Abstract
Background
Readmission after myocardial infarction (MI) is a publicly reported quality metric with hospital reimbursement linked to readmission rates. We describe the timing and pattern of readmission by cause within the first year after MI in consecutive patients, regardless of revascularization strategy, payer status, or age.
Methods and Results
We identified patients discharged after an MI from April 2008 to June 2012. Readmission within 12 months was the primary end point. Readmissions were classified into 4 groups: MI related, other cardiovascular, noncardiovascular, and planned. A total of 3069 patients were discharged after an MI (average age, 65±13 years; and 1941 [63%] men). A total of 655 patients (21.3%) were readmitted at least once (897 total readmissions). A total of 147 patients (4.8%) were readmitted ≥2 times, accounting for 389 readmissions (43%). The instantaneous risk of all‐cause readmission was highest (15 readmissions/100 patients per month; 95% confidence interval, 12–19 readmissions/100 patients per month) immediately after discharge, decreased by almost half (8.1 readmissions/100 patients per month; 95% confidence interval, 7.2–9.0 readmissions/100 patients per month) within 15 days, and was substantially lower and relatively constant (1.4 readmissions/100 patients per month; 95% confidence interval, 1.2–1.6 readmissions/100 patients per month) out to 1 year. Cardiovascular causes of readmission were more common early after discharge.
Conclusions
Most patients with MI are never readmitted, whereas a small minority (≈5%) account for nearly half of 1‐year readmissions. The readmission pattern after MI is characterized by an early peak (first 15 days) of cardiovascular readmissions, followed by a middle period (months 1–4) of noncardiovascular readmissions, and ending with a low‐risk period (>4 months) during which the risk appears independent of cause.
Keywords: coronary heart disease, hospital readmission follow‐up studies, myocardial infarction
Subject Categories: Myocardial Infarction, Quality and Outcomes
Short abstract
See Editorial by Levy and Allen
Clinical Perspective
What Is New?
Patients are at highest risk for readmission after an index myocardial infarction immediately after discharge.
Readmissions for cardiovascular causes are more common early in the discharge period, whereas noncardiovascular reasons for readmission are more likely later in the discharge period.
After ≈5 months, the risk of readmission after myocardial infarction is low and independent of cause.
What Are the Clinical Implications?
Clinicians need to be aware that the first days after discharge after an index myocardial contain the highest risk for readmission.
Carefully coordinated discharge planning and early physician follow‐up may mitigate this risk.
Introduction
Each year, >600 000 patients in the United States will experience a new myocardial infarction (MI), and an additional 300 000 will have a recurrent MI.1 Up to 20% of these patients will be readmitted within 30 days of the index discharge date.2, 3, 4, 5 In the United States, the approximate annual cost for all unplanned readmissions has been estimated at >$17 billion.6 Thirty‐day readmission rates have been proposed as a surrogate for measuring the quality of care provided by hospitals under the assumption that readmissions are preventable and associated with poor delivery of health care.7, 8 Using this as a quality metric, the Centers for Medicare and Medicaid Services began publicly reporting 30‐day readmission rates in 2009, and subsequently in 2012, the Centers for Medicare and Medicaid Services began levying financial penalties to hospitals with excessive readmissions.9 In response, nationwide efforts to reduce readmissions have been underway, but only modest improvements in readmissions after MI have been observed over the past 10 years.10 These persistently high rates of readmissions after MI highlight the need for further research to learn more about readmission patterns.
Patients who survive an index MI are at an increased risk for future adverse clinical events, particularly for future cardiovascular events, such as recurrent MI, heart failure, arrhythmia, and sudden cardiac death, all of which can lead to readmission.2, 3 Furthermore, the risk of these future events varies from patient to patient, and the risk of these events extends beyond 30 days. Despite these known long‐term effects of an index MI, most prior studies have focused on readmissions within 30 days because the current financial penalties only apply to excessive 30‐day readmission rates.2, 3, 4 However, payment bundles that extend to cover patient care for up to 90 days after MI have recently been proposed.11 We have previously shown that the risk for readmission after MI varies dramatically in the first 90 days after an MI when time is viewed as a continuous, not a categorical, variable and that this risk varies whether the cause of readmission is cardiovascular or noncardiovascular.12 As hospital reimbursement and payment structures continue to change and move toward bundled payments for cardiovascular care,11 the need to understand the long‐term pattern of readmissions after MI is critical to help provide quality care and manage costs. Rates of readmission 1 year after MI have been described in the Medicare population13 and in patients treated with percutaneous coronary intervention,14 but there have been no studies in a broad, unselected group of patients with MI. Understanding when and why patients are at greatest risk for readmission may allow hospitals to develop targeted, time‐based readmission prevention strategies and apply them to patients when they are at the greatest risk for readmission. We, therefore, sought to explore the risk of readmission by cause within 1 year after an index MI, regardless of patients’ revascularization strategy, payer status, or age.
Methods
The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure.
The Cleveland Clinic Health System is an 11‐hospital health system consisting of a main campus academic medical center and 10 regional hospitals in northeast Ohio. We retrospectively identified all patients who were admitted to our main campus hospital with a principal diagnosis of MI from April 2008 until June 2012 using discharge International Classification of Diseases, Ninth Revision (ICD‐9), diagnosis codes, including both ST‐segment–elevation and non–ST‐segment–elevation MI (ICD‐9 codes 410–410.9). Patients who died during their index admission for MI were excluded, and only patients discharged alive after MI remained in the study cohort. All readmissions, planned and unplanned, for any reason to any hospital within our institutional health system (including the main campus hospital and all regional hospitals in northeast Ohio) within 12 months of the index MI were identified using our institutional billing system. Readmissions to hospitals outside of our health system were not available and not included in the analysis. An internal audit of the institutional readmission tracking system has shown that 78.3% of all readmissions are captured by this method. After a readmission was identified, patients remained in the study cohort because they continued to be at risk for readmission. Repeated readmissions were counted as separate events. All patients were assumed to remain alive during the 12‐month study period after discharge and remained at risk for readmission.
Baseline demographic data during the index admission for MI were collected for the entire study cohort. The timing of readmission in relation to the date of discharge (time 0) was calculated. The time‐varying instantaneous risk of readmission was estimated for all readmissions over 12 months using a nonlinear parametric temporal decomposition model.15 The specific SAS procedure for this model can be accessed at http://www.lerner.ccf.org/qhs/software/hazard/documents/hazpred.pdf. This method is useful for a possibly nonproportional and complex time‐varying hazard by decomposing it into as many as 3 mathematically simple components, called phases, and for explicitly identifying the time‐varying hazard. The primary cause of each readmission was identified on the basis of principal diagnosis billing codes. The primary cause of readmission was available for 99.7% of all readmissions. The causes of 3 readmissions (0.3% of readmissions) could not be accurately determined from the available discharge billing codes and were subsequently excluded from further analysis. If the primary cause for readmission could not be accurately assigned with the available billing codes, they were excluded from further analysis. The causes for readmission were then categorized into 4 different groups on the basis of the billing codes: MI related, other cardiovascular related, noncardiovascular related, or planned (Table S1). All cardiovascular‐related readmissions were subdivided into MI related and other cardiovascular related because we hypothesized that the timing of MI‐related readmissions (periprocedural complications and recurrent infarctions) would differ from other cardiovascular‐related admissions. The instantaneous risk of readmission for each group (MI related, other cardiovascular related, noncardiovascular related, and planned) was subsequently calculated because each may be different.15
Descriptive statistics were used to summarize the data. Continuous variables are presented as mean±SD. Categorical data are described using frequencies and percentages. All analyses were performed using SAS statistical software (SAS v9.2; SAS, Inc, Cary, NC). The study protocol was approved by our Institutional Review Board, with a waiver of informed consent.
Results
The study population consisted of 3316 unique patients admitted for an index MI between April 2008 and June 2012 (Figure 1). The index in‐hospital mortality rate was 7.4% (247/3316), and these patients were excluded from the subsequent analysis, leaving 3069 patients in the study cohort. Baseline demographic data are shown in the Table. The study population was predominately men, with a mean age of 65 years, and most patients had non–ST‐segment–elevation MI. Within 12 months of the index MI, 655 patients (21%) were readmitted, leading to a total of 897 readmissions. Of the 655 patients readmitted, 508 (78%) were readmitted once and 147 (22%) were readmitted ≥2 times; these 147 patients represented 4.8% of the study cohort and accounted for 389 (43%) of the 897 readmissions. Within 30 days of discharge, 268 readmissions (30%) occurred, with 191 (21%) occurring within 15 days (Figure 2). The instantaneous risk of readmission for any cause after MI, composed of an early decreasing phase and a constant phase, was highest immediately after discharge (15 readmissions/100 patients per month; 95% confidence interval, 12–19 readmissions/100 patients per month) and then decreased rapidly early in the postdischarge period (8.1 readmissions/100 patients per month at 15 days; 95% confidence interval, 7.2–9.0 readmissions/100 patients per month at 15 days) (Figure 3 and Figure S1). After ≈6 months, the risk of readmission for any cause remained low and relatively constant (1.4 readmissions/100 patients per month; 95% confidence interval, 1.2–1.6 readmissions/100 patients per month). Two hundred sixty readmissions (29%) were MI‐related readmissions, and 177 (20%) were other cardiovascular‐related readmissions. All cardiovascular‐related readmissions accounted for 49% of all readmissions. Three hundred forty‐four readmissions (38%) were noncardiovascular related, and 113 readmissions (13%) were planned. The instantaneous risk of readmission by cause is shown in Figure 4, with the hazard phase(s) that compose each readmission cause (Figure S2A through S2D). The risk of MI‐related and other cardiovascular‐related readmissions was highest immediately after discharge and after ≈15 days; non–cardiovascular‐related causes posed the highest risk for readmission.
Figure 1.
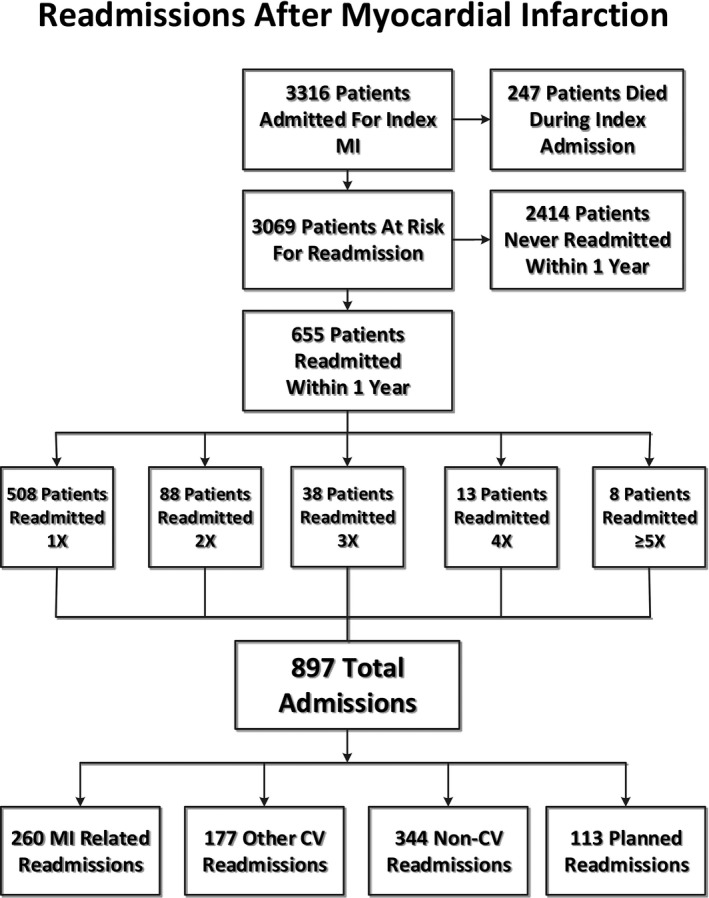
Patient flow sheet. *The causes of 3 could not be accurately determined on the basis of the available discharge billing codes. CV indicates cardiovascular; MI, myocardial infarction.
Table 1.
Patient Characteristics (of Patients Discharged Alive After MI)
| Characteristic | Value (n=3069) |
|---|---|
| Age, y | 65.1±13.3 |
| Male sex | 1941 (63) |
| White race | 2176 (72)a |
| STEMI | 1007 (33)b |
| NSTEMI | 2059 (67)b |
| LVEF, % | 45.9±13.2c |
| Length of stay, d | 3/4/9d |
Data are given as mean±SD or number (percentage). LVEF indicates left ventricular ejection fraction; MI, myocardial infarction; NSTEMI, non‐STEMI; and STEMI, ST‐segment–elevation myocardial infarction.
n=3026.
n=3066.
n=2431.
The 25/50/75 percentiles are given.
Figure 2.
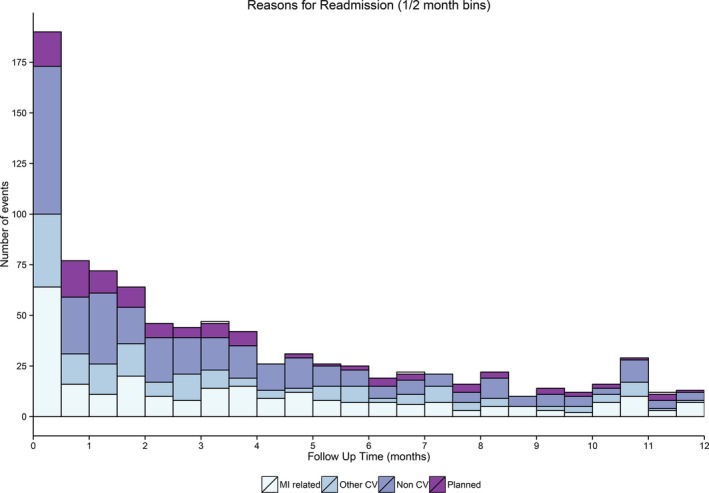
Frequency staked bar graph depicting the change in the number of readmissions after myocardial infarction (MI) for different reasons over 0.5‐month follow‐up time frames. CV indicates cardiovascular.
Figure 3.
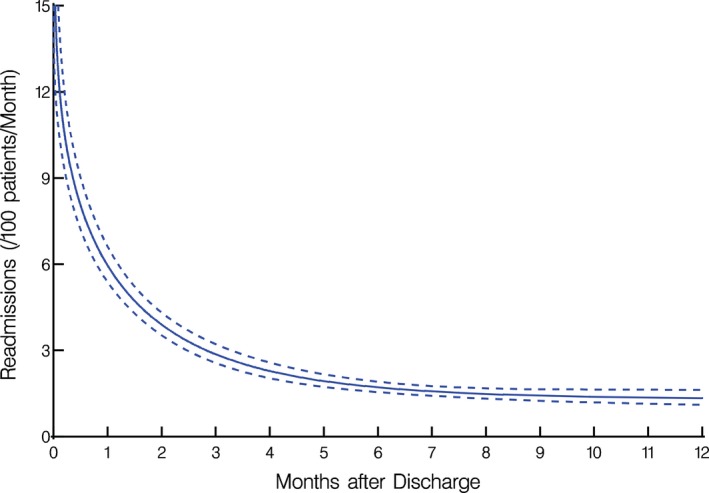
Twelve‐month instantaneous risk (hazard function) of readmission after myocardial infarction (solid line) enclosed within dashed 95% confidence bands.
Figure 4.
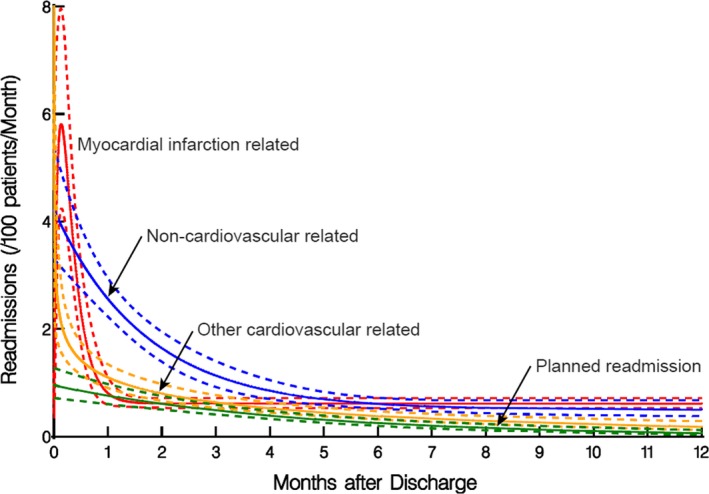
Twelve‐month instantaneous risk (hazard function) of readmission after myocardial infarction by cause (solid lines) enclosed within dashed 95% confidence bands. Red, myocardial infarction related; blue, noncardiovascular related; orange, other cardiovascular related; green, planned readmission.
Discussion
Most patients are never readmitted in the first year after an index MI, and of those patients who are readmitted, the risk of readmission varies dramatically among this small cohort and is dependent on the cause and timing of readmission. A minority of patients (≈5%) account for almost half of the readmissions. This risk of readmission is highest immediately after discharge, decreases exponentially in the first few weeks, and then remains low and relatively constant after ≈6 months from discharge. Classification on the basis of the primary determinant of readmission confirms that the risk for cardiovascular‐related readmissions peaks within 15 days of discharge and then decreases precipitously. After 15 days, the risk of readmission was highest for non–cardiovascular‐related causes until 5 months after discharge, when the risk of readmission is low, and this risk appears to be independent of cause.
Prior studies have described patterns of readmission after MI. Most have focused on readmission within 30 days,2, 3, 4 whereas others have described long‐term readmission patterns out to 1 year for Medicare patients and for those who received percutaneous coronary intervention after MI.13, 14 However, all readmissions after MI, regardless of management strategy or payer status, are used to calculate readmission rates for individual hospitals, and payment bundles for MI may soon extend beyond 30 days.11 Our study is the first to describe 1‐year readmission patterns by cause after MI in an unselected, consecutive patient cohort. Because patients may be readmitted more than once during the follow‐up period, a parametric analytic method for repeated time‐related events was used instead of traditional time‐to‐first‐event (survival) analysis.15 Therefore, unlike survival‐type analysis, patients remain at risk for another readmission after experiencing an event. Our study is the first to use this parametric analysis to evaluate the risk of readmission after MI.
Most patients are never readmitted after an index MI, even when the readmission window is lengthened to 1 year. Of patients who are readmitted, <25% accounted for nearly half (43%) of all the readmissions, reflecting that the risk of readmission is not the same from patient to patient. This varying risk is even more striking when viewed in the context of the entire cohort because the patients readmitted more than once only represent 4.8% of the total population of patients discharged alive after MI; yet, they account for nearly half of all readmissions within 12 months. This varying individual patient‐to‐patient risk may enable us to concentrate our readmission prevention strategies on certain high‐risk patients because nearly 80% of patients are never readmitted, ≈15% are readmitted once, and 5% are readmitted multiple times. Identifying the specific patients who have a dramatically higher risk for readmission after MI could help direct efforts to prevent future readmissions. However, the development of accurate readmission risk prediction models has remained elusive.16
The current 30‐day readmission rate time frame is arbitrary and has limitations in terms of its suitability as an accurate quality metric.17, 18, 19 This time frame was chosen by the Centers for Medicare and Medicaid Services instead of longer time frames (such as 90 days) because readmissions over a longer period may be influenced by factors outside of the hospital's control, such as patient compliance, comorbid conditions, or care provided at other institutions.20 The Centers for Medicare and Medicaid Services began focusing on reducing readmission rates in an effort to improve quality of care, but 30‐day readmission rates do not correlate strongly with mortality rates,21 and paradoxically, higher 30‐day readmissions rates may even be linked to lower mortality rates.22 The assumption that readmissions throughout this 30‐day time frame are similar does not appear to be true and subsequently may hinder the efficacy of strategies to reduce readmission rates. Our results support that the risk of readmission is particularly high in the first 30 days, but >70% of these 30‐day readmissions occur within the first 15 days, correlating with the substantially higher risk of readmission during this early period. In contrast, the rate of readmission is much lower after 30 days, and readmissions become increasingly noncardiovascular, highlighting a potential limitation of extending payment bundles beyond 30 days. Given the disproportionate number of readmissions that occur soon after discharge, the current 30‐day postdischarge period may be more appropriately separated into early and late readmission periods. Some have proposed an early (<15 days) and a late (days 16–30) readmission period,23 whereas others have suggested weighting financial penalties on the basis of the timing of readmission.24 Because payment bundles may be extended past 30 days,11 our results support the consideration of separating the postdischarge time into different periods, such as early (days 0–15), late (days 16–30), and very late (days 31 and beyond), because the risk and causes of readmission shift dramatically during these different time periods. Public reporting of readmission rates under this model may show that some hospitals have excessive rates of readmission during some or all these different time periods. This temporal knowledge would allow physicians and hospitals to identify when their patients are at highest risk for readmission. Our results also support the consideration of adjusting financial penalties on the basis of the risk of readmission at a particular time in the postdischarge period.
Prior studies have shown that the risk factors for early readmissions are different when compared with late readmissions.23 Early readmissions were associated with markers of both acute and chronic disease in contrast to late readmissions, which were found to be associated only with markers of chronic disease. Our study supports this finding because the risk for readmission was highest immediately after discharge, regardless of cause. This early risk likely reflects the acute illness burden of an MI and the complications related to the management of acute coronary syndrome, representing a posthospitalization syndrome,25 or unique clinical state when patients are particularly vulnerable to readmission. Because the risk for readmissions varies dramatically throughout the 30 days, strategies to prevent readmission that are applied broadly to the 30‐day window may have limited efficacy.
Early outpatient follow‐up has been viewed as a strategy to prevent readmission. However, optimal timing for outpatient follow‐up after MI has not been well established, and the effect of early outpatient follow‐up after MI is conflicting. Major societal guidelines endorse the development of posthospital systems of care in an effort to reduce hospital readmissions, but they do not recommend any specific timing for scheduled follow‐up with primary care physicians or with cardiologists.26, 27 Our results suggest that follow‐up should occur soon after discharge (within 1 week) if the goal of outpatient follow‐up is to reduce readmission rates, although a prior retrospective analysis of a Medicare MI registry did not show that early follow‐up was associated with decreased rates of readmission.5 Scheduling outpatient follow‐up later in the discharge period could leave patients at undue risk for readmission. A more recent study has shown that early physician follow‐up has led to a reduction in 30‐day readmission rates after non–ST‐segment–elevation MI, especially for those patients with MI who follow up with the same treating inpatient physician or a cardiologist.28 Early follow‐up with a cardiologist is supported by our findings because cardiovascular‐related readmissions predominate early in the discharge period. Follow‐up with a primary care physician may be more effective later in the discharge period when non–cardiovascular‐related readmissions are more common.
Readmissions have been historically viewed as a failure or breakdown in longitudinal care. However, inpatient care processes, such as length of stay, rapid response team activation, or discharge time, have been shown to be associated with readmission soon after discharge.23, 29 Our prior analysis12 and current study support this finding because the risk of readmission was highest immediately after discharge. These findings suggest that clinical events and decision making during the index hospitalization contribute to this heightened early risk of readmission, reflecting a breakdown in inpatient, not outpatient, care. If hospitals try to manage costs by focusing on decreased length of stay after MI, they must be careful to avoid potentially increasing the risk of readmission30 and exposing themselves to financial penalties attributable to excessive readmission rates. Efforts to reduce readmissions must focus on both the inpatient and outpatient arena because efforts focused solely on one will likely fall short, and these efforts should begin on the day of admission and not on the day of discharge.
Although our study has several strengths, we acknowledge limitations inherent to a single‐center retrospective study. In addition, our health system is an academic, quaternary referral center with 10 regional hospitals across northeast Ohio, thus potentially limiting the generalizability of our findings to community hospitals. Readmissions to hospitals outside our health system were not included, and our rate of readmission is underestimated. However, an internal audit of our institutional readmission tracking system has shown that ≈80% of all readmissions to any institution are captured within our health system, and our overall rate of readmission was similar to prior, larger studies.2, 3, 5 Furthermore, our study design allowed us to capture all patients with MI within our health system, regardless of their payer status, including self‐pay, and thus more accurately reflects the total population of patients with MI compared with prior analyses based solely on Medicare databases.13 This method was also readily available operationally and captures patients within the scope of direct control of our health system. We also assumed that all patients remained alive and at risk for readmission. Deaths that occurred after discharge would lead to an overestimation of the rate of readmission. However, contemporary estimates of 1‐year survival in patients who survive their index MI are 93% to 94%,31 and thus only a small portion of our cohort would have been removed from the analysis if mortality status was known. Identification of the initial cohort and the causes of readmission were determined by principal diagnosis billing codes, which could lead to misclassification if the coding was inaccurate. However, the use of administrative data has been shown to be accurate (94%) when compared with clinical medical record review.32
Our study demonstrates that the risk of readmission after MI varies dramatically by patient and over time when the discharge window is extended to 1 year. Most patients are never readmitted after an index MI, and a small minority (≈5%) of patients account for nearly half of all readmissions. Furthermore, the risk of readmission, particularly for cardiovascular causes, is highest early after readmissions, declines substantially by 15 days, and remains low after 30 days to 1‐year postdischarge. These findings highlight a major limitation to extending readmission penalties and cardiovascular payment bundles beyond 30 days and, in fact, suggest that the readmission window and payment bundle could even be shortened from 30 to 15 days to accurately capture cardiovascular readmissions. Readmission prevention strategies need to start in the hospital on admission given the early high risk of cardiovascular readmissions, and targeted strategies may be needed for the patients at highest risk of readmission. Finally, more research is needed to identify the high‐risk patients who are leading to recurrent readmissions and to elucidate what leads to the inordinately high risk of readmission early after MI.
Sources of Funding
The primary funding source was unrestricted philanthropic support to the Heart and Vascular Institute Center for Healthcare Delivery Innovation, Cleveland Clinic. The funding source had no role in the design or conduct of the study; collection, management, analyses, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Disclosures
Khot serves as a consultant for Astra Zeneca. The remaining authors have no disclosures to report.
Supporting information
Table S1. Categorical Assignment of Principal Diagnosis Billing Codes
Figure S1. Twelve‐month instantaneous risk (hazard function phases) of readmission after myocardial infarction.
Figure S2. A, Twelve‐month instantaneous risk (hazard function phases) of readmission after myocardial infarction for myocardial infarction related readmissions. B, Twelve‐month instantaneous risk (hazard function phases) of readmission after myocardial infarction for non‐cardiovascular related readmissions. C, Twelve‐month instantaneous risk (hazard function phases) of readmission after myocardial infarction for other cardiovascular related readmissions. D, Twelve‐month instantaneous risk (hazard function phases) of readmission after myocardial infarction for planned readmissions.
(J Am Heart Assoc. 2018;7:e009650 DOI: 10.1161/JAHA.118.009650.)
References
- 1. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322. [DOI] [PubMed] [Google Scholar]
- 2. Dunlay SM, Weston SA, Killian JM, Bell MR, Jaffe AS, Roger VL. Thirty‐day rehospitalizations after acute myocardial infarction: a cohort study. Ann Intern Med. 2012;157:11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, Barreto‐Filho JA, Kim N, Bernheim SM, Suter LG, Drye EE, Krumholz HM. Diagnoses and timing of 30‐day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ranasinghe I, Wang Y, Dharmarajan K, Hsieh AF, Bernheim SM, Krumholz HM. Readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia among young and middle‐aged adults: a retrospective observational cohort study. PLoS Med. 2014;11:e1001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hess CN, Shah BR, Peng SA, Thomas L, Roe MT, Peterson ED. Association of early physician follow‐up and 30‐day readmission after non‐ST‐segment‐elevation myocardial infarction among older patients. Circulation. 2013;128:1206–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee‐for‐service program. N Engl J Med. 2009;360:1418–1428. [DOI] [PubMed] [Google Scholar]
- 7. Report to Congress : Promoting Greater Efficiency in Medicare. Washington, DC: Medicare Payment Advisory Commission; 2007. [Google Scholar]
- 8. Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141:533–536. [DOI] [PubMed] [Google Scholar]
- 9. Readmissions Reduction Program (HRRP) . [Website]. 2016. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed May 4, 2016.
- 10. DeVore AD, Hammill BG, Hardy NC, Eapen ZJ, Peterson ED, Hernandez AF. Has public reporting of hospital readmission rates affected patient outcomes? Analysis of Medicare claims data. J Am Coll Cardiol. 2016;67:963–972. [DOI] [PubMed] [Google Scholar]
- 11. Notice of proposed rulemaking for bundled payment models for high‐quality, coordinated cardiac and hip fracture care [Website]. 2016. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2016-Fact-sheets-items/2016-07-25.html. Accessed August 4, 2016.
- 12. Khot UN, Johnson MJ, Lowry AM, Rajeswaran J, Kapadia S, Shishehbor MH, Menon V, Ellis SG, Goepfarth P, Blackstone EH. The time‐varying risk of cardiovascular and noncardiovascular readmissions early after acute myocardial infarction. J Am Coll Cardiol. 2017;70:1101–1103. [DOI] [PubMed] [Google Scholar]
- 13. Krumholz HM, Hsieh A, Dreyer RP, Welsh J, Desai NR, Dharmarajan K. Trajectories of risk for specific readmission diagnoses after hospitalization for heart failure, acute myocardial infarction, or pneumonia. PLoS One. 2016;11:e0160492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hess CN, Kaltenbach LA, Doll JA, Cohen DJ, Peterson ED, Wang TY. Race and sex differences in post‐myocardial infarction angina frequency and risk of 1‐year unplanned rehospitalization. Circulation. 2017;135:532–543. [DOI] [PubMed] [Google Scholar]
- 15. Blackstone EH, Naftel DC, Turner ME. The decomposition of time‐varying hazard into phases, each incorporating a separate stream of concomitant information. J Am Stat Assoc. 1986;81:615–624. [Google Scholar]
- 16. Kansagara D, Englander H, Salanitro A, Kagen D, Theobald C, Freeman M, Kripalani S. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Axon RN, Williams MV. Hospital readmission as an accountability measure. JAMA. 2011;305:504–505. [DOI] [PubMed] [Google Scholar]
- 18. Joynt KE, Jha AK. Thirty‐day readmissions: truth and consequences. N Engl J Med. 2012;366:1366–1369. [DOI] [PubMed] [Google Scholar]
- 19. Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009;361:2637–2645. [DOI] [PubMed] [Google Scholar]
- 20. 30‐Day unplanned readmission and death measures [Website]. 2016. https://www.medicare.gov/hospitalcompare/Data/30-day-measures.html. Accessed May 4, 2016.
- 21. Krumholz HM, Lin Z, Keenan PS, Chen J, Ross JS, Drye EE, Bernheim SM, Wang Y, Bradley EH, Han LF, Normand SL. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2013;309:587–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gorodeski EZ, Starling RC, Blackstone EH. Are all readmissions bad readmissions? N Engl J Med. 2010;363:297–298. [DOI] [PubMed] [Google Scholar]
- 23. Graham KL, Wilker EH, Howell MD, Davis RB, Marcantonio ER. Differences between early and late readmissions among patients: a cohort study. Ann Intern Med. 2015;162:741–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368:1175–1177. [DOI] [PubMed] [Google Scholar]
- 25. Krumholz HM. Post‐hospital syndrome: an acquired, transient condition of generalized risk. N Engl J Med. 2013;368:100–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis‐Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX. 2013 ACCF/AHA guideline for the management of ST‐elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2013;82:E1–E27. [DOI] [PubMed] [Google Scholar]
- 27. Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, Liebson PR, Mukherjee D, Peterson ED, Sabatine MS, Smalling RW, Zieman SJ. 2014 AHA/ACC guideline for the management of patients with non‐ST‐elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64:e139–e228. [DOI] [PubMed] [Google Scholar]
- 28. Tung Y, Chang G, Chang H, Yu T. Relationship between early physician follow‐up and 30‐day readmission after acute myocardial infarction and heart failure. PLoS One. 2017;12:e0170061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ashton CM, Del Junco DJ, Souchek J, Wray NP, Mansyur CL. The association between the quality of inpatient care and early readmission: a meta‐analysis of the evidence. Med Care. 1997;35:1044–1059. [DOI] [PubMed] [Google Scholar]
- 30. Kociol RD, Lopes RD, Clare R, Thomas L, Mehta RH, Kaul P, Pieper KS, Hochman JS, Weaver WD, Armstrong PW, Granger CB, Patel MR. International variation in and factors associated with hospital readmission after myocardial infarction. JAMA. 2012;307:66–74. [DOI] [PubMed] [Google Scholar]
- 31. Smolina K, Wright FL, Rayner M, Goldacre MJ. Long‐term survival and recurrence after acute myocardial infarction in England, 2004 to 2010. Circ Cardiovasc Qual Outcomes. 2012;5:532–540. [DOI] [PubMed] [Google Scholar]
- 32. Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH. Accuracy of Medicare claims‐based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. Am Heart J. 2004;148:99–104. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Categorical Assignment of Principal Diagnosis Billing Codes
Figure S1. Twelve‐month instantaneous risk (hazard function phases) of readmission after myocardial infarction.
Figure S2. A, Twelve‐month instantaneous risk (hazard function phases) of readmission after myocardial infarction for myocardial infarction related readmissions. B, Twelve‐month instantaneous risk (hazard function phases) of readmission after myocardial infarction for non‐cardiovascular related readmissions. C, Twelve‐month instantaneous risk (hazard function phases) of readmission after myocardial infarction for other cardiovascular related readmissions. D, Twelve‐month instantaneous risk (hazard function phases) of readmission after myocardial infarction for planned readmissions.


