Abstract
Background
Nursing practice is a key driver of quality care and can influence newborn health outcomes where nurses are the primary care givers to this highly dependent group. However, in sub-Saharan Africa, nursing work environments are characterized by heavy workloads, insufficient staffing and regular medical emergencies, which compromise the ability of nurses to provide quality care. Task shifting has been promoted as one strategy for making efficient use of human resources and addressing these issues.
Aims and objectives
We aimed to understand the nature and practice of neonatal nursing in public hospitals in Nairobi so as to determine what prospect there might be for relieving pressure by shifting nurses’ work to others.
Methods
This paper is based on an 18-month qualitative study of three newborn units of three public hospitals—all located in Nairobi county—using an ethnographic approach. We draw upon a mix of 32 interviews, over 250 h’ observations, field notes and informal conversations. Data were collected from senior nursing experts in newborn nursing, neonatal nurse in-charges, neonatal nurses, nursing students and support staff.
Results
To cope with difficult work conditions characterized by resource challenges and competing priorities, nurses have developed a ritualized schedule and a form of ‘subconscious triage’. Informal, organic task shifting was already taking place whereby particular nursing tasks were delegated to students, mothers and support staff, often without any structured supervision. Despite this practice, nurses were agnostic about formal institutionalization of task shifting due to concerns around professional boundaries and the practicality of integrating a new cadre into an already stressed health system.
Conclusion
Our findings revealed a routine template of neonatal nursing work which nurses used to control unpredictability. We found that this model of nursing encouraged delegation of less technical tasks to subordinates, parents and other staff through the process of ‘subconscious triage’. The rich insights we gained from this organic form of task shifting can inform more formal task-shifting projects as they seek to identify tasks most easily delegated, and how best to support and work with busy nurses.
Electronic supplementary material
The online version of this article (10.1186/s12960-019-0352-x) contains supplementary material, which is available to authorized users.
Keywords: Task shifting, Task sharing, Delegation, Neonatal nursing, Low- and middle-income countries (LMICs), Subconscious triage, Routines, Supervision
Background
Sustainable Development Goal 3.2 calls for a reduction in neonatal mortality to at least 12 per 1 000 live births [1]. High impact, low cost interventions could avert more than 71% of neonatal deaths, but depend to a large extent on effective coverage with facility-based care [2]. However, the performance of public sector hospitals in low- and middle-income countries (LMICs) is often poor [3, 4], and this is particularly the case for newborn care [5, 6]. Some of the contributing factors are inadequate material resources and equipment, poor adherence to evidence-based guidelines, inadequate human resources for health (HRH) and poor management of material and human resources [6–8].
Nurses are key to the provision of quality care and have a particular influence on newborn health outcomes in hospitals as primary care givers to this highly dependent group [9]. However, according to the Global Health Workforce Alliance (GHWA) 2014 report ‘A Universal Truth’, the global shortage of health workers is estimated to be over seven million [10]. Kenya has an acute shortage of nurses in the public sector, with densities ranging between 1.2 and 0.008 per 1 000 population across counties compared to a new suggested minimum health workforce threshold of 4.45/1000 population for doctors, nurses and midwives combined [11]. Nairobi county, the specific focus of our study, suffers from both major shortages of nurses providing frontline neonatal care in the public sector and very poor neonatal outcomes [12]. Indeed, in Nairobi’s public hospitals, recent work suggests nurse: baby ratios of 1:15 [13]. In countries such as the United Kingdom, even for babies who do not require intensive care, guidelines suggest one nurse for every two to four sick babies [14, 15] with evidence suggesting a relationship between lower nurse ratios and higher mortality [14]. Kenya’s public-sector nursing workforce challenge is however complex. Recent data reveals the country has more than 50 000 nurses registered to practice, but fewer than 17 000 offering care in the public sector, which is particularly relied upon by the poor for inpatient care because of inadequacies in public finance [16]. Workforce solutions must therefore carefully consider budget impacts.
The World Health Organization (WHO) suggests task shifting and sharing as a means to lessen the problems of HRH shortages, while potentially improving access and maintaining or improving quality [17]. ‘Task shifting’ is a phrase used to cover a variety of interventions, but WHO uses it to group activities in which: ‘…trained cadres who do not normally have competencies for specific tasks deliver them and thereby increase levels of health care access’ [18]. The related term ‘task sharing’ is described as ‘the rational distribution of tasks among trained and supervised health professionals and health workers’. In this study, we use the term task shifting although in the context under study tasks that are shifted might still be supervised by a nurse.
In most cases, task shifting and task sharing aim to provide services at reasonable cost through a new cadre of worker when an absolute shortage of staff puts unreasonable demands on existing cadres who are unable to meet requirements [19]. A series of studies and systematic reviews intended to inform WHO’s ‘Recommendations for Optimizing Health Worker Roles to Improve Access to key Maternal and Newborn Health Interventions through Task Shifting’ (OPTIMIZEMNH) (WHO [18]) have reported ‘barriers’ such as training and supervision challenges, problems with professional hierarchies and poor integration of new cadres into formal health systems [20, 21]. Reported facilitators of task shifting included public recognition, creation of visible ties to the formal system where formal health workers were involved in training new cadres [22, 23]. However, Mijovic et al. [24] highlight that in all the African case studies they reviewed, the cadre taking up additional shifted tasks exceeds the formal mandate, taking on responsibilities additional to those ‘shifted’. Hence, while the financial case for task shifting is clear [25], implementation is difficult and the intervention ought not be thought of as a ‘cure-all’.
Task sharing and shifting have been used extensively in LMIC contexts in response to HIV/AIDs and in anaesthetic and surgical care where tasks that are traditionally the preserve of trained physicians are performed by non-physician clinicians or nurses [26]. Task shifting and task sharing is also now common in high-income countries’ hospitals where health care assistants undertake many ‘basic’ nursing tasks under the supervision of nurses [27]. Historically, Kenya had a cadre of non-professional assistants referred to as ‘nurse aides’. Our respondents confirmed that this position was phased out in the early 1990s having been linked to reports nurse aides were over-stepping role boundaries (typically when operating without supervision) and thus putting patients at risk. This might partly explain reluctance to formally re-introduce such a cadre [28]. Anecdotal evidence indicates, however, that shifting of nursing tasks to non-qualified personnel is happening although not officially allowed in the Kenyan public sector.
Our work aimed to explore the potential for task shifting to support the provision of basic nursing care in hospitals’ neonatal units. In 2017, the Kenyan Ministry of Health launched the Task Sharing Policy 2017–2030 and the Task Sharing Policy Guidelines [29]. These policies focused on legitimating task-shifting between existing health professionals by redefining scopes of practice to reflect the realities of routine work and its evolution over more than 20 years (e.g. nurses run primary care, prescribe and put up intravenous fluids in clinical settings). The policy, however, makes no mention of new hospital-based cadres to support basic inpatient nursing care.
Prior task shifting and sharing approaches in LMICs highlight the importance of well-designed interventions linking newly established cadres to existing professionals at the micro level, and their integration into formal structures of health systems [20–22, 30, 31]. Relatedly, De Sardan [32] describes the disconnect resulting from implementing standardized interventions without consideration of everyday contexts. In particular, he describes ‘practical norms’ as ‘the various informal, de facto, tacit or latent norms that underlie the practices of actors, which diverge from the official norms (or social norms)’ ([33]: 26). It is important then to investigate the socio-cultural dimensions or ‘software’ of health systems, including practical norms, as part of any potential task-shifting design efforts [34, 35].
This study aimed to explore the current operation of Nairobi’s New Born Units (NBUs) using an ethnographic approach. It is part of a body of work exploring major gaps in quality of neonatal care and potential solutions, including task shifting. The study reveals nursing routines, highlights areas of working practice that might easily be shared with a lower cadre, describes nursing stakeholders and nurses’ perceptions of task-shifting for this context and explores the overall potential for task shifting in Nairobi’s public hospital NBUs.
Methodology
This work first started with an exploration of the views of influential nursing leaders on the idea of task shifting as a possible intervention to improve in-patient care for sick newborns. The results of the first phase were complemented by a formal stakeholder analysis [28] and informed empirical work in the second phase of the research. Phase two explored how nursing tasks are performed within the busy, highly normative culture of Kenyan newborn nursing.
Specific study sites
The second phase was conducted in Nairobi City county, within newborn units of three public hospitals. All hospitals offer inpatient and outpatient services (e.g. immunization, HIV treatment and care and maternity services), and one hospital is specifically a maternity hospital. The hospital descriptions are provided below (Table 1).
Table 1.
Description of structure and services of the study hospitals and their newborn units (unpublished data)
| Hospital | Description | |||||
|---|---|---|---|---|---|---|
| Hospital code | 1 | 2 | 3 | |||
| NBU bed capacity and no. of deliveries | 84 beds/cots with approximately 400 admissions monthly (4 800 yearly) | 31 bed/cots combined with approximately 150 admissions monthly | 35 beds/cots combined (15 cots) with 100 admissions monthly | |||
| NBU staffing | 32 staff | 16 staff | 17 staff | |||
| 2 paediatricians | 2 paediatricians | 1 paediatrician | ||||
| 6 medical officers | 1 medical officer | 1 medical officer | ||||
| 6 registered clinical officers | 0 registered clinical officers | 0 registered clinical officers | ||||
| 18 nurses | 12 nurses | 13 nurses | ||||
| 2 clinic assistants | 1 support staff | 2 support staff | ||||
| 2 support staff | ||||||
| Distribution of NBU nurses per shift | Weekdays | Weekends | Weekdays | Weekends | Weekdays | Weekends |
| Morning 4 | Morning 4 | Morning 2–3 | Morning 2–3 | Morning 2–3 | Morning 2 | |
| Afternoon 2 | Afternoon 2 | Afternoon 2 | Afternoon 2 | Afternoon 2 | Afternoon 1–2 | |
| Night 3 | Night 3 | Night 1 | Night 1 | Night 2 | Night 2 | |
Sampling
The first phase of this study involved a total of 10 interviews conducted with senior stakeholders (see Table 2). We then purposively sampled nurses who had significant work experience in the new born unit (our participants’ NBU experience ranges 1–5 years). These included support staff, nurse managers (in-charges) and frontline nurses (junior nurses), but in one setting, we also included nurse students (whose clinical rotations within the NBU typically last 2–6 weeks). To ensure maximum variation of the participants, we included different nursing grades and specialisms that pertain to neonatal nursing cognizant of gender and age variations across our samples. We conducted 22 interviews with hospital staff across all 3 hospitals.
Table 2.
Study sample size showing number of interviews in each hospital, cadre of health workers and details of stakeholders interviewed
| Hospital | Nurses | Support staff | Students | Stakeholders (n = 10) |
|---|---|---|---|---|
| 1 | 6 | 1 | Ministry of Health, Nairobi City County Health Team, Nursing Council of Kenya, National Nurses Association of Kenya, Kenya National Union of Nurses, Kenya Medical Training College, Kenya Paediatric Association and the Kenya Medical Association. | |
| 2 | 8 | 1 | 2 FGDs | |
| 3 | 3 | 1 | ||
| 17 | 3 | 2 |
Interviews were semi-structured and followed an ethnographic or long approach with the aim of not eliciting ‘answers’ but rather invoking narratives [36] and lasted 1–1.5 h. From these narratives, clarifying questions were developed to iteratively check and extend the theory being developed (see interview guide in the Additional file 1). The interviews were complemented by non-participatory observations of day and night shifts, over weekdays and weekends, across all the three hospitals’ neonatal wards (250 h in total).
Interviews were transcribed by one author (JJ), and both transcripts and field notes imported into Nvivo 10 Qualitative Software as a shared project. Three authors (JN, JM and JJ) independently coded data into emerging themes in a first phase of analysis. The team then agreed on a set of themes for the next round of analysis. Initial themes were refined during the research by modifying the interview guide to probe emerging theory, relating it to important questions in the literature on task shifting. In this way, we were able to usefully extend theories on task shifting [37, 38].
We present a full exploration of the ethnographic work elsewhere. Here, we draw on all the interviews and non-participant observation to present a detailed deep description of the organization of nursing work, specifically detailing the conduct of ‘nursing tasks’ and routines as part of inpatient neonatal care. We use the insights gained to explore the potential of task shifting in newborn units. Our findings should not be read as ‘barriers’ and ‘facilitators’ of task shifting but rather as rich description of an environment where task shifting might be implemented. We present findings under two main themes as described below.
Results
Organization of neonatal nursing work
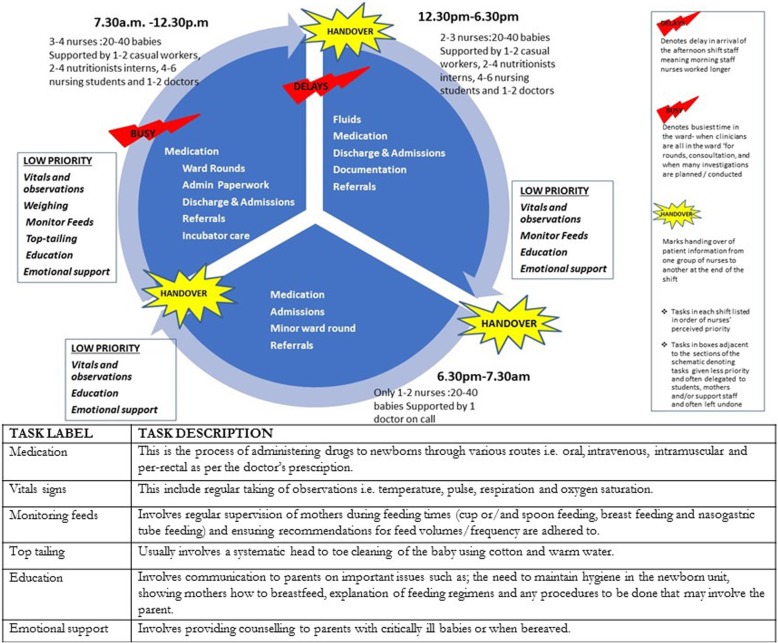
Nurses, even on these relatively large inpatient newborn units, very rarely have specific post-basic training in neonatal nursing with most being diploma level (registered) nurses who have 3 years general nursing training. In all three hospitals, nurses lacked explicit job descriptions and were not given formal orientation to the neonatal ward setting at the start of work in these units. Thus, nurses’ roles were implicitly drawn from their prior experience and immediate, experiential ‘on-job’ training with everyone expected to fit into roles as depicted in the schedule below (Fig. 1).
It is automatic – nursing is a routine so everyone who is on duty knows what to do in case the in charge is not around it is not new; in every ward you go that is the routine (NBU Nurse Hospital 2)
Across all hospitals, work in the NBU followed a standard routine (see Fig. 1) which was characterized by busy morning shifts where multiple clinicians, nurses, nutritionists and students were present; when care planning was largely conducted; and when most tasks were performed. Afternoon shifts were generally short, but commonly made longer by delays in the arrival of the oncoming shift nurses, and were understood to be less busy than morning and night shifts except when there were emergencies. The longest shift was the night shift, which was least staffed with often one nurse dealing with 15–20 babies over 13 h. Across all three shifts, nursing tasks were performed following a routine that prioritized technical tasks over other bedside care tasks as shown in Fig. 1.
Fig. 1.
Emerging template of neonatal care in study hospitals depicting how nursing tasks are organized (prioritized tasks in bold, low priority tasks in boxes) against the number of nurses on the three shifts. Of note, ‘Handovers’ with generally very busy morning shifts and delays in staff reporting for the afternoon shift
We observed that routines were disrupted by emergency admissions, unexpected staff absences and changing conditions of the very sick babies. In those situations, nurses were forced to make decisions about how to use their time, judging who needed immediate care and who could wait. They did this by using a type of ‘Subconscious Triage’. We use this term to characterize the response to the continual need to make decisions about allocating limited resources while under extreme pressure. We asked nurses what guides them when they have staff shortages:
When you are so tied up [due to shortages], you could start with the very sick one because we do it at 9 a.m. So, because you’re so busy, you do to the very sick ones first. So, make sure they are done at least if the doctors round is being done they need to know the vital signs. So, you do those ones. Then these other ones may not be strictly done at 9. You can even do it at 11, 12 when you are a little relaxed now. So, you can always postpone some and do them later. (NBU Nurse Hospital 1)
On close observation and reflection, we also noticed that nurses followed a common, implicit hierarchy in managing tasks. For example, typically, the provision of bedside care (personal, direct care, e.g. informing mothers of their baby’s condition) only occurred while on the way to perform more technically difficult clinical tasks such as administering intravenous medication or monitoring blood transfusion. Thus, there was tension between the nursing role as providing holistic care versus provision of the more technical, clinical tasks considered ‘crucial’ and often given priority over bedside caring tasks.
Our core thing is the baby, so our priority will be the wellness of the baby, so if I have all that to do there are things I will have to skip, doing resuscitation is a must that one is a must and that is a priority. So, we will have to stabilize the baby with the help of the COs, the clinicians, doctors, until you are sure that the baby is okay and stable. From there now you can do the other bit of it – giving treatment is a must and timings really matter. (NBU Nurse Hospital 2)
Resuscitations were regarded as a priority, but the ‘wellness of the baby’ was generally interpreted as whether or not the baby got all medical treatments and procedures prescribed. This is perhaps inevitable given the pressures that nurses work under and the frequency with which they are expected to deal with more technical, life-threatening issues such as resuscitations.
Task delegation in practice
The observations above are important because they indicate several areas in which a task-shifting cadre might add value in support of nurses’ work. They also provide essential context that might help design a programme likely to be accepted and supported by nurses. Indeed, we observed ad-hoc shifting and delegation of some tasks across all three NBUs. Our observations of tasks delegated in practice contrasted with those thought safe to delegate by senior nursing stakeholders in related research [39] as did the levels of supervision required for tasks delegated to students (Table 3).
Table 3.
Task delegation and shifting in practice based on our ward observations
| Category of delegation | Task areas |
|---|---|
| Tasks that can never be delegated to someone other than a qualified professional | Ordering supplies and equipment from the stores and pharmacy Resuscitation of babies Final assessment of nursing students to qualify as nurses Referral of babies from one hospital to an often-higher care hospital |
| Delegated to student nurses undertaking clinical training attachments | Weighing babies Taking vital signs observations Giving intravenous fluids Filling the nursing Kardex (a summary of individual patient needs used by nurses to communicate important information on their patient and often updated at every shift change). Giving treatments—either oral, intra-muscular or intravenous |
| Delegated to mothers | Cup and NGT (naso-gastric tube) feeding of babies Filling amounts of milk fed to babies on feeding chart Top tailing (cleaning baby from head to toe) |
| Delegated to support staffa | Dusting and cleaning incubators Cup and NGT (naso-gastric tube) feeding of babies Top tailing (cleaning baby from head to toe) |
| Tasks sometimes done/left undone | Education Emotional support |
aLong-term casual employees often sub-contracted by the hospital to primarily provide cleaning services within the hospital although they are also often used to run errands within the different departments in the hospital
We observed that it was mainly the non-clinical tasks that were delegated or shifted and that this happened only under authorization (but rarely supervision). The authorization only came from the more senior and experienced nurses in the ward and never the junior nurses.
I: You usually clean the babies?
R: Yes, those that are not very sick and their mothers are not coming, so you just can’t leave them dirty and their ointment is there, you wash them then you change then, you make the cots then you feed them, that’s when your work will be over
I: Is that also in your job description?
R: No, it isn’t there it is just helping. (Support Staff, Hospital 2)
A clear example of acceptance of a need for support (and therefore task-shifting) was seen in hospital 3 where the hospital had negotiated with its administration to have one support worker permanently allocated to the NBU ward. We observed this person undertaking a host of basic care tasks, e.g. cleaning incubators, top tailing and nasogastric tube feeding and also general management of patients.
They [support staff] are more accessible to patients because the nurse is in the station writing Kardex and doing/ handling other issues so the complaints from the patients they take them and they come to tell the nurse ‘patient so and so is requesting for this’…. (NBU nurse, Hospital 3)
Where nurses considered some tasks simple and therefore ‘safe’ to delegate, the important aspects of the logic behind such tasks was often lost to those it was delegated to. For example, clinical staff at Hospital 1 initiated teaching lessons for cleaners about infection control and its importance. While the cleaners ensured everything looked clean, they were often found to be wiping down surfaces with dirty cloths, unaware that surfaces may look clean while harbouring infection.
There are tasks that can be done by such a person [support staff] …, like feeding, changing, top tailing, or even dusting, even something like cleaning an incubator someone who is not skilled can be trained and do all that, we don’t have to have a nurse. Okay, the issues of infection prevention, but you can teach someone to do that…. (Nurse manager Hospital 1)
We found that tasks delegated were not always supervised, even where mentoring of students was expected. From our observations, nurses spend minimal time teaching junior staff and students despite these hospitals being training facilities. Nursing students, however, perceived this as the norm, accepting it as the learning culture in public hospitals:
R1: In comparison, we can say okay in our hospital you know our hospital is a private hospital, so in private, most of the tasks… we don’t do them, the nurses the qualified nurses are the ones who do
I: Tell me what they do
R2: Like the resuscitations, fixing of NG tubes, cannulas and giving some medications
I: And fixing NG tubes?
R1: Yeah, here [public hospitals] you do everything. In NBU we… you just find yourself giving treatment, doing something…. (Nursing students Hospital 2)
Our ethnographic observations of what routinely happened in the wards as described above contrasted with the ‘official position’ of senior nurses offered during interviews. The experts were concerned about safety and levels of competency and were cautious about what ought to be delegated and what ought to remain within the nursing profession (see stakeholders’ views in Additional file 1: Table S1). There was a general agreement that nurses could delegate a task to a student or other carer only if they retained responsibility for such tasks being carried out correctly and for appropriately supervising the student(s). The position of senior nurses not on the frontline of practice, was simply that, nurses had to work harder to comply with professional standards of care, regardless of the pressure they were under.
Discussion
Our work sought to gain an understanding of how neonatal care is organized and structured [40] on a daily basis and what opportunities exists for task shifting. We believe that the professional cultures, occupational jurisdictions and de facto templates of care of frontline workers will directly influence the success or failure of task-shifting interventions. We have attempted to reveal these contextual factors so that the design of any task-shifting intervention is more considered and hence more likely to succeed.
As there were no explicit job descriptions and standard work guidelines for routine newborn work, the working model of nursing was normatively formed over many years in response to the practical realities of the environment. Hospitals are replete with organizational timetables and schedules [41], but to the nurses, this structuring offered limited guidance on how to organize and delegate certain tasks. Therefore, as a way of coping with task ambiguity, nurses developed de facto routines that provided direction on what they should be doing at any given time (see Fig. 1). However, because of the unpredictable nature of events in these settings [42], the routines would often be disrupted, and nurses would find themselves quickly having to make difficult decisions. In such situations, nurses prioritized nursing tasks based on patient needs using ‘subconscious triage’, which often included delegating and shifting tasks to others.
Delegation of tasks was, however, ad hoc as support staff, students and mothers frequently worked without supervision, and none seemed concerned about undertaking tasks that they were not trained for. This contrasted with findings of an expert meeting conducted as part of our broader programme of work [39] where attendees firmly expressed consensus on tasks that should be formally conducted by nurses and on tasks where delegation might be allowable.
From a policy perspective, our insights suggest that there is potential space for formal task shifting within the everyday routines of neonatal nursing in Kenya. We suggest that careful study of context can help inform task-shifting design. When asked formally about the prospects for task-shifting, the nurses we spoke to had doubts and concerns, but their near continual reliance on organic forms of task shifting suggest that a carefully designed programme could be accepted. Kessler, Heron and Dopson [27] reveal in the United Kingdom health context that post-implementation, health care assistant roles are nearly always viewed very positively by nurses, patients and the new cadres themselves. They do however warn that the specific usefulness of these new human resources is rarely well understood, and hence, they are not strategically deployed despite their obvious potential in addressing HRH needs. Our findings also indicate that considerable work may be required at the policy level, dominated by professional institutions, experts and senior managers, to help bridge the apparent gap in acceptance of task shifting in this clinical arena.
Despite delegating many ‘nursing tasks’ to others, nurses maintained their distinctive role and power by authorizing to whom and how delegation of tasks was orchestrated in their wards. Their authority was mainly drawn from physically spending most of their time in the NBU and being constantly engaged in direct patient care, in contrast with the other more medical cadres. Nurses experiential knowledge of the wards, and what works and does not work, consequently authored the patterns of social organization and culture of work within the ward [43]. These are reinforced in the NBUs by the routines nurses keep. Routines and rituals exist to serve different needs [44, 45], and in our case, a template of routines helped nurses mentally manage tasks within shifts. They offer nurses a sense of control and accomplishment within chaotic work environments characterized by limited resources and staff shortages that make completion of all tasks, as the experts and seniors would have them conducted, an impossibility.
The description of organic practices and local norms established in response to work pressures provides useful guidance for the design of task-shifting initiatives [22]. For instance, we see that nurses prioritize their more technical roles. This inadvertently moves them further away from their traditional roles of providing bedside care and consequently helps delineate potentially acceptable nursing and task-shifting roles [46, 47]. To achieve multi-disciplinary holistic care, it is, however, important that professional role boundaries are negotiable and occupational jurisdictions remain flexible [43, 48], but the starting point for such endeavours is ensuring that roles are defined, that scopes of practice are understood, and that task allocations match capabilities.
Past studies in LMICs have described how lay health workers’ (LHWs) credibility is enhanced through visible ties to the health system through, among other things, visible contact with health professionals through referrals, supervisory visits and involving health professionals in training LHWs [20, 21]. In short, preliminary evidence suggests lay health workers are well-liked by patients. Health systems are however complex, dynamic and political systems, and this is particularly true in Kenya after the recent devolution, which has exacerbated human resources management challenges including disruptions, delays, and discrepancies in health workers’ salaries; resulted in political interference and discrimination in HRH management; and prompted frequent industrial actions by health workers [49]. The working environment of health workers across health facilities in the country has been characterized by fear, anxiety, mass resignations and low health worker morale. Many of these issues would affect a new cadre of health workers as they do the existing cadres. Challenges of health worker shortages and human HRH management in Kenya are chronic and largely remain unaddressed, and it is important that stakeholders do not perceive task shifting as a ‘fix all’ solution.
Limitations of the study
The title of this piece refers to ‘Kenyan hospitals’, but we recognize that our subset of urban examples may not address the experience of rural hospitals particularly well. It should be noted that rural hospitals often have even greater struggles in securing staff and so task-shifting may be more attractive to these organizations.
Further, we recognize that our research was conducted during a period of significant unrest in the Kenyan health system and that the strains we observed may have been exaggerated by this.
Finally, this study points to the potential space available for task shifting, and the needs such an approach might address, but it does not provide evidence of the likely success of task shifting in addressing major HRH shortfalls
Conclusion
In summary, our work described a routine template of neonatal nursing work which nurses used to enhance predictability when working in chaotic, resource-limited work environments. We detailed how this model of care deprioritizes less technical or less clinical tasks, which are then left to students, parents or other staff through ‘organic’ task shifting. Such insights are critical when considering more formal task-shifting projects as they help to delineate the tasks most easily shifted, and how best to support and work with busy nurses. While the profound effects of existing health system challenges (e.g. devolution, frequent strikes, delayed salaries and complexities around pay on hospital operations) on human resources management must also be addressed, our findings suggest there is space for a well-designed task-shifting programme that could have a positive and supportive effect on nursing care and on nurses themselves.
Additional file
Interview guide. (DOCX 23 kb)
Acknowledgements
We thank colleagues from the KEMRI-Wellcome Trust research programme, Prof Caroline Jones, Prof Gerry McGivern, the nurse stakeholders, participating hospitals and nurses that consented to the study for their support in the conduct of this review. This work is published with the permission of the Director of KEMRI.
Funding
The work of JN, JM and JJ was supported by a Health Systems Research Initiative joint grant provided by the Department for International Development, UK (DFID), Economic and Social Research Council (ESRC), Medical Research Council (MRC), and Wellcome Trust, grant number MR/M015386/1. ME’s work on this project was supported by a Wellcome Trust Senior Fellowship awarded to ME (#097170). All work benefited from additional funds from a Wellcome Trust core grant awarded to the KEMRI-Wellcome Trust Research Programme (#092654). This work is published with the permission of the Director of KEMRI.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- GHWA
Global Health Workforce Alliance
- HRH
Human resources for health
- LHWs
Lay health workers’
- LMICs
Low- and middle-income countries
- NBUs
Nairobi’s New Born Units
- NGT
Naso-gastric tube
- OPTIMIZEMNH
Optimizing Health Worker Roles to Improve Access to key Maternal and Newborn Health Interventions
- WHO
World Health Organization
Authors’ contributions
ME and JM designed the study with contributions from JN. JN and JM were responsible for the supervision of data collection which was primarily done by JJ supported by JN. JN and JM provided expertise on the data analysis which was conducted by JM, JN and JJ. JN wrote the manuscript with substantial critical input from all co-authors. All authors read and approved the final version of the manuscript.
Ethics approval and consent to participate
Ethical approval has been granted by the Kenya Medical Research Institute (KEMRI) Scientific and Ethics Review Unit (SSC protocol No. 2897).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jacinta Nzinga, Email: jnzinga@kemri-wellcome.org.
Jacob McKnight, Email: jacob.mcknight@ndm.ox.ac.uk.
Joyline Jepkosgei, Email: jjepkosgei@kemri-wellcome.org.
Mike English, Email: menglish@kemri-wellcome.org.
References
- 1.WHO . The Sustainable Development Goals Report 2018. 2018. [Google Scholar]
- 2.Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet. 2014;384(9940):347–370. doi: 10.1016/S0140-6736(14)60792-3. [DOI] [PubMed] [Google Scholar]
- 3.English M, Esamai F, Wasunna A, Were F, Ogutu B, Wamae A, et al. Delivery of paediatric care at the first-referral level in Kenya. Lancet. 2004;364(9445):1622–1629. doi: 10.1016/S0140-6736(04)17318-2. [DOI] [PubMed] [Google Scholar]
- 4.Van Lerberghe W. The world health report 2008: primary health care: now more than ever. Geneva: World Health Organization; 2008. 1211, 27.
- 5.Opondo C, Ntoburi S, Wagai J, Wafula J, Wasunna A, Were F, et al. Are hospitals prepared to support newborn survival?–an evaluation of eight first-referral level hospitals in Kenya. Tropical Med Int Health. 2009;14(10):1165–1172. doi: 10.1111/j.1365-3156.2009.02358.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aluvaala J, Nyamai R, Were F, Wasunna A, Kosgei R, Karumbi J, et al. Assessment of neonatal care in clinical training facilities in Kenya. Arch Dis Child. 2015;100(1):42–47. doi: 10.1136/archdischild-2014-306423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nzinga J, Mbindyo P, Mbaabu L, Warira A, English M. Documenting the experiences of health workers expected to implement guidelines during an intervention study in Kenyan hospitals. Implement Sci. 2009;4(1):44. doi: 10.1186/1748-5908-4-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gathara D, Opiyo N, Wagai J, Ntoburi S, Ayieko P, Opondo C, et al. Quality of hospital care for sick newborns and severely malnourished children in Kenya: a two-year descriptive study in 8 hospitals. BMC Health Serv Res. 2011;11(1):307. doi: 10.1186/1472-6963-11-307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Health Newborn Network . Saving premature babies by strengthening facility-based care in India. 2014. [Google Scholar]
- 10.Campbell J, Dussault G, Buchan J, Pozo-Martin F, Guerra Arias M, Leone C, Siyam A, Cometto G. A universal truth: no health without a workforce. Forum Report, Third Global Forum on Human Resources for Health, Recife, Brazil. Geneva, Global Health Workforce Alliance and World Health Organization, 2013.
- 11.Scheffler RM, Campbell J, Cometto G, Maeda A, Liu J, Bruckner TA, et al. Forecasting imbalances in the global health labor market and devising policy responses. Hum Resour Health. 2018;16(1):5. doi: 10.1186/s12960-017-0264-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murphy GA, Gathara D, Abuya N, Mwachiro J, Ochola S, Ayisi R, et al. What capacity exists to provide essential inpatient care to small and sick newborns in a high mortality urban setting?-a cross-sectional study in Nairobi City County, Kenya. PLoS One. 2018;13(4):e0196585. doi: 10.1371/journal.pone.0196585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murphy G, Gathara D, Mwachiro J, Abuya N, Aluvaala J, English M. Health Services that Deliver for Newborns Expert Group. Effective coverage of essential inpatient care for small and sick newborns in a high mortality urban setting: a cross-sectional study in Nairobi City County, Kenya. BMC medicine. 2018;16(1):72. 10.1186/s12916-018-1056-0. [DOI] [PMC free article] [PubMed]
- 14.British Association of Perinatal Medicine 2001. Standards for Hospitals Providing Neonatal Intensive and High Dependency Care and Categories of Babies requiring Neonatal Care. In: MEDICINE, B. A. O. P. (ed.). London.
- 15.NANN . Position statement #3009 - minimum RN staffing in NICUs. USA: National association neonatal nurses; 2009. [Google Scholar]
- 16.Wakaba M, Mbindyo P, Ochieng J, Kiriinya R, Todd J, Waudo A, et al. The public sector nursing workforce in Kenya: a county-level analysis. Hum Resour Health. 2014;12(1):6. doi: 10.1186/1478-4491-12-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organisation . Task shifting: rational redistribution of tasks among health workforce teams: global recommendations and guidelines. 2007. [Google Scholar]
- 18.World Health Organisation . WHO recommendations: optimizing health worker roles to improve access to key maternal and newborn health interventions through task shifting. Geneva: World Health Organization; 2012. [PubMed] [Google Scholar]
- 19.World Health Organization. The world health report 2006: working together for health. Geneva: World Health Organization; 2006.
- 20.Rashidian A, Shakibazadeh E, Karimi- Shahanjarini A, Glenton C, Noyes J, Lewin S, Colvin C, Laurant M. Barriers and facilitators to the implementation of doctor-nurse substitution strategies in primary care: qualitative evidence synthesis. Cochrane Database of Systematic Reviews. 2013; Issue 2. Art. No.: CD010412. 10.1002/14651858.CD010412. [DOI] [PMC free article] [PubMed]
- 21.Colvin CJ, de Heer J, Winterton L, Mellenkamp M, Glenton C, Noyes J, et al. A systematic review of qualitative evidence on barriers and facilitators to the implementation of task-shifting in midwifery services. Midwifery. 2013;29(10):1211–1221. doi: 10.1016/j.midw.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 22.Glenton C, Colvin CJ, Carlsen B, Swartz A, Lewin S, Noyes J, Rashidian A. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews. 2013; Issue 10. Art. No.:CD010414. 10.1002/14651858.CD010414.pub2. [DOI] [PMC free article] [PubMed]
- 23.Lewin S, Glenton C, Gulmezoglu A, Lavis J, Alvarez E. Optimizing health worker roles to improve access to key maternal and newborn health interventions through task shifting. WHO recommendations. 2012. [PubMed] [Google Scholar]
- 24.Mijovic H, McKnight J, English M. What does the literature tell us about health workers' experiences of task-shifting projects in sub-Saharan Africa? A systematic, qualitative review. Journal of clinical nursing, 2016;25(15-16):2083–100. [DOI] [PMC free article] [PubMed]
- 25.Seidman G, Atun R. Does task shifting yield cost savings and improve efficiency for health systems? A systematic review of evidence from low-income and middle-income countries. Hum Resour Health. 2017;15(1):29. doi: 10.1186/s12960-017-0200-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Church K, Lewin S. Delivering integrated HIV services: time for a client-centred approach to meet the sexual and reproductive health needs of people living with HIV? AIDS. 2010;24(2):189–193. doi: 10.1097/QAD.0b013e328333aeb3. [DOI] [PubMed] [Google Scholar]
- 27.Kessler I, Heron P, Dopson S. The modernization of the nursing workforce: valuing the healthcare assistant. Oxford: OUP; 2012. [Google Scholar]
- 28.Oluoch D, Murphy G, Gathara D, Abuya N, Nzinga J, English M, Jones C. Neonatal nursing policy and practice in Kenya: Key stakeholders and their views on task-shifting as an intervention to improve care quality. Wellcome Open Research, 3. 2018.
- 29.Ministry of Health RoK . Task Sharing Policy: 2017-2030. 2017. [Google Scholar]
- 30.Kane S, Kok M, Ormel H, Otiso L, Sidat M, Namakhoma I, et al. Limits and opportunities to community health worker empowerment: a multi-country comparative study. Soc Sci Med. 2016;164:27–34. doi: 10.1016/j.socscimed.2016.07.019. [DOI] [PubMed] [Google Scholar]
- 31.Mijovic H, McKnight J, English M. What does the literature tell us about health workers’ experiences of task-shifting projects in sub-Saharan Africa? A systematic, qualitative review. J Clin Nurs. 2016;25(15–16):2083–2100. doi: 10.1111/jocn.13349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.J-PO DS, Diarra A, Moha M. Travelling models and the challenge of pragmatic contexts and practical norms: the case of maternal health. Health Res Policy Syst. 2017;15(1):60. doi: 10.1186/s12961-017-0213-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.De Herdt T, De Sardan J-PO. Real Governance and Practical Norms in Sub-Saharan Africa: The game of the rules: Routledge: Abingdon; 2015.
- 34.Blaauw D, Gilson L, Penn-Kekana L, Schneider H. Organisational relationships and the? software? of health sector reform-background paper prepared for the Disease Control Priorities Project, Capacity Strengthening and Management reform. 2003. [Google Scholar]
- 35.Marchal B, Kegels G. Focusing on the software of managing health workers: what can we learn from high commitment management practices? Int J Health Plann Manag. 2008;23(4):299–311. doi: 10.1002/hpm.882. [DOI] [PubMed] [Google Scholar]
- 36.McCracken G. The long interview. Carlifornia: Sage; 1988.
- 37.Gioia DA, Corley KG, Hamilton AL. Seeking qualitative rigor in inductive research: notes on the Gioia methodology. Organ Res Methods. 2013;16(1):15–31. [Google Scholar]
- 38.Burawoy M. The extended case method. Sociol Theory. 1998;16(1):4–33. [Google Scholar]
- 39.Murphy GAV, Omondi GB, Gathara D, Abuya N, Mwachiro J, Kuria R, et al. Expectations for nursing care in newborn units in Kenya: moving from implicit to explicit standards. BMJ Global Health. 2018;3(2):e000645. doi: 10.1136/bmjgh-2017-000645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.GlDDENS A. The constitution of society. Outline of the theory of structuration. Cambridge: Polity; 1984. [Google Scholar]
- 41.Zerubavel E. Patterns of Time in Hospital Life. A Sociological Perspective. USA: University of Chicago Press; 1979.
- 42.Baker U, Hassan F, Hanson C, Manzi F, Marchant T, Peterson SS, et al. Unpredictability dictates quality of maternal and newborn care provision in rural Tanzania-a qualitative study of health workers’ perspectives. BMC Pregnancy Childbirth. 2017;17(1):55. doi: 10.1186/s12884-017-1230-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carmel S. Boundaries obscured and boundaries reinforced: incorporation as a strategy of occupational enhancement for intensive care. Sociol Health Illn. 2006;28(2):154–177. doi: 10.1111/j.1467-9566.2006.00486.x. [DOI] [PubMed] [Google Scholar]
- 44.Helman CG. Ritual and the Management of Misfortune. Culture, Health Illn. 2000:157–69.
- 45.Lewin S, Green J. Ritual and the organisation of care in primary care clinics in Cape Town, South Africa. Soc Sci Med. 2009;68(8):1464–1471. doi: 10.1016/j.socscimed.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 46.Dingwall R, Allen D. The implications of healthcare reforms for the profession of nursing. Nurs Inq. 2001;8(2):64–74. doi: 10.1046/j.1440-1800.2001.00100.x. [DOI] [PubMed] [Google Scholar]
- 47.Hasson F, McKenna HP, Keeney S. Perceptions of the unregistered healthcare worker’s role in pre-registration student nurses’ clinical training. J Adv Nurs. 2013;69(7):1618–1629. doi: 10.1111/jan.12023. [DOI] [PubMed] [Google Scholar]
- 48.Curtis P, Woodhill R, Stapleton H. The peer-professional interface in a community-based, breast feeding peer-support project. Midwifery. 2007;23(2):146–156. doi: 10.1016/j.midw.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 49.Tsofa B, Goodman C, Gilson L, Molyneux S. Devolution and its effects on health workforce and commodities management–early implementation experiences in Kilifi County, Kenya. Int J Equity Health. 2017;16(1):169. doi: 10.1186/s12939-017-0663-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Interview guide. (DOCX 23 kb)
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.