Abstract
Background
regular physical activity is one of the key components of a healthy lifestyle. It is associated with better physical and cognitive functioning in later life and with increased life expectancy. The purpose of this study was to evaluate the prevalence of, and factors related to, physical inactivity among older adults across Europe.
Methods
in this cross-sectional analysis, we used data from participants aged 55 or older in Wave 4 of the Survey of Health, Ageing, and Retirement in Europe (SHARE) database, a multidisciplinary and cross-national panel database covering health, socioeconomic status, and social and family networks. Individuals included in this study were classified as physically active or physically inactive. Clinical, psychosocial and sociodemographic variables were evaluated for their association with physical inactivity.
Results
from the total of 58,489 individuals in SHARE, we selected 19,298 people age 55 or older (mean age 67.8 ± 8.9 years; 11,430 (59.2%) female). The overall prevalence of inactivity among individuals age 55 or older in the 16 included countries was 12.5%. The prevalence of physical inactivity varied between countries, ranging from 4.9% (Sweden) to 29% (Portugal). Increasing age, depression, physical limitations, poor sense of meaning in life, social support and memory loss were significant variables associated with physical inactivity.
Conclusions
physical inactivity can be explained by physical, cognitive and psychological conditions. Interventions aimed at promoting physical activity among older people are needed to address this diversity of factors.
Keywords: physical inactivity, association, older people
Introduction
Physical inactivity in older adults is a major public health concern. It has been identified as the fourth leading risk factor for global mortality [1] and a major contributing factor for disability and poor health outcomes [2]. Lack of physical activity is related to approximately 3 million deaths per year and to 6–10% of the occurrence of major non-communicable diseases [3].
Insufficient levels of physical activity are prevalent worldwide, with almost two-thirds of adults and 80% of the young population in Europe not reaching the minimum recommended amounts of physical activity [4]. Older adults have a more sedentary lifestyle, spending more than 9.4 h in sedentary activities per day [5].
Regular physical activity is one of the key components of a healthy lifestyle; it is associated with better physical and cognitive functioning in older adults and also with improved life expectancy [6]. Moderate to vigorous physical activity is associated with a reduced risk of chronic diseases, including Type 2 diabetes, cardiovascular diseases, cancer, depression and metabolic syndrome [7]. Conversely, physical inactivity is associated with poor quality of life and frailty in older people [8]. Non-adherence to physical exercise, which is as prevalent as non-adherence to medicines, can lead to life-threatening conditions and sometimes even affect activities of daily living [9].
Most previous work has assessed the predictors of physical inactivity at a local level, limiting the scope for cross-cultural comparison [10] The purpose of this study was to identify the factors associated with physical inactivity across 16 European countries. The identification of factors associated with physical inactivity in ageing adults may result in the development of effective interventions for promoting regular physical activity across Europe.
Material and methods
The Survey of Health, Ageing, and Retirement in Europe (SHARE) is a multinational panel database that includes representative samples of community-based populations from 19 countries in Europe plus Israel. In the present cross-sectional analysis, data from Wave 4 of the SHARE survey was used, which included information about health, social and economic status, and family networks of individuals from 16 European countries (Austria, Belgium, Czech Republic, Denmark, Estonia, France, Germany, Hungary, Italy, Netherlands, Poland, Portugal, Slovenia, Spain, Sweden and Switzerland) [1]. This wave from 2010 contains data from 58,489 individuals aged 23–103. For the purpose of this analysis, the sample includes non-institutionalised individuals aged 55 or older who answered all of the questions included in this analysis [11].
Evaluation of physical inactivity
Physical inactivity was assessed via the following questions: ‘How often do you engage in activities that require a moderate level of energy such as gardening, cleaning the car, or doing a walk?’ and ‘We would like to know about the type and amount of physical activity you do in your daily life. How often do you engage in vigorous physical activity, such as sports, heavy housework, or a job that involves physical labour?’ Both questions had as possible answers: ‘More than once a week’, ‘Once a week’, ‘One to three times a month’ and ‘Hardly ever, or never’. Physical inactivity was defined as never or almost never engaging in moderate or vigorous physical activity through the response of ‘One to three times a month’ and ‘Hardly ever, or never’ to both questions.
Explanatory variables
The wide scope of information in the SHARE project led us to include a large number of putative explanatory variables such as socio-demographics (age, gender and education), functional limitations, subjective well-being, social support, depression, education, memory, number of chronic diseases and number of meals per day. Detailed information about explanatory variables is given in Appendix 1 of the supplementary data at (http://www.ageing.oxfordjournals.org/).
Statistical analysis
We performed descriptive analyses of outcomes to estimate the proportion of individuals with physical inactivity in the 16 European countries. Given the multilevel structure of data, with individuals nested in each country, we used a multilevel logistic regression approach, considering physical inactivity as the dependent variable.
We performed multilevel, univariable logistic regression, considering each covariate in turn, to identify factors potentially associated with the outcome variable. Significant covariates from this first step were included in a multilevel, multivariable logistic regression model. Country was entered as a random effect. The final model was composed only of significant covariates, selected using a backward selection method. Odds ratios (ORs) and 95% confidence intervals (CIs) are reported. All analyses were performed using the SPSS v23 (IBM, New York, USA). A P value of <0.05 was taken to be significant for all analyses.
Results
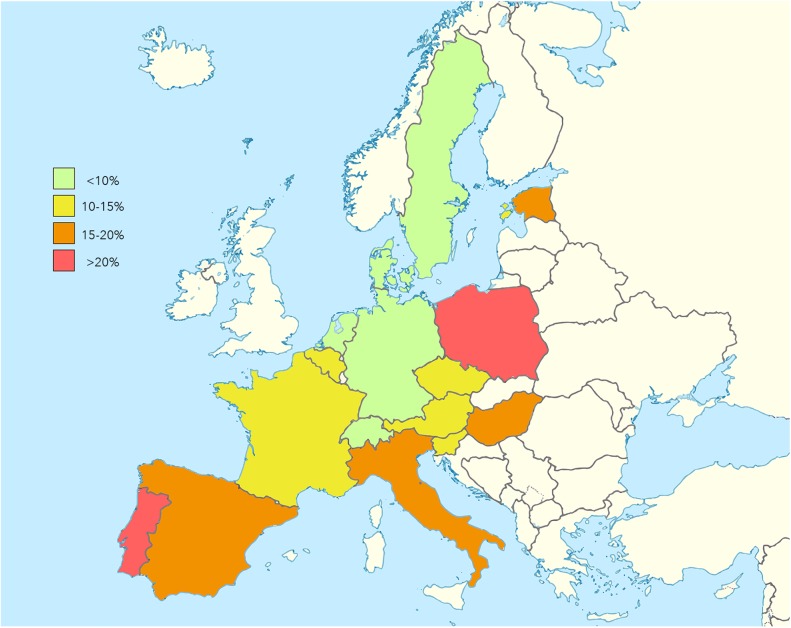
From the 58,489 individuals who participated in Wave 4 of the SHARE survey, we included 19,298 individuals, with a mean age of 67.8 (SD 8.9) years old; 11,430 (59.2%) were female. Of the sample population, 2,415 (12.5%) reported no vigorous or moderate physical activity. The geographic distribution of physical inactivity was unequal between the 16 evaluated countries (Figure 1), ranging from 4.9% (Sweden) to 29% (Portugal); results are shown in Table 1.
Figure 1.
Prevalence of physical inactivity in older people (55 years or older) across Europe.
Table 1.
Prevalence of physical inactivity in individuals 55 years or older across Europe
| Country | No vigorous or moderate physical activity (%) |
|---|---|
| Austria | 258/2,374 (10.9) |
| Germany | 51/635 (8.0) |
| Sweden | 34/692 (4.9) |
| Netherlands | 65/847 (7.7) |
| Spain | 256/1,309 (19.6) |
| Italy | 245/1,289 (19.0) |
| France | 109/953 (11.4) |
| Denmark | 78/1,046 (7.5) |
| Switzerland | 106/1,951 (5.4) |
| Belgium | 203/1,710 (11.9) |
| Czech | 213/1,951 (10.9) |
| Poland | 227/881 (25.8) |
| Hungary | 93/657 (14.2) |
| Portugal | 95/328 (29.0) |
| Slovenia | 24/204 (11.8) |
| Estonia | 358/2,471 (14.5) |
| Total | 2,415 (12.5) |
Analysing all countries together using unadjusted models, we found a significant association between all explanatory variables with physical inactivity (Supplementary Table). Using adjusted models (Table 2), however, we found that difficulties in walking 100 m (OR = 2.672 [95% CI, 2.318–3.081]) and changes in mobility, arm function and fine motor limitations (OR = 0.796 [95% CI, 0.775–0.817]) were associated with physical inactivity. Moreover, individuals who reported their own life has meaning often (OR = 1.794 [95% CI, 1.407–2.288]) and sometimes (OR = 1.282 [95% CI, 1.005–1.635]) showed less physical inactivity when compared with those who reported their own life never has meaning.
Table 2.
Association of explanatory variables with physical inactivity (adjusted models).
| n | Cases of physical inactivity n (%) | Adjusted | |||
|---|---|---|---|---|---|
| OR | CI 95% | P | |||
| Functional limitations | |||||
| Difficulties in walking 100 metres | |||||
| Yes | 2,337 | 1,147 48.8) | 1.000 | – | – |
| No | 16,961 | 1,275 (7.5) | 2.672 | 2.318–3.081 | <0.001 |
| Mobility, arm function and fine motor limitations | |||||
| 19,298 | 2,415 (12.5) | 0.796 | 0.775–0.817 | <0.001 | |
| Subjective well-being | |||||
| Life has meaning | |||||
| Never | 565 | 176 (31.2) | 1.000 | – | – |
| Rarely | 1,454 | 406 (27.9) | 1.096 | 0.842–1.426 | 0.497 |
| Sometimes | 4,586 | 814 (17.7) | 1.282 | 1.005–1.635 | 0.045 |
| Often | 12,693 | 1,019 (8.0) | 1.794 | 1.407–2.288 | <0.001 |
| Social Support | |||||
| Received help from others | |||||
| No | 15,244 | 1,462 (9.6) | 1.000 | – | – |
| Yes | 4,054 | 953 (23.5) | 0.744 | 0.661–0.837 | <0.001 |
| Given help last 12 months | |||||
| No | 14,357 | 2,227 (15.5) | 1.000 | – | – |
| Yes | 4,941 | 188 (3.8) | 2.841 | 2.404–3.356 | <0.001 |
| Memory | |||||
| Poor | 1,005 | 410 (40.8) | 1.000 | – | – |
| Fair | 4,493 | 765 (17.0) | 1.600 | 1.333–1.920 | <0.001 |
| Good | 8527 | 826 (9.7) | 1.618 | 1.345–1.947 | <0.001 |
| Very good | 4,006 | 303 (7.6) | 1.522 | 1.223–1.895 | <0.001 |
| Excellent | 1,267 | 112 (8.8) | 1.296 | 0.980–1.714 | 0.069 |
| Depression scale EURO-D—high is depressed | |||||
| 19,298 | 2,415 (12.5) | 0.973 | 0.949–0.997 | 0.014 | |
| Age | |||||
| 19,298 | 2,415 (12.5) | 0.958 | 0.953–0.964 | <0.001 | |
| Random effect | Estimate | Standard error | P | ||
| Variance (intercept) | 0.204 | 0.082 | 0.013 | ||
Individuals who received help from others (OR = 0.744 [95% CI, 0.661–0.837]) showed higher levels of physical inactivity, and those who gave help (OR = 2.841 [95% CI, 2.404–3.356]) to someone else in the past 12 months showed lower levels of physical inactivity.
Individuals who reported very good (OR = 1.522 [95% CI, 1.223–1.895]), good (OR = 1.618 [95% CI, 1.345–1.947]) or fair (OR = 1.600 [95% CI, 1.333–1.920]) memory showed less physical inactivity than those who reported poor memory. We also found that increasing age (OR = 0.958 [95% CI, 0.953–0.964]) and depression (OR = 0.973 [95% CI, 0.949–0.997]) were associated with increased physical inactivity.
Discussion
A number of epidemiological studies and clinical trials have suggested that any type of physical activity reduces the risk of developing chronic diseases such as hypertension, diabetes or stroke. Physical inactivity is a risk factor for frailty and disability among older adults and, therefore, older people should be encouraged to perform or maintain regular physical activities throughout their ageing process [12].
In this study, we analysed the prevalence of physical inactivity and its associated factors across 16 European countries. Overall, we found that the prevalence of physical inactivity was 12.5%. The findings suggest that functional limitations, subjective well-being, social support, memory, depression and age are associated with physical inactivity and are therefore potential factors on a pathway to poor health. Age emerged as a factor associated with physical inactivity, which is not surprising as physical activity levels are already known to decline with age. Such findings have several implications, however, as it is important to find strategies to encourage older people to engage in moderate levels of physical activity as this may provide protection from certain chronic diseases and prevent disability [13].
Not surprisingly, difficulty in walking 100 m and receiving help for personal care and household tasks in the past 12 months also were significant factors related to physical inactivity. Herein lies a paradoxical situation that confronts older people with a disability; they cannot engage in physical activity due to their functional limitation, but they cannot improve their functional performance if they do not engage in physical activity. Limitations in performing activities such as walking or performing basic and instrumental activities of daily living are common, and 80% of frail older people experience restricted participation in social activities, including outdoor activities [14]. On the other hand, a low level of physical activity is an important risk factor that contributes to decreased physical function. Therefore, it is crucial to develop physical activity programmes tailored to address barriers to mobility, increase functional performance and increase mobility outcomes. Ultimately, multifactorial interventions may have the potential to have an impact on morbidity, hospitalisation, admission to residential care facilities and care costs [14].
Previous studies have shown that a sense of meaning in life is positively associated with psychological and physical health [15], but much less is known about its relation to physical (in)activity. To pursue active and healthy ageing, people should keep physically active, and older individuals with a sense of meaning in life are more likely to engage in healthy behaviours including physical activity. This analysis helps to shed some light on this association as a poor sense of meaning emerged as a factor significantly associated with physical inactivity. Finding meaning in life might be an antidote to depression in a variety of situations. A study of cardiac patients showed that individuals who feel their lives are meaningful may be motivated to comply with physicians’ advice and engage in positive health behaviours [16], and in a study of posttraumatic stress disorder, patients with higher meaning of life were more resistant to stress and more likely to recover.
Park [17] suggested that a sense of meaning and purpose in life might act as a strong source of motivation for preserving and protecting one's health. On the contrary, people who lack a sense of meaning may be insufficiently motivated to engage in healthy behaviours (e.g. physical activity) [18] or might even engage in harmful health behaviours. In fact, meaningfulness is one of the three components of Antonovsky's sense of coherence theory, which suggests that as individuals develop deeper meaning in their lives, they are more likely to apply strategies to cope with stress and move toward greater health.
The direction of the association between meaning in life and physical activity is not clear and may be bidirectional. Some studies report that being physically active as well as being healthy and with better mobility contribute to a sense of meaning in life [19, 20]. This was corroborated in the Evergreen project in Finland [21], which showed activity as a predictor of mental well-being, defined by depressive symptoms and meaning in life. A meaningful life may derive from the ability to be physically active—‘moving becomes meaning’ [22]. However, our results showed that meaning in life predicts less inactivity suggesting that the association might act in both directions; people with higher in meaning in life will be more active and engage in more activity, which in turns reinforces a sense of meaning and well-being.
A eudaimonic approach to well-being can also help explain the links between a sense of meaning in life and lack of engagement in physical activity. From this view, well-being is not rooted in positive emotion or happiness (hedonic well-being) but rather on fulfilling one's potential, having a sense of meaning and purpose in life, and maintaining positive relations with others [23]. Based on the work of Ryff and Singer [24], eudaimonic living can be understood as a personal process individuals engage in to grow toward their own greater potential, which can influence quality of life, health behaviours and physical health [25].
Eudaimonic well-being has been associated with reduced levels of markers for disease, such as lower levels of salivary cortisol, pro-inflammatory cytokines, cardiovascular risk factors and longer duration rapid eye movement sleep [26]. Much less is known about the relationships between eudaimonic well-being and health behaviours such as physical activity. The limited available evidence suggests that individuals engaging in physical exercise rate higher in purpose in life, positive relations and personal growth than non-exercisers. Also, people who experience the greatest gains in life engagement have significant increases in the level of physical activity [25]. Our findings are in line with this previous research.
Conversely, a poor sense of meaning in life may be affected by a poor health status, which indirectly influences engagement in physical activity. There is a reciprocal and complex relationship between eudaimonic sense and health; additional investigation of this issue is warranted. Furthermore, the mediating pathway of life meaning in health behaviours, such as regular physical activity, remains understudied. A limited unidirectional model (life meaning/well-being leading to health) is typically applied, and almost all evidence is correlational and short term in nature [23].
Depression was also a factor associated with physical inactivity in our analysis. Depressed people appear to be more inactive, producing a negative spiral of poor physical and mental health (e.g. depressive symptomatology), more dependency and less activity. Depressive mood entails a loss of meaning in life, which is corroborated by our results concerning inactivity. This finding provides support for the well-established link between physical activity and depression. Previous epidemiological studies have shown the association between physical inactivity and higher levels of depressive symptoms among older adults [27]. Depression also has been shown to increase the risk of a sedentary lifestyle [27] and falls [12], which are major causes of mortality, morbidity and premature nursing home placement for older adults. Moreover, physical inactivity has been shown to be a partial mediator of the relationship between depression and cardiovascular events and mortality [28].
Therefore, these findings suggest that preventive health and wellness interventions for older adults, particularly those with depressive symptoms, should include enrolment and participation in exercise programmes [28]. Cognitive behavioural therapy, especially in combination with exercise, can reduce symptoms of depression, recurrent falls and improve a sense of self-efficacy [29].
Some limitations of this study require discussion. Physical inactivity was not the primary outcome of the SHARE survey, and this variable was assessed with two self-rated questions. It is well known that people who volunteer to participate in research surveys like SHARE are likely to be more motivated and healthier than those who decline to participate [30]. As a result, a high proportion of older people with multiple chronic conditions might have been excluded.
These limitations could underestimate the prevalence of physical inactivity. Well-designed studies with different, and highly reliable, valid measures of physical inactivity and adherence to physical activity therefore are needed to confirm the extent of these findings.
In conclusion, our results showed that physical inactivity is multifactorial and include factors related to physical, cognitive and psychological conditions. Interventions aiming to improve physical exercise among older adults need to consider this diversity of factors.
Key points.
Physical activity is a key component of a healthy lifestyle, yet many older people are inactive.
Rates of self-reported physical inactivity in those aged 55 years and older varied from 5 to 29% across Europe.
Factors associated with inactivity included age, depression, physical limitations, poor sense of meaning in life, social support and memory loss.
Poor sense of meaning is an understudied factor with potential to drive novel interventions to enhance physical activity.
Supplementary Material
Supplementary data
Supplementary data mentioned in the text are available to subscribers in Age and Ageing online.
Conflicts of interest
None declared.
Funding
This article uses data from SHARE Wave 4 release 1.1.1, as of 28 March, 2013 (DOI: 10.6103/SHARE.w4.111). The SHARE data collection has been primarily funded by the European Commission through the 5th Framework Programme (project QLK6-CT-2001-00360 in the thematic programme Quality of Life), through the 6th Framework Programme (projects SHARE-I3, RII-CT-2006-062193, COMPARE, CIT5- CT-2005-028857 and SHARELIFE, CIT4-CT-2006-028812) and through the 7th Framework Programme (SHARE-PREP, N° 211909, SHARE-LEAP, N° 227822 and SHARE M4, N° 261982). Additional funding from the US National Institute on Aging (U01 AG09740-13S2, P01 AG005842, P01 AG08291, P30 AG12815, R21 AG025169, Y1-AG-4553-01, IAG BSR06-11 and OGHA 04-064) and the German Ministry of Education and Research as well as from various national sources is gratefully acknowledged (see www.share-project.org for a full list of funding institutions). This work also is supported by FCT/MEC through national funds and co-financed by FEDER under the Partnership Agreement (PT2020UID/MULTI/04378/2013 – POCI/01/0145/FERDER/007728) and by FCT (UID/Multi/04378/2013), COMPETE-FEDER.
References
- 1. World Health Organization Global Recommendations on Physical Activity for Health. Geneva: World Health Organization, 2010. [PubMed] [Google Scholar]
- 2. Peterson MJ, Giuliani C, Morey MC et al. . Physical activity as a preventative factor for frailty: the health, aging, and body composition study. J Gerontol A Biol Sci Med Sci 2009; 64a: 61–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lim SS, Vos T, Flaxman AD et al. . A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012; 380: 247–57. [DOI] [PubMed] [Google Scholar]
- 5. Harvey JA, Chastin SF, Skelton DA. How sedentary are older people? A systematic review of the amount of sedentary behavior. J Aging Phys Act 2015; 23: 471–87. [DOI] [PubMed] [Google Scholar]
- 6. Benedict C, Brooks SJ, Kullberg J et al. . Association between physical activity and brain health in older adults. Neurobiol Aging 2013; 34: 83–90. [DOI] [PubMed] [Google Scholar]
- 7. Gill SJ, Friedenreich CM, Sajobi TT et al. . Association between lifetime physical activity and cognitive functioning in middle-aged and older community dwelling adults: Results from the Brain in Motion Study. J Int Neuropsychol Soc 2015; 21: 816–30. [DOI] [PubMed] [Google Scholar]
- 8. Vermeulen J, Neyens J, van Rossum E, Spreeuwenberg M, de Witte L. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: a systematic review. BMC Geriatr 2011; 11: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Figueiredo DT, Poveda V, Paúl C, Santos-Silva A, Costa E. Predictors of difficulty in medication intake in Europe: a cross-country analysis based on SHARE. Aging Dis 2016; 7: 246–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tiedemann A, Paul S, Ramsay E et al. . What is the effect of a combined physical activity and fall prevention intervention enhanced with health coaching and pedometers on older adults’ physical activity levels and mobility-related goals?: Study protocol for a randomised controlled trial. BMC Public Health 2015; 15: 477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Malter F, Börsch-Supan A. SHARE Wave 4: Innovations & Methodology. Munich: MEA, Max Planck Institute for Social Law and Social Policy, 2013. [Google Scholar]
- 12. Christensen U, Stovring N, Schultz-Larsen K, Schroll M, Avlund K. Functional ability at age 75: is there an impact of physical inactivity from middle age to early old age. Scand J Med Sci Sport 2006; 16: 245–51. [DOI] [PubMed] [Google Scholar]
- 13. DiPietro L. Physical activity in aging: changes in patterns and their relationship to health and function. J Gerontol A Biol Sci Med Sci 2001; 56: 13–22. [DOI] [PubMed] [Google Scholar]
- 14. Fairhall N, Sherrington C, Kurrle S, Lord SR, Lockwood K, Cameron I. Effect of a multifactorial interdisciplinary intervention on mobility-related disability in frail older people: randomised controlled trial. BMC Med 2012; 10: 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Homan KJ, Boyatzis CJ. Religiosity, sense of meaning, and health behavior in older adults. Int J Psychol Relig 2010; 20: 173–86. [Google Scholar]
- 16. Holahan CK, Holahan CJ, Suzuki R. Purposiveness, physical activity, and perceived health in cardiac patients. Disabil Rehabil 2008; 30: 1772–8. [DOI] [PubMed] [Google Scholar]
- 17. Park CL. Religiousness/spirituality and health: a meaning systems perspective. J Behav Med 2007; 30: 319–28. [DOI] [PubMed] [Google Scholar]
- 18. Dyer C, Pickens S, Burnett J. Vulnerable elders: when it is no longer safe to live alone. JAMA 2007; 298: 1448–50. [DOI] [PubMed] [Google Scholar]
- 19. Kahana E, Lawrence RH, Kahana B et al. . Long-term impact of preventive proactivity on quality of life of the old-old. Psychosom Med 2002; 64: 382–94. [DOI] [PubMed] [Google Scholar]
- 20. Takkinen S, Ruoppila I. Meaning in life in three samples of elderly persons with high cognitive functioning. Int J Aging Hum Dev 2001; 53: 51–73. [DOI] [PubMed] [Google Scholar]
- 21. Lampinen P, Heikkinen R-L, Kauppinen M, Heikkinen E. Activity as a predictor of mental well-being among older adults. Aging Ment Health 2006; 10: 454–66. [DOI] [PubMed] [Google Scholar]
- 22. Lassenius O, Arman M, Söderlund A, Åkerlind I, Wiklund-Gustin L. Moving toward reclaiming life: lived experiences of being physically active among persons with psychiatric disabilities. Issues Ment Health Nurs 2013; 34: 739–46. [DOI] [PubMed] [Google Scholar]
- 23. Friedman HS, Kern ML. Personality, well-being, and health. Annu Rev Psychol 2014; 65: 719–42. [DOI] [PubMed] [Google Scholar]
- 24. Ryff C, Singer B. Know thyself and become what you are: a eudaimonic approach to psychological well-being. J Happiness Stud 2008; 9: 13–39. [Google Scholar]
- 25. Lewis P, Kimiecik J, Horn T, Zullig KJ, Ward RM. Can becoming my self influence my health?: exploring the effects of a eudaimonic-enhancement process on psychological indicators of well-being and physical activity. Appl Res Qual Life 2014; 9: 643–65. [Google Scholar]
- 26. Ryff CD, Singer BH, Love GD. Positive health: connecting well-being with biology. Philos Trans R Soc Lond B Biol Sci 2004; 359: 1383–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lindwall M, Larsman P, Hagger MS. The reciprocal relationship between physical activity and depression in older European adults: a prospective cross-lagged panel design using SHARE data. Health Psychol 2011; 30: 453–62. [DOI] [PubMed] [Google Scholar]
- 28. Win S, Parakh K, Eze-Nliam CM, Gottdiener JS, Kop WJ, Ziegelstein RC. Depressive symptoms, physical inactivity and risk of cardiovascular mortality in older adults: the Cardiovascular Health Study. Heart 2011; 97: 500–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Delbaere K, Close JC, Brodaty H, Sachdev P, Lord SR. Determinants of disparities between perceived and physiological risk of falling among elderly people: cohort study. BMJ 2010; 341: c4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Purdie D, Dunne M, Boyle F, Cook M, Najman J. Health and demographic characteristics of respondents in an Australian national sexuality survey: comparison with population norms. J Epidemiol Community Health 2002; 56: 748–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.