Abstract
Background
Advances in diagnostic imaging techniques make it possible to detect tuberculosis (TB) lesions earlier, when only bone destruction or inflammatory infiltration is demonstrated. These techniques provide doctors with more opportunities to treat TB in the early stages of the disease. Traditional aggressive debridement surgery increases the risk of surgical complications. Therefore, we aimed to determine whether using percutaneous pedicle screw (PPS) fixation alone for the treatment of early spinal TB was a valid and less invasive surgical technique.
Material/Methods
We retrospectively reviewed the clinical and radiographic outcomes in cases with thoracic or lumbar TB treated with PPS surgery or hybrid surgery between January 2010 and January 2017. The operative time, blood loss, length of hospital stay, and hospitalization costs in the 2 groups were recorded and compared. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) before and at 18 months after surgery were tested to evaluate TB progress. Back pain was measured using the visual analog scale (VAS) before the operation and at the final follow-up. Radiological outcomes were evaluated at 1, 6, 12, and 18 months after surgery. A paired t-test was used to evaluate preoperative and postoperative clinical outcomes using SPSS 19.0 software. P values less than 0.05 were considered to be significant.
Results
A total of 42 patients were involved in this retrospective study. In both groups, the average preoperative ESR, CRP level, and VAS score for back pain significantly decreased after surgery. In the PPS group, the operative time, blood loss, hospital stay, and hospitalization costs were all significantly lower than those in the hybrid group. X-ray and CT images showed satisfactory bone fusion and good maintenance of spinal alignment in both groups at the final follow-up.
Conclusions
PPS fixation alone was a valid and less invasive surgery for the treatment of early spinal TB. Furthermore, the recovery process of spinal TB can be facilitated using a “simple” internal fixation procedure, and bone fusion can be achieved without aggressive debridement and bone graft surgery.
MeSH Keywords: Antitubercular Agents; Bone Screws; Debridement; Orthopedic Fixation Devices; Tuberculosis, Spinal
Background
Bone and joint tuberculosis (TB) are widespread and troublesome diseases that can lead to bone and joint destruction, deformity, and even disability. Spinal TB (Pott’ disease) is the most common and most dangerous form of musculoskeletal TB; it accounts for 1% of all TB cases and 50% of osseous TB [1,2]. The typical presentation of spinal TB involves systemic TB symptoms and imaging presentations, including damaged contiguous vertebral bodies and their intervertebral discs without the involvement of the posterior elements, which could be easily recognized and diagnosed. The simplest imaging technique to diagnose this disease is x-ray. However, it is hard to detect the early lesions of spinal TB using x-ray alone. Advances in diagnostic imaging techniques, such as high-resolution computed tomography (CT) and magnetic resonance imaging (MRI) make it possible to detect TB lesions earlier, when only bone destruction or inflammatory infiltration is demonstrated.
Surgical treatment is often required for late-stage patients who develop progressive kyphosis or neurological impairment. It is generally accepted that the surgical strategies for spinal TB include focal debridement, full decompression, internal fixation, and deformity correction if present [3–5]. However, this aggressive procedure is always associated with great surgical trauma and increased complications. Moreover, the disruption of healthy tissue around the lesion is unavoidable, which is also detrimental to TB recovery [4]. Modern anti-TB drugs have been shown to be more efficient in prolonging the progress of spinal TB, which provides the doctors with more opportunities to treat this disease in the early stage. Hence, the question as to whether aggressive debridement surgery is appropriate for the treatment of early spinal TB cases needs to be answered.
As indicated by Jain et al. [2], the treatment of early spinal TB relies mainly on non-surgical methods, including the administration of anti-TB drugs and prolonged bed rest. However, prolonged bed rest is associated with a high risk of complications, such as the loss of motor function, osteoporosis, and hypostatic pneumonia. Moreover, it has been reported that approximately 5–11% of spinal TB fails to respond to conventional conservative therapy [5]. On the other hand, Garg et al. [3] delineated progressive bone destruction, a high risk of vertebral deformity, and unrelieved pain as indications for early surgical intervention.
To date, studies of surgical intervention for the treatment of early spinal TB are lacking. Therefore, we aimed to determine whether or not stabilizing the affected segments with percutaneous pedicle screw (PPS) fixation alone was a valid surgical technique in some early TB cases to relieve pain and prevent angular kyphosis. In this study, we retrospectively analyzed and compared the clinical and radiographic outcomes in thoracic and lumbar TB patients who were treated with PPS surgery or hybrid surgery.
Material and Methods
Patients
This was a retrospective cohort study (UIN: researchregistry4241) that was approved by our institutional review board. Informed consent and protocols that included information on the mechanism of treatment, predictive outcomes, potential risks, and side effects were signed by all patients. We retrospectively reviewed clinical and radiographic data from 52 consecutive patients with thoracic or lumbar TB in our department between January 2010 and January 2017. Four patients treated with nonsurgical methods were excluded from this study. The remaining 48 patients had undergone either PPS fixation surgery or hybrid surgery. The indications for PPS fixation surgery included progressive bone destruction tending toward deformity, spinal instability, and poor outcomes (e.g., persistent pain). In contrast, patients with an established spinal deformity, neurological deficit, or large abscess who were contraindicated to PPS fixation surgery were excluded from this study. The choice of surgical modality was based on different time periods, and no other selection criterion was used. Hybrid surgery was performed during the first 4 years, while single PPS fixation surgery was performed during the more recent years. All operations were performed by the same surgical team.
Perioperative management
The diagnosis of spinal TB was based on clinical and radiographic evidences (x-ray, CT, and MRI), a blood test, and a histopathological examination. All patients were treated with RHZE therapy (isoniazid 300 mg/day, rifampin 600 mg/day, pyrazinamide 1500 mg/day, ethambutol 1000 mg/day) for at least 2 weeks before surgery. In general, surgery was performed when erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) decreased, and malnutrition improved. After surgery, a lumbar back brace was recommended for more than 6 weeks, RHZE chemotherapy was given for at least 9 months, and HRE (isoniazid, rifampicin and ethambutol) chemotherapy was given for another 3 months.
Operative techniques
PPS group
Patients were placed in the prone position under general anesthesia. A 1.0 cm transverse skin incision was performed after confirming the entry point of the PPS. Jamshidi needles were punctured into the pedicles under C-arm fluoroscopic guidance, and then a guide wire was inserted into the Jamshidi needle. A hollow tap was introduced to prepare the screw channel. Pedicle screws were implanted following the guide wire, and pre-bent titanium rods were placed to cross the screws. The PPS fixation system used in this procedure was the VIPER®2 MIS Spine Screws System (Depuy Synthes, Johnson & Johnson, NJ, USA).
Hybrid group
The hybrid surgery in this study was defined as radical debridement, interbody fusion, and open pedicle screw fixation. The pedicle screws used in this procedure were MOSS MIAMI System (Depuy Synthes, Johnson & Johnson, NJ, USA). The detailed protocol for hybrid surgery was performed as described by Güzey et al. [6].
Postoperative assessments
The operative time and blood loss were recorded for both groups. Plain radiographs and CT scans were taken at 1 month, 6 months, 12 months, and 18 months after surgery to assess the internal fixation position and fusion situation of local pathological vertebrae. Subsequently, the ESR and CRP of patients were tested at the final follow-up to evaluate the clinical progress of TB. Additionally, the visual analog scale (VAS) score for back pain was used to assess the status of pain control. All data were expressed as the mean ± standard deviation. A paired t-test was used to evaluate pre- and post-operative clinical outcomes using SPSS software (version 19.0, SPSS Inc., Chicago, IL, USA). P values of less than 0.05 were considered to be significant.
Results
In accordance with the inclusion criteria, 42 out of 48 patients were included in this study, consisting of 22 patients who underwent PPS fixation surgery and 20 patients who underwent hybrid surgery. The PPS group consisted of 8 thoracic TB cases and 14 lumbar TB cases. There were 7 thoracic TB cases and 13 lumbar TB cases included in the hybrid group. Patients’ age at the time of surgery ranged from 26 to 67 years old. There was no significant difference in sex or age between the 2 groups (P>0.05). Detailed clinical characteristics of the included patients are shown in Table 1.
Table 1.
Demographic and operation data of patients in PPS group and hybrid group.
| Characteristics | PPS (n=22) | Hybrid (n=20) |
|---|---|---|
| Gender (Male/Female) | 13/9 | 10/10 |
| Age (year) | 44.86±11.01 | 43.45±10.41 |
| Levels | ||
| Thoracic | 8 | 7 |
| Lumbar | 14 | 13 |
| Operation time (min) | 121.86±24.94 | 274.95±32.70 |
| Blood loss (mL) | 73.05±36.78 | 310.75±65.84 |
| Hospital stay (day) | 8.05±1.70 | 16.75±4.51 |
| Costs (yuan) | 75488.43±12828.13 | 103092.19±18037.11 |
PPS – percutaneous pedicle screw.
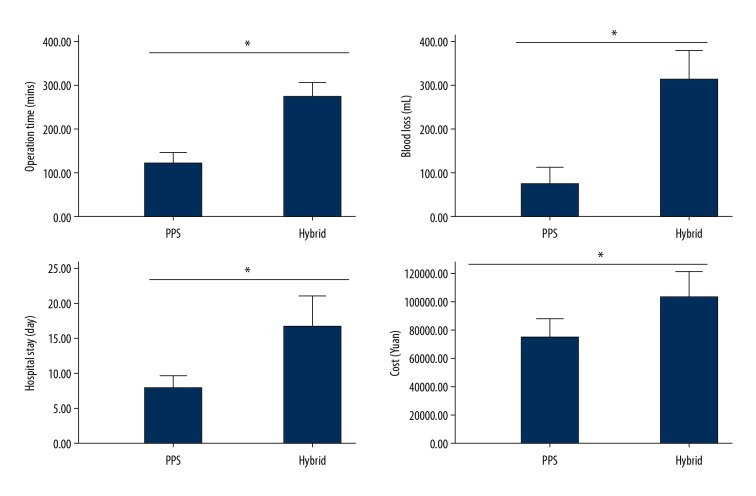
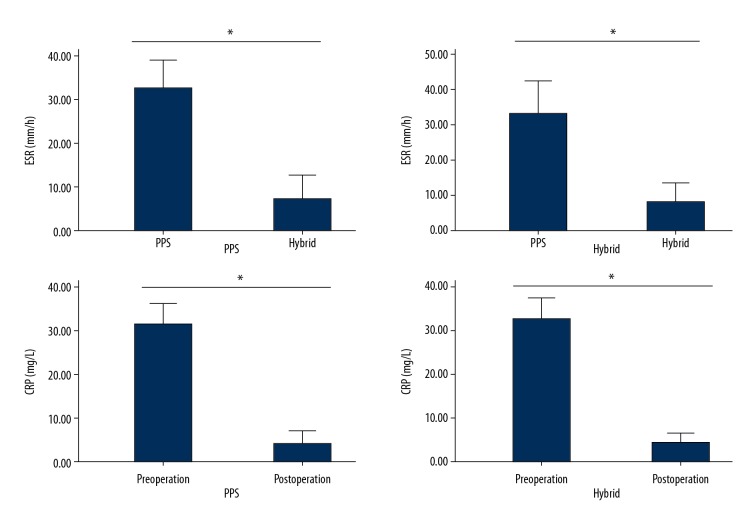
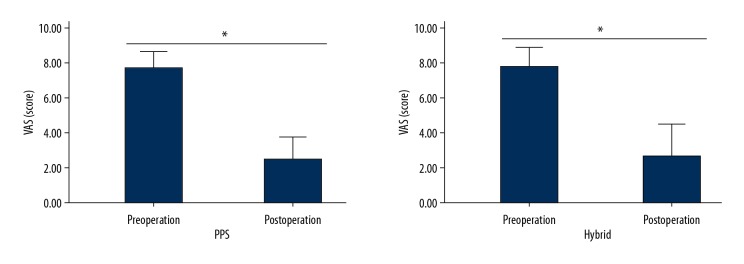
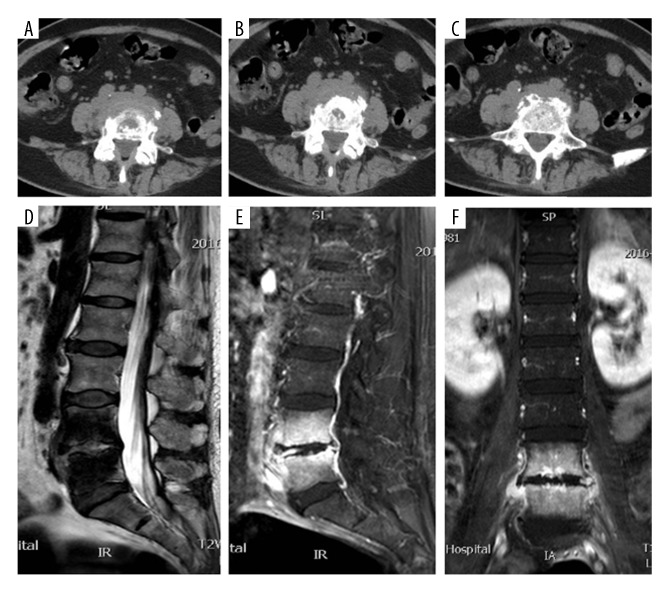
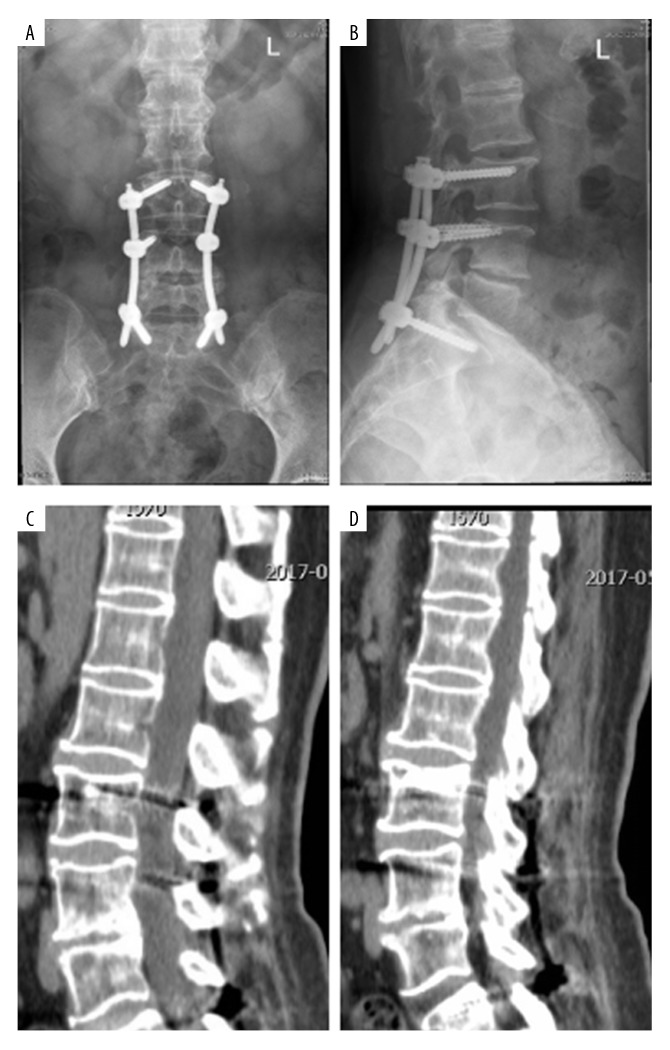
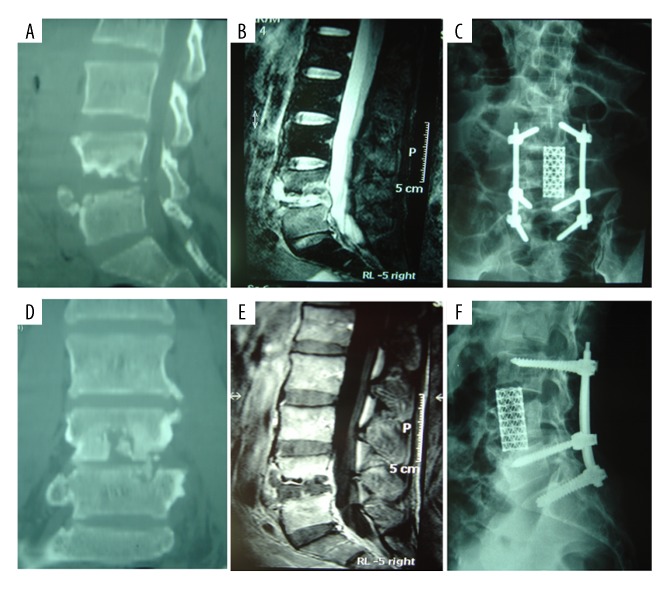
There were no operation-related complications in either group, and no local recurrence of TB was found at the final follow-up. Compared with the hybrid group, the average operative time, blood loss, length of hospital stay, and hospitalization costs were significantly reduced in the PPS group (P<0.05, Table 1, Figure 1). After surgery, the average ESR and CRP values in these 2 groups returned to normal levels at the final follow-up (Table 2, Figure 2). The preoperative average VAS scores were 7.64±0.95 and 7.75±1.07 in the PPS group and the hybrid group, respectively; one month after surgery, the average VAS scores recovered to 2.45±1.22 and 2.65±1.79, respectively (Table 3, Figure 3). With regard to the radiological outcomes, bone fusion and satisfactory spinal alignment were obtained in both groups at the final follow-up (Figures 4–6).
Figure 1.
Comparison of the operative time, blood loss, hospital stay and hospitalization costs in both the PPS and hybrid groups. The average operative time, blood loss, hospital stay and hospitalization costs in the PPS group were all significantly lower than those in the hybrid group (P<0.05). PPS – percutaneous pedicle screw.
Table 2.
ESR and CRP levels of patients in PPS group and hybrid group.
| Group | PPS (n=22) | Hybrid (n=20) |
|---|---|---|
| Preoperative ESR (mm) | 32.72±6.58 | 33.05±9.37 |
| Postoperative ESR (mm) | 7.18±5.42 | 7.90±5.61 |
| Preoperative CRP (mg/L) | 31.82±4.73 | 32.65±5.17 |
| Postoperative CRP (mg/L) | 4.68±2.57 | 4.35±2.30 |
ESR – erythrocyte sedimentation rate; CRP – C-reactive protein; PPS – percutaneous pedicle screw.
Figure 2.
Comparison of the preoperative and postoperative ESR and CRP in the PPS and hybrid groups. The postoperative average ESR levels in both groups were significantly decreased compared with the preoperative average ESR levels (P<0.05). The postoperative average CRP levels in both groups were significantly decreased compared with the preoperative average CRP levels (P<0.05). ESR – erythrocyte sedimentation rate; CRP – C-reactive protein; PPS – percutaneous pedicle screw.
Table 3.
VAS Scores for back pain in 42 patients before and 1 month after surgery.
| Group | Preoperative VAS | Postoperative VAS |
|---|---|---|
| PPS (n=22) | 7.64±0.95 | 2.45±1.22 |
| Hybrid (n=20) | 7.75±1.07 | 2.65±1.79 |
VAS – visual analog scale; PPS – percutaneous pedicle screw.
Figure 3.
Comparison of the preoperative and postoperative VAS in the PPS and hybrid groups. The postoperative average VAS scores in both groups were significantly decreased compared with the preoperative average VAS scores (P<0.05). PPS – percutaneous pedicle screw; VAS – visual analog scale.
Figure 4.
The CT and MRI images of one patient with L4–L5 spinal tuberculosis. Axial CT images show L4–L5 vertebrae destruction and a disc lesion (A–C); Sagittal and coronal MRI images show an extensive lesion on the L4–L5 vertebral body and disc without compression of the spinal cord (D–F). CT, computed tomography, MRI, magnet resonance imaging.
Figure 5.
Postoperative x-ray and CT images of the same patient in the PPS group at 18 months after surgery. Good maintenance of spinal alignment (A, B) and bone fusion (C, D) were obtained by using PPS fixation alone. CT – compute tomography; PPS – percutaneous pedicle screw.
Figure 6.
The pre- and post-operative images of another patient with L4–L5 spinal tuberculosis in the hybrid group. Preoperative CT (A, D) and MRI (B, E) images show an extensive lesion on the L4–L5 vertebral body and intervertebral disc without compression of the spinal cord. Postoperative x-ray (C, F) shows posterior reconstruction with a titanium mesh cage filled with autogenous bone following radical debridement. CT – computed tomography; MRI – magnetic resonance imaging.
Discussion
TB is an infectious disease that can be cured. Spinal TB remains prevalent throughout the world. Anti-TB chemotherapy has been regarded as the basic treatment. Various studies have shown that drug therapy is effective for controlling and curing a spinal TB infection [7–9]. Therefore, all patients included in this study received the standard chemotherapy treatment. At the final follow-up, the average ESR and CRP in both groups had recovered to normal levels. It was elucidated that mycobacterium TB was controlled by anti-TB chemotherapy, even in the PPS group in whom debridement was not performed. Perhaps the main debatable point about this study is whether or not surgical intervention is necessary for early spinal TB. In a systematic review, Jutte et al. [10] compared chemotherapy plus surgery with chemotherapy alone for treating spinal TB and found no significant benefit from surgery. In their view, routine surgery for spinal TB was not recommended. However, bed rest and immobilization as conventional treatment for spinal TB had at least two inherent defects. First, it was always associated with a high risk of complications such as loss of motor function, osteoporosis, hypostatic pneumonia, pulmonary embolism, and DVT. Second, even the “absolute” immobilization could not provide sufficient stability in the involved spinal segment, which was a common cause of back pain and progressive deformity.
In another review of spinal TB management, Garg et al. [3] suggested some specific indications for early surgical intervention in patients without neurological complications, which were similar to the inclusion criteria in our study. Traditional surgical strategies for spinal TB include focal debridement, complete decompression, and spinal stability reconstruction. However, damage to the vertebral column could lead to an increase of blood loss and a higher risk of nerve injury in the debridement surgery. In addition, interbody fusion with instrumentation is often needed after debridement. For patients without neurological complications, surgical intervention aimed to relieve pain earlier, reconstruct spinal stability, and prevent deformity. In such circumstances, is surgical debridement necessary?
To address this problem, we conducted this study to stabilize the pathological level of the spine by using PPS fixation. The concept of PPS insertion, initially described as an external fixator in the thoracic and lumbar spine, was introduced by Magerl [11]. Based on the Magerl technique, Wiesner et al. [12] reported a modified technique to improve the accuracy of PPS insertion by adjusting the location of the entry point. Since the invention of the specially designed PPS system by Foley and Gupta [13], the PPS technique has been increasingly popular in the treatment of spondylolisthesis, spinal fracture, tumors, etc. [14–16]. The PPS technique could provide adequate spinal stabilization with minimal disruption to the para-spinal muscles and soft tissues. In addition, indirect reduction techniques related to the PPS system could help correct spinal deformities [17]. On this account, we attempted to apply PPS fixation to some selected patients with early spinal TB.
As shown in our results, satisfactory clinical outcomes were achieved by PPS fixation alone, including rapid pain relief, good maintenance of spinal alignment, and prevention of kyphosis. Increases in ESR are related to inflammation, TB, autoimmune disorders, etc. The ESR is a much more sensitive parameter for TB than pyogenic infection. In TB, the highly raised ESR was in contrast to normal or mild to moderate leukocytosis unless there was a secondary infection. CRP is mainly used as a marker of inflammation and is highly increased in TB. Measuring and charting CRP values could prove useful in determining the disease progress or the effectiveness of treatment. CRP was a more sensitive and accurate reflection of the acute phase response compared to ESR. Therefore, ESR and CRP were not only useful in the diagnosis of spinal TB but were also reliable parameters in assessing the response to treatment and the progress of spinal TB. In the current study, all patients showed a significant increase of ESR and CRP before surgery. At the last follow-up, the average ESR and CRP in both groups had recovered to normal levels, which was because the standard anti-TB drug treatment was obtained for all patients. The VAS score showed all patients had moderate to severe back pain. The pain was mainly caused by destruction and instability at the pathological level. Both techniques could be employed to reconstruct the stability of the spine for pain relief. Therefore, the postoperative average VAS scores in the 2 groups decreased significantly.
Notably, good bone fusion was also obtained in the PPS group. Hence, it was reasonable to conclude that the local TB foci could be absorbed and replaced by regenerating bone tissue due to the effects of anti-TB drugs. The operative time, blood loss, hospital stay, and cost were significantly decreased in the PPS group compared with the hybrid group, which delineated that using the PPS technique is less invasive than standard debridement and internal fixation surgery for the treatment of spinal TB. Moreover, the complications related to long-term immobilization could be greatly reduced due to the early postoperative rehabilitation.
It should be noted that the basic principle of PPS technique in treatment of spinal TB is to provide strong stability to the affected spinal segment. Therefore, in cases with osteoporosis or severe bone destruction, screw augmentation technique [18] is needed. In addition, the modified pedicle screw system may improve the stability of TB-damaged spine [19].
Several limitations of this study should be mentioned. First, the study had a small sample size and a short follow-up period. To further determine the feasibility of this method, a longer follow-up with more cases needs to be carried out in future studies. Second, the course of spinal TB progress was not the same and might influence the outcomes. Third, the specific inclusion criteria in this study should be further evaluated.
Conclusions
In conclusion, PPS fixation alone as a less invasive surgery can stabilize the pathological level of the spine, relieve pain, facilitate bone fusion, and prevent deformity in the treatment of some selected patients with early spinal TB. Furthermore, the recovery process of spinal TB can be facilitated using a “simple” internal fixation procedure, and bone fusion can be achieved without aggressive debridement and bone graft surgery.
Footnotes
Source of support: This study was funded by Key Discipline Construction Project of Pudong Health Bureau of Shanghai (PWZxk2017-08)
References
- 1.Rasouli MR, Mirkoohi M, Vaccaro AR, et al. Spinal tuberculosis: Diagnosis and management. Asian Spine J. 2012;6(4):294–308. doi: 10.4184/asj.2012.6.4.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jain AK. Tuberculosis of the spine: A fresh look at an old disease. J Bone Joint Surg Br. 2010;92(7):905–13. doi: 10.1302/0301-620X.92B7.24668. [DOI] [PubMed] [Google Scholar]
- 3.Garg RK, Somvanshi DS. Spinal tuberculosis: A review. J Spinal Cord Med. 2011;34(5):440–54. doi: 10.1179/2045772311Y.0000000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tuli SM. Historical aspects of Pott’s disease (spinal tuberculosis) management. Eur Spine J. 2013;22(Suppl 4):529–38. doi: 10.1007/s00586-012-2388-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dunn RN, Ben Husien M. Spinal tuberculosis. Bone Joint J. 2018;100-B(4):425–31. doi: 10.1302/0301-620X.100B4.BJJ-2017-1040.R1. [DOI] [PubMed] [Google Scholar]
- 6.Güzey FK, Emel E, Bas NS, et al. Thoracic and lumbar tuberculous spondylitis treated by posterior debridement, graft placement, and instrumentation: A retrospective analysis in 19 cases. J Neurosurg Spine. 2005;3(6):450–58. doi: 10.3171/spi.2005.3.6.0450. [DOI] [PubMed] [Google Scholar]
- 7.Liu P, Zhu Q, Jiang J. Distribution of three anti-tuberculous drugs and their metabolites in different parts of pathological vertebrae with spinal tuberculosis. Spine. 2011;36(20):E1290–95. doi: 10.1097/BRS.0b013e31820beae3. [DOI] [PubMed] [Google Scholar]
- 8.Ge Z, Wang Z, Wei M. Measurement of the concentration of three anti-tuberculosis drugs in the focus of spinal tuberculosis. Eur Spine J. 2008;17(11):1482–87. doi: 10.1007/s00586-008-0778-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dai LY, Jiang LS, Wang YR, Jiang SD. Chemotherapy in anterior instrumentation for spinal tuberculosis: highlighting a 9-month three-drug regimen. World Neurosurg. 2010;73(5):560–64. doi: 10.1016/j.wneu.2010.02.023. [DOI] [PubMed] [Google Scholar]
- 10.Jutte PC, van Loenhout-Rooyackers JH. Routine surgery in addition to chemotherapy for treating spinal tuberculosis. Cochrane Database Syst Rev. 2006;25(5):CD004532. doi: 10.1002/14651858.CD004532.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Magerl FP. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res. 1984;189:125–41. [PubMed] [Google Scholar]
- 12.Wiesner L, Kothe R, Rüther W. Anatomic evaluation of two different techniques for the percutaneous insertion of pedicle screws in the lumbar spine. Spine. 1999;24(15):1599–603. doi: 10.1097/00007632-199908010-00015. [DOI] [PubMed] [Google Scholar]
- 13.Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine: Preliminary clinical results. J Neurosurg. 2002;97(1 Suppl):7–12. doi: 10.3171/spi.2002.97.1.0007. [DOI] [PubMed] [Google Scholar]
- 14.Kim JS, Choi WG, Lee SH. Minimally invasive anterior lumbar interbody fusion followed by percutaneous pedicle screw fixation for isthmic spondylolisthesis: Minimum 5-year follow-up. Spine J. 2010;10(5):404–9. doi: 10.1016/j.spinee.2010.02.022. [DOI] [PubMed] [Google Scholar]
- 15.Wang H, Zhou Y, Li C, et al. Comparison of open versus percutaneous pedicle screw fixation using the sextant system in the treatment of traumatic thoracolumbar fractures. Clin Spine Surg. 2017;30(3):E239–46. doi: 10.1097/BSD.0000000000000135. [DOI] [PubMed] [Google Scholar]
- 16.Mobbs RJ, Park A, Maharaj M, Phan K. Outcomes of percutaneous pedicle screw fixation for spinal trauma and tumors. J Clin Neurosci. 2016;23:88–94. doi: 10.1016/j.jocn.2015.05.046. [DOI] [PubMed] [Google Scholar]
- 17.Alander DH, Cui S. Percutaneous pedicle screw stabilization: Surgical technique, fracture reduction, and review of current spine trauma applications. J Am Acad Orthop Surg. 2018;26(7):231–40. doi: 10.5435/JAAOS-D-15-00638. [DOI] [PubMed] [Google Scholar]
- 18.Huang YS, Ge CY, Feng H, et al. Bone cement-augmented short-segment pedicle screw fixation for Kümmell disease with spinal canal stenosis. Med Sci Monit. 2018;24:928–35. doi: 10.12659/MSM.905804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mizuno T, Sakakibara T, Yoshikawa T, et al. Biomechanical stability of a cross-rod connection with a pedicle screw system. Med Sci Monit Basic Res. 2018;24:26–30. doi: 10.12659/MSMBR.906339. [DOI] [PMC free article] [PubMed] [Google Scholar]