Abstract
Introduction:
The dentist must be aware of this drug use in their individual patients to: (1) avoid possible contraindications during dental treatment, (2) be aware of the many oral and craniofacial manifestations of such drug use, (3) be able to provide necessary dental treatment to combat the dental/oral ravages of drug use, and (4) be able to refer such patients, if so desired by the patient.
Aims and Objectives:
The aim of the study is (1) To determine the knowledge of abusive drugs among dentists and (2) To determine the attitude and role of dentists in identifying patients with abusive drugs.
Subjects and Methods:
A modified 27-item questionnaire was formulated and distributed among the study. The participants were to return the filled questionnaire to the investigators within a week. A total of 203 validated entries were collected. Data were entered into Microsoft Excel 2007 and analyzed in SPSS V20. Associations between categorical variables were determined using Chi-square or Fisher's exact test. P < 0.05 was considered statistically significant.
Results:
Irrespective of the educational qualification drugs are perceived harmful with definite oral manifestations, and dentists should be concerned with identifying individuals with drugs. It is believed that trying drugs once could lead to possible addiction and that dental practitioners should have their skills developed to handle cases and referred to deaddiction centers with modification of treatment plans.
Conclusions:
Educating dental graduates and postgraduates about the oral implications of drugs intake and making it a part of the dental curriculum may help us dealing with the global issues of drugs. Even making dental students a part in counseling and part of the behavioral therapies advocated in treating drug addicts.
KEYWORDS: Abusive drugs, awareness, education, oral manifestations, perception, social implications
INTRODUCTION
Drug is any biologic substance, artificial or natural, that is, ingested for unhealthy needs. It is conventionally incorporated and introduced into an individual to catalyze its action.[1,2] It is evaluated that approximately 153 million people aged between 15 and 64 years who give a history of substance use with 99,000–253,000 deaths globally. In India, about 3 million population report for different kinds of drug usage.[3,4]
Awareness usage and dependence pertaining to the illicit drugs have dramatically increased globally. They have become an immensely colossal phenomenon in the past two decades affecting all segments of society. There are numerous social, cultural, and financial facets associated with drug abuse.[5] The introduction of nuclear family, the absence of love and care where parents are working, waning of faith in religion, relationships, and ethical values has led to an increase in the quantity of addicts who take drugs to avoid unyielding facts of the life.[1]
Drugs are separated into two classes:
Drugs that reason extreme mental and physical habit such as heroin and cocaine
Drugs which have lessened the potential for mental and of physical compulsion such as liquor, amphetamines, nicotine, stimulants, caffeine, weed, natural solvents, and so on.[3]
These substances may be introduced into the humans orally (alcohol and pills) smoking or inhaling (marijuana, cocaine, opium), nasally (cocaine, heroin), and subcutaneously and intravenously (heroin and cocaine).[5]
The common reasons of abuse are the inquisitiveness as to how it feels and utilization by companions or associates. In some cases, the parents and siblings also play an important role directly or indirectly in influencing the youngsters. There is an idea among the users that drugs make one look up-to-date, happening and requirement for socialization.[6] The utilization is related with expanded danger of communal issues that incorporates illicit drugs trafficking, theft, and prostitution by addicts to back their habit. Drugs related with misused substances effects society, treatment costs, needle-sharing practice, prostitution, HIV transmission, and indisputable compelling diseases which compels therapeutic challenge for society.
These drugs have some numerous ill effects on oral mucosa which is directly dependent on the type and duration of use along with lifestyle of the users.[5] The common oral changes are: candidiasis, angular cheilitis, median rhomboid glossitis, frictional hyperkeratosis, candidal leukoplakia, xerostomia, gingivostomatitis, hairy tongue, aphthous stomatitis, herpes simplex, and bruxism.[7,8]
The importance of oral care among drug users necessitates implementation of a comprehensive dental care program. Integrated health-care services should be programmed for the management of drug addiction as a multiorgan disease needs a multidisciplinary approach.[9]
SUBJECTS AND METHODS
This was a descriptive cross-sectional questionnaire survey which was conducted among registered dental practitioners who either had BDS or MDS degrees.
A 36-item anonymous questionnaire was developed through thorough review of the literature which was pilot tested on 30 participants discussed, and peer reviewed among the investigators. The questionnaire was modified, and a 27-item questionnaire was distributed among the study. The participants were to return the filled questionnaire to the investigators within a week, 203 validated entries were collected. The sample size was selected based on the previous studies and keeping the power of the study as 80%. The Cronbach's alpha value for the questionnaire was found to be 0.8, and later modified accordingly to identify the lacunae. The inter- and intra-observer reliability was assessed with kappa value of 0.8 to avoid interviewer bias, the term abusive drugs were avoided and only drugs were used instead. The questionnaire was divided into seven sections.
Demographic details, knowledge of abusive drugs, perceived extent of the drug problem, perceived drug use among young people, perceived harm and dangers associated with illegal drug use, and attitudes toward drug addicts and designed to assess the role of the dentist in identifying dental patients with drug abuse.[2,10,11,12,13]
This study was conducted in agreement with the Ethical Committee guidelines under Siksha O Anusandhan University (DMR/IMS-SH/SOA/16023 dated May 27, 2016). The study protocol was discussed with the participants and possible measures were taken to ensure the confidentiality of all participants with proper informed consents.
STATISTICAL ANALYSIS
Data were entered into Microsoft Excel 2007 and analyzed in SPSS version 18.0 (SPSS Inc., Chicago, USA). All the categorical variables were expressed in terms of number and percentages. Associations between categorical variables were determined using Chi-square or Fisher's exact test. P < 0.05 was considered statistically significant.
RESULTS
A total of 203 participants were included in the study, out of which 54.7% were from <30 years’ age bracket. The mean age of the participants was 30.01 ± 6.37 years. More than one-third of them (70%) were female. Regarding educational level, 69.5% has a bachelor degree, and others had a master degree. A major proportion (40.9%) of them were involved in nonteaching private practices, and rest of them were either involved in the teaching profession in dental college or involved in both teaching and private practice [Table 1].
Table 1.
Demographic data
| Variables | n (%) |
|---|---|
| Age (years) | |
| <30 | 111 (54.7) |
| ≥30 | 92 (45.3) |
| Sex | |
| Male | 61 (30.0) |
| Female | 142 (70.0) |
| Educational qualification | |
| BDS | 141 (69.5) |
| MDS | 62 (30.5) |
| Job profile | |
| Teaching professional | 59 (29.1) |
| Nonteaching/private practitioner | 83 (40.9) |
| Both | 61 (30.0) |
KNOWLEDGE ABOUT ABUSIVE DRUGS USE
Most of the study participants recognized cocaine (91.6%) as the most common form of drug used by drug abusers, followed by heroin (75.9), cannabis (72.4), and ecstasy (36.9%). Less than one-fifth of the study participants mention Lysergic acid diethylamide (LSD) and amphetamine as illicit drugs. More than half of the study participants (58.6%) told that the use of such substances has an effect on oral cavity, 16.7% gave a negative response, and the rest were unsure about the effect of substance abuse [Figure 1].
Figure 1.
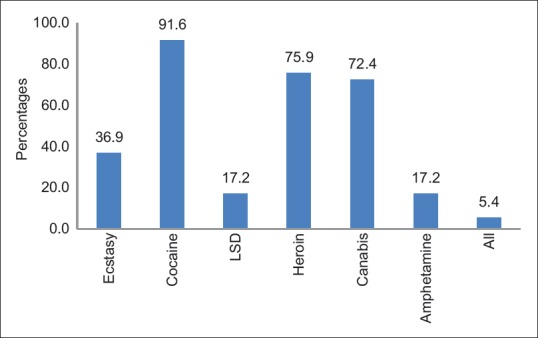
Type of drug use according to the study participants (n = 203)
PERCEIVED EXTENT OF THE DRUG PROBLEM
Regarding perceived problem/burden of drug abuse, most of the study participants (86.2%) denied drug abuse is a problem in there practice area. More than half (52.7%) of the study participants rated alcohol as a bigger problem than drug abuse. Almost one-fourth (24.6%) mentioned availability of illegal drugs pose threat to youth, and 38.4% said people are concerned. Around one-tenth (9.4%) of the study participant identified drug abuse related crime as a social issue [Table 2].
Table 2.
Perceived extent of the drug problem
| Yes (%) | No (%) | |
|---|---|---|
| Alcohol addiction causes more problems in society than drugs | 52.7 | 5.9 |
| Do you perceive drugs could be problematic at your area of practice | 86.2 | 13.8 |
| Drug usage and related crime is a major problem | 9.4 | 75.9 |
| Drugs causes economic compulsion | 24.6 | 65.5 |
PERCEIVED DRUG USE AMONG YOUNG PEOPLE
With respect to drug abuse problem among youth, most of the study participants rated cannabis (70.4%) as the most common form of substance abuse followed by ecstasy (65.5%). Around half of the study participants (45.3%) thought that it is normal to try drugs among youth, and almost similar proportion (48.3%) thought media exaggerated the drug abuse issue [Table 3].
Table 3.
Perceived Drug Use among Young People
| Yes (%) | No (%) | |
|---|---|---|
| Cannabis is the most popular drug | 70.4 | 8.9 |
| Youngsters are willing to try out ecstasy/LSD, etc., | 65.5 | 13.8 |
| Reports about the extent of drug usage among youngsters are exaggerated by the media | 45.3 | 18.7 |
| Does media influence youngsters to use drugs | 48.3 | 35.5 |
| It is normal that young people will try drugs at least once | 45.3 | 18.7 |
PERCEIVED HARM OF DRUG ABUSE
A higher proportion of participant possessing a master degree had mentioned all illegal drug are equally harmful when compared to participants with a bachelor degree and this difference showed a statistical significance (P = 0.017). They agreed trying drugs even once leads to addicted (P = 0.42). Other questions pertaining to perceived harm did not show any statistically significant difference [Table 4].
Table 4.
Perceived harm of drug abuse
| Educational_qualification | P | ||
|---|---|---|---|
| BDS, n (%) | MDS, n (%) | ||
| All drugs are equally harmful | |||
| Yes | 58 (59.8) | 39 (40.2) | 0.17 |
| No | 36 (72.0) | 14 (28.0) | |
| Unsure | 47 (83.9) | 9 (16.1) | |
| Trying drugs even once leads to addicted | |||
| Yes | 97 (68.8) | 44 (31.2) | 0.42 |
| No | 15 (62.5) | 9 (37.5) | |
| Unsure | 29 (76.3) | 9 (23.7) | |
| Use of drugs leads to physical and psychological imbalance | |||
| Yes | 74 (71.8) | 29 (31.7) | 0.63 |
| No | 11 (61.1) | 7 (38.9) | |
| Unsure | 56 (68.3) | 26 (31.7) | |
ATTITUDE OF DENTIST TOWARD DRUG ABUSERS
A higher proportion of the study participants having MDS degree mentioned drug abusers were victims, they were not given a fair chance in the society and were isolated (P = 0.50). About 6.5% of MDS participants thought drug addict himself are responsible for drug use as compared to only 22% of BDS participant, and 44% of MDS participants perceived addicts were threat to the society [Table 5].
Table 5.
Attitude towards drug abusers
| Educational_qualification | P | ||
|---|---|---|---|
| BDS, n (%) | MDS, n (%) | ||
| Are drug addict’s victims | |||
| Yes | 140 (69.3) | 62 (30.4) | 0.69 |
| Unsure | 1 (100) | 0 | |
| Are drug addict’s criminals | |||
| Yes | 84 (67.2) | 41 (32.8) | 0.65 |
| No | 43 (72.9) | 16 (27.1) | |
| Unsure | 14 (73.7) | 5 (26.3) | |
| Drug addicts are isolated | |||
| Yes | 134 (68.7) | 61 (31.3) | 0.50 |
| No | 1 (100.0) | 0 (0.0) | |
| Unsure | 6 (85.7) | 1 (14.3) | |
| Drug addicts are perceived threat to the society | |||
| Yes | 44 (68.8) | 20 (31.2) | 0.86 |
| No | 28 (66.7) | 14 (33.3) | |
| Unsure | 69 (71.1) | 28 (28.9) | |
ROLE OF DENTIST IN IDENTIFYING DENTAL PATIENTS WITH DRUG ABUSE
Irrespective of the educational qualification study, the participant agreed that drug abuser should be identified (P = 0.19) and all drugs have oral manifestations (P = 0.35). Majority of them agreed they have not encountered or identified patients on drugs (P = 0.34). Both groups of participants believed dental practitioners requires a modified treatment plan and have specialized skills to tackle such patients (P = 0.27). The dentist should allocate extra time to the patient and “listen him/her out” patients should be referred to deaddiction centers (P = 0.031) with modification of the treatment planning (P = 0.31) [Table 6].
Table 6.
Assess the role of dentist in identifying dental patients with drug abuse
| Educational qualification | P | ||
|---|---|---|---|
| BDS, n (%) | MDS, n (%) | ||
| Dentists should be concerned with identifying dental patients on drugs | |||
| Yes | 79 (72.5) | 30 (27.5) | 0.19 |
| No | 62 (66.0) | 32 (34.0) | |
| Do all drugs have an oral manifestation | |||
| Yes | 10 (62.5) | 6 (37.5) | 0.35 |
| No | 131 (70.1) | 56 (29.9) | |
| Have you encountered dental patients with drugs? | |||
| Yes | 68 (68.7) | 31 (31.3) | 0.34 |
| No | 73 (70.1) | 31 (29.8) | |
| Do you feel that dental practitioner’s skills have to be improved to help handle such cases? | |||
| Yes | 0.27 | ||
| No | 120 (70.6) | 50 (29.4) | |
| Unsure | 21 (63.6) | 12 (36.4) | |
| Dentist should allocate extra time to the patient and “listen him/her out” | |||
| Yes | 48 (64.9) | 26 (35.1) | 0.46 |
| No | 93 (72.1) | 36 (27.9) | |
| Dentist should refer the patient to deaddiction centers | |||
| Yes | 1 (20) | 26 (35.1) | 0.031 |
| No | 93 (72.1) | 36 (27.9) | |
| Do you feel that adequate communication is required between dental practitioners and medical practitioners/psychiatrists as well as the deaddiction centers regarding referred cases? | |||
| Yes | 12 (63.2) | 7 (36.8) | 0.91 |
| No | 129 (70.1) | 55 (29.9) | |
| Unsure | 141 (69.5) | 62 (30.5) | |
| According to your knowledge does drug abuse require any modification in the treatment planning? | |||
| Yes | 25 (71.4) | 10 (28.6) | 0.31 |
| No | 116 (69.5) | 51 (30.5) | |
| Unsure | 0 (0.0) | 1 (100) | |
| Do you think there are adequate deaddiction facilities in your state? | |||
| Yes | 110 (69.2) | 49 (30.8) | 0.96 |
| No | 13 (72.2) | 5 (27.8) | |
| Unsure | 18 (69.2) | 8 (30.8) | |
DISCUSSION
Teaching and awareness within the social media concerning the data of addiction in dental medicine is scarce. Prevailing articles and literature have targeted mostly on the deleterious effects of tobacco and to a minor extent on alcohol consumption.[10] Oral health implications, treatment modalities, counseling, and motivational interviewing techniques are more in giving support for quitting smoking and tobacco deaddiction.[11]
Cocaine was the most commonly recognized drug, and the least known being LSD and amphetamine. Literature shows cannabis and opioids are the most prominent substances of use in India, other substances are gradually emerging and slowly becoming popular. Because many of these substances can have life-threatening adverse effects, knowledge of general toxicology in recognizing acute intoxication and overdose; however, typical toxidromes (e.g., cholinergic, sympathomimetic, and opioid) are not precipitated by many of these agents.[12] Drugs are associated with serious oral health problems including decay, regressive alterations of teeth, mucosal irritation, and dryness of the mouth. Oral health care may be propagated for positive effects in recovery from drug abuse. Health-care programs worldwide deliver services but lack oral health-care programs.[9] Although majority of the study participant agreed these drugs had an effect on the oral cavity nothing was done for the same. The dental patient who has a history of substance abuse should be considered complex, considering most common oral manifestation of xerostomia, pain control, caries risk, noncarious tooth surface loss, soft tissue damage, predisposition to periodontal disease, and temporomandibular disorders.
The recognition and treatment of new drugs of abuse pose many challenges for health-care providers due to lack of quantitative reporting and routine surveillance, and the difficulty of detection in routine blood and urine analyzes.
In this study, the levels of acceptability and awareness of drugs were assessed among the dental practitioners. Here, majority of the participants were females of a mean age of 30 years, a female predominance was seen suggesting that India is following the trend where enrolment of students into dental education is about 50%–60%, and 15% of the heads in dental colleges across the country are females.[11] The sample comprised of both master's and bachelor's degree showing a predominance in bachelors and private dental practicing dentists.[12]
Of oral health care include practitioner scepticism, associated psychological factors, and perceptions.[13] Thus, its effect on the oral cavity cannot be denied.
Similarly, alcohol consumption is a risk factor in 25 chronic diseases and conditions, and alcohol plays a significant role in certain cancers, psychiatric conditions, and numerous cardiovascular and digestive diseases. In addition, alcohol consumption can increase the risk of diabetes, stroke, and heart disease. Thus, majority of the participants denied drugs to cause any problems in their practice area with alcohol being to cause bigger issues than drugs. It has been reported that alcohol kills more teenagers than all other drugs combined. Suggesting lack of awareness or ignorance among the participants of the effects of drugs.[14] Therefore, there was no stepped categorical distinction in harm between the different legal and illegal substances. Heroin was viewed as the most harmful, and cannabis the least harmful of the substances studied. Alcohol was ranked as the fourth most harmful substance, with alcohol, nicotine and volatile solvents being viewed as more harmful than some class A drugs.[15]
The media's influence on teen substance abuse is both subtle and distinct and cannot be denied which is in accordance to the findings. Impressions are made both consciously and subconsciously, as a result of constant exposure to media images in innumerable forms. Time to thoughtfully analyze a depiction or advertisement with a group of kids and introduce them to the ideas of emotional and psychological manipulation. Many teens are curious, and figure anything is worth a try. The problem is, once that realm is entered into, it becomes much easier to try other things which are destructive to their health and well-being. Of course, we all know that substance abuse and addiction can ruin relationships, careers, the ability to reason, etc., but that is only part of the problem. Young people who get involved with substance abuse is statistically more likely to acquire serious health problems later in life including stroke, liver disease, heart disease, and cancer.[14,15]
The finding that more educated participants rated some substances to be less harmful (heroin, cannabis, dextropropoxyphene, and raw opium) suggests that they might be more aware of the actual risks involved with these substances than mere portrayal. Lower harm rating of cannabis and raw opium by rural residents may be attributed to these products being used for a long time and being easily available in the rural setting, less restrictive enforcement, and ethnographic acceptance.[16]
Attitudes toward drug addicts are not exaggerated as drugs of diverse pharmacological classes induce alterations in social behavior, although they can be contrasting depending on several factors (drug, individual differences, and environmental conditions). Ethanol and nicotine increase the social interaction at low doses, but reduce it at high doses. Psychostimulants, 3,4-Methyl enedioxy methamphetamine (MDMA), and cannabinoids reduce social interaction, whereas opiates increase it. Ethanol and psychostimulants enhance aggression, whereas MDMA, opiates, cannabinoids, and nicotine reduce it. Prenatal drug exposure alters social behavior, whereas drug withdrawal decreases sociability and enhances aggression.[1]
Awareness is essential, and the role of dentist in identifying dental patients so as to avoid any possible contraindications during dental treatment, oral and craniofacial manifestations provide necessary dental treatment and to refer to professionals for counseling.[14]
Participants rated cannabis as the most common drug of use and thought it was normal for youth to try drugs with the issue being media exaggerated. Although media sometimes promotes and influences reactions to social issues such as crime or drug use it has enabled pathways for the implementation of harsh drug policies. In this sense, the future research on drug policies may find it useful to employ the data from this assessment in combination with a deeper evaluation of political campaign contributions, and the relationship between the pursuit of governmental and corporate interests, to track drug policy implementation.[15,16]
Although majority of the participants had a bachelor's degree participant with a master's degree thought all drugs are equally harmful with statistical significance. There was no variation in the attitude toward drug users was directly coordinated with the educational qualification. It was seen participants with a bachelor's degree had similar attitude when compared with those who had an master's degree.[17]
All participants thought a detailed history is necessary along with modification in treatment, counseling, and referral of patients to the deaddiction centers. Moreover, a lack of proper knowledge and communication between medical and dental professions makes medical practitioners better qualified to handle cases with drug usage.[18] Extra effort can be implemented to improve research on behavioral therapies, and to develop strategies to improve health of drug users who do not respond to existing treatments.[19,20]
Primary and secondary outcome is the knowledge of substances used for abuse because of the continued rapid increase in the number of drug users, dental health professionals find themselves knowingly or without knowledge treating patients who are addicted to substances. A number of drug abuse problems interface directly with dental care. Failure to recognize or to consider drug abuse can result in a wide range of outcomes.[11,21,22]
Thus, medical management of patients who abuse drugs largely need supportive care, along with the management and treatment for withdrawal or addiction, nutrition support, and potential for transmission of infectious diseases which dentists should be aware of.[17,23]
STRENGTHS
Dentist's knowledge and perception about substance abuse is assessed, as drugs are on rise and have a definite oral manifestation, it could be included in the curriculum.
LIMITATIONS
The small sample and dental student's perception could be included.
The interpretation of this survey is to empower dentists and make them part of drug rehabilitation settings to provide oral health education, educational materials, and also treatment of oral problems. Dental services should be provided at rehabilitation centers to improve the oral health. Dentists should be empowered in providing treatment services for addicts.
The systematic reviews are primarily on individual drugs and their treatments. Hence, dental professionals who usually have negative attitudes toward, and unwillingness to treat is not assessed. Moreover, addicts show a low demand and low priority for their oral health. In addition to the problems with utilization of dental services, they may have problems with compliance with treatment procedures and fail to accept the suggested treatment plan.
Controversies exists as dentists are inexperienced with providing assessments and referrals with lack of appropriate settings to conduct oral health studies, lack of valid inventories, and assessment protocols to detect common oro-dental pathologies among drug users; poor collaboration between dental and general health-care sectors serving drug addicts causes disparity.
Future research-based support is needed to identify effective prevention approaches to identify individuals and to be treated with a specific approach. Dentists should be provided to enhance dental services. Comprehensive information and interest should be created among dental professionals in treating addicts for research.
CONCLUSION
Our findings suggest that educating dental graduates and postgraduates about the oral implications of drugs intake and making it a part of dental curriculum may help us dealing with the global issues of drugs. Even making dental students a part in counseling, and part of the behavioral therapies advocated in treating drug addicts. The research on substance use disorder in India is constrained by the lack of trained workforce and funding. Although control measures have been instituted and implemented, further work needs to be done to effectively challenge the problem of addiction in India. As dental practitioners discussions should be carried out for a better understanding the implications of addiction in both academic and professional scenarios.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Kelly TM, Daley DC, Douaihy AB. Treatment of substance abusing patients with comorbid psychiatric disorders. Addict Behav. 2012;37:11–24. doi: 10.1016/j.addbeh.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehta P. Evaluative trends of illicit drugs uses in India and analysis of Indian and international laws of prohibition of drugs of abuse acta chim. Pharm Indica. 2011;1:32–43. [Google Scholar]
- 3.Ayer WA, Cutright DE. Dental treatment and heart valve complications in narcotic addicts. Oral Surg Oral Med Oral Pathol. 1974;37:359–63. doi: 10.1016/0030-4220(74)90107-8. [DOI] [PubMed] [Google Scholar]
- 4.Milrod B, Leon AC, Busch F, Rudden M, Schwalberg M, Clarkin J, et al. A randomized controlled clinical trial of psychoanalytic psychotherapy for panic disorder. Am J Psychiatry. 2007;164:265–72. doi: 10.1176/ajp.2007.164.2.265. [DOI] [PubMed] [Google Scholar]
- 5.Rogeberg O, Elvik R. The effects of cannabis intoxication on motor vehicle collision revisited and revised. Addiction. 2016;111:1348–59. doi: 10.1111/add.13347. [DOI] [PubMed] [Google Scholar]
- 6.Priyadarshini SR, Sahoo PK, Mohapatra A, Mohapatra A, Sahoo KK. Oral ornamentation an upcoming public health issue in India. Indian J Public Health Res Dev. 2018;9:1141–4. [Google Scholar]
- 7.Hamamoto DT, Rhodus NL. Methamphetamine abuse and dentistry. Oral Dis. 2009;15:27–37. doi: 10.1111/j.1601-0825.2008.01459.x. [DOI] [PubMed] [Google Scholar]
- 8.Hadzic S, Dedic A, Gojkov-Vukelic M, Mehic-Basara N, Hukic M, Babic M, et al. The effect of psychoactive substances (drugs) on the presence and frequency of oral candida species and candida dubliniensis. Mater Sociomed. 2013;25:223–5. doi: 10.5455/msm.2013.25.223-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shekarchizadeh H, Khami MR, Mohebbi SZ, Ekhtiari H, Virtanen JI. Oral health of drug abusers: A review of health effects and care. Iran J Public Health. 2013;42:929–40. [PMC free article] [PubMed] [Google Scholar]
- 10.Brondani MA, Pattanaporn K. P.H.I integrating issues of substance abuse and addiction into the predoctoral dental curriculum. J Dent Educ. 2017;77:3–13. [PubMed] [Google Scholar]
- 11.Deren S, Naegle M, Hagan H, Ompad DC. Continuing links between substance use and HIV highlight the importance of nursing roles. J Assoc Nurses AIDS Care. 2017;28:622–32. doi: 10.1016/j.jana.2017.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhalla A, Basu D, Singh S. Recreational drugs in India. J Mahatma Gandhi Inst Med Sci. 2015;20:20–30. [Google Scholar]
- 13.Solomons YF, Moipolai PD. Substance abuse: Case management and dental treatment. SADJ. 2014;69:298, 300–15. [PubMed] [Google Scholar]
- 14.Gmel G, Gutjahr E. Alcohol consumption and social harm: Quantitative research methodology. In: Klingemann H, Gmel G, editors. Mapping the Social Consequences of Alcohol Consumption. Dordrecht, Netherlands: Kluwer Academic Publishers; 2001. pp. 33–52. [Google Scholar]
- 15.Taylor M, Mackay K, Murphy J, McIntosh A, McIntosh C, Anderson S, et al. Quantifying the RR of harm to self and others from substance misuse: Results from a survey of clinical experts across Scotland. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2011-000774. pii: e000774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Strang J, Groshkova T, Uchtenhagen A, van den Brink W, Haasen C, Schechter MT, et al. Heroin on trial: Systematic review and meta-analysis of randomised trials of diamorphine-prescribing as treatment for refractory heroin addiction†. Br J Psychiatry. 2015;207:5–14. doi: 10.1192/bjp.bp.114.149195. [DOI] [PubMed] [Google Scholar]
- 17.Blanco-Gandía MC, Mateos-García A, García-Pardo MP, Montagud-Romero S, Rodríguez-Arias M, Miñarro J, et al. Effect of drugs of abuse on social behaviour: A review of animal models. Behav Pharmacol. 2015;26:541–70. doi: 10.1097/FBP.0000000000000162. [DOI] [PubMed] [Google Scholar]
- 18.Brown HE. Race, legality, and the social policy consequences of anti-immigration mobilization. Am Sociol Rev. 2013;78:290–314. [Google Scholar]
- 19.Sahoo PK, Priyadarshini S, Sen S. Electronic cigarette: A new modality for tobacco usage & cessation. Int J Curr Res. 2017;9:46299–304. [Google Scholar]
- 20.Priyadarshini SR, Sahoo PK, Bhuyan SK, Misra SR, Pati AR. Growing old is mandatory but growing up is optional: An explanation to geriatrics. J Clin Diagn Res. 2014;8:ZE22–4. doi: 10.7860/JCDR/2014/10393.5304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rech MA, Donahey E, Cappiello Dziedzic JM, Oh L, Greenhalgh E. New drugs of abuse. Pharmacotherapy. 2015;35:189–97. doi: 10.1002/phar.1522. [DOI] [PubMed] [Google Scholar]
- 22.Ramer R, Hinz B. New insights into antimetastatic and antiangiogenic effects of cannabinoids. Int Rev Cell Mol Biol. 2015;314:43–116. doi: 10.1016/bs.ircmb.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 23.Sheridan J, Aggleton M, Carson T. Dental health and access to dental treatment: A comparison of drug users and non-drug users attending community pharmacies. Br Dent J. 2001;191:453–7. doi: 10.1038/sj.bdj.4801206. [DOI] [PubMed] [Google Scholar]


