Abstract
Background:
Primary care teams face daily time pressures both during patient encounters and outside of appointments.
Objectives:
We theorize two types of time pressure, and test hypotheses about organizational determinants and patient consequences of time pressure.
Research Design:
Cross-sectional, observational analysis of data from concurrent surveys of care team members and their patients.
Subjects:
Patients (n=1291 respondents, 73.5% response rate) with diabetes and/or coronary artery disease established with practice teams (n=353 respondents, 84% response rate) at 16 primary care sites, randomly selected from two Accountable Care Organizations.
Measures and Analysis:
We measured team member perceptions of two potentially distinct time pressure constructs: 1) encounter-level, from seven questions about likelihood that time pressure results in missing patient management opportunities, and 2) practice-level, using practice atmosphere rating from calm to chaotic. The Patient Assessment of Chronic Illness Care (PACIC-11) instrument measured patient-reported experience. Multivariate logistic regression models examined organizational predictors of each time pressure type, and hierarchical models examined time pressure predictors of patient-reported experiences.
Results:
Encounter-level and practice-level time pressure measures were not correlated, nor predicted by the same organizational variables, supporting the hypothesis of two distinct time pressure constructs. More encounter-level time pressure was most strongly associated with less health information technology capability (OR 0.33, p<0.01). Greater practice-level time pressure (chaos) was associated with lower PACIC-11 scores (OR 0.74, p<0.01).
Conclusions:
Different organizational factors are associated with each forms of time pressure. Potential consequences for patients are missed opportunities in patient care and inadequate chronic care support.
Introduction
Almost 450 million patient visits occur annually in U.S. primary care offices.(1) Primary care teams face daily time pressures as they address patient needs.(2,3) Time constraints occur both within a patient encounter,(4,5) and more globally in work outside of appointments.(6,7)
Time pressure can affect altruistic behaviors, dramatically demonstrated in a laboratory study on seminarians who when rushed were less likely to help a man requiring emergency care.(8) A meta-analysis of studies with similar manipulations to create time stress conditions (e.g., pressure from instructions to go faster) compared to no time pressure showed modest detrimental effects on performance.(9) Despite the salience of time stress in care delivery with attendant concerns about quality and patient safety, scant evidence exists about types of time stress, the organizational factors that shape such stressors in routine care settings, and consequences for patients and practitioners alike.
In response, we theorize two types of time stressors – encounter-level and practice-level time pressure. We test hypotheses about organizational determinants and patient consequences of each using survey data from 16 randomly selected primary care practices associated with two large Accountable Care Organizations (ACOs), and their adult patients with cardiovascular disease (CVD), diabetes, or both.(10)
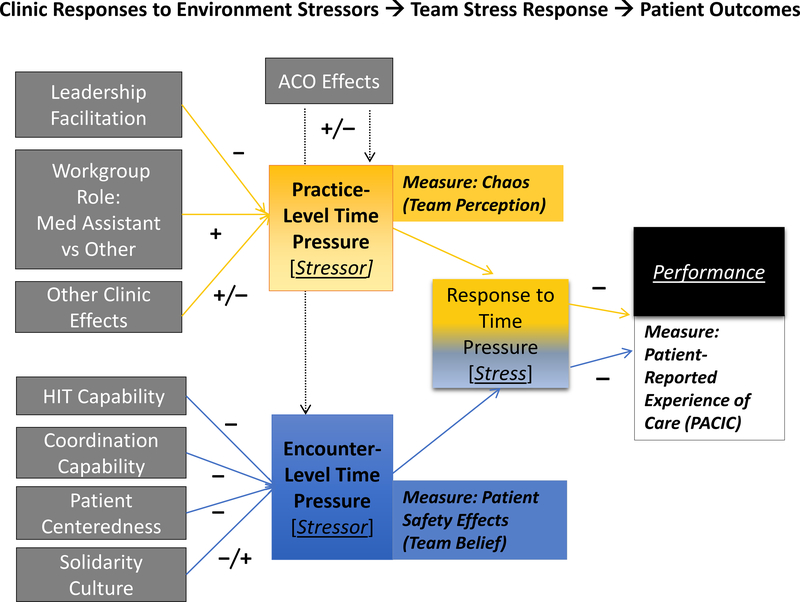
Theoretical Model of Time Stressors, Organizational Predictors and Patient Consequences
Organizational performance of a work team is affected, in part, by the way it handles stressors. Figure 1 depicts a theoretical relationship between stressor, stress response, and performance. (11) Corporate ACOs and their clinics, in responding to the external environment, have varying levels of time pressure stressors, which when experienced as stress by the clinic practice team, translate to performance hits. For example, new regulatory requirements related to quality metrics may increase documentation demands on clinics, increasing the time stress on practice teams. Clinic organizational level responses in terms of staffing models, leadership approach, and work processes may be more or less adaptive to such environmental pressures, resulting in varying stressor levels exerting force on the practice members.
Figure 1:
Stressor-Stress-Performance Theory Applied to Ambulatory Care. The diagram provides both the theoretical foundation for the study, and the linkages between theoretical concepts and the specific measures used to test hypotheses. The grey boxes show the organizational responses to environmental stressors that are hypothesized to influence time pressure stressors within appointments (encounter level, blue box) and in the clinic office (practice level, yellow box). Alongside each theoretical stressor concept is the related study measure (based on perceptions and beliefs of those in a clinic’s practice). In turn, the stress experienced from a time pressure stressor is posited to adversely affect the practice’s performance (black box) on any number of dimensions, including the patient-reported measure assessed in this study. Hypothesized positive (+) and negative (–) effects are shown for organizational determinants and patient consequences of each time pressure stressor.
We posit that specific clinic practice responses to the environment translate into two types of stressors related to time pressure: practice-level time pressure and encounter-level time pressure.(12,13) The stressor condition is similar to the weather – determined by both barometric pressure and temperature – in potentially different ways.
Greater time pressure resulting from activities outside of the individual patient encounter is reflected in higher levels of practice-level pace, operationalized as chaos in previous studies of doctor’s work conditions.(14,15) This study extends the assessment to include perceptions of the entire practice team, thereby reflecting a broader concept of practice-level time pressure. Production pressure to see more patients more quickly is conceptualized as time pressure within encounters. While previous studies have sought physician estimations of time allocated to appointments versus time needed to provide high quality care, (15,16) our study operationalizes patient encounter-level time pressure for the entire team, using a measure of perceived patient safety effects from time pressure within appointments, specifically missing important care opportunities for diagnosis and treatment.(12) Both forms of the time pressure stressor – within and outside of encounters with patients—are hypothesized to create a stress response at the individual and team level. In turn, their responses to time pressure (stress) will affect the practice’s performance.
In addition to the overarching proposition of two types of time pressure, we propose hypotheses related to three questions:
What clinic factors are associated with Practice-Level Time Pressure?
What clinic factors are associated with Encounter-Level Time Pressure?
Are these Time Pressure constructs associated with Patient-Reported Experiences?
For the first question, environmental stressors exert force on the practice as a whole, creating practice-level time pressure (as measured by practice chaos) to varying degrees that depend on leadership and workgroup role within the practice team. We hypothesize that those occupying lower status positions in the team, such as Medical Assistants (MA), will report higher levels of practice chaos as they perform multiple operational tasks with low control to make practice-level improvements, relative to those in higher status positions such as Primary Care Physician (PCP) and Nursing personnel. (17–19) More leadership responsiveness to frontline needs related to challenges underway from primary care transformation will be associated with less practice-level time pressure.(20,21)
For the second research question, encounter-level time pressure may be perceived by the practice team to adversely affect patient care. We posit that practices that are more patient-centered, that coordinate their interdependent work better (relational coordination), and that use more health information technology capabilities will be less likely to report patient safety effects from time pressure during patient encounters. (22–24) Solidarity among team members could produce better teamwork or such a group-oriented culture could distract attention away from patient care, producing mixed adverse encounter-level effects.
To address the third question, we theorize that practice-level and encounter-level time pressure effects each adversely influence patient-reported experiences of care since adequate time is a prerequisite for actions to meet patient’s chronic care needs. (25) We hypothesize that patients receiving care from more time stressed practices will report lower levels of chronic care support.
Methods
Study Design Overview
To test the study’s theory and hypotheses, we analyzed cross-sectional survey data collected from primary care teams and their patients, participating in the second wave (January-August, 2016) of a longitudinal study of 16 clinics. The parent study protocol, the characteristics of the two regional ACOs, the random selection of the clinics within patient engagement strata, and the first wave of data analysis are reported elsewhere. (10) Patients were randomly sampled from the subset of each clinic’s population that met inclusion criteria (adults, English or Spanish or unknown primary language, at least one visit to the practice in the previous year, and evidence of diabetes or cardiovascular disease).
The study received approval prior to data collection by the institutional review board (IRB) of the University of California, Berkeley.
Methods to Test Hypothesis of Two Distinct Types of Time Pressure
Clinic Data Source.
All personnel in each clinic’s practice team received a survey (Appendix 1) from January 27 to April 25, 2016 with a response rate of 84.37% (N=353). Based on the work of Linzer et al, (12,15) the survey incorporated questions about the perception of time pressure (encounter-level time stressor) affecting patient care and practice chaos (practice-level time stressor).
As part of the Minimizing Error, Maximizing Outcome (MEMO) study of primary care clinics, Linzer et al developed a novel scale (OSPRE-Occupational Stress and Preventable Error) to assess physicians’ self-reported likelihood of future errors committed in the management of common chronic medical conditions.(12) We adapted the scale to assess perceived time pressure effects by all members of a clinic’s practice team, not just physicians. The variable is a seven-item battery assessing how likely it is that time pressure causes the respondent’s care team to overlook a proactive need to diagnose or screen a patient for a health problem (5 questions), or miss an important treatment opportunity (2 questions). For example, how likely would it be to ‘overlook a diagnosis of hypertension for a patient with 2–3 elevated BPs’? (Appendix 1).
A separate single-item 5-level scale assessed practice atmosphere from calm to chaotic, developed for MEMO, (15) and reported in two subsequent studies. (26,27) Linzer et al found that physicians who rated their practice as chaotic or hectic (4 or more on the 5-point scale) were more likely to report higher stress and burnout. (15)
To test independence of the two time pressure constructs, we conducted correlation analysis on the continuous time stressor items.
Methods to Test Clinic Level Organizational Correlates of Two Types of Time Pressure
We constructed two dependent dichotomized variables, one for each time pressure stressor. For practice-level time pressure, we used a cutoff from prior methods (1): hectic/ chaotic practices (a 4 or 5 rating on the Likert scale) versus calm to “busy, but reasonable” ones (ratings of 1 to 3). For encounter-level time pressure perceived effects, we split responses into two clinically meaningful groups: not worried about missing management opportunities (a 5 or above cutoff endorsing unlikeliness of misses) versus concerned enough to endorse likely missed management opportunities or unable to rule out the chance of a threat to patient safety.
We constructed the independent variables from the practice team survey as reported previously for the first wave of the study(10) from multiple questions on patient-centeredness, (28) solidarity culture,(29) leadership efforts to facilitate change and support the frontline workers,(30) and relational coordination among the people on the team in their respective roles related to patient care. (31) The survey also included questions about health information technology capabilities, not included in the first wave. (14)
For all summary dependent and independent measures, we conducted factor analysis and obtained acceptable Cronbach alpha internal consistency reliability coefficients of .82 and above with all items loading on one factor for each measure. (32)
We examined the hypothesized associations between organizational factors and the two dichotomized time stressor measures using multivariate logistic regression models and robust variance estimators. We also ran a combined model with all organizational factors to test for hypothesized null relationships between predictors of one time stressor but not the other. Finally, we tested alternative specifications of the dependent variables (alternative cutoffs in logistic analysis and continuous measures with generalized linear models) and found no substantive differences.
Methods to Test Associations Between Two Types of Time Pressure and Patient Experience
Patient Data Source.
From May 16 to August 9, 2016, we fielded a survey by mail with telephone follow-up. The survey achieved a 73.48% response rate (N=1,291). We collected demographic information and data on patient-reported outcomes of care,(33) patient assessment of the chronic illness care that they received (PACIC-11),(25,34) and patient-reported activation (PAM).(35) In addition, the survey included CollaboRATE, a 3-item measure of the extent that patients believe that the practice team understands what matters to them, and facilitates collaboration between the practice team and the patient. (36) The survey also asks the patients whether members of the team in addition to the doctor played an important role in their care.
We examined the hypothesized association between each time stressor measure summarized at the clinic practice level (average percentage of respondents with ratings above the dichotomized threshold) and patient-reported experiences. We estimated hierarchical linear regression models to account for patients nested within clinics.(37,38) These models controlled for patient characteristics including age, educational attainment, English language proficiency, help responding to the survey, patient activation, patient-reported physical, social, and emotional health status. All hierarchical regression analyses were performed with restricted maximum likelihood (REML) estimators, advantageous for a small number of clusters.
For all models reported, we restricted the practice sample to the core medical team member roles: PCPs (N=75), nurses (N=70), MAs (N=110), and diabetic nurse educators (N=19) due to substantial missing data among receptionists for key variables, and very small sample size for the other roles. There was minimal missing data for patient variables (average 1.1%, range 0 to 3.4%) and for most team variables (average 1.9%, range 0 to 9.1%). As a sensitivity test, analyses were also conducted on the full practice sample, and found substantively similar. Data were analyzed using Stata 14.0 (StataCorp LP, College Station, TX) and regression coefficients at a level of < 0.05 were considered statistically significant.
Results
Practice Team and Patient Characteristics
Table 1 shows the descriptive statistics for key variables based on practice team respondents (n=353) and patient respondents (n=1291). For practice team characteristics, the medical subset reported similar values as the entire team for all variables.
Table 1.
Descriptive Statistics for Key Variables
| Practice Team Survey Variables | Medical Team (med) N=274 | All N=353 | Cronbach alpha* |
|---|---|---|---|
| Time Pressure Measures | |||
| Encounter-Level Time Pressure Effect, mean, SD [range: 1–6] N=249* | 4.94 (1.14) | 4.96 (1.16) | 0.95 (7 items) |
| Encounter-Level Time Pressure, dichotomized dependent variable | 95/249 (38.2%) | 101/280 (36.1%) | |
| Practice Atmosphere (calm to chaotic), mean, SD [range: 1–5] N=272* | 3.29 (0.84) | 3.26 (0.86) | |
| Practice-Level Time Pressure: chaos, dichotomized dependent variable | 91/272 (33.5%) | 117/351 (33.3%) | |
| Organizational Factors+ | |||
| Relational coordination (RC), mean (SD) [range: 96–336] | 256.16 (42.62) | 264.04 (46.46) | 0.90 (7 items) |
| Patient centeredness, mean (SD) [range: 0–25] | 21.01 (4.60) | 20.73 (4.69) | 0.92 (5 items) |
| Health information technology (HIT), mean (SD) [range: 1–4] N=264* | 3.52 (0.55) | 3.52 (0.58) | 0.88 (8 items) |
| Leadership facilitation, mean (SD) [range: 0–35] | 26.17 (7.49) | 26.19 (7.71) | 0.95 (7 items) |
| Solidarity culture, mean (SD) [range: 0–20] | 14.92 (3.88) | 14.78 (3.88) | 0.82 (4 items) |
| Respondent Characteristics, count | |||
| Physician | 75 | 75 | |
| Nurse | 70 | 70 | |
| Medical Assistant | 110 | 110 | |
| Diabetic Educator | 19 | 19 | |
| Receptionist | - | 74 | |
| Other Workgroup Role: Social Worker, Dietician | - | 5 | |
| ACO A | 185 | 247 | |
| ACO B | 89 | 106 | |
| Patient Survey Variables | N=1291 | Range + | |
| Patient Assessment of Chronic Illness Care (PACIC), mean (SD) N=1282 | 2.73 (0.82) | 1–4 | 0.92 (11 items) |
| CollaboRATE, mean (SD) N=1269 | 3.61 (1.08) | 1–5 | 0.91 (3 items) |
| Patient Activation Measure (PAM), mean (SD) | 3.25 (0.51) | 0–4 | 0.92 (13 items) |
| Patient-Reported Outcomes (higher scores →better function) | |||
| Emotional Functioning (PHQ-4/Depression), mean (std. dev.) N=1284 | 3.50 (0.72) | 1–4 | 0.89 (4 items) |
| Physical functioning, mean (SD) N=1290 | 3.93 (0.91) | 1–5 | 0.93 (10 items) |
| Social functioning, mean (SD) N=1288 | 3.61 (1.06) | 1–5 | 0.96 (8 items) |
| Age, years, count (%) N=1278 | |||
| 18–24 | 4 (0.3%) | ||
| 25–44 | 48 (3.8%) | ||
| 45–64 | 446 (34.9%) | ||
| 65+ | 780 (61.0%) | ||
| Sex, count (%) N=1282, Female | 733 (57.2%) | ||
| Education, count (%) N=1269 | |||
| Grade 8 or less | 152 (12.0%) | ||
| GED or some high school | 371 (29.2%) | ||
| Four-year college degree or some college | 573 (45.2%) | ||
| More than 4-year college degree | 173 (13.6%) | ||
| English language proficiency (good versus poor), count (%) N=1285 | 1060 (82.5%) | ||
| Help (patient received help with survey), count (%) N= 1283 | 98 (7.6%) | ||
| Doctor only**, count (%) N=1247 | 561 (45.0%) |
Abbreviations: N, observations; SD, standard deviation; ACO, Accountable Care Organizations; GED, general equivalency diploma
Numbers based on Medical Respondents for the Practice Survey
Ranges for the organizational factors use the original instrument scales for each summary factor. The low end of the range for all factors stands for the least amount possible of the factor, and the high end the most (e.g., worst to best relational coordination feasible). The Appendix includes the items and the response options.
Respondent answered that other practice team members beside the doctor did not play an important role in care
The adult patients with diabetes and/or CVD established with the 16 clinics’ practices were 57.2% female, predominantly English speaking (82.5%), and over 44 years old (95.9%) with at least some college exposure (58.8%). Patient-reported functional status averaged slightly higher than the midpoint of scales, and patient responses spanned the entire scale from poor health to full functioning.
Time Stressors: Encounter-Level and Practice-Level
One-third (33.3%) of medical team respondents indicated a chaotic practice atmosphere. Only 31.3% of the medical team responded that during patient encounters it was very unlikely (responding 6 on the 1–6 scale) for the team to miss all seven specific opportunities related to screening, diagnosis or treatment. These encounter-level time pressure effects were highly correlated (average 0.73, range 0.63 to 0.82 in pairwise comparisons among the items) indicating comparable concern for patient safety effects of missed screening, diagnosis, or treatment. Practice-level time pressure, based on atmosphere from calm to chaotic, was not correlated with any of the encounter-level time pressure effects (0.02–0.05), supporting the hypothesis of two distinct time stressor constructs.
Figure 2 displays the dichotomized stressor variables (encounter-level time pressure effect and practice-level time pressure [chaos]) for each clinic’s practice team. The proportion of personnel from a given practice who reported a stressor ranged from 20% to 89%. Perez et al classified practices as chaotic if more than 50% of physicians rated the atmosphere as a 4 or 5.(27) Four of 16 clinics had 50% or more medical personnel perceiving chaotic practice-level time pressure (clinics 1, 7, 12 and 14). Clinic 14 from the chaotic subgroup, and three other clinics (8, 9 and 10) had greater than 50% of the medical respondents reporting greater likelihood of encounter-level time pressure effects on patient management.
Figure 2:
Time Pressure Effects for 16 Primary Care Clinics. The diagram shows responses of the medical team (“Med Team”) and entire team (“All”) to dichotomized time pressure measures (yellow for practice level chaos; blue for encounter level perceived missed patient management opportunities).
Organizational Factors Associated with Each Type of Time Pressure
Table 2 shows three models each for practice-level (chaos) and encounter-level time pressure effects to test theorized hypotheses. In the ACO-only models, the ACO encounter-level time pressure effects are indistinguishable, but respondents from ACO B are less likely to report practice-level chaos (odds ratio (OR) 0.52, p=0.03).
Table 2
| Practice-Level Time Pressure (Chaos) Odds Ratio [95% Confidence Interval] |
Encounter-Level Time Pressure Odds Ratio [95% Confidence Interval] |
||||||
|---|---|---|---|---|---|---|---|
| Model 1: ACO | Model 2: Hypothesized | Model 3: All Factors | Model 1: ACO | Model 2: Hypothesized | Model 3: All Factors | ||
| ACO B (vs ACO A) | .52* [.29−.93] | 1.23 [.71−2.13] | |||||
| Patient Centered | 1.02 [.94−1.1] | .83*** [.75−.91] | .82*** [.74−.92] | ||||
| HIT | 1.24 [.66−2.34] | .41** [.23−.72] | .33** [.17−.65] | ||||
| RC | 1 [.99−1.01] | .99** [.98−.99] | .99** [.98−1] | ||||
| Solidarity | .93 [.82−1.05] | 1.04 [.94−1.16] | 1.04 [.89−1.21] | ||||
| Leadership | .92*** [.88−.96] | .94 [.87−1] | .95 [.88−1.02] | ||||
| Clinic 1 | Reference | Reference | Reference | ||||
| 2 | .15** [.04−.62] | .12** [.03−.52] | 2.21 [.38−12.79] | ||||
| 3 | .18 [.02−1.35] | .17 [.02−1.29] | .78 [.03−17.74] | ||||
| 4 | .19 [.01−3.19] | .17 [.01−2.97] | 5.28 [.24−118.31] | ||||
| 5 | .05* [.00−.49] | .05* [.00−.51] | 1.29 [.13−12.64] | ||||
| 6 | .17* [.04−.87] | .13* [.02−.76] | .57 [.05−6.17] | ||||
| 7 | 1.92 [.16−23.1] | 1.46 [.12−18.14] | .31 [.04−2.6] | ||||
| 8 | .1* [.02−.6] | .09** [.01−.55] | 5.53 [.41−74.19] | ||||
| 9 | .05* [.00−.67] | .04* [.00−.6] | 1.33* [1.21−88.04] | ||||
| 10 | .05** [.01−.49] | .05* [.00−.52] | 12.27* [1.54−97.69] | ||||
| 11 | .15* [.03−.66] | .14* [.03−.66] | 1.31 [.25−6.77] | ||||
| 12 | .71 [.11 −4.65] | .57 [.08−3.95] | 1.04 [.10−1.74] | ||||
| 13 | .14** [.03−.54] | .11** [.03−.49] | .64 [.11−3.78] | ||||
| 14 | .35 [.05−2.38] | .3 [.04−2.29] | 14.83* [1.40−157.46] | ||||
| 15 | .1* [.02−.72] | .08* [.01−.61] | 1.16 [.09−15.02] | ||||
| 16 | 1.48** [.02−.51] | 1.48** [.01−.48] | 1.81 [.24−13.44] | ||||
| Physician | Reference | Reference | Reference | ||||
| Diabetes Educator | 1.16 [.26−5.18] | 1.17 [.26−5.18] | .8 [.21−3.11] | ||||
| Medical Assistant | 2.27* [1.07−4.83] | 2.09 [.97−4.5] | .22*** [.09−.53] | ||||
| Nursing | 1.59 [.67−3.76] | 1.48 [.60−3.63] | .25** [.11−.61] | ||||
| Model Statistics | |||||||
| N | 272 | 272 | 263 | 249 | 245 | 245 | |
| Wald chi | 4.89 | 44.00 | 46.64 | .55 | 42.08 | 65.67 | |
| Prob >chi2 | .03 | .00 | .00 | .46 | .00 | .00 | |
| McFad R2 | .01 | .17 | .18 | .00 | .20 | .33 | |
p < 0.05
p < 0.01
p < 0.001
Abbreviations: ACO, Accountable Care Organization; HIT, Health Information Technology; RC, Relational Coordination; N, observations; Prob, probability; McFad, McFadden
The second set of multivariate models examine the impact of adding clinic organizational variables hypothesized to be related to each time stressor. As hypothesized, encounter-level time pressure adverse effects are associated with less patient-centeredness (OR 0.83, p<0.001), less HIT capability (OR 0.41, p<0.01), and less relational coordination among team members (OR 0.99, p<0.01). Solidarity culture was not associated with encounter-level time pressure effects. Supporting the hypothesized relationships for practice-level time pressure, MAs were more likely to report a chaotic practice compared to PCPs, (OR 2.27, p<0.05), and greater leadership facilitation was associated with lower odds of practice-level chaos (OR 0.92, p<0.001).
The third set of models incorporated all independent variables to test whether different organizational characteristics predict one of the two time stressors, but not the other as hypothesized (null theory). As hypothesized, leadership facilitation was not associated with encounter-level time pressure, and patient-centeredness, HIT capability, relational coordination and solidarity culture were not associated with the presence of practice-level chaos. Contrary to the hypothesized relationship, both nurses and MAs were significantly less likely to perceive adverse encounter-level time pressure effects on patient care compared to PCPs (OR 0.25, p<0.01 for nurses and OR 0.22, p<0.001 for MAs).
Two Types of Time Pressure and Patient-Reported Experience of Chronic Care
Greater practice-level time pressure (chaos) was associated with lower PACIC-11 mean scores (OR 0.72, p<0.05) reflecting less chronic care support, and remained significant in multivariate analysis including patient-reported characteristics and other experiences with the practice (OR 0.74, p<0.01) (Table 3). Encounter-level time pressure was not associated with PACIC-11 scores in either unadjusted or adjusted analyses, though the effect trended in the expected direction.
Table 3
| Patient Assessment of Chronic Illness Care (PACIC) (Mean) Coefficient [95% Confidence Interval] + |
||||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| Practice-Level Time Pressure (Chaos) | 0.72* [0.54−0.95] | 0.74** [0.62−0.89] | ||
| Encounter-Level Time Pressure | 0.76 [0.46−1.27] | 0.84 [0.59−1.22] | ||
| Good English Proficiency (versus poor) | 0.95 [0.84−1.08] | 0.94 [0.83−1.07] | ||
| Help with survey (versus responded alone) | 1.16* [1.03−1.31] | 1.16* [1.03−1.31] | ||
| Age (versus 18−24) | Reference | Reference | ||
| 25−44 | 1.45 [0.78−2.67] | 1.48 [0.80−2.73] | ||
| 45−64 | 1.39 [0.77−2.53] | 1.40 [0.77−2.55] | ||
| 65+ | 1.37 [0.75−2.49] | 1.38 [0.76−2.50] | ||
| Female | 0.91** [0.85−0.97] | 0.91** [0.86−0.97] | ||
| Education (versus Grade 8 or less) | Reference | Reference | ||
| GED or some high school | 0.83** [0.73−0.95] | 0.83** [0.72−0.95] | ||
| 4 year college degree or some college | 0.73*** [0.64−0.85] | 0.73*** [0.63−0.84] | ||
| More than 4 year college degree | 0.75*** [0.64−0.88] | 0.74*** [0.63−0.87] | ||
| Social Functioning | 0.98 [0.94−1.02] | 0.98 [0.94−1.03] | ||
| Physical Functioning | 1.00 [0.95−1.05] | 0.99 [0.94−1.04] | ||
| Emotional Functioning | 1.03 [0.98−1.09] | 1.03 [0.98−1.09] | ||
| Patient Activation Measure (PAM) | 1.31*** [1.21−1.42] | 1.31*** [1.21−1.42] | ||
| Other Providers Involved (versus Doctor only) | 1.11*** [1.04−1.19] | 1.11*** [1.04−1.19] | ||
| CollaboRATE (mean) | 1.64*** [1.59−1.70] | 1.64*** [1.58−1.70] | ||
| Observations | 1282 | 1282 | 1189 | 1189 |
| Akaike Information Criterion (AIC) | 3130 | 3132.4 | 1936.5 | 1942.3 |
| Bayesian Information Criterion (BIC) | 3150.7 | 3153 | 2033 | 2038.9 |
| Inter Cluster Correlation (ICC) | 0.012 | 0.019 | 0.010 | 0.026 |
Coefficients and confidence intervals are exponentiated
p < 0.05
p < 0.01
p < 0.001
Abbreviation: GED, General Equivalency Diploma
Among control variables (Table 3, Models 3 and 4), those receiving help responding to the survey reported higher PACIC scores than those filling out on their own, women reported lower PACIC scores than men, and those with an 8th grade education or less had higher PACIC scores than those with more education. Patients who indicated that team members in the primary care practice besides the doctor played an important role in their care reported higher PACIC scores. Higher levels of collaboration with the practice team, and greater patient activation levels were also significantly associated with higher PACIC scores.
Discussion
Our study builds on a limited base of organizational research about time-related stress among health care professionals, the work they do, and the consequences for patients. This study provides initial support for the notion that there are two distinct time stressor constructs (encounter-level and practice-level), each with distinct potential clinic practice level organizational contributors, as well as different possible consequences to patient care—missed clinical care opportunities and less chronic care support.
Work Group Role
Individual primary care team members experience encounter and practice-level time stressors in different ways and we found systematic differences by team member role. MAs were more likely to perceive chaos (practice-level stressor) compared to PCPs, controlling for other factors. Part of a medical assistant’s role is to help the doctor focus on direct patient care work by buffering any rough edges in logistics and communications outside the exam room.(17–19) Some MAs may protect doctors from such practice chaos. Alternatively, because of their lower positional status, they may not feel comfortable sharing information about the chaotic environment with physicians, or have much efficacy in addressing it. We hypothesized no relationship between work group role and time pressure effects within the encounter. However, PCPs were significantly more likely to perceive encounter-level time pressure effects on patient care compared to MAs and nursing personnel. Physicians may have the best sightline to actual risks from encounter-level time pressure, or they may simply worry more about adverse effects, relative to the other team members. If the former situation is true, safety concerns and the potential patient consequences merit attention to balancing physician loads, adding scribes, exploring delegation arrangements and other efforts to reduce encounter-level time pressure effects.
Other Organizational Factors
As hypothesized, several organizational factors were associated with each time stressor. At the practice site level, more leadership facilitation – including management assuring enough time to discuss changes to improve care – was associated with less chaos. At the encounter level, more patient-centeredness, better availability and use of HIT capabilities, and higher levels of relational coordination were associated with fewer time pressure effects. The protective direction for HIT on encounter-level time pressure was even stronger after controlling for work group and clinic site, suggesting HIT has a potentially pivotal role in alleviating time stress during patient-clinician interactions. Practices that are more patient-centered may provide more time to the clinical team to carry out their patient-facing work.
Patient Effects
For longitudinal chronic care management, time pressure both within and outside encounters is relevant to optimal patient care. In addition to concerns about missed opportunites for care management raised by practice respondents, this study found that patients experienced less chronic care support from teams reporting higher levels of practice-level chaos. Previous studies have shown that chaos is associated with adverse physician effects such as lower job satisfaction and more burnout, but results are mixed for patient safety and quality effects.(15,27) Given high burnout levels of primary care clinicians and staff,(39) identifying the determinants and consequences of different forms of time stress in primary care is key to developing mitigating strategies.
Limitations
Although this study benefits from multilevel data collected directly from patients and practice teams at randomly selected primary care clinics in two regions, it has several limitations. First, encounter-level time pressure effects on patient care are based on perception about likelihood of missing important care needs, and are not verified by medical record review. Second, neither time pressure variable is corroborated by in-depth interviews with practice teams, a priority for future research. Third, in the organizational factors analysis, but not the patient experience analysis, independent and dependent measures come from the same survey, resulting in potential for common method variance bias inflating correlations among the same individuals responding to all the questions, and increasing the chance of spurious associations.(40) Because we analyze two separate dependent variables in a full model of all organizational dependent variables with null results as predicted, this concern diminishes. Fourth, the cross-sectional nature of the study precludes conclusions about causal mechanisms. Finally, the study is limited to ACO-based primary care practices, and therefore may not generalize to other practice environments. Given the transformational goals of ACOs, however, our findings provide relevant insight into time pressures faced by primary care team members with considerable incentives to simultaneously improve quality of care and patient experiences, while also reducing total costs of patient care.(41,42)
Future Directions Particularly by ACOs Focused on Safe, High Quality Care
Given ACO’s increasing role in health care delivery, the finding about a corporate effect on practice-level time pressure underscores the utility of data collection and analysis at multiple levels – patient, clinic practice team, and parent organization. ACOs may want to monitor practice-level and encounter-level time pressure as early warning signals for their workers and patients, who together are co-producing health outcomes and assuring safe care.(43) The National Academies produced the Crossing the Quality Chasm series –from To Err is Human to most recently Improving Diagnosis—that puts the onus on organizations to take a systems perspective that recognizes their contributions to quality and safety beyond individual provider efforts. (44) Time stressors arise from multiple systems sources largely within the control of ACOs and their management practices.
ACOs and their frontline teams are positioned well to identify contributors to time stressors, and whether interventions tied to our findings merit testing. For example, HIT is often implicated as increasing clinician burden, (45,46) yet specific HIT capabilities assessed in this study are associated with perceptions of lower likelihood of missing care opportunities. Interventions that enhance capabilities such as ease of assessing basic data, integrating data, and communication with other providers and patients could reduce time stress at the encounter level, and in turn, potential adverse consequences to patients.(47,48) Likewise, the focus for team work (i.e., patient-centeredness) and how work is organized and coordinated (i.e. capabilities for relational coordination among the different roles) may be important for buffering physicians from missing care opportunities in the exam room.(49) In terms of reducing practice-level time pressure, recent research on chaotic practices suggests that leaders might focus first on specific office bottleneck challenges such as availability of interpreter services and phone access.(27)
Supplementary Material
Footnotes
Appendix 1. Team Assessment Survey-supplementary file
Contributor Information
Kathryn M. McDonald, Stanford University, Contact: kathmcd@stanford.edu
Hector P. Rodriguez, University of California, Berkeley, Contact: hrod@berkeley.edu
Stephen M. Shortell, University of California, Berkeley, Contact: shortell@berkeley.edu
References
- 1.Centers for Disease Control and Prevention, National Center for Health Statistics. National Ambulatory Medical Care Survey: 2012 Summary Tables. 2012.
- 2.American College of Physicians. Management tools for internists - Designing the patient schedule. Center for Practice Improvement & Innovation; 2010. [Google Scholar]
- 3.Mauksch LB, Dugdale DC, Dodson S, Epstein R. Relationship, communication, and efficiency in the medical encounter. Arch Intern Med. 2008;168(13):1387–95. [DOI] [PubMed] [Google Scholar]
- 4.Abbo ED, Zhang Q, Zelder M, Huang ES. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008;23(12):2058–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res. 2007;42(5):1871–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sinsky C, Colligan L, Li L, Prgomet M, Reynolds S, Goeders L, et al. Allocation of physician time in ambulatory practice: A time and motion study in 4 specialties. Ann Intern Med. 2016. December 6;165(11):753–760. [DOI] [PubMed] [Google Scholar]
- 7.Mechanic D How should hamsters run? Some observations about sufficient patient time in primary care. BMJ. 2001;323(August):266–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Darley JM, Batson CD. “From Jerusalem to Jericho”: A study of situational and dispositional variables in helping behavior. J Pers Soc Psychol. 1973;27(1):100–8. [Google Scholar]
- 9.Szalma J, Hancock P, Quinn S. A Meta-analysis of the effect of time pressure on human performance. Proceedings of the Human Factors Ergonomics Society Soc 52nd Annu Meet. 2008;52(19):1513–6. [Google Scholar]
- 10.Shortell SM, Poon BY, Ramsay PP, Rodriguez HP, Ivey SL, Huber T, et al. A multilevel analysis of patient engagement and patient-reported outcomes in primary care practices of accountable care organizations. J Gen Intern Med. 2017. 32, 640–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kavanagh J (RAND). Stress and performance. A review of the literature and its applicability to the military. RAND. 2005. p. 1–86. [Google Scholar]
- 12.Linzer M, Manwell LB, Mundt M, Williams E, Maguire A, McMurray J, et al. Organizational climate, stress, and error in primary care: The MEMO study. Adv Patient Saf From Res to Implement (Vol 1). 2005;65–78. [PubMed] [Google Scholar]
- 13.Kleiner S Subjective time pressure: General or domain specific? Soc Sci Res. 2014. September;47:108–20. [DOI] [PubMed] [Google Scholar]
- 14.Linzer M, Visser MRM, Oort FJ, Smets EMA, McMurray JE, De Haes HCJM. Predicting and preventing physician burnout: Results from the United States and the Netherlands. Am J Med. 2001;111(2):170–5. [DOI] [PubMed] [Google Scholar]
- 15.Linzer M, Manwell LB, Williams ES, Bobula JA, Brown RL, Varkey A, et al. Working conditions in primary care: Physician reactions and care quality. Ann Intern Med. 2009. July 7;151(1):28. [DOI] [PubMed] [Google Scholar]
- 16.Linzer M, Konrad TR, Douglas J, McMurray JE, Pathman DE, Williams ES, et al. Managed care, time pressure, and physician job satisfaction: results from the PhysicianWorklife Study. J Gen Intern Med. 2000;15(7):441–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chapman SA, Blash LK. New roles for medical assistants in innovative primary care practices. Health Serv Res. 2017. February;52(S1):383–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Malley AS, Gourevitch R, Draper K, Bond A, Tirodkar MA. Overcoming challenges to teamwork in patient-centered medical homes: A qualitative study. J Gen Intern Med. 2015. February 11;30(2):183–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wagner EH, Flinter M, Hsu C, Cromp D, Austin BT, Etz R, et al. Effective team-based primary care: observations from innovative practices. BMC Fam Pract. 2017;18(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wise CG, Alexander JA, Green LA, Cohen GR, Koster CR. Journey toward a patient-centered medical home: Readiness for change in primary care practices. Milbank Q. 2011. September;89(3):399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berta W, Cranley L, Dearing JW, Dogherty EJ, Squires JE, Estabrooks CA. Why (we think) facilitation works: insights from organizational learning theory. Implement Sci. 2015. December 6;10(1):141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carayon P, Hundt AS, Karsh B-T, Gurses AP, Alvarado CJ, Smith M, et al. Work system design for patient safety: the SEIPS model. Qual Saf Heal Care. 2006;15(Suppl I):i50–i58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Panesar SS, DeSilva D, Carson-Stevens A, Cresswell KM, Salvilla SA, Slight SP, et al. How safe is primary care? A systematic review. BMJ Qual Saf. 2016. July;25(7):544–53. [DOI] [PubMed] [Google Scholar]
- 24.Singh H, Sittig DF. Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ Qual Saf. 2015;24(2):103–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gugiu PC, Coryn C, Clark R, Kuehn A. Development and evaluation of the short version of the Patient Assessment of Chronic Illness Care instrument. Chronic Illn. 2009;5(4):268–76. [DOI] [PubMed] [Google Scholar]
- 26.Linzer M, Poplau S, Grossman E, Varkey A, Yale S, Williams E, et al. A Cluster Randomized Trial of Interventions to Improve Work Conditions and Clinician Burnout in Primary Care: Results from the Healthy Work Place (HWP) Study. J Gen Intern Med. 2015;30(8):1105–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perez HR, Beyrouty M, Bennett K, Baier Manwell L, Brown RL, Linzer M, et al. Chaos in the clinic. J Healthc Qual. 2017;39(1):43–53. [DOI] [PubMed] [Google Scholar]
- 28.Rittenhouse DR, Shortell SM, Casalino LP, Ramsay PP, Bibi S, Ryan AM, et al. Managing chronic illness: Physician practices increased the use of care management and medical home processes. Health Aff. 2015;34(1):78–86. [DOI] [PubMed] [Google Scholar]
- 29.Kralewski JE, Wingert TD, Barbouche MH. Assessing the culture of medical group practices. Med Care. 1996;34(5):377–88. [DOI] [PubMed] [Google Scholar]
- 30.Helfrich CD, Li YF, Sharp ND, Sales AE. Organizational readiness to change assessment (ORCA): development of an instrument based on the Promoting Action on Research in Health Services (PARIHS) framework. Implement Sci. 2009;4:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gittell J Organizing Work to Support Relational Coordination. Int J Hum Resour Manag. 2000;11(3):517–39. [Google Scholar]
- 32.Kaplan RM, Saccuzzo DP. Psychological testing: principles, applications, and issues. 7th Ed. Monterey, CA: Brooks/Cole; 1982. [Google Scholar]
- 33.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glasgow RE, Whitesides H, Nelson CC, King DK. Use of the patient assessment of chronic illness care (PACIC) with diabetic patients: Relationship to patient characteristics, receipt of care, and self-management. Diabetes Care. 2005;28(11):2655–61. [DOI] [PubMed] [Google Scholar]
- 35.Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 I):1918–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elwyn G, Barr PJ, Grande SW, Thompson R, Walsh T, Ozanne EM. Developing CollaboRATE: A fast and frugal patient-reported measure of shared decision making in clinical encounters. Patient Educ Couns. 2013;93(1):102–7. [DOI] [PubMed] [Google Scholar]
- 37.Bryk A, Raudenbush S. Hierarchical linear models: applications and data analysis methods. 2nd Ed. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 38.Rabe-Hesketh S, Skrondal A. Multilevel and longitudinal modeling using Stata. 3rd Ed. College Station, TX: Stata Press; 2012. [Google Scholar]
- 39.Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–13. [DOI] [PubMed] [Google Scholar]
- 40.Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;88(5):879–903. [DOI] [PubMed] [Google Scholar]
- 41.Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care — Two essential elements of delivery-system reform. N Engl J Med. 2009. December 10;361(24):2301–3. [DOI] [PubMed] [Google Scholar]
- 42.Herrel LA, Ayanian JZ, Hawken SR, Miller DC. Primary care focus and utilization in the Medicare shared savings program accountable care organizations. BMC Health Serv Res. 2017;17(1):139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Batalden M, Batalden P, Margolis P, Seid M, Armstrong G, Opipari-Arrigan L, et al. Coproduction of healthcare service. BMJ Qual Saf. 2016; 25, 509–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.National Academies of Sciences, Engineering and Medicine. Quality Chasm Series: Health Care Quality Reports. https://www.nap.edu/catalog/21895/quality-chasm-series-health-care-quality-reports. Accessed June 17, 2018.
- 45.Zulman DM, Shah NH, Verghese A, S S-C, RB P, CA L, et al. Evolutionary Pressures on the Electronic Health Record: Caring for Complexity. Jama. 2016;88(12):877–82. [DOI] [PubMed] [Google Scholar]
- 46.Martin SA, Sinsky CA. The map is not the territory: medical records and 21st century practice. Lancet. 2016;6736(16):1–4. [DOI] [PubMed] [Google Scholar]
- 47.Sittig DF, Singh H. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Health Care. 2010;19 Suppl 3(Suppl 3):i68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grant RW, Adams AS, Bayliss EA, Heisler M. Establishing visit priorities for complex patients: A summary of the literature and conceptual model to guide innovative interventions. Healthcare. 2013;1(3–4):117–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.ALQahtani DA, Rotgans JI, Mamede S, ALAlwan I, Magzoub MEM, Altayeb FM, et al. Does Time Pressure Have a Negative Effect on Diagnostic Accuracy? Acad Med. 2016;91(5):710–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.