Abstract
Chronic disease carries high morbidity and mortality in the United States, with large racial and ethnic disparities observed in chronic disease. Physical activity and healthy food are vital for chronic disease prevention yet challenging to access in economically distressed areas. Public health prevention efforts have become particularly prominent within faith-based organizations over the last three decades. This manuscript describes the protocol of the Church Challenge, a multilevel cluster-randomized controlled nutrition and physical activity trial across 24 churches to reduce blood pressure by 6 mmHg among 576 residents in Flint, MI. The Church Challenge was developed using community-based participatory approaches and is rooted in a church-based program developed by and for primarily African-American Flint church congregations. This three-level intervention addresses health at the community (level 3), church (level 2), and individual (level 1) to reduce blood pressure, reduce chronic disease risk, and promote health equity and wellbeing in Flint. Churches are randomized in a 1:1 ratio to a 16-week physical activity and nutrition program or a 4-session health and wellness workshop. Flint is not a unique community but has a history of traumatic community wide events; even now, the public health infrastructure continues to be a challenge and distract residents from focusing on their health. This trial is highly significant and innovative because it uses a combination of evidence-based practices simultaneously supporting health behavior change for individuals and their faith organizations, and evaluates multilevel efforts to sustain long-term health promotion activities in vulnerable communities like Flint.
Keywords: Blood pressure, African Americans, Diet, Physical activity, Spirituality, Community-based
1. Introduction
Chronic disease carries high morbidity and mortality in the United States with large racial and ethnic disparities. Almost half of U.S. adults had one or more chronic conditions as of 2012 [1]. Heart disease and cancer account for 46.5% of all deaths in 2012 [2], and mortality data suggest the cardiovascular age-adjusted death rates are about 34% higher for blacks than the overall U.S. populations [3]. Cancer incidence rates from 2011 were highest for black compared to other men in the U.S [4]. Obesity is highly prevalent, and affected 47.8% of Non-Hispanic blacks compared to 32.6% of Non-Hispanic whites in 2011–2012 [5]. Preventable chronic disease costs continue to rise in the United States- 2010 heart disease and stroke costs were about $315.4 billion [6], 2010 cancer care costs were $157 billion [7], 2012 diabetes costs were $245 billion [8], and 2008 obesity costs were about $147 billion [9].
Physical activity (PA) and good nutrition [10] are among the most preventive behaviors against chronic disease [11]. Evidence suggests that population-level health changes can best be achieved by changing physical and social environments for four key risk factors: tobacco use, unhealthy diet, lack of physical activity, and harmful use of alcohol [12]. Physical activity-related facilities [13] and healthy food outlets [14] are significantly less likely to be located in lower-income neighborhoods and in neighborhoods with more African American residents. Yet residents of these neighborhoods have been repeatedly overlooked for prevention efforts, and are directed to seek treatment after developing more severe and debilitating forms of various chronic conditions [15].
Inequities in chronic disease persist in the city of Flint, a predominantly African American (56.6%) city which represents over a quarter of the Genesee county population. Improving population health in this community and other similar communities requires sustainable strategies that: (1) capitalize on existing resources within underserved communities (such as the strength of church-based social networks), and (2) establish policy changes that will support long-term health promotion, including the establishment of healthy food and activity options for all, rather than select (and typically more advantaged) residents. In response to this need, the Flint Center for Health Equity Solutions (FCHES) was established and funded by the National Institute on Minority Health and Health Disparities (NIMHD) in 2016, a transdisciplinary collaborative center based on two distinct multilevel research studies that address physical (the intervention described in this manuscript) and mental health.
2. Methods
2.1. Overview
The community-based participatory research project described in this protocol paper evaluates the effectiveness of an intervention developed by primarily African-American Flint church congregations for primarily African-American Flint church congregations. It also examines the capacities of these churches to improve their engagement with healthy activities and with policy advocacy related to their parishioners’ ability to access healthy food and safe exercise opportunities in their communities. Finally, it examines the critical issue of church-level and individual-level sustainment of behavior change. The randomized trial engages church members and church staff. Distinct from the trial, church leaders engage in policy training work to improve their surrounding communities.
The Church Challenge RCT works within churches (level 2) and with individuals (level 1) and is designed to examine the effectiveness of community-designed, community-based, multilevel physical activity and nutrition program (PANP) relative to an enhanced treatment as usual-the Health and Wellness Program (HWP) among 576 people from 24 primarily African-American Flint-area churches using a cluster-randomized controlled trial (RCT) design randomized by church. The primary hypothesis is that participants in the 16-week activity group will show a 6 mmHg reduction in blood pressure 6 months after initial program participation.
At the community level (level 3), members of the church leadership from both the HWP and PANP churches are invited to participate in a set of policy-advocacy workshops to improve healthy land use in Flint (e.g., by reintroducing a large scale grocery market to the city of Flint, providing sidewalks, bike lanes, and other safe places for physical activity that do not require cars for residents to access). We will examine how the third level of intervention increases churches’ capacity for and participation in community advocacy around policy issues to increase impact and sustainability. This policy-level involvement of churches is highly feasible because many of the primarily African-American churches in this economically distressed community are already policy-active. By supporting and expanding indigenous solutions, we will increase the likelihood of sustainability of changes at all levels.
2.2. Community-partnered approach
Faith Based Organizations (FBOs), including churches, are pillars of the African American community, championing for the systemic, institutional, community, and individual level changes that create healthy and supportive living conditions required to sustain long-term well-being, and particularly within underserved communities [16]. FBOs in Flint, Michigan work with local government, other community organizations, and with community residents to continuously assess the needs and resources available within the community. Churches often engage in public sector work, including advocacy or election related efforts to bring about social improvements. Building upon their internal resources, Flint FBOs often serve as distribution sites for donations that are not consistently provided by external and private organizations. The role of FBOs has become an even more critical source of providing information and motivation for the communities they serve. Therefore, FBOs are an important touchpoint for multilevel interventions in underserved communities.
Chronic disease prevention efforts have become particularly prominent within FBOs over the last three decades. Multiple faith-placed health promotion interventions for a variety of health issues have been implemented in FBOs across the United States. These programs have intentionally drawn upon the strength of congregations to promote community action and yield substantial participation for health promotion activities. FBOs have also developed their own health improvement efforts, including community health promotion activities developed in collaboration with local public (e.g. health departments, non-profit organizations) and private (e.g. water donations from concerned private businesses) organizations. For example, increased adoption of community based participatory approaches have yielded FBO engagement in Flint, Michigan on health topics including stroke prevention, sexual health, and health screenings, as well as organizing community health fairs. Local FBO networks have engaged local and state politicians to address major health concerns, including the recent water crisis in which unsafe lead levels were detected in resident households throughout the city. In sum, FBOs can facilitate healthy living practices, and have a distinct role in doing so as they are able to deliver spiritually based information to motivate healthy behaviors among congregants. Improving population health in this community and others requires sustainable strategies that: (1) capitalize on existing resources within underserved communities (such as the strength of church-based social networks), and (2) establish policy changes that will support long-term health promotion, including the establishment of healthy food and activity options for all, rather than select (and typically more advantaged) residents. This three-level community based participatory research study originated from previous work-the original Church Challenge, which was a response to a community wide public health survey that highlighted poor health outcomes particularly in the African American community. The original work led by faith community members of the Community Outreach for Family and Youth center, New Jerusalem Full Gospel Baptist Church, Bridges Into the Future, and other members of the Flint faith community to engage local African American churches in a competition to promote health weight loss among African American adults in Flint. Given the critical need for effective programs that yield clinical benefit to the most vulnerable and at risk communities, this innovative study was developed to test the effectiveness of the Church Challenge as a systematic and packaged set of evidence-based interventions that could be disseminated and administered across faith settings with high fidelity, and to enhance the capacity of community organizations to support chronic disease risk reduction while responding to the physical and psychological effects of managing a history of traumatic community events. The Church Challenge is cluster-randomized controlled trial (RCT; randomized at the church level) of a three-level intervention with community (level 3), churches (level 2), and individuals (level 1) to reduce blood pressure, reduce chronic disease risk, and promote health equity and wellbeing in Flint.
2.3. Community-participatory study investigative team
The original Church Challenge was a community-based participatory project led by faith community members of the Community Outreach for Family and Youth (COFY) Center, New Jerusalem Full Gospel Baptist Church, Bridges Into the Future, and other members of the Flint faith community to engage local African American churches in a competition to promote health weight loss among African American adults in Flint. The Church Challenge was originally conceived as an effort that would involve some professional staff of the COFY Center and would also rely on volunteers. COFY also runs on this principle and prides itself that church members’ volunteer efforts (and donations) largely run the Center. In keeping with this spirit but acknowledging the developmental contributions of the COFY research team members, this study has paid research staff at both Michigan State University and at COFY.
Our interdisciplinary team partners have expertise in human services provision, FBO and church leadership, health education, clinical expertise, fitness instruction, public health, statistics, and psychology. The university research staff manages the majority of the research administration, but COFY staff and university staff collectively developed the project budget, the assessment questionnaires and physiological components, and have together worked to implement the RCT. All staff will: (1) complete MSU's human subjects protection certification; (2) attend initial training sessions and follow-up refresher trainings; and (3) be regularly reminded that study participation is voluntary and that research information is confidential. We may also drive this message home by deputizing them to train each other and others in the voluntary and confidential nature of research participation. In this large (n = 576) study, staff members from COFY and the university will administer or support (1) informed consent; (2) conducting study survey assessments; (3) calling to remind participants of study assessments; (4) helping to locate missing participants; and other study tasks, as needed.
2.4. Merging CBPR approaches with RCTs
Community Engaged Research (CEnR) has increased over the last couple of decades. Community engagement has been implemented various research designs, across various disciplines, and systems including learning health systems [17]. The National Institutes for Health, Clinical Translational Science Awards Programs has championed CEnR and believe it will yield innovative solutions for improving efficiency, quality and impact for translation to improve the health of individuals and communities [17]. Community Based Participatory Research (CBPR) is an approach to research that ensures community involvement in all phases of the research process and falls on the continuum of CEnR [17]. Guided by nine core principles, CBPR looks to ensure equity in decision making, power dynamics, and ownership of data [18,19]. One of the critiques of CBPR projects is the time intensive activities needed to build and establish trusting relationship [18].
CBPR attempts to combine science and community practice with a result of mutual benefit for both the institution and the community [20]. Blending science and practice resulting in effective evidence-based approaches to translation is ideal; initiatives to merge CBPR and RCTs are designed to do just that. Conducting CBPR-RCT initiatives appears to be an interesting, yet, often difficult feat. RCTs by nature, tend to be more rigid in time lines and associated protocols which contradicts CBPR's organic, consensus time intensive approach [21]. Goodkind (2017) shares that there are epistemological, methodological, and ethical challenges to consider when conducting community-based RCTs [22]. However, in spite of the inherent tensions of merging CBPR approaches within an RCT framework, there are successful examples in which the marriage of both yielded positive outcomes [[23], [24], [25], [26], [27]].
2.5. Study setting
In the face of numerous strengths and assets, Michigan has large disparities in morbidity and mortality, most notably among African Americans and Hispanics and economically disadvantaged populations. Michigan's communities differ widely. There is a large portion of Michigan that is well-educated, generally healthy, and economically thriving. On the other hand, there are pockets of concentrated poverty, areas with high racial segregation within the state where morbidity and mortality are substantially higher than the state average. For example, an analysis of 2010 Census data found that the Flint metropolitan area has a black-white dissimilarity index of 67, making it the 14th most segregated city in the nation [28]. Within the state of Michigan (MI), Genesee County (the county that contains Flint) is ranked 81st of 82 counties for health outcomes in the Robert Wood Johnson Foundation County Rankings, and ranked 76th of 82 for health factors (health behaviors, clinical care, social and economic factors, physical environment) [29]. In MI, poor health appears to be correlated with areas of concentrated poverty. The poverty rate in Flint, MI is almost 2.5 times as large as the state poverty level, and twice as high as the poverty level for Genesee County, and Flint has zip codes with average life expectancy under 65 years. In addition, the increased poverty in Flint also appears to be correlated with the increasing proportion of Black residents, decreasing employment rate, and decreasing levels of educational attainment in the comparison to both the state and the county.
Many northern Flint area census tracts are food deserts-defined by the Department of Health and Human services as low-income (poverty rates of 20% or greater or median family income at or below 80% of the area median family income) and low-access (at least 500 people or 33% live more than 1 mile from a supermarket or large grocery store in non-metropolitan tracts) communities [30]. Barriers to fresh fruit and vegetables in retail outlets are more common in urban minority neighborhoods than other, including rural communities [31]. Previous research has highlighted the potential value of church based produce cooperatives [32]; other work showed that the introduction of a farmer's market in a “food desert” resulted in decreasing neighborhood food prices [33]. Food pantries have been introduced in the research literature to increase food access to otherwise unserved communities [34]. However, no published RCT has evaluated a multilevel intervention for healthy eating and physical activity that includes a food pantry to achieve sustained health improvements.
2.6. Guiding frameworks
We use the socioecological model to frame the significance of this study and specifically to address the various upstream and contextual factors that influence chronic disease risk and health behaviors. This study uses Bronfenbrenner's ecologic framework to conceptualize behavioral changes-specifically- healthy eating and physical activity [34] is a comparable ecologic model to the study of behavior change pointing to social determinants of health across four nested levels of impact (individual, social environment, community/physical environment, and macro/societal levels; see Fig. 1).
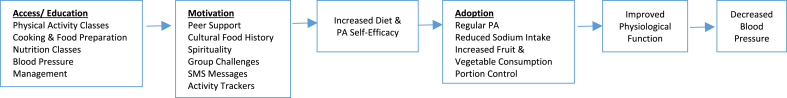
Fig. 1.
Conceptual model of the Church Challenge Physical Activity and Nutrition Program (PANP) intervention effects on blood pressure.
We use self-determination theory to inform the study design, incorporating a series of effective, theory-informed and evidence-based health promotion activities that have been previously shown to reduce chronic disease risk by promoting healthier diet and physical activity behaviors in combination with motivational and social support efforts [[35], [36], [37], [38], [39]]. Existing literature has shown the various components of this intervention to be individually effective for reducing chronic disease and hypertension risk, and in the most successful studies, program evaluation data suggest that the participants with the greatest health improvements made multiple lifestyle changes to improve their health and wellbeing. We use a multilevel and multidimensional intervention approach to evaluate the set of collective activities structured in the original community-developed Church Challenge, and centered this research study on investigating the effectiveness of this community-designed intervention program for creating clinical improvements in blood pressure among a primarily African American adult sample. The higher prevalence of hypertension within this population nationwide and persistent disparities in effective treatment and management of hypertension for African Americans compared to other racial/ethnic groups in the U.S. continue to reflect a critical need to extend the science of bringing effective interventions into regular practice.
2.7. Overall study design
The Church Challenge RCT uses a cluster-randomized trial design to promote healthy blood pressure and reduce chronic disease risk in Flint churches and individuals. Churches are randomized to the two study conditions after agreeing to participate in the research study: the Health and Wellness Program (HWP) and the Physical Activity and Nutrition Program (PANP). Randomization will be performed at the church level because much of the intervention is church-level. Church-level randomization will promote fidelity of the program within each church and will minimize contamination. Because our goal is to design a study that is most relevant to community and policy decisions, we decided to employ an enhanced treatment as usual (TAU) approach to defining the control condition. Using this HWP control condition will allow us to examine the naturalistic effects and costs of adding the multilevel Church Challenge intervention, and particularly to be consistent with the high level of ongoing health education happening in the Flint community as a result of the Flint Water Crisis. At the individual level (level 1), HWP church participants are invited to participate in 4 health workshops offered at their individual churches centered on chronic disease prevention and management, with topics selected by group of participants after initial study enrollment. PANP church participants commit to participate in a 16-week program with 1.5 h mandatory weekly workshops and asked to complete 150 min of physical activity each week. At the church level (level 2), in HWP churches, the health workshops offered to the study participants are open for attendance to anyone interested (in addition to the HWP study participants). PANP churches are provided with (1) health education materials for distribution within the church and (2) an invitation for 2–3 church representatives to receive motivational interviewing training to serve as a peer health counselor as a sustainable resource for the church. Leadership of all participating churches (HWP and PANP) are invited to participate in the policy advocacy workshops after participating in the RCT for 6 months and participate in a 24-month single-condition longitudinal evaluation. The evaluation assesses changes in policy and advocacy activities from baseline (start of the church's participation in the RCT, at the RCT primary (6 months) and secondary (12 months) endpoints.
The research team will work closely with members of the church who address health on behalf of the church (e.g. health ministry). Upon agreement to participate in the study, church leaders are asked to identify 2 members of their health ministry or church members to serve as their Church Challenge health team. The research team works with each church's health team over the study period to provide them with health education materials for dissemination at their churches and provide training for health team members to become peer counselors by the conclusion of the primary data collection period (6 months). As peer counselors, the health teams will have enhanced capacity to encourage healthy living behaviors both within their church community and beyond the walls of the church as well. Health team leaders will also directly engage with the research study participants, providing an opportunity for church-based conversations about practices that the study participants find helpful in promoting healthy living in their daily lives.
2.8. Interventions components
Each of the 24 churches will be randomized to participate in one of two programs, with 12 churches per condition: the control (Health and Wellness Program; HWP) or the active (Physical Activity and Nutrition Program; PANP) conditions. The research team will request the support of the church leaders and health teams to recruit 24 participants from each of their churches (or yield 24 study participants from combined efforts of smaller area churches). All assessments for HWP participants will be measured at their churches and all assessments for PANP participants will be measured at the Community Outreach for Family and Youth (COFY) center. The intervention components directly engage individuals (Level 1) and two groups of the church staff (Level 2), including church health teams (Level 2a) and church leaders (Level 2b).
3. Physical activity and nutrition program
3.1. Level 1: Individual Participants
The PANP treatment condition lasts 16 weeks. All participants of churches randomized to the PANP are asked to commit to at least 3 h of physical activity over the course of the week and to attend a 1.5-h session each week. Eight of the 16 weekly sessions are cooking workshops, 3 weekly sessions focus on health promotion, 3 weekly sessions offer group support, and 2 weekly sessions address spirituality and historical/cultural eating practices.
3.1.1. PANP weekly physical activity
Participants are expected to participate in 3 h of physical activity each week [40], including individual activity, community fitness activities, and project-sponsored classes. Participants are provided with a paper log to record their physical activity (and water intake) each week, and receive a fitness tracker by the fourth week to promote physical activity [41,42]. Community fitness activities are introduced to the participants at the initial introductory workshop, including a variety of free fitness activities (e.g. water aerobics, yoga, group fitness, etc.) sponsored by Commit 2 Fit of the Greater Flint Health Coalition (www.commit2fit.com). Participants are also invited to attend fitness classes led by the study team fitness instructors from the COFY center that follow the structure of previous evidence-based fitness programs to enhance health of older adults [43]. Classes last 1 h each and are offered during day and evening sessions on 2–3 weekdays each week and are commonly held immediately before or after the weekly workshops.
3.1.2. PANP Biweekly cooking workshops
The workshops focus on healthy food preparation and consumption through cooking demonstrations, recipe and ingredient provision [44], and nutrition education [45,46]. The cooking workshops are led by co-instructors, including one expert community partner strongly motivated to cook and prepare food, and including one nutrition instructor from our county Michigan State University Extension office. The instructors provide participants with a hands-on opportunity to prepare recipes that align with the Dietary Approaches to Stop Hypertension (DASH) diet recommendations (www.nhlbi.nih.gov/health-topics/dash-eating-plan). The recipes center on preparing vegetables and fruit with low sodium content. Participants work in small groups of 3–5 people to prepare the recipes, including food preparation, and cook the dishes in electric skillets. A select number of recipes are also included that require cooking in a conventional oven. All materials for the cooking classes were identified by the research team or through (evidence-based) nutrition resources available via MSU-Extension. During the recipe preparation, the instructors address the nutritional content of each recipe, highlighting strategies for the participants to use to flavor their foods, use healthy cooking techniques (e.g. baking, roasting, etc.) and limit sodium content. During each workshop, participants receive the key ingredients of the recipes they prepared during the cooking workshop to take home. They also periodically receive food preparation aids such as portioned plates (MyPlate) and measuring utensils, etc.
3.1.3. PANP health promotion workshops
These three workshops are held at the start (weeks 1–2), middle (weeks 4–5), and end (weeks 15–16) of the intervention. The first workshop defines hypertension and the roles of lifestyle behaviors including diet and physical activity in addition to clinical treatment for preventing and managing hypertension. The second workshop teaches participants about the use of technology and activity trackers to support and track their personal lifestyle behaviors around diet and physical activity. The participants receive fitness activity trackers (and instruction for use) during this workshop. The third workshop examines diet and nutrition as lifestyle behaviors that prevent and support hypertension management, and addresses the nutrition practices (e.g. grocery shopping, reading nutrition labels, portion control, sodium and sugar intake, meal preparation, etc.) presented and used in the cooking workshops. The workshops are led by a combination of study team staff and Flint-based MSU medical students.
3.1.4. PANP health promotion SMS messages
PANP participants receive weekly text message reminders to attend the 16-week program activities. If participants miss a weekly workshop, the research team provides a reminder phone call to the participant. PANP health teams from each church will contact the study participants from their churches between weeks 19–23 and ask the participants about the behaviors they have maintained since the final week of intervention activities (week 16). The health teams will also issue a final challenge competition to their participants with the winner announced at the 6 month data collection. At week 16, PANP participants receive information about the nutrition and physical activity classes and are invited (not mandatory) to attend ongoing classes to continue supporting their diet and physical activity behaviors.
3.1.5. PANP church group support workshops
The three support workshops provide an opportunity for the participants to discuss successes, challenges, barriers, and opportunities to reduce their chronic disease risk, increase their physical activity, improve their dietary patterns, and promote health for themselves and their families [47,48]. Participants are asked about the intervention activities they found most beneficial, their preparation of class recipes at home, and behaviors they have adopted outside of the intervention activities. The study team staff work with the groups to identify solutions challenges and barriers raised by the participants.
3.1.6. PANP spirituality and historical/cultural eating workshops
All participants have two of these workshops and are presented with information about historical and cultural eating patterns common to African American communities and how they have been informed by evolving spiritual beliefs and cultural practices [49,50]. The two sessions are led by a 4-person team of African American history experts local to Flint with expertise in teaching cultural awareness, self-love, and self-care. The instructors provide instruction and create a group conversation to engage the participants.
3.1.7. PANP competition challenges
The PANP participants are invited to participate in 5 competitions-“challenges”- over the 16-week intervention duration. The challenges are identified during the weekly workshops; two of the challenges are for the participants within the same weekly workshop to complete, and three of the challenges are for all of the active participants of that wave. The challenges center on participants' diet and physical activity behaviors; suggested challenge activities have included steps taken, recipe revisions, and water intake but additional challenges identified and recommended by the participants are encouraged.
3.1.8. Tips4Health text messaging
All study participants receive text message reminders for attending intervention activities and are also offered the option to participate in Tips4Health (www.tips4health.org), a text messaging program that delivers multiple weekly text messages focused on diet, physical activity, or smoking behaviors [51,52]. Participants receive a handout with instructions to enroll on the texting program at the baseline data collection and receive additional support for enrollment during the health promotion workshop centered on technology (in weeks 4–5).
3.2. Level 2a: Church health teams
The health team members are asked to endorse the Church Challenge through study participant recruitment, collect the names and contact information for church community members interested in participating in the study and provide the information to the research team, participate in 4 monthly meetings or health workshops with their church study participants, participate in 1–2 additional health-focused events at 6 months and 12 months from the study start for participant data collection, review and share health promotion materials for dissemination within the church, and complete 3 organizational assessments about (1) health and wellness activities at church and (2) how church leadership builds capacity to support church-based health and wellness activities in partnership with the church leadership. Optional activities that are offered to the health teams are training to become peer counselors to promote healthy diet and physical activity lifestyle behaviors, training to contact participants with this information, and training in responsible conduct of research.
3.2.1. Health team peer counseling training
Peer counseling is a confidential, one-on-one activity to help motivate church members to live a healthier life. The church health teams will be offered an optional free 4-h training to serve as peer counselors within their church during and after study completion. The peer counseling skills are based on motivational interviewing and centered on diet and physical activity behaviors [53,54]. The training will be offered to the health teams after the 16-week intervention for the health teams of the churches participating in the PANP. Peer counselors meet in person or by phone to provide support to members who want to see how a healthy lifestyle can fit into their daily lives. The church member and peer counselor come up with an action plan for eating healthier, getting more physical activity, or another health behavior the member is interested in doing. This approach empowers people to take more control over their health.
3.3. Level 2b: Church leadership
As the church leaders commit to the study, the research team will ask each church leadership team to identify their church health team. The church leaders are asked to endorse the research study, recruiting church members to participate, encourage study participants to complete data collection during the study, participate in cooking event(s) with church study participants, promote health and distribute health education materials within the church, complete organizational assessments prior to recruiting participants and after data collection at the primary endpoint at 6 months, select or develop 6 spiritual messages that incorporate bible verses and link health and spirituality and attending periodic meetings with the research team, health team, and other pastors to promote nutrition and physical activity in their church and larger community. They are also asked to connect and support a relationship to promote health between the research team with two of the church health leaders (health team).
4. Health and Wellness Program
4.1. Level 1: Individual Participants
Enrolled HWP participants are offered four health workshops lasting 1 h each, with the various health topics identified by the health team. Workshops are led by medical and academic health experts local to the community. Initial workshop topics offered to the HWP participating churches include stroke awareness, oral care, eye care, diabetes, mental health, stress management, and arthritis. These health workshops are also open for attendance by HWP churches congregants who are not enrolled in the RCT.
4.1.1. Tips4Health text messaging
All study participants receive text message reminders for attending intervention activities. All study participants are offered the option to participate in Tips4Health (www.tips4health.org), a text messaging program that delivers multiple weekly text messages focused on diet, physical activity, or smoking behaviors [51,52]. All HWP and PANP participants receive a handout with instructions to enroll on the texting program at the baseline data collection. PANP participants receive additional support for enrollment during the health promotion workshop centered on technology (in weeks 4–5). HWP participants receive a handout to enroll in the texting program.
4.2. Level 2a: Church health teams
The HWP health team members are asked to complete all of the same activities, but specifically with the HWP content, as the PANP church health teams. The peer counselor training will be offered to the HWP health teams after the 6-month data collection.
4.3. Level 2b: Church leadership
The HWP church leaders are asked to do many of the same activities as the PANP church leaders, but specifically encourage participation for the HWP participants in the health workshops and data collection points. These leaders also develop spiritual messages that incorporate bible verses and link health and spirituality and attending periodic meetings with the research team, health team, and other pastors to promote wellness in their church and larger community. They are also asked to connect and support a relationship to promote health between the research team with two of the church health leaders (health team).
4.4. Study participants
Because the Church Challenge involves church-level components, any (1) cognitively intact adult, (2) aged 18 or older, (3) who self-reports having medical clearance for exercise, (4) from a participating Church or FBO is eligible. Potential participants who, at baseline, are determined to have a clinical condition requiring immediate care (severe hypertension of 200+, for example) will be referred to their providers, and will be required to provide a letter of support from their provider to participate in the study. Given that we are targeting primarily African-American Flint-area churches, we anticipate that a large majority of participants will be African-American. However, individuals from participating churches of other races and ethnicities can be enrolled in the study. Furthermore, because we are randomizing at the church level, congregants may participate in church-level Church Challenge activities (like the weight-loss competition) without participating in the research study, per se.
4.5. RCT church recruitment
Led by the faith leaders on the research team, we will contact pastors, administrative teams, and health committees for existing churches throughout Flint and Genesee County. We will connect with churches with initial contact through churches administration, connection with existing church and larger FBO health committees, and congregants. Building upon our church and FBO study team partners’ extensive contact network of FBO pastors, we will contact the pastors and their administrative teams to establish conversations. We will also build upon the network of our CBOP community partners to contact congregants of FBOs for which we are unable to connect with their pastors, administrators, or health committees. There are at least 432 Protestant and Catholic Churches in Genesee County, and over 160 are African American Churches. Recruitment of churches to participate in the project began within 1 year of starting the project and is expected to continue on a rolling basis during the RCT in order to achieve the expected sample size.
Each church that reports serving primarily African-American Flint community residents (operationalized as the majority of those they serve are African-American) will be invited to participate in the program. This procedure offers the opportunity to have a variety of large and small congregations involved in the project, and further offers the opportunity to have representation of various small communities within the city of Flint. The program will be described as a four years commitment to promoting healthy living, through physical activity and healthy eating within the organization. FBOs will each be asked to establish or share information about their appointed church health team; and will be offered assistance to establish such a team if warranted. Participating leaders and health teams of each participating FBO will receive honorariums for their participation. We anticipate that we will engage at least 45 churches in these activities, with the goal of retaining at least 24 churches for participation in the RCT.
4.5.1. RCT study participant recruitment
At introduction sessions at each participating church, study staff will explain the study, and hand out interest slips for people to use to indicate that they are (or are not) interested in being approached for the study. We will also post flyers in the churches and FBOs with study contact information. Finally, we will make study flyers that can be handed out in the churches and FBOs. Once the study has names of potentially interested participants, informed consent will be take place privately by trained study staff. That person will explain all aspects of the study, including confidentiality and its limits, and address questions. We will emphasize the voluntary nature of study participation. Once the potential participant understands and agrees, s/he will be asked to sign the consent form, and will receive a copy. Recruitment at each church will take place prior to randomization of that church. Participant recruitment began February 1, 2018 and is anticipated to be complete by April 2019. Within that time, we will recruit an average of 24 participants within at least 24 churches that commit to the RCT, resulting in an enrolled sample size of 576.
4.6. Randomization
Churches will be randomized to the PANP or HWP in a 1:1 ratio. We will randomize at the church level but do so in small waves to concentrate particular study functions at particular times (making study operations more efficient). Notably, the Flint Water Crisis placed an extraordinary level of strain on CBOs and FBOs in Flint, as they were frequently asked for resources (human and financial) to support their program users. As such, we developed a randomization schedule that assigned churches to one of the two conditions as they committed to the RCT and sought to have a minimum of four churches commit to study participation during each wave, for a maximum total of 6 waves. Within each wave, we required at least two churches to be randomly assigned to the PANP to initiate a wave; among those churches within a wave, those randomized to the HWP completed baseline data collection prior to the start of the next wave. Recognizing the seasonal patterns of FBO community activities (e.g. revival, travel, vacation bible school, holiday activities), no waves are planned to start in August, November, or December. We will track cumulative projected vs. actual recruitment monthly.
4.7. Retention
We will employ several approaches that we have found helpful in achieving low attrition rates (0–20%) in other studies, including studies of very transitory, high-risk samples (such as those with substance dependence and those leaving prison) [[55], [56], [57], [58], [59], [60]]. These include study staff's strong relationships with participants and efforts to value and appreciate their study participation. Study staff will call participants and mail them letters to remind them of their appointments and maintain a list of 2 other people who will always know where participants reside. Locator information is updated at each study contact. Having some flexibility in scheduling follow-up assessments (i.e., on evenings or weekends) also facilitate participant retention. Finally, participants are remunerated $20 for each follow-up assessment, facilitating retention. Control churches and participants will also be offered Church Challenge activities and services at the end of their congregants' last study follow-up interview. They will also complete organizational surveys annually. In Year 1, we will also discuss with our Consortium partners additional ways to help control churches feel valued and included in the study, and to benefit from study participation.
4.8. Data collection
Table 1 provides an overview of the planned assessments at the church level with church leaders and health teams. The remainder of this section addresses data collection for the individual study participants in the PANP and HWP conditions. For the PANP condition, data collection occurs five times (baseline, 8 weeks, 16 weeks, 26 weeks, and 52 weeks). For the HWP condition, data collection occurs three times (baseline, 26 weeks, and 52 weeks). Data collection at week 52 for the PANP is to evaluate maintenance behaviors of the intervention treatment group participants. Data collections at 26 and 52 weeks will include additional activities aligned with improving nutrition, including a cooking competition for the best DASH recipes; HWP participants will additionally receive a fitness class demonstration, a recipe for a healthy meal and the key ingredients to take home.
Table 1.
Assessments with the church leaders and health teams.
| Assessments | Times of Collection | |
|---|---|---|
| Church Level (church leadership with health teams) of both HWP and PANP |
|
Baseline and every 6 months thereafter |
| Health Teams with PANP Participants |
|
Once every 4 weeks during the 16 week PANP |
|
1-2 times between weeks 16–26 after the PANP |
4.9. Screening and informed consent
All participants complete a 15-min screening process prior to study enrollment. The screening process includes the 22-item Telephone Interview for Cognitive Status [61,62] and a 17-item measure to assess physical activity readiness [63]. Participants who were unable to complete the screener questions or chose not to consent after completion of the screener did not complete any additional study activities or provide additional study information. Participants who completed the screener and consent process were then invited to complete the baseline data collection process. Participants who were screened and consented by phone were provided with electronic online links to access the baseline questionnaire in advance of the physiological assessments. Participants have the option of completing informed consent to complete the survey (through Qualtrics) prior to in person contact with the study team. All participants have the opportunity to ask questions of the study team and complete an informed consent process that additionally include the physiological data collection process at the in-person baseline data collection session. The baseline data collection process included three questionnaires on general wellbeing, nutrition and physical activity and physiological assessments.
4.10. Questionnaires
All participants complete the same baseline questionnaires. The questionnaires take approximately 1 h to complete. Participants will complete questionnaires (see Table 2) about general health, nutrition, and physical activity. The general questionnaire requires about 30 min to complete and addresses sociodemographics, general health behaviors [64,65], sleep disturbance [66], health service utilization [67], physical function [68], pain [69], and mental health [70], general health and quality of life [71], social support [72], anger [73], stress [74,75], life satisfaction [76], coping with stress [77], discrimination [78], religiousness/spirituality [79], neighborhood cohesion [80], and public trust in a disaster [81]. Participants will be asked to report their doctor diagnosed health conditions, and current medications being taken. The physical activity questionnaire requires about 10 min to complete and included questions from the CHAMPS survey for older adults [82], items from the 2011 Behavioral Risk Factor Surveillance System Physical Activity Rotating Core [83], and addressed motivation [84], self-efficacy [85] and social support for physical activity. The nutrition questionnaire requires about 20 min and addresses food attitude and behaviors [86,87], food security [88], sodium intake [89], social support for dietary intake [90], and eating habits [91].
Table 2.
Individual level assessments for church challenge RCT participants in the HWP and PANP.
| Individual Level Measures (HWP and PANP) | Baseline | 8 wks | 16 wks | 26 wks | 52 wks |
|---|---|---|---|---|---|
| Sociodemographics (e.g age, gender, education, income, marital status) | x | ||||
| Height, Weight, Waist Circumference, Blood Pressure and Heart Rate | x | x | x | x | x |
| HbA1c | x | x | x | ||
| Short Form (SF)-12 | x | x | x | x | x |
| Michigan Body Map and Severity Index | x | x | x | x | x |
| PROMIS Social Support | x | x | x | ||
| Public Health Disaster Scale | x | x | x | ||
| Exercise Self Efficacy | x | x | x | x | |
| Behavioral Regulation in Exercise Questionnaire (BREQ)-2 | x | x | x | x | |
| Patient Health Questionnaire (PHQ)-9 | x | x | x | x | |
| Spielberger Anger Expression Scale (STAX) | x | x | x | ||
| Everyday Discrimination Scale | x | x | x | ||
| Perceived Stress Scale | x | x | x | ||
| Satisfaction with Life Scale | x | x | x | x | |
| Brief Multidimensional Measure of Religiousness/Spirituality | x | x | x | x | |
| Ongoing Chronic Stressors | x | x | x | x | |
| Brief Coping Scale | x | x | x | x | |
| Community Healthy Activities Model Program for Seniors (CHAMPS) Questionnaire | x | x | x | x | |
| NHANES Health Care Utilization | x | x | x | x | |
| Block Sodium Screener | x | x | x | x | |
| Core Food Security Module (Brief) | x | x | x | x | |
| Food Attitudes and Behavior Survey | x | x | x | x | |
| PROMIS Sleep Disturbance | x | x | x | x | |
| Neighborhood Social Cohesion | x | x | x |
4.11. Physiological data collection
The in-person data collection collects blood pressure, height, weight, waist circumference, and hemoglobin A1c from each participant. During the screening calls, participants are also asked to bring their current medications, and during the in-person sessions, study staff record participant medications and the participant-reported purpose for using the medication. Systolic and diastolic blood pressure, weight, height, and waist circumference will be collected by a trained medical professional. Weight and height data will be collected from participants without shoes, and participants will be asked to wear no more than one lightweight layer of clothing during weight measures. After resting quietly in a seated position for 5 min, three consecutive heart rate and blood pressure readings will be obtained using an automated oscillometric blood pressure measuring device such as the OMRON 705IT [92]. If a blood pressure measurement is interrupted or incomplete, a fourth attempt may be made. Weight will be ascertained using digital scales [93]. Height and waist circumference will be measured using a fiberglass measuring tape; waist circumference measures will follow the recommended protocol outlined by Klein and colleagues [94]. In addition, the study team will retrieve step count data of the PANP group participants from the fitness trackers provided to each participant as a part of the PANP activities [95].
4.12. Biological biomarker data
PA and healthy eating interventions contribute to significant improvements in biological markers of cardiovascular risk [96,97]. Clinical professionals will collect blood specimens via finger pricks for each participant to measure non-fasting glycohemoglobin (HbA1c), HbA1c reflects plasma glucose for the previous 120 days, and is used to diagnose diabetes (6.5% or greater) and pre-diabetes (5.7%–6.4%). The blood specimens will be collected by the clinical project staff and transported to the Hurley Hospital pathology laboratory (in Flint, MI) for analysis.
4.13. Process and fidelity measures
Intervention fidelity measures at the church level will consist of checklists and weekly informal interviews about the church's Church Challenge activities. At the interventionist level, checklists for meeting/session components will be completed, and participant attendance recorded. At the participant level, we will track attendance at fitness classes and workshops, track objective measures using nurse assessment and pedometry, and assess eating, motivation, and social support activities through self-report. Intervention compliance will be used in dose-response, intervention process, and mediator analyses.
4.14. Data analysis
The primary study outcome is average systolic blood pressure change between the baseline and 6 month assessments. The primary hypothesis is that the average systolic blood pressure change between the baseline and 6 month assessments will be a 6 mmHg greater decrease among participants in the 16-week PANP activity group compared to participants in the HWP group. The null hypothesis is that there are no differences in the average systolic blood pressure change between the baseline and 6 month assessments when comparing the PANP and HWP group participants.
The primary analyses will assess improvements in average blood pressure at 6 months, using baseline blood pressure as a covariate, and comparing the PANP to HWP group participants. We will use random coefficients models to account for repeated measures and group level clustering within the FBO to evaluate the association between the Church Challenge intervention and the study outcomes over the study duration. In the statistical model, we will construct statistical linear combinations to perform statistical contrasts that assess whether the changes in blood pressure for participants in the PANP were at least 6 mmHg larger when compared to HWP group. All analyses will covary baseline values of the dependent variable. Our models will impose a linear or non-linear model structure for our continuously blood pressure measures, dependent upon the most appropriate functional form of the data. The model for our primary hypothesis test will use continuous measures of blood pressure [98]. We will specify statistical interaction terms to assess changes in body weight over time across the treatment conditions. We will perform similar methods to assess whether the treatment condition predicts statistical and clinically significantly greater improvement of the secondary outcomes as well. In particular, we will examine clinical significance of treatment differences in biomarkers as defined in the assessment section.
Primary analyses will be intent-to-treat; we will examine dose-response effects in secondary analyses. Primary tests will be 2-sided with alpha = 0.05. Descriptive statistics will include effect sizes and measures of clinical significance (i.e., area under the curve [AUC] [99]; number needed to treat [NNT]) for all major comparisons. We will separate primary hypotheses from remaining hypotheses. Standard post hoc procedures will be used to adjust for multiple comparisons when testing secondary hypotheses. There is no planned interim analysis. Analyses will adjust for baseline levels of dependent variables, gender, and age. Consistent with CONSORT [100] guidelines, we will prespecify covariates and will not adjust for imbalance observed post hoc.
4.14.1. Missing data
We will use multiple imputation to deal with missing data [101,102]. We will compare intervention conditions on rates of missingness and time to missingness and will test whether baseline characteristics are associated with missingness. Finally, we will perform a sensitivity analysis in which we impute extreme values for missing data to determine the sensitivity of analysis results to missing data.
4.15. Dose-response/mediator/process analyses
We will assess program fidelity (including number of intervention activities attended and level of physical activity) across the treatment conditions primarily using descriptive statistical methods and examine it as a predictor of outcomes. We will also evaluate proximal outcomes (i.e., physical activity, church-based social support, increased healthy eating) as mediators of physiologic and biomarker outcomes (especially our primary outcome) using MacKinnon's mediation method. We will also conduct dose-responses analyses. Finally, we will compute secondary, adjusted models that account for medication usage throughout the course of the study.
4.16. Predictors/personalization
We will explore organizational and personal readiness as a predictor of personal and church-level fidelity measures. We will also explore gender and social support for physical activity as moderators of intervention effects.
4.17. Power and sample size
We calculated needed sample sizes for a range of intraclass correlations of outcomes among participants nested within churches, a range of numbers of participants within each church with completed follow-ups (n = 10, 15, 20, 25), and a range of intervention effect sizes (Cohen's d = 0.25, 0.30, 0.35). In a cluster-randomized trial, randomizing slightly more churches with slightly fewer people each adequately powers the study with fewer participants overall, reducing study burden. We examined the 48 resulting needed sample sizes for each combination of intraclass correlation, participants within churches, and anticipated effect size. Our final power calculation assumes an intraclass correlation 0.02 [103], an effect size of d = 0.30 (consistent with a 6 mmHg decrease in systolic blood pressure and standard deviation of 19 mmHg, and in range of previous physical activity and healthy eating intervention studies studies [[104], [105], [106]]), 24 churches and 20 individuals with complete data within churches (n = 480 total) for adequate power (80% power with α = 0.05); correcting for attrition, our final sample size is 576 across 24 churches (288 HWP-control participants in 12 churches, and 288 PANP-treatment participants in 12 churches).
5. Discussion
Challenges with access to physical activity and healthy food are important drivers of health disparities. Public and private sector divestment has left disadvantaged areas without resources to support healthy living, such as healthy food outlets or places to exercise. For example, many of these communities lack supermarkets or have long distances to supermarkets [[107], [108], [109]], which are both associated with higher weight and lower fruit/vegetable intake [[110], [111], [112], [113]]. Without economic support, many outdoor community resources go unused due various factors, including a lack of area cleanliness (e.g. parks, streets, vacant properties), maintenance (e.g. sidewalk repair, street light replacement, lawn maintenance), and security (e.g. safe walking trails, absence of violence and illegal activities) that deter residents from active living in their communities, and limit private sector interest in coming to these areas. The resulting physical and social disorder in these neighborhoods, often comprised of majority-minority residents, has been strongly linked to health and health behaviors in previous research [114]. The absence of public and private sector support forces disadvantaged community members to re-evaluate the strategies and resources available that are not dependent on public/private sector options to address their needs, including those related to healthy living. Therefore, effective interventions for health promotion and chronic disease prevention require multilevel contributions targeting both individual behavior and community resources and infrastructure, especially in underserved communities.
This multilevel randomized controlled trial is highly significant and innovative because it uses a combination of evidence-based practices structured to improve individual physical health behavior change while simultaneously increasing the capacity of faith-based organizations to deliver long-term scripturally-based and faith-placed health promotion activities in vulnerable communities. Flint, MI is not a unique community, but has faced a history of traumatic community wide events that continue to challenge community public health infrastructures and distract residents from focusing on their health. If successful, this project will demonstrate the strength of community organizations, especially those from underserved communities, to create changes and establish audible, respected, and fundable voices that protect the health interests of their community residents. In addition, the resources and approaches (e.g., churches, community organizations, policy advocacy around the built environment, access to healthy food) can easily be leveraged to address a range of healthy behaviors and health issues, meaning that our results may have implications for many healthy behaviors that influence susceptibility to chronic disease in minority and underserved communities. This particular benefit of the Church Challenge is critical for the Flint community in light of ongoing efforts to support youth and families actively working to manage their health and recover from physical and psychological health concerns resulting from the Flint Water Crisis. This project reflects the necessity of combining evidence-based practices into a collective strategy that enables vulnerable community organizations and residents to overcome the negative social and health effects of community wide traumas, regain control of their personal health, and support chronic disease risk reduction and health equity of their own communities. Our efforts, should they be demonstrated as effective, offer strategies that can be translated for adaption in other disadvantaged communities, and particularly those that have experienced long term economic deprivation like Flint.
Conflict of interest declaration
None.
Acknowledgements
We would like to thank Dr. Ken Resnicow and Dr. Todd Yeary for offering their expertise for this work. We would also like to thank Bishop Bernadel Jefferson for her efforts, and we want to thank the COFY staff partners, including the fitness instructors, nutrition instructors, facilities staff, and clinical staff for their contributions in the development and implementation of the various program components.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.conctc.2019.100329.
Funding
Research reported in this publication was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under award number U54MD011227.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Ward B., Schiller J., Goodman R. Multiple chronic conditions among US adults: a 2012 update. Prev. Chronic Dis. 2014;(130389):11. doi: 10.5888/pcd11.130389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heron M. Deaths: leading causes for 2012. Natl. Vital Stat. Rep. 2015;64(10) [PubMed] [Google Scholar]
- 3.Worktable 293 . 1999-2007. Age-adjusted Death Rates for 113 Selected Causes, Alcohol-Induced Causes, Drug-Induced Causes, and Injury by Firearms by Race and Sex: United States.http://www.cdc.gov/nchs/nvss/mortality_tables.htm [Google Scholar]
- 4.Group USCSW, United States Cancer Statistics . 1999-2012. Incidence and Mortality Web-Based Report; p. GA2015. Atlanta. [Google Scholar]
- 5.Carroll M., Kit B., Flegal K. Prevalence of childhood and adult obesity in the United States, 2011-2012. J. Am. Med. Assoc. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Go A.S.M.D., Roger V.L., Benjamin E.J., Berry J.D., Blaha M.J., Dai S., Ford E.S., Fox C.S., Franco S., Fullerton H.J., Gillespie C., Hailpern S.M., Heit J.A., Howard V.J., Huffman M.D., Judd S.E., Kissela B.M., Kittner S.J., Lackland D.T., Lichtman J.H., Lisabeth L.D., Mackey R.H., Magid D.J., Marcus G.M., Marelli A., Matchar D.B., McGuire D.K., Mohler E.R., 3rd, Moy C.S., Mussolino M.E., Neumar R.W., Nichol G., Pandey D.K., Paynter N.P., Reeves M.J., Sorlie P.D., Stein J., Towfighi A., Turan T.N., Virani S.S., Wong N.D., Woo D., Turner M.B. American heart association statistics committee and stroke statistics subcommittee. Heart disease and stroke statistics--2014 update: a report from the American heart association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mariotto A., Yabroff K., Shao Y., Feuer E., Brown M. Projections of the cost of cancer care in the U.S.: 2010-2020. J Natl Cancer Institute. 2011;103(2):117–128. doi: 10.1093/jnci/djq495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Association A.D. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033–1046. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.FInkelstein E., Trogdon J., Cohen J., Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff. 2009;28(5):w822–831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 10.Access to Affordable and Nutrition Food: Measuring and Understanding Food Deserts and Their Consequences, Report to Congress. United States Department of Agriculture; 2009. [Google Scholar]
- 11.Lemacks J., Wells B., Ilich J., Ralston P. Interventions from improving nutrition and physical activity behaviors in adult African American populations: a systematic review, January 2000 through December 2011. Prev. Chronic Dis. 2013;10 doi: 10.5888/pcd10.120256. 120256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jørgensen T., Capewell S., Prescott E. Population-level changes to promote cardiovascular health. European journal of preventive cardiology. 2013;20(3):409–421. doi: 10.1177/2047487312441726. [DOI] [PubMed] [Google Scholar]
- 13.Powell L., Slater S., Chaloupka F., Harper D. Availability of physical activity-related facilites and neighborhod demographic and socioeconomic characteristics: a national study. Am. J. Public Health. 2006;96:1676–1680. doi: 10.2105/AJPH.2005.065573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lamichhane A., Warren J., Puett R. Spatial patterning of supermarkets and fast food outlets with respect to neighborhood characteristics. Health Place. 2013;23:157–164. doi: 10.1016/j.healthplace.2013.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferdinand K., Yadav K., Nasser S. Disparities in hypertension and cardiovascular disease in blacks: the critical role of medication adherence. J. Clin. Hypertens. 2017;19(10):1015–1024. doi: 10.1111/jch.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Branch PAaN. N.C. Division of Public Health; Raleigh, NC: 2010. African-American Churches: Eating Smart and Moving More. A Planning and Resource Guide. [Google Scholar]
- 17.Key K., Lewis E. Sustainable community engagement in a constantly changing health system. Learning Health Systems. 2018;2(3):1–5. doi: 10.1002/lrh2.10053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Israel B., Eng E., Schulz A., Parker E. Josey-Bass; San Francisco, CA: 2005. Methods in Community-Based Participatory for Health. [Google Scholar]
- 19.Wallerstein N., Curan B., Minkler M. Developing and maintaining partnerships with communities. In: Barbara Israel E.E., Schulz Amy, Parker Edith, editors. Methods in Community-Based Participatory Research for Health. Jossey-Bass; San Francisco, CA: 2005. pp. 31–51. [Google Scholar]
- 20.Minkler M., Wallerstein N. Jossey-Bass; San Francisco, CA: 2012. Community-based Participatory Research for Health from Process to Outcomes. [Google Scholar]
- 21.Rosenthal E., Balcazar H., DeHeer H., Wise S., FLores L., Aguirre M. Critical reflections on the role of CBPR within an RCT community health worker prevention intervention. J. Ambul. Care Manag. 2014;37(3):2241–2249. doi: 10.1097/JAC.0000000000000010. [DOI] [PubMed] [Google Scholar]
- 22.Goodkind J., Amer S., Christian C. Challenges and innovations in a community-based participatory randomized controlled trial. Health Educ. Behav. 2017;44(1):123–130. doi: 10.1177/1090198116639243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horne K., McCracken L., Dino G., Brayboy M. Applying community-based participatory research principles to the development of a smoking-cessation program for American Indian teens: “Telling our story.”. Health Educ. Behav. 2008;35:44–69. doi: 10.1177/1090198105285372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones L., Koegel P., Wells K. Bringing experimental design to community-partnered participatory research. In: M Minkler N.W., editor. Community-based Participatory Research for Health. Jossey-Bass; San Francisco, CA: 2008. pp. 67–85. [Google Scholar]
- 25.Parker E., Israel B., Robins T. Evaluation of Community health worker intervention to improve children's asthma-related health by reducing household environmental triggers for asthma. Health Educ. Behav. 2008;35:276–395. doi: 10.1177/1090198106290622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krieger J., Takaro T., Song L., Beaudet N., Edwards K. A randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am. J. Public Health. 2009;163:141–149. doi: 10.2105/AJPH.2004.042994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Salvatore A., Chevrier J., Bradman A. A community-based participatory worksite intervention to reduce pesticide exposures to farmworkers and their families. Am. J. Public Health. 2009;99:S578–S581. doi: 10.2105/AJPH.2008.149146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jacobs J., Kiersz A., Lubin G. Business Insider; 2013. The 25 Most Segregated Cities in America.http://www.businessinsider.com/most-segregated-cities-in-america-2013-11?op=1 [Google Scholar]
- 29.Foundation RWJ. 2015 County Health Rankings. 2015. Michigan. [Google Scholar]
- 30.Agriculture USDo. Food Deserts. 2015. https://apps.ams.usda.gov/fooddeserts/fooddeserts.aspx [Google Scholar]
- 31.Hosler A.S.R.D., Fredrick B.L., Ronsani A.E. Assessing retail fruit and vegetable availability in urban and rural underserved communities. Prev. Chronic Dis. 2008;5(4):A123. [PMC free article] [PubMed] [Google Scholar]
- 32.Glanz K., Yaroch A. Strategies for increasing fruit and vegetable intake in grocery stores and communities: policy, pricing, and evironmental change. Prev. Med. 2004;39:S75–S80. doi: 10.1016/j.ypmed.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 33.Larsen K., Gilliland J. A farmers' market in a food desert: evaluating impacts on availability of healthy food. Health Place. 2009;15:11158–11162. doi: 10.1016/j.healthplace.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 34.Story M., Kaphingst K., Robinson-O'Brien R., Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu. Rev. Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 35.Moreno J., Gonzalez-Cutre D., Sicilia A., Spray C. Motivation in the exercise setting: integrating constructs from the approach-avoidance achievement goal framework and self-determination theory. Psychol. Sport Exerc. 2010;11:542–550. [Google Scholar]
- 36.Teixeira P., Carraca E., Markland D., Silva M., Ryan R. Exercise, physical activity, and self-determination theory: a systematic review. Int. J. Behav. Nutr. Phys. Activ. 2012;9:78. doi: 10.1186/1479-5868-9-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Palmeira A., Teixeira P., Branco T. Predicting short-term weight loss using four leading health behavior change theories. Int. J. Behav. Nutr. Phys. Activ. 2007;4:14. doi: 10.1186/1479-5868-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Achterberg C., Miller C. Is one theory better than another in nutrition education? A viewpoint: more is better. J. Nutr. Educ. Behav. 2004;36:40–42. doi: 10.1016/s1499-4046(06)60127-9. [DOI] [PubMed] [Google Scholar]
- 39.Spahn J., Reeves R., Keim K. State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. J. Am. Diet Assoc. 2010;110:879–891. doi: 10.1016/j.jada.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 40.Cornelissen V., Smart N. Exercise training for blood pressure: a systematic review and meta-analysis. J. Am. Med. Assoc. 2013;2 doi: 10.1161/JAHA.112.004473. e004473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sullivan A., Lachman M. Behavior change with fitness technology in sedentary adults: a review of the evidence for increasing physical activity. Frontiers in Public Health. 2017;4(1):289. doi: 10.3389/fpubh.2016.00289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chiauzzi E., Rodarte C., DasMahapatra P. Patient-centered activity monitoring in the self-managment of chronic conditions. BMC Bedicine. 2015;13:77. doi: 10.1186/s12916-015-0319-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Belza B., Shumway-Cook A., Phelan E., WIlliams B., Snyder S., LoGergo J. The effects of a community-based exercise program on function and health in older adults: the EnhanceFitness Program. J. Appl. Gerontol. 2006;25(4) [Google Scholar]
- 44.Dubowitz T., Zenk S., Ghosh-Dastidar B. Healthy food access for urban food desert residents: examination of the food environment, food purchasing practices, diet, and body mass index. Publ. Health Nutr. 2015;18(12):2220–2230. doi: 10.1017/S1368980014002742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Walker O'Neal C., Wickrama K., Ralston P. Eating behaviors of older African Americans: an application of the theory of planned behavior. Gerontol. 2012;54(2):211–220. doi: 10.1093/geront/gns155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reicks M., Trofholz A., Stang J., Laska M. Impact of cooking and home food preparation interventions among adults: outcomes and implications for future programs. J. Nutr. Educ. Behav. 2014;46(4):259–276. doi: 10.1016/j.jneb.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang M., Pbert L., Lemon S. The influence of family, friend, and coworker social support and social undermining on weight gain prevention among adults. Obesity. 2015;22(9):1973–1980. doi: 10.1002/oby.20814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ammerman A., Lindquist C., Lohr K., Hersey J. The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: a review of the evidence. Prev. Med. 2002;35:25–41. doi: 10.1006/pmed.2002.1028. [DOI] [PubMed] [Google Scholar]
- 49.Geyen D. Behavioral changes for African American to improve health, embrace culture, and minimize disparities. ECI Interdisciplinary Journal for Legal and Social Policy. 2012;2(1) [Google Scholar]
- 50.Wallach J. 2014. How to Eat to Live: Black Nationalism and the Post-1964 Culinary Turn. Study the South. [Google Scholar]
- 51.Wang J., Cadmus-Bertram L., Natarajan L. Wearable sensor/device (fitbit one) and SMS text-messaging prompts to increase physical activity in overweight and obese adults: a randomized controlled trial. Telemedicine and e-Health. 2015;21(10):782. doi: 10.1089/tmj.2014.0176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patrick K., Raab F., Adams M. A text message-based intervention for weight loss: randomized controlled trial. J. Med. Internet Res. 2009;11(1) doi: 10.2196/jmir.1100. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Resnicow K., DilIorio C., Soet J., Borrelli B., Hecht J., Ernst D. Motivational interviewing in health promotion: it sounds like something is changing. Health Psychol. 2002;21(5):444–451. [PubMed] [Google Scholar]
- 54.Resnicow K., Jackson A., Wang T. A motivational interviewing intervention to increase fruit and vegetable intake through black churches: results of the eat for life trial. Am. J. Public Health. 2001;91(10):1686–1693. doi: 10.2105/ajph.91.10.1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zlotnick C., Johnson J., Najavits L.M. Randomized controlled pilot study of cognitive-behavioral therapy in a sample of incarcerated women with substance use disorder and PTSD. Behav. Ther. 2009;40(4):325–336. doi: 10.1016/j.beth.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Stein M., Caviness C., Anderson B., Hebert M., Clarke J. A brief alcohol intervention for hazardously-drinking incarcerated women. Addiction. 2010;105(3):466–475. doi: 10.1111/j.1360-0443.2009.02813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Johnson J., Zlotnick C. Pilot study of treatment for major depression among women prisoners with substance use disorder. J. Psychiatr. Res. 2012;46(9):1174–1183. doi: 10.1016/j.jpsychires.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Johnson J.E., Zlotnick C. A pilot study of group interpersonal psychotherapy for depression in substance-abusing female prisoners. J. Subst. Abuse Treat. 2008;34(4):371–377. doi: 10.1016/j.jsat.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 59.Stein M.D., Hagerty C.E., Herman D.S., Phipps M.G., Anderson B.J. A brief marijuana intervention for non-treatment-seeking young adult women. J. Subst. Abuse Treat. 2011;40(2):189–198. doi: 10.1016/j.jsat.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stein M., Charuvastra A., Maksad J., Anderson B. A randomized trial of a brief alcohol intervention for needle exchangers (BRAINE) Addiction. 2002;97(6):691–700. doi: 10.1046/j.1360-0443.2002.00102.x. [DOI] [PubMed] [Google Scholar]
- 61.Espeland M., Rapp S., Katyla J. Telephone interview for cognitive status (TICS) screening for clinical trials of physical activity and cognitive training: the seniors health and activity research program pilot (SHARP-P) study. Int. J. Geriatr. Psychiatr. 2011;26(2):135–143. doi: 10.1002/gps.2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Knopman D., Roberts R., Geda Y., Pankratz V., Christianson T., Petersen R. Validation of the telephone interview for cognitive status-modified in subjects with normal cognition, mild cognitive impairment, or dementia. Neuroepidemiology. 2010;34:34–42. doi: 10.1159/000255464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Warburton D., Jamnik V., Bredin S., Gledhill N., Collaboration P.-Q. The physical activity readiness questionnaire for everyone (PAR-Q+) and electronic physical activity readiness medical examination (ePARmed-X+) Health and Fitness Journal of Canada. 2011;4(2):3–23. [Google Scholar]
- 64.2011-2012 Data Documentation, Codebook, and Frequencies: Alcohol Use. 2013. 2018. https://wwwn.cdc.gov/Nchs/Nhanes/2011-2012/ALQ_G.htm [Google Scholar]
- 65.2011-2012 Data Documentation, Codebook, and Frequencies: Smoking- Cigarette Use. 2013. 2018. https://wwwn.cdc.gov/Nchs/Nhanes/2011-2012/SMQ_G.htm [Google Scholar]
- 66.Toolbox N. PROMIS Item Bank; 2018. Sleep Disturbance- Short Form 8a.http://www.healthmeasures.net/administrator/components/com_instruments/uploads/PROMIS%20SF%20v1.0%20-%20Sleep%20Disturbance%208a%206-2-2016.pdf v1.0 2016. [Google Scholar]
- 67.Hospital Utilization and Access to Care-HUQ. 2012. http://www.cdc.gov/nchs/data/nhanes/nhanes_13_14/HUQ_H.pdf [Google Scholar]
- 68.Toolbox N. 2018. Physical Function- Short Form 20a. PROMIS Item Bank v1.0 2012. [Google Scholar]
- 69.Brummett C., Bakshi R., Goesling J. Preliminary validation of the Michigan body map. Pain. 2016;157(6):1205–1212. doi: 10.1097/j.pain.0000000000000506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kroenke K., Spitzer R., Williams J. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ware J., Kosinksi M., Keller S. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med. Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 72.Toolbox N. 2018. Emotional Support.http://www.healthmeasures.net/administrator/components/com_instruments/uploads/TOOLBOX%20FF%20v2.0%20-%20Emotional%20Support%2018%20plus_11-17-2016.pdf [Google Scholar]
- 73.Forgays D., Spielberger C., Ottaway S., Forgays D. Factor structure of the state-trait anger expression inventory for middle-aged men and women. Assessment. 1998;5:141–155. doi: 10.1177/107319119800500205. [DOI] [PubMed] [Google Scholar]
- 74.Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24:386–396. [PubMed] [Google Scholar]
- 75.Troxel W., Matthews K., Bromberger J., Sutton-Tyrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychol. 2003;22(3):300–309. doi: 10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]
- 76.Diener E., Emmons R., Larsen R., Griffin S. The satisfaction with life scale. J. Pers. Assess. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 77.Carver C. You want to measure coping but your protocol's too long: consider the Brief COPE. Int. J. Behav. Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 78.Williams D., Yu Y., Jackson J., Anderson N. Racial differences in physical and mental health: socioeconomic status, stress, and discrimination. J. Health Psychol. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 79.Institute F. Brief multidimensional measure of religiousness/spirituality: 1999. In: Group NW, editor. Multidimensional Measurement of Religiousness/spirituality for Use in Health Research: A Report of the Fetzer Institute/National Institute on Aging Working Group. second ed. John E. Fetzer Institute; Kalamazoo, MI: 2003. pp. 85–88. [Google Scholar]
- 80.Mendes de Leon C., Cagney K., Bienias J. Neighborhood social cohesion and disorder in relation to walking in community-dwelling older adults: a multilevel analysis. J. Aging Health. 2009;21(1):155–171. doi: 10.1177/0898264308328650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Eisenmann D., Williams M., Glik D., Long A., Plough A., Ong M. A measure to assess trust in publi health in a disaster. J Public Health Management. 2011;18(4):E11–E18. doi: 10.1097/PHH.0b013e31823991e8. [DOI] [PubMed] [Google Scholar]
- 82.Resnicow K., Mccarty F., Blissett D., Wang T., Heitzler C., Lee R. Validity of a modified CHAMPS physical activity questionnaire among African-Americans. Medicine and science in sports science. 2003;35(9):1537–1545. doi: 10.1249/01.MSS.0000084419.64044.2B. [DOI] [PubMed] [Google Scholar]
- 83.Promotion NCfCDPaH. A Data Users Guide to the BRFSS Physical Activity Questions: How to Assess the 2008 Physical Activity Guidelines for Americans. Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 84.Markland D., Tobin V. A modification to the bheavioral regulation in exercise questionnaire to include an assessment of amotivation. J. Sport Exerc. Psychol. 2004;26:191–196. [Google Scholar]
- 85.Sallis J., Pinski R., Grossman R., Patterson T., Nader P. The development of self-efficacy scales for health-related diet and exercise behaviors. Health Educ. Res. 1988;3:283–292. [Google Scholar]
- 86.FAB Study: Food Attitudes and Behaviors Survey. 2009. [Google Scholar]
- 87.Yaroch A., Tooze J., Thompson F. Evaluation of three short dietary instruments to assess fruit and vegetable intake: the National Cancer Institute's food attitudes and behaviors survey. J. Acad. Nutr. Diet. 2012;112(10):1570–1577. doi: 10.1016/j.jand.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.US Household Food Security Survey Model: Three-Stage Design, with Screeners. United States Department of Agriculture; 2012. [Google Scholar]
- 89.Tangney C., Rasmussen H., Rusch J. Validation of a sodium screener in two samples. Federation of American Societies For Experimental Biology. 2016;30(1) [Google Scholar]
- 90.Sallis J., Grossman R., Pinski R., Patterson T., Nader P. The development of scales to measure social support for diet and exercise behaviors. Prev. Med. 1987;16:825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 91.Institute D-FC. Dana-Farber Cancer Institute Eating Habits Questionnaire.
- 92.Mengden T., Asmar R., Kandra A., Di Giovanni R., Brudi P., Parati G. Use of automated blood pressure measurements in clinical trials and registration studies: data from the VALTOP Study. Blood Press. Monit. 2010;15(4):188–194. doi: 10.1097/MBP.0b013e328339d516. [DOI] [PubMed] [Google Scholar]
- 93.Yorkin M., Spaccarotella K., Martin-Bigger J., Quick V., Byrd-Bredbenner C. Accuracy and consistency of weights provided by home bathrooms scales. BMC Public Health. 2013;13:1194. doi: 10.1186/1471-2458-13-1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Klein S., Allison D., Heymsfield S., Kelley D., Leibel R., Nonas C. Waist circumference and cardiometabolic risk: a consensus statement from shaping America's health: association for weight management and obesity prevention; NAASO, the obesity society; the American society for nutrition; and the American diabetes association. Am. J. Clin. Nutr. 2007;85:1197–1202. doi: 10.1093/ajcn/85.5.1197. [DOI] [PubMed] [Google Scholar]
- 95.Bravata D., Smith-Spangler C., Sundaram V. Using pedometers to increase physical activity and improve HealthA systematic review. J. Am. Med. Assoc. 2007;298(19):2296–2304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- 96.American Heart Association Nutrition Committee L.A., Appel L.J., Brands M., Carnethon M., Daniels S., Franch H.A., Franklin B., Kris-Etherton P., Harris W.S., Howard B., Karanja N., Lefevre M., Rudel L., Sacks F., Van Horn L., Winston M., Wylie-Rosett J. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114(1):82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 97.Phlotnikoff R., Costigan S., Karuynamuni N., Lubans D. Community-based physical activity interventions for treatment of type 2 diabetes: a systematic review with meta-analysis. Front. Endocrinol. 2013;4(3):1–17. doi: 10.3389/fendo.2013.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Appel L. Lifestyle modification as a means to prevent and treat high blood pressure. J. Am. Soc. Nephrol. 2003;14(S2):S99–S102. doi: 10.1097/01.asn.0000070141.69483.5a. [DOI] [PubMed] [Google Scholar]
- 99.Kraemer H., Morgan G.A., Leech N.L., Gliner J.A., Vaske J.J., Harmon R.J. Measures of clinical significance. J. Am. Acad. Child Adolesc. Psychiatr. 2003;42(12):1524–1529. doi: 10.1097/00004583-200312000-00022. [DOI] [PubMed] [Google Scholar]
- 100.CONSORT . 2010. CONSORT: Transparent Reporting of Trials.http://www.consort-statement.org/ [Google Scholar]
- 101.Little R., Rubin D. John Wiley and Sons; New York: 1987. Statistical Analysis with Missing Data. [Google Scholar]
- 102.Allison P.D. Sage Publications; Thousand Oaks, CA: 2002. Missing Data. [Google Scholar]
- 103.Campbell M., James A., Hudson M. Improving multiple behaviors for colorectal cancer prevention among African American church members. Health Psychol. 2004;2(5):492–502. doi: 10.1037/0278-6133.23.5.492. [DOI] [PubMed] [Google Scholar]
- 104.Balk E., Earley A., Raman G., Avendano E., Pittas A., Remington P. Combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the community preventive services task force. Ann. Intern. Med. 2015;163(6):437–451. doi: 10.7326/M15-0452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Donnelly J., Blair S., Jakicic J. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Medicine and science in sports science. 2009;41(2):459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 106.Resnicow K., Campbell M., Carr C. Body and soul. A dietary intervention conducted through African-American churches. Am. J. Prev. Med. 2004;27(2):97–105. doi: 10.1016/j.amepre.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 107.Morland K., Wing S., Diez-Roux A. The contextual effect of the local food environment on residents' diets: the atherosclerosis risk in communities study. Am. J. Public Health. 2002;92(11) doi: 10.2105/ajph.92.11.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Walker R., Keane C., Burke J. Disparities and access to healthy food in the United States: a review of food deserts literature. Health Place. 2010;16(5):876–884. doi: 10.1016/j.healthplace.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 109.Powell L., Slater S., Mirtcheva D., Bao Y., Chaloupka F. Food store availability and neighborhood characteristics in the United States. Prev. Med. 2007;44(3):189–195. doi: 10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 110.Kamphuis CB1 G.K., de Bruijn G.J., Wendel-Vos W., Brug J., van Lenthe F.J. Environmental determinants of fruit and vegetable consumption among adults: a systematic review. Br. J. Nutr. 2006;96(4):620–635. [PubMed] [Google Scholar]
- 111.Casagrande S., Whitt-Glover M., Lancaster K., Odoms-Young A., Gary T. Built environment and health behaviors among African Americans: a systematic review. Am. J. Prev. Med. 2009;36(2):174–181. doi: 10.1016/j.amepre.2008.09.037. [DOI] [PubMed] [Google Scholar]
- 112.Ford P., Dzewaltowski D. Disparities in obesity prevalence due to variation in the retail food environment: three testable hypotheses. Nutr. Rev. 2008;66(4):216–228. doi: 10.1111/j.1753-4887.2008.00026.x. [DOI] [PubMed] [Google Scholar]
- 113.Papas MA A.A., Ewing R., Helzlsouer K.J., Gary T.L., Klassen A.C. The built environment and obesity. Epidemiol. Rev. 2007;29:129–143. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- 114.Ross C., Mirowsky J. Neighborhood disadavantage, disorder, and health. J. Health Soc. Behav. 2001;42(3):258–276. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.