Abstract
Background
orthostatic hypotension (OH) is one out of many risk factors believed to contribute to an increased fall risk in elderly subjects but it is unclear whether an independent association between OH and falling exists.
Objectives
to perform an individual patient data (IPD) meta-analysis of prospective observational studies investigating the relationship between OH and falling.
Design
MEDLINE, EMBASE, the Cochrane Library and the abstracts of annual meetings of selected hypertension societies were searched. Both one-stage (analysing all IPD from all studies simultaneously) and two-stage (analysing IPD per study, and then pooling the results) methods were used, and both logistic and cox regression analyses were performed. The study protocol was published on PROSPERO (2015:CRD42015019178).
Results
from 34 selected abstracts, 6 studies were included. IPD were provided in 1,022 patients from 3 cohorts and were included in the IPD meta-analysis. The one-stage meta-analysis showed a significant relationship between OH and time to first fall incident (hazard ratio (HR) 1.52 (95% Confidence Interval (CI) 1.23–1.88)). No significant relationship between OH and falling was found in the one-stage logistic regression analysis and the two-stage logistic and cox regression analyses.
Conclusions
this IPD meta-analysis of prospective observational studies showed a clear and significant relationship between OH and time to first fall incident. Although the ORs of falling was not significantly different for patients with and without OH, a the cox regression analyses reporting HRs and including time to incident provided more clinically relevant information in present meta-analysis.
Keywords: Orthostatic hypotension; fall-risk; individual patient data; meta-analysis, older people
Introduction
The prevalence of orthostatic hypotension (OH), defined as a decrease in systolic blood pressure (SBP) by at least 20 mm Hg or a decrease in diastolic blood pressure by at least 10 mm Hg within 3 min after changing to standing position, increases with advancing age [1, 2]. OH is associated with cardiovascular disease and all-cause mortality, especially in elderly [3]. Furthermore, OH is presumed to be associated with an increased fall risk. Especially in frail elderly, OH and the subsequent increased risk of falling are considered to potentially lead to severe morbidity [4–7]. Equivalent to the aetiology of OH, fall risk is a complex and multifactorial phenomenon and OH is one out of many risk factors believed to contribute to an increased fall risk in elderly [4, 5].
Previous studies on the relationship between OH and fall risk were mostly performed in nursing homes and reported a positive association [8–10]. These results cannot be directly extrapolated to home dwelling elderly. Several reviews described a relationship, but did not perform a meta-analysis with the available data due to the small number of studies [4, 5].
It remains unclear whether there is an independent association between OH and falling. Therefore, we aimed to investigate whether OH contributes to falling in a meta-analysis of individual patient data (IPD). When IPD could not be retrieved, an alternative analysis was pre-planned that aimed to perform a meta-analysis of published study results.
Methods
Protocol
The pre-specified objectives, eligibility criteria, quality assessment and main analyses were published on PROSPERO (2015:CRD42015019178). PRISMA recommendations were followed throughout the design, implementation, analysis and reporting of this study [11].
A study was considered eligible if it was a prospective study that used the 1,996 consensus definition of OH [1, 2], included adults, and described the relationship between OH and fall incidents.
Data sources and searches
An electronic search of MEDLINE, EMBASE, the Cochrane Library and the abstracts of the 2012, 2013 and 2014 annual meetings of the International society of hypertension and American Society of Hypertension, was performed on 14 April 2015 and updated on 12 February 2016. The search was restricted to the English-language literature.
Additional studies were retrieved by hand searching references of selected articles. Clinical trials registries (www.clinicaltrials.gov, www.clinicaltrialsregister.eu and www.trialregister.nl) were searched for unpublished data. The complete search strategy is presented in Supplementary data, Appendix 1, are available in Age and Ageing online.
Study selection
Publications retrieved were imported in Endnote reference management software. Duplicates were removed and, two reviewers independently screened abstracts. For abstract selection and full-text selection inclusion criteria were used. The two reviewers extracted data and assessed the quality of each study. Differences in opinion between reviewers were resolved by consensus with a third reviewer. Two reviewers independently searched the trial registers.
Data collection and data items
From each study, data were extracted concerning; authors, year of publication, studied population, sample size, participants’ baseline characteristics (age, gender, blood pressure, OH, body mass index (BMI), medication, hypertension, Parkinson's disease); and fall incidents (yes/no).
Objective
The primary objective was to investigate whether OH contributes to risk of falling in a meta-analysis of IPD. When IPD could not be retrieved, an alternative analysis was pre-planned that aimed to perform a meta-analysis of published study results.
Missing data and multiple reports
Authors of the selected papers were contacted and asked whether they were willing to share (anonymous) IPD. In case IPD were not provided, published data were used.
Risk-of-bias assessment
The quality of each study was assessed using the Newcastle–Ottowa Scale (NOS) [12]. On a nine-point scale, the NOS evaluate the quality of observational studies on three broad categories: selection of the study groups, comparability of the groups, and ascertainment of the outcome of interest. Two reviewers independently assessed quality.
Statistical analysis
IPD analyses were performed using one-stage and two-stage methods [13–15]. In a one-stage method, analyses are performed with all IPD from all studies simultaneously, just as if they would belong to a single trial. In a two-stage method, analyses are first performed for all individual studies separately and then pooled into a meta-analysis for estimating the overall effect [16].
Univariate binary logistic regression analyses and subsequently multivariate binary logistic regression analyses were performed to assess the association of OH and falling (yes/no). A cox proportional hazard modelling was used to investigate the relation between OH and the first fall incident. Three different predefined models were used. In Model 1, unadjusted analyses were performed. In Model 2, only age and gender were taken into account as possible confounders. Model 3 was adjusted for age, gender, BMI, use of antihypertensive medication, SBP, diabetes mellitus (DM) and the total number of drugs. Logistic regression and cox proportional hazard analyses were performed in both one-stage and two-stage methods. Odds ratios (OR) and hazard ratios (HR) between patients with OH compared to patients without OH and 95% confidence intervals (CIs) were calculated. Because of the observational design of all studies, heterogeneity was expected, therefore initially a random effects model was used. In case of no significant heterogeneity, a fixed effect model was also applied. Heterogeneity was considered relevant if the P value was < 0.10 [17].
Logistic regression and cox proportional hazard analyses were performed using SPSS, version 22. Pooling of results and analyses regarding heterogeneity were performed with RevMan 5.3.
Sensitivity and subgroup analyses
In case of significant heterogeneity, sensitivity analyses were planned to explore the possible source of heterogeneity. In the one-stage method, predefined subgroup analyses were planned and registered at PROSPERO regarding the following variables: age, patient group, community-dwelling or nursing home patients, study quality and specific patients groups; e.g. hypertension, DM and Parkinson. The predefined subgroup analyses were only performed in case of an adequate number of patients to justify the subgroup analyses. In the two-stage method, subgroup and meta-regression analyses were considered with 10 or more included studies [17].
Results
Search results
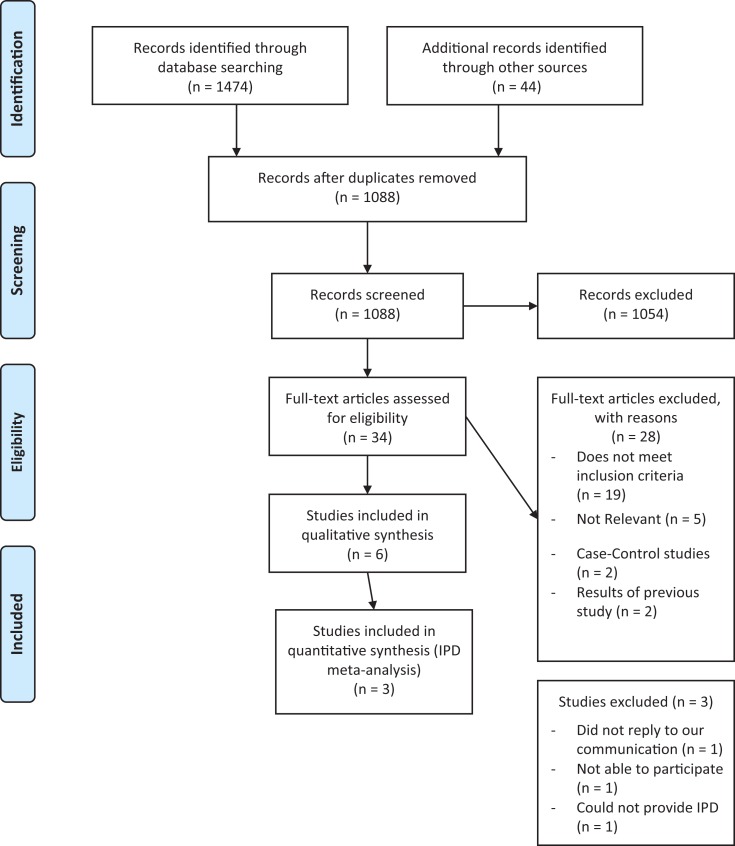
In total, 34 abstracts [6, 7, 9, 18–48] were selected for full-text evaluation, 6 of these were included in the meta-analysis (Figure 1) (see Supplementary data, Appendix Table 1, available in Age and Ageing online) [6, 7, 9, 19, 35, 37]. The authors of these studies were contacted for sharing IPD. IPD were provided from three studies [6, 7, 19]. The authors of one study did not reply to several attempts to make email (or telephone) contact [35], one was not able to participate in the study without giving a specific reason [37], and one could not provide IPD because data were no longer available [9]. Also, results as published could not be used from these studies because only HRs or ORs of subgroup analyses were published instead of results of the total study group regarding OH and falling. In addition, different endpoints were described and therefore these published results could not be included into the current meta-analysis.
Figure 1.
Flowchart.
Study characteristics
The baseline characteristics of the three included studies are shown in Table 1. The follow-up period in all included studies was approximately 1 year.
Table 1.
Baseline table of IPD
| Total (n = 1,022) | Allan et al., [19] 2009 (n = 216) | Gangavati et al., [6] 2011 (n = 736) | Heitterachi et al., [7] 2002 (n = 70) | |
|---|---|---|---|---|
| OH | 282 (28) | 178 (82) | 83 (11) | 21 (30) |
| Falling | 621 (61) | 129 (60) | 456 (62) | 36 (51) |
| Age (years) | 77 (73–81) | 76 (71–81) | 77 (74–82) | 76 (72–80) |
| Female gender | 602 (58%) | 85 (38%) | 461 (63%) | 56 (80%) |
| BMI (kg/m2) | 27 (24–29) | 25 (23–28) | 27 (24–30) | 26 (23–28) |
| DM, DM versus control | 177 (17%) | 18 (8%) | 149 (20%) | 10 (14%) |
| Antihypertensive medication | 624 (61%) | 75 (33%) | 519 (71%) | 30 (43%) |
| Number of medication | 10 (4–13) | 4 (2–6) | 10 (7–14) | 3 (2–5) |
| SBP (mm Hg) | 129 (119–143) | 135 (121–149) | 131 (119–140) | 125 (108–147) |
Data are means (±SD), medians (interquartile range) or n (%).
The participants of the three studies included in the IPD meta-analysis were all community-dwelling elderly [6, 7, 19]. The sample size of the cohorts ranged from 70 to 736 subjects. The median (interquartile range) age was 77 years (73–81). The prevalence of OH ranged from 11% to 82% and the prevalence of one or more fall incidents ranged from 51% to 62%. Fall incidents were retrieved by fall calendars [6], monthly questionnaires [7] or fall diaries [19].
Risk-of-bias assessment
The three studies all scored six out of nine stars, meaning that the overall quality of the included studies was moderate [6, 7, 19]. Because all studies had an equal NOS score, no subgroup analysis was performed regarding study quality. See Supplementary data, Appendix Table 2, available in Age and Ageing online for the detailed NOS score of the three included studies in the IPD meta-analysis.
Effect of OH on falling; one-stage method
No significant relationship between OH and falling was found in the one-stage logistic regression analysis. From the three studies, two studies [6, 19] collected data on the time to first fall incident (Table 2).
Table 2.
Adjusted ORs and HRs for the effect of OH on the risk of falling with IPD (one-stage method). The ORs can be interpreted as a measure of the association of OH to falling (the dependent variables). HRs refer to time to first fall incident.
| OR (95% CI) (three studies) | HR (95% CI) (two studies) | |
|---|---|---|
| OH (Model 1) | 0.92 (0.69–1.21) (n = 1022) | 1.30 (1.08–1.57) (n = 952) |
| OH (Model 2) | 0.94 (0.70–1.24) (n = 1022) | 1.30 (1.08–1.57) (n = 952) |
| OH (Model 3) | 1.21 (0.87–1.68) (n = 954) | 1.52 (1.23–1.88) (n = 884) |
Model 1, unadjusted. Model 2, adjusted for gender and age. Model 3, adjusted for gender, age, BMI, DM, antihypertensive medication, number of medication and SBP.
These two studies could be used in the Cox analyses regarding the relationship between OH and first fall incident. A significant relationship was observed in the Cox regression analysis, HR 1.52 (95% CI: 1.23–1.88). The chance of a first fall incident was 52% higher for patients with OH compared to those without. Supplementary data,Appendix Figure 1, available in Age and Ageing online shows the cumulative proportion of first fall incident for patients with and without OH.
Post hoc logistic regression analyses were performed with IPD of the same two studies as used in the Cox regression analysis; results did not relevantly change (Model 1: OR 0.87 (95% CI: 0.65–1.16), Model 2: OR 0.89 (95% CI: 0.66–1.20) and Model 3: OR 1.17 (95% CI: 0.83–1.65)).
Effect of OH on falling; two-stage method
For the two-stage method, ORs and HRs were analysed for each individual study separately and then pooled in the meta-analysis. A Cox regression analysis was only performed for two studies [6, 19] because Heitterachi et al. did not report the time to first fall incident in their study [7].
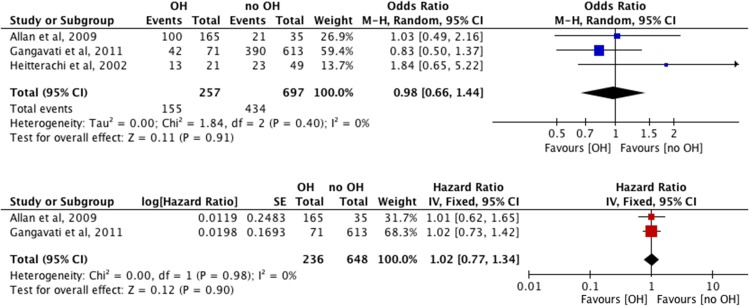
No significant relationships were seen between OH and falling in the three individual studies analysed separately and together, in both the logistic and Cox regression analyses (Figure 2).
Figure 2.
Forrest Plot of the adjusted ORs and HRs for the effect of OH on the risk of falling with IPD for each study (two-stage method). Adjusted for age, gender, BMI, DM, antihypertensive medication, number of medication and mean SBP.
As no heterogeneity (I2 = 0%) was observed, also a fixed effect model was applied. When pooling the ORs, no significant relationship was seen between OH and falling, with both the random and fixed effect models. The unadjusted and adjusted ORs of the fixed effect models were 0.95 (95% CI: 0.66–1.36; I2 = 0%; P = 0.39) and 0.98 (95% CI: 0.66–1.44; I2 = 0%; P = 0.40), respectively (Figure 2).
No significant relationship between OH and time to first fall incident was seen. The pooled unadjusted and fully adjusted HRs were 0.95 (95% CI: 0.74–1.22; I2 = 0%; P = 0.70) and 1.02 (95% CI: 0.77–1.34; I2 = 0%; P = 0.98), respectively (Figure 2).
Sensitivity analyses in both the logistic and Cox regression analysis were not performed because no heterogeneity was present.
Subgroup analyses
The three studies were comparable with respect to age, patient group, community-dwelling or nursing home patient and study quality, therefore subgroup analyses regarding this variables would not provide additional information and was thus not performed. A subgroup analysis on the covariate Parkinson's disease could not be performed due to a low number of patients with Parkinson's disease.
No significant relation was seen between OH and falling within the logistic regression analysis stratified to hypertension and diabetes (see Supplementary data, Appendix Table 3, available at Age and Ageing online). When stratified according to diabetes status within the cox regression analysis, a significant relation was seen within non-diabetic patients in all three models; unadjusted HR 1.29 (95% CI: 1.05–1.59), age- and gender-adjusted HR 1.29 (95% CI: 1.05–1.58), and fully adjusted HR 1.53 (95% CI: 1.21–1.93). The stratified analysis regarding to hypertension did not relevantly change the results (see Supplementary data, Appendix Table 3, available at Age and Ageing online). Interaction between diabetes and OH, and hypertension and OH, was analysed and no interaction was seen, P = 0.53 and P = 0.86, respectively. In the two-stage method no subgroup or meta-regression analyses were performed because of the low number of studies included.
Discussion
The one-stage meta-analysis showed a clear and significant relationship between OH and time to first fall incident. Although the OR of falling was not significantly different for patients with and without OH, the width of the 95% CI does not exclude a relevant clinical association. The results of the two-stage method, in which the results of the separate studies are pooled together, showed no significant relationship between OH and falling.
In the predefined protocol published on PROSPERO no preference was expressed about using logistic regression or cox proportional hazard analysis. Since both analyses can be useful to investigate the relationship between a causal factor and an outcome, both were used. While in the cox proportional hazard analysis the time to the first fall incident is the outcome measure from which the influence of OH on a fall incident is investigated, the ORs resulting from a logistic regression analysis only present cross-sectional information about this relationship after a (arbitrarily) fixed period of time. In the present meta-analysis, patients with OH had a 52% higher hazard on the first fall incident compared to patients without OH at any time during the follow-up period. Since patients can experience recurrent fall incidents over a longer period of time, a time to event analysis such as the cox regression analysis has a distinctive advantage over a binary logistic regression. In different studies, OH seems to be related to recurrent falling in elderly patient [13, 32]. All things considered, the cox proportional hazard analysis provided more clinical relevant information in the present meta-analysis [49, 50].
In an IPD meta-analysis, both one-stage and two-stage methods can be used. Although both types of analyses use similar IPD, the choice of a one- or two-stage method could result in different conclusions [15]. In a two-stage method, a summary effect size (OR or HR) is calculated for each study and secondly combined for all included studies, accounting for heterogeneity. In a one-stage method, all analyses are performed with all IPD from all studies simultaneously. Because a two-stage method assumes asymptotic normality and the one-stage method facilitates adjustment for confounders, this may result in different outcomes when a small number of studies are included. In the present meta-analysis this phenomenon was seen, HRs were different in one- and two-stage method, leading to different results. Debray et al. described differences between one- and two-stage methods and preferred the one-stage method, particularly in a meta-analysis with only a few studies [15]. Therefore, the conclusion in the present study is mainly based on the one-stage analyses.
This study is the first to aggregate results from observational studies into one IPD meta-analysis. In the prospective studies, inconsistent results regarding the relationship between OH and fall incidents were reported [6, 7, 9, 19, 35, 37] and had important limitations.
First, only in 1 out of the 6 selected studies the results for the total study population were reported [37]. The other selected studies mainly presented the results of subgroups or described different endpoints regarding the relationship between OH and fall incidents [6, 9, 19, 35, 37]. Maurer et al. [37] described no relation of OH and time to first fall incident in nursing home residents. Only HRs of systolic or diastolic blood pressure decrease at different time-points were presented. In the study of Gangavati, a significant relationship was only seen within a subgroup of participants with systolic OH at 1 min [6] and Allan described only symptomatic OH as a significant predictor of falls in patients with dementia [19]. Besides, Luukinen described the relationship of OH and falling in the subgroup recurrent fallers [35]; no significant association between OH and recurrent falling was seen. However, Ooi reported that OH was an independent risk factor for recurrent falls [9].
Second, two out of six studies did not adjust for important confounders [7, 37]. Heiterrachi described an increased risk of falls in older people with a decrease in SBP ≥20 mm Hg [7], but no confounders were taken into account. Maurer did also not adjust for any confounders; a post hoc analysis was performed in which was adjusted for available medications only [37].
Third, 2 out of the 6 selected studies did not use the International consensus definition of OH when analysing results [6, 37]. Maurer and Gangavati only described HRs at 1 or 3 min after standing separately, while the International consensus definition includes a decrease of blood pressure within 3 min [1].
Considering the results of all above-mentioned studies, none of the studies showed a clear relationship between OH and falling. Several reviews described a theoretical relationship, but could not perform a meta-analysis considering the low number of studies [4, 5].
Subgroup analyses
Only one-stage subgroup analyses regarding to diabetes and hypertension were performed. Only a significant relation was seen within non-diabetic patients in all three models; unadjusted HR 1.29 (95% CI: 1.05–1.59), age- and gender-adjusted HR 1.29 (95% CI: 1.05–1.58) and fully adjusted HR 1.53 (95% CI: 1.21–1.93). Although OH is considered to be a clinical manifestation of diabetic autonomic neuropathy in diabetic patients, a previous study has shown no significant relationship between OH and falling in diabetic patients. In present IPD meta-analysis, the proportion of diabetic patients is relatively small, 17% versus 83% non-diabetic patients. The group of diabetic patients is too small to draw definite conclusions.
Strengths and limitations
Despite the small number of studies, the current study is the only study, to the best of our knowledge that used the consensus definition of OH, which included a representative group of elderly, and adjusted for important confounders. No heterogeneity was observed and follow-up of all included studies was sufficient.
We acknowledge several limitations of our analysis. First, only a small number of studies and a limited number of patients were included in the meta-analysis. Unfortunately, one study did not report the time to first fall incident [7] and therefore the Cox regression analysis was only performed on two out of three studies [6, 19]. In addition, both results of the one-stage and two-stage methods showed wide CIs that indicate additional information is needed for more precise estimates [17]. Therefore, more prospective studies are needed for a precise estimate of the relationship between OH and falling.
Besides, because of the limited number of studies included into the meta-analysis no subgroup or meta-regression analyses could be performed. A subgroup analysis according to Parkinson's disease or dementia would have been useful since both could have influenced the relationship with falling [19]. In addition, subgroup analysis regarding study quality was preferred. However, all three included studies scored equal, allowing no subgroup analysis.
Also, a subgroup analysis regarding community-dwelling or nursing home patients was desirable since the positive association between OH and fall risk was frequently described in nursing home patients [8–10]. However, the studies including nursing home patients failed to deliver us the IPD. Therefore, in the present study only studies of community-dwelling elderly were included and the conclusions only refer to this group of elderly. Furthermore, OH was assessed within 3 min of postural change, thus not taking into account ‘delayed OH’. Also, we did not perform an analysis regarding recurrent falling. Only falling (yes/no) or time to first fall incident was analysed.
Finally, both one and two-stage IPD was performed, leading to different results. It is known that one or two-stage IPD occasionally could lead to different conclusions [15].
Conclusions
This IPD meta-analysis of prospective observational studies showed a significant relationship between OH and time to first fall incident. However, since the small number of prospective studies included in present meta-analysis, more of these studies are needed for a more precise estimate of the relationship between OH and falling.
Key points.
orthostatic hypotension (OH) is presumed to be associated with an increased fall risk.
A significant relationship exists between OH and time to first fall incident.
More studies are needed for a more precise estimate of the relationship between OH and falling.
Supplementary Material
Acknowledgements
The authors would like to thank Louise M. Allan, Lewis A. Lipsitz, Margaret Bryan, Robert McLean and Stephen Lord for providing individual patient data of their published studies [6, 7, 19].
Supplementary data
Authors consent
All authors read and approved the final manuscripts. We also state that this manuscript is not under review in another journal.
Conflicts of interest
All authors declare that they have no (financial) conflicts of interest.
Funding
This study had no external funding source. The MOBILIZE Boston Study was supported by the National Institute on Aging of the National Institutes of Health under Award Numbers AG04390 and AG041785.
Sponsor's role
This study had no external funding source.
Ethical approval and Clinical Trial registration
This study was performed in accordance with the Declaration of Helsinki. According to Dutch guidelines, this study did not fall under the scope of the Medical Research Involving Human Subjects Act, and therefore this study did not need a formal approval of an accredited medical ethics committee. All data were analysed anonymously. The eligibility criteria, outcomes, and analyses were pre-specified and published on PROSPERO (2015: CRD42015019178).
References
- (The Very Long List of References Supporting this Review Has Meant that only the Most Important are Listed here and are Represented by Bold Type Throughout the Text. The Full List of References is Available on the Journal website http://www.ageing.oxfordjournals.org/ as Appendix 2)
- 1. Lahrmann H, Cortelli P, Hilz M et al. EFNS guidelines on the diagnosis and management of orthostatic hypotension. Eur J Neurol 2006; 13: 930–6. [DOI] [PubMed] [Google Scholar]
- 2. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy The Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Neurology 1996; 46: 1470. [DOI] [PubMed] [Google Scholar]
- 3. Xin W, Lin Z, Mi S. Orthostatic hypotension and mortality risk: a meta-analysis of cohort studies. Heart 2014; 100: 406–13. [DOI] [PubMed] [Google Scholar]
- 4. Shaw BH, Claydon VE. The relationship between orthostatic hypotension and falling in older adults. Clin Auton Res 2014; 24: 3–13. [DOI] [PubMed] [Google Scholar]
- 5. Angelousi A, Girerd N, Benetos A et al. Association between orthostatic hypotension and cardiovascular risk, cerebrovascular risk, cognitive decline and falls as well as overall mortality: a systematic review and meta-analysis. J Hypertens 2014; 32: 1562–71; discussion 71. [DOI] [PubMed] [Google Scholar]
- 6. Gangavati A, Hajjar I, Quach L et al. Hypertension, orthostatic hypotension, and the risk of falls in a community-dwelling elderly population: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. J Am Geriatr Soc 2011. Mar; 59: 383–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Heitterachi E, Lord SR, Meyerkort P, McCloskey I, Fitzpatrick R. Blood pressure changes on upright tilting predict falls in older people. Age Ageing 2002; 31: 181–6. [DOI] [PubMed] [Google Scholar]
- 8. Graafmans WC, Ooms ME, Hofstee HM et al. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol 1996; 143: 1129–36. [DOI] [PubMed] [Google Scholar]
- 9. Ooi WL, Hossain M, Lipsitz LA. The association between orthostatic hypotension and recurrent falls in nursing home residents. Am J Med 2000; 108: 106–11. [DOI] [PubMed] [Google Scholar]
- 10. Rubenstein LZ, Josephson KR, Robbins AS. Falls in the nursing home. Ann Intern Med 1994; 121: 442–51. [DOI] [PubMed] [Google Scholar]
- 11. Stewart LA, Clarke M, Rovers M et al. Preferred reporting items for systematic review and meta-analyses of individual participant data: the PRISMA-IPD Statement. JAMA 2015; 313: 1657–65. [DOI] [PubMed] [Google Scholar]
- 12. Wells GA, Shea BJ, O'Connell D, et al. The Newcastle-Ottowa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-analyses. 2010; Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 13. Bekkering GE, Cools F, Aertgeerts B et al. [Meta-analyses based on individual patient data (IPD)]. Ned Tijdschr Geneeskd 2009; 153: 402–6. [PubMed] [Google Scholar]
- 14. Simmonds MC, Higgins JP, Stewart LA et al. Meta-analysis of individual patient data from randomized trials: a review of methods used in practice. Clin Trials 2005; 2: 209–17. [DOI] [PubMed] [Google Scholar]
- 15. Debray TP, Moons KGM, Abo-Zaid GMA, Koffijberg H, Riley RD Individual participant data meta-analysis for a binary outcome: one-stage or two-stage? 20130415 DCOM- 20131022(1932–6203 (Electronic)). [DOI] [PMC free article] [PubMed]
- 16. Bowden J, Tierney JF, Simmonds M, Copas AJ, Higgins JP. Individual patient data meta-analysis of time-to-event outcomes: one-stage versus two-stage approaches for estimating the hazard ratio under a random effects model. Res Synth Methods 2011; 2: 150–62. [DOI] [PubMed] [Google Scholar]
- 17. Higgins JPT, Green S, Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions: Version 5.1.0. The Cochrane Collaboration. http://www.cochrane-handbook.org. Updated March 2011. Chichester, England; Hoboken, NJ: Wiley-Blackwell; 2011.
- 19. Allan LM, Ballard CG, Rowan EN, Kenny RA. Incidence and prediction of falls in dementia: a prospective study in older people. PLoS One 2009; 4: e5521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kruse WH. Falls in community-dwelling older persons. J Am Geriatr Soc 1996; 44: 1010. [DOI] [PubMed] [Google Scholar]
- 35. Luukinen H, Koski K, Kivela SL, Laippala P. Social status, life changes, housing conditions, health, functional abilities and life-style as risk factors for recurrent falls among the home-dwelling elderly. Public health 1996; 110: 115–8. [DOI] [PubMed] [Google Scholar]
- 37. Maurer MS, Cohen S, Cheng H. The degree and timing of orthostatic blood pressure changes in relation to falls in nursing home residents. J Am Med Dir Assoc 2004; 5: 233–8. [DOI] [PubMed] [Google Scholar]
- 49. Green MS, Symons MJ A comparison of the logistic risk function and the proportional hazards model in prospective epidemiologic studies. 19831217 DCOM- 19831217(0021–9681 (Print)). [DOI] [PubMed]
- 50. Hosmer DWLS. Applied Survival Analysis: Regression Modeling of Time to Event Data. Chicester, UK: Wiley-Interscience, 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.