Abstract
Objectives:
Anxiety regarding dental procedures is a universal challenge for every patient and the treating dental surgeon. Measurement of heart rate, blood pressure, and oxygen saturation is now commonly accepted by the scientific community as an accurate and objective measurement of the patient's anxiety compared to other subjective assessments. The aim of this study was to assess the influence of educational videos demonstrating transalveolar extraction of mandibular third molars on hemodynamic parameters.
Materials and Methods:
The study was designed as a prospective clinical trial. The modified dental anxiety scale was used to assess the preoperative anxiety of the patient. Participating patients were divided randomly into two groups (verbal and video group). Each patient's hemodynamic parameters such as heart rate, blood pressure, and oxygen saturation were measured in the waiting area, sitting on the dental chair, incision, bone drilling, tooth elevation, suturing, and in the postoperative area. All the analysis was done using the SPSS version 18 software.
Results:
Overall, there were no significant differences between the two groups with respect to hemodynamic parameters. The mean heart rate and blood pressure of patients between both groups were comparatively consistent and did not very much from the onset of procedure to the end. On the other hand, oxygen saturation levels were statistically significantly higher in the video group at the onset of incision and drilling.
Conclusions:
Videos can be interpreted in different ways by patients. Overall, hemodynamic parameters are overall not influenced with videos.
KEYWORDS: Anxiety, extraction, heart rate, hemodynamic parameters, third molar, video
INTRODUCTION
Transalveolar extraction involves the removal of an impacted mandibular third molar often with the minor drilling of bone and sectioning of the crown under local anesthesia. Despite adequate reassurance, explanation, and precautions, transalveolar extractions continue to be associated with significant psychological stress, fear, and anxiety. Anxiety in the patient adds additional stress to all health-care professionals and further results as barriers to patient's returning for further dental care; strains the patient–doctor trust and relationship, and can further result in a prolonged treatment time, longer postoperative pain, and larger doses of analgesics.[1] Distressing emotions alter the neurovascular functions of the patient resulting in detrimental consequences of pain, ulcerations, and other adverse effects which are palpably displayed with the sensitive oral mucosa.[2]
Heart rate variability is influenced by the physiological counterplay between the sympathetic and parasympathetic nervous systems. This hemodynamic parameter has been acclaimed by previous authors as a credible way to assess stress levels during dental research.[3,4] However, this can be influenced by age, medications (e.g., beta blockers, benzodiazepines, and calcium channel blockers), thyroid disease, and other pathology.
The past research has been conducted, utilizing stress relieving techniques such as aromatherapy with ambient orange fragrance, PowerPoint presentations, videos, and anxiety surveys as nonpharmacologic stress releasing techniques in the dental setting.[5,6,7]
The purpose of this study was to assess the influence of an educational nonanimated procedural video that demonstrated transalveolar extraction of mandibular third molars on the patient's hemodynamic parameters. The hypothesis proposed was that there would be no significant difference in the hemodynamic parameters between verbal and video groups (null hypothesis).
MATERIALS AND METHODS
This prospective, randomized controlled trial was conducted over a period of 6 months (February 2018 to July 2018) among individuals visiting the oral and maxillofacial surgery outpatient department. Inclusion criteria were: individuals aged between 18 and 40 years, those required removal of a mandible third molar under local anesthesia, and those willing to participate. Participants with decompensated systemic diseases as a serious contraindication to dental treatment, prior history of transalveolar extraction, hypertension with or without medications, and comprehension problems were excluded. The protocol was approved by the Institutional Ethics Committee, and informed consent was sought from all patients. The trial was registered with the clinical trial registry of India (CTRI/2018/04/013031).
QUESTIONNAIRE MEASUREMENTS
Information on age, gender, and history of prior transalveolar extraction, any hypersensitivity or allergies were recorded in a structured format. A self-administered questionnaire was filled by patients that had five questions from the “modified dental anxiety scale” (MDAS). Previous studies have suggested that filling this questionnaire helps reduce anxiety overall, and is relatively easier to analyze, and promotes a better outcome.[8,9,10]
HEMODYNAMIC PARAMETERS
Heart rate and oxygen saturation were recorded over seven occasions (waiting area, sitting on the dental chair, incision, bone drilling, tooth elevation, suturing, and in the postoperative period) during transalveolar extractions of impacted mandibular third molars. The heart rate was assessed by the Mio Global Alpha 2 watch (Mio Alpha; Mio Global Physical Enterprises Inc., Vancouver, British Columbia, Canada) during the span of the procedure in the form of a linear graph with the Mio PAI Health app on the mobile phone with Bluetooth connection. The accuracy of this instrument has been reported to be equivalent to an electrocardiogram.[11,12] Oxygen saturation was recorded with the Oxee Check Pulse Oximeter (Romsons Scientific and Surgical Pvt. Ltd., 63 Industrial Estate, Nunhai, Agra, Uttar Pradesh, India) placed on the index finger. Blood pressure (systolic and diastolic) was measured 15 min before (preoperative period) and 15 min after the procedure (postoperative period) with a standard sphygmomanometer (Diamond, Industrial-Electronic and Allied Products, 34, Electronic Co-op Estate, Pune-Satara Road, Pune, Maharashtra, India).
STUDY DESIGN
Consented individuals were randomly divided into one of the two study groups (verbal or video group) [Figure 1]. Randomization was done using the table of random numbers, and a sequence was generated by one of the investigators (PKC). Individuals were enrolled and assigned to intervention by another investigator (RRS). Individuals were blinded until the allocation of groups. Researchers, operating surgeon, and outcome assessor were blinded throughout. Outcome assessment was done by one trained and calibrated recording clerk who was unaware of the participant's group status. Individual in the verbal group were explained about the nature of the procedure through verbal communication in a structured manner by one of the investigators (RRS). Individuals in the video group were made to watch a 10-min video clip that demonstrated transalveolar extraction of the impacted mandible third molar on a laptop. Individuals in the video group could stop, pause, or rewind the video accordingly. Individuals were subsequently asked to fill in the MDAS questionnaire after randomization and before undergoing the transalveolar extraction to check if the video or verbal interventions had any effect on the dental anxiety status. The sample size calculation was based on the findings from the previous study done on video watching on anxiety level.[6] A sample size of 26 (13 per group) was obtained after substituting the mean values of dental anxiety (immediately postoperative) which yielded an effect size of one with 80% power and confidence level of 0.05. We have not anticipated any dropouts owing to the study design, immediate outcome assessments, and lack of postoperative recall assessment.
Figure 1.
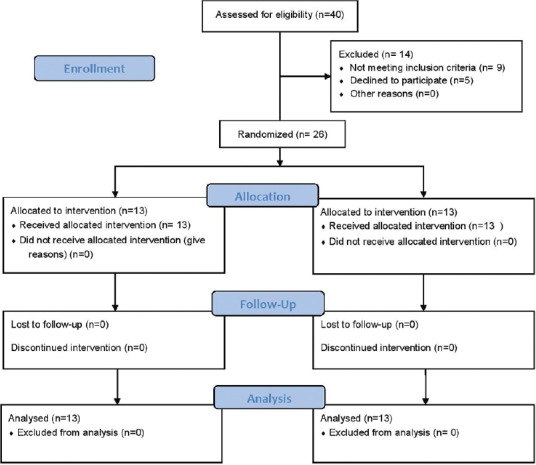
Consort flow chart
PROCEDURE FOR TRANSALVEOLAR EXTRACTION
One experienced oral surgeon (SG) performed the extractions and was unaware about the group allocation. An incision was made with No. 15 Bard–Parker Blade beginning at the external oblique ridge and extending it to the distal aspect of the second molar with careful attention to the anatomical proximity of the lingual nerve. If there was a greater requirement for further exposure, the incision was extended up to the first molar. Then, a vertical releasing incision was made in an oblique direction downward and forward through the vestibular tissues, hence creating the triangular flap. The mucoperiosteal flap was reflected as per the incision. After adequate exposure of the impacted tooth was obtained, any bone hindrance situated along the extraction path was removed with the micromotor handpiece and round bur; generous amount of saline irrigation was used during bone removal. Then, a groove was created around the buccal and distal aspect of the impacted tooth, allowing adequate stability during luxation of the impacted tooth. The impacted tooth's crown was sectioned as per the root morphology of the third molars in a buccal-lingual direction. This allowed the straight elevator to be placed between the sections of the crown creating a fulcrum of rotation to separate the parts of the tooth with sufficient force. The osteotome and mallet were utilized only when required. The straight elevator was used to luxate the separated parts of the tooth. Afterward, the fractured parts of the tooth were placed together to determine if any fragments were left behind. The extraction site was irrigated, and any remnants of follicle tissue and bone were curetted followed by silk sutures (3–0). Postoperative antibiotics and analgesics (tablet amoxicillin and clavulanic acid 625 mg t.i.d/5 days, tablet diclofenac t.i.d/5 days, and tablet metronidazole 400 mg t.i.d/3 days) were prescribed as per standard protocol.
STATISTICAL ANALYSIS
All the analysis was done using the Statistical Package for the Social Sciences version 18 (SPSS Inc., Ill, Chicago, USA).P < 0.05 was considered statistically significant. Intragroup comparison of mean values was done using repeated measures ANOVA/paired t-test. Intergroup comparisons were done using independent sample t-test. Categorical variables were compared using the Chi-square test.
RESULTS
A total of 26 patients (13 in each group) agreed to participate in this trial. The mean age in video and verbal group was 25.46 ± 3.43 and 23.31 ± 3.99 years (P = 0.153), respectively. The video group consisted of 7 females (53.8%), while the verbal group had 9 females (69.2%). No significant differences were seen with respect to gender distribution between video and verbal groups (P = 0.42). The comparison of dental anxiety status at baseline before the transalveolar extraction (MDAS) showed no significant differences in the mean MDAS scores in the verbal (11.54 ± 2.6) and video groups (11.85 ± 3.98; P = 0.817).
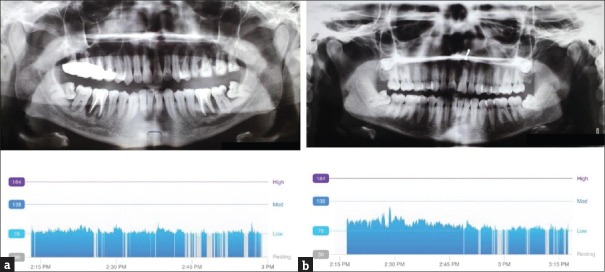
There were no significant differences in the mean heart rate between the verbal and video groups at waiting area, on dental chair, at incision, drilling, elevation of flap, suturing, and postoperative waiting area (P = 0.096, 0.373, 0.581, 0.376, 0.717, 0.369, and 0.368), respectively. Similarly, there was no significant difference in the mean heart rate from the “waiting area” through “postoperative waiting area” among the video and verbal groups (P = 0.536 and 0.126), respectively [Table 1 and Figure 2].
Table 1.
Inter- and intra-group comparisons of heart rate
| Heart rate | Group, mean±SD | P† | |
|---|---|---|---|
| Video | Verbal | ||
| Waiting area | 92.15±15.37 | 83.15±10.75 | 0.096 |
| Dental chair | 85.46±11.08 | 92.69±26.51 | 0.373 |
| Incision | 92.31±16.27 | 96.62±22.51 | 0.581 |
| Drilling | 102.38±33.42 | 92.54±20.80 | 0.376 |
| Elevation | 100.23±33.73 | 96.46±14.95 | 0.717 |
| Suturing | 94.85±30.45 | 85.23±22.50 | 0.369 |
| Postoperative | 90.92±30.13 | 82.92±8.86 | 0.368 |
| P‡ | 0.536 | 0.126 | |
‡P-value from repeated measures ANOVA; †P-value from independent sample t-test. SD=Standard deviation
Figure 2.
(a) Heart rate of one patient in verbal group during the transalveolar extraction of 32. (b) Heart rate of one patient in video group during the transalveolar extraction of 32
No significant differences in the mean oxygen saturation levels were seen between the verbal and video groups at waiting area, on dental chair, elevation of flap, suturing, and postoperative waiting area (P = 0.508, 0.174, 0.102, 0.136, and 0.164), respectively. However, there were a significant higher mean oxygen saturation readings in the video group than the verbal group at incision and drilling (P = 0.02 and 0.017), respectively. There were no significant differences in the mean oxygen saturation from the “waiting area” through “postoperative waiting area” among the video and verbal groups (P = 0.282 and 0.105), respectively [Table 2].
Table 2.
Inter- and intra-group comparisons of oxygen saturation
| Oxygen saturation | Group, mean±SD | P† | |
|---|---|---|---|
| Video | Verbal | ||
| Waiting area | 98.23±0.73 | 98.00±1.00 | 0.508 |
| Dental chair | 98.23±0.83 | 97.69±1.11 | 0.174 |
| Incision | 98.46±0.66 | 96.92±2.02 | 0.02 |
| Drilling | 98.46±0.66 | 97.08±1.75 | 0.017 |
| Elevation | 98.23±0.73 | 97.38±1.61 | 0.102 |
| Suturing | 98.38±0.77 | 97.31±2.39 | 0.136 |
| Postoperative | 98.15±0.80 | 97.38±1.76 | 0.164 |
| P‡ | 0.282 | 0.105 | |
‡P value from repeated measures ANOVA; †P value from independent sample t-test. SD=Standard deviation
Intergroup comparisons of mean systolic blood pressure before and after the procedure between verbal and video groups showed no significant difference (P = 0.29 and 0.383), respectively. A similar trend was seen with respect to mean diastolic blood pressure (P = 0.296 and 0.415). No significant difference was seen with respect to mean systolic and diastolic blood pressure before and after in with the video group (P = 0.054 and 0.054), respectively. Similarly, a trend was seen in the verbal group (P = 0.475 and 0.499), respectively [Table 3].
Table 3.
Inter- and intra-group comparisons of blood pressure (systole and diastole)
| Blood pressure | Group, mean±SD | P† | |
|---|---|---|---|
| Video | Verbal | ||
| Systole before | 125.54±9.06 | 121.69±9.06 | 0.29 |
| Systole after | 123.23±7.28 | 120.54±8.13 | 0.383 |
| P‡ | 0.054 | 0.475 | |
| Diastole before | 79.69±5.09 | 82.00±5.89 | 0.296 |
| Diastole after | 78.92±4.44 | 80.92±7.47 | 0.415 |
| P‡ | 0.054 | 0.499 | |
‡P value from paired t-test; †P value from independent sample t-test. SD=Standard deviation
DISCUSSION
Hemodynamic parameters are relied on by health practitioners to aid in their diagnosis and treatment planning. As a result, health practitioners are now expected to have a thorough knowledge about the influence of technology on these parameters and anxiety. Overall, there were no significant differences in hemodynamic parameters (heart rate, oxygen saturation, and blood pressure) between both groups (verbal and video group). This is clinically significant because this may provide health-care practitioners the opportunity to utilize videos more often as an educational intervention to manage dental anxiety.
Patients are frequently hesitant to discuss their fears with the dentist. Inadequate education regarding the treatment procedure has been reported as the third most common anxiety provoking factor in the preoperative period in oral surgery.[6] It is therefore of paramount importance to educate patients on all aspects of the treatment through some means. The verbal discussion has been the usual method but is variable depending on the surgeon's eloquence, available time, patient's language skills, level of cognition, and hearing. Videos are a significant educational asset conveying information to all despite barriers in linguistics and literacy rates.[6] The use of video is versatile ranging from not only teaching patients but also being a beneficial educational asset to dental students.[13] Educational videos are a perfect example of the “tell-show-do” technique. This technique has no specific contraindications, and is suitable for any age range.[14] Although videos provide an overall summary of the procedure, individual variations must still be discussed with the patients.[15] Watching videos that show surgical field, instruments, bleeding, and operatory sound can be distressing for some patients, but coincidently helps their understanding of the procedure and eliminate any unanswered doubts. However, Kazancioglu et al. reported that patients who watched prior movies on the internet regarding oral surgical procedures demonstrated greater anxiety levels during the extraction compared to those who did not watch them.[6] On the other hand, Done and Lee reported that videos do not have major effect in altering the anxiety levels of patients before the anesthesia procedure, but patients who watched videos before the procedure were better informed and able to recollect information, later on, regarding risks and misconceptions.[15] Our results confirmed these findings.
Videos as an educational asset can be interpreted in dissimilar ways by different patients. In some patients, the procedural video can be distressing while others found it to be useful. One patient in our study did not want to continue with the treatment after watching 7 min of the 10-min video. While this refusal represents an exercise of freedom of consent based on adequacy of information, it could also be construed as a prospective introduction of unreasonable fear in the mind of the patient and defeats the purpose of health-care delivery. A future study could assess whether an animated video is better suited to inform the patient, because it may not show bleeding and surgical instruments. Similarly, another aspect that could also help would be showing the video several days before the procedure to allow time for patients to ask questions and compose their emotions.
Alemany-Martínez et al. assessed hemodynamic parameters and anxiety measured with Corah's Dental Anxiety Scale as well as Kleinknecht's Dental Fear Scale, before and during extraction of lower third molars.[16] They reported a statistically nonsignificant trend towards lower blood pressure but increased heart rate with increasing levels of anxiety. They also reported no significant changes in oxygen saturation before, during, or after the procedure. They concluded that deviations in blood pressure and heart rate are influenced by personal factors including age, gender, and prior dental experience. Our study found statistically significant higher oxygen saturations during incision and drilling in the video group. This is in line with the physiological response of the body to this stressful situation; this also introduces the need for identifying less distressing methods when performing core procedures, for instance, usage of nonpharmacological means or distraction methods for the patient (playing music in the room).
Nichols discussed the differences in blood pressure before and after dental procedures and found that systolic and diastolic blood pressure readings were higher before the procedure than afterward.[17] Our results confirmed this finding. This may be attributed due to increased physiological sympathetic activity and decreased arterial compliance. Furthermore, this is of clinical importance to dental practitioners, because lack of this knowledge could result in redundant physician consultations due to misdiagnosed “hypertension.”[17]
Some anticipated limitations were encountered during the clinical trial. Six patients required a second inferior alveolar nerve block compared to others due to anatomical variation. The procedures varied in time, as predicted, depending on the morphology of the mandible third molar which could not be standardized. Moreover, anxiety itself could not be evaluated in every phase of the procedure. Another limitation of our study was the lack of rest breaks. Rest breaks may be initiated either by the practitioner or the patient and overall promotes patient's autonomy.[14] In fact, they could have helped to counter the jaw fatigue. Patients were of different ages, which also could have an indirect role in their interpretation and resilience towards anxiety and the nature of these procedures; further studies can benefit by attempting to match patients as closely as possible in factors such as age and gender.
Overall, this study has further contributed to the controversial results regarding utilizing videos as a nonpharmacological anxiety relieving intervention. However, it has to be noted that the conflicting results between different studies may be due to the variations between procedures. Measuring the parameters through noninvasive interventions is always preferable compared to minimal invasiveness techniques. Furthermore, hemodynamic parameters may be difficult to compare overall because of no optimal values relevant to all patients.[18] A systematic review and meta-analysis on the role of educational interventions in mitigating hemodynamic parameters and anxiety would help us draw conclusive evidence on this controversy.
CONCLUSION
The results of the study did collaborate with our proposed hypothesis. Anxiety cannot be pinpointed to one specific factor type but is influenced by numerous internal and external factors. The use of educational nonanimated videos could be inferred by patients in different ways. Our study found that hemodynamic parameters are not mitigated or exacerbated through the use of videos.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Wang TF, Wu YT, Tseng CF, Chou C. Associations between dental anxiety and postoperative pain following extraction of horizontally impacted wisdom teeth: A prospective observational study. Medicine (Baltimore) 2017;96:e8665. doi: 10.1097/MD.0000000000008665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suresh KV, Shenai P, Chatra L, Ronad YA, Bilahari N, Pramod RC, et al. Oral mucosal diseases in anxiety and depression patients: Hospital based observational study from South India. J Clin Exp Dent. 2015;7:e95–9. doi: 10.4317/jced.51764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Santana MD, de Souza AC, de Abreu LC, Valenti VE. Association between oral variables and heart rate variability. Int Arch Med. 2013;6:49. doi: 10.1186/1755-7682-6-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Le SH, Tonami K, Umemori S, Nguyen LT, Ngo LT, Mataki S, et al. The potential of heart rate variability for exploring dental anxiety in mandibular third molar surgery. Int J Oral Maxillofac Surg. 2018;47:809–15. doi: 10.1016/j.ijom.2018.01.019. [DOI] [PubMed] [Google Scholar]
- 5.Hasheminia D, Kalantar Motamedi MR, Karimi Ahmadabadi F, Hashemzehi H, Haghighat A. Can ambient orange fragrance reduce patient anxiety during surgical removal of impacted mandibular third molars? J Oral Maxillofac Surg. 2014;72:1671–6. doi: 10.1016/j.joms.2014.03.031. [DOI] [PubMed] [Google Scholar]
- 6.Kazancioglu HO, Tek M, Ezirganli S, Demirtas N. Does watching a video on third molar surgery increase patients’ anxiety level? Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119:272–7. doi: 10.1016/j.oooo.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 7.Choi SH, Won JH, Cha JY, Hwang CJ. Effect of audiovisual treatment information on relieving anxiety in patients undergoing impacted mandibular third molar removal. J Oral Maxillofac Surg. 2015;73:2087–92. doi: 10.1016/j.joms.2015.06.175. [DOI] [PubMed] [Google Scholar]
- 8.Humphris GM, Dyer TA, Robinson PG. The modified dental anxiety scale: UK general public population norms in 2008 with further psychometrics and effects of age. BMC Oral Health. 2009;9:20. doi: 10.1186/1472-6831-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acharya S. Factors affecting dental anxiety and beliefs in an Indian population. J Oral Rehabil. 2008;35:259–67. doi: 10.1111/j.1365-2842.2007.01777.x. [DOI] [PubMed] [Google Scholar]
- 10.Garcia-Blanco M, Gualtieri AF, Puia SA. A randomized controlled trial comparing nerve block and mandibular infiltration techniques in posterior mandible implant surgeries. J Clin Exp Dent. 2018;10:e1003–10. doi: 10.4317/jced.54330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hollander MH, Schortinghuis J, Vissink A. Changes in heart rate during third molar surgery. Int J Oral Maxillofac Surg. 2016;45:1652–7. doi: 10.1016/j.ijom.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Valenti G, Westerterp K. 2013 IEEE International Conference on Consumer Electronics (ICCE) Las Vegas, NV: 2013. Optical heart rate monitoring module validation study; pp. 195–6. [Google Scholar]
- 13.Naseri M, Shantiaee Y, Rasekhi J, Zadsirjan S, Mojtahed Bidabadi M, Khayat A. Efficacy of video-assisted instruction on knowledge and performance of dental students in access cavity preparation. Iran Endod J. 2016;11:329–31. doi: 10.22037/iej.2016.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Armfield JM, Heaton LJ. Management of fear and anxiety in the dental clinic: A review. Aust Dent J. 2013;58:390–407. doi: 10.1111/adj.12118. [DOI] [PubMed] [Google Scholar]
- 15.Done ML, Lee A. The use of a video to convey preanesthetic information to patients undergoing ambulatory surgery. Anesth Analg. 1998;87:531–6. doi: 10.1097/00000539-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Alemany-Martínez A, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Hemodynamic changes during the surgical removal of lower third molars. J Oral Maxillofac Surg. 2008;66:453–61. doi: 10.1016/j.joms.2007.06.634. [DOI] [PubMed] [Google Scholar]
- 17.Nichols C. Dentistry and hypertension. J Am Dent Assoc. 1997;128:1557–62. doi: 10.14219/jada.archive.1997.0096. [DOI] [PubMed] [Google Scholar]
- 18.Vincent JL, Rhodes A, Perel A, Martin GS, Della Rocca G, Vallet B, et al. Clinical review: Update on hemodynamic monitoring – A consensus of 16. Crit Care. 2011;15:229. doi: 10.1186/cc10291. [DOI] [PMC free article] [PubMed] [Google Scholar]