Abstract
Introduction
In the last decade, there has been an increased interest in exploring the impact of the physical birth environment on birth outcomes. The birth environment might have an important role in facilitating the production of the hormone oxytocin that causes contractions during labour. Oxytocin is released in a safe, secure and confidence-inducing environment, and environments focused on technology and medical interventions to achieve birth may disrupt the production of oxytocin and slow down the progress of labour. An experimental “birth environment room” was designed, inspired by knowledge from evidence-based healthcare design, which advocates bringing nature into the room to reduce stress. The purpose is to examine whether the ‘birth environment room’, with its design and decor to minimise stress, has an impact on birth outcomes and the birth experience of the woman and her partner.
Materials and methods
A randomised controlled trial will recruit 680 nulliparous women at term who will be randomly allocated to either the “birth environment room” or a standard room. The study will take place at the Department of Obstetrics and Gynecology at Herning Hospital, with recruitment from May 2015. Randomisation to either the “birth environment room” or standard room takes place just before admission to a birth room during labour. The primary outcome is augmentation of labour, and the study has 80% power to detect a 10% difference between the two groups (two-sided α = 0.05). Secondary outcomes are duration of labour, use of pharmacological pain relief, mode of birth, and rating of the birth experience by women and their partners.
Trial registration
NCT02478385(10/08/2016).
Article summary
Article focus
-
•
The production of oxytocin, that causes contractions during labour, may be disturbed in environments focused on technology and medical interventions.
-
•
This study will examine how a physical birth environment, designed to reduce stress, affects the outcome of labour and the birth experience of women and their partners.
Strengths and limitations of this study
-
•
This randomised controlled trial is the largest of its kind and is adequately designed to study the effect of birth environment on augmentation of labour.
-
•
Only nulliparous women in spontaneous labour at term are included in the study, which limits the possibility to generalise the results to multiparous women or women in preterm labour.
1. Introduction
1.1. Background and rationale
There is no doubt that maternity care practices need to be based on evidence ensuring safety for mother and child. Many initiatives have been implemented over the past 30 or more years to increase the safety of childbirth, for example the ability to perform an emergency caesarean within 30 min and interdisciplinary team training in acute situations [1,2]. We do not question the importance of relationships in maternity care practice which has led to the implementation of different models of care including caseload midwifery with its focus on continuity of care and carer [3,4].
This study is based on the hypothesis that the environment for birth needs greater attention to improve some of the existing challenges in modern obstetric practice. The main focus is the increasing use of augmentation during labour. The use of synthetic oxytocin has become a normal part of obstetric practice in uncomplicated nulliparous women with a spontaneous onset of labour [5]. In Scandinavian countries, the rate of augmentation in nulliparous women has reached 50% [[6], [7], [8]] with similar rates reflected in many other industrialised countries [9,10]. Use of synthetic oxytocin has severe side-effects, including hyper-stimulation, which may cause fetal distress and operative delivery [[11], [12], [13]].
Knowledge from evidence-based health care design has grown rapidly in the last decade, supporting the argument that more knowledge is needed about the effect of the design of the birth environment and design in hospitals in general [14,15]. Research from Australia and England have shown that the birth environment does not only have an impact on the birth experience and birth outcomes for women and neonates, but also on the woman's birth supporters and maternity care staff [[15], [16], [17], [18], [19], [20], [21]].
It has been hypothesised that the design of the birth environment may influence birth outcomes by altering the release of particular neuro-hormones during labour if the space is perceived as highly stressful [21]. Birth is a complex process dependent on the release of the endogenous hormone oxytocin to induce contractions. In labour, endogenous oxytocin also increases the pain threshold and has an anxiolytic effect [22]. However, few experimental studies have been performed to evaluate whether the birth environment has an impact on birth outcomes. Results from three randomised controlled trials indicate that the birth environment may affect duration of labour, pain intensity, and use of augmentation, but sample sizes were small, and further adequately powered trials are needed [17,23,24].
The aim of this study is to examine whether a birth room using an immersive decor carefully designed to minimise stress has an impact on the outcome of labour and the birth experience of the woman and her partner.
1.2. Primary hypothesis
For women labouring and birthing in “the birth environment room”, use of synthetic oxytocin to augment labour is lower than in women labouring and birthing in a standard room.
1.3. Secondary hypotheses
Giving birth in the “birth environment room” is associated with:
-
•
Shorter length of labour.
-
•
Lower use of epidural analgesia.
-
•
More uncomplicated vaginal births
-
•
An optimized better birth experience of the woman and her partner
-
•
Higher rate of breastfeeding 6 weeks post-partum
2. Materials and methods
2.1. Design
This study is a randomised controlled trial with two study arms, comparing birth outcomes between “the birth environment room” and a standard birth room.
2.2. Setting
The study will take place at the Department of Obstetrics and Gynecology at Herning Hospital, Denmark with recruitment from May 2015 to March 2018. The Obstetric Department is a specialized unit with 2500 births per year.
Before the start of the study, all midwives at the Obstetric Unit received a one-hour introduction to the project. Midwives subsequently employed are introduced to the study by project personnel and a 20-min film describing the study and recruitment procedure.
2.3. Participants and eligibility
A total of 680 women will be included according to the following criteria:
Inclusion criteria:
-
•
Nulliparous women with a spontaneous onset of labour and a baby in head-down (vertex) position
-
•
Singleton pregnancy
-
•
Maternal age of at least 18 years
-
•
Gestational age between 37 and 42 weeks
Exclusion criteria:
-
•
Lack of consent
-
•
Women with no or little ability to understand and speak Danish
2.4. Recruitment
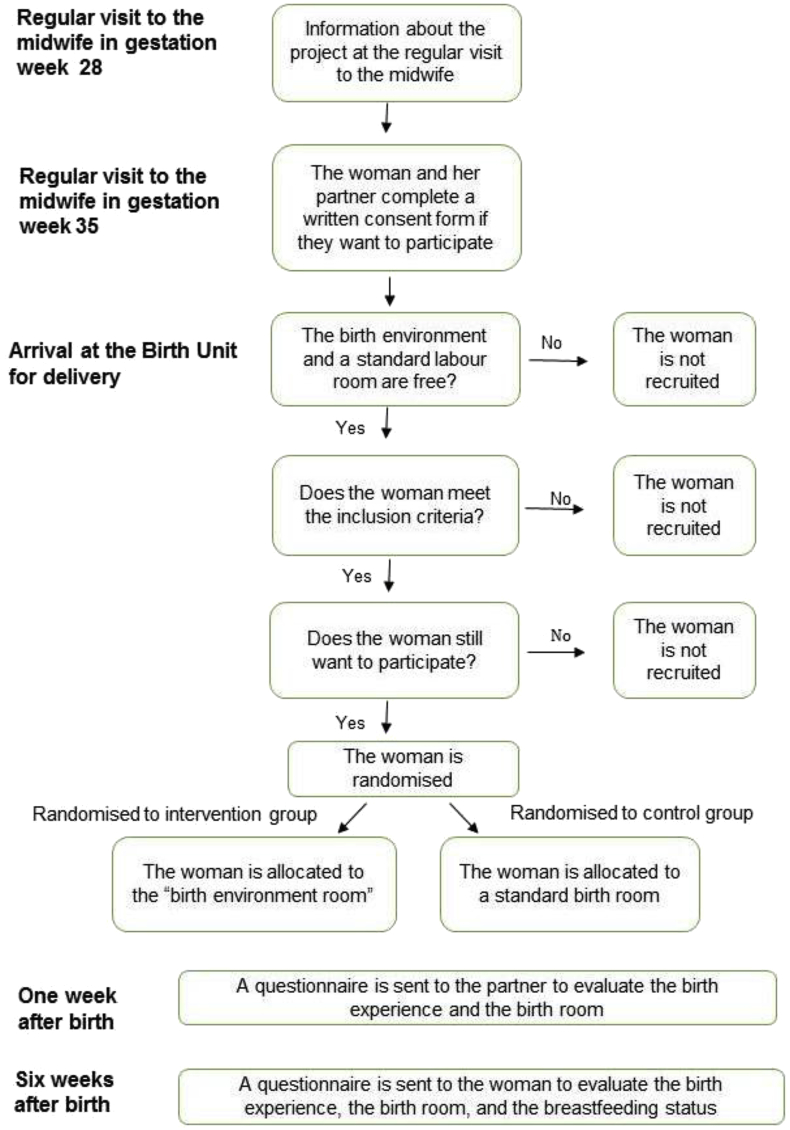
The midwife informs eligible woman about the study at the regular antenatal visit at 28 weeks gestation. The woman and her partner receive an information sheet and a consent form and are invited to bring the papers to the next visit at 35 weeks gestation. At this visit, the midwife asks the woman and her partner to complete the consent form if they are willing to participate and bring it to the labour ward. She makes sure that there are no remaining questions about the details of the study. A flowchart of the process is shown in Fig. 1. The investigators are not a part of the recruitment process.
Fig. 1.
Study flowchart.(Single column fitting image).
2.5. Randomisation
The woman and her partner are randomised to either the “birth environment room” or standard birth room at the time of arrival at the birth unit. The woman and her partner are not told whether the birth environment room is free when they contact the maternity ward as randomisation is only performed if both a standard birth room and the “birth environment room” are available. The midwife, who welcomes the couple to the birth unit, completes a questionnaire to ensure that the woman meets all inclusion criteria before randomisation. The labour onset has to be spontaneous but the woman does not need to be in active labour at the time of randomisation. When the woman arrives at the birth unit, the midwife assesses whether labour is established and contractions are progressive. If both rooms are available she can be randomised, after informed consent.
Randomisation occurs in a series of blocks of 40 using sequentially numbered opaque envelopes. Randomisation is carried out as the midwife opens the next sequentially numbered sealed opaque envelope. The envelope contains a sheet of paper specifying allocation to either "birth environment room" or standard labour room. Immediately after randomisation, the woman and her partner are admitted to the allocated room where they stay throughout labour, birth of the baby, and the first hours afterwards.
Midwives who enroll participants in the study are not aware of the randomisation sequence. A checklist has been made listing the numbers on the envelopes with information about allocation. After the trial, the investigator will ensure that the randomisation procedure was followed.
2.6. Blinding
It is not possible to blind the midwife, the woman or her partner to the allocated room. Birth outcome data are recorded by the attending midwife on a specially designed data form. Questionnaire data are entered into the database by a research assistant blinded to group allocation. The statistician who will undertake the data analysis is blinded to group allocation.
To prevent high expectations of the “birth environment room” and disappointment if the woman and her partner are allocated to a standard birth room, no pictures from the birth environment room appear on the health service website or in the information sheets given to the woman and her partner. The information sheet informs participants that the study aims to examine whether the environment has an impact on labour, but does not describe different kinds of birth environments.
2.7. Design of the intervention
2.7.1. The standard birth room
At the birth unit, there are five standard birth rooms, all having similar décor. As indicated in Fig. 2, Fig. 3, each room is 55 square meters and contains equipment such as a cardiotocography and intravenous pole. All rooms have a birth pool and an ensuite bathroom with toilet and shower. The rooms also include chairs for the woman, her partner and the midwife. The labour bed is placed in a central position, which enables a fast exit in case of an emergency. Next to the labour bed is a lounge chair for the woman's partner. The resuscitation table for the newborn is placed on the opposite side of the labour bed. There is a compact disc player available in the room, and compact discs with quiet music are available at the birth unit. The woman and her partner can also choose to bring their own compact discs.
Fig. 2.
Standard birth room, showing the adjustable height birth pool and a birthing chair positioned beside the window. In the right side of the picture is a workplace for the midwife.(2-column fitting image).
Fig. 3.
Standard birth room showing the labour bed and chair for the partner. At the opposite side is the resuscitation table for the newborn. (2-column fitting image).
2.7.2. The “birth environment room”
The major differences between the birth environment room and a standard birth room are the use of wood material, non-clinical furniture that is home-like and the projection of nature scenes on the walls. Below follows a description of the design process and the features of the room.
The process of designing and rebuilding one of the existing birth rooms took place during 2014. An interprofessional design team including midwives, a zookeeper, a design psychologist, a wellness expert, a game developer, an architect and a theatre set-designer met for two workshops to inspire and create new ideas for the design and décor of a birth environment room of the future. Each came with the views of their own profession on what was important to take into account in the design and decor of the room. The workshops brought forth a number of different perspectives and understandings of birth, and together with knowledge from research literature about healing architecture and the effect of oxytocin, four important principles emerged: the room has to be home-like and to bring nature into the room; it has to promote the partner's active support role and the woman's mobility during labour, and it has to be flexible, so it is possible for the couple to create and personalise their own birth environment on arrival, during labour, and during the birth of their infant (Link: Video birth environment room).
Supplementary video related to this article can be found at https://doi.org/10.1016/j.conctc.2019.100336.
The following is the supplementary data related to this article:
A main principle in the design of the room was not to make any compromises as far as security and safety are concerned. This means that any emergency procedures can be performed as fast and easy as in all other birth rooms.
In the development of “the birth environment room of the future”, it was necessary to rethink and challenge existing design practices. New solutions were found to bring plants and nature-based materials into the room and still comply with hygiene requirements. During the design process a specially designed double-sized mattress was developed which was covered by a number of pillows to allow changing the bed to a sofa or a nest for the woman. The textile used to cover the sofa and the pillows differs in texture from clinical hospital furniture textiles.
An innovative, interactive, digital projection system was developed by a specialist in light, sound and video design to transform the ambiance/atmosphere of the birth room. The system is operated by an iPad that the couple can easily use without introduction. Four projectors in the ceiling simultaneously project a scenic nature “movie”, onto three walls of the room. The couple can choose any of four scenarios: a ‘forest winter landscape’, ‘beach with waves’, ‘forest springtime’, and ‘forest autumn’. Two of the movies also include sounds from nature. Music for relaxation from “MusiCure” provides the background in the other two movies [25]. It is also possible for the couple to bring their own music and play it on the sound system in the room. The woman and her partner design their own birth setting by choosing a personalised relaxing atmosphere through sound, light and nature scenes.
The projection of nature scenes may provide the illusion and experience of being in the middle of nature; in a snowy landscape, in a forest with leaves falling from the trees, on a beach with crashing waves, or in the beech forest in spring with wildflowers and baby animals. The woman and her partner can match the scenes to the stages of labour, dependent on the need for hard work or relaxation, including turning them off. The nature scenes have been developed on the Snoezelen principle. The Snoezelen concept derives from Holland and combines the two words: “snuffelen” and “doezlen” that means to sniff and to doze off. The goal is to deliver stimuli to various senses by adapting the lighting, atmosphere, sounds, and textures to the individual needs of the labouring woman and her partner at the time of use [26].
The “birth environment room”, which is 39 square meters, is furnished with modern tables, lamps and chairs as indicated in Fig. 4, Fig. 5. The cardiotocography and intravenous pole are placed outside the room. The room is divided into three different zones – a wellness zone, an active zone, and a birth zone. In the wellness zone, the birth pool has a central position. In this zone, there are also hot-stones, massage oil and a small table for drinks. The birthing ball is beside the birth pool. Located in the active zone is a double-sized sofa. It is possible to adjust the height of the sofa so the woman can lean across it in an upright position.
Fig. 4.
The “birth environment room” showing the nature scene projected onto three walls. This is the active zone. (2-column fitting image).
Fig. 5.
The “birth environment room” showing the standard labour equipment in the background and the adjustable height birth pool in the foreground. (2-column fitting image).
The labour/birth bed is located in the last zone, the birth zone, with the standard bed in the same position as in the five standard birth rooms. The labour bed is covered with a blanket until needed, nudging the woman to not choose a lying down position from the start of her labour. The resuscitation equipment for the newborn is placed next to the bed. On the other side of the bed is a bar stool, so that the partner can be in an upright and high position next to the woman during the second stage of labour if this occurs on the bed. Next to the bed, a ”partner's cupboard” is located, containing face cloths, vomit-bags, water glasses and straws, with an invitation to use freely in response to the woman's needs.
2.8. Outcome measures
2.8.1. Primary outcome
The primary outcome of this study is augmentation of labour, and is measured as the proportion of women who are augmented during labour (defined as the need for synthetic oxytocin infusion because of dystocia/slow progress in labour). Cervix dilation at the time of augmentation is also measured. See Table 1 for details.
Table 1.
Timing and source of data collection for primary and secondary outcomes.
| Immediately after birth | 1 week after birth | 6 weeks after birth | |
|---|---|---|---|
| Primary outcome | |||
| Use of oxytocin for dystocia | Medical record | ||
| Secondary outcome | |||
| Length of labour | Medical record | ||
| Use of pain relief | Medical record | ||
| Uncomplicated birth | Medical record | ||
| The woman's birth experience | Questionnaire | ||
| The partner's birth experience | Questionnaire | ||
| Breastfeeding duration | Questionnaire | ||
2.8.2. Secondary outcomes
Length of labour is measured as time spent at the birth unit from randomisation to birth of the baby. Cervix dilation is measured when the woman enters the birth room to determine any difference in the two groups regarding labour progress at the time of randomisation.
Use of pain relief during labour is measured as the proportion of women receiving epidural anesthesia, inhalation analgesia, morphine, acupuncture, transcutaneous electrical nerve stimulation and birth pool for labour pain.
Number of uncomplicated vaginal births is measured as the proportion of uncomplicated births in the two groups, defined as a spontaneous birth without episiotomy, estimated bleeding less than 1000 ml, no 3rd or 4th degree perineal lacerations, and an infant with Apgar score >9 after 5 min.
The woman's birth experience is measured by the WOCCA questionnaire [27]. The WOCCA is a validated 15-item questionnaire with a 6-point Likert scale evaluating the woman's birth experience. The questionnaire evaluates the birth experience including questions about satisfaction with care, support, presence of midwife, information, feeling of being listened to, attentiveness towards psychological needs and birth wishes, participation in decision making, usefulness of suggestions for pain relief, support for partner, support from partner, and loss of internal and external control. It is an electronic questionnaire sent to the woman 6 weeks after birth of the baby.
The partners' birth experience is measured by an adjusted version of the WOCCA questionnaire, sent as an electronic questionnaire to the partner 1–2 weeks after birth. Before using the adjusted questionnaire, a validation study was carried out, interviewing 5 partners 1–7 days after birth. The partner's questionnaire contains 15 questions about the birth experience of the father, including satisfaction with care, support, presence of midwife, information, feeling of being listened to, attentiveness towards psychological needs and birth wishes, participation in decision making, usefulness of suggestions for pain relief, support for partner, support from midwife, and loss of internal and external control. Duration of breast-feeding 6 weeks post partum is measured by additional questions in the electronic questionnaire sent to the woman at this point in time. The woman is asked if she is still full or partly breastfeeding or if she is not breastfeeding anymore.
The questionnaires to the woman and her partner also include questions about level of education and civil/marriage status. They are also asked if they had any preferences for type of labour/birth room before enrollment, and if this preference was important for them after they entered the allocated room. For the couples allocated to the birth environment room, four additional questions about the nature scenes and music were added.
2.9. Data collection and management
Data are collected from a questionnaire completed by the attending midwife together with information from the hospital records and from postpartum questionnaires about birth experience completed by the woman and her partner. Printed Case Report Forms are used to record data whereafter data are entered into an electronic database (www.survey-xact.com).
Data are anonymised using a study identity number. Variables that might identify individuals will only be accessible by the midwives who enroll participants and by the primary investigator of the study.
2.10. Statistical methods
2.10.1. Power calculation
The sample size calculation is based on the primary outcome measure, augmentation of labour. Using a 2-sided alpha of 5%, 328 women should be included in each group to have a power of 80% to detect a difference of 10% in the proportion of women who receive augmentation. With drop-out in mind, we increased this sample size to 680.
2.10.2. Data analysis
Data will be analysed according to the intention-to-treat principle. The statistician will be blinded to group allocation until the completion of the analysis. Descriptive statistics will be used to examine baseline characteristics of the participants. If there are any differences in the two groups regarding confounding variables such as age, body-mass index or smoking status, these will be adjusted for in the analysis using a logistic regression model. Also, it will be possible to control for level of cervical dilation at time of randomisation, and the number of midwives responsible for the woman's care from randomisation to birth of the baby.
Continuous data will be analysed using the t-test for normally distributed data and Mann-Whitney U test for not normally distributed data. Categorical data will be analysed using chi-square test. The significance level will be set at P = 0.05. Depending on the number of missing data, imputation of missing values may be carried out and added to the data set in a supplementary analysis. Details of all women who meet the inclusion criteria but who do not participate in the study will be collected to describe the reasons for non-participation.
3. Discussion
One of the strengths of this study is the randomised design. Moreover, all midwives employed at the research site have received training in the use of the newly built “birth environment room” and are aware that there is no difference in the standard of care available for women in either the standard or experimental room. Four months before the start of the study, the room was used for as many birthing women as possible, to ensure that the midwives were familiar with the room. Great effort has been made to minimise any subject-expectancy effect. Therefore it is not possible to find pictures of the room on the hospital website, and the information sheet given to the couple is described in a neutral way to avoid high expectations of the “birth environment room” before randomisation. Furthermore, the midwives are aware of having the same positive attitude during the randomisation procedure regardless of allocation.
Women allocated to the study are nulliparous, in spontaneous labour at term with a singleton pregnancy in the head down position. These inclusion criteria were chosen to ensure that women are as comparable as possible. This selection of participants may limit the possibility to generalise the results of this study to multiparous women or women in preterm labour.
The use of a validated questionnaire (WOCCA) to measure the woman's birth experience is a strength of the study. The questionnaire has already been used in a Danish setting and no translation of the questionnaire was necessary. The questionnaire was tested for validity during pilot studies including test-retest reliability (Spearman coefficient, 0.95 for birth experience and between 0.8 and 1 for all other questions). Chronbachs alpha for internal consistency was 0.963 (missing data less than 1%) [24].
A potential limitation of the study is the use of a revised version of the WOCCA questionnaire to evaluate the partner's birth experience. However, we found that with only a few changes the WOCCA questionnaire for women included the relevant content that we intended to measure in their partners. An expert group, including the first author of the WOCCA, was involved in the revision. Validity testing included interviewing five partners who completed the questionnaire within one week after birth. Small changes were made after these interviews, and the final version was approved by the expert group.
Ethics and dissemination
The study was reported to the local scientific ethical committee and in accordance with the Declaration of Helsinki. The study was granted exemption from requiring ethical approval by the Ethical committee (Reference number: 247/2014). The study has been reported to the Danish Data Protection Agency (reference number: 1-16-02-34-15) and the clinical trials registration website of the National Institutes of Health (NCT02478385).
Board Name: The Central Denmark Region Committees on Health Research Ethics Board Affiliation: The Central Denmark Region Committees on Health Research Ethics. Phone: +45 7841 0182. Email: komite@rm.dk.
Details of funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. The study is financed by the Department of Obstetrics and Gynaecology at Herning Hospital. Ann Fogsgaard is director of the Department of Obstetrics and Gynaecology and also co-author. Ann Fogsgaard has no authority to influence publication of the study findings and is independent of the statistical analysis.
Patient involvement
Patients were involved in the design process of the birth environment room and also in the revision of the WOCCA questionnaire evaluating the partner's birth experience. The research design was completed without patient involvement and patients were not invited to contribute to the writing or editing of this document for readability or accuracy.
Consent to participate
When the woman and her partner decide to participate in the study, they complete a written consent form. The consent form is kept together with their data. They are informed that refusal to participate in no way will influence their care. They may withdraw at any time without any consequences for them. The couple is anonymous in the reported material and none of the health professionals responsible for the care are aware of the answers given in the questionnaires.
Consent for publication
The study findings will be presented at international conferences, published in peer-reviewed journals, and communicated to healthcare professionals and the layman press.
Data sharing
We did not plan for the dataset to be shared when the study protocol was developed. Therefore, we have not obtained consent from the study participants to share the data. Thus, the data will not be shared.
Authors' contributions
Iben Lorentzen(guarantor): designed and initiated the trial, made a substantial contribution to acquisition of data, and wrote the first draft of the manuscript.
Charlotte Sander Andersen: made a substantial contribution to acquisition of data and took part in revising the manuscript.
Ann Fogsgaard: contributed to conception and design and took part in revising the manuscript.
Henriette Svenstrup: contributed to conception and design and took part in revising the manuscript.
Maralyn Foureur: contributed to the design of the study and took part in revising the manuscript.
Finn Lauszus: made a substantial contribution to the planning of statistical analysis and power calculation and took part in revising the manuscript.
Ellen Aagaard Nohr: contributed to the design of the study and took part in revising the manuscript.
All authors have approved the final version of the manuscript.
Acknowledgements
We are grateful to all the women and their partners who participate in the study and to the midwives at the department of Obstetrics and Gynecology in Herning Hospital who recruited women and partners to the study.
We are grateful to Charlotte Overgaard who kindly gave permission to use the WOCCA questionnaire to evaluate the women's birth experience and for invaluable advice in validation of the questionnaire to evaluate the partner's birth experience.
We are grateful to all midwives and all other professionals for participating in the workshops and their invaluable contribution to the design of the room.
We also owe a debt of gratitude to the traders who developed specially designed equipment for the room.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.conctc.2019.100336.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Multimedia component 1
References
- 1.Posthumus A.G., Scholmerich V.L., Waelput A.J. Bridging between professionals in perinatal care: towards shared care in The Netherlands. Matern. Child Health J. 2013;17(10):1981–1989. doi: 10.1007/s10995-012-1207-4. [DOI] [PubMed] [Google Scholar]
- 2.Kesmodel U.S., Jolving L.R. Measuring and improving quality in obstetrics--the implementation of national indicators in Denmark. Acta Obstet. Gynecol. Scand. 2011;90(4):295–304. doi: 10.1111/j.1600-0412.2011.01078.x. [DOI] [PubMed] [Google Scholar]
- 3.Sandall J., Soltani H., Gates S., Shennan A., Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst. Rev. 2016;4:CD004667. doi: 10.1002/14651858.CD004667.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hodnett E.D., Gates S., Hofmeyr G.J., Sakala C. Continuous support for women during childbirth. Cochrane Database Syst. Rev. 2013;7:CD003766. doi: 10.1002/14651858.CD003766.pub5. [DOI] [PubMed] [Google Scholar]
- 5.Brown H.C., Paranjothy S., Dowswell T., Thomas J. Package of care for active management in labour for reducing caesarean section rates in low-risk women. Cochrane Database Syst. Rev. 2013;9:CD004907. doi: 10.1002/14651858.CD004907.pub3. DOI: (9):CD004907. [DOI] [PubMed] [Google Scholar]
- 6.Gottvall K., Waldenstrom U., Tingstig C., Grunewald C. In-hospital birth center with the same medical guidelines as standard care: a comparative study of obstetric interventions and outcomes. Birth. 2011;38(2):120–128. doi: 10.1111/j.1523-536X.2010.00461.x. [DOI] [PubMed] [Google Scholar]
- 7.Blix E., Pettersen S.H., Eriksen H., Royset B., Pedersen E.H., Oian P. Use of oxytocin augmentation after spontaneous onset of labor. Tidsskr. Nor. Laegeforen. 2002;122(14):1359–1362. PII: 548516. [PubMed] [Google Scholar]
- 8.Kjaergaard H., Olsen J., Ottesen B., Dykes A.K. Incidence and outcomes of dystocia in the active phase of labor in term nulliparous women with spontaneous labor onset. Acta Obstet. Gynecol. Scand. 2009;88(4):402–407. doi: 10.1080/00016340902811001. [DOI] [PubMed] [Google Scholar]
- 9.Tracy S.K., Welsh A., Hall B. Caseload midwifery compared to standard or private obstetric care for first time mothers in a public teaching hospital in Australia: a cross sectional study of cost and birth outcomes. BMC Pregnancy Childbirth. 2014;14 doi: 10.1186/1471-2393-14-46. 46-2393-14-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beckmann M., Kildea S., Gibbons K. Midwifery group practice and mode of birth. Women Birth. 2012;25(4):187–193. doi: 10.1016/j.wombi.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Berglund S., Grunewald C., Pettersson H., Cnattingius S. Severe asphyxia due to delivery-related malpractice in Sweden 1990-2005. BJOG. 2008 Feb;115(3):316–323. doi: 10.1111/j.1471-0528.2007.01602.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berglund S., Grunewald C., Pettersson H., Cnattingius S. Risk factors for asphyxia associated with substandard care during labor. Acta Obstet. Gynecol. Scand. 2010;89(1):39–48. doi: 10.3109/00016340903418751. [DOI] [PubMed] [Google Scholar]
- 13.Oscarsson M.E., Amer-Wahlin I., Rydhstroem H., Kallen K. Outcome in obstetric care related to oxytocin use. A population-based study. Acta Obstet. Gynecol. Scand. 2006;85(9):1094–1098. doi: 10.1080/00016340600804530. [DOI] [PubMed] [Google Scholar]
- 14.Berry L.L., Parker D., Coile R.C., Jr., Hamilton D.K., O'Neill D.D., Sadler B.L. The business case for better buildings. Front. Health Serv. Manag. 2004;21(1):3–24. PMID: 15469120. [PubMed] [Google Scholar]
- 15.Jiang S., Verderber S. On the planning and design of hospital circulation zones: a review of the evidence-based literature. HERD. 2016 doi: 10.1177/1937586716672041. [DOI] [PubMed] [Google Scholar]
- 16.Fahy K.M., Parratt J.A. Birth territory: a theory for midwifery practice. Women Birth. 2006;19(2):45–50. doi: 10.1016/j.wombi.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Hodnett E.D., Stremler R., Weston J.A., McKeever P. Re-conceptualizing the hospital labor room: the PLACE (pregnant and laboring in an ambient clinical environment) pilot trial. Birth. 2009;36(2):159–166. doi: 10.1111/j.1523-536X.2009.00311.x. [DOI] [PubMed] [Google Scholar]
- 18.Singh D., Newburn M. Feathering the nest: what women want from the birth environment. RCM Midwives. 2006;9(7):266–269. [PubMed] [Google Scholar]
- 19.Foureur M., Davis D., Fenwick J. The relationship between birth unit design and safe, satisfying birth: developing a hypothetical model. Midwifery. 2010;26(5):520–525. doi: 10.1016/j.midw.2010.05.015. [DOI] [PubMed] [Google Scholar]
- 20.Hammond A., Foureur M., Homer C.S. The hardware and software implications of hospital birth room design: a midwifery perspective. Midwifery. 2014;30(7):825–830. doi: 10.1016/j.midw.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 21.Hammond A., Foureur M., Homer C.S., Davis D. Space, place and the midwife: exploring the relationship between the birth environment, neurobiology and midwifery practice. Women Birth. 2013;26(4):277–281. doi: 10.1016/j.wombi.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 22.Uvnas-Moberg K., Petersson M. Oxytocin, a mediator of anti-stress, well-being, social interaction, growth and healing. Z. Psychosom. Med. Psychother. 2005;51(1):57–80. doi: 10.13109/zptm.2005.51.1.57. PMID: 15834840. [DOI] [PubMed] [Google Scholar]
- 23.MacVicar J., Dobbie G., Owen-Johnstone L., Jagger C., Hopkins M., Kennedy J. Simulated home delivery in hospital: a randomised controlled trial. BJOG An Int. J. Obstet. Gynaecol. 1993;100(4):316–323. doi: 10.1111/j.1471-0528.1993.tb12972.x. [DOI] [PubMed] [Google Scholar]
- 24.Jamshidi Manesh M., Kalati M., Hosseini F. Snoezelen room and childbirth outcome: a randomized clinical trial. Iran. Red Crescent Med. J. 2015;17(5) doi: 10.5812/ircmj.17(5)2015.18373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.MusiCure music as medicine. http://musicure.com/. Accessed 15 January 2017.
- 26.Mertens K. 2018. International Snoezelen Association ISNA - Snoezelen professional e.V.https://snoezelen-professional.com/en/ Available at: 10/17, 2014. [Google Scholar]
- 27.Overgaard C., Fenger-Gron M., Sandall J. The impact of birthplace on women's birth experiences and perceptions of care. Soc. Sci. Med. 2012;74(7):973–981. doi: 10.1016/j.socscimed.2011.12.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1