Abstract
Objectives
There has been an increase in the number of women Veterans with service connected disabilities, which are illnesses or injuries incurred or aggravated during military service. We compared military service and disability characteristics in women and men ≤50 years of age.
Methods
This study included 4,029,672 living Veterans who had at least 1 service connected condition and an active award status as of October 1, 2016. The date of last award as well as demographic, military service, and disability characteristics were obtained from the Veterans Benefits Administration (VBA) VETSNET file.
Results
Among 388,947 women Veterans with service connected conditions, almost 60% (n = 231,364) were ≤50 years of age. Roughly 55% of both women and men ≤50 years had a ≥50% combined rating, although there were differences with respect to individual service connected conditions. Women less often had service connected post traumatic stress disorder (23% vs 32%), but more often had major depression (15% vs 7%). While traumatic brain disease was more common in men, migraine headache was much more common in women (32% vs 18%). Less than half had a VA outpatient visit in the previous year.
Conclusions
The findings of significant numbers of younger women with service connected PTSD, depression, or migraine headache should be considered within the context of post deployment health. These findings raise questions regarding outreach to women Veterans who have these conditions, but do not use VA health care.
Keyword: Public health
1. Background
Since the early 1970s the number of women serving in the Armed Forces of the United States has increased significantly [1]. The percent of all Veterans who were women increased from 6.0% in 2000 to 9.4% in 2015. By the year 2040, women are expected to comprise about 16% of Veterans [1]. Due to the increasing numbers of women serving in and being discharged from the military, there has also been an increase in the number of women Veterans with service connected disabilities, which are illnesses or injuries incurred or aggravated during military service [2, 3, 4, 5].
Several studies have examined sex differences in mental and physical health conditions in Veterans generally and in Veterans with specific service connected conditions such as post traumatic stress disorder (PTSD). In the National Health and Resilience in Veterans Study, compared to men, women had higher prevalence estimates of PTSD, major depression, or migraine headache, but had lower prevalence estimates of nicotine dependence, alcohol use, drug use, diabetes, heart attack, or high blood pressure [6]. Other studies have reported increased levels of pain and musculoskeletal disorders in women Veterans [7], as well as increased prevalence of migraine headache [8, 9] and major depression [10, 11]. In a study of Veterans applying for compensation for PTSD, women were less likely to gain and more likely to lose service connection for PTSD [5, 12].
Relatively little is known about sex differences with respect to demographic, military service, and disability characteristics of Veterans receiving compensation for service connected disabilities. In a study of cause of death in deceased Veterans with service connected disabilities, women decedents born after 1957 more often had migraine headache (20% vs 10%) or major depression (17% vs 10%) than their male counterparts. Both 20% of women and men had service connected PTSD [3]. Among Veterans currently receiving compensation, women Veterans were less likely to use Department of Veterans Affairs (VA) health care services [2].
The overall purpose of this paper is to better understand the characteristics of women with service connected disabilities. The first aim is to describe the military service and disability characteristics of women according to age, defined as younger (≤50), middle age (51–64), or older (≥65). The second aim is to compare military service and disability characteristics in women and men in the younger age group, as most women with service connected conditions are ≤50 years of age. We focused on the younger group, because its members are likely to receive benefits for another 30–40 years.
2. Materials and methods
2.1. Study population
This study included 4,029,672 living Veterans, including 3,640,725 (90%) men and 388,947 (10%) women, who had at least 1 service connected condition and an active award status as of October 1, 2016. The date of last award as well as demographic, military service, and disability characteristics were obtained from the Veterans Benefits Administration (VBA) VETSNET file, which is a one-time view of demographic, disability, and financial characteristics of Veterans receiving a variety of benefits from VBA. Unfortunately, the VETSNET file did not report when compensation was first awarded, meaning that the benefit duration was unknown. The focus of this paper is on women who received compensation in October 2016.
2.2. Study variables
Variables of interest included age, sex, military paygrade, branch of service, number of service connected conditions, type of service connected condition determined from VBA disability codes, combined disability rating, and ≥1 VA outpatient visit in the previous year. Military rank was based on paygrade and was categorized as 1) enlisted, 2) warrant officer, 3) officer, or 4) missing. Age was also categorized as 1) ≤ 50, 2) 51–64, or 3) ≥ 65; corresponding to younger, middle age, and older Veterans. Outpatient visits were obtained from Veterans Health Administration health care utilization files.
With respect to determining service connected disability, procedures for rating individual service connected conditions are described in the web automated reference material system [13]. Each service connected condition is assigned a % rating with a minimum of 0% and maximum of 100%. The combined rating ranges from 0% to 100% and is reported in increments of 10. The 0% rating means that a disability was present but was insufficient to warrant compensation. For Veterans with more than 1 service connected condition, the overall disability rating is determined according to the combined rating table [14]. The most common service connected conditions were identified using VBA disability codes and included tinnitus (code 6260), hearing loss (code 6100), asthma (code 6602), sleep apnea (code 6847), traumatic brain disease (code 8045), migraine (code 8100), anxiety (code 9400), PTSD (code 9411), and major depression (code 9434).
2.3. Statistical analysis
We compared military service and disability service characteristics by the 3 age categories separately for women and men. For Veterans ≤50 years of age, we compared military service and disability characteristics for women and men. Logistic regression was used to assess the association between sex and 3 important service connected conditions, (PTSD, major depression, and migraine headache) for which significant sex differences have been observed. Age, military service, and disability characteristics were entered in the model as was sex. Odds ratios (OR) and 95% confidence intervals (CI) are reported. Given the large sample size, p values are not reported as even the smallest differences achieve statistical significance.
3. Results
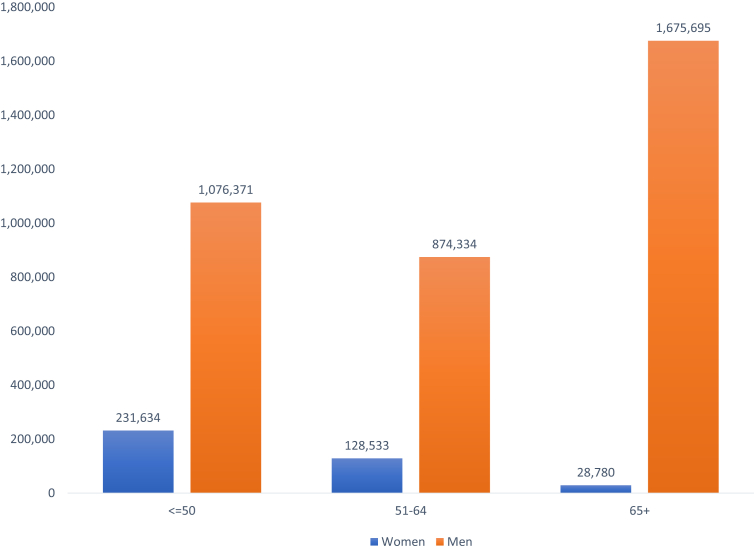
Among 388,947 (10%) women Veterans with service connected conditions, almost 60% were ≤50 years of age (Fig. 1). There were almost 10 times as many men, although only 30% of men were ≤50 years old. Older men or those ≥65 comprised 46% of all men, whereas older women comprised only 7% of all women. Men were on average 13 years older than women.
Fig. 1.
Number of women and men with service connected conditions by age.
Almost half of women served in the US Army, and nearly 25% in the US Air Force (Table 1). The proportion of women who were enlisted personnel was much higher in the younger age group than in the middle or older groups. The extent of missing data with respect to paygrade was much higher in older age group, whose VETSNET records were not as complete. Nearly, 60% of all 3 age groups had a combined disability rating ≥50%. Two of the most common service connected conditions, hearing loss and tinnitus, were also present in women of all ages. Of importance was that compared to middle age and older women, a higher percent of younger women had at least 1 of 3 mental health service connected conditions: anxiety, PTSD, or major depression. Almost 160,000 (65%) younger women had 1 or more of these conditions as opposed to 76,000 (31%) and 10,000 (4%) middle age and older women, respectively. Nearly, 1/3 of younger women had service connected migraine headache; the numbers of younger women with this condition far exceeded the numbers of middle age and older women with service connected migraine. Last, utilization of VA health care in 2015 varied by age group with utilization being highest for older women.
Table 1.
Demographic, service, and disability characteristics of women by age categories.
| Age category | ||||
|---|---|---|---|---|
| Characteristic | ≤50 (n = 231,634) | 51–64 (n = 128,533) | ≥65 (n = 28,780) | All (n = 388,947) |
| Age (years) | 37 ± 7 | 56 ± 4 | 70 ± 6 | 46 ± 13 |
| Service branch | ||||
| US Air Force | 49,287 (22%) | 34,613 (28%) | 7698 (28%) | 91,598 (24%) |
| US Army | 103,397 (48%) | 59,962 (48%) | 13,396 (49%) | 182,755 (48%) |
| US Coast Guard | 2193 (1%) | 1246 (1%) | 129 (<1%) | 3568 (1%) |
| US Marines | 18,308 (8%) | 4312 (4%) | 958 (4%) | 23,578 (6%) |
| US Navy | 46,770 (21%) | 23194 (19%) | 4605 (17%) | 74,569 (20%) |
| Other | 73 (<1%) | 374 (<1%) | 398 (2%) | 845 (<1%) |
| Rank | ||||
| Enlisted | 201,532 (87%) | 95,478 (74%) | 14,350 (50%) | 311,360 (80%) |
| Warrant officer | 649 (<1%) | 1096 (1%) | 190 (<1%) | 1935 (<1%) |
| Officer | 14357 (6%) | 15,190 (12%) | 5640 (20%) | 35,187 (9%) |
| Missing | 15,096 (6%) | 16,769 (13%) | 8600 (30%) | 40,465 (10%) |
| Number service connected conditions | 6.0 ± 5.1 | 6.0 ± 5.4 | 4.7 ± 4.3 | 5.9 ± 5.2 |
| Combined disability rating | ||||
| 100% | 20,779 (9%) | 17,456 (14%) | 3873 (14%) | 42,108 (11%) |
| 50%–90% | 108,031 (47%) | 58,909 (46%) | 12,742 (44%) | 179,682 (46%) |
| 10%–40% | 102,618 (44%) | 51,902 (40%) | 12,064 (42%) | 166,584 (43%) |
| 0% | 206 (<1%) | 266 (<1%) | 101 (<1%) | 573 (<1%) |
| Condition | ||||
| Hearing loss | 21,345 (9%) | 13,899 (11%) | 3638 (13%) | 38,882 (10%) |
| Tinnitus | 51,028 (22%) | 20,974 (16%) | 3532 (12%) | 75,534 (19%) |
| Asthma | 19,819 (9%) | 8880 (7%) | 1601 (65) | 30,300 (8%) |
| Sleep apnea | 11,262 (5%) | 7213 (6%) | 719 (2%) | 19,194 (5%) |
| Anxiety | 18,723 (8%) | 5221 (4%) | 1212 (4%) | 25,456 (6%) |
| Post traumatic stress disorder | 52,572 (23%) | 22,685 (18%) | 4232 (15%) | 79,489 (20%) |
| Major depression | 34,045 (15%) | 16,634 (13%) | 2693 (9%) | 53,372 (14%) |
| Migraine | 73,060 (32%) | 26,766 (21%) | 3306 (12%) | 103,142 (26%) |
| Traumatic brain disease | 5698 (3%) | 2162 (2%) | 385 (1%) | 8245 (2%) |
| VA health care utilization in 2015 | 109,875 (47%) | 56,723 (56%) | 17,195 (60%) | 19,880 (51%) |
In the younger age group, about half of both women and men served in the US Army, although women served more often in the US Air Force and men more often in the US Marines (Table 2). Nearly 90% of both sexes were enlisted personnel with relatively few in the officer category. Roughly 55% of both women and men had a ≥50% combined rating, although there were differences with respect to individual service connected conditions. Men had far more hearing loss or tinnitus with nearly half having tinnitus. Men more often had service connected sleep apnea and women more often had service connected asthma.
Table 2.
Demographic, service, and disability characteristics of women and men ≤50 years of age.
| Characteristic | Women (n = 231,634) | Men (n = 1,076,371) |
|---|---|---|
| Age (years) | 37 ± 7 | 38 ± 7 |
| Service branch | ||
| US Air Force | 49,287 (22%) | 132,370 (12%) |
| US Army | 109,397 (48%) | 526,912 (50%) |
| US Coast Guard | 2193 (1%) | 9433 (1%) |
| US Marines | 18,308 (8%) | 219694 (21%) |
| US Navy | 46,770 (21%) | 167,768 (16%) |
| Rank | ||
| Enlisted | 201,532 (87%) | 953,736 (89%) |
| Warrant officer | 649 (<1%) | 5968 (<1%) |
| Officer | 14,357 (6%) | 49,861 (5%) |
| Missing | 15,096 (7%) | 66,806 (6%) |
| Number service connected conditions | 6.0 ± 5.1 | 5.9 ± 5.1 |
| Combined disability rating | ||
| 100% | 20,779 (9%) | 97,624 (9%) |
| 50%–90% | 108,031 (47%) | 497,740 (46%) |
| 10%–40% | 102,618 (44%) | 480,351 (45%) |
| 0% | 206 (<1%) | 656 (<1%) |
| Condition | ||
| Hearing loss | 21,345 (9%) | 264,388 (25%) |
| Tinnitus | 51,028 (22%) | 480,577 (45%) |
| Asthma | 19,819 (9%) | 48,871 (4%) |
| Sleep apnea | 11,262 (5%) | 166,776 (16%) |
| Anxiety | 18,723 (8%) | 73,700 (7%) |
| Post traumatic stress disorder | 52,272 (23%) | 341,721 (32%) |
| Major depression | 34,045 (15%) | 77,276 (7%) |
| Migraine | 73,060 (32%) | 190,906 (18%) |
| Traumatic brain disease | 5698 (3%) | 80,747 (8%) |
| VA health care utilization in 2015 | 109,875 (47%) | 452,870 (42%) |
There were large sex differences with respect to mental health conditions and migraine headache as seen in Table 2. Women less often had service connected PTSD (23% vs 32%), but more often had major depression (15% vs 7%); the distribution of anxiety was similar for younger women and men. While traumatic brain disease was more common in men, migraine headache was much more common in women (32% vs 18%). Logistic regression analysis indicated that women had 23% lower odds of having PTSD (OR = 0.77, 95% CI = 0.76–0.78), yet had 83% higher odds of having major depression (OR = 1.83, 95% CI = 1.80–1.86). The odds of women having migraine headache were nearly 2.3 times that of men (OR = 2.28, 95% CI = 2.26–2.30).
To better understand service connected migraine headache, we compared characteristics of younger women and men with the condition (Table 3). Of note, nearly 70% of women and 75% of men had a ≥50% rating and the percent with a 100% rating was higher than it was for other younger Veterans. The percent of women and men with PTSD was also higher in the group with migraine than it was in other younger Veterans. Overall, Veterans with migraine headache seemed to have more severe disability and more mental health conditions than did those without migraine headache.
Table 3.
Demographic, service, and disability characteristics of women and men ≤50 years of age: migraine headache.
| Characteristic | Women (n = 73,060) | Men (n = 190,906) |
|---|---|---|
| Age (years) | 37 ± 7 | 37 ± 7 |
| Service branch | ||
| US Air Force | 16,656 (23%) | 20,703 (11%) |
| US Army | 33,627 (47%) | 104,776 (55%) |
| US Coast Guard | 622 (0.9%) | 1246 (0.7%) |
| US Marines | 5075 (7%) | 35,654 (19%) |
| US Navy | 15,889 (22%) | 26,427 (14%) |
| Rank | ||
| Enlisted | 65,670 (90%) | 175,987 (92%) |
| Warrant officer | 228 (0.3%) | 1052 (0.6%) |
| Officer | 4041 (6%) | 6778 (4%) |
| Missing | 3121 (4%) | 7089 (4%) |
| Number service connected conditions | 7.4 ± 5.5 | 7.9 ± 5.8 |
| Combined disability rating | ||
| 100% | 9341 (13%) | 32,619 (17%) |
| 50%–90% | 41,247 (56%) | 108,335 (57%) |
| 10%–40% | 22,450 (31%) | 49,902 (26%) |
| 0% | 22 (0%) | 54 (0%) |
| Condition | ||
| Auditory | 5664 (8%) | 38,322 (20%) |
| Tinnitus | 17,763 (24%) | 95,901 (50%) |
| Asthma | 6688 (9%) | 8829 (5%) |
| Sleep apnea | 4270 (6%) | 35,649 (19%) |
| Anxiety | 6774 (9%) | 15,146 (8%) |
| Post traumatic stress disorder | 18,497 (25%) | 84,191 (44%) |
| Major depression | 12,434 (17%) | 15,897 (6%) |
| Traumatic brain disease | 5698 (3%) | 80,747 (8%) |
| VA health care utilization in 2015 | 37,437 (51%) | 95,393 (50%) |
Compared to younger men, younger women were more likely to use VA health care services, although less than 50% of both groups used care in the year prior to October 2016. Younger women Veterans with service connected hearing loss were more likely to use VA health care than men (48% vs 41%). A higher percent of Veterans with mental health related service connected disabilities used VA health care. For Veterans with PTSD, 62% of women and 56% of men had VA health care utilization and for major depression, 57% of women and 55% of men used VA care. For those with a 100% rating, 68% of women and 66% of men used VA health care during the year prior to the most current award.
4. Discussion
In October 2016, there were almost 400,000 women Veterans with service connected conditions and nearly 60% were ≤50 years of age. Although there were 10 times as many men with service connected conditions, only 30% of men were in the younger age category. This finding reflects the increasing numbers of women serving in the military [1]. It also may reflect the unprecedented numbers of women exposed to the many stressors associated with deployment to combat zones. Both younger women and men had significant disabilities in that over half had combined ratings ≥50% and 9% had a 100% rating. While about half of younger women and men served in the US Army, women more often served in the US Air Force and men in the US Marines, nearly 90% of both groups were enlisted personnel [15, 16].
There were noticeable sex differences with respect to type of service connected condition for younger women and men. Hearing loss, tinnitus, and sleep apnea were more common in men, while asthma was more common in women. With respect to mental health conditions, PTSD was more common in men, although over 20% of women had service connected PTSD. The percent of women with major depression was over twice that for men. These findings further emphasize the burden of mental health conditions among Veterans with service connected conditions [2, 17].
For younger Veterans, a higher percent of women had service connected migraine headache. The odds of having migraine headache were 2.3 times higher for women than men. In a study of headache diagnosis among Iraq and Afghanistan war Veterans who used VA health care, the odds of a medical diagnosis of migraine headache were 2.7 times higher for women [9]. The authors of this study concluded that headache is not an isolated condition but is part of a complex set of post-deployment health problems, including musculoskeletal pain and mental health disorders. While similar increased risks of migraine headache were observed in both the current and Carlson studies, it is important to know that Carlson et al used ICD-9 diagnosis codes, whereas VA disability codes were used in the current study. VA disability codes are not medical diagnosis codes but signify conditions or injuries that were related to military service and contributed to the combined disability rating which is a measure of impairment in earning capacity [18]. Also, there were Veterans in the current study who did not use VA health care; by definition, all Veterans in the Carlson study used VA health care.
Two studies have also noted that women Veterans are more likely to have major depression than their male counterparts [10, 11]. In a sample of current-era US Veterans, Curry et al [10] found that 46% of women and 36% of men had a major depressive disorder as determined by the Structured Clinical Interview, whereas Maguen et al [11] reported that 23% and 17% of women and men, respectively, had major depression as defined by ICD-9 diagnosis codes. As was the case with migraine headache, medical diagnosis of depression is not necessarily the same thing as service connected depression. It is noteworthy, however, that a sex difference was noted for both medical and service connected definitions of major depression.
The focus of this study was on younger Veterans with service connected disabilities, as they will likely be receiving benefits for at least another 30–40 years given that they were on average 37 years of age in October 2016. Although we do not have information regarding where these Veterans served and whether they were deployed to combat zones, it is highly likely that many served in Iraq and Afghanistan under combat conditions. From a policy perspective, VA has a long-standing commitment to provide an integrated array of benefits, including compensation and health care, for these individuals and in some instances for their families, who may be eligible for certain benefits such as disability indemnity compensation for surviving spouses and vocational and college tuition for children.
In response to the increasing numbers of women serving in the military, VA has for many years offered an array of benefits, including women's health services. Women Veterans with service connected conditions, including depression, PTSD, and migraine headache, need financial, medical, and social support as they adjust to life in the post deployment world [19, 20]. For women with service connected conditions compensation and health care are benefits designed to provide that support.
In this study of Veterans with service connected conditions, < 50% of younger Veterans used VA health care, although use varied by condition with higher utilization for those with mental health conditions. In general, women Veterans tended to use services more than men. Findings from a national survey suggest that VA health care utilization for those with a medical diagnosis of PTSD or depression approaches 70%, although those with alcohol use disorders are less likely to engage in care [21].
A limitation of the current study is the absence of information regarding the use of non-VA health care. It is possible that Veterans with service connected conditions received their care from non-VA providers. Knowing more about this is critical for those with mental health conditions, as younger women Veterans with service connected PTSD or major depression are more likely to die from suicide or accidental causes [3]. There is an opportunity for outreach to those Veterans who have service connected mental health conditions, but do not use VA health care [22]. It should be recognized that barriers to accessing care may be different from barriers to engaging in care, particularly for younger Veterans with mental health conditions [21]. For Veterans with a combined rating ≥50%, barriers to care are reduced, because VA health care is provided at little or no cost. On the other hand, stigma associated with mental health conditions as well as reluctance to seek care in settings where men comprise the majority of patients are just 2 factors which may make it difficult for Veterans to engage in care.
In addition to not having information about deployment and combat exposure, we did not have information about military sexual trauma (MST) and its influence on the determination of disability and the combined rating. It is likely that MST was associated with many disabilities, including mental health conditions as well as traumatic brain disease and migraine headache [20]. While both men and women are affected by MST, a higher proportion of women have reported MST [23, 24].
5. Conclusions
The number of women serving in the military has increased significantly over the past 40–50 years, as has the number of women with service connected conditions. Among younger women with service connected conditions, mental health conditions, including PTSD and major depression, were highly prevalent as was migraine headache. Both conditions should be considered within the context of post deployment health and the military service experiences of women Veterans. These findings raise policy questions regarding women who have service connected conditions and are users of VA health care as well as outreach to Veterans who have service connected conditions, but do not use VA health care. This outreach should emphasize the broad array of integrated services VA offers to Veterans who have served their country and suffered illnesses or injuries that in many cases have significantly altered their lives.
Declarations
Author contribution statement
Charles Maynard: Conceived and designed the analysis; Analyzed and interpreted the data; Contributed analysis tools or data; Wrote the paper.
Karin Nelson, Stephan D Fihn: Analyzed and interpreted the data; Wrote the paper.
Funding statement
This work was supported by the Department of Veterans Affairs, Clinical System Development and Evaluation.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.National Center for Veterans Analysis and Statistics The past, present, and future of women Veterans. https://www.va.gov/vetdata/docs/SpecialReports/Women_Veterans_2015_Final.pdf Available:
- 2.Maynard C., Batten A., Liu C.F. The burden of mental illness among Veterans. Med. Care. 2017;55:965–969. doi: 10.1097/MLR.0000000000000806. [DOI] [PubMed] [Google Scholar]
- 3.Maynard C., Trivedi R., Nelson K. Disability rating, age at death, and cause of death in US Veteran with service connected conditions. Mil. Med. 2018;183:e371–e376. doi: 10.1093/milmed/usy040. [DOI] [PubMed] [Google Scholar]
- 4.Maynard C., Nelson K., Fihn S.D. Disability rating and one-year mortality in Veterans with service connected conditions. Publ. Health Rep. 2018;133:141–146. doi: 10.1177/0033354918794929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murdoch M., Hodges J., Hunt C. Gender differences in service connection for PTSD. Med. Care. 2003;41:950–961. doi: 10.1097/00005650-200308000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Ziobrowski H., Sartor C.E., Tsai J. Gender differences in mental and physical health conditions in US veterans: results from the national health and resilience in veterans study. J. Psychosom. Res. 2017;101:110–113. doi: 10.1016/j.jpsychores.2017.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Higgins D.M., Fenton B.T., Driscoll M.A. Gender differences in demographic and clinical correlates among Veterans with musculoskeletal disorders. Wom. Health Issues. 2017;27:463–470. doi: 10.1016/j.whi.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 8.Altalib H.H., Fenton B.T., Sico J. Increase in migraine diagnoses and guideline-concordant treatment in veterans, 2004-2012. Cephalagia. 2017;37:3–10. doi: 10.1177/0333102416631959. [DOI] [PubMed] [Google Scholar]
- 9.Carlson K.F., Taylor B.C., Hagel E.M. Headache diagnoses among Iraq and Afghanistan war Veterans enrolled in VA: a gender comparison. Headache. 2013;53:1573–1582. doi: 10.1111/head.12216. [DOI] [PubMed] [Google Scholar]
- 10.Curry J.F., Aubuchon-Endsley N., Brancu M. Lifetime major depression and comorbid disorders among current-era women veterans. J. Affect. Disord. 2014;152–154:434–440. doi: 10.1016/j.jad.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 11.Maguen S., Ren L., Bosch J.O. Gender differences in mental health diagnoses among Iraq and Afghanistan Veterans enrolled in Veterans Affairs health care. Am. J. Public Health. 2010;105:2450–2456. doi: 10.2105/AJPH.2009.166165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sayer N.A., Hagel E.M., Noorbaloochi S. Gender differences in VA disability status for PTSD over time. Psychiatr. Serv. 2014;65:663–669. doi: 10.1176/appi.ps.201300017. [DOI] [PubMed] [Google Scholar]
- 13.Veterans Benefits Administration 38 CFR Book C—Schedule for Rating Disabilities. https://www.benefits.va.gov/warms/bookc.asp
- 14.Veterans Benefits Administration Combined ratings. https://www.benefits.va.gov/compensation/rates-index.asp
- 15.MacLean A., Edwards R.D. The pervasive role of rank in the health of US Veterans. Armed Forces Soc. 2010;36:765–785. doi: 10.1177/0095327X09356166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maynard C., Blalock A. The welfare state within the military. J. Sociol. Soc. Welfare. 1977;4:494–521. [Google Scholar]
- 17.Trivedi R.B., Post E.P., Sun H. Prevalence, comorbidity, and prognosis of mental health among US Veterans. Am. J. Public Health. 2015;105:2564–2569. doi: 10.2105/AJPH.2015.302836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meshberg-Cohen S., DeViva J.C. Counseling Veterans applying for service connection status for mental health conditions. Psychiatr. Serv. 2017;68:396–399. doi: 10.1176/appi.ps.201500533. [DOI] [PubMed] [Google Scholar]
- 19.Sairsingh H., Solomon P., Helstrom A. Depression in female Veterans returning from deployment: the role of social factors. Mil. Med. 2018;183:e133–e139. doi: 10.1093/milmed/usx065. [DOI] [PubMed] [Google Scholar]
- 20.Frayne S.M., Phibbs C.S., Saecho F. Department of Veterans Affairs; 2018. Sourcebook: Women Veterans in the Veterans Health Administration, Volume 4: Longitudinal Trends in Sociodemographics, Utilization, Health Profile, and Geographic Distribution; pp. 1–132.https://www.womenshealth.va.gov/WOMENSHEALTH/docs/WHS_Sourcebook_Vol-IV_508c.pdf [Google Scholar]
- 21.Elbogen E.B., Wagner H.R., Johnson S.C. Are Iraq and Afghanistan Veterans using mental health services? New data from a national random-sample survey. Psychiatr. Serv. 2013;64:134–141. doi: 10.1176/appi.ps.004792011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sripada R.K., Hannemann C.M., Schnurr P.P. Mental health service utilization before and after receipt of a service-connected disability award for PTSD: findings from a national sample. Health Serv. Res. 2018;53:4565–4583. doi: 10.1111/1475-6773.12859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kimerling R., Gima K., Smith M.W. The Veterans Health Administration and military sexual trauma. Am. J. Public Health. 2007;97:2160–2166. doi: 10.2105/AJPH.2006.092999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kimerling R., Street A.E., Pavao J. Military-related sexual trauma among Veterans Health Administration patients returning from Afghanistan and Iraq. Am. J. Public Health. 2010;100:1409–1412. doi: 10.2105/AJPH.2009.171793. [DOI] [PMC free article] [PubMed] [Google Scholar]