Abstract
Background
Suicide attempts and non-suicidal self-harm (NSSH) are major public health concerns that affect millions of young people worldwide. Consequently, there is a strong need for up-to-date epidemiological data in this population.
Aims
To provide prevalence and trend estimates of suicidal thoughts and behaviours and NSSH thoughts and behaviour in university students.
Method
Data are from a 2018 national health survey for higher education in Norway. A total of 50 054 full-time students (69.1% women) aged 18–35 years participated (response rate 31%). Suicidal ideation, suicide attempts and NSSH were assessed with three items drawn from the Adult Psychiatric Morbidity Survey, and thoughts of NSSH were assessed with one item from the Child and Adolescent Self-Harm in Europe study.
Results
Lifetime suicidal thoughts were reported by 21.0%, and 7.2% reported having such thoughts within the past year. In total, 4.2% reported a suicide attempt, of whom 0.4% reported attempting suicide within the past year. The prevalence of lifetime NSSH behaviour and thoughts was 19.6% and 22.6%, respectively. All four suicidal behaviour and NSSH variables were more common among students who were single, living alone and with a low annual income, as well as among immigrants. There was an increase in suicidal thoughts from 2010 (7.7%) to 2018 (11.4%), which was evident in both men and women.
Conclusions
The observed high and increasing prevalence of suicidal thoughts and NSSH among college and university students is alarming, underscoring the need for further research, preferably registry-linked studies, to confirm whether the reported prevalence is representative of the student population as a whole.
Declaration of interest
None.
Keywords: Deliberate self-harm, epidemiology, suicide
Suicide attempts and non-suicidal self-harm (NSSH) are major public health concerns that affect millions worldwide, particularly young people.1,2 They are important markers of unbearable distress as well as predictors of future suicide.3 Indeed, history of any suicide attempts or NSSH is one of the most robust predictors of future suicide.3–5 One of the challenges when conducting research in the field is that there is no consensus as to how best to conceptualise these behaviours, with some studies describing all self-injurious behaviours as self-harm irrespective of motive,6 and others distinguishing between NSSH or non-suicidal self-injury versus suicide attempts.7,8 Although we recognise the difficulty in defining self-injurious behaviours, in the present study we report NSSH and suicide attempts separately.
Prevalence rates
Despite the renewed focus on identifying the scale of these behaviours,1,9 there remain many gaps in our knowledge. Specifically, relatively little large-scale research has focused on quantifying the prevalence of NSSH and suicide attempts in young adults beyond their teenage years. This is an important gap in our knowledge, as it is unclear to what extent the rates of NSSH and suicide attempts increase or decrease in young adulthood. A recent exception was a population-based prevalence study conducted in Scotland, which demonstrated that 11% of 18- to 34 year-olds reported a suicide attempt at some stage in their lives, and 16% reported NSSH.8 For NSSH, there is a clear developmental pattern; it is rare before puberty, peaking in adolescence, with a reduced prevalence in the early adult years.10 However, few studies have covered the range of young adulthood and included measures of both NSSH and suicide attempt thoughts and behaviours. As noted above, it is crucial that we clarify the developmental course of these behaviours.10
In this study of young adults, we have focused specifically on university and college students, as self-injurious behaviours have been shown to be frequent in this group. This transition from the teenage years to adulthood is important because it involves multiple domains of challenge: (a) parental guidance and monitoring diminish; (b) the transition to college may be stressful; (c) increased challenges give more opportunities to access a wide range of risky activities; and (d) the stress associated with facing life decisions across multiple domains that may have a long-term impact on future functioning including educational/career decisions and decisions relating to marriage and starting a family.11–14 Indeed, a recent meta-analysis of college student samples also indicated a high rate of suicidal ideation and suicide attempts.15 However, most of the studies included in the meta-analysis were based on undergraduate students in the USA, thereby highlighting the need for well-powered studies from other countries and in different age groups.15
Study aims
Given the dearth of large-scale studies of NSSH and suicide attempts in young adults, and the fact that no trend study on suicidality has been conducted among this group, the aim of the present study is to examine the prevalence of suicidal thoughts and suicide attempts and NSSH thoughts and behaviour in a large sample of college students aged between 18 and 35 years in 2018, as well as to examine potential changes in suicidal ideation from 2010 to 2018, in this population.
Method
Procedure
The SHoT study (Students' Health and Wellbeing Study) is a national student survey for higher education in Norway, initiated by three largest welfare associations. So far, three health surveys of the student population (aged 18–35) in Norway have been completed (2010, 2014 and 2018), and all three waves were collected electronically through a web-based platform. The three studies were conducted separately (not a longitudinal data collection). Details of the SHoT study has been published elsewhere.16
The SHoT2018 was conducted between 6 February and 5 April 2018 inviting all full-time Norwegian students pursuing higher education (both in Norway and abroad) to participate. For the SHoT2018 study, 162 512 students fulfilled the inclusion criteria, of whom 50 054 students completed the online questionnaires, yielding a response rate of 30.8%. The SHoT2014 study was conducted between 24 February and 27 March 2014. An invitation email containing a link to an anonymous online questionnaire was sent to 47 514 randomly selected students and stratified by study institutions, faculties and departments. The overall response rate was 28.5% and included 13 525 students. The SHoT2010 study was conducted between 11 October and 8 November 2010. The target group was a random sample of 26 779 Norwegian full-time students, of whom 6053 students completed the survey, yielding a response rate of 22.6%.
Ethics
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human participants/patients were approved by the Regional Committee for Medical and Health Research Ethics in Western Norway (no. 2017/1176 (SHOT2018)). Informed consent was obtained electronically after the participants had received a detailed introduction to the study. Approvals for conducting the SHoT2010 and SHoT2014 studies were granted by the Data Protection Officer for research at the Norwegian Centre for Research Data.
Instruments
Demographic information (SHoT2018)
All participants indicated their gender and age, and to enable comparisons across similar studies the participants were categorised into three age groups (18–23 years (62.2%, n = 31 118); 24–29 years (31.1%, n = 15 584); and 30–35 years (5.3%, n = 2640)). Participants were also asked about their household status (coded as ‘living alone’ versus ‘living with others’), as well as their relationship status (coded as ‘single’ versus ‘married’/‘partner’ or ‘girl-/boyfriend’). Economic activity was coded dichotomously according to self-reported annual income (before tax and deductions, and not including loans and scholarships): ‘economically active’ (annual income >10 000 Norwegian Krone (NOK)) versus ‘economically inactive’ (<10 000 NOK). The reason for excluding loans and scholarships from the annual income, was that all students taking higher education in Norway receive near-identical loans/scholarships, and in this respect, we were more interested in students earning additional money working alongside being a full-time student. Finally, participants were categorised as an immigrant if either the student or his/her parents were born outside Norway.
Suicidal thoughts, suicidal attempts and NSSH (SHoT2018)
History of suicidal thoughts, suicide attempts and NSSH were assessed with three items drawn from the Adult Psychiatric Morbidity Survey (APMS);17 ‘Have you ever seriously thought of taking your life, but not actually attempted to do so?’, ‘Have you ever made an attempt to take your life, by taking an overdose of tablets or in some other way?’, and ‘Have you ever deliberately harmed yourself in any way but not with the intention of killing yourself? (i.e. self-harm)’. The question about NSSH thoughts was adapted from the Child and Adolescent Self-Harm in Europe study (CASE).18 ‘Have you ever seriously thought about trying to deliberately harm yourself but not with the intention of killing yourself, but not actually done so?’. If respondents answered yes to any item, the timing of the most recent episode was assessed, using the following response options: ‘last week’, ‘past year’, ‘more than a year ago, but after I started studying at the university’, and ‘before I started studying at university’. In the current study, we defined ‘recent’ event as an episode having occurred within the past 12 months (the first two response options). In addition, the frequency of episodes (response options: ‘1’ through ‘10 or more’) and age at first onset (response options: ‘younger than 10 years’ through ‘35 years’) were also assessed for each of the four items.
Suicidal thoughts in all three SHoT studies
In addition to the four suicidal and non-suicidal thoughts and behaviour questions asked in SHoT2018, suicidal thoughts were also measured by one item of the depression subscale of the Hopkins Symptom Checklist (HSCL-25)19 (‘in the past two weeks, including today, how much have you been bothered by thoughts of ending your life’) across all three SHoT study waves. The response options were ‘not at all’, ‘a little’, ‘quite a bit’, and ‘extremely’.
Statistics
IBM SPSS version 25 for Mac was used for all analyses. χ2 tests and logistic regression analyses were used to examine differences in suicidal thoughts, suicide attempts, NSSH thoughts and behaviour across demographic characteristics. We also calculated the prevalence ratios (corresponding to the relative risk) for women and men by dividing the prevalence estimates of women by those of men. As a test of precision, we calculated the positive predictive value (PPV) and negative predictive value (NPV) of the single suicidal ideation item included in the HSCL-25 of the SHoT2018 study against the dichotomised suicidal ideation item from the APMS instrument. Pearson's χ2 tests were used to test for significant changes in suicidal ideation (coded dichotomously) over time. As the three surveys included somewhat different welfare associations and institutions, sensitivity analyses were performed only including the institutions included in all three surveys. The samples included in these analyses were n = 24 298 (48.5%) in 2018, n = 6681 (49.4%) in 2014 and n = 4369 (72.2%) in 2010. Missing values were handled using listwise deletion, and there was generally little missing data (n<270 of 50 054 on the four main suicidal and non-suicidal thoughts and behaviour questions.
Results
The data reported focuses on the 2018 data-set, with the exception of trends in suicidal thoughts.
Descriptive statistics
Compared with all invited students (58.1% women and 41.9% men), the current sample included a larger proportion of women (69.1%) than men (30.9%). The mean age was 23.2 years (s.d. = 3.3), and the age distribution of participating students (18–20 years (18%, n = 8832), 21–22 years (31%, n = 15 471), 23–25 years (32%, n = 15 902), 26–28 years (11%, n = 5710) and 29–35 years (7%, n = 3427)), was almost identical to that of all invited students (18–20 years (18%, n = 28 996), 21–22 years (31%, n = 49 731), 23–25 years (32%, n = 51 714), 26–28 years (12%, n = 19 901) and 29–35 years (6%, n = 10 216)).
In terms of accommodation status, 19.3% reported living alone (n = 9675 (women: 18.7%, men: 20.7%, P<0.001)) and 49.9% (n = 24 969) reported being single (women: 47.2%, men: 56.0%, P<0.001). The majority of the participants (87.5%, n = 43 778) had an annual income of more than 10 000 NOK (women: 88.9%, men: 84.5%, P<0.001). A total of 8% of the participants (n = 4010) were immigrants, defined as either the student or his/her parents being born outside Norway (women: 7.9%, men: 8.2%, P = 0.292).
Prevalence of NSSH, NSSH thoughts, suicide attempts and suicidal thoughts
As detailed in Table 1, lifetime suicidal thoughts were reported by 21.0% (n = 10 494) of the students, and 7.2% reported experiencing such thoughts within the past year. Significantly more women than men reported lifetime suicidal thoughts (lifetime: 22.1% v. 18.3%, prevalence ratio, 1.21; odds ratio (OR) = 1.27, 95% CI 1.21–1.33, P<0.001). A similar gender effect was also observed for past year suicidal thoughts.
Table 1.
Rates of suicidal thoughts, suicide attempts, non-suicidal self-harm (NSSH) thoughts and NSSH by age group
| 18–23 years | 24–29 years | 30–35 years | All age groups | |||||
|---|---|---|---|---|---|---|---|---|
| Lifetime | Past year | Lifetime | Past year | Lifetime | Past year | Lifetime | Past year | |
| All students, % (95% CI) | ||||||||
| Suicidal thoughts | 19.8 (19.4 to 20.3) | 7.0 (6.7 to 7.2) | 22.3 (21.7 to 23.0) | 7.5 (7.1 to 7.9) | 27.6 (25.9 to 29.3) | 7.5 (6.5 to 8.5) | 21.0 (20.7 to 21.4) | 7.2 (6.9 to 7.4) |
| Suicide attempts | 3.7 (3.5 to 3.9) | 0.4 (0.4 to 0.5) | 4.7 (4.3 to 5.0) | 0.5 (0.4 to 0.6) | 7.9 (6.9 to 8.9) | 0.3 (0.1 to 0.5) | 4.2 (4.1 to 4.4) | 0.4 (0.4 to 0.5) |
| NSSH thoughts | 23.8 (23.3 to 24.3) | 9.7 (9.3 to 10.0) | 20.7 (20.3 to 21.2) | 7.7 (7.3 to 8.1) | 20.9 (19.4 to 22.5) | 6.4 (5.5 to 7.4) | 22.6 (22.3 to 23.0) | 8.8 (8.6 to 9.1) |
| NSSH | 20.0 (19.5 to 20.4) | 4.6 (4.4 to 4.8) | 19.2 (18.5 to 19.8) | 3.3 (3.1 to 3.6) | 19.1 (18.5 to 19.7) | 2.0 (1.5 to 2.6) | 19.6 (19.3 to 20.0) | 4.1 (3.9 to 4.2) |
| Women, % (95% CI) | ||||||||
| Suicidal thoughts | 20.9 (20.4 to 21.5) | 7.0 (6.7 to 7.4) | 23.7 (22.9 to 24.5) | 7.8 (7.3 to 8.3) | 27.8 (25.7 to 29.9) | 7.4 (6.1 to 8.6) | 22.1 (21.7 to 22.6) | 7.3 (7.0 to 7.6) |
| Suicide attempts | 4.1 (3.8 to 4.3) | 0.5 (0.4 to 0.5) | 5.4 (4.9 to 5.8) | 0.5 (0.4 to 0.6) | 9.1 (7.7 to 10.4) | 0.2 (0.0 to 0.5) | 4.7 (4.5 to 4.9) | 0.5 (0.4 to 0.5) |
| NSSH thoughts | 28.1 (27.5 to 28.7) | 11.6 (11.2 to 12.0) | 25.0 (24.4 to 25.6) | 9.6 (9.0 to 10.1) | 23.4 (21.4 to 25.4) | 6.9 (5.7 to 8.1) | 26.9 (26.5 to 27.4) | 10.7 (10.4 to 11.1) |
| NSSH | 23.7 (23.2 to 24.3) | 5.4 (5.1 to 5.7) | 23.9 (23.0 to 24.7) | 4.2 (3.8 to 4.6) | 21.1 (20.3 to 21.9) | 2.4 (1.7 to 3.1) | 23.6 (23.2 to 24.1) | 4.9 (4.7 to 5.1) |
| Men, % (95% CI) | ||||||||
| Suicidal thoughts | 16.6 (15.8 to 17.4) | 6.6 (6.1 to 7.1) | 19.6 (18.5 to 20.6) | 6.8 (6.2 to 7.5) | 26.6 (23.7 to 29.5) | 7.2 (5.5 to 8.9) | 18.3 (17.7 to 18.9) | 6.7 (6.3 to 7.1) |
| Suicide attempts | 2.6 (2.3 to 2.9) | 0.4 (0.3 to 0.5) | 3.3 (2.8 to 3.8) | 0.4 (0.3 to 0.6) | 4.8 (3.4 to 6.2) | 0.2 (−0.1 to 0.5) | 3.0 (2.7 to 3.3) | 0.4 (0.3 to 0.5) |
| NSSH thoughts | 12.7 (12.0 to 13.4) | 4.6 (4.2 to 5.0) | 12.6 (11.9 to 13.3) | 4.2 (3.7 to 4.8) | 15.6 (13.2 to 18.0) | 5.0 (3.6 to 6.4) | 12.8 (12.3 to 13.4) | 4.5 (4.2 to 4.8) |
| NSSH | 10.1 (9.5 to 10.7) | 2.5 (2.2 to 2.8) | 10.3 (9.5 to 11.1) | 1.7 (1.3 to 2.0) | 14.5 (13.6 to 15.4) | 0.9 (0.3 to 1.5) | 10.4 (9.9 to 10.9) | 2.1 (1.9 to 2.3) |
| Prevalence ratiosa | ||||||||
| Suicidal thoughts | 1.26 | 1.07 | 1.21 | 1.14 | 1.05 | 1.02 | 1.21 | 1.09 |
| Suicide attempts | 1.56 | 1.14 | 1.61 | 1.12 | 1.88 | 1.04 | 1.57 | 1.13 |
| NSSH thoughts | 2.21 | 2.52 | 1.99 | 2.26 | 1.50 | 1.38 | 2.10 | 2.39 |
| NSSH | 2.35 | 2.18 | 2.31 | 2.50 | 1.46 | 2.67 | 2.27 | 2.33 |
| Women versus men, OR (95% CI) | ||||||||
| Suicidal thoughts | 1.33 (1.25 to 1.42) | 1.08 (0.98 to 1.19) | 1.28 (1.18 to 1.39) | 1.15 (1.02 to 1.31) | 1.06 (0.89 to 1.28) | 1.02 (0.75 to 1.39) | 1.27 (1.21 to 1.33) | 1.10 (1.02 to 1.19) |
| Suicide attempts | 1.59 (1.37 to 1.84) | 1.15 (0.78 to 1.68) | 1.64 (1.39 to 1.96) | 1.12 (0.69 to 1.82) | 1.97 (1.39 to 2.79) | 1.04 (0.19 to 5.69) | 1.61 (1.45 to 1.79) | 1.14 (0.85 to 1.53) |
| NSSH thoughts | 2.68 (2.50 to 2.88) | 2.72 (2.44 to 3.02) | 2.32 (2.12 to 2.55) | 2.40 (2.07 to 2.78) | 1.65 (1.34 to 2.04) | 1.40 (0.99 to 2.00) | 2.52 (2.39 to 2.65) | 2.55 (2.35 to 2.78) |
| NSSH | 2.78 (2.57 to 3.00) | 2.25 (1.94 to 2.61) | 2.72 (2.47 to 3.01) | 2.57 (2.04 to 3.23) | 1.58 (1.27 to 1.97) | 2.71 (1.26 to 5.80) | 2.65 (2.50 to 2.80) | 2.39 (2.12 to 2.70) |
a. A prevalence ratio >1 means that women are more likely to report the thought/behaviour, with a prevalence ratio <1 indicating that men are more likely to report the thought/behaviour.
In total, 4.2% of the students (n = 2112) reported having attempted suicide, of whom the majority (3.1%, n = 1570) reported that the (last) suicide attempt occurred before they started studying. In all, 220 students (0.4%) reported having attempted suicide within the past year. A similar pattern was observed for both genders. As with suicidal thoughts, lifetime suicide attempts were more prevalent in women (4.7%) compared with men (3.0%, prevalence ratio, 1.57; OR = 1.61, 95% CI 1.45–1.79, P<0.001). There was no gender difference in past year suicide attempt.
NSSH thoughts were reported by 22.6% (n = 11 301) of the students, and 8.8% (n = 4414) of the participants reported such thoughts during the past year. Women were much more likely than men to experience lifetime NSSH thoughts (26.9% and 12.8%, respectively, prevalence ratio, 2.10; OR = 2.52, 95% CI 2.39–2.65, P<0.001), and a similar gender effect was observed for past year NSSH thoughts.
NSSH was reported by 19.6% (n = 9821) of the students and was significantly more frequent among women (23.6%) than among men (10.4%, prevalence ratio, 2.27; OR = 2.65, 95% CI 2.50–2.80, P<0.001). In terms of recent NSSH, 4.1% of the students reported NSSH within the past year, and a similar gender effect was observed (4.9% in women and 2.1% in men).
Number of occurrences of NSSH, NSSH thoughts, suicide attempts and suicidal thoughts
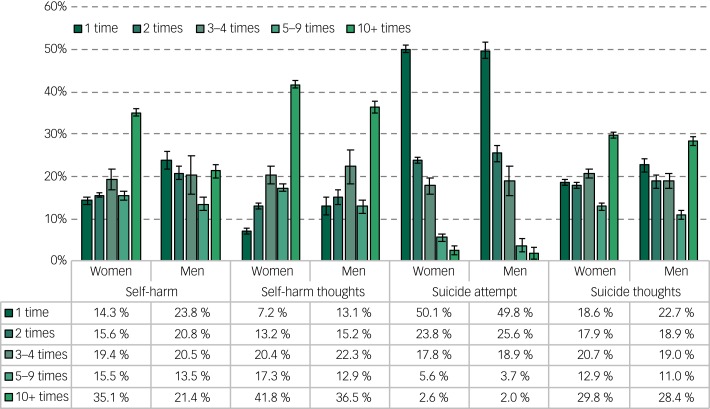
As detailed in Fig. 1, the majority of students who reported NSSH engaged in NSSH on multiple occasions. Among those reporting NSSH, a significantly larger proportion of women (35.1%, n = 2768) than men (21.4%, n = 331) reported repeated NSSH behaviour (defined as more than ten times). A similar pattern was observed for NSSH thoughts, with the 10+ category being the most frequently reported (see Fig. 1 for details).
Fig. 1.
Prevalence of non-suicidal self-harm, non-suicidal self-harm thoughts, suicide attempts and suicidal thoughts, stratified by gender.
Error bars represent 95% CIs.
Among those reporting a lifetime suicide attempt, 49% (n = 1041) had only done so once, whereas, 24% (n = 507) reported two suicide attempts. In contrast, 2.5% (n = 52) of students reporting a suicide attempt had done so ten times or more. These patterns were similar for both men and women. As also displayed in Fig. 1, there were no marked gender differences in the distribution of frequency of suicidal thoughts.
Age of first occurrences of NSSH, NSSH thoughts, suicide attempt and suicidal thoughts
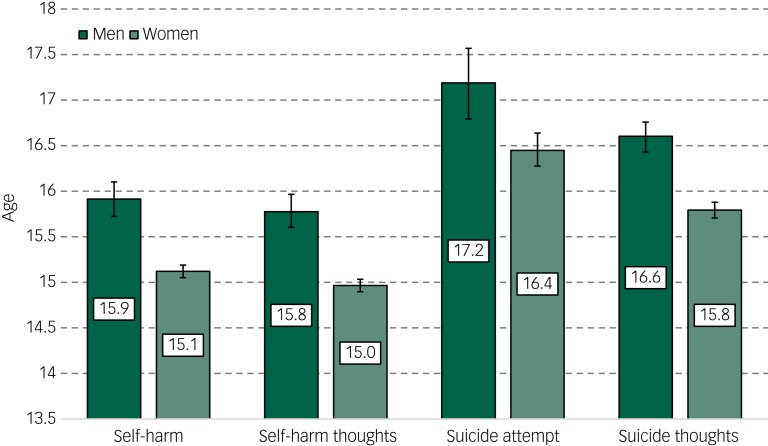
Students reporting NSSH were, on average, 15.2 years old when they first harmed themselves. As detailed in Fig. 2, women were younger (mean 15.1 years) than men (mean 15.9 years). Similar patterns were observed for NSSH thoughts. Students reporting a suicide attempt were, on average, 16.6 years old when they first attempted, compared with 16.0 years old when they first had thoughts of suicide. Women were an average of 0.8 years younger than men when they had their first occurrence of both a suicide attempt and suicidal thoughts.
Fig. 2.
Age in years of first occurrence of non-suicidal self-harm, non-suicidal self-harm thoughts, suicide attempts and suicide thoughts by gender.
Error bars represent 95% CIs.
Recent NSSH, NSSH thoughts, suicide attempts and suicidal thoughts across age groups
The prevalence of both NSSH and NSSH thoughts reported within the past 12 months decreased significantly in the older age groups. While 4.6% of the students aged 18–23 years reported past year NSSH, only 2.0% of those aged between 30 and 35 reported this. Similarly, while 9.7% of students aged 18–23 years reported recent NSSH thoughts, 6.4% reported this in the oldest age group. In contrast, there were no significant age differences in the prevalence of past year suicide attempt, or suicidal thoughts (see Table 1 for details).
Sociodemographic characteristics and suicidal thoughts, suicide attempts and NSSH and NSSH thoughts
As detailed in Table 2, compared with students living with others, students living alone had significantly higher rates of both past year suicidal thoughts (10.2% v. 6.4%), suicide attempts (0.8% v. 0.4%), NSSH thoughts (11.8% v. 8.2%) and NSSH (5.5% v. 3.7%). Similar effects were observed for relationship status, where single students had higher rates of recent suicidal thoughts (8.7% v. 5.7%), suicide attempts (0.6% v. 0.3%), NSSH thoughts (9.8% v. 8.0%) and NSSH (4.5% v. 3.6%) compared with students in a relationship.
Table 2.
Rates of suicidal thoughts, suicide attempts, non-suicidal self-harm (NSSH) thoughts and NSSH by sociodemographic characteristics
| Suicidal thoughts | Suicide attempts | NSSH thoughts | NSSH | |||||
|---|---|---|---|---|---|---|---|---|
| Lifetime | Past year | Lifetime | Past year | Lifetime | Past year | Lifetime | Past year | |
| Accommodation | ||||||||
| Lives with others, % (95% CI) (n = 40 379) | 19.8 (19.4–20.1) | 6.4 (6.2–6.7) | 3.9 (3.7–4.1) | 0.4 (0.3–0.4) | 21.8 (21.4–22.2) | 8.2 (7.9–8.5) | 19.0 (18.6–19.3) | 3.7 (3.6–3.9) |
| Lives alone, % (95% CI) (n = 9675) | 26.5 (25.6–27.3) | 10.2 (9.6–10.8) | 5.7 (5.2–6.1) | 0.8 (0.6–1.0) | 26.3 (25.4–27.2) | 11.8 (11.2–12.5) | 22.7 (21.9–23.6) | 5.5 (5.0–6.0) |
| Prevalence ratio | 1.34 | 1.59 | 1.46 | 2.00 | 1.21 | 1.44 | 1.19 | 1.49 |
| Relationship status | ||||||||
| Partner/married, % (95% CI) (n = 25 085) | 19.7 (19.2–20.2) | 5.7 (5.4–6.0) | 4.3 (4.1–4.6) | 0.3 (0.2–0–4) | 22.6 (22.1–23.2) | 8.0 (7.7–8.3) | 20.4 (19.9–20.9) | 3.6 (3.4–3.9) |
| Single, % (95% CI) (n = 24 969) | 22.4 (21.9–22.9) | 8.7 (8.3–9.0) | 4.2 (3.9–4.4) | 0.6 (0.5–0.7) | 22.8 (22.2–23.3) | 9.8 (9.4–10.2) | 18.9 (18.4–19.4) | 4.5 (4.3–4.8) |
| Prevalence ratio | 1.14 | 1.53 | 0.98 | 2.00 | 1.01 | 1.23 | 0.93 | 1.25 |
| Economic activity | ||||||||
| Economically active, >10 000 NOK, % (95% CI) (n = 43 600) | 20.0 (19.6–20.3) | 6.5 (6.3–6.8) | 3.9 (3.7–4.1) | 0.4 (0.3–0.5) | 21.8 (21.5–22.2) | 8.3 (8.1–8.6) | 18.9 (18.5–19.3) | 3.7 (3.5–3.8) |
| Economically inactive, % (95% CI) (n = 6245) | 28.7 (27.6–29.8) | 11.6 (10.8–12.4) | 6.5 (5.8–7.1) | 0.8 (0.6–1.0) | 28.6 (27.5–29.8) | 12.8 (12.0–13.6) | 25.2 (24.1–26.3) | 6.9 (6.3–7.5) |
| Prevalence ratio | 1.44 | 1.78 | 1.67 | 2.00 | 1.31 | 1.54 | 1.33 | 1.86 |
| Ethnicity | ||||||||
| Ethnic Norwegian, % (95% CI) (n = 46 044) | 20.7 (20.4–21.1) | 7.0 (6.7–7.2) | 4.0 (3.8–4.2) | 0.4 (0.3–0.5) | 22.5 (22.1–22.9) | 8.8 (8.5–9.1) | 19.7 (19.3–20.1) | 4.0 (3.9–4.2) |
| Immigrant, % (95% CI) (n = 4010) | 24.8 (23.4–26.1) | 9.5 (8.6–10.4) | 6.7 (5.9–7.5) | 0.9 (0.6–1.2) | 25.1 (23.7–26.4) | 10.2 (9.3–11.1) | 19.4 (18.1–20.6) | 4.4 (3.8–5.1) |
| Prevalence ratio | 1.20 | 1.36 | 1.68 | 2.25 | 1.12 | 1.16 | 0.98 | 1.10 |
NOK, Norwegian Krone.
In terms of economic activity, students with little or no additional income (beyond student loans and scholarships) had higher rates of both recent suicidal thoughts (11.6% v. 6.5%), suicide attempts (0.8% v. 0.4%), NSSH thoughts (12.8% v. 8.3%) and NSSH (6.9% v. 3.7%).
Finally, compared with ethnic Norwegians, immigrants had higher rates of both recent suicidal thoughts (9.5% v. 7.0%), recent suicide attempts (0.9% v. 0.4%) and recent NSSH thoughts (10.2% v. 8.8%), but not recent NSSH.
Trends in suicidal thoughts from 2010 to 2018
The PPV and NPV of the dichotomous suicidal thoughts item from the HSCL-25 (‘quite a bit’ and ‘extremely’ versus ‘not at all’ and ‘a little’) with regards to the dichotomous suicidal thoughts item from the APMS instrument were 81.5 and 81.1, respectively.
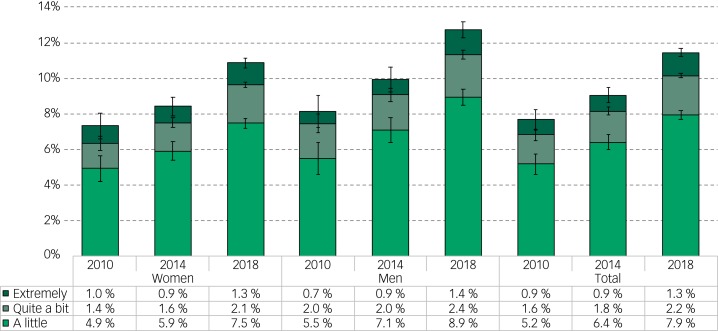
Figure 3 shows the prevalence of suicidal thoughts across all three SHoT studies from 2010 to 2018. There was a significant overall increase in students reporting suicidal thoughts (‘a little’, ‘quite a bit’ or ‘extremely’) from 2010 (7.7%) to 2014 (9.1%) to 2018 (11.4%; χ2= 62.8 (d.f. = 2, n = 69 119) P<0.001). The increase was significant in both genders (P<0.001), The increase was evident in both men and women, and across all three response categories (especially from 2014 to 2018 for ‘extremely’; see Fig. 3 for details).
Fig. 3.
Prevalence of suicidal thoughts from 2010 to 2018 by gender.
Error bars represent 95% CIs.
Sensitivity analyses, including only the institutions included in all three surveys, gave overall near-identical results.
Discussion
This large national survey from 2018, in which all full-time Norwegian university and college students aged 18–35 were invited to participate (response rate 31%), showed that suicide attempts and NSSH among Norwegian college and university students are prevalent. More than one in five students reported lifetime suicide thoughts (21%), NSSH thoughts (23%) as well NSSH behaviours (20%). Around 4% had attempted to take their own life. The prevalence rates of both suicidal thoughts and NSSH were higher among women, as well as among students who were single, living alone, with a lower annual income and among immigrants. There was a significant increase in suicidal thoughts from 2010 (7.7%) to 2018 (11.4%), and the increase was evident in both men and women.
The current study used a similar operationalisation of suicide attempts and NSSH as a recent Scottish prevalence study8 of young adults aged 18–34 years, as well as an English study of 16- to 24-year-olds.20 Although the prevalence of lifetime suicide attempts was notably lower in the current study (4.2%), compared with both the Scottish (11.3%) and English study (9%), the level of NSSH was at a similar level, or slightly higher, in Norway (19.7%), compared with Scotland and England (16.2% and 17.5%, respectively).
Regarding the observed gender differences, we observed similar prevalence ratios between men and women for both suicidal thoughts and attempts compared with the Scottish study. However, the gender differences were notably larger for NSSH in the current study (prevalence ratios 2.3–2.4 higher for women), compared with the Scottish study (prevalence ratios 1.5–1.8 for women).8 Of interest, we also found that the prevalence of recent NSSH (happening within the past year) was highest in the youngest age cohort (18–23 years), and decreased in the older cohorts. Several explanations are possible for this observed age difference, including a ‘healthy survivor effect’ in which the healthiest students pursued long-term education, a differential study participation by age, cohort differences in perception of and/or reporting of NSSH behaviour. The age findings reported herein mirror the previously reported developmental pattern in NSSH behaviour.10 However, this age effect was not found for suicide attempts, which goes against the mentioned ‘healthy survivor’ interpretation. As NSSH is known to peak in the teenage years,1 this may explain the differential effect.
It should be noted that the samples differed across the three studies. Whereas the Scottish and English studies included adolescents/young adults recruited from the general population, the current study included only a student population, skewing the present sample socioeconomically (higher) and potentially contributing to the higher rates of NSSH found. In terms of previous Norwegian studies, similar rates of lifetime suicide attempt (4%) were reported in a Norwegian study of adults aged 18–65 years,21 whereas in a web-based survey of young adults (average age 25.5 years) the lifetime prevalence of self-harm was 28%.22
Methodological considerations
A notable limitation of the present study is the modest response rate. As response rates are particularly important in prevalence studies, great care should be taken when generalising the current findings to the whole student population. Rather, it may be more appropriate to emphasise the relative differences between men and women, as well as different age cohorts and sociodemographic factors found in the current study, as these estimates are less prone to selection bias. It is possible that the use of a web-based survey approach contributed to the low response rate, as electronic platforms typically yield lower overall participation rates when compared with traditional postal mail approaches, such as paper-based surveys or face-to-face interviews.23 Related to this is the 69% female composition of the participants, which may represent a bias for the overall estimates, as women generally report worse health across most parameters compared with men. The strengths of the present study include the combination of very large sample size, and the inclusion of an established instrument assessing suicide attempts and NSSH.
Study implications
The findings have notable clinical implications, as they call attention to both the observed high level of suicide attempts and NSSH in this age cohort, as well as identifying important sociodemographic high-risk groups. Regarding the prevalence, further research, preferably registry linkage studies, is needed to confirm whether the observed level is representative of the total student population. Importantly, and consistent with O'Connor et al's Scottish study,8 among those students reporting NSSH and suicide attempts, the majority had done so on multiple occasions, which underscores the importance of clinicians being vigilant when students present with a history of suicide attempts or NSSH. It is also concerning that, consistent with McManus et al,17 the rates of suicidal thoughts also appear to have increased in recent years. Further research is required to investigate the factors that may account for this increase. Given the strong link to future suicide,1 clinicians should also assess potential risk factors that may increase the likelihood of self-injurious behaviours.
Our finding that suicide attempts and NSSH are more common among single and poor students, as well as among students with non-Norwegian ethnicity, have obvious implications both from a public health perspective, but especially for student welfare organisations. Concerning those defined as immigrants, it should be noted that this group is heterogeneous. Specifically, they have immigrated from many different countries, their reasons for immigration differ, as does their length of stay in Norway. These are all factors associated with adverse health outcomes, and likely also associated with NSSH. As emphasised in the Scottish study, prospective data are needed to establish the direction of association between such sociodemographic factors and suicide attempts and NSSH. Still, the findings are in line with existing studies showing a consistent social gradient across health measures, including in relatively egalitarian societies, such as Norway.
Acknowledgements
We wish to thank all students participating in the study, as well as the three largest student welfare associations in Norway (SiO, Sammen, and SiT), who initiated and designed the SHoT study.
Funding
SHoT2018 has received funding from the Norwegian Ministry of Education and Research (2017) and the Norwegian Ministry of Health and Care Services (2016).
References
- 1.Hawton K, Saunders KE, O'Connor RC. Self-harm and suicide in adolescents. Lancet 2012; 379: 2373–82. [DOI] [PubMed] [Google Scholar]
- 2.Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet 2016; 387: 1227–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry 2014; 1: 73–85. [DOI] [PubMed] [Google Scholar]
- 4.Chan MK, Bhatti H, Meader N, Stockton S, Evans J, O'Connor RC, et al. Predicting suicide following self-harm: systematic review of risk factors and risk scales. Br J Psychiatry 2016; 209: 277–83. [DOI] [PubMed] [Google Scholar]
- 5.Cooper J, Kapur N, Webb R, Lawlor M, Guthrie E, Mackway-Jones K, et al. Suicide after deliberate self-harm: a 4-year cohort study. Am J Psychiatry 2005; 162: 297–303. [DOI] [PubMed] [Google Scholar]
- 6.Kapur N, Cooper J, O'Connor RC, Hawton K. Non-suicidal self-injury v. attempted suicide: new diagnosis or false dichotomy? Br J Psychiatry 2013; 202: 326–8. [DOI] [PubMed] [Google Scholar]
- 7.Klonsky ED, May AM, Glenn CR. The relationship between nonsuicidal self-injury and attempted suicide: converging evidence from four samples. J Abnorm Psychol 2013; 122: 231–7. [DOI] [PubMed] [Google Scholar]
- 8.O'Connor RC, Wetherall K, Cleare S, Eschle S, Drummond J, Ferguson E, et al. Suicide attempts and non-suicidal self-harm: national prevalence study of young adults. BJPsych Open 2018; 4: 142–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Preventing Suicide: A Global Imperative. WHO, 2014. [Google Scholar]
- 10.Plener PL, Schumacher TS, Munz LM, Groschwitz RC. The longitudinal course of non-suicidal self-injury and deliberate self-harm: a systematic review of the literature. Borderline Personal Disord Emot Dysregul 2015; 2: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jessor R, Donovan J, Costa F. Beyond Adolescence: Problem Behavior and Young Adult Development. Cambridge University Press, 1991. [Google Scholar]
- 12.Bachman J, Johnston L, O'Malley P, Schulenberg J. Transitions in drug use during late adolescence and young adulthood In Transitions Through Adolescence: Interpersonal Domains and Context (eds Graber J, Brooks-Gunn J, Petersen A): 111–40. Lawrence Erlbaum Associates, Inc, 1996. [Google Scholar]
- 13.Boles SA. A model of parental representations, second individuation, and psychological adjustment in late adolescence. J Clin Psychol 1999; 55: 497–512. [DOI] [PubMed] [Google Scholar]
- 14.Arnett JJ. Emerging adulthood – a theory of development from the late teens through the twenties. Am Psychol 2000; 55: 469–80. [PubMed] [Google Scholar]
- 15.Mortier P, Cuijpers P, Kiekens G, Auerbach RP, Demyttenaere K, Green JG, et al. The prevalence of suicidal thoughts and behaviours among college students: a meta-analysis. Psychol Med 2018; 48: 554–65. [DOI] [PubMed] [Google Scholar]
- 16.Sivertsen B, Råkil H, Munkvik E, Lønning K. Cohort profile: the SHoT-study, a national survey of all Norwegian university students. BMJ Open 2019; 9: e025200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McManus S, Bebbington P, Jenkins R, Brugha T. Mental Health and Wellbeing in England: Adult Psychiatric Morbidity Survey 2014. NHS Digital, 2016. [Google Scholar]
- 18.Madge N, Hewitt A, Hawton K, de Wilde EJ, Corcoran P, Fekete S, et al. Deliberate self-harm within an international community sample of young people: comparative findings from the Child & Adolescent Self-harm in Europe (CASE) Study. J Child Psychol Psyc 2008; 49: 667–77. [DOI] [PubMed] [Google Scholar]
- 19.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci 1974; 19: 1–15. [DOI] [PubMed] [Google Scholar]
- 20.McManus S, Hassiotis A, Jenkins R, Dennis M, Aznar C, Appleby L. Suicidal thoughts, suicide attempts and self-harm In Mental Health and Wellbeing in England: Adult Psychiatric Morbidity Survey 2014 (eds McManus S, Bebbington P, Jenkins R, Brugha T). NHS Digital, 2016. [Google Scholar]
- 21.Hjelmeland H, Knizek B. Suicide is not an alternative: attitudes towards suicide and suicide prevention among mental health professionals, students and lay people in Norway. Tidsskr Norsk Psykologfore 2010; 47: 908–15. [Google Scholar]
- 22.Straiton ML, Roen K, Hjelmeland H. Gender roles, suicidal ideation, and self-harming in young adults. Arch Suicide Res 2012; 16: 29–43. [DOI] [PubMed] [Google Scholar]
- 23.Dykema J, Stevenson J, Klein L, Kim Y, Day B. Effects of E-mailed versus mailed invitations and incentives on response rates, data quality, and costs in a web survey of university faculty. Soc Sci Comput Rev 2013; 31: 359–70. [Google Scholar]