To the Editor:
Patient healthcare satisfaction has become increasingly important since Medicare’s introduction of the Hospital Care Quality Information from the Consumer Perspective (HCAHPS) survey [1]. Greater satisfaction is associated with important healthcare outcomes including lower risk of 30-day readmission [2].
While many factors contribute to patient satisfaction, communication likely plays an underappreciated role [3,4]. Hearing loss (HL) is a barrier to effective communication and highly prevalent, affecting 38 million Americans and increasing with age such that two-thirds of adults over the age of 70 have HL [5]. An emerging body of literature has found HL associated with poorer healthcare outcomes, including increased healthcare costs [6], and increased risk of hospitalization [7].
Hearing loss strains communication and may increase cognitive load via degraded auditory encoding, thereby further inhibiting the ability to process and comprehend speech. However, despite its role in communication, there is a paucity of research exploring the impact of HL on satisfaction with care. Notably, a limitation of current research is a use of self-report hearing, which is known to differ from objective measures by important characteristics (e.g. sex, race) that may be related to satisfaction [8]. Given its high prevalence, exploring HL’s impact on patient satisfaction has implications for public health and clinical care planning.
METHODS
Study population
A hearing pilot study was conducted in Washington County, MD in the Atherosclerosis Risk in Communities (ARIC) Study in 2013. 256 participants (mean age = 77.4 years) completed audiometric hearing measurements. Due to small numbers, we excluded non-white (n=3) and Medicaid (n=3) participants, as well as those missing outcome (n=3) and/or covariate (n=2) measures, resulting in an analytic sample of 248 Medicare beneficiaries.
Outcome measure
Participants were asked: “Overall, how satisfied are you with the quality of care you received from your healthcare providers over the past 12 months?” – “very dissatisfied”, “somewhat dissatisfied”, “somewhat satisfied” or “very satisfied”. We defined satisfaction with care as a binary outcome: less than optimally satisfied (somewhat satisfied, somewhat dissatisfied, or very dissatisfied) vs. optimally satisfied (very satisfied).
Hearing
Pure-tone air conduction hearing thresholds at the 500, 1000, 2000, and 4000 Hertz frequencies were obtained using clinically-accepted testing methods in a sound-attenuating booth with a calibrated audiometer. A pure-tone average (PTA) of the four frequencies in decibels hearing level (dB HL) was calculated to identify normal (<25 dB HL), mild (25–40 dB HL), and moderate (>40 dB HL) HL in the better-hearing ear.
Statistical analysis
The association between HL (modeled continuously as the better-hearing ear PTA) and satisfaction with care was modeled using logistic regression, adjusting for age, sex, cognition [9] (a global composite z-score of 3 tests measuring 3 domains), and count of comorbidities. We explored for interactions between HL and demographic variables (age, sex). A sensitivity analysis also adjusted for self-reported perceived health compared to peers of the same age.
RESULTS
70 (28%) participants had normal, 95 (38%) had mild, and 83 (34%) had moderate or greater HL. 178 (72%) reported being very satisfied, 55 (22%) somewhat satisfied, 8 (3%) somewhat dissatisfied, and 7 (3%) very dissatisfied with their medical care over the past 12 months.
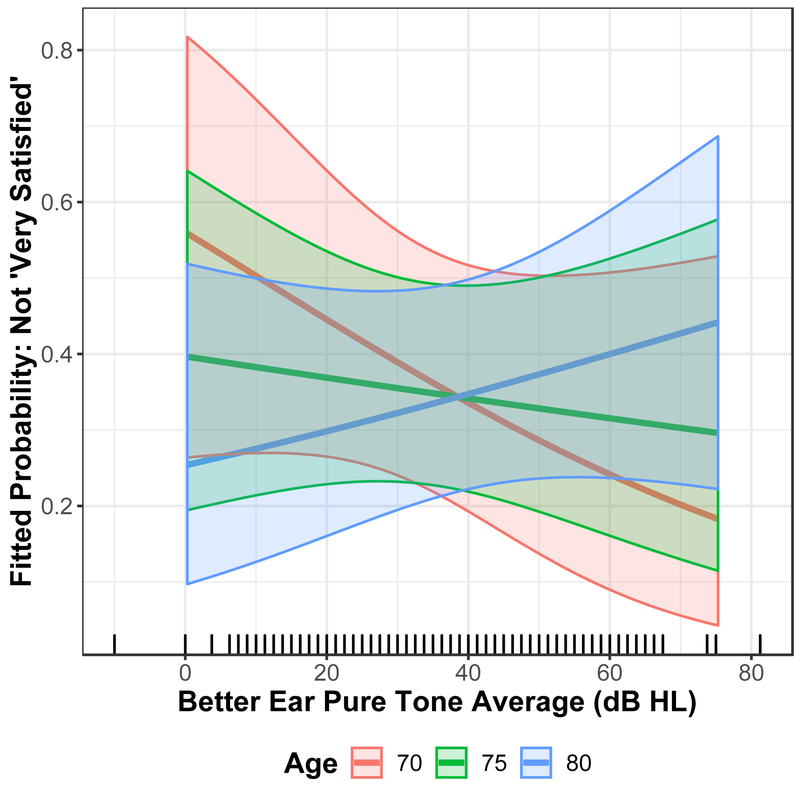
In multivariable-adjusted analyses, there was a significant (p=.033) interaction between HL and age such that HL had a greater impact on odds of being less than optimally satisfied among older adults (figure 1). For example, in a 75-year-old participant, for every 10 dB increase in HL, the odds of being less than optimally satisfied increased .94 (95% Confidence Interval [CI]:0.74–1.20). However, in an 85-year-old participant, for every 10 dB increase in HL, the odds of being less than optimally satisfied increased 1.33 (95% CI:0.96–1.83). Sensitivity analysis did not alter inference.
Figure 1.
The Probability of Being Less than Optimally Satisfied (not ‘Very Satisfied’) by Hearing Loss for a 70-, 75-, and 80-year old. Logistic regression model for odds of less than optimal satisfaction and hearing loss adjusted for age, sex, global cognitive score, comorbidity count (diabetes, hypertension, myocardial infarction, asthma, cancer, stroke, and hospital stay).
CONCLUSIONS
In this pilot study of 248 Medicare beneficiaries (67–89 years), HL is associated with being less than optimally satisfied with healthcare over the past year among older individuals. However, HL did not impact satisfaction with care among younger participants. To our knowledge, this is the first analysis to quantify the association of objective (i.e., audiometric) HL and healthcare satisfaction.
Our findings support a previous study indicating self-reported communication problems are associated with reduced healthcare satisfaction [3]. Hearing loss’ negative impact on patient-provider communication may contribute to this relationship. Our findings suggest an interaction between age and HL. It may be that younger adults are better able to cope with HL’ impact on their cognitive load. Future studies are needed to replicate these findings.
Our study is limited by demographic homogeneity and modest sample size. These results lend support for recent calls to address HL via screening and intervention techniques to improve patient-provider communication in the healthcare system [10].
Acknowledgments
Conflict of Interest
JAD was supported by National Institutes of Health/National Institute on Aging Grant K01AG054693. NSR was supported by National Institutes of Health Grant 5KL2TR001077–05. The Atherosclerosis Risk in Communities study has been funded in whole or in part with Federal funds from the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, under Contract nos. (HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700005I, HHSN268201700004I). The authors thank the staff and participants of the ARIC study for their important contributions. NSR reports non-financial scientific advisory role with Clearwater Clinical. FRL reports being a consultant to Cochlear and receiving speaker honoraria from Amplifon. No other reported conflicts of interest.
Footnotes
Sponsor’s Role
Sponsors had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of this study.
References
- 1.Centers for Medicare and Medicaid Services. (2011). Hospital care quality information from the consumer perspective. [Google Scholar]
- 2.Boulding W, Glickman SW, Manary MP, Schulman KA, & Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care 2011; 17(1): 41–48. [PubMed] [Google Scholar]
- 3.Barnett DD, Koul R, Coppola NM. Satisfaction with health care among people with hearing impairment: a survey of Medicare beneficiaries. Disabil Rehabil 2014; 36(1):39–48. [DOI] [PubMed] [Google Scholar]
- 4.Mick P, Foley DM, Lin FR. Hearing loss is associated with poorer ratings of patient–physician communication and healthcare quality. J Am Geriatr Soc 2014; 62(11):2207–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin FR, Niparko JK, Ferrucci L. Hearing loss prevalence in the United States. Arch Intern Med. 2011. November 14; 171(20):1851–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Foley DM, Frick KD, Lin FR. Association between hearing loss and healthcare expenditures in older adults. J Am Geriatr Soc. 2014; 62(6):1188–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Genther DJ, Betz J, Pratt S, et al. Health, Aging and Body Composition Study. Association between hearing impairment and risk of hospitalization in older adults. J Am Geriatr Soc 2015; 63(6):1146–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agrawal Y, Platz EA, Niparko JK. Prevalence of hearing loss and differences by demographic characteristics among US adults: data from the National Health and Nutrition Examination Survey, 1999–2004. Arch Intern Med. 2008; 168(14):1522–30. [DOI] [PubMed] [Google Scholar]
- 9.Deal JA, Sharrett AR, Albert MS, et al. Hearing impairment and cognitive decline: a pilot study conducted within the atherosclerosis risk in communities neurocognitive study. AM J Epidemiol. 2015; 181(9):680–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blustein J, Weinstein BE, Chodosh J. Tackling hearing loss to improve the care of older adults. BMJ, 2018; 360: k21. [DOI] [PubMed] [Google Scholar]