Abstract
Background
Firefighter first responders dispatched in parallel with emergency medical services (EMS) personnel for out‐of‐hospital cardiac arrests (OHCA) can provide early defibrillation to improve survival. We examined whether survival following first responder defibrillation differed according to driving distance from nearest fire station to OHCA site.
Methods and Results
From the CARES (Cardiac Arrest Registry to Enhance Survival) registry, we identified non‐EMS witnessed OHCAs of presumed cardiac cause from 2010 to 2014 in Durham, Mecklenburg, and Wake counties, North Carolina. We used logistic regression to estimate the association between calculated driving distances (≤1, 1–1.5, 1.5–2, and >2 miles) and survival to hospital discharge following first responder defibrillation compared with defibrillation by EMS personnel. In total, 5020 OHCAs were included in the study. First responders more often applied the first automated external defibrillators at the shortest distances (≤1 mile) versus longest distances (>2 miles) (53.4% versus 46.6%, respectively, P<0.001). When compared with EMS defibrillation, first responder defibrillation within 1 mile and 1 to 1.5 miles of the nearest fire station was associated with increased survival to hospital discharge (odds ratio 2.01 [95% confidence interval 1.46–2.78] and odds ratio 1.61 [95% confidence interval 1.10–2.35], respectively). However, at the longest distances (1.5–2.0 and >2.0 miles), survival following first responder defibrillation did not differ from EMS defibrillation (odds ratio 0.77 [95% confidence interval 0.48–1.21] and odds ratio 0.97 [95% confidence interval 0.67–1.41], respectively).
Conclusions
Shorter driving distance from nearest fire station to OHCA location was associated with improved survival following defibrillation by first responders. These results suggest that the location of first responder units should be considered when organizing prehospital systems of OHCA care.
Keywords: driving distance, early defibrillation, firefighter, first responder, out‐of‐hospital cardiac arrest
Subject Categories: Cardiopulmonary Resuscitation and Emergency Cardiac Care, Sudden Cardiac Death
Clinical Perspective
What Is New?
This study examined whether shorter driving distances to fire stations was associated with improved survival following first responder defibrillation of out‐of‐hospital cardiac arrests where firefighters function as first responders.
The study included 5020 out‐of‐hospital cardiac arrests, and first responder defibrillation within 1 mile and 1 to 1.5 miles of nearest fire station was associated with increased survival (odds ratio 2.01 and odds ratio 1.61, respectively) when compared with emergency medical services defibrillation.
At longer distances, survival following first responder defibrillation did not differ from emergency medical services defibrillation.
What Are the Clinical Implications?
The importance of the location of first responder units and optimal travel distance in order to provide effective early defibrillation should be considered when organizing prehospital systems of out‐of‐hospital cardiac arrest care.
Future studies should examine how first responder initiatives could be combined with placement of publicly available onsite automated external defibrillators to optimize early defibrillation in different locations of out‐of‐hospital cardiac arrest.
Defibrillation of out‐of‐hospital cardiac arrest (OHCA) patients by automated external defibrillators (AEDs) before the arrival of an ambulance has the potential to increase survival for those with shockable rhythms to 74%.1, 2, 3 However, the high survival rates following early defibrillation are highly dependent on early defibrillation within 3 to 5 minutes after OHCA.3 Furthermore, the longer the delay before the application of a defibrillator, the higher the risk that an initial shockable rhythm has deteriorated to a nonshockable rhythm, limiting the potential benefit of defibrillators and decreasing the chances of survival.4, 5, 6 First responders who travel to an OHCA site equipped with AEDs have the potential to provide AED coverage in areas not easily covered by onsite AEDs, including residential locations.7, 8 Implementation of first responders as a supplement to resuscitation performed by layperson bystanders and emergency medical services (EMS) personnel has been associated with improvements in early defibrillation, cardiopulmonary resuscitation (CPR), and survival following OHCA.7, 9, 10, 11 However, limited knowledge is available about the relationship between distance from the OHCA location to the first responder location (fire stations), including how this distance may influence outcomes. Understanding this relationship is important for communities attempting to implement first responder programs, as recommended by the Institute of Medicine.12
In North Carolina, firefighter first responders have been integrated in the emergency care system available for dispatch in parallel with the EMS in the event of medical emergencies, including OHCAs.9, 13 In nearly all cases, the firefighters are dispatched from their home fire station. In this study, we examined the association between driving distance from the nearest fire station to the OHCA site and survival and favorable neurological outcome following first responder defibrillation.
Methods
Study Design, Setting, and OHCAs
Using the CARES (Cardiac Arrest Registry to Enhance Survival) registry, we included OHCAs from 2010 to 2014 from Durham, Mecklenburg, and Wake counties in North Carolina, United States. Each of the 3 counties have a major city (Durham, Charlotte, and Raleigh, respectively) as well as suburban and rural areas. In 2014, the 3 counties had a total population of 2 203 435 inhabitants covering 22.6% of the population in North Carolina.14
The CARES registry has been described previously.15, 16 In summary, the CARES registry contains OHCA information collected from the 911 call centers, EMS, and receiving hospital. Overall, the registry includes exact geographic locations of 97% of the OHCAs.9 For this study the following information was included: age, sex, who were the first to apply an AED and potentially defibrillate the patient, who initiated CPR, initial cardiac rhythm, location of OHCA, witnessed or unwitnessed status, status at hospital arrival, time to defibrillation, EMS and first responder response times, and hospital data (survival to hospital discharge and Cerebral Performance Score at hospital discharge). For all 3 study counties, a complete case capture was available during the study period.9 This project was conducted under the approval of the Duke Institutional Review Board, with a waiver for informed patient consent.
The data used in this study will not be made publicly available to other researchers for purposes of reproducing the results or replicating the procedure. The CARES surveillance group needs to accept any use of the study data.
Fire Stations
Information on the location of each fire station with firefighter first responders in Durham, Wake, and Mecklenburg was collected from online publicly available databases and reviewed in collaboration with fire department administrators. Fire stations not operational in the study period were excluded. Fire stations that became operational or were closed during the study period were only considered for the time they were operational. Furthermore, only fire stations staffed with firefighters 24 hours per day and 7 days per week were considered in this study (Table S1).
Socioeconomic Characteristics in Different Locations
North Carolina census tract information from the Census 2010 and the American Community Survey 2010–2014 was collected for each cardiac arrest in the CARES data set including rate of unemployment, the poverty rate, and racial distributions to evaluate the neighborhood characteristics for each OHCA.17
EMS and First Responders
For the CARES registry, EMS personnel are defined as personnel who respond to medical emergencies as an official capacity (eg, respond to 911 calls) as part of an organized medical response team and who is the designated transporter of the involved patient to the receiving hospital. In the study areas, EMS is provided by independent EMS agencies that are unrelated to the fire department stations. EMS units are often dispatched while mobile or utilizing flexible deployment strategies. CARES does not record the ambulance location at the time of dispatch. First responders are personnel who are called to the emergency scene by emergency medical dispatch centers as an organized team, but who are not the designated transporter of the involved patient to the receiving hospital.9, 18 The EMS ambulance response units are usually distributed to different locations on county road networks to ensure a low average response time. During the study period, the firefighter first responders in Durham County responded from a fire station in 96% of all dispatches. This average included 94% of dispatches during daytime and 98% of dispatches during nighttime (Durham County Fire Department, unpublished data, 2016).
Outcomes
The primary outcome measure was survival to hospital discharge. The secondary outcome was survival with a favorable neurological outcome defined as cerebral performance category 1 or 2 at hospital discharge. Category 1 represented full recovery or mild disability and 2 represented moderate disability but ability to function independently in activities of daily living.19
Statistics
Categorical variables were presented as counts and percentages, and continuous variables as medians with first and third quartiles (Q1–Q3). To test for differences between discrete categorical variables, a χ2 test was used. For comparison of medians, we used the Kruskal–Wallis rank‐sum test.
For each OHCA in the 3 study counties, the driving distance in miles from the nearest fire station to each OHCA was calculated using the Esri business analyst road network in the ArcGis 10.4.1 Network Analyst extension.20 Figure S1 is an example for Durham County using randomly generated points. The calculated driving distances were divided in 4 groups with cut values at 1, 1.5, and 2 miles. These cut values were selected based on 25th, median, and 75th driving distance percentiles (0.98, 1.46, and 2.12 miles, respectively), and involved distances that were applicable to public policy deliberations. Using logistic regression, the associations between the different driving distances and survival to hospital discharge and a good cerebral performance outcome were estimated. Both crude and adjusted analyses were conducted. The adjusted analysis included age, sex, witnessed arrest status, OHCA location (public or residential), layperson CPR, year of arrest, and neighborhood characteristics (unemployment rate, percentage of white race, or other races, and poverty percentage). Odds ratios with EMS defibrillation as reference were calculated and presented using Forest plots. To evaluate the association between driving distance from the OHCA site location from nearest fire station and outcomes, restricted cubic splines (knots at 1, 1.5, and 2 miles) were used to model the outcome in a logistic regression with driving distance as a continuous variable. Figure S2 is an additional model with spline knots at 10th, median, and 90th percentiles. Trends in survival and favorable neurological outcome at discharge according to driving distances were tested using univariate logistic regression.
We performed a sensitivity analysis where EMS response time was added to the adjusted logistic regression model using multiple imputation with 100 imputed data sets.21
Data management and analyses were performed using SAS 9.4 (SAS Institute Inc) and R.22
Results
In total, we included 5020 OHCAs as the study population (Figure 1). Table shows baseline characteristics according to different driving distances from the nearest fire station to the OHCA site. No differences in age and sex at different distances were observed. Most OHCA patients were male (61.4%). Areas with the shortest distances to OHCAs from fire stations had a higher percentage of poverty and unemployment compared with those with the longest driving distances. Regarding racial distributions, longer distances were associated with higher percentage of whites. At shortest distances from fire stations, OHCAs were more likely to occur in a public location (31.7%) compared with OHCAs at the longest distances (17.9%).
Figure 1.
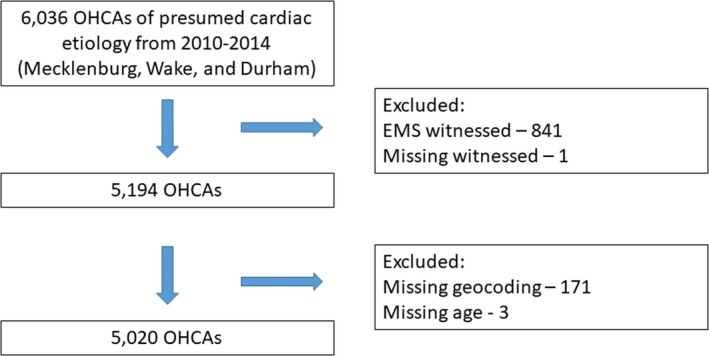
Flowchart showing the out‐of‐hospital cardiac arrest study population. EMS indicates emergency medical service; OHCA, out‐of‐hospital cardiac arrest.
Table 1.
Out‐of‐Hospital Cardiac Arrest Characteristics According to Different Distances From Nearest Fire Station
| Variable | ≤1 mile | 1 to 1.5 miles | 1.5 to 2 miles | >2 miles | Total | P Value |
|---|---|---|---|---|---|---|
| Count, n | 1324 | 1262 | 1009 | 1425 | 5020 | |
| Age, median [Q1–Q3] (y) | 65.0 [53.8, 77.0] | 66.0 [54.0, 78.0] | 66.0 [54.0, 78.0] | 65.0 [54.0, 76.0] | 65.0 [54.0, 77.0] | 0.65 |
| Sex, male | 795 (60.0) | 759 (60.1) | 621 (61.5) | 908 (63.7) | 3083 (61.4) | 0.16 |
| Percent white in local neighborhood, median [Q1–Q3] (%) | 43.8 [20.4, 73.9] | 46.2 [16.5, 70.8] | 49.2 [20.5, 72.3] | 56.4 [29.8, 75.5] | 49.4 [20.6, 73.7] | <0.001 |
| Percent black in local neighborhood, median [Q1–Q3] (%) | 33.7 [12.4, 53.9] | 30.5 [13.2, 55.6] | 26.9 [12.4, 51.2] | 25.3 [10.0, 42.8] | 28.1 [12.2, 50.9] | <0.001 |
| Percent of people in poverty, median [Q1–Q3] (%) | 15.9 [8.4, 28.6] | 18.3 [7.3, 25.8] | 14.0 [7.2, 23.5] | 10.0 [5.1, 18.8] | 14.3 [6.9, 23.6] | <0.001 |
| Percent unemployment, median [Q1–Q3] (%) | 9.1 [6.3, 15.1] | 9.2 [5.3, 14.4] | 9.3 [5.4, 13.7] | 8.2 [5.9, 12.2] | 8.9 [5.8, 13.7] | <0.001 |
| Rural area, population cluster of <2500, N (%) | 17 (1.3) | 18 (1.4) | 28 (2.8) | 136 (9.5) | 199 (4.0) | |
| Urban cluster, population cluster of 2500 to 50 000, N (%) | 22 (1.7) | 10 (0.8) | 5 (0.5) | 12 (0.8) | 49 (1.0) | |
| Urbanized area, population cluster of >50 000, N (%) | 1285 (97.1) | 1234 (97.8) | 976 (96.7) | 1277 (89.6) | 4772 (95.1) | <0.001 |
| Who defibrillated first | ||||||
| Not defibrillated | 894 (67.5) | 879 (69.7) | 676 (67.0) | 929 (65.2) | 3378 (67.3) | |
| LP | 34 (2.6) | 48 (3.8) | 29 (2.9) | 30 (2.1) | 141 (2.8) | |
| FR | 237 (17.9) | 163 (12.9) | 153 (15.2) | 223 (15.6) | 776 (15.5) | |
| EMS | 159 (12.0) | 172 (13.6) | 151 (15.0) | 243 (17.1) | 725 (14.4) | <0.001 |
| Who applied an AED first | ||||||
| EMS | 541 (41.0) | 568 (45.1) | 472 (47.0) | 709 (49.9) | 2290 (45.7) | |
| FR | 705 (53.4) | 576 (45.7) | 480 (47.8) | 662 (46.6) | 2423 (48.4) | |
| LP | 74 (5.6) | 116 (9.2) | 53 (5.3) | 50 (3.5) | 293 (5.9) | <0.001 |
| Missing | 4 | 2 | 4 | 4 | 14 | |
| Who initiated CPR first | ||||||
| EMS | 155 (12.0) | 141 (11.4) | 129 (13.1) | 197 (14.0) | 622 (12.7) | |
| FR | 581 (45.1) | 466 (37.6) | 413 (42.1) | 527 (37.5) | 1987 (40.4) | |
| LP | 553 (42.9) | 633 (51.0) | 439 (44.8) | 681 (48.5) | 2306 (46.9) | <0.001 |
| Missing | 35 | 22 | 28 | 20 | 105 | |
| Layperson CPR | ||||||
| No | 771 (58.2) | 629 (49.8) | 570 (56.5) | 744 (52.2) | 2714 (54.1) | |
| Yes | 553 (41.8) | 633 (50.2) | 439 (43.5) | 681 (47.8) | 2306 (45.9) | <0.001 |
| Witnessed status | ||||||
| Unwitnessed | 780 (58.9) | 750 (59.4) | 589 (58.4) | 763 (53.5) | 2882 (57.4) | |
| Witnessed | 544 (41.1) | 512 (40.6) | 420 (41.6) | 662 (46.5) | 2138 (42.6) | 0.005 |
| Survival until discharge | ||||||
| Yes | 176 (13.3) | 132 (10.5) | 91 (9.0) | 152 (10.7) | 551 (11.0) | |
| No | 1148 (86.7) | 1130 (89.5) | 918 (91.0) | 1273 (89.3) | 4469 (89.0) | 0.008 |
| Status at ED arrival | ||||||
| No pulse at ED arrival | 901 (68.1) | 877 (69.5) | 706 (70.0) | 986 (69.2) | 3470 (69.1) | |
| Pulse at ED arrival | 423 (31.9) | 385 (30.5) | 303 (30.0) | 439 (30.8) | 1550 (30.9) | 0.77 |
| Neurologic status at discharge | ||||||
| Favorable neurological outcome | 158 (11.9) | 118 (9.4) | 74 (7.3) | 133 (9.3) | 483 (9.6) | 0.002 |
| Location | ||||||
| Residential | 904 (68.3) | 904 (71.6) | 834 (82.7) | 1170 (82.1) | 3812 (75.9) | |
| Public | 420 (31.7) | 358 (28.4) | 175 (17.3) | 255 (17.9) | 1208 (24.1) | <0.001 |
| First rhythm | ||||||
| Nonshockable | 1023 (77.3) | 1013 (80.3) | 793 (78.6) | 1079 (75.7) | 3908 (77.8) | |
| Shockable | 301 (22.7) | 249 (19.7) | 216 (21.4) | 346 (24.3) | 1112 (22.2) | 0.03 |
| EMS response time | ||||||
| Median [Q1–Q3] (min) | 6.8 [5.2, 8.9] | 7.2 [5.6, 9.1] | 7.8 [6.2, 9.6] | 8.3 [6.8, 10.4] | 7.6 [5.9, 9.5] | 0.07 |
| Missing values | 91 | 99 | 100 | 127 | 417 | |
| First responders response time | ||||||
| Median [Q1–Q3] (min) | 5.0 [4.0, 6.8] | 5.7 [4.5, 7.2] | 6.5 [5.1, 8.2] | 7.6 [6.2, 9.3] | 6.2 [4.8, 8.0] | 0.006 |
| Missing values | 798 | 781 | 575 | 952 | 3106 | |
| Time to defibrillationa | ||||||
| Median [Q1–Q3] (min) | 9.2 [6.2, 16.4] | 11.0 [7.1, 19.9] | 11.6 [8.0, 20.7] | 11.7 [8.5, 18.2] | 10.9 [7.5, 18.6] | 0.72 |
| Missing values | 99 | 72 | 70 | 142 | 383 | |
| Delay between EMS and first responder dispatch | ||||||
| Median [Q1–Q3] (min) | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.47 |
| Missing values | 804 | 780 | 569 | 958 | 3111 | |
| First responder first arrivals | ||||||
| No | 151 (28.8) | 154 (32.0) | 126 (29.1) | 188 (39.7) | 619 (32.4) | |
| Yes | 374 (71.2) | 327 (68.0) | 307 (70.9) | 285 (60.3) | 1293 (67.6) | <0.001 |
| Missing values | 799 | 781 | 576 | 952 | 3108 | |
| Patients defibrillated within 5 mina | ||||||
| No | 286 (86.4) | 282 (90.7) | 245 (93.2) | 327 (92.4) | 1140 (90.5) | |
| Yes | 45 (13.6) | 29 (9.3) | 18 (6.8) | 27 (7.6) | 119 (9.5) | 0.02 |
| Missing values | 99 | 72 | 70 | 142 | 383 | |
All results are reported as the number of patients (%) unless otherwise specified. AED indicates automated external defibrillator; CPR, cardiopulmonary resuscitation; ED, emergency department; EMS, emergency medical services; FR, first responder; LP, layperson.
Only patients who were defibrillated (n=1642).
For OHCAs within the shortest distances (≤1 mile) to the nearest fire station, first responders more often applied the first AED than at the longest distances (>2 miles) (53.4% versus 46.6%, respectively, P<0.001). At the longest distances, EMS more often applied the first AED (49.9% at longest distances versus 41.0% at shortest distances). CPR performed by laypeople before the arrival of first responders or EMS was more likely at longer distances than shorter distances (P<0.001). At shortest distances, first responders arrived before EMS in 71.2% of cases compared with 60.3% at the longest distances (P<0.001).
We observed faster first responder response times at the shortest distances from fire stations compared with the longest distances (5 minutes [Q1–Q3 4.0–6.8] versus 7.6 minutes [Q1–Q3 6.2–9.3], P=0.006). Trends in EMS response time and time to defibrillation showed a shorter time at the shortest distances from fire stations compared with longest distances.
Overall, there was a limited delay between the dispatch of the first responder compared with EMS personnel.
Survival to Hospital Discharge and Favorable Neurological Outcome at Hospital Discharge
Figure 2A shows the crude and adjusted association between first responder defibrillation at different distances to fire stations and survival to hospital discharge. In crude analysis, first responder defibrillation within 1 mile and 1 to 1.5 miles of nearest fire station was associated with an increased survival to hospital discharge following OHCA when compared with EMS defibrillation (odds ratio [OR] 2.01 [95% confidence interval [CI] 1.46–2.78] and OR 1.61 [95% CI 1.10–2.35], respectively). At the long distances (1.5–2.0 miles and >2.0 miles), survival following first responder defibrillation did not differ from EMS defibrillation (OR 0.77 [95% CI 0.48–1.21] and OR 0.97 [95% CI 0.67–1.41], respectively). In adjusted analysis, first responder defibrillation remained associated with improved survival within 1 mile and 1 to 1.5 miles compared with EMS defibrillation (OR 1.84 [95% CI 1.30–2.59] and OR 1.52 [95% CI 1.02–2.29], respectively) while no difference between the 2 was observed at 1.5 to 2.0 miles and >2.0 miles (OR 0.72 [95% CI 0.44–1.16] and OR 0.90 [95% CI 0.61–1.33], respectively).
Figure 2.
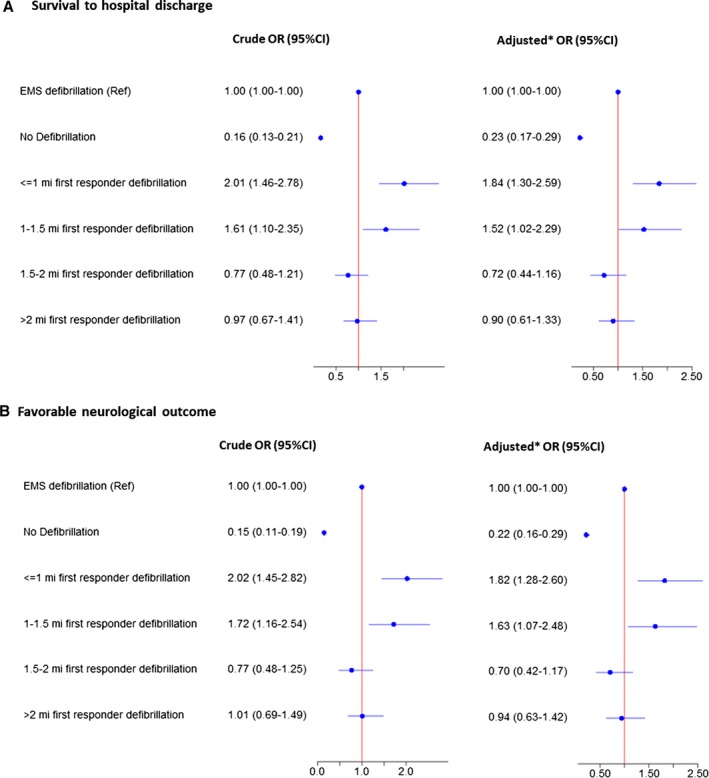
Survival and favorable neurological outcome according to distance to nearest fire station. Odds ratios of survival to discharge after out‐of‐hospital cardiac arrest for patients defibrillated by first responders within 1 mile, 1 to 1.5 miles, 1.5 to 2 miles, and >2 miles, and patients not defibrillated compared with defibrillation by emergency medical services personnel (reference). A, Associations for survival to hospital discharge. B, Associations for a favorable neurological outcome for both unadjusted and adjusted logistic regression analyses. *Adjusted for age, sex, layperson CPR, location of arrest, witnessed arrest status, year of arrest, and neighborhood characteristics (unemployment rate, poverty rate, and percentage of white or other races). CI indicates confidence interval; CPR, cardiopulmonary resuscitation; EMS, emergency medical services; OR, odds ratio.
A sensitivity analysis, with imputed EMS response times, showed similar results. Compared with EMS defibrillation, first responder defibrillation was associated with improved survival within 1 mile and 1 to 1.5 miles (OR 1.97 [95% CI 1.39–2.78] and OR 1.71 [95% CI 1.13–2.58], respectively) with no difference at 1.5 to 2.0 miles and >2.0 miles (OR 0.82 [95% CI 0.50–1.35] and OR 1.07 [95% CI 0.71–1.61], respectively) (Figure S3).
Likewise, for patients with a witnessed arrest and a shockable rhythm, survival following first responder defibrillation (n=398) was higher within 1 mile and 1 to 1.5 miles compared with EMS defibrillation (n=327) (OR 1.98 [95% CI 1.28–3.08] and OR 1.72 [95% CI 1.03–2.87], respectively) while no difference was observed at 1.5 to 2.0 miles and >2.0 miles (OR 0.66 [95% CI 0.37–1.17] and OR 0.99 [95% CI 0.62–1.56], respectively) (Figure S4).
For survival with a favorable neurological outcome, first responder defibrillation was associated with a favorable outcome compared with EMS defibrillation within 1 mile (OR 1.82 [95% CI 1.28–2.60]) and 1 to 1.5 miles (OR 1.63 [95% CI 1.07–2.48]) of the nearest fire station in adjusted analysis (Figure 2B).
Figure 3A shows survival to hospital discharge following first responder or EMS defibrillation according to different driving distances from nearest fire station. Survival following first responder defibrillation was significantly higher at shorter distances than longer distances (P=0.001), while survival following EMS defibrillation did not differ according to different driving distances (P=0.58). The results for survival with a favorable neurological outcome showed a similar pattern as survival at hospital discharge (Figure 3B).
Figure 3.
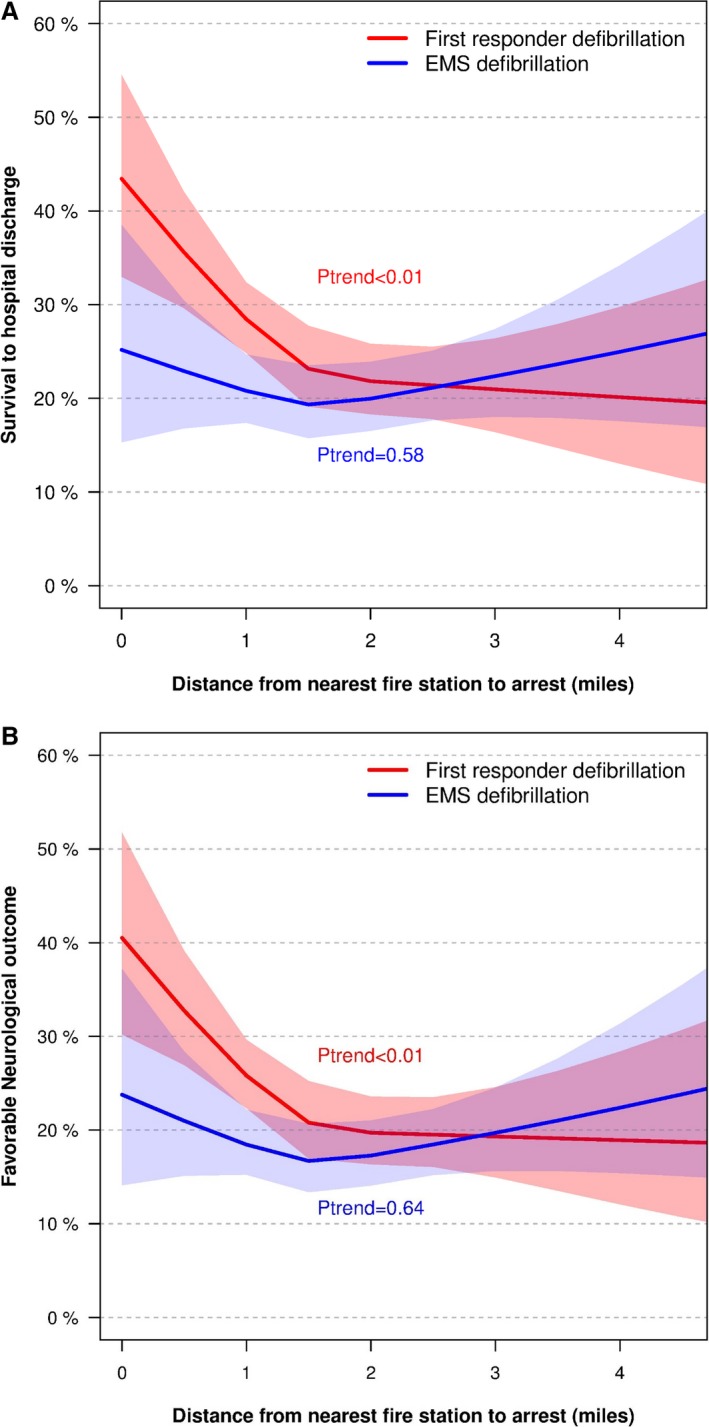
Survival to hospital discharge and favorable neurological outcome following first responder or EMS defibrillation at different driving distances from fire stations to OHCA sites. A, Survival to hospital discharge following first responder defibrillation (n=776) or EMS defibrillation (n=725) at different driving distances from nearest fire station. B, Survival with a favorable neurological outcome following first responder defibrillation (n=776) or EMS defibrillation (n=725) at different driving distances from nearest fire station. Logistic regression with restricted cubic splines (knots at 1, 1.5, and 2 miles) was used to make the models. EMS, emergency medical services; OHCA, out‐of‐hospital cardiac arrest.
Figure 4 shows survival to hospital discharge at different driving distances from fire stations for all OHCAs in the study population. Overall survival was higher at shortest distances compared with the longest distances (P=0.04). There was a trend for greater survival with favorable neurological outcome at shorter driving distances for all OHCA patients (P=0.06) (Figure S5).
Figure 4.
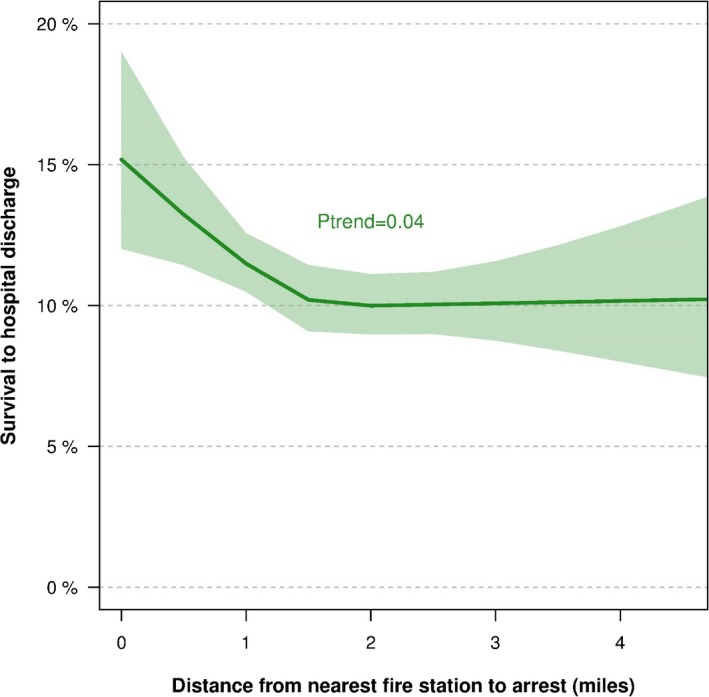
Overall out‐of‐hospital cardiac arrest survival to hospital discharge at different driving distances from fire stations to OHCA sites. Overall survival for all OHCA patients (n=5020) to hospital discharge according to driving distance from nearest fire station to the OHCA site. Logistic regression with restricted cubic splines (knots at 1, 1.5, and 2 miles) was used to make the model. OHCA indicates out‐of‐hospital cardiac arrest.
Discussion
This study showed that OHCA patients within close proximity to fire stations were more likely to be defibrillated by first responders than EMS personnel. Compared with defibrillation by EMS personnel, survival was higher when performed by first responders within a distance of 1.5 miles of the nearest fire station. However, survival following first responder defibrillation did not differ from EMS defibrillation at distances >1.5 miles to fire stations. Furthermore, overall OHCA survival to hospital discharge was higher within shorter distance to an OHCA site from a nearest fire station.
In North Carolina, firefighters function as first responders dispatched to medical emergencies in addition to responding to fire emergencies, doing inspections, and providing education of citizens in local communities. First responder programs have previously included different types of first responders including laypeople, police officers, firefighters, home care providers, and any combination thereof.7, 10, 11, 12, 23 While the use of different first responders for rapid defibrillation has been well described, it is less clear how distance between the OHCA site and a first responder unit may relate to outcomes. In the present study, survival and a favorable neurological outcome following first responder defibrillation were higher within ≈1.5 miles driving distance between the OHCA site and the nearest fire station compared with EMS defibrillation.
In many first responder programs, the first responders are only dispatched in the event of an OHCA.7, 10, 24, 25, 26, 27 Identifying a medical emergency as an OHCA instead of another condition (eg, seizure) can cause a delay before dispatch of first responders who are only dispatched to OHCA events and not other medical emergencies.24, 26, 27, 28, 29 Such delays may potentially reduce the effectiveness of first responders and can be difficult to shorten without increasing the risk of dispatching the first responders to non‐OHCA situations.30 In the present study, a dispatch delay between first responders and EMS personnel was not observed. This could be explained by the fact that the firefighter first responders in North Carolina are dispatched to many medical emergencies (not only OHCAs) to assist and treat the patient before the arrival of EMS, limiting the problem with identifying OHCA cases at dispatch centers. Similarly, rates of first responder arrivals before EMS were high compared with other studies, especially at the shortest distances from fire stations (71.2%).24, 27 The principle of dispatching firefighter first responders to many medical emergencies could explain some of the efficacy of the firefighter first responders in North Carolina and could be considered when organizing prehospital systems of OHCA care.9
All firefighters in North Carolina are educated to perform basic life support and to provide basic treatment in the event of medical emergencies, which is likely to decrease the time before an AED is applied and shock is delivered.31, 32 Finally, the firefighter first responders are available 24 hours a day to respond promptly to fire and medical emergencies and have the option to use a siren when driving, potentially bypassing traffic.
In the present study, EMS were more likely to be the first to defibrillate the patient at longer driving distances than at shorter distances. However, at distances >2 miles first responders were still the first to defibrillate the OHCA patient in almost half of cases. Furthermore, survival following first responder defibrillation at distances >2 miles was comparable to survival following EMS defibrillation. Consequently, our results demonstrate that first responders can still help provide early defibrillation at longer distances, especially in areas with long EMS response times.
Most OHCAs occur in residential locations where survival rates following OHCA are lower than at public locations.33 Other first responder programs have shown that first responders were more likely to arrive before EMS in residential locations, potentially improving outcomes in such locations.7, 26 In our study, OHCAs that were closer to fire stations were more likely to be in public locations than at longer distances to the fire stations. Consequently, the placement of fire stations favored optimal response to OHCAs in public locations, potentially limiting the benefit of first responder defibrillation in residential locations.
Bystander CPR delays the time to when an initial shockable rhythm deteriorates to a nonshockable rhythm that makes defibrillation less likely.5, 6, 34 Thus, prompt initiation of CPR in the event of an OHCA is essential to improve the chance of and efficacy of early defibrillation. In this study, layperson CPR rates were lower for OHCAs within 1 mile of fire stations compared with OHCAs where the distance to the nearest fire station was >1 mile. This could lower the chance of early defibrillation and survival following OHCA. However, our adjusted results did not change our conclusions from the unadjusted logistic regression results. When comparing the layperson CPR rates in the present study with other studies, additional improvements in bystander CPR might be achievable and offer a potential to further increase early defibrillation and improve survival following OHCA.10, 35
Limitations
Several limitations to our study should be considered when interpreting the results. Because of the observational design, associations do not mean causal relations. Furthermore, we cannot exclude residual confounding related to the different driving distances that might affect our results even though our adjusted analysis did not change our conclusions. However, if there was residual confounding, we might expect survival following EMS defibrillation to also differ based on distance from fire stations, which we did not observe.
Our study did not have information on where exactly the firefighters were when they were dispatched to the OHCA sites. However, data from Durham Fire Department showed that the firefighters in most cases (96%) responded from fire stations during the study period. If the location of the firefighter first responders was not at or in close proximity to the different fire stations when dispatched but instead on the road, that would have moved our results towards the null. Consequently, the true association of driving distances of first responders may well be stronger than found in this study.
We did not have information on police officer first responders during the study period. We consulted local EMS authorities, who confirmed that early defibrillation performed by police first responders was minimal during the study period. Again, if early defibrillation by police officers was indeed significant during the study period, that would move our results towards the null as the police officers usually are on the road and not related to fire station locations, similar to EMS personnel.
For this study, only fire stations staffed 24 hours per day and 7 days per week were considered. As such, our results do not necessarily apply to communities covered by volunteer fire departments where the fire stations are not consistently staffed. In such communities, the driving distance optimal ranges for the first responders are likely to be shorter.
Our study had a proportion of missing values on time estimates primarily because of response times being supplemental to the data collection in the CARES registry. An adjusted logistic regression sensitivity analysis with imputed EMS missing response times did not change our conclusions.
Conclusion
Compared with EMS defibrillation, driving distances from nearest fire station to an OHCA site shorter than 1.5 miles were associated with improved survival and a favorable neurological outcome following first responder defibrillation. Furthermore, overall survival following OHCA was higher within 1.5 miles of the nearest fire station. These results highlight the critical role of first responders, and their distances to scenes of cardiac arrests, in the United States. Locations of fire stations and first responder units should be considered when organizing prehospital systems of cardiac arrest care.
Sources of Funding
The present study was supported by the HeartRescue Project, which is funded by the Medtronic Foundation. Dr Steen M. Hansen has received economic support from The Danish Heart Foundation and the Laerdal Foundationer. None of the study sponsors had any role in the design and conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Disclosures
Dr S.M. Hansen has received research grants from the Danish Foundation Trygfonden (significant), the Danish Heart Foundation (significant), and the Laerdal Foundation (significant). Dr C. Torp‐Pedersen has served as a consultant for Cardiome, Merck, Sanofi, Daiichi, and has received grants from Bristol‐Myers Squibb. Dr C. B. Fordyce reported serving on an advisory board for Bayer, Novo Nordisk, Sanofi, and Boehringer Ingelheim. Dr C. M. Hansen reported receiving research grants from the Laerdal Foundation, TrygFonden, and Helsefonden. Dr J. Jollis reported receiving grants from the Medtronic Foundation. Dr C. B. Granger reported receiving grants from the Medtronic Foundation.
Supporting information
Table S1. List of Fire Stations Staffed 24 Hours Per Day and 7 Days Per Week
Figure S1. Map of Durham county with fire stations, simulated out‐of‐hospital cardiac arrests (randomly generated points), and nearest driving distance routes.
Figure S2. Out‐of‐hospital cardiac arrest survival to hospital discharge at different driving distances from fire stations according to whether the patient was defibrillated by first responders or EMS.
Figure S3. Imputation analysis: Out‐of‐hospital cardiac arrest survival following first responder defibrillation at different driving distances from fire stations to OHCA sites compared with EMS defibrillation.
Figure S4. Out‐of‐hospital cardiac arrest survival following first responder defibrillation at different driving distances from fire stations to OHCA sites compared with EMS defibrillation for patients with witnessed arrest and a shockable heart rhythm.
Figure S5. Overall out‐of‐hospital cardiac arrest favorable neurological outcome at different driving distances from fire stations to OHCA sites.
Acknowledgments
The CARES Surveillance Group comprises all members of contributing EMS agencies and hospitals. We appreciate the efforts made by these individuals and organizations to further the understanding of care and outcomes of patients with out‐of‐hospital cardiac arrest. Many thanks to Brandon S. Mitchell for his assistance with validating the fire stations and help with understanding the EMS organizations in the study counties, Maria Ratliff for her dedicated help with providing data on how often the firefighters were dispatched from the fire stations in Durham County, and Brian Frizzelle for his advice on how to conduct the geospatial analyses.
(J Am Heart Assoc. 2018;7:e008771 DOI: 10.1161/JAHA.118.008771.)
References
- 1. Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med. 2002;347:1242–1247. [DOI] [PubMed] [Google Scholar]
- 2. Page RL, Joglar JA, Kowal RC, Zagrodzky JD, Nelson LL, Ramaswamy K, Barbera SJ, Hamdan MH, McKenas DK. Use of automated external defibrillators by a U.S. airline. N Engl J Med. 2000;343:1210–1216. [DOI] [PubMed] [Google Scholar]
- 3. Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW, Hardman RG. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343:1206–1209. [DOI] [PubMed] [Google Scholar]
- 4. Renkiewicz GK, Hubble MW, Wesley DR, Dorian PA, Losh MJ, Swain R, Taylor SE. Probability of a shockable presenting rhythm as a function of EMS response time. Prehosp Emerg Care. 2014;18:224–230. [DOI] [PubMed] [Google Scholar]
- 5. Waalewijn RA, Nijpels MA, Tijssen JG, Koster RW. Prevention of deterioration of ventricular fibrillation by basic life support during out‐of‐hospital cardiac arrest. Resuscitation. 2002;54:31–36. [DOI] [PubMed] [Google Scholar]
- 6. Rajan S, Wissenberg M, Folke F, Hansen SM, Gerds TA, Kragholm K, Hansen CM, Karlsson L, Lippert FK, Køber L, Gislason GH, Torp‐Pedersen C. Association of bystander cardiopulmonary resuscitation and survival according to ambulance response times after out‐of‐hospital cardiac arrest. Circulation. 2016;134:2095–2104. [DOI] [PubMed] [Google Scholar]
- 7. Zijlstra JA, Stieglis R, Riedijk F, Smeekes M, van der Worp WE, Koster RW. Local lay rescuers with AEDs, alerted by text messages, contribute to early defibrillation in a Dutch out‐of‐hospital cardiac arrest dispatch system. Resuscitation. 2014;85:1444–1449. [DOI] [PubMed] [Google Scholar]
- 8. Hansen SM, Hansen CM, Folke F, Rajan S, Kragholm K, Ejlskov L, Gislason G, Køber L, Gerds TA, Hjortshøj S, Lippert F, Torp‐Pedersen C, Wissenberg M. Bystander defibrillation for out‐of‐hospital cardiac arrest in public vs residential locations. JAMA Cardiol. 2017;2:507–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Malta Hansen C, Kragholm K, Pearson DA, Tyson C, Monk L, Myers B, Nelson D, Dupre ME, Fosbøl EL, Jollis JG, Strauss B, Anderson ML, McNally B, Granger CB. Association of bystander and first‐responder intervention with survival after out‐of‐hospital cardiac arrest in North Carolina, 2010–2013. JAMA. 2015;314:255. [DOI] [PubMed] [Google Scholar]
- 10. Blom MT, Beesems SG, Homma PCM, Zijlstra JA, Hulleman M, van Hoeijen DA, Bardai A, Tijssen JGP, Tan HL, Koster RW. Improved survival after out‐of‐hospital cardiac arrest and use of automated external defibrillators. Circulation. 2014;130:1868–1875. [DOI] [PubMed] [Google Scholar]
- 11. Ringh M, Rosenqvist M, Hollenberg J, Jonsson M, Fredman D, Nordberg P, Järnbert‐Pettersson H, Hasselqvist‐Ax I, Riva G, Svensson L. Mobile‐phone dispatch of laypersons for CPR in out‐of‐hospital cardiac arrest. N Engl J Med. 2015;372:2316–2325. [DOI] [PubMed] [Google Scholar]
- 12. Graham R, Mccoy MA, Schultz AM. Strategies to improve cardiac arrest survival: a time to act. Available at: http://iom.nationalacademies.org/Reports/2015/Strategies-to-Improve-Cardiac-Arrest-Survival.aspx. Accessed September 1, 2016. [PubMed]
- 13. Hansen CM, Kragholm K, Granger CB, Pearson DA, Tyson C, Monk L, Corbett C, Nelson RD, Dupre ME, Fosbøl EL, Strauss B, Fordyce CB, McNally B, Jollis JG. The role of bystanders, first responders, and emergency medical service providers in timely defibrillation and related outcomes after out‐of‐hospital cardiac arrest: results from a statewide registry. Resuscitation. 2015;96:303–309. [DOI] [PubMed] [Google Scholar]
- 14. United States Census Bureau. American FactFinder . Available at: https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed February 9, 2017.
- 15. McNally B, Stokes A, Crouch A, Kellermann AL; CARES Surveillance Group . CARES: cardiac arrest registry to enhance survival. Ann Emerg Med. 2009;54:674–683.e2. [DOI] [PubMed] [Google Scholar]
- 16. McNally B, Robb R, Mehta M, Vellano K, Valderrama AL, Yoon PW, Sasson C, Crouch A, Perez AB, Merritt R, Kellermann A; Centers for Disease Control and Prevention . Out‐of‐hospital cardiac arrest surveillance—Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005–December 31, 2010. MMWR Surveill Summ. 2011;60:1–19. [PubMed] [Google Scholar]
- 17. Fosbøl EL, Dupre ME, Strauss B, Swanson DR, Myers B, McNally BF, Anderson ML, Bagai A, Monk L, Garvey JL, Bitner M, Jollis JG, Granger CB. Association of neighborhood characteristics with incidence of out‐of‐hospital cardiac arrest and rates of bystander‐initiated CPR: implications for community‐based education intervention. Resuscitation. 2014;85:1512–1517. [DOI] [PubMed] [Google Scholar]
- 18. McNally B. Cardiac Arrest Registry to Enhance Survival — CARES Complete Data Set for EMS, Hospital, and CAD Participants and Instructions for Abstracting and Coding Data Elements. 2013;1:58 Available at: https://mycares.net/downloads/Data Dictionary (2013).pdf. Accessed October 18, 2018. [Google Scholar]
- 19. Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–484. [DOI] [PubMed] [Google Scholar]
- 20. ESRI . ESRI Network Analyst. Available at: http://www.esri.com/software/arcgis/extensions/networkanalyst. Accessed February 10, 2017.
- 21. van Buuren S, Groothuis‐Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45:67. [Google Scholar]
- 22. R Core Team . R: A Language and Environment for Statistical Computing, 2015. [Google Scholar]
- 23. Husain S, Eisenberg M. Police AED programs: a systematic review and meta‐analysis. Resuscitation. 2013;84:1184–1191. [DOI] [PubMed] [Google Scholar]
- 24. Hollenberg J, Riva G, Bohm K, Nordberg P, Larsen R, Herlitz J, Pettersson H, Rosenqvist M, Svensson L. Dual dispatch early defibrillation in out‐of‐hospital cardiac arrest: the SALSA‐pilot. Eur Heart J. 2009;30:1781–1789. [DOI] [PubMed] [Google Scholar]
- 25. Ringh M, Jonsson M, Nordberg P, Fredman D, Hasselqvist‐Ax I, Håkansson F, Claesson A, Riva G, Hollenberg J. Survival after public access defibrillation in Stockholm, Sweden—a striking success. Resuscitation. 2015;91:1–7. [DOI] [PubMed] [Google Scholar]
- 26. Hansen SM, Brøndum S, Thomas G, Rasmussen SR, Kvist B, Christensen A, Lyng C, Lindberg J, Lauritsen TLB, Lippert FK, Torp‐Pedersen C, Hansen PA. Home care providers to the rescue: a novel first‐responder programme. PLoS One. 2015;10:e0141352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Becker L, Husain S, Kudenchuk P, Doll A, Rea T, Eisenberg M. Treatment of cardiac arrest with rapid defibrillation by police in King County, Washington. Prehosp Emerg Care. 2013;18:22–27. [DOI] [PubMed] [Google Scholar]
- 28. Lewis M, Stubbs BA, Eisenberg MS. Dispatcher‐assisted cardiopulmonary resuscitation: time to identify cardiac arrest and deliver chest compression instructions. Circulation. 2013;128:1522–1530. [DOI] [PubMed] [Google Scholar]
- 29. Travers S, Jost D, Gillard Y, Lanoë V, Bignand M, Domanski L, Tourtier JP, Bon O, Briche F, Cocault P, Dang Minh P, Frattini B, Galinou N, Genotelle N, Lemoine F, Maurin O, Mendibil A. Out‐of‐hospital cardiac arrest phone detection: those who most need chest compressions are the most difficult to recognize. Resuscitation. 2014;85:1720–1725. [DOI] [PubMed] [Google Scholar]
- 30. Høyer CB, Christensen EF. Fire fighters as basic life support responders: a study of successful implementation. Scand J Trauma Resusc Emerg Med. 2009;17:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. North Carolina Department of Insurance Office of State Fire Marshall . Certification and training—NC fire fighter certification. Available at: http://www.ncdoi.com/OSFM/Fire_Rescue_Commission/Default.aspx?field1=Certification_and_Training_-_NC_Fire_Fighter_Certification&user=Certification_and_Training. Accessed February 14, 2017.
- 32. Yeung J, Okamoto D, Soar J, Perkins GD. AED training and its impact on skill acquisition, retention and performance—a systematic review of alternative training methods. Resuscitation. 2011;82:657–664. [DOI] [PubMed] [Google Scholar]
- 33. Folke F, Gislason GH, Lippert FK, Nielsen SL, Weeke P, Hansen ML, Fosbøl EL, Andersen SS, Rasmussen S, Schramm TK, Køber L, Torp‐Pedersen C. Differences between out‐of‐hospital cardiac arrest in residential and public locations and implications for public‐access defibrillation. Circulation. 2010;122:623–630. [DOI] [PubMed] [Google Scholar]
- 34. Weisfeldt ML, Becker LB. Resuscitation after cardiac arrest: a 3‐phase time‐sensitive model. JAMA. 2002;288:3035–3038. [DOI] [PubMed] [Google Scholar]
- 35. Hasselqvist‐Ax I, Riva G, Herlitz J, Rosenqvist M, Hollenberg J, Nordberg P, Ringh M, Jonsson M, Axelsson C, Lindqvist J, Karlsson T, Svensson L. Early cardiopulmonary resuscitation in out‐of‐hospital cardiac arrest. N Engl J Med. 2015;372:2307–2315. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. List of Fire Stations Staffed 24 Hours Per Day and 7 Days Per Week
Figure S1. Map of Durham county with fire stations, simulated out‐of‐hospital cardiac arrests (randomly generated points), and nearest driving distance routes.
Figure S2. Out‐of‐hospital cardiac arrest survival to hospital discharge at different driving distances from fire stations according to whether the patient was defibrillated by first responders or EMS.
Figure S3. Imputation analysis: Out‐of‐hospital cardiac arrest survival following first responder defibrillation at different driving distances from fire stations to OHCA sites compared with EMS defibrillation.
Figure S4. Out‐of‐hospital cardiac arrest survival following first responder defibrillation at different driving distances from fire stations to OHCA sites compared with EMS defibrillation for patients with witnessed arrest and a shockable heart rhythm.
Figure S5. Overall out‐of‐hospital cardiac arrest favorable neurological outcome at different driving distances from fire stations to OHCA sites.


