Abstract.
Human protothecosis is a rare algal infection caused by Prototheca; it is a ubiquitous achlorophyllic alga, which rarely causes human disease. Currently, the pathogenesis remains unclear and no treatment options have been elucidated. We present a case of olecranon bursitis caused by Prototheca wickerhamii in an immunocompromised patient. A 45-year-old man presented with left elbow pain after scraping his elbow on a tree. He reported significant pain and swelling of the elbow after injury, which resolved without intervention. He was diagnosed with HIV/AIDS infection and started on antiretroviral therapy. Afterward, he experienced recurrent elbow swelling and pain; an incision and drainage was performed and cultures demonstrated P. wickerhamii. Unsuccessful treatment with oral voriconazole led to an attempt at therapy with parental amphotericin and oral doxycycline; however the patient left against medical advice. He presented to our facility and both parental amphotericin and doxycycline were initiated with planned outpatient bursectomy. He clinically improved on that regimen but left against medical advice before completing his recommended course of IV amphotericin and oral doxycycline. Patients diagnosed with disseminated protothecosis can have a mortality rate upward of 67%. Given the rarity of this pathogen, no official treatment guidelines exist and there are few studies analyzing the antimicrobial susceptibility of Prototheca. Management is challenging because of slow-growing nature of the algae, paucity of research studies, and limited susceptibility of this pathogen. This case adds to the limited body of literature by demonstrating the clinical presentation of protothecosis and highlighting the pathology and current treatment options.
INTRODUCTION
We present a case of protothecosis, a rare algae infection that more commonly infects the immunocompromised. It is an achlorophyllous algae of the genus Prototheca and was first documented to infect humans in 1964. Two species of the genus Prototheca are known to infect humans, including Prototheca wickerhamii and Prototheca zopfii. Clinical presentation is highly variable, but they can cause cutaneous disease, olecranon bursitis, or disseminated disease. Whereas disseminated disease occurs almost always in immunocompromised patients, olecranon bursitis is more prevalent in immunocompetent patients. Treatment is challenging because of the limited susceptibility, slow-growing nature of the algae, and paucity of studies. Although in vitro studies have shown susceptibility to a few antifungal medications, they have not been correlated to clinical response.1 In general, there are no solidified treatment guidelines and no randomized studies because of the inadequate number of cases. Therefore, we present our case to illustrate the need for guided treatment for this rare infection.
CASE DESCRIPTION
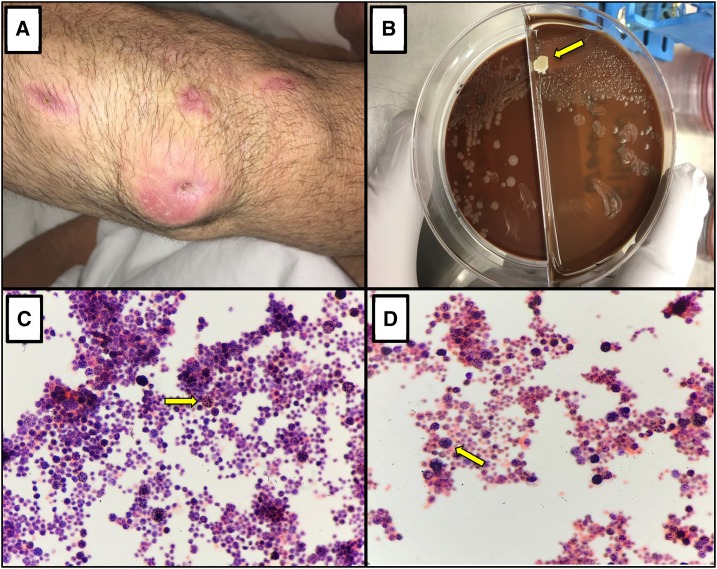
A 45-year-old Caucasian man presented to the emergency room with left elbow pain. Approximately 6 months before admission, the patient reported scraping his left elbow on a tree while doing yard work outside after a recent hurricane in the area. He had significant pain after this injury and reported swelling to the elbow for a few days, which resolved on its own after using ice and over-the-counter nonsteroidal anti-inflammatory drugs. Two months after this initial injury, the patient was ill and sought medical care at an outside hospital, where he was diagnosed with HIV/AIDS (CD4+: 1 cells/mm3; viral load: three million virion copies). He was started on emtricitabine, tenofovir-alafenamide, and dolutegravir along with dapsone for Pneumocystis prophylaxis at the local health department. Repeat HIV testing 2 months later revealed an undetectable viral load and CD4+ of 6 cells/mm3. Two months later, the patient had worsening pain and swelling of his left elbow which prompted him to return to the outside hospital for evaluation (Figure 1A). During this admission, his HIV viral load remained undetectable and CD4+ count was 50 cells/mm3. An incision and drainage was performed by surgery, and he was sent home with oral cephalexin. Preliminary cultures from the incision and drainage demonstrated a yeast, and they were sent to a laboratory in Virginia for further speciation (Figure 1B). Final speciation via matrix-assisted laser desorption/ionization mass spectrometry (MALDI-TOF) was determined to be P. wickerhamii, and the patient was started on oral voriconazole 200 mg twice daily as outpatient. The patient completed 5 days of oral voriconazole therapy but unfortunately continued to have worsening pain and swelling of the left elbow and returned to the outside hospital. He had a second incision and drainage with preliminary cultures showing same species. Parenteral amphotericin B was initiated, along with doxycycline 100 mg oral twice daily, as per Infectious Disease recommendations. The patient left against medical advice after starting his antibiotics at the outside hospital and presented to our facility for further treatment. At our facility, Infectious Disease was consulted, and it was noted that the outside laboratory records demonstrated P. wickerhamii sensitivity to amphotericin B, voriconazole, and micafungin. There was no concern for disseminated infection; however, given prior treatment failure with oral voriconazole, the patient was continued on doxycycline 100 mg oral twice daily along with IV liposomal amphotericin B. Surgery was consulted for left elbow bursectomy and recommended continuing antibiotics with consideration of bursectomy as an outpatient procedure. The patient clinically improved after 3 days on IV amphotericin and oral doxycycline; however, he left against medical advice before completing his antibiotic course. We recommended a 6-week total course of antibiotics because of the high risk of recurrence of infection and that a surgical bursectomy was not performed. The patient was also advised to continue following at health department for HIV management, treatment, and prophylaxis.
Figure 1.
(A) Patient’s arm with an erythematous and indurated bursa. Three other satellite lesions located beyond the region of the olecranon bursa are scars from previous incision and drainages. (B) Isolate of Prototheca wickerhamii on chocolate blood agar, showing a smooth white to cream colored colony. (C–D) Gram stain of P. wickerhamii isolate, demonstrating round to spheroid organisms of different sizes, consisting of multiple small endospores within the wall of the parent cell and in a morula configuration. Magnification ×1,000.
DISCUSSION
Human protothecosis is a rare algae infection with organisms of the Prototheca genus. This is the only algae known to cause human disease. These single-celled organisms (Figure 1C–D) are considered to be achlorophyllic algae and are fairly widespread in nature, located in all continents and especially in sewages and aquatic systems contaminated with animal wastes.2 The two species implicated in human infection thus far are P. wickerhamii and P. zopfii. Clinical presentation varies significantly; the exact pathogenesis of protothecosis in humans remains unclear. Three different clinical forms of protothecosis have been classified thus far: cutaneous, olecranon bursitis, and dissemination. These typically occur only in immunosuppressed individuals; however, olecranon bursitis can occur in immunocompetent individuals who have reported some type of penetrating trauma to the elbow.3 Skin lesions of cutaneous protothecosis can present with plaques, papules, vesicles, or ulcers; traumatic inoculation is by far the most common source of infection; however, inoculation from surgical procedures and insect bites have also been reported.4,5 Disseminated protothecosis only occurs in patients with significant immunosuppression. Most cases have described disseminated protothecosis affecting the gastrointestinal, pulmonary, and central nervous systems.6,7 Furthermore, disseminated disease was detected in patients with hematological malignancies such as leukemia or myelodysplastic syndrome.5 Olecranon bursitis occurs when the olecranon bursa becomes infected, often because of a penetrating injury. It is unclear why this particular area is at higher risk of developing localized protothecosis but may be explained by the increased likelihood of repeated trauma to that area. Patients develop erythema and tenderness over the area, and various amounts of serosanguinous fluid can be locally produced. As in most cases of protothecosis, symptoms are indolent and typically develop over multiple weeks following inoculation.3,4 In the case of our patient, it is likely that his recurrence of symptoms was due to immune reconstitution inflammatory syndrome; his elbow pain and swelling returned and worsened after he was started on appropriate antiretroviral therapy for his HIV/AIDS.
Not every type of immunosuppression predisposes patients to protothecosis. Specifically, neutrophils are known to play a critical role in defense against P. wickerhamii; patients with functional neutropenia are unable to properly protect themselves from protothecosis and are at a higher risk of dissemination. Interestingly, neutropenia in cancer patients does not seem to be a major risk factor,8 suggesting that qualitative factors of neutrophils play a bigger role than quantitative factors. Furthermore, patients with HIV/AIDS are also not at an increased risk of developing protothecosis; one case study found a patient with a CD4+ count of 38 cells/mm3 did not develop disseminated protothecosis, indicating that a different category of immunodeficiency is required for protothecosis dissemination.9
Few studies analyzing the susceptibility of Prototheca species are available. The most common anti-infective agents used previously have been antifungals and tetracyclines. A review of present literature suggests that intravenous liposomal amphotericin B has the highest success rate to treat all clinical types of protothecosis either alone (77%) or in combination with other agents such as tetracyclines (86%).6,10 Overall, treatment success rates are higher for cutaneous and olecranon bursitis (73% and 83%, respectively) compared with disseminated protothecosis (33%). Because of the paucity of susceptibility information of Prototheca species infection, it is recommended to perform susceptibility testing on these algae when identified as a source of infection. Finally, it should be stressed that in cases such as these—immunocompromised patients who have had an integumental penetration injury and also have been exposed to water/soil—that Prototheca species be included in the differential diagnosis.
REFERENCES
- 1.Lass-Flörl C, Mayr A, 2007. Human protothecosis. Clin Microbiol Rev 20: 230–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huerre M, Ravisse P, Solomon H, Ave P, Briquelet N, Maurin S, Wuscher N, 1993. Human protothecosis and environment. Bull Soc Pathol Exot 86: 484–488. [PubMed] [Google Scholar]
- 3.De Montclos M, Chatte G, Perrin-Fayolle M, Flandrois JP, 1995. Olecranon bursitis due to Prototheca wickerhamii, an algal opportunistic pathogen. Eur J Clin Microbiol Infect Dis 14: 561–562. [DOI] [PubMed] [Google Scholar]
- 4.Thiele D, Bergmann A, 2002. Protothecosis in human medicine. Int J Hyg Environ Health 204: 297–302. [DOI] [PubMed] [Google Scholar]
- 5.Mayorga J, Barba-Gomez JF, Verduzco-Martinez AP, Munoz-Estrada VF, Welsh O, 2012. Protothecosis. Clin Dermatol 30: 432–436. [DOI] [PubMed] [Google Scholar]
- 6.Todd JR, King JW, Oberle A, Matsumoto T, Odaka Y, Fowler M, Sanusi ID, 2012. Protothecosis: report of a case with 20-year follow-up, and review of previously published cases. Med Mycol 50: 673–689. [DOI] [PubMed] [Google Scholar]
- 7.Żak I, Jagielski T, Kwiatkowski S, Bielecki J, 2012. Prototheca wickerhamii as a cause of neuroinfection in a child with congenital hydrocephalus. First case of human protothecosis in Poland. Diagn Microbiol Infect Dis 74: 186–189. [DOI] [PubMed] [Google Scholar]
- 8.Torres HA, Bodey GP, Tarrand JJ, Kontoyiannis DP, 2003. Protothecosis in patients with cancer: case series and literature review. Clin Microbiol Infect 9: 786–792. [DOI] [PubMed] [Google Scholar]
- 9.Carey WP, Kaykova Y, Bandres JC, Sidhu GS, Bräu N, 1997. Cutaneous protothecosis in a patient with AIDS and a severe functional neutrophil defect: successful therapy with amphotericin B. Clin Infect Dis 25: 1265–1266. [DOI] [PubMed] [Google Scholar]
- 10.McMullan B, Pollett S, Biswas C, Packham D, 2016. Successful treatment of cutaneous protothecosis with liposomal amphotericin and oral itraconazole. Med Mycol Case Rep 12: 21–23. [DOI] [PMC free article] [PubMed] [Google Scholar]