Abstract
Perfectionism may be a clinically relevant problem on its own or as part of the etiology and maintenance of psychiatric disorders, e.g., anxiety disorders, depression, and eating disorders. Cognitive behavior therapy has been shown to be a promising treatment for managing perfectionism and its associated problems, including when being administered via the Internet, i.e., Internet-based cognitive behavioral therapy (ICBT). In the current study, seventy-eight self-referred participants underwent ICBT after an initial eight-week wait-list period, i.e., second wave of treatment. These were randomized to receive regular support from a therapist (ICBT-support) or ICBT with support on request (ICBT-request), in an eight-week treatment of perfectionism. Assessments of perfectionism were made at pre-, mid-, and post-treatment, as well as six-month follow-up, using the Frost Multidimensional Perfectionism Scale, subscale Concern over Mistakes. Mixed effects models revealed large symptom reductions for both conditions; Concern over Mistakes, Cohen's d = 1.40, 95% Confidence Interval (CI) [0.85, 1.95] for ICBT-support, and d = 1.00, 95% CI [0.51, 1.47] for ICBT-request. The effects were maintained at six-month follow-up and there were no differences between the conditions in terms of the results, opened modules, or completed exercises. A total of 28 out of 70 participants (42.4%; ICBT-support, 37.8%; ICBT-request) were classified as improved at post-treatment. Both types of ICBT may thus be beneficial in treating perfectionism, suggesting that just having the opportunity to ask for support from a therapist, when regular support is not provided, could be sufficient for many participants undergoing ICBT. However, the study was underpowered to detect differences between the conditions. The lack of a cutoff also makes it difficult to differentiate a dysfunctional from a functional population in terms of perfectionism. In addition, the study design could have affected the participants' motivational level from start, given their initial eight-week wait-list period. Recommendations for future studies include recruiting a larger sample size, a clearer cutoff for perfectionism, and the use of a non-inferiority test with a predetermined margin of change.
Keywords: Perfectionism, Cognitive behavioral therapy, Internet, Randomized controlled trial, Support
Highlights
-
•
Internet-based cognitive behavioral therapy is effective in treating perfectionism.
-
•
Overall, participants completed 5.39 (SD = 2.88) out of eight treatment modules.
-
•
No differences were observed between different types of support, i.e., regular support versus support on request.
-
•
Only 27% of the participants in the support on request condition actively sought contact with their therapist during treatment.
-
•
A total of 42.4% receiving regular support were classified as improved, as compared to 37.8% in support on request.
1. Introduction
A distinction can be made between a healthy type of perfectionism that is associated with striving for achievement and success, and a problematic form of perfectionism that is related to different forms of distress (Frost et al., 1990). Of clinical interest is first and foremost the negative impact perfectionism can have on individuals, which primarily involves emotional aspects such as lower mood, social issues like interpersonal difficulties, and physical complaints characterized by insomnia and stress, but also leads to cognitive and behavioral consequences such as problems concentrating, repeated checking, and procrastination (Shafran et al., 2002). Historically, perfectionism has been conceptualized as both a multidimensional and unidimensional construct (Egan et al., 2011). Current evidence points to the existence of two higher-order dimensions: perfectionistic concerns (being overly concerned about making mistakes, doubting one's actions, and believing others impose high standards on oneself), and perfectionistic strivings (setting high standards and imposing these on oneself), both being linked to psychopathology (Stairs et al., 2012). From a clinical perspective, perfectionism has been defined as “[t]he overdependence of self-evaluation on the determined pursuit of personally demanding, self-imposed, standards in at least one highly salient domain, despite adverse consequences” (Shafran et al., 2002; p. 778). It is considered a transdiagnostic process that plays a part in the etiology and maintenance of several psychiatric disorders including anxiety disorders, depression, and eating disorders (Egan et al., 2011). A meta-analysis by Limburg et al. (2017) showed that the dimension of perfectionistic concerns is correlated with depression, r = 0.40, and anxiety disorders, r = 0.30, while perfectionistic strivings is correlated with anorexia nervosa, r = 0.56, and bulimia nervosa, r = 0.36, suggesting that different interventions might be useful for different patient populations depending on the nature of their perfectionism.
In terms of treatment, few clinical trials have been performed. A meta-analysis by Lloyd et al. (2015) on a total of six studies however suggested that Cognitive Behavioral Therapy (CBT) can be successful in treating perfectionism and in reducing symptoms of related conditions, thus lending some support to the idea of perfectionism as a transdiagnostic process. For one of the main measures of perfectionism, the Concern over Mistakes subscale from the Frost Multidimensional Perfectionism Scale (FMPS; Frost et al., 1990), the reported average within-group Hedges g effect size between pre- and posttreatment was 1.32 (95% CI 1.02–1.64) (Lloyd et al., 2015). FMPS is the measure most often used in a clinical setting and particularly relevant for assessing perfectionistic concerns (Sirois et al., 2017). In addition, applying the Clinical Perfectionism Questionnaire (CPQ; Fairburn et al., 2003), a measure for determining both perfectionistic concerns and perfectionistic strivings, the results ranged between g 0.90–1.24 (Lloyd et al., 2015). So far, CBT for perfectionism has been conducted individually with participants (Riley et al., 2007), in groups (Handley et al., 2015), in self-help formats (Pleva and Wade, 2007; Steele and Wade, 2008), as well as with Internet-based treatments (Arpin-Cribbie et al., 2012; Egan et al., 2014; Radhu et al., 2012; Rozental et al., 2017; Shafran et al., 2017). Two studies have also looked at the long-term results at six months (Egan et al., 2014), and twelve months (Rozental et al., 2018), implying that benefits seem to be maintained over time.
Internet-based CBT (ICBT) has primarily been used to treat mild to moderate psychological and somatic conditions such as depression, panic disorder, social anxiety, chronic pain, and generalized anxiety disorder (Andersson, 2016). ICBT can be more time efficient for the therapist in comparison to face-to-face therapy and facilitates symptom data collection (Andersson et al., 2019). For many conditions the effects are also comparable to face-to-face therapy (Carlbring et al., 2018). ICBT can be delivered in different formats with different amount of therapist support (Andersson, 2016). Guided treatments are generally recommended over unguided treatments, and have in several studies yielded greater effect sizes in comparison to unguided treatments (Baumeister et al., 2014), although exceptions exist (Titov et al., 2016). Furthermore, unguided treatments have also been shown to lead to higher dropout rates than guided treatments (Andersson et al., 2015). However, there may be other factors than therapist support that could help to explain differences in treatment outcome between guided and unguided treatments. Aspects such as the extensiveness of the screening process, the comprehensiveness of the treatment program, the presence of a clear deadline (Andersson et al., 2009), as well as automated reminders (Titov et al., 2013; Titov et al., 2009) have all been suggested to improve adherence in ICBT.
So far, the majority of studies conducted on ICBT have either included regular weekly therapist support or no support at all. Recently, a few studies have investigated a form of ICBT without regular support, but with the possibility of requesting therapist support. This could potentially reduce time associated with delivering therapy, which in turn could possibly increase the availability of evidenced based care. Also this format may better suite participants who do not require regular support, but who still may desire support during some part of the treatment program. This form of ICBT has been tried for treating panic disorder (Oromendia et al., 2016), chronic pain (Dear et al., 2015), mixed anxiety and depression (Hadjistavropoulos et al., 2017), and social anxiety (Berger et al., 2011). Results from these studies have been mostly promising with the optional support condition rendering comparable results to regular support, with the exception of the study by Oromendia et al. (2016), where findings were in favor of the scheduled support group. Also, completion rates were lower in the study by Hadjistavropoulos et al. (2017).
The preceding studies by Rozental et al. (2017) and Shafran et al. (2017) were the first to investigate the efficacy of guided ICBT for perfectionism in large-scale clinical trials, resulting in large positive impacts on measures of perfectionism. Between-group effect sizes Cohen's d, when compared to wait-list control on the FMPS Concern over Mistakes, were 1.00–1.01, and d of 0.92–1.15 on the CPQ. The results also indicated moderate to large benefits on measures of depression, anxiety, dysfunctional attitudes (a proxy for self-criticism commonly seen in perfectionism), self-compassion, and quality of life. Hence, although not explicitly targeted as part of treatment, ICBT for perfectionism also seems to yield positive outcomes on other forms of distress and transdiagnostic processes. Likewise, the results were maintained over time (Rozental et al., 2018), implying that more long-term change is possible to achieve.
As clinical interest in perfectionism is growing, a question of interest is how ICBT can be delivered in a way that is most efficient and beneficial for the individual. One aim of the current study was therefore to compare two ways of delivering ICBT in order to improve dissemination: ICBT with regular support and ICBT with the possibility of requesting support, both in an eight-week treatment specifically developed for targeting perfectionism (Shafran et al., 2010). It was designed to be an extension of the study by Rozental et al. (2017) by randomizing participants from the original wait-list control to two different forms of support. This allowed for an investigation on how support in ICBT for perfectionism influences treatment, most notably on measures of perfectionism. The main hypothesis was that the two conditions would be comparable in terms of their overall results, producing large effects d on the primary outcomes. Furthermore, given the proposed link between perfectionism and the etiology and maintenance of psychiatric disorders (Egan et al., 2011), measures of depression, anxiety, and dysfunctional attitudes were also included, the latter often being used as a proxy for investigating the connection between self-criticism and perfectionism (Dunkley et al., 2006). It was hypothesized that both conditions would obtain similar, albeit small to moderate effects d on these secondary outcomes. Meanwhile, given that one of the modules specifically involved the practice of self-compassion, and one important part of treatment was to rely less on performance for self-evaluation, measures of self-compassion and quality of life were also distributed. Again, with a hypothesis that treatment would lead to small to moderate effects d. In addition to this, other relevant aspects more directly related to the influence of different levels of support were also explored, such as attrition, the number of opened modules, and contact with a therapist. The hypotheses were that attrition would be lower, while the completed modules and contact with a therapist would be higher for those participants receiving regular support.
2. Method
2.1. Participants
Recruitment to the study was made via advertisements in Swedish media and on social media platforms during February and March 2016. Participants consisted of self-referrals who completed an online screening process and provided written informed consent on a secure platform connected to a website that was created for the purpose of the study (Vlaescu et al., 2016). Inclusion criteria were; minimum of 18 years of age, fluent in Swedish as assessed during a clinical interview via telephone, and having clinical perfectionism as the primary concern (as determined on a case-by-case basis, no cutoff was however used to determine the severity level). Exclusion criteria were; ongoing psychological treatment or counseling, any change in psychotropic medication three months prior to entering treatment, pregnancy (given the potential difficulties of completing the treatment period and/or assessments), and any condition warranting immediate care, e.g., psychosis, anorexia nervosa, severe depression, and suicidal ideation, established by the MINI-International Neuropsychiatric interview (MINI; Lecrubier et al., 1997). Other psychiatric disorders were, however, allowed as long as perfectionism was regarded as the principal problem.
2.2. Procedure
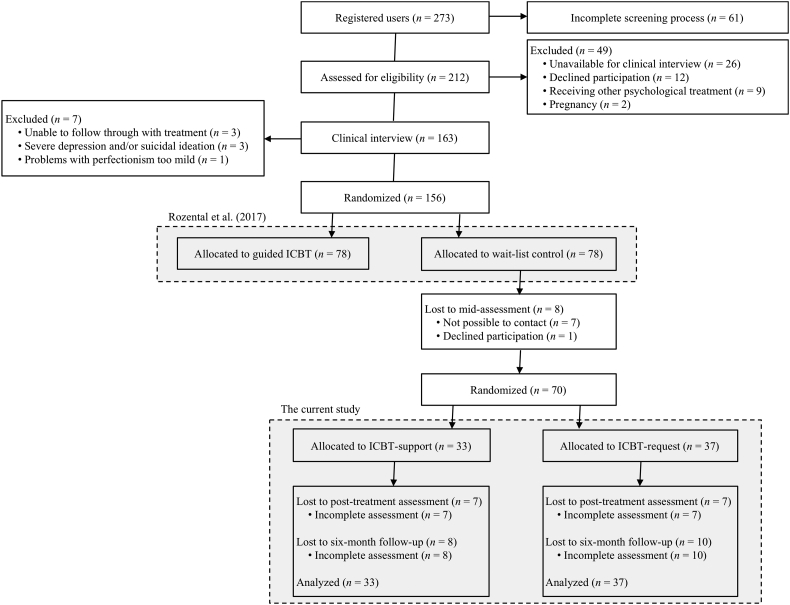
Individuals interested in participating entered the study website and completed an online screening process consisting of sociodemographic variables and several self-report measures. In total, 212 people were assessed for eligibility, of which 163 were contacted via telephone for a clinical interview (see Fig. 1 for a flow chart including reasons for exclusion). Each case was after this reviewed by the therapists together with the principal investigator (GA), who then made the final decision on inclusion and assumed overall clinical responsibility. In the end, 156 individuals were included and randomized using a random numbers generator (www.random.org) in a 1:1 ratio to one of two conditions; treatment (n = 78) or wait-list control (n = 78). Those allocated to treatment immediately received ICBT with therapist support (Rozental et al., 2017), but those assigned to wait-list control received ICBT after the initial treatment period of eight weeks had ended. The current study thus involves the second wave of treatment, and prior to beginning the treatment program, participants in wait-list control completed a mid-assessment consisting of the same self-report measures as during the screening process. The participants were also telephoned to determine their current motivation to commence. In total, eight participants were lost at this point, either declining participation (n = 1) or not being possible to contact (n = 7), making the total sample size 70. No monetary compensation was given to the participants.
Fig. 1.
A consort diagram of participant flow.
In order to investigate the impact of having therapist support, participants were randomized to obtain either ICBT-support, i.e., the same as the first wave of treatment, or ICBT-request, i.e., having the option to contact an assigned therapist when needed, but not receiving any further support. Due to a human error, the randomization at this stage was made using the original 78 participants allocated to wait-list control, disregarding the eight that were lost to mid-assessment, making the two conditions unbalanced; ICBT-support, n = 33, and ICBT-request, n = 37. Still, no significant differences between the two conditions were found for any of the sociodemographic variables or for the self-report measures at mid-assessment. For a flow-chart of the current study and the sociodemographics of its participants, see Fig. 1 and Table 1.
Table 1.
Sociodemographic characteristics of participants at pre-treatment assessment.
| ICBT-support (n = 33) | ICBT-request (n = 37) | Full sample (n = 70) | |
|---|---|---|---|
| Gender: n (% female) | 29 (87.9) | 34 (91.9) | 63 (90) |
| Age (years): M (SD) | 33.5 (8.2) | 34.1 (7.6) | 33.8 (7.8) |
| Marital status: n (%) | |||
| Single | 7 (21.2) | 9 (24.3) | 16 (22.9) |
| Married/partner | 25 (75.8) | 27 (73.0) | 52 (74.3) |
| Divorced/widow | 1 (3.0) | 1 (2.7) | 2 (2.9) |
| Children: n (% yes) | 12 (36.4) | 20 (54.1) | 32 (45.7) |
| Highest educational level: n (%) | |||
| Elementary school | 0 (0.0) | 1 (2.7) | 1 (1.4) |
| High school/college | 7 (21.2) | 10 (27.0) | 17 (24.3) |
| University | 26 (78.8) | 24 (64.9) | 50 (71.4) |
| Postgraduate | 0 (0.0) | 2 (5.4) | 2 (2.9) |
| Employment: n (%) | |||
| Unemployed | 1 (3.0) | 3 (8.1) | 4 (5.7) |
| Student | 12 (36.4) | 7 (18.9) | 19 (27.1) |
| Employed | 18 (54.5) | 22 (59.5) | 40 (57.1) |
| Parental leave | 0 (0.0) | 3 (8.1) | 3 (4.3) |
| Sick leave (>3 months) | 0 (0.0) | 2 (5.4) | 2 (2.9) |
| Other | 2 (6.1) | 0 (0.0) | 2 (2.9) |
| Previous psychological treatment: n (% yes) | 3 (9.1) | 2 (5.4) | 5 (7.1) |
| Previous psychotropic medication: n (% yes) | 6 (18.2) | 7 (18.9) | 13 (18.6) |
All communication between the participants, their therapists, and the study supervisors was made over the secure platform, on which the self-report measures were also completed at the post-treatment and six-month follow-up. To log on the participants used an autogenerated identifier that was given during the online screening process, e.g., 1234abcd, together with a personal password and a six-letter code sent via SMS. Many banks and government agencies often use this type of two-step verification, ensuring anonymity and confidentiality during the treatment period. Furthermore, since all of the self-report measures were filled out electronically, the risk of data loss and data distortion was minimized (Vlaescu et al., 2016). The current study received ethics approval from the Regional Ethical Board in Linköping, Sweden (Dnr: 2015/419-31), but was not pre-registered in an international clinical trials registry.
2.3. Measures
2.3.1. Primary outcome measure
The Concern over Mistakes subscale from the FMPS (Frost et al., 1990) was used to assess change during the treatment period. The FMPS as a whole consists of 35 items and covers six dimensions of clinical perfectionism. The Concern over Mistakes subscale is commonly employed in clinical trials (Shafran et al., 2002). This nine-item subscale is scored on a five-point Likert-scale, “Strongly disagree” (1) to “Strongly agree” (5), with scores ranging from 9 to 45. The subscale correlates well with other self-report measures of perfectionism and has demonstrated excellent internal consistency, Concern over Mistakes has a Cronbach's α 0.88 (Frost et al., 1990), in the current study 0.85.
2.3.2. Secondary outcome measures
The other subscales of the FMPS were also distributed to the participants, that is Personal Standards, Doubts about Action, Parental Expectation, Parental Criticism, and Organization, but were only explored for secondary analyses. The number of items on each subscale varies between four to seven (range in scores in parentheses), with internal consistencies ranging from adequate to excellent, 0.77–0.93 (Frost et al., 1990), albeit less reliably so in the current study for some of the subscales; Personal Standards, 0.65 (7–35), Doubts about Action, 0.52 (4–20), Parental Expectation, 0.90 (5–25), Parental Criticism, 0.86 (4–20), and Organization, 0.83 (6–30).
In addition, the twelve-item CPQ was used (Fairburn et al., 2003), which is another self-report measure of perfectionism, scored on a four-point Likert-Scale, “Not at all” (1) to “All of the time” (4), range in scores 12–48. The CPQ has demonstrated adequate internal consistency (0.73), the current study, 0.66, and is believed to capture dimensions of perfectionistic concerns and strivings. Similarly, the Patient Health Questionnaire – 9 Items was included (PHQ-9; Löwe et al., 2004), investigating the degree of depression. The PHQ-9 is scored on a four-point Likert-scale, “Not at all” (0) to “Nearly every day” (3), range in scores 0–27, and has obtained excellent internal consistency, 0.89, the current study 0.84. The Generalized Anxiety Disorder – 7 Items was also used to assess the level of anxiety (GAD-7; Dear et al., 2011). The GAD-7 is scored on a four-point Likert-scale, “Not at all” (0) to “Nearly every day” (3), range in scores 0–21, and has demonstrated excellent internal consistency, 0.92, the current study 0.87. Furthermore, the forty-item Dysfunctional Attitude Scale was distributed to explore self-criticism among the participants (DAS; Weissman and Beck, 1978), and is scored on a seven-point Likert-scale, “Strongly disagree” (1) to “Strongly agree” (7), range in scores 40–280. The DAS has revealed an excellent internal consistency, 0.93, the current study, 0.91. Also, the twelve-item Brunnsviken Brief Quality of Life Scale (Lindner et al., 2016) was administered to investigate the satisfaction in six different life domains among the participants, e.g., relationships, as well as their respective level of importance, e.g., “Friends and friendship are important for my quality of life”. The BBQ is thus scored both in terms of satisfaction and importance on a five-point Likert-scale, “Strongly disagree” (0) to “Strongly agree” (4), which is then weighted by multiplying both scores for each life domain, range in scores 0–96. The BBQ has demonstrated good internal consistency, 0.86, the current study 0.79. Lastly, the twelve-item Self-Compassion Scale – Short Form (SCS-SF; Raes et al., 2011) was used to determine the degree of self-compassion exhibited by the participants. The SCS-SF is scored on five-point Likert-scale, “Almost never” (1) to “Almost always” (5), and has obtained good internal consistency, 0.86, the current study, 0.79.
Moreover, satisfaction with the treatment program was also investigated using a self-report measure consisting of eight items, e.g., “How would you judge the overall quality of the treatment you have received” (Item 1). Rating were given using a four-point Likert-Scale, “Not at all pleased” (1) to “Very pleased” (4), and then divided by the number of items.
2.4. Treatment and therapists
The treatment program used in the current study was developed by Shafran et al. (2010) and targets perfectionism using a rationale and interventions stemming from CBT, e.g., behavioral experiments, identifying maladaptive thoughts and beliefs, and implementing problem-solving techniques. In total, the treatment program consisted of eight modules, or, chapters; 1) Understanding your perfectionism, 2) Your own model, values, and motivation, 3) Surveys and experiments, 4) Dealing with perfectionistic behaviors, 5) New ways of thinking, 6) Self-criticism or self-compassion, 7) Self-worth, and 8) Maintain and continue positive change. However, in comparison to the original outline, some minor modifications were made, primarily related to a greater emphasis on behavioral interventions. The eight modules were administered to the participants weekly throughout the treatment period, each module consisting of approximately twelve pages of text, graphics, and videos and exercises to be completed every week, totaling 121 pages and 33 exercises. The treatment program in the current study was the same as the first wave of treatment (Rozental et al., 2017), the only difference relates to the type of guidance provided by the therapists. Those in ICBT-support completed their reading and exercises and sent the results to their assigned therapists on Thursdays, while homework assignments were handed in on Sundays. The therapists then provided feedback within 24 h on each of these occasions. Those in ICBT-request received exactly the same treatment program, including homework assignments. However, they did not get any assistance from their assigned therapists unless they explicitly requested this. They did receive automated weekly reminders informing them that a new module was available. If the participants in this condition wanted feedback or help, the therapists were able to deliver this within 24 h. The participants were also monitored with regard to their completion of the modules and having logged on to the secure platform, resulting in an attempt to contact the participants if adherence was too low.
The therapists were five master's degree students in clinical psychology and four psychotherapist students. In Sweden, the clinical psychology program is a five-year vocational education that includes one and a half year of clinical training under supervision, as well as a clinical placement. Upon graduation and working one year with patients, one can apply for a clinical psychology-license, which is regulated by the National Board of Health and Welfare. For further clinical training one can also attend the psychotherapist program at the university, which is a three-year advance clinical education for clinicians with several years of patient experience. Hence, all of the therapists in the current study had at least a basic clinical training in CBT. The therapists were also provided one-hour of weekly supervision by AR and RS, following the guidelines for delivering therapist-assisted ICBT (Hadjistavropoulos et al., 2018).
The participants in the current study were allocated to the therapists by randomization. Each therapist was responsible for between two and 16 participants from both conditions, median for ICBT-support was three and ICBT-request four. They were recommended to spend 15 min per participant per week in ICBT-support, on average, giving feedback and assistance. No time restrictions were imposed for ICBT-request, except the fact that they were not to engage with the participants unless explicitly requested by them to do so. However, the exact amount of time spent per participant in both of the conditions was not controlled for.
2.5. Statistical analysis
Because the current study involved the second wave of treatment, and that only those participants originally in wait-list control were eligible to participate (i.e., no additional recruitment was made), a priori power was not deemed necessary to calculate. However, a post-hoc power calculation with the obtained between-group effect d on the FMPS Concern over Mistakes, α of 0.05, and two conditions with 33 and 37 participants in each indicated that the power to detect a difference was only 0.24.
All statistical analyses were based on the intention-to-treat principle (ITT; Hollis and Campbell, 1999), using mixed effects models to investigate the differences between conditions and time points, as well as interaction effects (Gueorguieva and Krystal, 2004). An unstructured covariance structure was implemented as the repeated covariance type, which is suitable for repeated measures in clinical trials. Maximum likelihood estimation with 100 iterations was used to account for missing data, and post hoc tests with Bonferroni-correction were performed to adjust for multiple comparisons for the more exploratory secondary outcome measures.
Within-group effect sizes were calculated using the difference in means between time points for each condition and dividing the results with the pooled standard deviation. Between-group effect sizes were calculated in a similar manner, but instead using the difference in means between the conditions. All effect sizes were reported together with 95% Confidence Intervals (CI) and compared to other similar estimates, where applicable (Cumming and Finch, 2001). Clinically significant change was also explored to establish the number of participants presumed to have moved outside the range of a dysfunctional population. In the current study, which followed the same procedure as Rozental et al. (2017), a score at post-treatment of <29 on the FMPS Concern over Mistakes was considered to reflect clinically significant change, in line with the recommendations by Suddarth and Slaney (2001). However, to be classified as improved, the participant also had to reach the criteria for a reliable change using the Reliable Change Index, in this case a change score of at least 6.79. The same number but in a negative direction was used to determine the number of participants showing a reliable deterioration (Rozental et al., 2014). Improvement and deterioration rates were calculated with the total number of participants (n = 70) as the denominator, i.e., ITT.
3. Results
3.1. Attrition, adherence, and satisfaction with treatment
Attrition was defined as those participants not completing the assessment at post-treatment or six-month follow-up. In total, 14 participants (20.0%) did not complete the self-report measures at post-treatment and 18 participants (25.7%) at six-month follow-up. However, no significant difference between completers and non-completers were detected when comparing them on any of the sociodemographic variables or self-report measures at pre-treatment.
In terms of opened modules, the mean number opened by the participants was 5.39 (SD = 2.88) out of eight, suggesting that they accessed approximately two-thirds of the treatment program (see Table 2). No significant difference was however revealed between the conditions, t(68) = −1.19, 95% CI [−2.19, 0.55]. The mean number of completed exercises by the participants was 17.77 (SD = 10.78) out of 33 (51.5%). Again, no significant difference was detected between the conditions, t(63) = 1.32, 95% CI [−1.80, 8.85].
Table 2.
Number of opened modules (%) during the treatment period.
| ICBT-support | ICBT-request | Total | |
|---|---|---|---|
| One module | 31 (93.9) | 34 (91.9) | 65 (92.9) |
| Two modules | 28 (84.8) | 30 (81.1) | 58 (82.9) |
| Three modules | 26 (78.8) | 29 (78.4) | 55 (78.6) |
| Four modules | 25 (75.8) | 26 (70.3) | 51 (72.9) |
| Five modules | 23 (69.7) | 20 (54.1) | 43 (61.4) |
| Six modules | 22 (66.7) | 17 (45.9) | 39 (55.7) |
| Seven modules | 20 (60.6) | 17 (45.9) | 37 (52.9) |
| Eight modules | 17 (51.5) | 12 (32.4) | 29 (41.4) |
With regard to therapist contact, 25 (75.8%) of the participant in ICBT-support actively sought help and guidance from their therapists, compared to only 10 participants (27%) in ICBT-request, a difference that was significant, t(35) = −4.45, 95% CI [−2.93, −1.09].
As for satisfaction with the treatment program, the participants' impression of the treatment program was, on average 3.31 (SD = 0.72) for ICBT-support and 2.75 (SD = 0.56) for ICBT-request, i.e., “Mostly satisfying” (scored on a four-point Likert-scale 1–4). A significant difference was obtained between the conditions, t(54), −3.29, 95% CI [−0.91, −0.22], suggesting that those in ICBT-support were more satisfied with the treatment program than those in ICBT-request.
3.2. Treatment results
The results from the mixed effects models (ITT) revealed a main effect of Time for the primary outcome measure, FMPS Concern over Mistakes, up to post-treatment, with both conditions improving over time, F(3, 78) = 20.14, p < .01. Similar results were obtained for the FMPS Personal Standards and Doubts about Action subscales, CPQ, PHQ-9, GAD-7, DAS, BBQ, and SCS-SF, Fs (3, 77–92) = 3.72–24.18, ps < .01, albeit not for FMPS Parental Expectations, Parental Criticism, and Organization subscales, Fs (3, 77–84) = 2.09–2.53, ps > .05. In addition, no main effect of Group or interaction effects were detected between the conditions, suggesting that no significant difference was possible to detect between ICBT-support and ICBT-request in terms of treatment gains on any of the measures.
As for the assessment at the six-month follow-up, no main effect of Time or Group or interaction effects were possible to discern between post-treatment and the long-term results, indicating that the benefits were maintained over time or remained unchanged.
Estimated marginal means and standard deviations for both conditions and every assessment can be found in Table 3, and effect sizes in Table 4.
Table 3.
Estimated marginal means and standard deviations for each outcome measure divided by condition and assessment.a
| Measure and condition | Pre-treatment assessment |
Mid-assessment |
Post-treatment assessment |
Six-month follow-up |
||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | |
| FMPS Concern over Mistakes | ||||||||
| ICBT-support | 35.79 | 6.06 | 35.06 | 7.55 | 25.88 | 7.95 | 27.46 | 8.96 |
| ICBT-request | 34.81 | 6.07 | 34.20 | 7.59 | 27.70 | 8.00 | 26.57 | 9.06 |
| FMPS Personal Standards | ||||||||
| ICBT-support | 28.79 | 3.92 | 28.39 | 4.77 | 24.79 | 4.75 | 25.60 | 6.30 |
| ICBT-request | 28.08 | 3.92 | 27.92 | 4.81 | 24.93 | 4.78 | 23.56 | 6.39 |
| FMPS Doubts about Action | ||||||||
| ICBT-support | 13.94 | 2.89 | 13.55 | 3.27 | 11.45 | 3.73 | 11.50 | 3.91 |
| ICBT-request | 13.65 | 2.89 | 13.96 | 3.30 | 12.32 | 3.75 | 11.31 | 3.97 |
| FMPS Parental Expectations | ||||||||
| ICBT-support | 11.85 | 5.34 | 11.46 | 5.46 | 10.42 | 5.16 | 10.20 | 4.92 |
| ICBT-request | 12.54 | 5.33 | 12.22 | 5.48 | 11.33 | 5.18 | 11.21 | 4.95 |
| FMPS Parental Criticism | ||||||||
| ICBT-support | 9.09 | 4.02 | 9.12 | 4.12 | 7.79 | 4.30 | 8.13 | 3.97 |
| ICBT-request | 9.35 | 4.02 | 8.87 | 4.16 | 8.93 | 4.31 | 8.40 | 4.00 |
| FMPS Organization | ||||||||
| ICBT-support | 24.55 | 4.23 | 24.00 | 4.29 | 22.31 | 4.51 | 22.70 | 5.26 |
| ICBT-request | 24.35 | 4.23 | 24.89 | 4.31 | 23.25 | 4.53 | 22.53 | 5.32 |
| Clinical Perfectionism Questionnaire | ||||||||
| ICBT-support | 38.49 | 4.41 | 38.15 | 5.11 | 30.30 | 6.83 | 32.13 | 7.75 |
| ICBT-request | 38.00 | 4.42 | 37.47 | 5.15 | 31.15 | 6.87 | 31.38 | 7.88 |
| Patient Health Questionnaire – 9 Items | ||||||||
| ICBT-support | 10.15 | 5.39 | 9.12 | 6.09 | 6.04 | 6.01 | 6.91 | 6.60 |
| ICBT-request | 9.43 | 5.39 | 8.94 | 6.13 | 6.66 | 5.97 | 6.90 | 6.68 |
| Generalized Anxiety Disorder – 7 Items | ||||||||
| ICBT-support | 9.61 | 5.21 | 7.46 | 5.38 | 5.00 | 4.73 | 7.33 | 6.15 |
| ICBT-request | 8.30 | 5.21 | 7.00 | 5.42 | 4.70 | 4.68 | 5.38 | 6.20 |
| Dysfunctional Attitude Scale | ||||||||
| ICBT-support | 174.49 | 30.94 | 177.52 | 34.69 | 128.69 | 39.90 | 140.02 | 44.28 |
| ICBT-request | 180.05 | 30.94 | 174.20 | 34.83 | 140.13 | 39.26 | 138.63 | 44.33 |
| Brunnsviken Brief Quality of Life Scale | ||||||||
| ICBT-support | 43.64 | 16.26 | 46.88 | 15.79 | 57.60 | 17.03 | 55.74 | 18.89 |
| ICBT-request | 40.86 | 16.26 | 44.65 | 15.90 | 50.63 | 17.10 | 50.79 | 19.22 |
| Self-Compassion Scale – Short-Form | ||||||||
| ICBT-support | 26.46 | 6.28 | 26.39 | 6.77 | 35.71 | 8.20 | 34.69 | 9.92 |
| ICBT-request | 26.08 | 6.28 | 26.22 | 6.81 | 34.44 | 8.22 | 34.43 | 10.01 |
FMPS = Frost Multidimensional Perfectionism Scale; ICBT = Internet-based Cognitive Behavior Therapy.
ICBT-support N = 33; ICBT-request N = 37.
Table 4.
Within-group effect sizes and between-group effect sizes Cohen's d [95% CI] for all outcome measures.
| Measure and condition | Pre- to post-treatment assessment | Post-treatment assessment to six-month follow-up |
|---|---|---|
| FMPS Concern over Mistakes | ||
| ICBT-support | 1.40 [0.85, 1.92] | −0.19 [−0.67, 0.30] |
| ICBT-request | 1.00 [0.51, 1.47] | 0.13 [−0.33, 0.59] |
| ICBT-support vs. ICBT-request | 0.23 [−0.25, 0.70] | 0.10 [−0.37, 0.57] |
| FMPS Personal Standards | ||
| ICBT-support | 0.92 [0.40, 1.41] | −0.15 [−0.63, 0.34] |
| ICBT-request | 0.72 [0.24, 1.18] | 0.24 [−0.22, 0.70] |
| ICBT-support vs. ICBT-request | 0.03 [−0.44, 0.50] | 0.32 [−0.15, 0.79] |
| FMPS Doubts about Action | ||
| ICBT-support | 0.75 [0.24, 1.24] | −0.01 [−0.50, 0.47] |
| ICBT-request | 0.40 [−0.07, 0.85] | 0.26 [−0.20, 0.72] |
| ICBT-support vs. ICBT-request | 0.23 [−0.24, 0.70] | 0.05 [−0.42, 0.52] |
| FMPS Parental Expectations | ||
| ICBT-support | 0.27 [−0.22, 0.75] | 0.04 [−0.44, 0.53] |
| ICBT-request | 0.23 [−0.23, 0.68] | 0.02 [−0.43, 0.48] |
| ICBT-support vs. ICBT-request | 0.18 [−0.30, 0.64] | 0.20 [−0.27, 0.67] |
| FMPS Parental Criticism | ||
| ICBT-support | 0.31 [−0.18, 0.79] | −0.08 [−0.56, 0.40] |
| Wait-list | 0.10 [−0.36, 0.56] | 0.13 [−0.33, 0.58] |
| ICBT-support vs. ICBT-request | 0.26 [−0.21, 0.73] | 0.07 [−0.40, 0.54] |
| FMPS Organization | ||
| ICBT-support | 0.51 [0.02, 1.00] | −0.08 [−0.56, 0.40] |
| Wait-list | 0.25 [−0.21, 0.71] | 0.15 [−0.31, 0.60] |
| ICBT-support vs. ICBT-request | 0.21 [−0.26, 0.68] | 0.03 [−0.44, 0.50] |
| Clinical Perfectionism Questionnaire | ||
| ICBT-support | 1.41 [0.87, 1.95] | −0.25 [−0.73, 0.24] |
| ICBT-request | 1.19 [0.68, 1.67] | −0.03 [−0.49, 0.42] |
| ICBT-support vs. ICBT-request | 0.12 [−0.35, 0.59] | 0.10 [−0.37, 0.56] |
| Patient Health Questionnaire – 9 Items | ||
| ICBT-support | 0.72 [0.21, 1.21] | −0.14 [−0.62, 0.35] |
| ICBT-request | 0.49 [0.02, 0.94] | −0.04 [−0.49, 0.42] |
| ICBT-support vs. ICBT-request | 0.10 [−0.37, 0.57] | 0.00 [−0.47, 0.47] |
| Generalized Anxiety Disorder – 7 Items | ||
| ICBT-support | 0.93 [0.41, 1.42] | −0.42 [−0.91, 0.07] |
| ICBT-request | 0.73 [0.25, 1.19] | −0.12 [−0.58, 0.33] |
| ICBT-support vs. ICBT-request | 0.06 [−0.41, 0.53] | 0.32 [−0.16, 0.78] |
| Dysfunctional Attitude Scale | ||
| ICBT-support | 1.28 [0.74, 1.80] | −0.27 [−0.75, 0.22] |
| ICBT-request | 1.13 [0.63, 1.61] | 0.04 [−0.42, 0.49] |
| ICBT-support vs. ICBT-request | 0.29 [−0.19, 0.76] | 0.03 [−0.44, 0.50] |
| Brunnsviken Brief Quality of Life Scale | ||
| ICBT-support | 0.84 [0.33, 1.33] | −0.10 [−0.59, 0.38] |
| ICBT-request | 0.59 [0.11, 1.04] | 0.01 [−0.45, 0.46] |
| ICBT-support vs. ICBT-request | 0.41 [−0.07, 0.88] | 0.26 [−0.21, 0.73] |
| Self-Compassion Scale – Short-Form | ||
| ICBT-support | 1.27 [0.72, 1.78] | −0.11 [−0.59, 0.37] |
| ICBT-request | 1.14 [0.64, 1.62] | 0.00 [−0.45, 0.46] |
| ICBT-support vs. ICBT-request | 0.16 [−0.31, 0.63] | 0.03 [−0.44, 0.50] |
FMPS = Frost Multidimensional Perfectionism Scale; ICBT = Internet-Based Cognitive Behavior Therapy.
3.3. Improvement and deterioration
Improvement was predetermined as having achieved both clinically significant change, i.e., <29 on the FMPS Concern over Mistakes, and having a change score of at least 6.79, i.e., exceeding the Reliable Change Index. Using this criterion, 28 out of 70 participants (40.0%) were identified as improved as post-treatment, and 24 out of 70 participants (34.3%) at six-month follow-up (see Table 5 for the numbers in each condition). No significant difference was detected between the conditions, χ2 (1) = 0.15, p = .70, and χ2 (1) = 0.44, p = .51.
Table 5.
Improvement and deterioration rates on the FMPS concern over mistakes divided by condition and assessment.
| Improvement |
Deterioration |
|||
|---|---|---|---|---|
| Post-treatment assessment | Six-month follow-up | Post-treatment assessment | Six-month follow-up | |
| ICBT-support | 14 (42.4%) | 10 (30.3%) | 0 (0.0%) | 0 (0.0%) |
| ICBT-request | 14 (37.8%) | 14 (37.8%) | 1 (2.7%) | 0 (0.0%) |
| Total | 28 (40.0%) | 24 (34.3%) | 1 (1.4%) | 0 (0.0%) |
FMPS = Frost Multidimensional Perfectionism Scale; ICBT = Internet-based Cognitive Behavior Therapy.
In terms of deterioration, i.e., having a negative change score of at least 6.79 on the FMPS Concern over Mistakes, only one out of 70 participants deteriorated to post-treatment, and none to six-month follow-up.
4. Discussion
The current study is part of a series of clinical trials investigating the efficacy of an eight-week ICBT-program for perfectionism (Rozental et al., 2017; Shafran et al., 2017; Rozental et al., 2018). The purpose of the current study was to compare two types of ICBT, one with regular support and one with support on request. Overall, the results mirrored those of previous studies, suggesting that ICBT can yield large within-group effect sizes on measures of perfectionism, and additional but more moderate benefits on other forms of distress and transdiagnostic processes. The results also revealed that the level of support did not differentiate the two conditions in terms of treatment outcome, opened modules, attrition, or rates of improvement and deterioration. Between-group effect sizes ranged from barely distinguishable to small for the primary outcome measure, FMPS Concern over Mistakes, as well as for the secondary outcome measures. Furthermore, the findings also suggested that outcomes were maintained or remained unchanged at six-month follow-up, again with no difference detected between the conditions, implying that participants can benefit from treatment both when receiving regular support and when support is only provided upon request. However, no differences were found over time for the FMPS Parental Expectations, Parental Criticism, and Organization subscales, similar to what is usually seen in research of treatments of perfectionism (Rozental et al., 2017; Shafran et al., 2017). According to Rozental et al. (2017) one possible explanation for this could be that these subscales capture aspects of perfectionism that are not easily targeted by treatment, for instance potential onset mechanisms for developing perfectionism in the first place, e.g., parental influence.
Along with the clinical trials by Rozental et al. (2017) and Shafran et al. (2017), as well as Arpin-Cribbie et al. (2012), Egan et al. (2014), and Radhu et al. (2012), the findings from the current study provide further support for the use of Internet-based treatments for perfectionism. The results also lend support to the growing amount of evidence suggesting that CBT can be effective in treating perfectionism, as suggested by Lloyd et al. (2015). In terms of the lack of differences between the two conditions, this goes in line with other studies comparing these two types of ICBT (Berger et al., 2011; Dear et al., 2015; Hadjistavropoulos et al., 2017), which might suggest that regular support is not necessary for all participants in order to benefit from treatment. One possible explanation for this might be that the mere perception of having a therapist to contact is enough for some participants in order to progress through treatment. However, in retrospect, the study was underpowered to find differences between the conditions and relied on a study design that made it difficult to explore one of its purposes, namely to compare two ways of delivering ICBT. It should therefore not be concluded that both were equal in terms of treatment outcome, and future studies should investigate this issue further, preferably by recruiting a larger sample size to begin with, and to conduct a non-inferiority test with a predetermined margin of change. Moreover, although the between-group comparisons were not significant, there still appears to exist a small and possibly clinically relevant difference between the conditions when looking at the within-group changes that occurred. This goes for both the primary outcome measure and for most of the secondary measures. Although highly tentative, this could point to the advantages of receiving ICBT with regular support for perfectionism, as noted by for Baumeister et al. (2014).
Nonetheless, a few differences were observed. Not surprisingly the results showed that participants in ICBT-support were in contact with their therapists more frequently, i.e., sent more messages, in comparison to participants in ICBT-request. In other words, as participants in ICBT-support received regular feedback from their therapists this presumably facilitated further communication between the participants and the therapists. Meanwhile, participants in ICBT-request sent few, if any, messages to their therapists. Why this might be the case is not known. Andersson and Titov (2014) suggested that therapist expertise could be less important in Internet-based treatments in comparison to face-to-face treatments, as long as the treatment program in itself is of adequate quality and sufficiently engaging. It is therefore possible that the participants in ICBT-request received all of the help they needed from the treatment modules, making additional support unnecessary. The amount of therapist support sought in the current study resembles numbers reported in other clinical trials that have included a support on request condition (Dear et al., 2015; Hadjistavropoulos et al., 2017; Oromendia et al., 2016). One notable exception is the study Berger et al. (2011) where the proportion of participants seeking additional support was considerably larger. A reason for this may have been that participants in the Berger et al. (2011) study were automatically asked at the end of each module if they wished to receive additional support. Interestingly, it should be noted that there was a difference between the conditions concerning overall satisfaction with treatment in the current study, in favor of ICBT-support. The reason for this is not known, but a possible interpretation of these findings is that regular support may have not been crucial for improvement, yet it may have influenced the participants' personal experiences of the treatment.
The number of treatment modules opened and number of completed exercises did not significantly differ between the groups. However, there was a tendency towards greater adherence in ICBT-support. A difference between the conditions can be observed when comparing the number of participants opening the fifth treatment module. This difference also seems to be maintained until the last treatment module, 17 participants (51.5%; ICBT-support) versus 12 participants (32.4%; ICBT-request). One possible explanation for this might be that as the treatment program became increasingly demanding more participants dropped-out or did not continue at the same speed as before, making regular support more important. A similar pattern was found in the study by Hadjistavropoulos et al. (2017). Finding ways of preventing attrition in Internet-based treatments without regular support is therefore warranted. In the study by Berger et al. (2011) no differences in adherence were found between the conditions, suggesting that the presence of an online discussion forum may have enhanced motivation and increased adherence for those without regular support.
A few limitations should be mentioned regarding the study. First, the design of the current study poses some limitations in that it constitutes the second wave of large-scale clinical trial and therefore does not include a wait-list condition. Also the absence of a completely unguided condition makes it difficult to assess the actual contribution of having therapist support, even if it was only given upon request. A pure self-help comparator would have been useful in order to benchmark such aspects as attrition against the findings in the study, and should be explored in the future. There is also a risk of having participants commence treatment after an initial wait-list period in that they might have been more motivated to complete the modules than in the first wave of treatment, thereby affecting the generalizability of the results. The sample size also risks being underpowered for detecting differences of effects between the conditions. Second, a predefined cutoff (>29) was used in the study to differentiate a dysfunctional from a functional population on the FMPS Concern over Mistakes at post-treatment and six-month follow-up (Suddarth and Slaney, 2001). Average scores at pre-treatment and mid-assessment were above this value, ranging from 34.20 to 35.79 (SD = 6.06–7.59), which is higher than other clinical populations reviewed by Egan et al. (2011). For instance, in a study by Sassaroli et al. (2008), individuals with eating disorders scored 35.10 (SD = 8.30), depression 27.80 (SD = 5.90), and obsessive-compulsive disorder 29.00 (SD = 7.7). However, some participants in the current study did fall below >29. In addition, inclusion on the basis of perfectionism was determined on a case-by-case basis rather than using a clear severity level. This could suggest that some participants may not have experienced problems related to perfectionism at a “clinical” level. Furthermore, it is still unclear if the applied cutoff is clinically relevant, that is whether it can distinguish those with more severe perfectionism. Third, the sociodemographic characteristics of the sample used may limit the generalizability of the findings, as the participants were composed of predominantly women (90%) with a university level degree (70%). However, even though these percentages do not resemble the general population they are not unlike those individuals that tend to seek mental health care (Howard, 1996), including Internet-based treatments (Andersson and Titov, 2014). Fourth, although the results from the current study suggest that there was difference between the conditions in terms of seeking contact with the therapists, this was only possible to investigate with regard to number of messages sent rather than the total amount of time or type of messages sent. Hence, it is possible that the lack of regular feedback and guidance for ICBT-request actually resulted in more time spent per participant than in ICBT-support, for instance, having to clarify certain aspects of the modules. Future research should investigate this by recording how much time is in fact allocated, thereby allowing a more reliable comparison of therapist contact. Furthermore, a more thorough and qualitative analysis of the type of messages sent by the participants could have been informative in order to understand how the support was actually being used. Likewise, asking participants in ICBT-request at post-treatment why they did not seek additional support could have been valuable. Also therapist specific effects could have been looked at (Magnusson et al., 2018). However, these were considered unlikely due to that the feedback was generally limited in nature, and regular supervision ensured a common approach. In addition, the relatively large number of therapists delivering the treatment reduced the risk of bias. Lastly, a proper evaluation of the potential cost-effectiveness of ICBT-request in comparison to ICBT-support, taking into consideration time therapists spent on each group, was not performed, making it impossible to conclude that one condition was more cost-efficient than the other.
In sum, the current study suggests that ICBT with support on request may be a viable alternative to ICBT with regular support in the treatment of perfectionism. Along with the study by Rozental et al. (2017) and Shafran et al. (2017) this suggests that perfectionism may be successfully treated with ICBT with different levels of support. Finding new ways of treating perfectionism is of clinical interest as it is being identified as a transdiagnostic area of importance for several psychiatric disorders (Egan et al., 2011). The current study also contributes to the growing number of clinical trials demonstrating that ICBT delivered with support on request may be a useful alternative to ICBT with regular support (Berger et al., 2011; Dear et al., 2015; Hadjistavropoulos et al., 2017), or with no support at all (Rozental et al., 2015). However more research is needed on this topic, particularly with regard to matching individuals seeking Internet-based treatment to different types of support in order to improve adherence and outcome while also reaching out to as many people as possible.
Conflict of interest
Professor Roz Shafran receives royalties for the self-help book that was used for the treatment program in the current study. None of the other authors have any conflicts of interest to report.
References
- Andersson G. Internet-delivered psychological treatments. Annu. Rev. Clin. Psychol. 2016;12(1):157–179. doi: 10.1146/annurev-clinpsy-021815-093006. [DOI] [PubMed] [Google Scholar]
- Andersson G., Titov N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry. 2014;13(1):4–11. doi: 10.1002/wps.20083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G., Carlbring P., Berger T., Almlöv J., Cuijpers P. What makes internet therapy work? Cogn. Behav. Ther. 2009;38(Suppl. 1):55–60. doi: 10.1080/16506070902916400. [DOI] [PubMed] [Google Scholar]
- Andersson G., Rozental A., Rück C., Carlbring P. Guided Internet-delivered CBT: can it really be as good as seeing a therapist? Behav. Ther. 2015;38(5):123–126. [Google Scholar]
- Andersson G., Titov N., Dear B.F., Rozental A., Carlbring P. Internet-delivered psychological treatments: from innovation to implementation. World Psychiatry. 2019;18:20–28. doi: 10.1002/wps.20610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arpin-Cribbie C., Irvine J., Ritvo P. Web-based cognitive-behavioral therapy for perfectionism: a randomized controlled trial. Psychother. Res. 2012;22(2):194–207. doi: 10.1080/10503307.2011.637242. [DOI] [PubMed] [Google Scholar]
- Baumeister H., Reichler L., Munzinger M., Lin J. The impact of guidance on Internet-based mental health interventions – a systematic review. Internet Interv. 2014;1(4):205–215. [Google Scholar]
- Berger T., Caspar F., Richardson R., Kneubühler B., Sutter D., Andersson G. Internet-based treatment of social phobia: a randomized controlled trial comparing unguided with two types of guided self-help. Behav. Res. Ther. 2011;49(3):158–169. doi: 10.1016/j.brat.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Carlbring P., Andersson G., Cuijpers P., Riper H., Hedman-Lagerlöf E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cogn. Behav. Ther. 2018;47(1):1–18. doi: 10.1080/16506073.2017.1401115. [DOI] [PubMed] [Google Scholar]
- Cumming G., Finch S. A primer on the understanding, use, and calculation of confidence intervals that are based on central and noncentral distributions. Educ. Psychol. Meas. 2001;61(4):532–574. [Google Scholar]
- Dear B.F., Titov N., Sunderland M., McMillan D., Anderson T., Lorian C., Robinson E. Psychometric comparison of the Generalized Anxiety Disorder Scale-7 and the Penn State Worry Questionnaire for measuring response during treatment of generalised anxiety disorder. Cogn. Behav. Ther. 2011;40(3):216–227. doi: 10.1080/16506073.2011.582138. [DOI] [PubMed] [Google Scholar]
- Dear B.F., Gandy M., Karin E., Staples L.G., Johnston L., Fogliati V.J.…Titov N. The Pain Course: a randomised controlled trial examining an internet-delivered pain management program when provided with different levels of clinician support. Pain. 2015;156(10):1920–1935. doi: 10.1097/j.pain.0000000000000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkley D.M., Sanislow C.A., Grilo C.M., McGlashan T.H. Perfectionism and depressive symptoms 3 years later: negative social interactions, avoidant coping, and perceived social support as mediators. Compr. Psychiatry. 2006;47(2):106–115. doi: 10.1016/j.comppsych.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Egan S.J., Wade T.D., Shafran R. Perfectionism as a transdiagnostic process: a clinical review. Clin. Psychol. Rev. 2011;31(2):203–212. doi: 10.1016/j.cpr.2010.04.009. [DOI] [PubMed] [Google Scholar]
- Egan S.J., van Noort E., Chee A., Kane R.T., Hoiles K.J., Shafran R., Wade T.D. A randomised controlled trial of face to face versus pure online self-help cognitive behavioural treatment for perfectionism. Behav. Res. Ther. 2014;63:107–113. doi: 10.1016/j.brat.2014.09.009. [DOI] [PubMed] [Google Scholar]
- Fairburn C., Cooper Z., Shafran R. Department of Psychiatry, University of Oxford; Oxford, UK: 2003. Clinical Perfectionism Questionnaire. [Google Scholar]
- Frost R.O., Marten P., Lahart C., Rosenblate R. The dimensions of perfectionism. Cogn. Ther. Res. 1990;14(5):449–468. [Google Scholar]
- Gueorguieva R., Krystal J.H. Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the Archives of General Psychiatry. Arch. Gen. Psychiatry. 2004;61(3):310–317. doi: 10.1001/archpsyc.61.3.310. [DOI] [PubMed] [Google Scholar]
- Hadjistavropoulos H.D., Schneider L., Edmonds M., Karin E., Nugent M.M., Dirkse D., Dear B.F., Titov N. Randomized controlled trial of Internet-delivered cognitive behaviour therapy comparing standard weekly versus optional weekly therapist support. J. Anxiety Disord. 2017;52:15–24. doi: 10.1016/j.janxdis.2017.09.006. [DOI] [PubMed] [Google Scholar]
- Hadjistavropoulos H.D., Schneider L.H., Klassen K., Dear B.F., Titov N. Development and evaluation of a scale assessing therapist fidelity to guidelines for delivering therapist-assisted Internet-delivered cognitive behaviour therapy. Cogn. Behav. Ther. 2018:1–15. doi: 10.1080/16506073.2018.1457079. [DOI] [PubMed] [Google Scholar]
- Handley A.K., Egan S.J., Kane R.T., Rees C.S. A randomised controlled trial of group cognitive behavioural therapy for perfectionism. Behav. Res. Ther. 2015;68:37–47. doi: 10.1016/j.brat.2015.02.006. [DOI] [PubMed] [Google Scholar]
- Hollis S., Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ. 1999;319:670. doi: 10.1136/bmj.319.7211.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard K.I. Patterns of mental health service utilization. Arch. Gen. Psychiatry. 1996;53(8):696. doi: 10.1001/archpsyc.1996.01830080048009. [DOI] [PubMed] [Google Scholar]
- Lecrubier Y., Sheehan D.V., Weiller E., Amorim P., Bonora I., Sheehan K.H.…Dunbar G.C. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. Eur. Psychiatry. 1997;12(5):224–231. [Google Scholar]
- Limburg K., Watson H.J., Hagger M.S., Egan S.J. The relationship between perfectionism and psychopathology: a meta-analysis. J. Clin. Psychol. 2017;73(10):1301–1326. doi: 10.1002/jclp.22435. [DOI] [PubMed] [Google Scholar]
- Lindner P., Frykheden O., Forsström D., Andersson E., Ljótsson B., Hedman E. The Brunnsviken Brief Quality of Life Scale (BBQ): development and psychometric evaluation. Cogn. Behav. Ther. 2016;45(3):182–195. doi: 10.1080/16506073.2016.1143526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd S., Schmidt U., Khondoker M., Tchanturia K. Can psychological interventions reduce perfectionism? A systematic review and meta-analysis. Behav. Cogn. Psychother. 2015;43:705–731. doi: 10.1017/S1352465814000162. [DOI] [PubMed] [Google Scholar]
- Löwe B., Kroenke K., Herzog W., Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9) J. Affect. Disord. 2004;81(1):61–66. doi: 10.1016/S0165-0327(03)00198-8. [DOI] [PubMed] [Google Scholar]
- Magnusson K., Andersson G., Carlbring P. The consequences of ignoring therapist effects in trials with longitudinal data: a simulation study. J. Consult. Clin. Psychol. 2018 doi: 10.1037/ccp0000333. [DOI] [PubMed] [Google Scholar]
- Oromendia P., Orrego J., Bonillo A., Molinuevo B. Internet-based self-help treatment for panic disorder: a randomized controlled trial comparing mandatory versus optional complementary psychological support. Cogn. Behav. Ther. 2016;45(4):270–286. doi: 10.1080/16506073.2016.1163615. [DOI] [PubMed] [Google Scholar]
- Pleva J., Wade T.D. Guided self-help versus pure self-help for perfectionism: a randomised controlled trial. Behav. Res. Ther. 2007;45(5):849–861. doi: 10.1016/j.brat.2006.08.009. [DOI] [PubMed] [Google Scholar]
- Radhu N., Daskalakis Z.J., Arpin-Cribbie C.A., Irvine J., Ritvo P. Evaluating a web-based cognitive-behavioral therapy for maladaptive perfectionism in university students. J. Am. Coll. Heal. 2012;60(5):357–366. doi: 10.1080/07448481.2011.630703. [DOI] [PubMed] [Google Scholar]
- Raes F., Pommier E., Neff K.D., Van Gucht D. Construction and factorial validation of a short form of the Self-Compassion Scale. Clin. Psychol. Psychother. 2011;18(3):250–255. doi: 10.1002/cpp.702. [DOI] [PubMed] [Google Scholar]
- Riley C., Lee M., Cooper Z., Fairburn C.G., Shafran R. A randomised controlled trial of cognitive-behaviour therapy for clinical perfectionism: a preliminary study. Behav. Res. Ther. 2007;45(9):2221–2231. doi: 10.1016/j.brat.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozental A., Andersson G., Boettcher J., Ebert D.D., Cuijpers P., Knaevelsrud C.…Carlbring P. Consensus statement on defining and measuring negative effects of Internet interventions. Internet Interv. 2014;1(1):12–19. [Google Scholar]
- Rozental A., Forsell E., Svensson A., Andersson G., Carlbring P. Internet-based cognitive-behavior therapy for procrastination: a randomized controlled trial. J. Consult. Clin. Psychol. 2015;83(4):808–824. doi: 10.1037/ccp0000023. http://psycnet.apa.org/doi/10.1037/ccp0000023 [DOI] [PubMed] [Google Scholar]
- Rozental A., Shafran R., Wade T., Egan S., Nordgren L.B., Carlbring P.…Andersson G. A randomized controlled trial of Internet-Based Cognitive Behavior Therapy for perfectionism including an investigation of outcome predictors. Behav. Res. Ther. 2017;95:79–86. doi: 10.1016/j.brat.2017.05.015. [DOI] [PubMed] [Google Scholar]
- Rozental A., Shafran R., Wade T.D., Kothari R., Egan S.J., Ekberg L.…Andersson G. Guided web-based cognitive behavior therapy for perfectionism: results from two different randomized controlled trials. J. Med. Internet Res. 2018;20(4):e154. doi: 10.2196/jmir.9823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sassaroli S., Lauro L.J.R., Ruggiero G.M., Mauri M.C., Vinai P., Frost R. Perfectionism in depression, obsessive–compulsive disorder and eating disorders. Behav. Res. Ther. 2008;46:757–765. doi: 10.1016/j.brat.2008.02.007. [DOI] [PubMed] [Google Scholar]
- Shafran R., Cooper Z., Fairburn C.G. Clinical perfectionism: a cognitive–behavioural analysis. Behav. Res. Ther. 2002;40(7):773–791. doi: 10.1016/s0005-7967(01)00059-6. [DOI] [PubMed] [Google Scholar]
- Shafran R., Egan S., Wade T. Robinson Publishing; United Kingdom: 2010. Overcoming Perfectionism: A Self-help Guide Using Scientifically Supported Cognitive Behavioural Techniques. [Google Scholar]
- Shafran R., Wade T.D., Egan S.J., Kothari R., Allcott-Watson H., Carlbring P.…Andersson G. Is the devil in the detail? A randomised controlled trial of guided internet-based CBT for perfectionism. Behav. Res. Ther. 2017;95:99–106. doi: 10.1016/j.brat.2017.05.014. [DOI] [PubMed] [Google Scholar]
- Sirois F.M., Molnar D.S., Hirsch J.K. A meta-analytic and conceptual update on the associations between procrastination and multidimensional perfectionism. Eur. J. Personal. 2017;31(2):137–159. [Google Scholar]
- Stairs A.M., Smith G.T., Zapolski T.C.B., Combs J.L., Settles R.E. Clarifying the construct of perfectionism. Assessment. 2012;19(2):146–166. doi: 10.1177/1073191111411663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele A.L., Wade T.D. A randomised trial investigating guided self-help to reduce perfectionism and its impact on bulimia nervosa: a pilot study. Behav. Res. Ther. 2008;46(12):1316–1323. doi: 10.1016/j.brat.2008.09.006. [DOI] [PubMed] [Google Scholar]
- Suddarth B.H., Slaney R.B. An investigation of the dimensions of perfectionism in college students. Meas. Eval. Couns. Dev. 2001;34:157–165. [Google Scholar]
- Titov N., Andrews G., Choi I., Schwencke G., Johnston L. Randomized controlled trial of web-based treatment of social phobia without clinician guidance. Aust. N. Z. J. Psychiatry. 2009;43:913–919. [Google Scholar]
- Titov N., Dear B.F., Johnston L., Lorian C., Zou J., Wootton B.…Rapee R.M. Improving adherence and clinical outcomes in self-guided Internet treatment for anxiety and depression: randomised controlled trial. PLoS One. 2013;8(7) doi: 10.1371/journal.pone.0062873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N., Fogliati V., Staples L., Gandy M., Johnston L., Wootton B.…Dear B. Treating anxiety and depression in older adults: randomised controlled trial comparing guided v. self-guided internet-delivered cognitive-behavioural therapy. BJPsych Open. 2016;2(1):50–58. doi: 10.1192/bjpo.bp.115.002139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlaescu G., Alasjö A., Miloff A., Carlbring P., Andersson G. Features and functionality of the Iterapi platform for internet-based psychological treatment. Internet Interv. 2016;6:107–114. doi: 10.1016/j.invent.2016.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman A.N., Beck A.T. 1978. Development and Validation of the Dysfunctional Attitude Scale: A Preliminary Investigation. (Paper Presented at the 86th Annual Convention of the American Psychological Association, Toronto, Canada). [Google Scholar]