Abstract
Background:
Firefighters represent an occupational group at increased suicide risk. How suicidality develops among firefighters is poorly understood. The depression-distress amplification model posits that the effects of depression symptoms on suicide risk will be intensified in the context of anxiety sensitivity (AS) cognitive concerns. The current study tested this model among firefighters.
Methods:
Overall, 831 firefighters participated (mean [SD] age = 38.37 y [8.53 y]; 94.5% male; 75.2% White). The Center for Epidemiologic Studies Depression Scale (CES-D), Anxiety Sensitivity Index—3 (ASI-3), and Suicidal Behaviors Questionnaire—Revised (SBQ-R) were utilized to assess for depression symptoms, AS concerns (cognitive, physical, social), and suicide risk, respectively. Linear regression interaction models were tested.
Results:
The effects of elevated depression symptoms on increased suicide risk were augmented when AS cognitive concerns were also elevated. Unexpectedly, depression symptoms also interacted with AS social concerns; however, consistent with expectations, depression symptoms did not interact with AS physical concerns in the prediction of suicide risk.
Conclusions:
In the context of elevated depression symptoms, suicide risk is potentiated among firefighters reporting elevated AS cognitive and AS social concerns. Findings support and extend the depression-distress amplification model of suicide risk within a sample of firefighters. Interventions that successfully impact AS concerns may, in turn, mitigate suicide risk among this at-risk population.
1. Background
Suicide represents a significant public health concern, with over 40,000 individuals in the United States (U.S.) dying by suicide annually [1]. One segment of the U.S. population that research has revealed may be at a particularly increased risk for suicide is firefighters [2]. For example, Stanley et al. [3] examined 1027 current and retired firefighters throughout the U.S. and found career rates (i.e., those occurring throughout one’s tenure as a firefighter) of suicidal ideation and suicide attempts to be 46.8% and 16.4%, respectively. Martin et al. [4] examined 3036 firefighters from a single large, urban fire department and found rates of career suicidal ideation and attempts to be 9.8% and 1.4%, respectively.1 Finally, a study of women firefighters found rates of career suicidal ideation and attempts to be 37.7% and 3.5%, respectively [5]. Converging research has highlighted that protective service workers, a category inclusive of firefighters, evince relatively higher rates of death by suicide [6,7], underscoring the need to understand factors that may amplify suicide risk among firefighters in order to inform prevention and intervention efforts.
One construct that has demonstrated robust associations with suicide risk is anxiety sensitivity (AS) [8,9], defined as the fear of anxious arousal due to misinterpretations that these anxiety-related symptoms have negative ramifications [10–13]. The general AS construct has three lower-order factors: cognitive, physical, and social AS concerns [12]. While global AS concerns are linked to suicide risk [14], it appears that the association is most robust for AS cognitive concerns [9,15,16]. AS cognitive concerns are characterized by perceptions that anxiety-related sensations have catastrophic psychological outcomes, such as “going crazy.” Recently, Stanley et al. [17] found that AS—specifically, AS cognitive concerns—mediated the relationship between posttraumatic stress disorder symptoms (PTSD) symptoms (cf. anxiety-related sensations) and suicide risk among a sample of female firefighters; this finding was replicated in a sample of male firefighters [18]. In sum, AS cognitive concerns are implicated in increased suicide risk in the context of other psychiatric symptoms, and this effect is also relevant to conceptualizing suicide risk among firefighters.
However, risk factors for suicide and suicide-related outcomes do not operate in isolation, and it is important to understand how vulnerability factors interact to confer risk [19]. For example, a corpus of research has also implicated depression in the pathogenesis of suicide risk [20,21], although we emphasize that depression, too, is insufficient as a single-construct indicator of suicide risk [19]. Research has also demonstrated links between increased depression symptoms and suicide risk among firefighter samples [4]. Importantly, rates of depression appear to be elevated among firefighters [22,23], making depression a theoretically relevant construct to consider in examining suicide risk among this population. Given strong and replicated independent links between AS and suicide risk as well as depression and suicide risk, how might these domains interact to confer suicide risk?
Theoretical models may be illuminative in this regard. The depression-distress amplification model of suicidal behavior, proposed by Capron et al. [24], highlights that (1) uncomfortable sensations, such as difficulties concentrating, occur in the context of depression; (2) AS cognitive concerns (i.e., catastrophic reactions to the sensation of difficulty concentrating, such as fears of “going crazy”) intensify these sensations; (3) suicidal ideation emerges in the context of worsening depression symptoms; and (4) the effects of worsening depression symptoms on suicidal ideation are further amplified at higher levels of AS cognitive concerns. The model has been supported among samples of undergraduates reporting suicidal ideation [26], substance users in residential treatment [27], and psychiatric outpatients [24].
While Norr et al. [28] did not find support for the model in a sample of psychiatric outpatients, they did find an alternate model such that AS cognitive concerns were related to suicidal ideation via a mediational pathway of cognitive depression symptoms. The authors observed that although this finding is somewhat contrary to the core tenets of the depression-distress amplification model, suicidal ideation, which served as their outcome variable, may have been insufficient as a test of this model. Instead, the authors proposed testing suicide attempts as the outcome variable in the interaction between AS cognitive concerns and depression. Thus, moving forward, it will be important for research to examine the propositions of the depression-distress amplification model in the prediction of suicide risk potential more broadly. Given that past suicide attempts as well as levels of self-reported suicidal intent are each associated with the prediction of suicidal behaviors [19,33], a variable assessing these multiple aspects of suicide risk may enhance clinical relevance. Of note, no study of which we are aware has examined the depression-distress amplification model among firefighters, despite the potential importance of this model for informing suicide prevention and intervention work among this at-risk population.
1.1. The current study
The purpose of this cross-sectional study was to test predictions of the depression-distress amplification model of suicide risk among a large sample of firefighters. Specifically, we predicted that depression symptoms and AS cognitive concerns would interact to predict suicide risk, such that suicide risk would be potentiated at high levels of both depression symptoms and AS cognitive concerns. The current study extends the literature in two important ways. First, as noted, suicide risk appears to be elevated among firefighters, yet there is a dearth of data regarding suicidality among this particular population [2]; this study endeavors to help address that gap. Second, findings from past research have highlighted the importance of examining the depression-distress amplification model with regard to suicide risk (rather than suicidal ideation) as the criterion variable [28].
2. Materials and methods
2.1. Participants
Data from 831 firefighters were available for the current study, which was part of a larger ongoing project examining stress and health-related behaviors among firefighters in a large southern U.S. metropolitan area. In this department, all firefighters also perform emergency medical service (EMS) duties. To be included in the study, participants must have been current firefighters aged 18 years of age or older. See Table 1 for a summary of participant characteristics.
Table 1.
Firefighter Sociodemographic Characteristics (N = 831).
| Characteristic | Value |
|---|---|
| Age, mean (SD) [range: 20 y–63 y] | 38.37 y (8.53 y) |
| Sex | |
| Male | 785 (94.5%) |
| Female | 40 (4.8%) |
| Transgender | 6 (0.7%) |
| Race, no. (valid %) | |
| White/Caucasian | 625 (75.2%) |
| Black/African American | 106 (12.8%) |
| Native American or Alaska Native | 13 (1.6%) |
| Asian/Pacific Islander | 12 (1.4%) |
| Native Hawaiian or other pacific islander | 1 (0.1%) |
| Other | 74 (8.9%) |
| Ethnicity, no. (valid %) | |
| Hispanic or Latino/a | 216 (26.0%) |
| Not Hispanic or Latino/a | 615 (74.0%) |
| Education, no. (valid %) | |
| Did not complete high school | 11 (1.3%) |
| High school graduate/GED | 67 (8.1%) |
| Some college | 387 (46.6%) |
| College graduate | 366 (44.0%) |
| Total years as a firefighter, mean (SD) [range: 0 y–42 y] | 13.02 y (8.71 y) |
| Military status, no. (valid %) | |
| Active duty in the past (not now) | 188 (22.6%) |
| Active duty (now) | 4 (0.5%) |
| Participated in initial/basic training only | 20 (2.4%) |
| No military experience | 691 (74.5%) |
2.2. Procedure
Firefighters completed a voluntary online survey that included questions about stress and mental health. A department-wide email was sent to all firefighters, notifying them of the opportunity to complete an online research survey for one continuing education (CE) credit and a chance to win one of several raffle prizes (e.g., restaurant gift cards, movie theatre passes, drink tumblers). Monthly reminders regarding the survey were sent via the department-wide email notification system. All notification emails indicated that the purpose of the survey was to better understand how firefighters cope with stress and how much firefighters engage in health-related behaviors. The Department employs approximately 4035 firefighters. Data collection from this Department is ongoing; thus, a precise response rate is indeterminable. However, to date, 977 firefighters have responded to the survey, yielding a response rate of approximately 24.2%.
Firefighters were given access to the informed consent form and survey through an online fire department CE portal. After firefighters accessed the fire department CE portal, they were provided with a description of the survey and the opportunity to review the informed consent form, which delineated all aspects of the study. Participants who then indicated that they were interested in participating (by clicking ‘yes’) were automatically directed to the study informed consent form in Qualtrics. Firefighters had the option to discontinue participation at any time without penalty. The current study is based on secondary data analyses of firefighters who provided data on the variables of interest. The study has been approved by all relevant institutional review boards.
2.3. Measures
2.3.1. Demographic questionnaire
Participants reported demographic information including sociodemographic factors and information regarding fire department service (Table 1).
2.3.2. Anxiety Sensitivity Index-3 (ASI-3) [12]
The ASI-3 is an 18-item, self-report measure that assesses sensitivity to and discomfort with arousal or sensations associated with anxiety [13]. Items are rated on a scale from 0 (very little) to 4 (very much) regarding the degree to which individuals fear the potentially negative consequences of anxiety-related symptoms and/or sensations. The ASI-3 is a multidimensional measure that also includes three 6-item subscales: cognitive (e.g., “When my mind goes blank, I worry there is something terribly wrong with me”), physical (e.g., “It scares me when my heart beats rapidly”), and social (e.g., “It scares me when I blush in front of people”) concerns. While these subscales are highly correlated, factor analytic evidence suggests they are distinct constructs [12]. Subscale (range = 0–24) and total (range = 0–72) scores are calculated by summing relevant items, with higher scores indicating higher levels of AS. The ASI-3 has good internal consistency (α’s range from 0.76 to 0.86 for physical concerns, 0.79 to 0.91 for cognitive concerns, and 0.73 to 0.86 for social concerns), and good convergent, discriminant, structural, and criterion-related validity [12]. In this study, the ASI-3 total and subscale scoreswereusedaspredictorvariablesandtheinternalconsistencywasexcellent for the global score (α = 0.93) as well as the cognitive (α = 0.92) and physical (α = 0.90) sub-factors; it was good for the social sub-factor (α = 0.81).
2.3.3. Center for Epidemiologic Studies Depression Scale (CES-D) [34]
The 20-item CES-D, a scale established to measure the depressive symptomatology of community populations, was used to measure depressive symptom severity. Respondents report the frequency of self-perceived symptoms in the past week by using a 4-point scale (0 = “never or rarely”/<1 day per week to 3 = “almost all the time”/5–7 days per week), with higher total scores indicating higher depressive symptom severity. The CES-D also provides cutoff scores (e.g., 16 or greater) to aid in identifying individuals at risk for clinical depression, with good sensitivity and specificity and high internal consistency [35]. This instrument has been validated in a wide range of samples [36,37], including firefighters [38], and alpha coefficients ranging from 0.63 to 0.93 have been demonstrated across groups of healthy and clinical populations [34,39,40]. In the current study, the CESD-total score was used as a predictor variable to index depressive symptom severity and the internal consistency was good (α =0.82).
2.3.4. Suicidal behaviors questionnaire-revised (SBQ-R) [41]
The SBQ-R is a 4-item self-report measure used to assess global suicide risk. Each of the four items on the SBQ-R assess a different aspect of suicidality: Item 1 assesses lifetime suicide ideation and/or suicide attempts (i.e., “Have you ever thought about or attempted to kill yourself?”; 1 = Never to 4 = I have attempted to kill myself, and really hoped to die); Item 2 assesses the frequency of suicidal ideation over the past twelve months (i.e., “Have often have you thought about killing yourself in the past year?”; 1 = never to 5 = very often [5 or more times]); Item 3 assesses the threat of suicide attempt (i.e., “Have you ever told someone that you were going to commit suicide, or that you might do it?; 1 = No to 3 = Yes, more than once, but did not want to do it / Yes, more than once, and really wanted to do it); and Item 4 evaluates the self-reported likelihood of suicidal behavior in the future (i.e., “How likely is it that you will attempt suicide someday?”; 0 = never to 6 = very likely). Of note, Item 4 has been utilized in past research as a single-item indicator of suicidal intent [42,43], given the immense clinical significance of this variable regardless of the presence/absence of concomitant suicidal symptoms [44].
Total scores for the full SBQ-R range from 3 to 18, with higher scores indicating greater levels of overall suicide risk. Suggested cutoff scores to identify at-risk individuals and specific risk behaviors for the adult general population and psychiatric inpatients are ≥7 and ≥8, respectively [41]. The total SBQ-R demonstrates good psychometric properties for adult inpatient populations, including sensitivity (93%), specificity (95%), positive predictive value (0.87), and discrimination (0.89) for classifying suicidal and non-suicidal subgroups in cross-sectional analyses [41]. A recent systematic review of measures that assess suicidal thoughts and behaviors identified the SBQ-R to be a psychometrically sound measure to use in population-based research [45]. For the current study, the total SBQ-R score was used as an outcome variable to measure global suicidality and the internal consistency was acceptable (α = 0.77).
2.4. Data analysis strategy
First, variables were screened for outliers and violations of normality. The SBQ-R evinced violations of normality (skew = 3.015; kurtosis = 11.175). As such, we applied a log transformation to the SBQ-R, which reduced the skew (1.918) and kurtosis (3.179) to acceptable levels. The ASI-3 subscale variables were also examined for multicollinearity; values were within acceptable ranges (VIFs < 3), suggesting multicollinearity is not a problem for these variables. To test the interaction between CES-D depression symptoms and ASI-3 AS cognitive concerns in the prediction of SBQ-R suicide risk, we utilized linear regression modeling within the PROCESS macro for SPSS [46]. Predictor variables were centered around their means. Interactions were probed at the mean as well as low (−1 SD) and high (+1 SD) levels. We additionally tested alternative models: (a) the interaction of depression symptoms and AS physical concerns; (b) the interaction of depression symptoms and AS social concerns; and (c) depression symptoms as a mediator of the relationship between AS cognitive concerns and suicide risk [28]. For this mediation model, we utilized bootstrap mediation (5000 resamples) as described by Hayes [46]; a 95% bias-corrected confidence interval that does not cross zero indicates a statistically significant effect.
3. Results
Means, standard deviations, normality statistics, and intercorrelations between study variables are presented in Table 2. Results of regression analyses are presented in Table 3. The average scores of CES-D depression symptoms in our study were lower than the CES-D scores reported by Hom et al. [23] in a separate sample of 880 current and retired firefighters (M [SD] = 10.60 [7.80] vs. M [SD] = 13.49 [11.24], t[1709] = −6.145, p < 0.001). The average scores of ASI-3 global AS were also lower in our study than the ASI-3 scores reported by Stanley et al. [17] in a separate sample of 254 current women firefighters (M [SD] = 8.10 [10.46] vs. M [SD] = 16.92 [13.38], t [1083] = −10.974, p < 0.001), although gender differences in the AS construct may in part account for these differences [47–49]. Finally, the average scores of SBQ-R suicide risk were also lower than those reported by Stanley et al. [17] among that same sample (M [SD] = 3.85 [1.79] vs. M [SD] = 5.83 [2.90], t [1083] = −13.135, p < 0.001). In the present sample, a total of 15.9% (n = 132) and 8.2% (n = 68) of participants exceeded previously established cutoff scores indicating clinically significant depression symptoms [34,35] and suicide risk [41], respectively. Although 8.2% of the sample reported clinically significant suicide risk, 30.6% of respondents reported nonzero SBQ-R levels.
Table 2.
Study variable means, standard deviations, and intercorrelations (N = 831).
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | α | M | SD | Range |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. CES-D depression | – | 0.82 | 10.60 | 7.80 | 0–49 | ||||||
| 2. ASI-3 global AS | 0.391** | – | 0.93 | 8.10 | 10.46 | 0–72 | |||||
| 3. ASI-3 cognitive AS | 0.432** | 0.906** | – | 0.92 | 1.86 | 3.70 | 0–24 | ||||
| 4. ASI-3 physical AS | 0.287** | 0.878** | 0.771** | – | 0.90 | 1.87 | 3.57 | 0–24 | |||
| 5. ASI-3 social AS | 0.324** | 0.877** | 0.668** | 0.609** | – | 0.81 | 4.38 | 4.53 | 0–24 | ||
| 6. SBQ-R suicide risk | 0.370** | 0.270** | 0.254** | 0.127** | 0.315** | – | 0.77 | 3.85 | 1.79 | 3–16 | |
| 7. SBQ-R item 4 (suicidal intent) | 0.298** | 0.215** | 0.172** | 0.107** | 0.271** | 0.830** | – | – | 0.30 | 0.73 | 0–6 |
p < 0.05
p < 0.01.
AS = anxiety sensitivity; ASI-3 = Anxiety Sensitivity Index—3; CES-D = Center for Epidemiologic Studies Depression Scale; SBQ-R = Suicidal Behaviors Questionnaire—Revised (SBQ-R).
Table 3.
Results from Linear Regression Analyses Predicting Suicide Risk (N = 831).
| B | SE | p | |
|---|---|---|---|
| Model 1 (F [3827] = 44.549, p < 0.001; R2 = 13.9%; f2 = 0.161) | |||
| CES-D depression | 0.005 | 0.001 | <0.001 |
| ASI-3 cognitive AS | 0.001 | 0.002 | 0.598 |
| CES-D depression × ASI-3 cognitive AS ΔR2 due to the interaction: 1.5% | 0.001 | 0.0001 | <0.001 |
| Model 2 (F [3827] = 36.881, p < 0.001; R2 = 11.8%; f2 = 0.134) | |||
| CES-D depression | 0.006 | 0.001 | <0.001 |
| ASI-3 physical AS | 0.001 | 0.002 | 0.451 |
| CES-D depression × ASI-3 physical AS ΔR2 due to the interaction: <0.1% | <−0.001 | 0.001 | 0.685 |
| Model 3 (F [3827] = 59.021, p < 0.001; R2 = 17.6%; f2 = 0.214) | |||
| CES-D depression | 0.004 | 0.001 | <0.001 |
| ASI-3 social AS | 0.006 | 0.001 | <0.001 |
| CES-D depression × ASI-3 Social AS ΔR2 due to the interaction: 1.5% | 0.001 | 0.001 | <0.001 |
| Model 4 (F [5825] = 38.222, p < 0.001; R2 = 18.8%; f2 = 0.232) | |||
| CES-D depression | 0.005 | 0.001 | <0.001 |
| ASI-3 cognitive AS | −0.002 | 0.002 | 0.381 |
| ASI-3 physical AS | −0.006 | 0.002 | 0.006 |
| ASI-3 social AS | 0.010 | 0.001 | <0.001 |
| CES-D depression × ASI-3 cognitive AS ΔR2 due to the interaction: 1.2% | 0.001 | 0.001 | <0.001 |
| Model 5 (F [5825] = 35.208, p < 0.001; R2 = 17.6%; f2 = 0.214) | |||
| CES-D depression | 0.005 | 0.001 | <0.001 |
| ASI-3 cognitive AS | 0.001 | 0.002 | 0.564 |
| ASI-3 physical AS | −0.007 | 0.002 | 0.001 |
| ASI-3 social AS | 0.010 | 0.001 | <0.001 |
| CES-D depression × ASI-3 physical AS ΔR2 due to the interaction: <0.1% | <0.001 | <0.001 | 0.906 |
| Model 6 (F [5825] = 38.941, p < 0.001; R2 = 19.1%; f2 = 0.236) | |||
| CES-D depression | 0.004 | 0.001 | <0.001 |
| ASI-3 cognitive AS | −0.001 | 0.002 | 0.816 |
| ASI-3 physical AS | −0.006 | 0.002 | 0.004 |
| ASI-3 social AS | 0.009 | 0.001 | <0.001 |
| CES-D depression × ASI-3 social AS ΔR2 due to the interaction: 1.5% | <0.001 | <0.001 | <0.001 |
Significant effects are depicted in bold. Suicide risk was assessed via the Suicidal Behaviors Questionnaire—Revised (SBQ-R; Osman et al., 2001). AS=anxiety sensitivity; ASI-3=Anxiety Sensitivity Index—3; CES-D=Center for Epidemiologic Studies Depression Scale.
3.1. Primary analyses
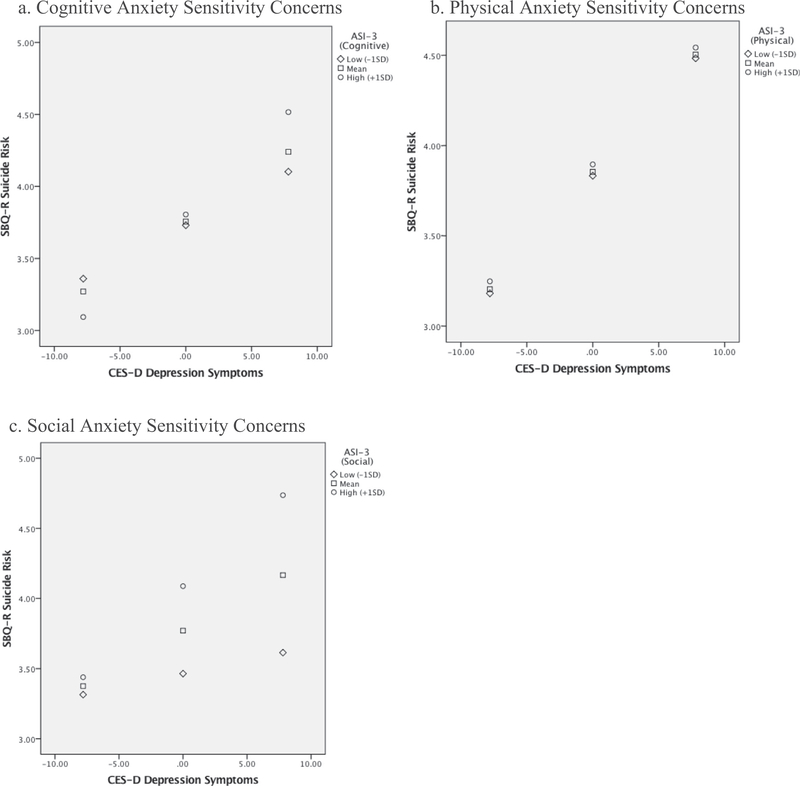
Model 1—the full model specifically testing the depression-distress amplification model—was statistically significant (F [3827] = 44.549, p < 0.001) and accounted for 13.9% of the variance in SBQ-R suicide risk (see Table 3). The interaction between CES-D depression symptoms and ASI-3 AS cognitive concerns was statistically significant (B = 0.001, SE = 0.0001, p < 0.001). The form of the interaction indicates that the effects of CES-D depression symptoms on SBQ-R suicide risk are potentiated when ASI-3 AS cognitive concerns are also elevated. When probed, an examination of the conditional effects indicates that the effects of CES-D depression symptoms on SBQ-R suicide risk were statistically significant at low (i.e., −1 SD: B = 0.004, SE = 0.001, p < 0.001), mean (B = 0.005, SE = 0.001, p b 0.001), and high (i.e., +1 SD: B = 0.007, SE = 0.001, p < 0.001) values of ASI-3 AS cognitive concerns (see Fig. 1a).2
Fig. 1.
Depiction of the interactions between depression symptoms and anxiety sensitivity subscales in the prediction of suicide risk. a. Cognitive Anxiety Sensitivity Concerns. b. Physical Anxiety Sensitivity Concerns. c. Social Anxiety Sensitivity Concerns.
3.2. Alternative moderation models
Although the depression-distress amplification model suggests that depression symptoms interact with AS cognitive concerns (and not AS physical or AS social concerns) to predict suicide risk, we tested the specificity of the model by also examining the interactions of depression symptoms with (a) AS physical concerns and (b) AS social concerns in the prediction of suicide risk. Model 2—the interaction of CES-D depression symptoms and ASI-3 AS physical concerns in the prediction of SBQ-R suicide risk—was statistically significant (F [3827] = 36.881, p < 0.001) and accounted for 11.8% of the variance in SBQ-R suicide risk (see Table 3). The interaction between CES-D depression symptoms and ASI-3 AS physical concerns was not statistically significant (B - 0.0001, SE = 0.0001, p = 0.685; see Fig. 1b).
Model 3—the interaction of CES-D depression symptoms and ASI-3 AS social concerns in the prediction of SBQ-R suicide risk—was statistically significant (F [3827] = 59.021, p < 0.001) and accounted for 17.6% of the variance in SBQ-R suicide risk (see Table 3). The interaction between CES-D depression symptoms and ASI-3 AS social concerns was statistically significant (B = 0.0004, SE = 0.0001, p < 0.001). The form of the interaction indicates that the effects of CES-D depression symptoms on SBQ-R suicide risk are potentiated when ASI-3 AS social concerns are also elevated. When probed, an examination of the conditional effects indicates that the effects of CES-D depression symptoms on SBQ-R suicide risk were statistically significant at low (i.e., −1 SD: B = 0.002, SE = 0.001, p = 0.024), mean (B = 0.004, SE = 0.001, p < 0.001), and high (i.e., +1 SD: B = 0.006, SE = 0.001, p < 0.001) values of ASI-3 AS social concerns (see Fig. 1c).
3.3. Exploratory moderation analyses
3.3.1. Specificity
In exploratory analyses, we tested additional models to demonstrate the robustness with which CES-D depression symptoms interacted with each ASI-3 AS subscale in the prediction of SBQ-R suicide risk, while also controlling for the effects of the other ASI-3 AS subscales. We did not present these analyses as primary, given the possibility for spurious findings when covarying for other ASI-3 subscales for which the intercorrelations are high (Table 2). Please see Table 3 (Models 4 to 6) for these results.
3.3.2. Suicidal intent
As noted, past research has utilized Item 4 of the SBQ-R as a single-item indicator of suicidal intent [42,43]. Consistent with this literature, we reconstructed Model 1 (AS cognitive concerns) and Model 3 (AS social concerns) by examining SBQ-R Item 4 as the criterion variable. AS cognitive concerns significantly interacted with CES-D depression symptoms to predict SBQ-R suicidal intent (B = 0.003, SE = 0.001, p < 0.001); when probed, an examination of the conditional effects indicated that the effects of CES-D depression symptoms on SBQ-R suicidal intent were significant at low (i.e., −1 SD: B = 0.016, SE = 0.004, p < 0.001), mean (B = 0.022, SE = 0.004, p < 0.001), and high (i.e., +1 SD: B = 0.032, SE = 0.004, p < 0.001) values of ASI-3 AS cognitive concerns. AS social concerns also significantly interacted with CES-D depression symptoms to predict SBQ-R suicidal intent (B = 0.003, SE = 0.001, p < 0.001); when probed, an examination of the conditional effects indicated that the effects of CES-D depression symptoms on SBQR suicidal intent were significant at mean (B = 0.014, SE = 0.003, p < 0.001) and high (i.e., +1 SD: B = 0.028, SE = 0.003, p < 0.001) values of ASI-3 AS social concerns, but not at low levels (i.e., −1 SD: B = 0.001, SE = 0.005, p = 0.822).
3.3.3. Alternate mediation model
Consistent with Norr et al. [28], we found that AS cognitive concerns were related to suicide risk via a mediational pathway of depression symptoms as measured by the CES-D total score (B = 0.0051, SE = 0.0011, bootstrap 95% CI = 0.0032, 0.0075). More specifically, Norr et al. [28] found that the cognitive symptoms of depression were a statistically significant mediator of the relationship between AS cognitive concerns and suicidal ideation; we, too, found support for this mediation model utilizing the CES-D depression/cognitive subscale (B = 0.0059, SE = 0.0012, bootstrap 95% CI = 0.0036, 0.0085), although we note that our criterion variable was global suicide risk (compared to suicidal ideation in Norr et al. [28]). To determine specificity of the proposed model, we switched the order of the proposed independent and mediator variables and found a statistically significant indirect effect when examining the CES-D total score (B = 0.0007, SE = 0.0014, bootstrap 95% CI = 0.0001, 0.0016) but not the CES-D depression/cognitive subscale (B = 0.0012, SE = 0.0008, bootstrap 95% CI = −0.0001, 0.0029) as the independent variable.
4. Discussion
The purpose of the current study was to test the depression-distress amplification model of suicide risk among a large sample of firefighters. Findings revealed that the effects of depression symptoms on suicide risk are amplified by AS cognitive concerns. This finding persisted even after controlling for other domains of AS concerns (i.e., physical, social), demonstrating the strength with which AS cognitive concerns may make an individual experiencing depressed mood vulnerable to suicidality. Overall, the pattern of findings in this study is consistent with propositions of the depression-distress amplification model, which has previously been supported among adolescents [25], undergraduates selected for suicide vulnerability [26], substance users in residential treatment [27], and psychiatric outpatients [24].
The present study extends previous research by examining the depression-distress amplification model among firefighters, specifically. Firefighters, as noted, represent a segment of the U.S. population at increased risk for suicide [2–5]. Understanding the role of transdiagnostic vulnerability factors, such as AS, in suicide risk formulation may have particular relevance to this population. For example, firefighters are routinely exposed to traumatic events as part of their occupational duties. Although the vast majority of individuals exposed to traumatic events do not go on to develop PTSD [50], the repeated traumatic exposures inherent in firefighting may serve to enhance the exacerbation of pre-existing vulnerabilities for both PTSD and suicidality, such as AS [51]. Thus, regarding firefighters, it is possible that the distress conferred by repeated occupational exposures (e.g., house fires, medical emergencies, suicide deaths of others; [52,53]) may increase levels of AS. This increase, in turn, may serve to amplify the effects of AS on depression symptoms (which themselves overlap, in part, with PTSD symptoms; [54]) in the prediction of suicide risk, consistent with the propositions of the depression-distress amplification model. We emphasize that these conjectures are speculative, and thus must undergo empirical scrutiny in future research.
We would be remiss if we did not underscore that, while support was found for the depression-distress amplification model of suicide risk, alternative configurations of depression symptoms and the lower order AS factors emerged. While there was no significant interaction between depression symptoms and AS physical concerns, there was a significant interaction between depression symptoms and AS social concerns in the prediction of suicide risk. The AS social concerns subfactor is characterized by thoughts such as, “I worry that other people will notice my anxiety” and “When I begin to sweat in social situations, I fear people will think negatively of me” [12]. Given that stoicism is valued within the fire service [55], any demonstration of fear or anxiety may contribute to perceptions of social isolation, which, in turn, may exacerbate depression and distress. Shame, too, is relevant to the AS social concerns factor. In a sample of military personnel, greater shame was found to be associated with more severe suicidal ideation [56]; however, we are unaware of any study examining this among firefighters.
Nevertheless, AS social concerns may be particularly important to understanding suicide risk among firefighters and may signal the need for a culture shift within the fire service to normalize emotional expressions [55,57]. There does not appear to be a replicable pattern of relative mean AS subscale scores across samples of undergraduates [26], psychiatric outpatients [24], male substance users [27], and firefighters (this study) testing the depression-distress amplification model. Within our sample, there were two findings that are worthy of further investigation regarding the role of AS social concerns: (1) the AS social concerns subscale mean in this sample was higher than the AS cognitive or physical concerns subscale means; and (2) the model testing the interaction between depression symptoms and the AS social concerns subscale explained descriptively more variance than did the model in which testing the interaction between depression symptoms and AS cognitive concerns (17.6% vs. 13.9%). These findings suggest that AS social concerns, perhaps in relation to stoicism and/or shame, may be particularly relevant to firefighters. Interestingly, past research has demonstrated that elevated AS social concerns are observed among individuals with social anxiety disorder (SAD) [58]. Thus, findings of the current study are consistent with epidemiological studies that have demonstrated that SAD predicts suicide attempts among ideators [31].
Further, although the depression-distress amplification model posits that AS cognitive concerns interact with depression symptoms to predict suicidality (i.e., a moderation model), as noted, Norr et al. [28] found support for a mediation model whereby AS cognitive concerns are related to suicidal ideation via cognitive symptoms of depression. In the present study, we found support for Norr et al.’s [28] alternate configuration of the model. Notably, we utilized global suicide risk (and not suicidal ideation) as the criterion variable, suggesting the depression-distress amplification model may benefit from refinement, pending replication. Future research in this area is necessary and encouraged. Importantly, we note that the results from these mediation models should be interpreted with caution given the cross-sectional nature of our data.
One finding that has remained consistent across investigations of the depression-distress amplification model is the central role of AS cognitive concerns in amplifying suicide risk [9]. We emphasize that the existing literature examining propositions of the depression-distress amplification model has exclusively utilized cross-sectional data [24–27]. Thus, the causal role of model components (i.e., depression symptoms, AS cognitive concerns) in suicide risk cannot be ascertained from the extant literature on the model. Interestingly, intervention studies that are focused specifically on the amelioration of AS cognitive concerns have consistently found that changes in AS cognitive concerns mediate changes in suicidality at follow-up [59–61]. Importantly, these interventions are brief in duration (e.g., 1 h) and deliverable through web-based interfaces [60]. Of note, although these interventions are designed to target AS cognitive concerns, comparable intervention effects have been observed for both AS cognitive (d = 0.85) and AS social (d = 0.94) concerns. In this regard, given the findings of the present study demonstrating associations between both AS cognitive and social concerns and suicide risk potential, these interventions might be relevant for firefighters as well. However, these interventions have not been tested among firefighters. Research among similar populations (e.g., military Veterans) has found these interventions to be highly acceptable [62], suggesting an avenue for future research.
Indeed, there are several factors related to the fire service that may make web-based interventions particularly advantageous. For one, past research among firefighters reporting a career history of suicidality has found that stigma-related concerns (e.g., concerns about reputation, embarrassment) differentiated treatment users from nonusers [57]; web-based treatments may help circumvent stigma-related barriers because an individual could complete these treatments at home. Further, costs of treatments are an important consideration [63], especially for large organizations with potential budgetary constraints; here, too, web-based treatments may help circumvent cost-related concerns to fire departments. In this regard, scalability could also be enhanced. A final consideration is that the brief nature of web-based interventions poses unique opportunities due to the time-sensitive environment of the fire service. In sum, findings from the current study underscore the potential applicability of interventions targeting AS cognitive concerns to addressing suicidality and suicide-related conditions among firefighters is worth further inquiry.
4.1. Limitations and future directions
This study is not without limitations. First, we examined study hypotheses among a single fire department in a large southern U.S. metropolitan city, and thus results may not generalize to the fire service at large. The generalizability of our findings is further hampered by the relatively low survey response rate (i.e., 24.2%); however, data collection in this Department is ongoing and thus it is likely that more firefighters will ultimately respond to the survey. Moreover, the department represents firefighters serving predominately in a full-time, paid capacity. This point is important in light of previous research demonstrating that career firefighters report, on average, less severe psychiatric symptoms than volunteer firefighters [64]. This may, in part, explain the relatively lower depression symptoms, AS concerns, and suicide risk scores in this sample compared to previous firefighter investigations; as noted above, this fire department has also proactively provisioned internal suicide prevention efforts [65]. Another related issue is that the firefighters in the present sample were all active duty and thus may have underreported psychiatric symptoms due to fears of negative job ramifications [66]. Relatedly, the variances accounted for by our models were modest, accounting for b20% of the variance in SBQ-R suicide risk. Although the variances accounted for were modest, the corresponding effect sizes were moderate in magnitude [67], signaling clinical relevance. We acknowledge, however, that the inclusion of other clinically-relevant variables would likely increase statistical power, underscoring the importance of not conceptualizing suicide risk within a vacuum [19].
An additional limitation of this study is that, although the SBQ-R is a psychometrically sound assessment of suicide risk [41,45], there are issues inherent in self-report of suicide risk, including the possibility of misclassification [68,69]. Moving forward, research is needed to triangulate suicide risk assessment methodologies (e.g., self-report, clinician interview, behavioral tasks). Additionally, the SBQ-R examines suicide risk broadly and future research utilizing a more clinically severe sample should also examine the depression-distress amplification model in the prediction of suicide attempts among a sample of suicide ideators. This would position the model within the ideation-to-action framework [30,70,71], allowing for a determination of the role of AS cognitive concerns in predicting the transition from thinking about suicide to actually engaging in suicidal behavior. A study of this magnitude would be enhanced by a longitudinal design; indeed, the cross-sectional nature of the present study minimizes the causal inferences that can be made. The cross-sectional data also do not capture the fluidity of suicide risk [72] or its risk factors [73], hampering our ability to identify AS cognitive concerns as a potential acute warning sign for suicide risk. Finally, although this study was the first study, to our knowledge, of the depression-distress amplification model to employ the CES-D, a gold standard measure of depression symptoms, future research may benefit from more nuanced assessments of depression (e.g., semi-structured clinical interview).
4.2. Conclusions
Among a large sample of firefighters, depression symptoms interacted each with AS cognitive concerns and AS social concerns to predict elevated suicide risk. These findings support and extend the depression-distress amplification model of suicide risk. AS concerns are a transdiagnostic risk factor that is amenable to therapeutic interventions. Importantly, interventions exist demonstrating efficacy in reducing AS cognitive concerns, and for which this reduction mediates suicidality outcomes. Findings of this study highlight that treating AS cognitive concerns may attenuate suicide risk among firefighters.
Acknowledgment
This work was supported in part by the Military Suicide Research Consortium (MSRC), an effort supported by the Office of the Assistant Secretary of Defense for Health Affairs under Award Nos. (W81XWH10-2-0181, W81XWH-16-2-0003). Opinions, interpretations, conclusions and recommendations are those of the authors and are not necessarily endorsed by the MSRC or the Department of Defense. The funders had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Footnotes
Conflicts of interest: none.
It should be noted that this fire department is at the forefront of efforts to prevent suicide in the fire service [65] and, thus, may represent a relatively healthier group of firefighters with regard to suicidal symptoms. An alternative yet compatible explanation for the relatively lower rates of suicidal symptoms found in this study is that the sample was composed exclusively of active duty firefighters, and active duty firefighters may underreport symptoms due to fears of being considered unfit for duty [66].
This pattern of findings remained unchanged when the non-transformed SBQ-R variable was used as the outcome variable. Here, too, the interaction was statistically significant in the expected direction (B=0.008, SE=0.002, p < 0.001).
References
- [1].Centers for Disease Control and Prevention [CDC]. WISQARS: web-based injury statistics query and reporting system; 2018.
- [2].Stanley IH, Hom MA, Joiner TE. A systematic review of suicidal thoughts and behaviors among police officers, firefighters, EMTs, and paramedics. Clin Psychol Rev 2016;44:25–44. 10.1016/j.cpr.2015.12.002. [DOI] [PubMed] [Google Scholar]
- [3].Stanley IH, Hom MA, Hagan CR, Joiner TE. Career prevalence and correlates of suicidal thoughts and behaviors among firefighters. J Affect Disord 2015;187:163–71. 10.1016/j.jad.2015.08.007. [DOI] [PubMed] [Google Scholar]
- [4].Martin CE, Tran JK, Buser SJ. Correlates of suicidality in firefighter/EMS personnel. J Affect Disord 2016;208:177–83. 10.1016/j.jad.2016.08.078. [DOI] [PubMed] [Google Scholar]
- [5].Stanley IH, Hom MA, Spencer-Thomas S, Joiner TE. Suicidal thoughts and behaviors among women firefighters: an examination of associated features and comparison of pre-career and career prevalence rates. J Affect Disord 2017;221:107–14. 10.1016/j.jad.2017.06.016. [DOI] [PubMed] [Google Scholar]
- [6].Tiesman HM, Konda S, Hartley D, Menéndez CC, Ridenour M, Hendricks S . Suicide in U.S workplaces, 2003–2010. Am J Prev Med 2015;48:674–82. 10.1016/j.amepre.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].McIntosh WL, Spies E, Stone DM, Lokey CN, Trudeau A-RT, Bartholow B. Suicide rates by occupational group — 17 states, 2012. Morb Mortal Wkly Rep 2016;65:641–5. [DOI] [PubMed] [Google Scholar]
- [8].Capron DW, Cougle JR, Ribeiro JD, Joiner TE, Schmidt NB. An interactive model of anxiety sensitivity relevant to suicide attempt history and future suicidal ideation. J Psychiatr Res 2012;46:174–80. 10.1016/j.jpsychires.2011.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Oglesby ME, Capron DW, Raines AM, Schmidt NB. Anxiety sensitivity cognitive concerns predict suicide risk. Psychiatry Res 2015;226:252–6. [DOI] [PubMed] [Google Scholar]
- [10].Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav Res Ther 1986;24:1–8. [DOI] [PubMed] [Google Scholar]
- [11].Taylor S Anxiety sensitivity: theory, research, and treatment of the fear of anxiety. New York, NY: Routledge; 1999. [Google Scholar]
- [12].Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, et al. Robust dimensions of anxiety sensitivity: development and initial validation of the anxiety sensitivity index-3. Psychol Assess 2007;19:176–88. [DOI] [PubMed] [Google Scholar]
- [13].Reiss S, McNally RJ. Expectancy model of fear In: Reiss S, Bootzin R, editors. Theor. Issues Behav. Ther San Diego, CA: Academic Press; 1985. p. 107–21. [Google Scholar]
- [14].Allan NP, Norr AM, Boffa JW, Durmaz D, Raines AM, Schmidt NB. Examining the unique relations between anxiety sensitivity factors and suicidal ideation and past suicide attempts. Psychiatry Res 2015;228:441–7. 10.1016/j.psychres.2015.05.066. [DOI] [PubMed] [Google Scholar]
- [15].Capron DW, Fitch K, Medley A, Blagg C, Mallott M, Joiner T. Role of anxiety sensitivity subfactors in suicidal ideation and suicide attempt history. Depress Anxiety 2012; 29:195–201. 10.1002/da.20871. [DOI] [PubMed] [Google Scholar]
- [16].Capron DW, Blumenthal H, Medley AN, Lewis S, Feldner MT, Zvolensky MJ, et al. Anxiety sensitivity cognitive concerns predict suicidality among smokers. J Affect Disord 2012;138:239–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Stanley IH, Hom MA, Spencer-Thomas S, Joiner TE. Examining anxiety sensitivity as a mediator of the association between PTSD symptoms and suicide risk among women firefighters. J Anxiety Disord 2017;50:94–102. 10.1016/j.janxdis.2017.06.003. [DOI] [PubMed] [Google Scholar]
- [18].Boffa JW, Stanley IH, Smith LJ, Mathes BM, Tran JK, Buser SJ, et al. Posttraumatic stress disorder symptoms and suicide risk in male firefighters: the mediating role of anxiety sensitivity. J Nerv Ment Dis 2018:1 10.1097/NMD.0000000000000779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, et al. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull 2017;143:187–232. 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]
- [20].Harris EC, Barraclough B. Suicide as an outcome for mental disorders: a meta-analysis. Br J Psychiatry 1997;170:205–28. 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- [21].Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med 2003;33:395–405. 10.1017/S0033291702006943. [DOI] [PubMed] [Google Scholar]
- [22].Carey MG, Al-Zaiti SS, Dean GE, Sessanna L, Finnell DS. Sleep problems, depression, substance use, social bonding, and quality of life in professional firefighters. J Occup Environ Med 2011;53:928–33. 10.1097/JOM.0b013e318225898f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Hom MA, Stanley IH, Rogers ML, Tzoneva M, Bernert RA, Joiner TE. The association between sleep disturbances and depression among firefighters: emotion dysregulation as an explanatory factor. J Clin Sleep Med 2016;12:235–45. 10.5664/jcsm.5492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Capron DW, Norr AM, Macatee RJ, Schmidt NB. Distress tolerance and anxiety sensitivity cognitive concerns: testing the incremental contributions of affect dysregulation constructs on suicidal ideation and suicide attempt. Behav Ther 2013;44: 349–58. 10.1016/j.beth.2012.12.002. [DOI] [PubMed] [Google Scholar]
- [25].Capron DW, Allan NP, Ialongo NS, Leen-Feldner E, Schmidt NB. The depression distress amplification model in adolescents: a longitudinal examination of anxiety sensitivity cognitive concerns, depression and suicidal ideation. J Adolesc 2015;41: 17–24. 10.1016/j.adolescence.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Capron DW, Lamis DA, Schmidt NB. Test of the depression distress amplification model in young adults with elevated risk of current suicidality. Psychiatry Res 2014;219:531–5. 10.1016/j.psychres.2014.07.005. [DOI] [PubMed] [Google Scholar]
- [27].Capron DW, Bujarski SJ, Gratz KL, Anestis MD, Fairholme CP, Tull MT. Suicide risk among male substance users in residential treatment: evaluation of the depression-distress amplification model. Psychiatry Res 2016;237:22–6. 10.1016/j.psychres.2016.01.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Norr AM, Allan NP, Macatee RJ, Capron DW, Schmidt NB. The role of anxiety sensitivity cognitive concerns in suicidal ideation: a test of the depression-distress amplification model in clinical outpatients. Psychiatry Res 2016;238:74–80. [DOI] [PubMed] [Google Scholar]
- [30].Klonsky ED, May AM, Saffer BY. Suicide, suicide attempts, and suicidal ideation. Annu Rev Clin Psychol 2016;12:307–30. 10.1146/annurev-clinpsy021815-093204. [DOI] [PubMed] [Google Scholar]
- [31].Cougle JR, Keough ME, Riccardi CJ, Sachs-Ericsson N. Anxiety disorders and suicidality in the National Comorbidity Survey-Replication. J Psychiatr Res 2009; 43(9):825 10.1016/j.jpsychires.2008.12.004. [DOI] [PubMed] [Google Scholar]
- [33].Brown GK, Henriques GR, Sosdjan D, Beck AT. Suicide intent and accurate expectations of lethality: predictors of medical lethality of suicide attempts. J Consult Clin Psychol 2004;72:1170–4. 10.1037/0022-006X.72.6.1170. [DOI] [PubMed] [Google Scholar]
- [34].Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Measur 1977;1:385–401. 10.1177/014662167700100306. [DOI] [Google Scholar]
- [35].Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging 1997;12:277–87. [DOI] [PubMed] [Google Scholar]
- [36].Morin AJS, Moullec G, Maïano C, Layet L, Just J-L, Ninot G. Psychometric properties of the Center for Epidemiologic Studies Depression Scale (CES-D) in French clinical and nonclinical adults. Rev Epidemiol Sante Publique 2011;59:327–40. 10.1016/j.respe.2011.03.061. [DOI] [PubMed] [Google Scholar]
- [37].Myers JK, Weissman MM. Use of a self-report symptom scale to detect depression in a community sample. Am J Psychiatry 1980;137:1081–4. 10.1176/ajp.137.9.1081. [DOI] [PubMed] [Google Scholar]
- [38].Chiu S, Webber MP, Zeig-Owens R, Gustave J, Lee R, Kelly KJ, et al. Validation of the Center for Epidemiologic Studies Depression Scale in screening for major depressive disorder among retired firefighters exposed to the world trade center disaster. J Affect Disord 2010;121:212–9. 10.1016/j.jad.2009.05.028. [DOI] [PubMed] [Google Scholar]
- [39].Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients. J Psychosom Res 1999;46:437–43. 10.1016/S0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- [40].Verdier-Taillefer M-H, Gourlet V, Fuhrer R, Alpérovitch A. Psychometric properties of the Center for Epidemiologic Studies-Depression Scale in multiple sclerosis. Neuroepidemiology 2001;20:262–7. 10.1159/000054800. [DOI] [PubMed] [Google Scholar]
- [41].Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The suicidal behaviors questionnaire-revised (SBQ-R): validation with clinical and nonclinical samples. Assessment 2001;8:443–54. 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- [42].Boffa JW, King SL, Turecki G, Schmidt NB. Investigating the role of hopelessness in the relationship between PTSD symptom change and suicidality. J Affect Disord 2018;225:298–301. 10.1016/j.jad.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Stanley IH, Joiner TE, Bryan CJ. Mild traumatic brain injury and suicide risk among a clinical sample of deployed military personnel: evidence for a serial mediation model of anger and depression. J Psychiatr Res 2017;84:161–8. 10.1016/j.jpsychires.2016.10.004. [DOI] [PubMed] [Google Scholar]
- [44].Chu C, Klein KM, Buchman-Schmitt JM, Hom MA, Hagan CR, Joiner TE. Routinized assessment of suicide risk in clinical practice: an empirically informed update. J Clin Psychol 2015;71:1186–200. 10.1002/jclp.22210. [DOI] [PubMed] [Google Scholar]
- [45].Batterham PJ, Ftanou M, Pirkis J, Brewer JL, Mackinnon AJ, Beautrais A, et al. A systematic review and evaluation of measures for suicidal ideation and behaviors in population-based research. Psychol Assess 2015;27:501–12. 10.1037/pas0000053. [DOI] [PubMed] [Google Scholar]
- [46].Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford Press; 2013. [Google Scholar]
- [47].Norr AM, Albanese BJ, Allan NP, Schmidt NB. Anxiety sensitivity as a mechanism for gender discrepancies in anxiety and mood symptoms. J Psychiatr Res 2015;62: 101–7. 10.1016/j.jpsychires.2015.01.014. [DOI] [PubMed] [Google Scholar]
- [48].Stewart SH, Taylor S, Baker JM. Gender differences in dimensions of anxiety sensitivity. J Anxiety Disord 1997;11:179–200. 10.1016/S08876185(97)00005-4. [DOI] [PubMed] [Google Scholar]
- [49].Zvolensky MJ, McNeil DW, Porter CA, Stewart SH. Assessment of anxiety sensitivity in young American Indians and Alaska natives. Behav Res Ther 2001;39:477–93. 10.1016/S0005-7967(00)00010-3. [DOI] [PubMed] [Google Scholar]
- [50].Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB . Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52:1048–60. 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- [51].Marshall GN, Miles JNV, Stewart SH. Anxiety sensitivity and PTSD symptom severity are reciprocally related: evidence from a longitudinal study of physical trauma survivors. J Abnorm Psychol 2010;119:143–50. 10.1037/a0018009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Kimbrel NA, Pennington ML, Cammarata CM, Leto F, Ostiguy WJ, Gulliver SB. Is cumulative exposure to suicide attempts and deaths a risk factor for suicidal behavior among firefighters? A preliminary study. Suicide Life Threat Behav 2016;46:669–77. 10.1111/sltb.12248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Kimbrel NA, Steffen LE, Meyer EC, Kruse MI, Knight JA, Zimering RT, et al. A revised measure of occupational stress for firefighters: psychometric properties and relationship to posttraumatic stress disorder, depression, and substance abuse. Psychol Serv 2011;8:294–306. 10.1037/a0025845. [DOI] [Google Scholar]
- [54].American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fifth edition: DSM-5. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- [55].Henderson SN, Van Hasselt VB, LeDuc TJ, Couwels J. Firefighter suicide: understanding cultural challenges for mental health professionals. Prof Psychol Res Pract 2016. 10.1037/pro0000072. [DOI] [Google Scholar]
- [56].Bryan CJ, Morrow CE, Etienne N, Ray-Sannerud B. Guilt, shame, and suicidal ideation in a military outpatient clinical sample. Depress Anxiety 2013;30:55–60. 10.1002/da.22002. [DOI] [PubMed] [Google Scholar]
- [57].Hom MA, Stanley IH, Ringer FB, Joiner TE. Mental health service use among firefighters with suicidal thoughts and behaviors. Psychiatr Serv 2016;67 10.1176/appi.ps.201500177. [DOI] [PubMed] [Google Scholar]
- [58].Rector NA, Szacun-Shimizu K, Leybman M. Anxiety sensitivity within the anxiety disorders: disorder-specific sensitivities and depression comorbidity. Behav Res Ther 2007;45:1967–75. 10.1016/j.brat.2006.09.017. [DOI] [PubMed] [Google Scholar]
- [59].Schmidt NB, Capron DW, Raines AM, Allan NP. Randomized clinical trial evaluating the efficacy of a brief intervention targeting anxiety sensitivity cognitive concerns. J Consult Clin Psychol 2014;82:1023–33. [DOI] [PubMed] [Google Scholar]
- [60].Schmidt NB, Norr AM, Allan NP, Raines AM, Capron DW. A randomized clinical trial targeting anxiety sensitivity for patients with suicidal ideation. J Consult Clin Psychol 2017;85:596–610. 10.1037/ccp0000195. [DOI] [PubMed] [Google Scholar]
- [61].Raines AM, Short NA, Allan NP, Oglesby ME, Schmidt NB. Examination of a brief anxiety sensitivity cognitive concerns intervention on suicidality among individuals with obsessive-compulsive symptoms. Contemp Clin Trials 2015;45:191–5. 10.1016/j.cct.2015.09.006. [DOI] [PubMed] [Google Scholar]
- [62].Short NA, Fuller K, Norr AM, Schmidt NB. Acceptability of a brief computerized intervention targeting anxiety sensitivity. Cogn Behav Ther 2016:1–15. 10.1080/16506073.2016.1232748. [DOI] [PubMed] [Google Scholar]
- [63].Cougle JR. What makes a quality therapy? A consideration of parsimony, ease, and efficiency. Behav Ther 2012;43:468–81. 10.1016/j.beth.2010.12.007. [DOI] [PubMed] [Google Scholar]
- [64].Stanley IH, Boffa JW, Hom MA, Kimbrel NA, Joiner TE . Differences in psychiatric symptoms and barriers to mental health care between volunteer and career firefighters. Psychiatry Res 2017;247:236–42. 10.1016/j.psychres.2016.11.037. [DOI] [PubMed] [Google Scholar]
- [65].Finney EJ, Buser SJ, Schwartz J, Archibald L, Swanson R. Suicide prevention in fire service: the Houston fire department (HFD) model. Aggress Violent Behav 2015;21: 1–4. 10.1016/j.avb.2014.12.012. [DOI] [Google Scholar]
- [66].Anestis MD, Green BA. The impact of varying levels of confidentiality on disclosure of suicidal thoughts in a sample of United States National Guard personnel. J Clin Psychol 2015;71:1023–30. 10.1002/jclp.22198. [DOI] [PubMed] [Google Scholar]
- [67].Cohen J Statistical power analysis for the behavioral sciences. Routledge Academic: New York, NY; 1988. [Google Scholar]
- [68].Hom MA, Joiner TE, Bernert RA. Limitations of a single-item assessment of suicide attempt history: implications for standardized suicide risk assessment. Psychol Assess 2016;28:1026–30. 10.1037/pas0000241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Millner AJ, Lee MD, Nock MK. Single-item measurement of suicidal behaviors: validity and consequences of misclassification. PLoS One 2015;10:e0141606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Klonsky ED, May AM. Differentiating suicide attempters from suicide ideators: a critical frontier for suicidology research. Suicide Life Threat Behav 2014;44:1–5. 10.1111/sltb.12068. [DOI] [PubMed] [Google Scholar]
- [71].Nock MK, Kessler RC, Franklin JC. Risk factors for suicide ideation differ from those for the transition to suicide attempt: the importance of creativity, rigor, and urgency in suicide research. Clin Psychol Sci Pract 2016;23:31–4. 10.1111/cpsp.12133. [DOI] [Google Scholar]
- [72].Bryan CJ, Rudd MD. The importance of temporal dynamics in the transition from suicidal thought to behavior. Clin Psychol Sci Pract 2016;23:21–5. 10.1111/cpsp.12135. [DOI] [Google Scholar]
- [73].Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, Nock MK. Examination of realtime fluctuations in suicidal ideation and its risk factors: results from two ecological momentary assessment studies. J Abnorm Psychol 2017. 10.1037/abn0000273. [DOI] [PubMed] [Google Scholar]