Abstract
Aims and Objectives:
Discomfort associated with the use of fixed orthodontic appliances may have a negative influence on the patient's oral health-related quality of life (OHRQoL). In general, OHRQoL assessments have the potential to provide information on the need to improve the overall quality of care. This study aims to assess the impact of fixed orthodontic appliances on OHRQoL of Saudi population and to explore the impact of the patient's gender and age on perceived treatment.
Subjects and Methods:
This cross-sectional study used a generic measure of OHRQoL the Arabic version of the Oral Health Impact Profile (OHIP-14), which is a responsive measure to changes in oral health conditions. Data were collected using self-completed e-questionnaire which was distributed through social media and were analyzed using Statistical Package for Social Sciences (SPSS) version 21.0.
Results:
A total of 149 subjects, 110 (73.8%) were females and 39 (26.2%) were males. Adolescents between 13 and 20 years were 63 (42.3%) and adults between 21 and 30 years were 86 (75.7%). A response rate of 100% was obtained. The prevalence of oral health impacts according to OHP-14 was 22.5%. OHIP-14 consists of 14 items covering seven domains. A three-dimensional structure was used to test the existence of separate dimensions: functional limitation, pain discomfort, and psychosocial impact. A significant difference was found between males and females in the first dimension (P = 0.038) and the third dimension (P = 0.022). In addition, a significant difference was also found between the two age groups included in the study within the third dimension (P = 0.025).
Conclusion:
Fixed orthodontic appliances had an evident impact on OHRQoL. However, males had significantly altered functional limitations while females had a higher psychological impact. Furthermore, adults had a significantly higher psychological impact than adolescents.
KEYWORDS: Fixed orthodontic appliances, oral health-related quality of life, quality of life, Saudi patients
INTRODUCTION
Oral health-related quality of life (OHRQoL) has been defined as “the absence of negative impacts of oral conditions on social life and a positive sense of dentofacial self-confidence.”[1] Measuring the OHRQoL provides an insight into how individual oral health status affects the overall quality of life and how oral health care brings about improvements to patients’ overall quality of life.[2,3]
Unlike other medical interventions orthodontic treatment does not cure or treat a condition; rather it aims to correct variations from an arbitrary norm.[3] Quality of life measures are becoming increasingly significant; hence, clinician-based measures of treatment need do not account for patient perceptions or opinions.[4] Nowadays, it is expected from clinicians to show responsibility with respect to the effectiveness of treatment and efficient use of resources. This increased emphasis on patient-based outcome measures including changes in health-related quality of life. This maybe particularly important in cosmetic or elective interventions including orthodontic treatment.[5] Indeed, measuring the impact of fixed appliances on daily life would be a practical way to show the problems that the patient may experience during the treatment. This, in turn, has the potential to provide information about treatment needs and outcomes and to improve care in the long term.
Several studies have shown that discomfort associated with the use of fixed orthodontic appliances had a negative influence on patient's OHRQoL.[6,7] Besides, some researchers suggested that according to the phase of the treatment, orthodontic treatment may either compromise or improve OHQoL.[8,9] Furthermore, a study suggested that the patient's age could be a detrimental factor influencing OHRQoL as younger patients were more adaptable to treatment with fixed appliances.[10]
In general, OHRQoL assessments are recommended in orthodontics to improve the overall quality of care. Accordingly, the present study aims to assess the impact of fixed orthodontic appliances on oral health-related quality of life in Saudi patients.
SUBJECTS AND METHODS
ETHICAL APPROVAL
This study was approved by the Dental Ethics committee of Qassim University (Ex/3005/2018). Participants received a letter describing the study and requesting their consent to access the e-questionnaire.
STUDY POPULATION
The study population consisted of 149 fixed orthodontic appliances wearers in Saudi Arabia consisting of 110 (73.8%) females and 39 (26.2%) males. Furthermore, it included two age groups. Adolescents between 13 and 20 years were 63 (42.3%) and adults between 21 and 30 years were 86 (75.7%); however, the sample size could not be calculated because the number of population is not available. Inclusion criteria included Saudi patients undergoing orthodontic treatment with fixed appliances within the age range of 13–30 years. There were 18 participants excluded with regard to our exclusion criteria which consisted of non-Saudi patients, removable appliances wearers, the presence of a mental or psychological disorder or use of antipsychotic medication.
INSTRUMENTS AND MEASURES
This cross-sectional study used a generic measure of OHRQoL the Arabic version of the Oral Health Impact Profile (OHIP-14), which has been to have face and content validity and reliability for different populations and also have been demonstrated to be responsive to changes in oral health conditions.[11,12,13]
The OHIP-14 comprises 14 items that explore seven aspects of impact: functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap. The responses were classified using the Likert scale with five options ranging from “never” (0) to “very often (4).”
More attention has been focused on the multidimensional construct. A study that used the OHIP-14 showed a three-factor structure for the OHIP-14. These results confirmed the existence of a set of three underlying factors considered as functional limitation, pain-discomfort, and psychosocial impacts, that showed high consistency and construct validity [Figure 1].[14,15]
Figure 1.
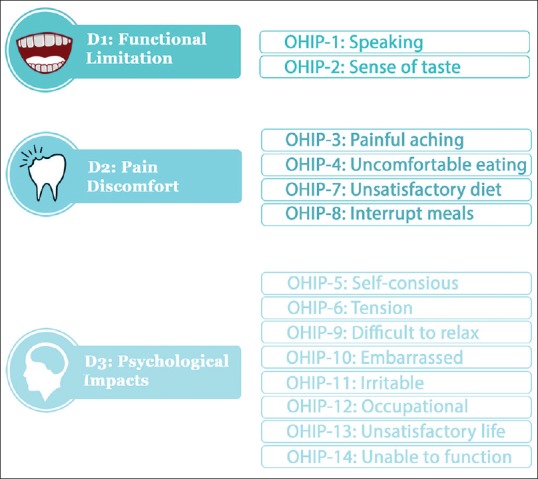
Three dimensional model of oral health impact profile-14
Data were collected using self-completed e-questionnaire which was distributed through social media. The analysis was conducted by using SPSS version 21.0 (IBM Corp., Armonk, NY, USA).
RESULTS
A total of 149 participants have fulfilled the study criteria. The overall rate of the response obtained was 100%. The overall prevalence of oral health impacts according to OHP-14 was 22.5% of the involved sample experienced impact on their OHRQoL.
Data analysis revealed the presence of influence of age and sex on the impact of fixed appliances on daily life. A significant difference was found between males and females in the first dimension (P = 0.038) and the third dimension (P = 0.022) [Table 1] indicating a higher impact on males’ functional limitations by their fixed appliances while females had a higher impact on psychological aspect. However, no significant difference was noticed in the second dimension which means that the pain perception was equal between both sexes. Also found to be statistically significant between the two age groups included in the study was noticed within the third dimension (P = 0.025) indicating that adults had a higher upon psychological aspect than that of adolescents based on the responses.
Table 1.
Three dimensional model for both genders
| Dimension | Components | Gender | Mean | P |
|---|---|---|---|---|
| Functional limitation | OHIP-1 | Males | 0.64+0.778 | 0.016** |
| Pronouncing problems | Females | 0.80+1.107 | ||
| OHIP-2 | Males | 0.67+0.982 | 0.003** | |
| Taste problems | Females | 0.35+0.724 | ||
| Pain-discomfort | OHIP-3 | Males | 1.54+0.854 | 0.553 |
| Aching pain | Females | 1.56+0.953 | ||
| OHIP-4 | Males | 1.85+1.089 | 0.653 | |
| Eating problems | Females | 1.88+1.1788 | ||
| OHIP-7 | Males | 0.46+0.884 | 0.909 | |
| Unsatisfactory diet | Females | 0.46+0.885 | ||
| OHIP-8 | Males | 1.05+0.887 | 0.140 | |
| Meals interruption | Females | 1.26+1.089 | ||
| Psychosocial impacts | OHIP-5 | Males | 0.59+0.880 | 0.222 |
| Self-conscious | Females | 0.42+0.806 | ||
| OHIP-6 | Males | 0.85+0.812 | 0.002** | |
| Tension | Females | 1.25+1.182 | ||
| OHIP-9 | Males | 0.92+1.061 | 0.275 | |
| Relaxation problems | Females | 1.35+1.097 | ||
| OHIP-10 | Males | 1.18+1.144 | 0.826 | |
| Embarrassed | Females | 1.16+1.129 | ||
| OHIP-11 | Males | 1.18+1.167 | 0.975 | |
| Irritability | Females | 1.12+1.139 | ||
| OHIP-12 | Males | 0.59+0.938 | 0.381 | |
| Occupational problems | Females | 0.50+0.886 | ||
| OHIP-13 | Males | 0.41+0.850 | 0.137 | |
| Life satisfaction | Females | 0.35+0.612 | ||
| OHIP-14 | Males | 0.28+0.605 | 0.987 | |
| Function inability | Females | 0.30+0.567 |
In general, the overall mean score for the three dimensions showed an increased score in females more than males [Figure 2].
Figure 2.
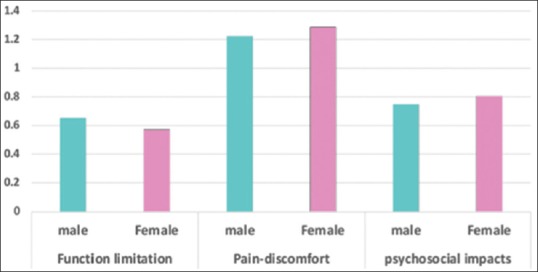
The mean overall score for the three dimensions
DISCUSSION
Within the field of orthodontic there is a longstanding recognition of the role of OHRQoL measures and how they can affect the quality of care.[5]
Interestingly, with our cross-sectional self-reported data covering 149 fixed orthodontic appliance wearier, there was a distinct influence on OHRQoL of Saudi patients was spotted in this study. According to OHIP-14, the prevalence of the oral health impact was high as 22.5% of the study population reported having experienced dental impacts on their daily life activities with fixed orthodontic appliances. Nevertheless, it was not as high as de Oliveira and Sheiham study[9] where they reported having 32.8% prevalence of dental impact among the Brazilian adolescents. However, later on, Marques et al.[6] recounted a prevalence of 15.9% impact on OHRQoL in 2014.
As has been noted, the present study has covered three aspects of OHQoL: functional limitations, pain-discomfort, and psychosocial impacts using OHIP-14 measure.[15] Studying the effect of orthodontic treatment from three aspects has offered a broader understanding of how fixed appliances can specifically affect different aspects of the patient's daily life.
In the long run, it was revealed that orthodontic treatment with fixed appliances can be significantly affected with the patient's age and gender in this study as well as previous studies.[6,7,9,10]
In terms of gender influence, there was a significant difference between males and females throughout the aspects covered in this study. Let us take the case of the first dimension, i.e., functional limitations, as was noticed males had significantly higher impact upon their pronouncing and taste functions. This finding is compatible with Nagarajappa et al.[10] study where they found a higher effect on males’ functional limitations among Indian adolescents as well, however, this difference was not significant in their study. Nevertheless, according to de Oliveira and Sheiham[9] females had experienced more dental impact than males within Brazilian adolescents. Furthermore, the third dimension, psychosocial impact, showed a statically significant difference too in which females were affected more. This finding was also compatible with Nagarajappa et al.[10] study. We can attribute that psychosocial impact is due to the fact that women usually tend to be more concern about their appearance as many of them find the fixed metallic appliances unaesthetic. However, more male sample should be included in later studies with linear measurements to further assess the impact of gender difference.
Apart from gender, testing the age factor divulged a higher psychosocial impact on adults than adolescents which coincides with Nagarajappa et al.[10] findings as they noticed an earlier adaptation for fixed appliances within younger patients. They recommended administering orthodontic treatment as early as possible. Moreover, Marques et al.[6] disclosed an earlier adaptation for younger patients as well.
On the other hand, several studies had assessed the impact of malocclusion on OHRQoL especially in cases where anterior segments were involved.[16,17] Although Dimberg et al. reported that dental fear and headache had more distinct impact factors on OHRQoL than malocclusions or orthodontic treatment need.[18] However, this finding does not deny the role of malocclusion on OHRQoL as it has been established in several studies that the more severe the malocclusion, the worse was the impact on some physical domains and all psychosocial domains of OHRQoL.[19,20]
The influence of self-esteem on the relationship between orthodontic treatment need and OHRQoL has been investigated as well. In one study, they concluded that aesthetic dental needs interfere in the OHRQoL and the self-esteem of patients seeking for treatment.[21] Similarly, another study has established that self-esteem modifies the relationship between subjective orthodontic need and OHRQoL.[22] Moreover, in relation to subjective orthodontic treatment need and OHRQoL, it has been proved that OHRQoL is poorer in children with subjective orthodontic treatment need.[23]
Aydoǧan C had investigated the effects of personality traits as he concluded that they moderate the relationships between orthodontic treatment need and OHRQoL in adolescents. His finding showed that adolescents with higher extraversion and openness to experience are less affected by increased orthodontic treatment need.[24]
Recently, Alghamdi et al. have compared the impact of palatal expanders and fixed orthodontic appliances on OHRQoL. They concluded that palatal expanders had a significantly greater negative impact on some aspects of OHRQoL when compared with fixed orthodontic appliances in adolescents and young adults.[25]
CONCLUSION
Orthodontic treatment with fixed appliances should be given to each patient regarding their age and gender with a satisfactory constructed explanation. Likewise, as long as the patient recognizes the limitations of treatment with fixed appliances, this will ensure an absolute compliance to the whole treatment process since there will be a lesser chance of developing unrealistic expectation and erroneous understanding from the outcome of treatment.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
ACKNOWLEDGMENT
We owe many thanks to our supervisor Dr. Ramy Elmoazen for his guidance expert advices and encouragement. We would also extend our gratitude to Dr. Rabia Bilal for providing me with guidance.
REFERENCES
- 1.Inglehart M, Bagramian RA. Chicago: Quintessence Chicago; 2002. Oral Health-Related Quality of Life; pp. 1–6. [Google Scholar]
- 2.Williams KB, Gadbury-Amyot CC, Bray KK, Manne D, Collins P. Oral health-related quality of life: A model for dental hygiene. J Dent Hyg. 1998;72:19–26. [PubMed] [Google Scholar]
- 3.Cunningham SJ, O’Brien C. Quality of life and orthodontics. Semin Orthod. 2007;13:96–103. [Google Scholar]
- 4.Mandall NA, Matthew S, Fox D, Wright J, Conboy FM, O’Brien KD, et al. Prediction of compliance and completion of orthodontic treatment: Are quality of life measures important? Eur J Orthod. 2008;30:40–5. doi: 10.1093/ejo/cjm077. [DOI] [PubMed] [Google Scholar]
- 5.Cunningham SJ, Hunt NP. Quality of life and its importance in orthodontics. J Orthod. 2001;28:152–8. doi: 10.1093/ortho/28.2.152. [DOI] [PubMed] [Google Scholar]
- 6.Marques LS, Paiva SM, Vieira-Andrade RG, Pereira LJ, Ramos-Jorge ML. Discomfort associated with fixed orthodontic appliances: Determinant factors and influence on quality of life. Dental Press J Orthod. 2014;19:102–7. doi: 10.1590/2176-9451.19.3.102-107.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feu D, Miguel JA, Celeste RK, Oliveira BH. Effect of orthodontic treatment on oral health-related quality of life. Angle Orthod. 2013;83:892–8. doi: 10.2319/100412-781.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen M, Wang DW, Wu LP. Fixed orthodontic appliance therapy and its impact on oral health-related quality of life in Chinese patients. Angle Orthod. 2010;80:49–53. doi: 10.2319/010509-9.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Oliveira CM, Sheiham A. Orthodontic treatment and its impact on oral health-related quality of life in Brazilian adolescents. J Orthod. 2004;31:20–7. doi: 10.1179/146531204225011364. [DOI] [PubMed] [Google Scholar]
- 10.Nagarajappa R, Ramesh G, Sandesh N, Lingesha RT, Hussain MA. Impact of fixed orthodontic appliances on quality of life among adolescents’ in India. J Clin Exp Dent. 2014;6:e389–94. doi: 10.4317/jced.51651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–90. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 12.Al Habashneh R, Khader YS, Salameh S. Use of the Arabic version of oral health impact profile-14 to evaluate the impact of periodontal disease on oral health-related quality of life among Jordanian adults. J Oral Sci. 2012;54:113–20. doi: 10.2334/josnusd.54.113. [DOI] [PubMed] [Google Scholar]
- 13.Locker D, Jokovic A, Clarke M. Assessing the responsiveness of measures of oral health-related quality of life. Community Dent Oral Epidemiol. 2004;32:10–8. doi: 10.1111/j.1600-0528.2004.00114.x. [DOI] [PubMed] [Google Scholar]
- 14.Montero J, Bravo M, Vicente MP, Galindo MP, López JF, Albaladejo A. Dimensional structure of the oral health-related quality of life in healthy Spanish workers. Health Qual Life Outcomes. 2010;8:24. doi: 10.1186/1477-7525-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santos CM, Oliveira BH, Nadanovsky P, Hilgert JB, Celeste RK, Hugo FN. The oral health impact profile-14: A unidimensional scale? Cad Saude Publica. 2013;29:749–57. doi: 10.1590/s0102-311x2013000800012. [DOI] [PubMed] [Google Scholar]
- 16.Sardenberg F, Martins MT, Bendo CB, Pordeus IA, Paiva SM, Auad SM, et al. Malocclusion and oral health-related quality of life in Brazilian school children. Angle Orthod. 2013;83:83–9. doi: 10.2319/010912-20.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guimarães SP, Jorge KO, Fontes MJ, Ramos-Jorge ML, Araújo CT, Ferreira EF, et al. Impact of malocclusion on oral health-related quality of life among schoolchildren. Braz Oral Res. 2018;32:e95. doi: 10.1590/1807-3107bor-2018.vol32.0095. [DOI] [PubMed] [Google Scholar]
- 18.Dimberg L, Lennartsson B, Bondemark L, Arnrup K. Oral health-related quality-of-life among children in Swedish dental care: The impact from malocclusions or orthodontic treatment need. Acta Odontol Scand. 2016;74:127–33. doi: 10.3109/00016357.2015.1059485. [DOI] [PubMed] [Google Scholar]
- 19.Sun L, Wong HM, McGrath CP. Relationship between the severity of malocclusion and oral health related quality of life: A systematic review and meta-analysis. Oral Health Prev Dent. 2017;15:503–17. doi: 10.3290/j.ohpd.a38994. [DOI] [PubMed] [Google Scholar]
- 20.Sun L, Wong HM, McGrath CP. Association between the severity of malocclusion, assessed by occlusal indices, and oral health related quality of life: A systematic review and meta-analysis. Oral Health Prev Dent. 2018;16:211–23. doi: 10.3290/j.ohpd.a40761. [DOI] [PubMed] [Google Scholar]
- 21.Rizzardi KF, Vieira LC, Parisotto TM, Pinto CF Do aesthetics dental needs interfere in theoral health-related quality of life and in the self-steem of patients seeking for treatment at University São Francisco Dental School? [Last accessed on 2018 Dec 04];Braz J Oral Sci. 2017 16:e17006. Available from: https://www.fop.unicamp.br/bjos/index.php/bjos/article/view/ e17006 . [Google Scholar]
- 22.Kragt L, Wolvius EB, Jaddoe VW, Tiemeier H, Ongkosuwito EM. Influence of self-esteem on perceived orthodontic treatment need and oral health-related quality of life in children: The generation R study. Eur J Orthod. 2018;40:254–61. doi: 10.1093/ejo/cjx054. [DOI] [PubMed] [Google Scholar]
- 23.Kragt L, Jaddoe V, Wolvius E, Ongkosuwito E. The association of subjective orthodontic treatment need with oral health-related quality of life. Community Dent Oral Epidemiol. 2017;45:365–71. doi: 10.1111/cdoe.12299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aydoǧan C. Extraversion and openness to experience moderate the relationship between orthodontic treatment need and oral health-related quality of life in adolescents: A cross-sectional study. Angle Orthod. 2018;88:617–23. doi: 10.2319/103117-737.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alghamdi MA, Farsi NJ, Hassan AH. Comparison of oral health-related quality of life of patients treated by palatal expanders with patients treated by fixed orthodontic appliances. Patient Prefer Adherence. 2017;11:699–705. doi: 10.2147/PPA.S124519. [DOI] [PMC free article] [PubMed] [Google Scholar]


