Abstract
Background:
The quadriceps tendon is a versatile graft option, and the clinical implications of a quadriceps tendon harvest need to be further defined.
Purpose:
To review surgical considerations for the safe harvest of a quadriceps tendon autograft for anterior cruciate ligament (ACL) reconstruction, with a focus on the risk of patellar fractures.
Study Design:
Case series; Level of evidence, 4.
Methods:
A series of 57 patients underwent ACL reconstruction with a quadriceps tendon autograft with a patellar bone block from March 2011 to December 2012 at a single institution. Patients who sustained a patellar fracture were identified. The clinical course for each patient was reviewed with International Knee Documentation Committee (IKDC) subjective knee form scores through 2-year follow-up.
Results:
The incidence of patellar fractures was 3.5% intraoperatively and 8.8% at 2 years. This included 2 intraoperative fractures, 1 fracture during strength testing, and 2 occult fractures detected on computed tomography (CT) performed 6 months postoperatively for research purposes in asymptomatic participants. For the 5 patients with a patellar fracture with 24-month follow-up, the IKDC scores were 91.95, 91.95, 100.00, 100.00, and 64.37.
Conclusion:
Careful consideration of the quadriceps tendon and patellar anatomy is needed to safely harvest the bone plug from the superior pole of the patella. The consequences of a quadriceps tendon autograft harvest, specifically with regard to the risks associated with fractures of the patella during the harvest, demand full consideration. Postoperative imaging with CT may identify abnormalities in patients who are otherwise asymptomatic.
Keywords: ACL reconstruction, quadriceps tendon, patella, graft harvest
An autogenous quadriceps tendon is a versatile graft option for anterior cruciate ligament (ACL) reconstruction. Since Blauth2 first described the quadriceps tendon as a graft for ACL reconstruction, various modifications to the technique have been described that demonstrate this graft’s versatility to address the unique needs of each case. Initial descriptions of the use of the quadriceps tendon for ACL reconstruction included the harvest of a bone block from the superior pole of the patella2,6,13,17; however, subsequent publications of the quadriceps tendon harvest describe a graft consisting of soft tissue alone. This graft may be used for single-bundle or double-bundle ACL reconstruction and is also an option for revision ACL reconstruction.2,15
The quadriceps tendon is formed by the confluence of the anterior thigh musculature. The central third of this tendon consists primarily of fibers from the rectus femoris and vastus intermedius, resulting in a natural plane, which may be utilized to separate the quadriceps tendon into 2 separate tendons for double-bundle ACL reconstruction. Additionally, imaging studies have demonstrated that the quadriceps tendon thickness doubles that of the patellar tendon.22 Magnetic resonance imaging (MRI) has demonstrated that a quadriceps tendon length of 7 to 8 cm can be consistently obtained, providing an adequate graft length for ACL reconstruction.22
Further studies of biomechanical properties and clinical outcomes are favorable to other autograft options. The biomechanical properties are similar to patellar tendon grafts and are capable of exceeding the properties of the native ACL.7,8,18 Clinical studies comparing quadriceps tendon grafts with patellar tendon grafts have shown biomechanical advantages and favorable clinical outcomes, including a lower incidence of anterior knee pain.10–12,16–19 The objective of this case series was to review surgical considerations for the safe harvest of a quadriceps tendon autograft for use during ACL reconstruction, with a special focus on the risk of patellar fractures.
Methods
Patient Selection
This study involved a series of 57 patients undergoing ACL reconstruction with a quadriceps tendon autograft at our institution from March 2011 through December 2012. These patients were enrolled as participants in a separate randomized clinical trial, funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), to compare single-bundle versus double-bundle ACL reconstruction. Inclusion criteria for this study required age 14 to 50 years, with a rupture of both bundles of the ACL, scheduled ACL reconstruction within 1 year of injury, participation in level 1 (eg, football, basketball, soccer) or level 2 (eg, racquet sports, skiing, manual labor) activities for more than 100 hours per year, willingness to participate in follow-up regardless of relocation, tibial and femoral insertion sites measuring 14 to 18 mm, and a notch width at least 12 mm as measured at the time of surgery. Patients were excluded from participation if there was a history of surgery on the involved or uninvolved knee, open physes, greater than grade 1 concomitant ligament knee injuries, full-thickness articular cartilage injuries, degenerative changes of the quadriceps tendon on MRI or a measurement less than 7 mm thick, inflammatory arthritis, injuries preventing participation in level 1 or level 2 activities, or plans to become pregnant within the 2-year follow-up period. Before participation in the clinical trial, all patients signed an informed consent form approved by the institutional review board at our institution. Postoperative anteroposterior and lateral radiographs were obtained at the initial postoperative visit as the standard of care. Helical computed tomography (CT) with a 1.25-mm slice thickness was performed 6 months after surgery as part of the research protocol to create bone and cartilage models that were necessary for the accurate assessment of knee kinematics and joint contact mechanics.
Surgical Technique
Patients were positioned supine in an arthroscopic leg holder. A longitudinal incision was made following the central axis of the tendon to a point 1 cm distal to the superior pole of the patella with the knee flexed. Hemostasis was obtained during exposure to maintain optimal visualization during the graft harvest. Skin flaps were developed to expose the full extent of the quadriceps tendon to the superior pole of the patella. The central fibers were followed to the insertion on the superior pole of the patella. A 10 mm–wide segment of the central quadriceps tendon was incised with a No. 10 blade to a depth of 7 to 8 mm.
A bone block measuring 18 to 20 mm long by 10 mm wide was harvested. The longitudinal incisions from the central quadriceps tendon were extended over the anterior patella to produce a planned 10 mm–wide bone block. An oscillating saw was utilized to create longitudinal and transverse cuts no deeper than 8 to 10 mm in the superior pole of the patella. The bone block was then freed from the superior pole of the patella with a quarter-inch osteotome. The tendon was released proximally at least 6 cm proximal to the superior pole of the patella. Routine bone grafting of the patellar defect was not performed.
Results
The cohort consisted of 57 patients with advanced imaging at 6 months postoperatively. Two intraoperative fractures were identified (3.5%). Two additional fractures were identified on advanced imaging as part of the research protocol, and 1 fracture occurred during strength testing 6 months after surgery. Over the full duration of the study, a patellar fracture occurred in 5 of the 57 (8.8%) patients who met the study eligibility criteria.
Data at 24-month follow-up were available for 51 patients (89.5%). The 24-month International Knee Documentation Committee (IKDC) subjective knee form scores for the 5 patients with a patellar fracture were 91.95, 91.95, 100.00, 100.00, and 64.37 (mean, 89.66 ± 14.70 [range, 64.37-100.00]). For the remaining 46 patients without a patellar fracture the mean IKDC score at 24-month follow-up was 89.81 ± 10.29 (range, 55.17-100.00). The Wilcoxon rank-sum test between the groups resulted in a P value of .56.
A review of this cohort provided information to establish criteria to identify patients at risk for patellar fractures (Table 1). The following is a case-by-case summary of the 5 patients who sustained a patellar fracture after ACL reconstruction with a quadriceps tendon autograft with a bone block harvested from the superior pole of the patella.
TABLE 1.
Potential Risk Factors for a Patellar Fracture After Quadriceps Tendon Harvest
|
Patient 1
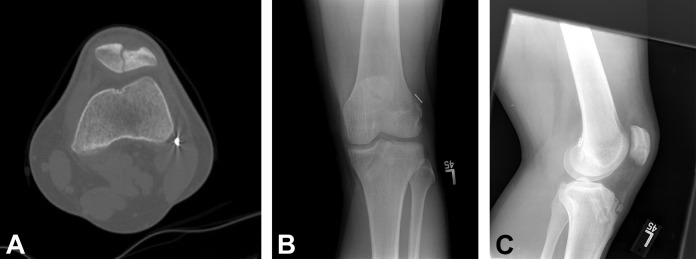
A 24-year-old male patient underwent ACL reconstruction in June 2011 with a quadriceps tendon autograft with a bone block measuring 18 mm long by 11 mm wide. Postoperative radiographs demonstrated no fracture, and the patient progressed through postoperative rehabilitation without incidence. He returned to full activities 6 months after surgery. CT was performed at 6 months as part of research procedures and demonstrated a subacute, nondisplaced fracture (Figure 1). The patient had no clinical sequelae and returned to full activities. Eighteen months after ACL reconstruction, he sustained a direct impact to the knee and noted tenderness and swelling. On examination, he had no effusion and a strong quadriceps contraction and could perform straight-leg raises without a lag. He was mildly tender at the quadriceps tendon insertion. Follow-up imaging including plain radiographs and MRI demonstrated healing of the prior fracture, unchanged from imaging performed at 6-month follow-up. Strength testing 24 months after surgery revealed no pain or objective weakness. The patient’s IKDC score at that time was 91.95, and he had returned to full activities.
Figure 1.
Computed tomography scan of patient 1 demonstrating an occult fracture at 6-month follow-up.
Patient 2
Patient 2 was an 18-year-old male football player who sustained a noncontact knee injury. He underwent ACL reconstruction in August 2011 with a quadriceps tendon autograft with a bone plug that measured 20 mm long and 10 mm wide. He progressed through postoperative rehabilitation uneventfully. Routine postoperative CT was performed as per the study protocol 6 months after ACL reconstruction. CT demonstrated prominent bony overgrowth of the lateral patella at the vastus lateralis insertion, representing heterotopic ossification or a periosteal reaction at an occult fracture site. Follow-up radiographs demonstrated ossification at the lateral insertion of the quadriceps tendon on the patella. He noted occasional knee pain. His patella was nontender with symmetric mobility. He has returned to playing competitive football without functional limitations. At the 24-month research visit, his IKDC score was 91.95.
Patient 3
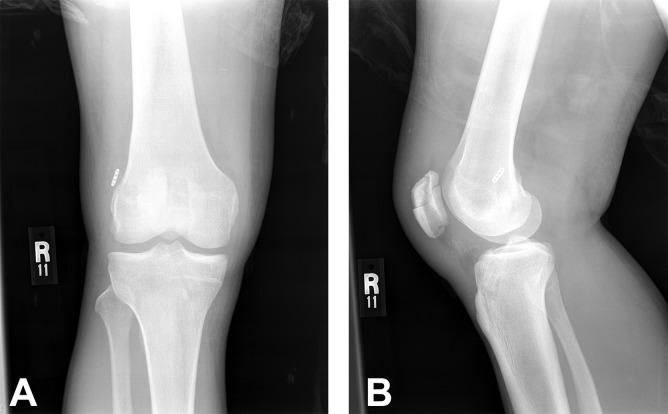
Patient 3 was a 17-year-old male football and volleyball player who injured his left knee after a contact injury during a football game. He underwent ACL reconstruction with a quadriceps tendon autograft with a 20-mm by 11-mm bone block in October 2011. He progressed well through his postoperative rehabilitation. Six months after surgery, he was preparing to return to sport activities and underwent isometric strength testing with a Biodex isokinetic dynamometer with the knee flexed to 75° to determine his readiness for return to sports. During a maximal isometric contraction of the quadriceps, the patient felt a pop, and pain was experienced anteriorly over the patella. Imaging demonstrated an oblique, nondisplaced patellar fracture of the superior pole of the patella (Figure 2). The fracture was treated nonoperatively with immobilization in full extension for 8 weeks and went on to heal clinically and radiographically. He returned to full participation in football and volleyball in August 2012. At the 24-month study visit, his IKDC score was 100.00.
Figure 2.
(A) Computed tomography scan and (B) anteroposterior and (C) lateral radiographs of patient 3 after strength testing at 6-month follow-up.
Patient 4
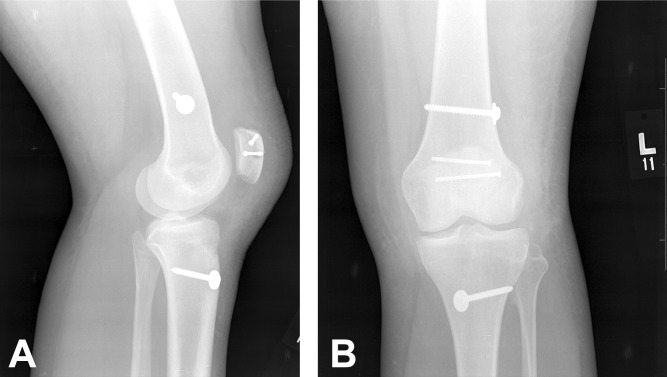
Patient 4 was a 25-year-old man who sustained a complete rupture of his ACL after a noncontact injury to his right knee while playing soccer. He underwent ACL reconstruction in November 2011 with a quadriceps tendon autograft including a bone block measuring 20 mm long by 10 mm wide. Intraoperatively, no fracture was apparent. At his first follow-up visit, postoperative anteroposterior and lateral radiographs were obtained and revealed a nondisplaced fracture at the donor site within the superior pole of the patella (Figure 3). The fracture was treated nonoperatively, with immobilization in full extension for 4 weeks, at which time there was no displacement of the fracture. Range of motion was limited for an additional 2 weeks. The fracture showed radiographic healing at the 6-month follow-up visit. At 8 months postoperatively, the patient had no symptoms and had returned to full activities, participating in recreational sports without issue. At the 24-month research visit, the patient’s IKDC score was 100.00.
Figure 3.
(A) Anteroposterior and (B) lateral radiographs of patient 4 after strength testing at 6-month follow-up.
Patient 5
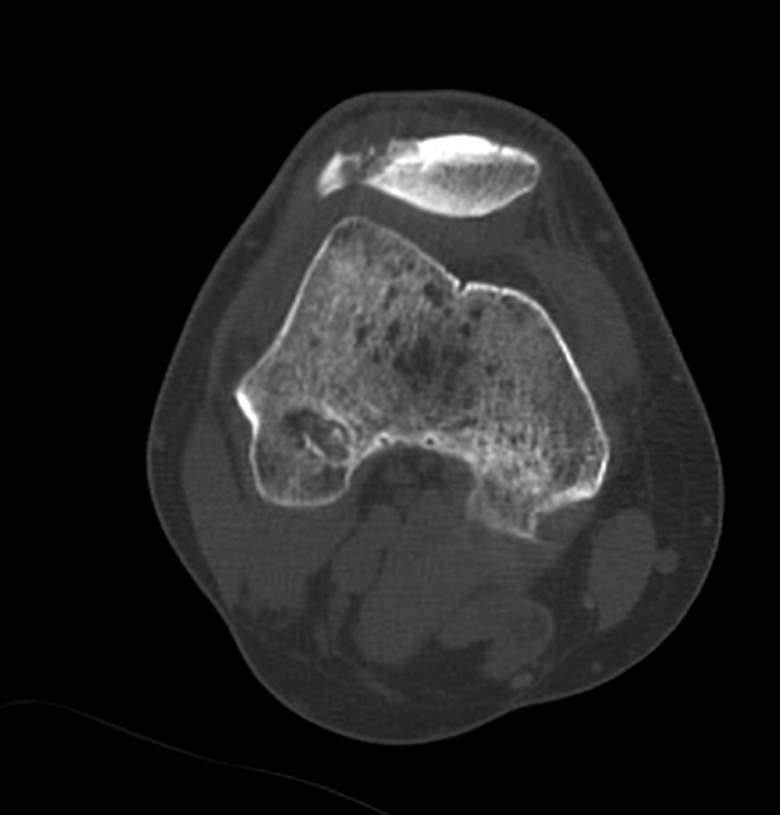
A 17-year-old female patient sustained a noncontact injury in her left knee while playing softball. ACL reconstruction of the left knee was performed in June 2012, during which a 10 mm–wide by 20 mm–long bone block was harvested. A nondisplaced fracture was identified as the bone plug was freed from the superior pole of the patella; the fracture line extended to the lateral cortex of the patella. The quadriceps tendon was released from its insertion on the bone block/superior pole of the patella, and the soft tissue graft was utilized for ACL reconstruction. The bone block remained in situ and was fixed using a standard fracture management technique using two 3.0-mm screws in a lateral-to-medial direction (Figure 4). Postoperatively, the patient’s brace was locked in extension for 2 weeks, and flexion was limited until 6 weeks, at which point unrestricted motion was allowed. She achieved full range of motion by 3 months postoperatively, with clinical and radiographic signs of healing of her patellar fracture. At 24-month follow-up, she had discomfort with standing for prolonged periods of time at work. She did not require the removal of hardware. Her IKDC score at the 24-month research visit was 64.37.
Figure 4.
(A) Anteroposterior and (B) lateral radiographs of patient 5 after fixation of a patellar fracture.
Discussion
In this series of 57 patients who were recruited to participate in a NIAMS-funded clinical trial, the incidence of intraoperative patellar fractures was 3.5%. Three-dimensional CT and MRI were performed at 6 months as part of the research protocol. Over the duration of the study, the incidence of patellar fractures increased to 8.8%. By including 3-dimensional imaging in the postoperative evaluation, we were able to obtain an increased sensitivity for detecting the consequences of harvesting a patellar bone block for a quadriceps tendon graft that otherwise would have not been detected. Two of the 5 fractures identified in this cohort were only identified by the 3-dimensional CT imaging. These patients were asymptomatic and did not require modification of their postoperative rehabilitation. The 24-month IKDC scores for both of these patients were 91.95, while the mean IKDC score for patients without a fracture was 89.81. However, these fractures require consideration for further studies examining a quadriceps tendon autograft with a bone block.
Lee et al11 reported the outcomes of the harvest of a quadriceps tendon with a bone block in a cohort of 247 patients with a minimum 24-month follow-up. A 10 mm–wide bone block was harvested for all patients. Three patients in their cohort had a patellar fracture involving the donor site for the graft harvest. One patient developed a longitudinal, nondisplaced patellar fracture after a fall on the operative knee 5 months after surgery and was treated nonoperatively. Two fractures occurred intraoperatively and were treated by internal fixation with 4.0-mm cannulated screws. The postoperative rehabilitation was not modified for these patients. Three-dimensional imaging was not routinely performed for all patients within this cohort to evaluate for complications related to the patellar donor site.4 Cross-sectional imaging may have identified occult fractures in asymptomatic patients, as was demonstrated in the present study.
The utilization of the quadriceps tendon as an autograft for ACL reconstruction has gained attention recently. A recent systematic review demonstrated similar clinical outcomes for the Lachman and pivot-shift tests between the quadriceps tendon and more commonly used graft options.14 The risks associated with the quadriceps tendon graft harvest have not been as clearly outlined as for other graft options for ACL reconstruction. Numerous outcome studies exist on ACL reconstruction with hamstring and patellar tendon autografts, allowing surgeons to better understand the potential risks associated with these graft options.
The incidence of patellar fractures has been more extensively studied after the harvest of a bone–patellar tendon–bone autograft. The reported risk of patellar fractures after the harvest of this type of graft ranges from 0.2% to 1.8%.3,21 Most studies examining fractures after the patellar tendon autograft harvest include larger cohorts than those reported for quadriceps tendon autografts.
In 2008, Lee et al9 reported on 1725 patellar tendon harvests with a disruption of the extensor mechanism in 3 patients. Stein et al20 reported on a cohort of 618 patients undergoing a patellar tendon graft harvest with a 1.3% incidence rate of patellar fractures. A mean follow-up of 4 years in patients with a patellar fracture showed a mean Lysholm score of 89.6.20 These studies, however, did not perform routine cross-sectional imaging and may not have identified asymptomatic fractures.
During the graft harvest within the current study group, a uniform graft was obtained to minimize variation among patients enrolled in the clinical trial. A standardized graft measuring 10 to 11 mm in diameter with a bone plug 18 to 20 mm in length was used for all patients. Additionally, the location of the graft harvest was determined by the insertion of the central fibers of the quadriceps tendon. Fulkerson and Langeland6 recently demonstrated that the central fibers of the quadriceps tendon insert eccentrically on the patella. This insertion is most commonly in a lateral position.6 Care to harvest the bone block from a central position is necessary, as a bone block positioned too medially or, more commonly, too laterally may lead to an insufficient bone bridge and increases the risk of fractures. Additionally, the depth of the patellar harvest site may influence the risk of fractures. The patella has a nonuniform geometry, and a bone block harvest should be individualized to the patient’s anatomy. Computerized modeling has demonstrated that a lateral harvest site and depth greater than 30% of the patella result in a diminished bone bridge that may be associated with an increased risk of patellar fractures.5
Bone grafting the patellar defect may provide clinical benefits to improve patient outcomes. Akoto and Hoeher1 reported on a series of 30 patients undergoing ACL reconstruction with bone grafting of the patellar defect from a quadriceps autograft. This series reported good functional outcomes at 1-year follow-up. Bone grafting the patellar defect may improve patient outcomes after an autograft harvest and reduce the incidence of late fractures in these patients.
A review of the patients involved in this study aimed to identify risk factors for a patellar fracture after the harvest of a patellar bone block (see Table 1). In this cohort, patellar fractures occurred in those with a harvest of the bone plug from the lateral portion of the patella and in those in which the depth of the harvest was greater than 50% of the depth of the patella. In addition to the 5 patients who had a patellar fracture, a review of postoperative radiographs and CT and MRI scans obtained for research purposes 6 months after surgery revealed that an additional 5 patients had a harvest of a bone plug that was greater than 50% of the thickness of the patella or too lateral. These findings were only detectable by CT. None of these patients have suffered a patellar fracture or have limitations due to patellar symptoms.
After a review of patients enrolled in the study, modifications to the graft harvest were introduced to minimize the risk of fractures (Table 2). These modifications included harvesting the bone plug from the central region of the superior pole of the patella, bone grafting the patellar defect, and limiting the depth of the bone harvest to less than 50% of the patellar depth, with a shorter bone plug length (less than 50% of the length of the patella). Longitudinal cuts were angled centrally to produce a trapezoidal bone block with less deep cancellous bone removal. Finally, the bone graft obtained from the tibial tunnel was used to fill the patellar defect. Recent studies have demonstrated that thinner bone bridges are associated with an increased risk of fractures, and these modifications assist in maximizing the bone bridge at the harvest site.5
TABLE 2.
Modifications to Bone Block Harvest to Reduce the Risk of Fractures
|
Since making the modifications to the procedures for the harvest of the patellar bone block, we have continued to selectively perform ACL reconstruction using a quadriceps tendon graft with a patellar bone plug when the soft tissue length of the graft is less than 7 cm. The harvest of a quadriceps tendon autograft with a bone block has been performed on an additional 40 patients, and no further patellar fractures have occurred.
The presented data are subject to some important limitations. Specifically, the data presented are relevant to a case series and subject to all limitations inherent in this study design. This study included patients from a randomized controlled trial. All patients from that cohort were included regardless of symptoms or the presence of a patellar fracture. Patients in a randomized controlled trial may not generalize to clinical practice. Further limitations of this study include a relatively small sample size of 57 patients.
Conclusion
The quadriceps tendon is a versatile graft for utilization in ACL reconstruction. The biomechanical properties may be superior to more common autograft options and approximate those of the native ACL. A patellar fracture occurred in 8.8% of patients with a quadriceps tendon autograft with a bone block in this study. Two of 5 fractures were identified intraoperatively. Late, nondisplaced fractures can be treated nonoperatively. Precautions need to be taken to minimize the risk of patellar fractures. In patients who experience a patellar fracture after a bone block harvest, clinical outcomes are not significantly different from patients without a fracture at 2-year follow-up. Postoperative imaging with CT may identify abnormalities in patients who are otherwise asymptomatic. Further studies are necessary to elucidate clinical outcomes after ACL reconstruction with a quadriceps tendon autograft.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was supported in part by funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (grant AR056630-01A2). S.J.R. has received educational funding from Mid-Atlantic Surgical Systems. R.V.W. has received speaking fees from Arthrex. AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Pittsburgh Institutional Review Board (No. REN14030002).
References
- 1. Akoto R, Hoeher J. Anterior cruciate ligament (ACL) reconstruction with quadriceps tendon autograft and press-fit fixation using an anteromedial portal technique. BMC Musculoskelet Disord. 2012;13:161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Blauth W. [A new drill template for the operative treatment of injuries of the anterior cruciate ligament]. Unfallheilkunde. 1984;87(11):463–466. [PubMed] [Google Scholar]
- 3. Christen B, Jakob RP. Fractures associated with patellar ligament grafts in cruciate ligament surgery. J Bone Joint Surg Br. 1992;74(4):617–619. [DOI] [PubMed] [Google Scholar]
- 4. DeAngelis JP, Fulkerson JP. Quadriceps tendon: a reliable alternative for reconstruction of the anterior cruciate ligament. Clin Sports Med. 2007;26(4):587–596. [DOI] [PubMed] [Google Scholar]
- 5. Ferrer GA, Miller RM, Murawski CD, et al. A quantitative analysis of the patella following the harvest of a quadriceps tendon autograft with a bone block. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2899–2905. [DOI] [PubMed] [Google Scholar]
- 6. Fulkerson JP, Langeland R. An alternative cruciate reconstruction graft: the central quadriceps tendon. Arthroscopy. 1995;11(2):252–254. [DOI] [PubMed] [Google Scholar]
- 7. Harris NL, Smith DA, Lamoreaux L, Purnell M. Central quadriceps tendon for anterior cruciate ligament reconstruction, part I: morphometric and biomechanical evaluation. Am J Sports Med. 1997;25(1):23–28. [DOI] [PubMed] [Google Scholar]
- 8. Herbort M, Tecklenburg K, Zantop T, et al. Single-bundle anterior cruciate ligament reconstruction: a biomechanical cadaveric study of a rectangular quadriceps and bone--patellar tendon--bone graft configuration versus a round hamstring graft. Arthroscopy. 2013;29(12):1981–1990. [DOI] [PubMed] [Google Scholar]
- 9. Lee G, McCulloch P, Cole BJ, Bush-Joseph CA, Bach BR. The incidence of acute patellar tendon harvest complications for anterior cruciate ligament reconstruction. Arthroscopy. 2008;24(2):162–166. [DOI] [PubMed] [Google Scholar]
- 10. Lee JK, Lee S, Lee MC. Outcomes of anterior cruciate ligament reconstruction using quadriceps tendon autograft. Am J Sports Med. 2016;44(9):2323–2329. [DOI] [PubMed] [Google Scholar]
- 11. Lee S, Seong SC, Jo CH, Han HS, An JH, Lee MC. Anterior cruciate ligament reconstruction with use of autologous quadriceps tendon graft. J Bone Joint Surg Am. 2007;89(suppl 3):116–126. [DOI] [PubMed] [Google Scholar]
- 12. Lee S, Seong SC, Jo H, Park YK, Lee MC. Outcome of anterior cruciate ligament reconstruction using quadriceps tendon autograft. Arthroscopy. 2004;20(8):795–802. [DOI] [PubMed] [Google Scholar]
- 13. Lippe J, Armstrong A, Fulkerson JP. Anatomic guidelines for harvesting a quadriceps free tendon autograft for anterior cruciate ligament reconstruction. Arthroscopy. 2012;28(7):980–984. [DOI] [PubMed] [Google Scholar]
- 14. Mulford JS, Hutchinson SE, Hang JR. Outcomes for primary anterior cruciate reconstruction with the quadriceps autograft: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2013;21(8):1882–1888. [DOI] [PubMed] [Google Scholar]
- 15. Rabuck SJ, Musahl V, Fu FH, West RV. Anatomic anterior cruciate ligament reconstruction with quadriceps tendon autograft. Clin Sports Med. 2013;32(1):155–164. [DOI] [PubMed] [Google Scholar]
- 16. Slone HS, Romine SE, Premkumar A, Xerogeanes JW. Quadriceps tendon autograft for anterior cruciate ligament reconstruction: a comprehensive review of current literature and systematic review of clinical results. Arthroscopy. 2015;31(3):541–554. [DOI] [PubMed] [Google Scholar]
- 17. Staubli HU, Jakob RP. Central quadriceps tendon for anterior cruciate ligament reconstruction, part I: morphometric and biochemical evaluation. Am J Sports Med. 1997;25(5):725–727. [PubMed] [Google Scholar]
- 18. Staubli HU, Schatzmann L, Brunner P, Rincon L, Nolte LP. Mechanical tensile properties of the quadriceps tendon and patellar ligament in young adults. Am J Sports Med. 1999;27(1):27–34. [DOI] [PubMed] [Google Scholar]
- 19. Staubli HU, Schatzmann L, Brunner P, Rincon L, Nolte LP. Quadriceps tendon and patellar ligament: cryosectional anatomy and structural properties in young adults. Knee Surg Sports Traumatol Arthrosc. 1996;4(2):100–110. [DOI] [PubMed] [Google Scholar]
- 20. Stein DA, Hunt SA, Rosen JE, Sherman OH. The incidence and outcome of patella fractures after anterior cruciate ligament reconstruction. Arthroscopy. 2002;18(6):578–583. [DOI] [PubMed] [Google Scholar]
- 21. Viola R, Vianello R. Three cases of patella fracture in 1,320 anterior cruciate ligament reconstructions with bone-patellar tendon-bone autograft. Arthroscopy. 1999;15(1):93–97. [DOI] [PubMed] [Google Scholar]
- 22. Xerogeanes JW, Mitchell PM, Karasev PA, Kolesov IA, Romine SE. Anatomic and morphological evaluation of the quadriceps tendon using 3-dimensional magnetic resonance imaging reconstruction: applications for anterior cruciate ligament autograft choice and procurement. Am J Sports Med. 2013;41(10):2392–2399. [DOI] [PubMed] [Google Scholar]