Abstract
Rationale and Objectives:
The objective of this study was to evaluate the association of communication practices with timely follow-up of screening mammograms read as Breast Imaging Reporting and Data Systems (BI-RADS) 0 in the Population-based Research Optimizing Screening through Personalized Regimens (PROSPR) consortium.
Materials and Methods:
A radiology facility survey was conducted in 2015 with responses linked to screening mammograms obtained in 2011–2014. We considered timely follow-up to be within 15 days of the screening mammogram. Generalized estimating equation models were used to evaluate the association between modes of communication with patients and providers and timely follow-up, adjusting for PROSPR site, patient age, and race and ethnicity.
Results:
The analysis included 34,680 mammography examinations with a BI-RADS 0 assessment among 28 facilities. Across facilities, 85.6% of examinations had a follow-up within 15 days. Patients in a facility where routine practice was to contact the patient by phone if follow-up imaging was recommended were more likely to have timely follow-up (odds ratio [OR] 4.63, 95% confidence interval [CI] 2.76–7.76), whereas standard use of mail was associated with reduced timely follow-up (OR 0.47, 95% CI 0.30–0.75). Facilities that had standard use of electronic medical records to report the need for follow-up imaging to a provider had less timely follow-up (OR 0.56, 95% CI 0.35–0.90). Facilities that routinely contacted patients by mail if they missed a follow-up imaging visit were more likely to have timely follow-up (OR 1.65, 95% CI 1.02–2.69).
Conclusions:
Our findings support the value of telephone communication to patients in relation to timely follow-up. Future research is needed to evaluate the role of communication in completing the breast cancer screening episode.
Keywords: Screening mammography, communication, timely follow-up
INTRODUCTION
Mammography screening reduces breast cancer mortality among women aged 40–74 years (1). Progression through the screening process, from initial screening, through follow-up of abnormal results, to treatment, can fail at multiple points in the screening episode (2–4). Lack of effective communication between facilities, providers, and patients may delay follow-up and lead to adverse health outcomes, including anxiety, delay in diagnosis, and widening of cancer outcome disparities (5–10).
Mode of communication can impact timely follow-up of abnormal mammograms. Commonly used modes of communicating mammography results to patients include verbal communication (including in-person communication, by telephone, and leaving a voice message) and written communication by conventional mail or through a patient portal to the electronic medical record (EMR). In a study among women of diverse ethnicity who had a screening mammogram and a Breast Imaging Reporting and Data Systems (BIRADS) 0 result, discussion of results with a provider was associated with more timely follow-up, although this finding did not persist on multivariate analysis controlling for insurance status (11). Communication factors such as patients asking questions, receiving next-step information, and being told that follow-up is needed have also been associated with timely follow-up of an abnormal mammogram (12,13).
The approach used to communicating mammography results to the clinician who ordered the mammogram may also be associated with timely follow-up of abnormal mammograms (11,13,14). Common modes of communicating mammography results to the ordering provider include verbal communication by phone, written communication by conventional mail, sending a notification of results through the EMR, and sending the mammography report by fax.
Timely follow-up for a BI-RADS 0 assessment has been defined in various ways. The Mammography Quality Standards Act (MQSA) states that results of a mammogram can be reported to a woman at the time of the examination or mailed to her within 30 days of the examination. The MQSA also states “The FDA (U.S. Food & Drug Administration) believes that communication of suspicious or highly suggestive results can ordinarily be accomplished within 5 working days” and “In the case of exams where the assessment is ‘incomplete, needs additional imaging evaluation’, FDA recommends that facilities communicate this (verbally or in writing) to the patient as soon as possible to avoid delays in patient work-up” (15). The Food and Drug Administration supports effective communication systems, but the system details are left to each facility. Guidelines for expected time to follow-up vary in different countries, but the European guidelines include quality indicators of 10 workdays for a notification and an additional 5 workdays until the follow-up test is obtained (16). The New Zealand guidelines also recommend a follow-up assessment within 15 days (17). The United Kingdom guidelines recommend a follow-up assessment within 3 weeks (18), and Canadian and Australian guidelines recommend follow-up between 28 days and 5 weeks, respectively (19,20).
The objectives of the present study were (1) to describe radiology facility communication modalities used as standard practice for communicating a category BI-RADS 0 result of a screening mammogram and (2) to evaluate the association of communication practices with timely follow-up of BIRADS 0 screening mammograms.
MATERIALS AND METHODS
The Population-based Research Optimizing Screening through Personalized Regimens (PROSPR) consortium is a National Cancer Institute-funded consortium with the overall aim to conduct multisite, coordinated, and transdisciplinary research to evaluate and improve cancer screening processes for breast, cervical, and colorectal cancer. The present study focuses on breast cancer screening. We conducted a cross-sectional survey of all radiology facilities within the clinical care networks affiliated with Brigham and Women’s Hospital, Boston, Massachusetts; Dartmouth-Hitchcock Health System, New Hampshire; the University of Pennsylvania, Philadelphia, Pennsylvania; and in the statewide Vermont Breast Cancer Surveillance System. Each site’s institutional review board approved the study. Patient-level data were obtained from PROSPR’s central data repository, including race and ethnicity (Asian, black, Hispanic, white, other, and unknown), age at screening (40–49 years, 50–64 years, and 65–74 years), screening examination date, and the types and results of screening and follow-up examinations.
Survey Content and Coding of Responses
The survey queried a range of communication practices of mammography facilities, including two clinical scenarios directly related to timely follow-up of BI-RADS 0: (1) additional imaging is recommended by the radiologist after a screening mammogram and (2) patient misses a scheduled appointment for additional imaging. For each scenario, the survey assessed the standard communication modalities used. The survey was piloted for clarity among radiologists and radiology facility directors within the PROSPR network and revised according to feedback obtained (see Appendix S1 for full survey).
The scenarios regarding communication used the stem, “How does your facility communicate with the patient (or provider) regarding the following reports or clinical scenarios? Identify the one approach that reflects your standard practice. Only choose additional options if they are routinely used for all patients.” Response options for patients were listed as phone, regular mail, online patient portal, in person, other, not applicable, or unknown. Response options for providers were listed as phone, regular mail, EMR, fax, not applicable, other, or unknown. If a given modality was identified, the response was coded as using that modality whether or not additional responses were coded.
Survey Protocol
All radiology facilities affiliated with the PROSPR programs consortium were invited to participate in the online survey. A $50 incentive for survey completion was offered for all clinical care networks, but one network chose not to use the incentive to be consistent with procedures for data collection in PROSPR (Vermont). A facility director or a lead technologist was identified as the respondent at each site based upon input from leaders in the radiology department at each program. The survey was administered from July 7, 2015, to October 2, 2015.
Statistical Analysis
The analysis of follow-up time was restricted to women aged 40–74 who had no record of previous breast cancer. Screening mammograms were defined as having screening as an indication and no breast imaging within the prior 90 days. All screening mammograms performed at the participating facilities in the years 2011–2014 were identified, as well as follow-up procedures including diagnostic mammogram, ultrasound, magnetic resonance imaging, or biopsy. A BI-RADS 0 was either assigned by the facility or inferred for the initial screen if the patient underwent further diagnostic workup on the same day as the screening examination. The BI-RADS 0 category included recommendations for further imaging or retrieval of prior examinations. When a zero was assigned as a placeholder pending receipt of previous images, the zero was replaced by the assigned assessment after comparisons were made and transmitted to the central data repository. However, zeros that were not resolved remained zero. To adequately assess follow-up, we included only examinations with at least 90 days of subsequent follow-up.
We examined rates of timely follow-up in examinations assigned a BI-RADS 0 to determine overall rates of timely follow-up within 0–15 days and described variation in timely follow-up across radiology facilities. However, because same-day follow-up involves only in-person communication, we excluded the same-day follow-up examinations from the analysis of the relationship of survey responses to timely follow-up within 1–15 days.
We described reported use by radiology facilities of modalities to communicate screening results to patients and to the ordering providers in the following clinical scenarios:(1) additional imaging is recommended and (2) patient misses a scheduled appointment for additional imaging.
We evaluated the association of survey responses with follow-up while adjusting for woman-level characteristics. To control for correlation of outcomes within each facility, we used a generalized estimating equation logistic regression model to evaluate the association of provider communication modality with timely follow-up, clustering by the radiology facility and controlling for the woman’s age, race, and ethnicity. Each communication modality was coded as 1 or 0 (respondent identified whether this modality was part of standard practice or not). Respondents for each facility could identify one or more than one mode of communication as part of routine practice for a given scenario. We first examined whether each mode of communication was associated with timely follow-up or not, as measured by the odds ratio (OR), adjusting for woman-level characteristics. In a sensitivity analysis, we controlled for average household income in the woman’s zip code, categorized into quartiles, to assess the effect of socioeconomic indicators on the model. Modes of communication that were statistically significantly associated with timely follow-up were included in a more complex joint model for communication that adjusted for all individually significant modes of communication for that survey question.
RESULTS
Of 31 radiology facilities invited to participate, 28 (90%) completed the survey. Of the 28 facilities, 1 conducted only screening mammograms and the remainder conducted both screening and diagnostic examinations. These facilities conducted a total of 325,485 screening mammograms during the study window. We restricted our analysis to the 34,680 examinations (10.7%) with a BI-RADS 0 result (Table 1). These examinations were for 31,775 women, of whom 8% had more than one incomplete BI-RADS 0 in the study window. The demographic characteristics of the patients who underwent the screening examinations are presented in Table 2.
TABLE 1.
Facilities, Screening Examinations (2011–2014), BI-RADS 0, and Timely Follow-up
| Health-care Setting (PROSPR Center) | Number of Facilities | Screening Examinations | Number of Months of Examinations Included | BI-RADS 0 | Follow-up, ≤15 d | Follow-up, Same Day | Follow-up, Days 1–15 |
|---|---|---|---|---|---|---|---|
| n (%) | n (%)* | n (%) | n (%) | ||||
| A | 7 | 69,038 | 24 | 7,125(10.3) | 5,983 (84.0) | 2,402 (40.1) | 3,581 (59.9) |
| B | 5 | 15,362 | 45 | 1,013 (6.7) | 768 (75.8) | 185 (24.1) | 583 (75.9) |
| C | 3 | 43,074 | 48 | 4,069 (9.5) | 3,358 (82.5) | 196 (5.8) | 3,162 (94.2) |
| D | 13 | 198,011 | 45 | 22,473 (11.4) | 19,589 (87.2) | 3,519 (18.0) | 16,070 (82.0) |
| Total | 28 | 325,485 | 34,680 (10.7) | 29,698 (85.6) | 6,302 (21.2) | 23,396 (78.8) |
BI-RADS, Breast Imaging Reporting and Data Systems; PROSPR, Population-based Research Optimizing Screening through Personalized Regimens.
Column of timely follow-up within 15 days is inclusive of both follow-up on the same day and follow-up within days 1–15.
TABLE 2.
Demographic Characteristics of Screening Mammograms
| Patient Characteristics | Screening Mammograms n |
Abnormal Screening Results BI-RADS 0 n (%) |
Follow-up, <15 d n (%) |
|---|---|---|---|
| Age (y) | |||
| 40‒49 | 87,472 | 12,829 (14.7) | 10,969 (85.5) |
| 50‒64 | 168,714 | 16,083(9.9) | 13,696 (85.2) |
| 65‒74 | 69,299 | 5,768 (8.3) | 5,033 (87.3) |
| Race and ethnicity | |||
| White non-Hispanic | 279,252 | 29,466 (10.5) | 25,605 (86.9) |
| Black non-Hispanic | 23,345 | 2,531 (10.8) | 1,895 (74.9) |
| Hispanic | 6,037 | 665 (11.0) | 538 (80.9) |
| Asian non-Hispanic | 4,726 | 478 (10.1) | 374 (78.2) |
| Other non-Hispanic | 6,561 | 808 (12.3) | 668 (82.7) |
| Missing | 5,564 | 732 (13.2) | 618 (84.4) |
| Total | 325,485 | 34,680 (10.7) | 29,698 (85.6) |
BI-RADS, Breast Imaging Reporting and Data Systems.
The proportion of patients with follow-up within 15 days was 85.6% overall and varied from 75.8% to 87.2% across the PROSPR centers (Table 1). The percentage of BI-RAD 0’s that had follow-up imaging or a procedure on the same day overall was 21.2%, although this percentage varied widely by health-care PROSPR center (Table 1). Figure 1 shows the percentage of BI-RADS 0 readings with timely follow-up (same day and days 1–15) by facility with the facilities ordered by the volume of BI-RADS 0 from smallest to largest.
Figure 1.
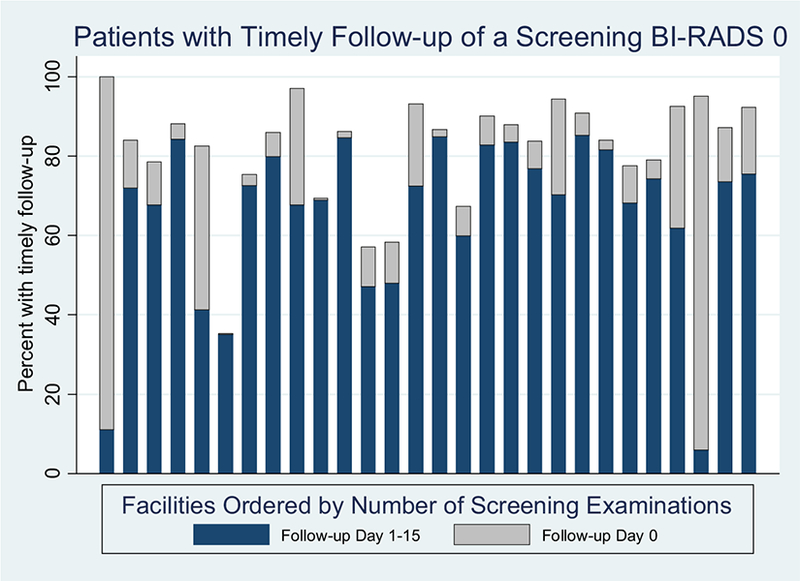
Percentage with timely follow-up of a screening BI-RADS 0 by patient contact modality. The percentage of patients with timely follow-up within 0–15 days is shown after a screening mammogram assessed an incomplete BI-RADS 0 ordered by the number of screening mammograms with a BI-RADS 0 in the data collection period. Timely follow-up is divided into those followed up on the same day as the screening mammogram vs 1–15 days after the initial screening mammogram. The x−axis presents the 28 facilities ordered from those with the lowest to those with the highest number of mammography screening examinations in the study. BI-RADS, Breast Imaging Reporting and Data Systems.
Communication of Mammography Results
Two of the 28 facilities reported that they asked patients for their preferred modality to receive screening results. Facilities used a range of modalities to communicate mammography results to patients and their providers. The most common modality used to communicate the scenario of additional imaging recommended to the patient was by phone (89.3%), and the most common modality used to communicate the scenario to the provider was through the EMR (82.1%).
The most common modality used to communicate mammography results in the scenario of patient misses a scheduled appointment for additional imaging to the patient was by phone(71.4%); this was also the single most common modality used to communicate this result to the ordering provider (28.6%) (Table 3).
TABLE 3.
Association of Timely Follow-up and Facility-level Communication Modality
| Communication Type | Patient Misses Scheduled Appointment for Additional Imaging | |||
|---|---|---|---|---|
| Facilities Endorsing in Survey (%) | Follow-up in 1–15 d When Endorsed (%) vs Not Endorsed (%) | Impact on Timely Follow-up After Adjustment* (P Value) | OR (95% CI) | |
| To patient | ||||
| Phone | 71.4 | 85.5 vs 72.8 | .08 | 1.81 (0.93–3.53) |
| 32.1 | 85.1 vs 80.3 | .0429 | 1.65 (1.02–2.69) | |
| Patient portal | 3.6 | 81.8 vs 82.4 | <.0001 | 2.05 (1.73–2.41) |
| In person | 0.0 | − | − | − |
| To provider | ||||
| Phone | 28.6 | 89.3 vs 77.3 | .0012 | 2.61 (1.46–4.66) |
| 17.9 | 76.9 vs 83.1 | .63 | 1.30 (0.45–3.79) | |
| Electronic medical record | 21.4 | 78.0 vs 83.3 | .95 | 0.98(0.49–1.93) |
| Fax | 7.1 | 82.2 vs 82.5 | .57 | 0.79 (0.35–1.79) |
CI, confidence interval; OR, odds ratio; PROSPR, Population-based Research Optimizing Screening through Personalized Regimens.
The generalized estimating equation model controlled for age, race and ethnicity, PROSPR site, and the correlation of outcomes within a radiology facility. Results are presented for the patient and the provider among the 28 facilities for the scenario of patient misses a scheduled appointment for additional imaging.
Bivariate Analysis
Facilities that used the standard approach to communicate results to patients verbally by phone in the scenario of additional imaging recommended had higher rates of timely follow-up for BI-RADS 0 findings than facilities that did not (OR 4.63, 95% confidence interval [CI] 2.76–7.76; P < .0001). Facilities whose standard approach to communicate results in written form by conventional mail for this scenario had lower rates of timely follow-up (OR 0.47, 95% CI 0.30–0.75; P = .0012).Facilities whose standard approach is to use the EMR to communicate screening results to providers in this scenario also had lower rates of timely follow-up (OR 0.56, 95% CI 0.35–0.90; P = .0163) (Table 4).
TABLE 4.
Association of Timely Follow-up and Facility-level Communication Modality
| Communication Type | Additional Imaging Recommended | |||
|---|---|---|---|---|
| Facilities Endorsing in Survey (%) | Follow-up in 1–15 d When Endorsed (%) vs Not Endorsed (%) | Impact on Timely Follow-up After Adjustment* (P Value) | OR (95% CI) | |
| To patient | ||||
| Phone | 89.3 | 83.5 vs 53.1 | <.0001 | 4.63 (2.76–7.76) |
| 57.1 | 77.3 vs 87.8 | .0012 | 0.47 (0.30–0.75) | |
| Patient portal | 39.3 | 77.7 vs 85.4 | .13 | 0.66 (0.39–1.12) |
| In person | 10.7 | 65.2 vs 82.7 | .17 | 0.56 (0.25–1.27) |
| To provider | ||||
| Phone | 3.6 | 70.3 vs 82.5 | .0051 | 1.24 (1.07–1.44) |
| 14.3 | 77.9 vs 83.5 | .58 | 0.80 (0.36–1.76) | |
| Electronic medical record | 82.1 | 81.9 vs 89.2 | .0163 | 0.56 (0.35–0.90) |
| Fax | 42.9 | 81.3 vs 82.9 | .65 | 0.85 (0.42–1.71) |
CI, confidence interval; OR, odds ratio; PROSPR, Population-based Research Optimizing Screening through Personalized Regimens.
The generalized estimating equation model controlled for age, race and ethnicity, PROSPR site, and the correlation of outcomes within a radiology facility. Results are presented for the patient and the provider among the 28 facilities for the scenario of additional imaging recommended, when not performed on the same day as the screening examination.
In the scenario of patient misses a scheduled appointment for additional imaging, facilities that used verbal communication by phone to convey results to the ordering provider had higher rates of timely follow-up than those that did not (OR 2.61, 95% CI 1.46–4.66; P = .0012).
Multivariate Analysis
For each scenario and each type of communication (to the patient or the ordering provider), we considered how the individually significant strategies might operate jointly on timely follow-up (Table 5). In the scenario of additional imaging recommended, communication to the patient by phone remained positively associated with timely follow-up, and communication to the patient by conventional mail remained negatively associated with timely follow-up (Table 5, model A). Of note, only two facilities used conventional mail as the only approach to communicate with patients in this scenario (Fig 2a). In the scenario of additional imaging recommended, communication to the ordering provider through the EMR remained negatively associated with timely follow-up in the joint analysis. However, communication to the provider by phone was no longer associated with timely follow-up (Table 5, model B). Of note, most of the facilities using EMR for provider communication in this scenario used this as their sole approach (Fig 2b).
TABLE 5.
Association of Patient and Provider Communication Strategies with Timely Follow-up in Multivariate Analyses
| Variable | OR | 95% CI | P Value |
|---|---|---|---|
| Model A: Additional imaging recommended—patient communication* | |||
| Patient phone communication | 3.63 | 2.29–5.76 | <.0001 |
| Patient mail communication | 0.53 | 0.34–0.81 | .003 |
| Model B: Additional imaging recommended—provider communication* | |||
| Provider electronic medical recordcommunication | 0.52 | 0.29–0.92 | .02 |
| Provider phone communication | 0.64 | 0.36–1.16 | .14 |
| Model C: Patient misses scheduled appointment for additional imaging-patient communication* | |||
| Patient mail communication | 1.65 | 1.01–2.69 | .04 |
| Patient portal communication | 1.28 | 0.79–2.07 | .32 |
CI, confidence interval; OR, odds ratio; PROSPR, Population-based Research Optimizing Screening through Personalized Regimens.
The generalized estimating equation models controlled for age, race and ethnicity, PROSPR site, and the correlation of outcomes within a radiology facility.
Figure 2.
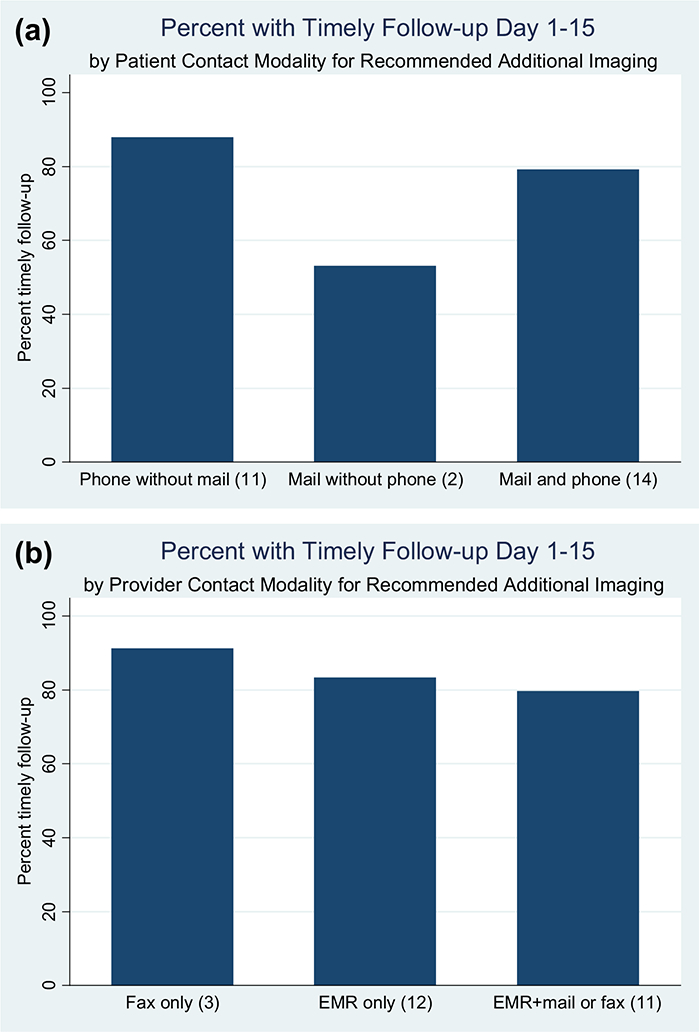
(a) Percentage with timely follow-up within days 1–15 by patient contact modality. The percentage of patients with timely follow-up within 1–15 days is shown after a screening mammogram assessed an incomplete BI-RADS 0 by facility type of communication with the patient. Facilities are classified by mail or phone communication to illustrate findings of the multivariate model. Additional methods (patient portal, in person) may also have been used. One facility using neither mail nor phone is not depicted. The number of facilities using that combination of mail or phone communication modality is given in parentheses. (b) Percentage with timely follow-up within days 1–15 by provider contact modality. The percentage of patients with timely follow-up within 1–15 days is shown after a screening mammogram assessed an incomplete BI-RADS 0 by facility type of communication with the health-care provider. Facilities are classified by fax only, electronic medical record only, or electronic medical record + fax or mail to further illustrate findings of the multivariate model. One facility using phone only and one facility reporting no routine communication with the provider in this scenario are not depicted. The number of facilities using that provider mode of communication is given in parentheses. BI-RADS, Breast Imaging Reporting and Data Systems.
In the scenario of patient misses a scheduled appointment for additional imaging, facilities that used conventional mail to communicate results to patients maintained higher rates of timely follow-up in the multivariate model. However, facilities that used written communication through the patient portal did not (Table 5, model C). Of note, only one facility used the patient portal in this scenario and that facility also used conventional mail. Modes of provider communication in this scenario that were statistically significant in bivariate analysis were limited to the phone (Table 3), so a multivariate model was not fit. In the sensitivity analysis, the results of these models did not vary when adjusting for derived income and income was not a significant predictor of the timely follow-up.
Sensitivity Analysis
We conducted a sensitivity analysis to evaluate whether a 30-day window for timely follow-up would lead to different results compared to our 15-day definition. If day 0 follow-ups are excluded, then 82.4% of the remaining examinations have follow-ups within 15 days and 93.9% have follow-ups within 30 days. Results for the patient communication variables in the scenario additional imaging recommended that were significantly associated with timely follow-up in the baseline analysis (Table 5) remained significant and were of similar direction and magnitude. In that scenario, the provider communication variables showed a reduced effect with no significant provider communication variables. For the scenario of patient misses a scheduled appointment for additional imaging, patient phone communication became statistically significant and positively associated with timely follow-up, and patient mail communication remained statistically significant and positively associated with timely follow-up. As in the baseline analysis, the use of the patient portal for communication was not associated with timely follow-up. In summary, using the 30-day compared to the 15-day window did not change the primary findings of the study.
DISCUSSION
Our study is the first to assess communication practices at the radiology facility level and its relationship to timely follow-up. In a multilevel analysis, we evaluated facility-level standard practices regarding modes of communication routinely used when additional imaging is recommended or the patient misses her appointment for additional imaging. For both scenarios, verbal communication by phone (patient in one scenario and provider in the other) was associated with timely follow-up. In contrast, our results suggest that written communication through the EMR may be negatively associated with timely follow-up.
Our study and others report that common modes of communication used for patient and provider communication of mammography results include verbal (telephone and in person) and written (mail, EMR, patient portal, and fax) (14). However, the use of written reports (mail or EMR) has limitations. Mammography reports may not be written using principles of clear communication and plain language (21), and patients whose primary language is other than English face an additional barrier to understanding the mammography report (21–24).
Verbal communication, by phone or in person, offers an opportunity for discussion and interaction and in some studies has been preferred by women (25) and associated with a higher likelihood of follow-up (23,26,27). In addition to patients with low English proficiency, there are additional system barriers to in-person verbal communication for mammography screening. These system barriers include the time and space required for consultations, proper training for facility staff in communication, and the practice of batch reading of screening mammograms at a later time (28,29). Batch reading has the advantage of decreasing interruptions and distractions during interpretation and has been associated with decreased recall rates without difference in cancer detection rates (30–32). A study that surveyed 257 radiologists associated with the Breast Cancer Surveillance Consortium found that fewer than 6% report routinely verbally communicating in person or on the phone with women when their screening mammograms were either normal or abnormal (33). However, in our study, verbal communication by telephone to both patient and provider were associated with timely follow-up.
Telephone communication regarding mammography results is a common modality used by radiology facilities for abnormal mammograms. A national survey of 228 mammography centers reports that 59.2% communicate results of a BI-RADS 0 by telephone, a finding comparable to the results of the current study (14). However, telephone communication also has limitations, including frequent changes in telephone numbers and the need for translators for patients who do not use English as their primary language. In the national survey of 228 mammography centers, 85% of facilities had multilingual staff or medical interpreters available to answer patient questions (14). A previous study of 970 women of diverse race and ethnicity found that notification of an abnormal mammogram by letter or telephone compared to in-person communication was associated with delay in diagnosis; other patient factors associated with delay in diagnosis in that study were black race, lower income, and limited understanding of the meaning of an abnormal mammogram (27). Telephone follow-up also requires resources. For example, one of the radiology facilities in the study with an annual volume of at least 23,000 screening mammograms estimates that it takes more than 60% of a full-time mammography liaison position for this activity, an effort that could be invested in other patient-centered activities. Evidence that verbal communication by phone improves follow-up can help justify this use of resources.
We were surprised to find that routine use of the EMR to communicate results of mammograms to providers was associated with less timely follow-up for BI-RADS 0. EMRs have the ability to alert physicians when reports are added to patient records. However, not all facilities use this feature for mammography reports. Meaningful use of the EMR and the patient portal holds promise for improved coordination of care through the mammography screening process (34). Our finding, however, suggests that the EMR was not being used effectively for this purpose. Excessive use of physician alerts with inability of physicians to acknowledge and act on alerts consistently is a barrier to applicable use of the EMR (35–37). Timely follow-up after screening mammograms was more likely when verbal communication occurs between the provider and the radiologist (38).
Our study design used a multilevel analysis to evaluate timely follow-up of incomplete BI-RADS 0 assessment. Previous studies establish the importance of a multilevel approach to understanding predictors of timely follow-up of abnormal screening tests. In a study of women in the United States undergoing mammography screening, hospital-based screening was associated with longer follow-up times when additional imaging was recommended and significant variation between facilities in follow-up by 15 days, and the median time to follow-up imaging care was 14 days (39). A prior PROSPR network study of women aged 40–75 with an abnormal mammogram (BI-RADs 0, 4, or 5) found that, compared to white women, black women are less likely to undergo timely follow-up and Hispanic women are more likely to undergo timely follow-up (defined by additional imaging or biopsy within 3 months) (40). In a retrospective cohort study of women at mammography facilities participating in the San Francisco Mammography Registry, facilities serving higher proportions of non–English speaking patients had longer delays to follow-up in comparison to those with lower proportions of non–English speaking patients (22).
Our study adds to existing literature supporting a relationship of communication factors to timely follow-up of abnormal screening mammograms. In a study of 184 black women who had an abnormal screening mammogram, two communication factors were associated with resolution of abnormal findings by 3 months: (1) asking questions during the screening mammogram and (2) receiving next-step information at the time of the screening mammogram (12). In a second study of 181 women with an abnormal mammogram requiring short-term follow-up imaging, a multivariate analysis controlling for patient-level and communication factors found that women whose physicians documented the follow-up plan in the medical record or women who reported being told that follow-up was needed were independently more likely to undergo appropriate follow-up (26).
The present study has limitations. Facility communication practice was collected by self-report and in the year after the cancer screening episodes observed in the study. Despite representing facility policy, the stated communication practices may not be uniformly implemented at the facility and communication practices could have changed over time. The study was cross-sectional, limiting any inferences of causality. Facilities may have other factors, such as limited appointments, that may influence timely follow-up. Our study did not systematically collect data on availability of appointments for follow-up diagnostic testing. Some facilities leave spots open on their daily schedule for follow-up testing with the number of spots based upon the facility’s call-back rate, but this practice is likely to vary across facilities. For patients requiring both ultrasound and mammogram, scheduling may be more complex and may lead to a greater delay. Our findings reflect practices across health-care settings located in the Northeast of the United States and may not be generalizable to the rest of the United States or other countries. We used a definition of timely follow-up of 15 days from the time of the screening mammogram to the first follow-up diagnostic assessment—a time frame that aligned with the median time to further diagnostic studies in our study cohort. Although variation exists, 15 days is consistent with guidelines in many countries. European guidelines directed by expert opinion have developed quality goals of knowing results of screening within 10 working days and being offered a further assessment if needed within an additional 5 working days (16). Guidelines in the countries of New Zealand, Australia, Canada, and the United Kingdom set quality goals of being offered a follow-up assessment between 15 days of a mammogram (United Kingdom) and 5 weeks (Canada) (17–20). The Food and Drug Administration, through the MQSA, recommends that facilities communicate this to the patient as soon as possible to avoid delays in patient workup. To evaluate the robustness of the 15-day definition for timely follow-up, we conducted a sensitivity analysis using a definition of within 30 days. We found that our primary findings persisted. The strengths of the study include the diversity of the patient population, prospective collection of screening episode data, and the ability to link facility-level data with patient outcomes.
CONCLUSIONS
In conclusion, we report variation in mammography facility communication practices and the association of communication modalities with timely follow-up of screening mammograms interpreted as BI-RADS 0. Communication by the facility to ordering providers and patients provides critical links in an effective cancer screening episode. In contrast to patient-level communication interventions, few studies have been designed to improve guideline-adherent screening by targeting system-level communication strategies (41). Communication practices are an essential factor in a system-level approach to appropriate and timely follow-up of screening mammograms.
Footnotes
APPENDIX. SUPPLEMENTARY DATA
Supplementary data related to this article can be found at https://doi.org/10.1016/j.acra.2017.12.028.
REFERENCES
- 1.Siu AL, Force USPST. Screening for breast cancer: U.S. preventive services task force recommendation statement. Ann Intern Med 2016; 164:279–296. [DOI] [PubMed] [Google Scholar]
- 2.Zapka JG, Taplin SH, Solberg LI, et al. A framework for improving the quality of cancer care: the case of breast and cervical cancer screening. Cancer Epidemiol Biomarkers Prev 2003; 12:4–13. [PubMed] [Google Scholar]
- 3.Beaber EF, Kim JJ, Schapira MM, et al. Unifying screening processes within the PROSPR consortium: a conceptual model for breast, cervical, and colorectal cancer screening. J Natl Cancer Inst 2015; 107:djv120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Onega T, Beaber EF, Sprague BL, et al. Breast cancer screening in an era of personalized regimens: a conceptual model and National Cancer Institute initiative for risk-based and preference-based approaches at a population level. Cancer 2014; 120:2955–2964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rudin RS, Bates DW . Let the left hand know what the right is doing: a vision for care coordination and electronic health records. J Am Med Inf Assoc 2014; 21:13–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tosteson AN, Fryback DG, Hammond CS, et al. Consequences of false-positive screening mammograms. JAMA Intern Med 2014; 174:954–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elmore JG, Nakano CY, Linden HM, et al. Racial inequities in the timing of breast cancer detection, diagnosis, and initiation of treatment. Med Care 2005; 43:141–148. [DOI] [PubMed] [Google Scholar]
- 8.Wujcik D, Shyr Y, Li M, et al. Delay in diagnostic testing after abnormal mammography in low-income women. Oncol Nurs Forum 2009; 36:709–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Press R, Carrasquillo O, Sciacca RR, et al. Racial/ethnic disparities in time to follow-up after an abnormal mammogram. J Womens Health 2008; 17:923–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ashing-Giwa KT, Gonzalez P, Lim JW, et al. Diagnostic and therapeutic delays among a multiethnic sample of breast and cervical cancer survivors. Cancer 2010; 116:3195–3204. [DOI] [PubMed] [Google Scholar]
- 11.Molina Y, Beresford SAA, Hayes Constant T, et al. Conversations about abnormal mammograms on distress and timely follow-up across ethnicity. J Cancer Educ 2017; 32:320–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kerner JF, Yedidia M, Padgett D, et al. Realizing the promise of breast cancer screening: clinical follow-up after abnormal screening among Black women. Prev Med 2003; 37:92–101. [DOI] [PubMed] [Google Scholar]
- 13.Poon EG, Haas JS, Louise Puopolo A, et al. Communication factors in the follow-up of abnormal mammograms. J Gen Intern Med 2004; 19:316–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marcus EN, Koru-Sengul T, Miao F, et al. How do breast imaging centers communicate results to women with limited English proficiency and other barriers to care? J Immigr Minor Health 2014; 16:401–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.What constitutes an acceptable system for notifying patients of examination results. 2017. Available at: https://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActandProgram/Guidance/PolicyGuidanceHelpSystem/ucm135579.htm. U.S. Department of Health and Human Services: U.S. Food & Drug Administration. Accessed December 14, 2017.
- 16.Perry N, Broeders M, de Wolf C, et al. European guidelines for quality assurance in breast cancer screening and diagnosis. Fourth edition—summary document. Ann Oncol 2008; 19:614–622. [DOI] [PubMed] [Google Scholar]
- 17.Ministry of Health. 2013. BreastScreen Aotearoa National Policy and Quality Standards Wellington: Ministry of Health. Published in December 2013 (revised December 2016) by the Ministry of Health, PO Box 5013, Wellington 6145, New Zealand: ISBN 978–0-478–41584-1. [Google Scholar]
- 18.Breast screening: Consolidated programme standards. PHE Publications gateway number: 2016720 PDF, 492KB. Updated 15 August 2017. [Google Scholar]
- 19.Report from the evaluation indicators working group Guidelines for monitoring breast cancer screening program performance. Third Edition Canadian partnership against cancer; 2013. [Google Scholar]
- 20.BreastScreen Australia: A joint Australian State and Territory Government Program Breastscreen Australia National Accreditation Handbook. March 2015. Endorsed by the Standard Committee on Screening 12 March 2015 Updated under the asupices of the BreastScreen Australia Accreditation Review Committee 21 September 2017. [Google Scholar]
- 21.Marcus EN, Sanders LM, Pereyra M, et al. Mammography result notification letters: are they easy to read and understand? J Womens Health (Larchmt) 2011; 20:545–551. [DOI] [PubMed] [Google Scholar]
- 22.Karliner LS, Ma L, Hofmann M, et al. Language barriers, location of care, and delays in follow-up of abnormal mammograms. Med Care 2012; 50:171–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Allen JD, Shelton RC, Harden E, et al. Follow-up of abnormal screening mammograms among low-income ethnically diverse women: findings from a qualitative study. Patient Educ Couns 2008; 72:283–292. [DOI] [PubMed] [Google Scholar]
- 24.Molina Y, Hohl SD, Ko LK, et al. Understanding the patient-provider communication needs and experiences of latina and non-latina white women following an abnormal mammogram. J Cancer Educ 2014; 29:781–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marcus EN, Drummond D, Dietz N. Urban women’s preferences for learning of their mammogram result: a qualitative study. J Cancer Educ 2012; 27:156–164. [DOI] [PubMed] [Google Scholar]
- 26.Poon EG, Haas JS, Puopolo AL, et al. Communication factors in the follow-up of abnormal mammograms. J Gen Intern Med 2004; 19:316–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perez-Stable EJ, Afable-Munsuz A, Kaplan CP, et al. Factors influencing time to diagnosis after abnormal mammography in diverse women. J Womens Health (Larchmt) 2013; 22:159–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wujcik D, Fair AM. Barriers to diagnostic resolution after abnormal mammography: a review of the literature. Cancer Nurs 2008; 31:E16–E30. [DOI] [PubMed] [Google Scholar]
- 29.Sasson JP, Zand T, Lown BA. Communication in the diagnostic mammography suite: implications for practice and training. Acad Radiol 2008; 15:417–424. [DOI] [PubMed] [Google Scholar]
- 30.Stewart KA, Neumann PJ, Fletcher SW, et al. The effect of immediate reading of screening mammograms on medical care utilization and costs after false-positive mammograms. Health Serv Res 2007; 42:1464–1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burnside ES, Park JM, Fine JP, et al. The use of batch reading to improve the performance of screening mammography. AJR Am J Roentgenol 2005; 185:790–796. [DOI] [PubMed] [Google Scholar]
- 32.Ghate SV, Soo MS, Baker JA, et al. Comparison of recall and cancer detection rates for immediate versus batch interpretation of screening mammograms. Radiology 2005; 235:31–35. [DOI] [PubMed] [Google Scholar]
- 33.Carney PA, Kettler M, Cook AJ, et al. An assessment of the likelihood, frequency, and content of verbal communication between radiologists and women receiving screening and diagnostic mammography. Acad Radiol 2009; 16:1056–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Neuner J, Fedders M, Caravella M, et al. Meaningful use and the patient portal: patient enrollment, use, and satisfaction with patient portals at a later-adopting center. Am J Med Qual 2015; 30:105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ip IK, Lacson R, Hentel K, et al. JOURNAL CLUB: predictors of provider response to clinical decision support: lessons learned from the Medicare imaging demonstration. AJR Am J Roentgenol 2017; 208:351–357. [DOI] [PubMed] [Google Scholar]
- 36.Gregory ME, Russo E, Singh H. Electronic health record alert-related workload as a predictor of burnout in primary care providers. Appl Clin Inform 2017; 8:686–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ancker JS, Edwards A, Nosal S, et al. Effects of workload, work complexity, and repeated alerts on alert fatigue in a clinical decision support system. BMC Med Inform Decis Mak 2017; 17:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Singh H, Thomas EJ, Mani S, et al. Timely follow-up of abnormal diagnostic imaging test results in an outpatient setting are electronic medical records achieving their potential? Arch Intern Med 2009; 169:1578–1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosenberg RD, Haneuse SJ, Geller BM, et al. Timeliness of follow-up after abnormal screening mammogram: variability of facilities. Radiology 2011; 261:404–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCarthy AM, Kim JJ, Beaber EF, et al. Follow-up of abnormal breast and colorectal cancer screening by race/ethnicity. Am J Prev Med 2016; 51:507–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Anhang Price R, Zapka J, Edwards H, et al. Organizational factors and the cancer screening process. J Natl Cancer Inst Monogr 2010; 2010:38–57. [DOI] [PMC free article] [PubMed] [Google Scholar]


