Abstract
Introduction:
Prior studies have found that women with disabilities are less likely to receive adequate prenatal care than women without disabilities. However, little is known about differences in patterns of prenatal care by type of disability. Therefore, this study examined timing and frequency of prenatal care among women with physical, sensory, or intellectual/developmental disabilities compared with women without disabilities.
Methods:
This was a retrospective cohort study using linked maternal and infant hospital discharge and birth certificate data for all births in California in 2000–2012 (N=6,745,201). Analyses were conducted in 2017–2018. Modified Poisson regression analyses compared women with each type of disability with women without disabilities on trimester of prenatal care initiation and number of prenatal care visits.
Results:
Women with intellectual/developmental disabilities or with limited hearing had significantly higher RR of delaying prenatal care initiation until the second or third trimester (intellectual/developmental disabilities: adjusted RR=1.21, 95% CI=1.09, 1.33; hearing: adjusted RR=1.11, 95% CI=1.02, 1.21), whereas women with physical disabilities and limited vision had lower risk of delaying care (physical: adjusted RR=0.91, 95% CI=0.88, 0.94; vision: adjusted RR=0.85, 95% CI=0.73, 0.99). Women with limited hearing or vision or intellectual/developmental disabilities had higher risk of receiving fewer prenatal visits than recommended, compared with women without disabilities. Women with physical disabilities or intellectual/developmental disabilities had higher RR of receiving more than the typical number of visits.
Conclusions:
There were key differences in prenatal care utilization by disability type, reflective of particularly pronounced disparities for women with intellectual/developmental disabilities and women with limited hearing. Delays in receipt of prenatal care and low numbers of prenatal care visits may contribute to the poorer birth outcomes that have been observed previously in these groups. Targeted interventions are needed to improve uptake of prenatal care in these vulnerable populations.
INTRODUCTION
Several recent studies have reported poorer birth outcomes for women with disabilities compared with their counterparts without disabilities. Adverse outcomes include higher proportions of preterm births, low birthweight infants, and stillbirths.1–11 Women with disabilities are also substantially more likely to deliver by cesarean, with the medical necessity of cesarean delivery not always clear.3,4,10–14 In addition, women with disabilities are more likely to experience pregnancy complications, such as gestational diabetes and preeclampsia.2,5,8–11,13 The reasons for these adverse outcomes among women with disabilities are not fully understood. They may be due in part to underlying medical conditions contributing to disability or to aspects of the life circumstances of women with disabilities (e.g., accumulated stress associated with marginalization) that are difficult to fully control for in regression models.11
Delayed or insufficient prenatal care may also contribute to disparities in outcomes for women with disabilities. Multiple studies in the general obstetric population have found that inadequate prenatal care is significantly associated with preterm birth, low birthweight, and infants that are small for gestational age.15–20 Prior studies of women with disabilities overall and women with intellectual and developmental disabilities (IDD) specifically have found that these groups are less likely to receive timely and adequate prenatal care compared with women without disabilities.3,7,8 However, little is known about how patterns of prenatal care differ by functional category of disability (physical, vision, hearing, and intellectual/developmental) in comparison with women without disabilities. A better understanding of prenatal care utilization patterns among subgroups of women with different types of disabilities is needed in order to effectively target interventions to improve care for these women.
The purpose of this study is to examine and describe the timing and frequency of prenatal care among women with physical, or sensory disabilities, or IDD compared with women without disabilities. It is hypothesized that women with IDD are the group least likely to initiate prenatal care during the first trimester and the group least likely to receive the recommended number of prenatal care visits.
METHODS
Study Sample
The study design was a retrospective cohort study using linked maternal and infant hospital discharge and vital records data (birth certificates and death files) for all births in California between 2000 and 2012 (N=6,745,201).21 This study was approved by the California Office of Statewide Health Planning and Development, and the IRB of Oregon Health & Science University. Analyses were conducted in 2017–2018.
Measures
Multiple gestations (identified from the birth certificate, n=178,135) and births to women with chronic hypertension (identified either from the birth certificate or from ICD-9 codes 410.0, 642.0–642.2, n=70,979) or pregestational diabetes (identified from ICD-9 code 250, n=43,075) were excluded, as these pregnancies are likely to require more than standard prenatal care. The final analytic sample included 6,453,012 births.
Dependent variables were timing of prenatal care initiation and number of prenatal care visits. Prenatal care initiation was measured as the month of pregnancy in which prenatal care was initiated, determined from the birth certificate. Initiation was then grouped by trimester of pregnancy (months 1–3, 4–6, and 7–9). Number of prenatal care visits was recorded on the birth certificate. For this study, numbers were grouped according to whether women received the typically recommended 11–14 visits,22 less than that number (zero to ten visits), somewhat more than that number (15–20 visits), or substantially more than that number (≥21 visits).
The key independent variable was disability status and type, which was identified using the ICD-9-CM diagnosis and procedure codes from the mother’s discharge file. Disability was classified as either present or absent, and (when present) into subgroups of physical, or hearing, or vision disabilities, or IDD using the coding scheme published by Darney and colleagues14 (Appendix 1, as well as alternate versions in Appendix 2). An individual woman could be in more than one disability group if she had multiple disability codes recorded on her discharge record.
Sociodemographic covariates included maternal race/ethnicity (non-Hispanic white as referent, non-Hispanic black, Hispanic, non-Hispanic Asian, non-Hispanic other), maternal education (completion of high school/GED and aged ≥16 years as the referent), advanced maternal age (<35 years at birth as referent), insurance status (public insurance as referent, private insurance, none), and parity (nulliparous versus multiparous). Other covariates included maternal comorbidities: gestational hypertension/preeclampsia (ICD-9 codes 642.3–642.5), gestational diabetes (ICD-9 codes 648.0, 648.8), and mental health diagnosis as identified by ICD-9 codes 295–298, 300, or 311.14 Year of delivery was included as a categorical variable (2012 as referent). Additionally, gestational age (in weeks) was included as a covariate in analyses of number of prenatal care visits.
Statistical Analyses
Chi-square tests compared the characteristics of mothers with and without disabilities. Multivariable modified Poisson regressions with robust variance estimation were used to examine both trimester of prenatal care initiation and number of prenatal care visits while adjusting for covariates. The regression model examining initiation of prenatal care calculated the RR of women in each disability group (compared with those without disabilities) delaying care until the second or third trimester instead of initiating care in the first trimester (reference level). In the regression models of number of prenatal visits, the typically recommended number of visits (11–14) was the reference level. Two analyses were conducted to calculate the RR of women with disabilities having: (1) fewer visits than recommended (zero to ten vs 11–14) and (2) more than the typically recommended number of visits (≥15 vs 11–14). Analyses were clustered by woman to account for the possibility that more than one delivery per woman could be included in the dataset. Sensitivity analyses were also conducted with alternate methods of categorizing disability; details and results are presented in Appendix 2. All analyses were performed in Stata, version 14.2. Figure 1 was prepared in R, version 3.4.2.
RESULTS
Within the analytic sample, deliveries to women with disabilities comprised 0.52% (33,383/6,453,012). Compared with women without disabilities, higher proportions of women with disabilities were non-Hispanic white (40.9% vs 27.5%), high school graduates (78.1% vs 69.8%), aged ≥35 years (23.2% vs 16.8%), and nulliparous (44.3% vs 39.5%). Women with disabilities also had higher proportions of gestational hypertension/preeclampsia (7.8% vs 5.1%), gestational diabetes (8.5% vs 6.2%), and mental health diagnoses (7.4% vs 1.2%) than women without disabilities (p<0.001 for all; Table 1).
Table 1.
Demographic Characteristics of the Analytic Sample
| Characteristics | Cohort | Disability status | Disability type | ||||
|---|---|---|---|---|---|---|---|
| No disability | Any disability | Physical | Hearing | Vision | IDD | ||
| Total | 6,453,012 | 6,419,629 (99.48) | 33,383 (0.52) | 27,891 (0.43) | 2,790 (0.04) | 1,270 (0.02) | 1,670 (0.03) |
| Race/Ethnicity | |||||||
| White | 1,776,336 (27.53) | 1,762,668 (27.46) | 13,668 (40.94) | 11,844 (42.47) | 921 (33.01) | 415 (31.13) | 602 (36.05) |
| Black | 340,194 (5.27) | 337,724 (5.26) | 2,470 (7.40) | 2,009 (7.20) | 183 (6.56) | 126 (9.45) | 191 (11.44) |
| Hispanic | 3,464,500 (53.69) | 3,450,659 (53.75) | 13,841 (41.46) | 11,306 (40.54) | 1,330 (47.67) | 589 (44.19) | 735 (44.01) |
| Asian | 706,393 (10.95) | 703,906 (10.96) | 2,487 (7.45) | 1,947 (6.98) | 295 (10.57) | 169 (12.68) | 100 (5.99) |
| Other | 128,948 (2.00) | 128,221 (2.00) | 727 (2.18) | 628 (2.25) | 45 (1.61) | 26 (1.95) | 31 (1.86) |
| Education, at least high school diploma/GED | 4,504,437 (69.80) | 4,478,373 (69.76) | 26,064 (78.08) | 22,032 (78.99) | 2,078 (74.48) | 1,030 (77.27) | 1,144 (68.50) |
| Insurance | |||||||
| Public | 3,089,174 (47.87) | 3,074,387 (47.89) | 14,787 (44.30) | 11,702 (41.96) | 1,598 (57.28) | 618 (46.36) | 1,065 (63.77) |
| Private | 3,224,192 (49.96) | 3,205,999 (50.66) | 18,193 (54.50) | 15,851 (56.83) | 1,165 (41.76) | 697 (52.29) | 583 (34.91) |
| None | 138,726 (2.15) | 138,324 (2.15) | 402 (1.20) | 337 (1.21) | 27 (0.97) | 18 (1.35) | 22 (1.32) |
| Advanced maternal age (≥35 years) | 1,085,849 (16.83) | 1,078,091 (16.79) | 7,758 (23.24) | 6,524 (23.39) | 619 (22.19) | 365 (27.38) | 310 (18.56) |
| Nulliparous | 2,548,932 (39.50) | 2,534,144 (39.47) | 14,788 (44.30) | 12,226 (43.83) | 1,182 (42.37) | 653 (48.99) | 895 (53.59) |
| Gestational hypertension/preeclampsia | 331,193 (5.13) | 328,602 (5.12) | 2,591 (7.76) | 2,015 (7.22) | 201 (7.20) | 237 (17.78) | 178 (10.66) |
| Gestational diabetes | 399,947 (6.20) | 397,109 (6.19) | 2,838 (8.50) | 2,331 (8.36) | 277 (9.93) | 121 (9.08) | 135 (8.08) |
| Mental health diagnosis | 81,441 (1.26) | 78,976 (1.23) | 2,465 (7.38) | 2,135 (7.65) | 131 (4.70) | 74 (5.55) | 152 (9.10) |
| Preterm birth | 566,072 (8.77) | 561,747 (8.75) | 4,325 (12.96) | 3,534 (12.67) | 319 (11.43) | 247 (18.53) | 282 (16.89) |
Notes: Boldface values are statistically significantly different from the no disability group at p<0.001. Data presented as n (%).
IDD, intellectual and developmental disabilities; GED, General Education Diploma (high school equivalency certificate).
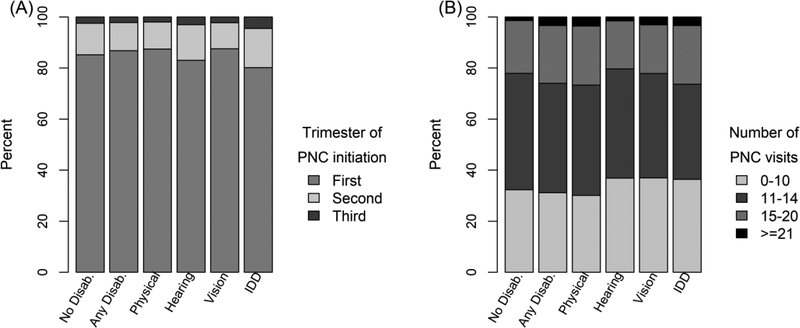
Overall, a slightly higher proportion of women with disabilities initiated prenatal care during the first trimester (86.7% vs 85.2% of women without disabilities, p<0.001). However, patterns of prenatal care initiation differed by disability type (Figure 1A). Women with physical disabilities or with limited vision had significantly higher proportions initiating prenatal care in the first trimester (87.4% and 87.6% respectively) compared with women without disabilities. Women with limited hearing or with IDD were significantly less likely to have initiated care during the first trimester (83.0% and 80.2% respectively). Further, women with IDD had the highest proportion (4.5%) with entry to care delayed until the third trimester (Figure 1A). Associations between disability and prenatal care initiation remained significant when adjusting for covariates. Women with limited hearing and with IDD had significantly higher adjusted risk of delaying care initiation until the second or third trimester, whereas women with physical disabilities or limited vision had significantly lower risk (Table 2).
Figure 1.
Trimester of prenatal care initiation and number of prenatal visits by presence and type of disability.
Note: Column labels refer to type of disability.
No Disab, no disability; Any Disab, any disability, IDD, intellectual and developmental disabilities.
Table 2.
Adjusted Risk Ratios (95% CIs)a for Prenatal Care Initiation and Frequency
| Dependent variable | Disability status | Disability type | ||||
|---|---|---|---|---|---|---|
| No disability (n=6,080,127) | Any disability (n=31,101) | Physical (n=26,084) | Hearing (n=2,550) | Vision (n=1,231) | IDD (n=1,499) | |
| Prenatal care initiation | ||||||
| Second/third vs first (ref) (n=6,111,228) | ref | 0.94 (0.91, 0.97) | 0.91 (0.88, 0.94) | 1.11 (1.02, 1.21) | 0.85 (0.73, 0.99) | 1.21 (1.09, 1.33) |
| Number of visits | ||||||
| Few/none (0–10) vs recommended (11–14, ref) (n=4,589,666)b | ref | 1.02 (1.00, 1.03) | 1.00 (0.99, 1.02) | 1.12 (1.07, 1.17) | 1.08 (1.01, 1.16) | 1.08 (1.01, 1.15) |
| Excess (≥15) vs recommended (ref) (n=4,009,424)c | ref | 1.13 (1.11, 1.15) | 1.14 (1.12, 1.16) | 0.98 (0.91, 1.05) | 1.01 (0.92, 1.12) | 1.23 (1.14, 1.32) |
Notes: Boldface indicates statistical significance at p<0.05.
Adjusted for race, education, insurance, age, parity, gestational hypertension/preeclampsia, gestational diabetes, mental health diagnosis, and year. Number of visits also adjusted for gestational age.
Women with ≥15 visits were not included in this analysis.
Women with 0–10 visits were not included in this analysis.
IDD, intellectual and developmental disabilities.
Number of prenatal visits also differed by disability status and type. Among women with physical disabilities, higher proportions had 15–20 visits (23.1% vs 20.7% of women without disabilities) or ≥21 visits (3.5% vs 1.4%), whereas fewer had zero to ten visits (30.1% vs 32.4%). Conversely, women with hearing or vision disabilities were more likely to have zero to ten visits (36.9% for both) compared with women without disabilities. Women with IDD were overrepresented at both the upper and lower ends of the distribution of number of visits: 26.4% had ≥15 visits whereas 36.4% had zero to ten visits (Figure 1B). In adjusted regression models with the typically recommended number of visits (11–14) as the reference category, women with limited hearing or vision or IDD had greater risk of receiving fewer visits than recommended, compared with women without disabilities. Women with physical disabilities or IDD had higher RR of receiving more than the typical number of visits (Table 2).
DISCUSSION
Prior research has found that women with disabilities are less likely to receive prenatal care as early or often as recommended,3,7,8 but there has been limited information about how patterns may vary by type of disability. This study found key differences in prenatal care utilization patterns by disability type, reflective of particularly pronounced disparities for women with limited hearing and women with IDD. Although other research has found that women with IDD are less likely to receive adequate prenatal care compared with women without disabilities,7 the present study demonstrates that women with IDD not only are disadvantaged relative to women without disabilities, they also experience greater disparities than many other women with disabilities. When adjusting for covariates, significant disparities were apparent in both timing and frequency of prenatal care for women with IDD and women with limited hearing. Disparities on only one of these aspects of care were found for women with vision disabilities, and there was no evidence of late or insufficient care for women with physical disabilities.
Women with IDD were the group least likely to receive care during the first trimester and most likely to wait until the third trimester to initiate care. Delayed entry into prenatal care for women with IDD may be related to delayed recognition of pregnancy in this group.7 Women with IDD may be less attuned to signs of pregnancy, especially if pregnancies are unplanned.23
Unfortunately, women with IDD are also more likely to have modifiable risk factors for adverse pregnancy outcomes (e.g., smoking, obesity)4,7,24 and thus have a particular need for prompt care in order to have the healthiest pregnancies possible. These issues speak to the need for preconception care that assesses sexual activity and pregnancy desires of women with IDD and directly addresses pregnancy planning and appropriate preparations.
This study also builds on previous indications that women with IDD are overrepresented at both the low and the high end of the prenatal care utilization spectrum.7 In the main analyses, women with IDD were unique in having this pattern; the pattern was not apparent for women with other types of disabilities. In sensitivity analyses separating out women with multiple disabilities, these women with multiple disabilities exhibited this pattern instead (Appendix 2), suggesting that women with IDD who also have another type of disability are particularly likely to have either low or high numbers of visits. Women with IDD with fewer visits than recommended may constitute a particularly hard to reach subpopulation without well-established connections to healthcare systems or strong patient–physician relationships. Women with IDD who had more than the typical number of visits may have had risk factors other than the ones available as covariates in this dataset; such risk factors may have led their prenatal care providers to believe additional visits were warranted. Utilization of prenatal care among women with IDD may also be closely tied to the level of support women receive from family members or others in scheduling and getting to appointments.25
In contrast to women with IDD, women with physical disabilities were the group most likely to initiate care in the first trimester and also most likely to have an ample number of prenatal visits. Women with physical disabilities may anticipate difficulty accessing high quality prenatal care and be proactive in seeking out care settings and clinicians equipped to address their needs.26 Early and frequent receipt of prenatal care among women with physical disabilities may be because of maternal or physician concerns about potential pregnancy complications for these women.27 Although higher numbers of visits may be necessary, they may also be challenging and stressful for mothers with physical disabilities if clinics are not fully accessible. For example, transferring to an exam table that is not height adjustable may be difficult and potentially dangerous for a woman with a physical disability, particularly as pregnancy progresses. Adhering to standards for accessible facilities and equipment28–30 will help ensure safety and accessibility for patients across the full spectrum of physical abilities and body types.
Women with hearing disabilities had elevated risk of entering care late and of receiving fewer prenatal care visits than recommended. Low health literacy and substantial barriers in communicating with clinicians are common among people who are deaf or hard of hearing.31 Low health literacy may limit women’s understanding of the importance of timely and ongoing prenatal care. Additionally, women who need sign language interpreters may encounter challenges with obtaining interpreter services, which could result in delayed appointments and suboptimal care. Prior research has found that when language barriers are well-addressed (either with providers who sign or with full-time availability of interpreters), receipt of preventive care improves.32,33 Prenatal care could similarly be improved with routine provision of quality interpretation services, and with incorporation of educational videos in sign language. For women with vision-related disabilities, the elevated risk of receiving fewer prenatal visits than recommended despite initiating care on time raises questions as to whether communication barriers may interfere with optimal delivery of care for this group as well, as women may not be able to read written information about the recommended frequency of visits. Ensuring that key information is presented orally and that return appointments are scheduled at the end of each visit may help address such barriers.
Limitations
This study was limited to identifying women with disabilities based on diagnosis codes. This is an imperfect science, as the ICD-9 classification system does not provide a comprehensive approach to delineating functional status, and the degree of functional limitation associated with any given diagnosis may vary considerably.34 Furthermore, the dataset only included ICD-9 codes from the perinatal period and may therefore have missed relevant diagnoses from a woman’s prior medical history. The means of ascertaining disability likely resulted in identification of disabilities that were perceived as pertinent to clinical management of pregnancy and delivery. Results of this study may not be generalizable to less obvious or severe disabilities. The dataset also precluded identification of women with mental health diagnoses elsewhere in their medical histories if those diagnoses were not reflected in the hospital discharge record; thus, the analyses may have undercontrolled for the presence of mental health conditions.
Data for this study were not able to provide information about the quality of prenatal care, but only the quantity and timing of care. Qualitative research suggests that obstetricians and midwives have limited training and experience with disability and may not be prepared to provide care that addresses the needs and concerns of women with disabilities.35–37 It is also possible that prenatal care for women with disabilities may have improved since 2012, which was the most recent year of data available at the time this study was conducted. It would be relevant for future research to conduct similar analyses with newer data as they become available. An important strength of the present study is the size and inclusiveness of the dataset. California is the most populous state in the country and has one of the most diverse populations.38 These data are a complete census (rather than a sample) of births in California during the study period. Moreover, pooling multiple years of data yielded sufficient cell sizes to examine differences in patterns for women with different types of disabilities.
CONCLUSIONS
This study expands on existing literature by examining patterns of prenatal care receipt in relation to type of disability. The findings highlight the particularly pronounced disparities in care for women with IDD and women with limited hearing. Given the increased risk of adverse outcomes among women in both of these groups,1,2,4–7 the observed delays in receipt of prenatal care and low numbers of prenatal care visits for large proportions of these women are especially worrying. For women with IDD, the number of prenatal visits varied more than was the case in other disability groups, reflecting both underutilization and intensive utilization of prenatal care among women with IDD. Additional research is needed on predictors of low versus adequate or high utilization within this population in order to target interventions to women most at risk of not obtaining adequate prenatal care.
Supplementary Material
ACKNOWLEDGMENTS
The research reported here was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of NIH under Award Number R21HD081309 (Horner-Johnson, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH. Support for Dr. Horner-Johnson’s time was provided by grant number K12HS022981 from the Agency for Healthcare Research and Quality (Guise, PI).
No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Akobirshoev I, Parish SL, Mitra M, Rosenthal E. Birth outcomes among U.S. women with intellectual and developmental disabilities. Disabil Health J. 2017;10(3):406–412. 10.1016/j.dhjo.2017.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown H, Cobigo V, Lunsky Y, Vigod S. Maternal and offspring outcomes in women with intellectual and developmental disabilities: a population-based cohort study. BJOG. 2017;124(5):757–765. 10.1111/1471-0528.14120. [DOI] [PubMed] [Google Scholar]
- 3.Gavin NI, Benedict MB, Adams EK. Health service use and outcomes among disabled Medicaid pregnant women. Womens Health Issues. 2006;16(6):313–322. 10.1016/j.whi.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 4.Hoglund B, Lindgren P, Larsson M. Pregnancy and birth outcomes of women with intellectual disability in Sweden: a national register study. Acta Obstet Gynecol Scand. 2012;91(12):1381–1387. 10.1111/j.1600-0412.2012.01509.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McConnell D, Mayes R, Llewellyn G. Women with intellectual disability at risk of adverse pregnancy and birth outcomes. J Intellect Disabil Res. 2008;52(pt 6):529–535. 10.1111/j.1365-2788.2008.01061.x. [DOI] [PubMed] [Google Scholar]
- 6.Mitra M, Akobirshoev I, McKee MM, Iezzoni LI. Birth outcomes among U.S. women with hearing loss. Am J Prev Med. 2016;51(6):865–873. 10.1016/j.amepre.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitra M, Parish SL, Clements KM, Cui X, Diop H. Pregnancy outcomes among women with intellectual and developmental disabilities. Am J Prev Med. 2015;48(3):300–308. 10.1016/j.amepre.2014.09.032. [DOI] [PubMed] [Google Scholar]
- 8.Mitra M, Clements KM, Zhang J, Iezzoni LI, Smeltzer SC, Long-Bellil LM. Maternal characteristics, pregnancy complications, and adverse birth outcomes among women with disabilities. Med Care. 2015;53(12):1027–1032. 10.1097/MLR.0000000000000427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morton C, Le JT, Shahbandar L, Hammond C, Murphy EA, Kirschner KL. Pregnancy outcomes of women with physical disabilities: a matched cohort study. PM R. 2013;5(2):90–98. 10.1016/j.pmrj.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 10.Parish SL, Mitra M, Son E, Bonardi A, Swoboda PT, Igdalsky L. Pregnancy outcomes among U.S. women with intellectual and developmental disabilities. Am J Intellect Dev Disabil. 2015;120(5):433–443. 10.1352/1944-7558-120.5.433. [DOI] [PubMed] [Google Scholar]
- 11.Signore C, Spong CY, Krotoski D, Shinowara NL, Blackwell SC. Pregnancy in women with physical disabilities. Obstet Gynecol. 2011;117(4):935–947. 10.1097/AOG.0b013e3182118d59. [DOI] [PubMed] [Google Scholar]
- 12.Biel FM, Horner-Johnson W, Darney BG, Caughey AB. Time trends in, and medical indications for, primary cesarean delivery among women with and without disabilities American Public Health Association Annual Meeting; 2016; Denver, CO. [Google Scholar]
- 13.Brown HK, Kirkham YA, Cobigo V, Lunsky Y, Vigod SN. Labour and delivery interventions in women with intellectual and developmental disabilities: a population-based cohort study. J Epidemiol Community Health. 2016;70(3):238–244. 10.1136/jech-2015-206426. [DOI] [PubMed] [Google Scholar]
- 14.Darney BG, Biel FM, Quigley BP, Caughey AB, Horner-Johnson W. Primary cesarean delivery patterns among women with physical, sensory, or intellectual disabilities. Womens Health Issues. 2017;27(3):336–344. 10.1016/j.whi.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barros H, Tavares M, Rodrigues T. Role of prenatal care in preterm birth and low birthweight in Portugal. J Public Health Med. 1996;18(3):321–328. 10.1093/oxfordjournals.pubmed.a024513. [DOI] [PubMed] [Google Scholar]
- 16.Carvahlo Padilha CD, Accioly E, Chagas C, Portela E, DaSilva CL, Saunders C. Birth weight variations according to maternal characteristics and gestational weight gain in Brazilian women. Nutricio Hospitalaria. 2009;24:207–212. [PubMed] [Google Scholar]
- 17.Cox RG, Zhang L, Zotti ME, Graham J. Prenatal care utilization in Mississippi: racial disparities and implications for unfavorable birth outcomes. Matern Child Health J. 2011;15(7):931–942. 10.1007/s10995-009-0542-6. [DOI] [PubMed] [Google Scholar]
- 18.Heaman MI, Newburn-Cook CV, Green CG, Elliott LJ, Helewa ME. Inadequate prenatal care and its association with adverse pregnancy outcomes: a comparison of indices. BMC Pregnancy Childbirth. 2008;8:15 10.1186/1471-2393-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krueger PM, Scholl TO. Adequacy of prenatal care and pregnancy outcomes. J Am Osteopath Assoc. 2000;100(8):485–492. [PubMed] [Google Scholar]
- 20.Raatikainen K, Heiskanen N, Heinonen S. Under-attending free antenatal care is associated with adverse pregnancy outcomes. BMC Public Health. 2007;7:268 10.1186/1471-2458-7-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.California Office of Statewide Health Planning and Development. Types of OSHPD patient-level data. www.oshpd.ca.gov/HID/Data_Request_Center/Types_of_Data.html. Last updated April 2, 2018. Accessed October 15, 2018.
- 22.American Academy of Pediatrics, American College of Gynecologists. Guidelines for Perinatal Care, 7th Edition Washington, DC: American College of Obstetricians and Gynecologists; 2012. [Google Scholar]
- 23.Guastaferro K, Benka-Coker ML, Lutzker JR. A story of mothers wity intellectual and developmental disabilities In: Lutzker JR, Guastaferro K, Benka-Corker ML, eds. Maltreatment of People with Intellectual and Developmental Disabilities. Washington, DC: American Association on Intellectual and Developmental Disabilities; 2016:187–206. [Google Scholar]
- 24.Brown HK, Lunsky Y, Wilton AS, Cobigo V, Vigod SN. Pregnancy in women with intellectual and developmental disabilities. J Obstet Gynaecol Can. 2016;38(1):9–16. 10.1016/j.jogc.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 25.Potvin LA, Brown HK, Cobigo V. Social support received by women with intellectual and developmental disabilities during pregnancy and childbirth: an exploratory qualitative study. Midwifery. 2016;37:57–64. 10.1016/j.midw.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 26.Mitra M, Akobirshoev I, Moring NS, et al. Access to and satisfaction with prenatal care among pregnant women with physical disabilities: findings from a national survey. J Womens Health. 2017;26(12):1356–1363. 10.1089/jwh.2016.6297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tarasoff LA. Experiences of women with physical disabilities during the perinatal period: a review of the literature and recommendations to improve care. Health Care Women Int. 2015;36(1):88–107. 10.1080/07399332.2013.815756. [DOI] [PubMed] [Google Scholar]
- 28.2010 ADA Standards for Accessible Design. Washington, DC: Department of Justice, 2010. [Google Scholar]
- 29.Department of Justice, HHS. Access to Medical Care for Individuals with Mobility Disabilities. www.ada.gov/medcare_mobility_ta/medcare_ta.pdf Published 2010 Accessed October 15, 2018.
- 30.Architectural and Transportation Barriers Compliance Board (U.S. Access Board). Standards for accessible medical diagnostic equipment. Federal Register. 2017;82(5): 36. [PubMed] [Google Scholar]
- 31.Barnett S, McKee M, Smith SR, Pearson TA. Deaf sign language users, health inequities, and public health: opportunity for social justice. Prev Chronic Dis. 2011;8(2):A45 www.cdc.gov/pcd/issues/2011/mar/10_0065.htm. Accessed October 15, 2018. [PMC free article] [PubMed] [Google Scholar]
- 32.McKee MM, Barnett SL, Block RC, Pearson TA. Impact of communication on preventive services among Deaf American Sign Language users. Am J Prev Med. 2011;41(1):75–79. 10.1016/j.amepre.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McKinney TG, Walters D, Bird GL, Nattinger AB. Improvements in preventive care and communication for deaf patients: results of a novel primary health care program. J Gen Intern Med. 1995;10(3):133–137. 10.1007/BF02599667. [DOI] [PubMed] [Google Scholar]
- 34.Iezzoni LI. Multiple chronic conditions and disabilities: implications for health services research and data demands. Health Serv Res. 2010;45(5 pt 2):1523–1540. 10.1111/j.1475-6773.2010.01145.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Castell E, Stenfert Kroese B. Midwives experiences of caring for women with learning disabilities: a qualitative study. Midwifery. 2016;36:35–42. 10.1016/j.midw.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 36.Mitra M, Smith LD, Smeltzer SC, Long-Bellil LM, Sammet Moring N, Iezzoni LI. Barriers to providing maternity care to women with physical disabilities: perspectives from health care practitioners. Disabil Health J. 2017;10(3):445–450. 10.1016/j.dhjo.2016.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smeltzer SC, Mitra M, Long-Bellil L, Iezzoni LI, Smith LD. Obstetric clinicians’ experiences and educational preparation for caring for pregnant women with physical disabilities: a qualitative study. Disabil Health J. 2018;11(1):8–13. 10.1016/j.dhjo.2017.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johnson H California’s Population. www.ppic.org/content/pubs/jtf/JTF_PopulationJTF.pdf Published 2017 Accessed April 6, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.