell KH, Lenke LG, Dávila-Román VG, Bodor GS, Ladenson JH and Jaffe AS. Diagnosis of perioperative myocardial infarction with measurement of cardiac troponin I. N Engl J Med. 1994;330:670–4. [DOI] [PubMed] [Google Scholar]
- 3.Taggart DP, Hadjinikolas L, Wong K, Yap J, Hooper J, Kemp M, Hue D, Yacoub M and Lincoln JC. Vulnerability of paediatric myocardium to cardiac surgery. Heart. 1996;76:214–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taggart DP, Hadjinikolas L, Hooper J, Albert J, Kemp M, Hue D, Yacoub M and Lincoln JC. Effects of age and ischemic times on biochemical evidence of myocardial injury after pediatric cardiac operations. J Thorac Cardiovasc Surg. 1997;113:728–35. [DOI] [PubMed] [Google Scholar]
- 5.Hirsch R, Landt Y, Porter S, Canter CE, Jaffe AS, Ladenson JH, Grant JW and Landt M. Cardiac troponin I in pediatrics: normal values and potential use in the assessment of cardiac injury. J Pediatr. 1997;130:872–7. [DOI] [PubMed] [Google Scholar]
- 6.Immer FF, Stocker FP, Seiler AM, Pfammatter JP, Printzen G and Carrel TP. Comparison of troponin-I and troponin-T after pediatric cardiovascular operation. Ann Thorac Surg. 1998;66:2073–7. [DOI] [PubMed] [Google Scholar]
- 7.Modi P, Imura H, Angelini GD, Pawade A, Parry AJ, Suleiman MS and Caputo M. Pathology-related troponin I release and clinical outcome after pediatric open heart surgery. J Card Surg. 2003;18:295–300. [DOI] [PubMed] [Google Scholar]
- 8.Hirsch R, Dent CL, Wood MK, Huddleston CB, Mendeloff EN, Balzer DT, Landt Y, Parvin CA, Landt M, Ladenson JH and Canter CE. Patterns and potential value of cardiac troponin I elevations after pediatric cardiac operations. Ann Thorac Surg. 1998;65:1394–9. [DOI] [PubMed] [Google Scholar]
- 9.Immer FF, Stocker F, Seiler AM, Pfammatter JP, Bachmann D, Printzen G and Carrel T. Troponin-I for prediction of early postoperative course after pediatric cardiac surgery. J Am Coll Cardiol. 1999;33:1719–23. [DOI] [PubMed] [Google Scholar]
- 10.Bottio T, Vida V, Padalino M, Gerosa G and Stellin G. Early and long-term prognostic value of Troponin-I after cardiac surgery in newborns and children. Eur J Cardiothorac Surg. 2006;30:250–5. [DOI] [PubMed] [Google Scholar]
- 11.Froese NR, Sett SS, Mock T and Krahn GE. Does troponin-I measurement predict low cardiac output syndrome following cardiac surgery in children? Crit Care Resusc. 2009;11:116–21. [PubMed] [Google Scholar]
- 12.Gaies MG, Gurney JG, Yen AH, Napoli ML, Gajarski RJ, Ohye RG, Charpie JR and Hirsch JC. Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med. 2010;11:234–8. [DOI] [PubMed] [Google Scholar]
- 13.Modan-Moses D, Prince A, Kanety H, Pariente C, Dagan O, Roller M, Vishne T, Efrati O and Paret G. Patterns and prognostic value of troponin, interleukin-6, and leptin after pediatric open-heart surgery. J Crit Care. 2009;24:419–25. [DOI] [PubMed] [Google Scholar]
- 14.Alves RL, Aragão e Silva AL, Kraychete NC, Campos GO, Martins MeJ and Módolo NS. Intraoperative lactate levels and postoperative complications of pediatric cardiac surgery. Paediatr Anaesth. 2012;22:812–7. [DOI] [PubMed] [Google Scholar]
- 15.Nawaytou H and Bernstein HS. Biomarkers in pediatric heart disease. Biomark Med. 2014;8:943–63. [DOI] [PubMed] [Google Scholar]
- 16.Niedner MF, Foley JL, Riffenburgh RH, Bichell DP, Peterson BM and Rodarte A. B-type natriuretic peptide: perioperative patterns in congenital heart disease. Congenit Heart Dis. 2010;5:243–55. [DOI] [PubMed] [Google Scholar]
- 17.Amirnovin R, Keller RL, Herrera C, Hsu JH, Datar S, Karl TR, Adatia I, Oishi P and Fineman JR. B-type natriuretic peptide levels predict outcomes in infants undergoing cardiac surgery in a lesion-dependent fashion. J Thorac Cardiovasc Surg. 2013;145:1279–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gupta-Malhotra M, Kern JH, Flynn PA, Schiller MS, Quaegebeur JM and Friedman DM. Cardiac troponin I after cardiopulmonary bypass in infants in comparison with older children. Cardiol Young. 2013;23:431–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Montgomery VL, Sullivan JE and Buchino JJ. Prognostic value of pre- and postoperative cardiac troponin I measurement in children having cardiac surgery. Pediatr Dev Pathol. 2000;3:53–60. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.