Abstract
This systematic review examined factors associated with overuse of colorectal cancer (CRC) screening. The authors searched MEDLINE and EMBASE from January 1998 to March 2017. Studies were included if they were written in English, contained original data, involved a US population, and examined factors potentially associated with overuse of CRC screening. Paired reviewers independently screened abstracts, assessed quality, and extracted data. In 8 studies, the associations between patient factors, including age, sex, race, and number of comorbidities, were tested and were inconsistently associated with CRC screening overuse. Overuse of screening was greater in the Northeast/Mid-Atlantic regions and in urban areas and was lower in academically affiliated centers. Although the literature supports important overuse of CRC screening, it remains unclear what drives these practices. Future research should thoroughly explore these factors and test the impact of interventions to reduce overuse of screening.
Keywords: screening, overuse, colorectal cancer
Health outcomes in the United States lag behind those of other developed nations despite higher health expenditures.1–4 The disparity between costs and outcomes of care in the United States suggests that health care services are over-used in the United States,5 including screening for cancers. Clinical practice guidelines typically make recommendations to screen patients for cancer if they are from populations who are likely to benefit and at intervals that do not raise the false positive rates of cancer detection excessively. Despite these recommendations, excessive screening likely is widespread in the United States across cancer types.6–9
The lists of the Choosing Wisely campaign include at least 22 items for discussion about cancer screening.10 Colorectal screening typically is recommended for asymptomatic, average-risk adults aged 50 to 75 years (US Preventive Services Task Force [USPSTF]), but screening contrary to guideline recommendations is prevalent.6,11 However, the determinants of this screening overuse are poorly understood. This is additionally complicated in that the factors that drive the overuse of initial colorectal cancer (CRC) screening, which often is ordered by a primary care provider, may differ from those driving overuse of repeat screening, which is influenced more by the involved gastroenterologist. Therefore, this study sought to systematically review the literature to identify factors that have been identified to be positively or negatively associated with overuse of initial and repeat CRC screening. An understanding of the drivers of this practice should inform clinical and policy interventions to lessen this type of overuse.
Methods
Data Sources and Searches
Reported here is a segment of the results from a broader systematic review on determinants of overuse of health services. The protocol was registered in Prospero (#42015029482). In framing this systematic review, the research team considered overuse to be the provision of health care services when the likelihood of harm exceeds the likelihood of benefit.12
The team searched MEDLINE and EMBASE from January 1998 through July 2016 and developed a search strategy by using medical subject heading (MeSH) terms and keywords relevant to the overuse of health care services, including procedures and diagnostic tests to define the breadth of this literature. The first search included “medical overuse,” OR “health services misuse,” OR “health services overutilization,” OR “unnecessary procedures,” OR “medically unnecessary procedures,” OR “diagnostic tests, routine/utilization,” OR “defensive medicine,” OR “practice patterns,” OR “health services abuse,” OR “health services overuse,” OR “medical overutilization,” OR “inappropriate utilization.”
The search was then updated through March 2017 with a specific search for articles addressing cancer screening. The focused search included “early detection of cancer OR mass screening,” OR “breast neoplasms,” OR “mammography,” OR “Papanicolaou test,” OR “uterine cervical neo-plasms,” OR “vaginal smears,” OR “colorectal neoplasms,” OR “colonoscopy,” OR “breast cancer screening,” OR “colorectal cancer screening,” OR “cervical cancer screening,” OR “prostate cancer screening,” OR “endoscopic,” OR “Pap tests,” OR “prostate-specific antigen.”
The research team limited the search start date to January 1998 given differences in the health care environment since that time. The team hand searched the reference lists of each included article as well as related systematic reviews for additional articles. The team did not contact any authors and did not include any unpublished studies.
Study Selection
Two reviewers independently screened titles, abstracts, and articles and came to consensus about inclusion. Inclusions were original, English-language studies not exclusively describing care delivered outside of the United States. Included studies needed to describe the use of a test for detection of CRC, and explore the association between a hypothesized determinant and overuse of the test, as operationalized by the authors (Table 1). There were no restrictions regarding study design, including both quantitative and qualitative studies, but excluding studies that exclusively used data collected prior to 1996.
Table 1.
Definitions of Overuse in Included Studies.
| Definitions of Overuse of Colorectal Cancer Screening in Included Studies |
|---|
| Too frequent |
| • Too frequent screening colonoscopies14,18 |
| • Too frequent fecal occult blood testing (FOBT) use following previous FOBT test16 |
| • Too frequent FOBT test following another procedure (colonoscopy or barium enema)16 |
| • Too frequent screening (FOBT, sigmoidoscopy, or colonoscopy) following previous screening21 |
| Early repeat |
| • Early repeat colonoscopy without indication17 |
| • Physician recommendation for early follow-up after a normal colonoscopy20 |
| Population unlikely to benefit |
| • Inappropriate colonoscopies in older patients15 |
| • Inappropriate screening in patients with limited life expectancy18,21 |
| Guideline nonadherence |
| • Physician nonadherence to colonoscopy guidelines19 |
Data Extraction, Quality, and Applicability Assessment
The research team created and pilot tested data extraction forms in Excel (Microsoft, Redmond, WA). Reviewers extracted information on the study and participant characteristics, the methods of data collection, the screening event, the factors evaluated, and the factors identified as being significantly (as defined in the article) associated with the overused screening event. The factors were classified as being related to the patient, clinician, or environment, which includes the health system. One reviewer completed the data abstraction, and a second reviewer checked the first reviewer’s abstraction for completeness and accuracy. Differences of opinion were resolved through discussion and, as needed, through consensus among the team.
Two reviewers independently assessed the quality of individual studies. Critical Appraisal Checklist (Center for Evidence-Based Management) was used to appraise included studies.13
Data Synthesis and Analysis
The research team created a set of detailed evidence tables. The team qualitatively synthesized the results by the category of the factors (patient, clinician, environment) and created summary tables of these results. Highlighted in the text are the most consistent results across studies. The team recognizes that the statistical significance of each factor may depend on what other factors were included in multivariate models.
Results
A total of 12 583 titles were identified that met the inclusion criteria (Figure 1). From these, 564 articles were identified for full-text review, 8 of which examined factors of overuse of CRC screening.14–21
Figure 1.
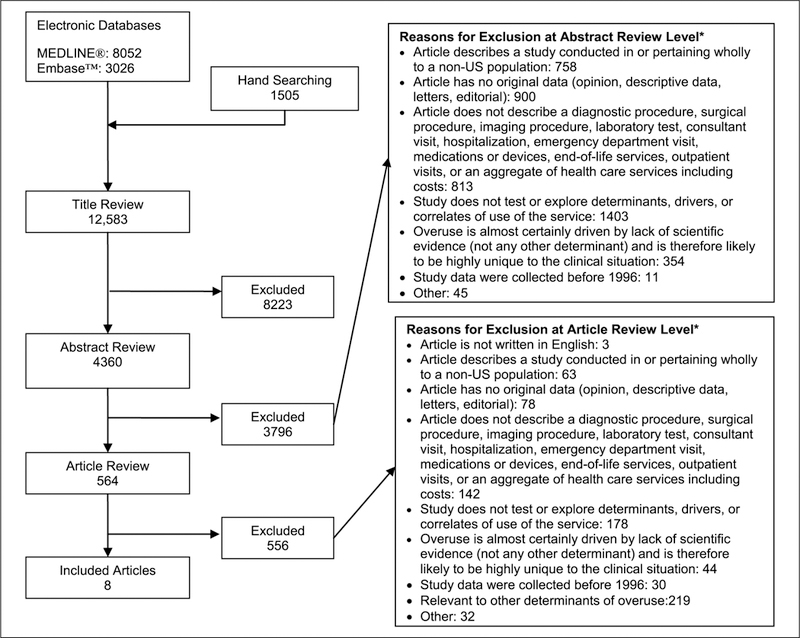
Summary of the literature search.
*Reviewers did not need to agree on reason for exclusion.
Characteristics of Included Studies
Among the included studies were 6 retrospective cohort studies,14,15,17,19–21 1 survey-based study,16 and 1 cross-sectional analysis.18 Colon cancer screening modalities included colonoscopy, sigmoidoscopy, and fecal occult blood testing (FOBT). The definitions of overuse varied widely across studies and included screening more frequently than recommended by guidelines, screening in older patients unlikely to benefit, and lack of physician knowledge of guidelines (Table 1).
Risk of Bias
The risk of bias was assessed as low in 7 of the 8 studies. One study had a moderate risk of bias because of the lack of information about physicians recommending follow-up and the use of a nonvalidated scale.20
Factors Associated With Overuse of Colorectal Cancer Screening
The results of the abstraction are found in Table 2, which shows the factors found to be statistically significant predictors of overuse in the final multivariable model in each included study. Table 3 shows these models, presenting both the variables found to be statistically significant and the other covariates included.
Table 2.
Colorectal Cancer Screening and Significant Findings.
| Author, Year; Study Design | Sampling Frame; Data Source | Population Experiencing an Overuse Event | Rate of Observations of Overuse Events | Significant Determinants of Screening Overuse |
|---|---|---|---|---|
| Initial colonoscopy | ||||
| Kruse, 201514; retrospective cohort; n = 1429 | Health system; 17 ambulatory sites across Massachusetts (multispecialty group practice, primary care patients—Harvard Vanguard) | Patients having endoscopists who recommend early interval follow-up | 382 (88.2%) Exams among screening colonoscopies were considered overuse | Clinician: early interval follow-up recommended by the endoscopist |
| Powell, 201518; cross-sectional; n = 1 035 627 | Health system; VHA Administrative Claims database | Patients aged 50 years and older | 26% of FOBT screening and 14% of screening colonoscopies were potentially inappropriatea | Patient: each additional 10 years of age,
female, African American or Hispanic or other (American Indian),
divorced/separated, single or widowed System and environment: complexity score of middle third |
| Repeat colonoscopy | ||||
| Goodwin, 201117; retrospective cohort; n = 24 071 | National; 5% Medicare sample | Men aged 66 years or older | 24% Early repeated colonoscopy without clear indication (out of 24 071 patients who underwent normal screening colonoscopy) | Patient: younger, male, less education, 1 or
more comorbidity Clinician: high volume of colonoscopies System and environment: office initial place of service, metropolitan, Mid-Atlantic |
| Partin, 201216; survey; n = 1844 | Health system; VHA facility patients (nationally representative sample from 24 VHA facilities) | Patients aged 50–75 years after prior
FOBT Patients aged 50–75 years after other procedure |
323 FOBT (8%) 562 FOBT (13%) |
Patient: increased with number of outpatient
visits System and environment: significantly lower in the Midwest and Northwest |
| Sheffield, 201315; retrospective cohort; n = 74 681 | State; 100% Medicare claims (Texas), enrollment files (Texas), AMA physician file | Patients aged 76 years or older Patients aged 76 years or older with no indication or claims for 3 months Patients aged 70–75 years | 23% of Colonoscopies were potentially inappropriate 19% of Colonoscopies were probably inappropriate 10% of Colonoscopy patients aged >70 years were potentially inappropriate | Patient: male, fewer comorbidities, less
education Clinician: generalists, surgeon, and other specialties, more volume colonoscopies, US-trained colonoscopist System and environment: metropolitan, colonoscopy in ambulatory surgical center or office setting |
| Menees, 201420; retrospective cohort; n = 1387 | VHA Administrative Claims database (Ann Arbor VAHCS), 2 University of Michigan outpatient ASCs | Patients aged 50 years and older with no polyps identified during colonoscopy | 332 of 1387 Patients (23.9%) received followup instructions inconsistent with guidelines | Patient: age (older than 70 years), fair or poor bowel prep, type of bowel preparation (did not use MiraLAX/Gatorade prep) |
| Saini, 201421; retrospective cohort; n = 399 067 | National; VHA Administrative Claims database | Patients aged 50 years and older | 3516 of 8814 Patients (40%) with limited life expectancy had screening test within 24 months | Patient: age and health status interaction (overuse seen in patients with both CCI >3 and ages between 70 and 75 years old) |
| Repeat, surveillance | ||||
| Murphy, 201619; retrospective cohort; n = 1455 | Health system; VHA Administrative Claims database for 25 Veterans Health Centers | Patients aged 50–64 years with no adenomas | Overused colonoscopies for 16% of patients with no adenomas | Clinician: nonadherent followup
recommendation System and environment: non-academically affiliated facility |
Abbreviations: AMA, American Medical Association; ASC, ambulatory surgery center; CCI, Charlson Comorbidity Index; FOBT, fecal occult blood testing; VAHCS, Veterans Affairs Health Care System; VHA, Veterans Health Administration.
This study uses 5 definitions of overuse. These two are included for illustrative purposes.
Table 3.
Comparison of Models Used in Each Study.a
| Author, year | Patient Factors |
Clinician Factors |
System/Environmental
Factors |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | Sex/Gender | Race/Ethnicity | Income | Marital Status | Education | Comorbidities | Bowel Preparation | Prior Exam Findings | Utilization | Specialty | Volume | Country of Training | Age | Clinician Recommendation | GI Fellow Involvement | Clinic/Hospital/ASC | Geography | Utilization (System-Wide) | Insurance Status | Urban/Rural | Academic | |
| Goodwin, 201117 | X | X | O | X | X | O | X | X | X | X | ||||||||||||
| Partin, 201216 | O | O | O | O | O | X | O | X | X | |||||||||||||
| Sheffield, 201315 | O | X | X | X | X | X | X | X | O | X | O | X | ||||||||||
| Menees, 201420 | X | O | O | O | X | O | O | |||||||||||||||
| Saini, 201421 | Xb | O | Xb | O | ||||||||||||||||||
| Kruse, 201514 | O | O | O | O | O | O | X | O | ||||||||||||||
| Powell, 201518,c | X | X | X | X | O | O | O | O | ||||||||||||||
| Murphy, 201619 | O | O | O | O | O | O | X | O | X | |||||||||||||
Abbreviations: ASC, ambulatory surgery center; GI, gastrointestinal.
X = Found to be significantly associated with overuse. O = Included in the model but was not found to be significantly associated with overuse. Blank = Not included in model.
Age and sex interaction was found to be significantly associated with overuse.
Multiple models—these factors were found to be significant in the majority of them.
Patient Factors
All 8 studies evaluated patient factors contributing to overuse.14–21 All 8 evaluated the association between patient sex and screening overuse; 2 reported that men were at higher risk of overuse than women15,17; one study found that women were at higher risk for too frequent screening with FOBT compared to men, but men with short life expectancy were at greater risk for too frequent screening with FOBT and colonoscopy than similar women.18 The other 5 studies found no association between sex and screening overuse.14,16,19–21
Age was explored as a possible contributor to overuse in all 8 studies, with markedly inconsistent findings about the relationship between age and screening overuse.14–21 One retrospective cohort20 and one cross-sectional study18 found higher rates of overuse in older patients (defined as patients older than age 70 years in the retrospective cohort20 and each additional 10 years of age in the crosssectional study18), whereas another retrospective cohort17 found higher rates of overuse in younger patients (those younger than 75 years). Additionally, 5 studies found no relationship between age and overuse (though one found that an interaction between age and comorbidities was associated with overuse21).14–16,19,21 Seven studies14–20 evaluated the relationship between race or ethnicity and overuse, with 2 finding a significant association.15,18 One study found higher rates of excessive screening in patients who were African American, Hispanic, or other races (ie, American Indian) relative to white patients. Another study reported that whites had higher odds of potentially inappropriate colonoscopies relative to blacks.15
Educational attainment was explored as a determinant in 3 studies.15–17 In the 2 cohort studies using Medicare data, lower rates of education were associated with overuse within a region; this was operationalized as the educational level within the zip code of residence.15,17
Comorbidities were studied as determinants in 5 studies.15,17,19–21 Two cohort studies using Medicare claims15,17 found significant, although different, results. CRC screening overuse was higher among people with more comorbidities relative to fewer in one study.17 However, in the cohort study by Sheffield et al,15 people with fewer comorbidities were at greater risk of inappropriate colonoscopies. This cohort was restricted to individuals aged 75 years and older. One study examined the impact of the interaction between age and comorbidities, finding significantly greater odds of excessive screening test use in patients between the ages of 70 and 75 years with a high Charlson Comorbidity Index (CCI) score than in patients 76 years old with low CCI scores.21 Three studies found no association between patient comorbidities and overuse.18–20
One study found that patients having more outpatient visits were more likely to experience overuse relative to patients with fewer outpatient visits,16 whereas 2 found no association between number of visits and overuse.14,21 Two studies looked at the quality of the patient’s bowel preparation. One study found fair or poor bowel preparation during the initial colonoscopy to be significantly associated with recommendation for an early follow-up colonoscopy,20 whereas the other found no effect of bowel preparation on actual early follow-up.14 Several other factors were examined in independent studies, including income (not significant),16 marital status (more overuse in people single, divorced, or widowed compared to married),18 and prior exam findings (not significant).14
Clinician Factors
Six of the 8 studies evaluated clinician factors as determinants of overuse.14,15,17–20 Two cohort studies using Medicare data reported that a higher volume of colonoscopies per endoscopist was significantly associated with CRC screening overuse.15,17 Two cohort studies reported that a recommendation for an early repeat procedure by the endoscopist was a significant determinant of overuse of screening colonoscopies.14,19
One study reported that US-trained colonoscopists were significantly more likely to perform potentially inappropriate colonoscopies than internationally trained doctors.15 Two studies reported that clinician specialty was not a significant determinant of overuse17,19; however, another study reported that surgeons were more likely to overutilize colonoscopies than gastroenterologists.15 The latter study was much larger and better powered to detect differences.15 Two retrospective cohort studies found that the number of years in practice was not predictive of overuse of CRC screening.15,19
One study found that the presence of fellows during the initial colonoscopy was not predictive of excessively early follow-up.20
System or Environmental Factors
Seven of the 8 studies evaluated systemic or environmental factors as determinants of overuse of CRC screening.14–20 One cohort study of patients in Massachusetts14 reported that insurance status was not significantly associated with colonoscopy overuse. Two claims-based cohort studies found that unnecessary early follow-up was more likely to be recommended at an ambulatory surgical center15 or office15,17 as compared to a hospital-based facility. Nonacademic facilities had more overuse of colonoscopy and lower reported adherence to guidelines in one study.19 High-volume sites had more colonoscopy and FOBT overuse in 2 studies.16,18
Five15–19 studies evaluated geographic region as a determinant of overuse, with one finding significantly higher rates of overuse in the Northeast, South, and Southwest (compared to Midwest and Northwest)16 and another finding greater overuse in the Mid-Atlantic than any other region.17 Two reported that overuse was significantly associated with residence in metropolitan areas compared to nonmetropolitan areas.15,17
Discussion
The research team identified 8 studies evaluating patient, clinician, or environmental factors associated with overuse of CRC screening. Although there have been recent systematic reviews quantifying overuse of CRC screening and surveillance,22,23 these reviews did not seek to summarize why this happens, as was done here.
Most of the included studies used definitions for overuse that reflect guideline-discordant care: overuse defined as screening more frequently than guidelines recommend, or in a population who are unlikely to benefit (such as because of a competing risk of death), or where there is little evidence of clinical utility. Some of the overuse definitions, however, reflect the use of testing where the downstream harms may be prominent even if the direct harms of screening are few, such as too frequent FOBT testing. Despite these differences in the outcome definitions, the research team identified consistent associations that may prove to be actionable.
A factor that was consistent across studies was that physicians who are unaware of guidelines, or who have low confidence in guidelines, or who perceive conflict in the recommendations across guidelines are more likely to overuse screening than clinicians who are committed to practicing guideline-concordant care. This was a more consistent factor influencing overuse than characteristics of the physician, such as specialty, site of training, or age, or characteristics of the patient, such as age, sex, or race/ethnicity. Other clinician factors that were found to be determinants of overuse include higher volumes of colonoscopies performed by the endoscopist and the endoscopist’s recommendation for early follow-up.
There were conflicting results about the relationship between bowel preparation prior to screening colonoscopy and overuse. One study found “fair or poor” bowel preparation to be highly predictive of overuse,20 whereas the other did not.12 The reader might argue that studies of the impact of inadequate bowel preparation on utilization are unfairly included in this review; however, the research team opted to use the definitions of overuse as provided by the study authors. It should be noted, however, that bowel preparation quality was described in only 2 of the 7 observational studies.14,20 The absence of description of bowel preparation adequacy hampers the interpretation of the other studies. Future studies exploring determinants of colonoscopy overuse should aim to assess the adequacy of bowel preparation and report it with a validated measure of bowel preparation adequacy (eg, Aronchick Scale, the Boston Bowel Preparation Scale).24
Which of these factors identified as being associated with inappropriate CRC screening might be modifiable—acknowledging that this must not interrupt necessary and appropriate screening? The USPSTF, established in 1984, makes evidence-based recommendations regarding effective preventive services,25 yet its recommendations are not always concordant with the recommendations from professional societies, especially as more stool-based tests such as the multi-targeted stool DNA test become available26 and are added to recommendations. This discordance almost certainly contributes to a lack of confidence among clinicians. Attention to the quality and evidence base of guidelines may increase physician confidence in guidelines; efforts for consistency across guidelines from professional societies and from other guideline-producing organizations may go a long way toward confident application of guideline recommendations. Additionally, further study is needed to determine how the design of quality measures influences adherence to guidelines. For example, although many quality measures use age as a key factor to determine which patients are eligible for inclusion in a measure’s denominator, projected life expectancy as determined by a measure of comorbidity may be a more important factor for inclusion. One of the included studies explored this phenomenon in detail, finding suspected overuse of screening colonoscopy in ill 74-year-olds but underuse in healthy 76-year-olds.21
Additionally, practitioners developing interventions and researchers conducting studies should account for potential substitution effects. For example, if an effort to reduce use of too frequent FOBT results in an uptick in unnecessary screening colonoscopies, this would be an unintended, harmful consequence of the intervention.
The factors that appear to be driven by market forces may be amenable to regulation. Because several studies found an association between a higher volume of colonoscopies performed by a provider and a higher proportion of potentially inappropriate procedures, these high-volume providers may warrant oversight. Additionally, because the geographic region in which a clinic is located can be a driver of overuse, the research team wonders about the value of a demonstration of regional need before new endoscopy facilities are authorized, such as is done with Certification of Need state laws,27 although at present these laws are applied only to hospital and nursing home beds, and hospice services.
This systematic review necessarily has limitations. A major limitation is the varying definitions of overuse across the studies. Some studies characterized overuse as intent to have an unnecessary treatment, and other studies characterized overuse by looking at actual procedures performed. Additionally, some studies looked at initial screening, and others looked at repeat screening. Although this systematic review did not find any major differences between the factors associated with overuse in initial and repeat screening, future studies of overuse should consider that factors may vary across these different types of screening and the types of clinicians who order them (primary care physicians compared with specialists). The research team also found 2 survey-based studies that measured physician attitudes toward overuse and recommendations in response to clinical vignettes but did not include these in the final analysis because they did not measure actual overuse.28,29
Five of the 8 studies used data about veterans’ use of CRC screening (4 used data from the Veterans Health Administration [VHA] exclusively). This limits the generalizability of the findings because the patient populations are predominantly male and have baseline levels of education, income, and other social factors that differ from the general US population. Additionally, the salaried physicians working at the VHA face different financial incentives than gastroenterologists who receive fee-for-service reimbursements from both public and private payers. Furthermore, veterans receiving some of their care outside of the VHA may not have all of their utilization included in these analyses.
Although there were some limitations to this review, there were many strengths. The use of a second reviewer minimized the likelihood of incorrect extraction of data about factors of overuse. The research team assessed the quality of the included articles using validity instruments.
Conclusion
This review summarized factors that were hypothesized to contribute to overuse of CRC screening. Although the literature has richly established that CRC screening overuse is prevalent, it remains unclear as to what is driving these screening practices. The literature investigating this is sparse. Differences among patients do not appear to consistently drive the overuse in CRC screening. Most of the impactful factors are attributes of the clinician or the clinician’s site of practice. Future research should test the impact of interventions to reduce overuse of CRC screening, but not until the determinants are better understood. This research needs to be done with the utmost attention to maintaining appropriate CRC screening among patients who can be expected to benefit.
Acknowledgment
We would like to acknowledge Madeline Jackson, BA, who helped with article screening and data abstraction checking.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: We acknowledge the funding support from K24 AG049036–01A1 from the National Institute on Aging (JBS, RS); U1QHP28710 from the Health Resource and Services Administration (SN); 2016 MSTAR Summer Scholar from the American Federation for Research Training (JP); the Johns Hopkins University Dean’s Fund (MT); the Agency for Healthcare Research and Quality T32 Institutional Predoctoral Training Grant to Johns Hopkins University (ZP). The funders had no role in the study.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA 2012;307:1801–1802. [DOI] [PubMed] [Google Scholar]
- 2.Grady D, Redberg RF. Less is more: how less health care can result in better health. Arch Intern Med 2010;170:749–750. [DOI] [PubMed] [Google Scholar]
- 3.Ackerman S, Gonzales R. The context of antibiotic overuse. Ann Intern Med 2012;157:211–212. [DOI] [PubMed] [Google Scholar]
- 4.US Government Accountability Office. Patient Protection and Affordable Care Act: effect of long-term federal budget outlook depends on cost containment sustained http://www.gao.gov/assets/660/651702.pdf. Accessed October 14, 2014.
- 5.Reinhardt UE, Hussey PS, Anderson GF. U.S. health care spending in an international context. Health Aff (Millwood) 2004;23(3):10–25. [DOI] [PubMed] [Google Scholar]
- 6.Korenstein D, Falk R, Howell EA, Bishop T, Keyhani S. Overuse of health care services in the United States: an understudied problem. Arch Intern Med 2012;172:171–178. [DOI] [PubMed] [Google Scholar]
- 7.Baxi SS, Kale M, Keyhani S, et al. Overuse of health care services in the management of cancer: a systematic review. Med Care 2017;55:723–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kale MS, Bishop TF, Federman AD, Keyhani S. Trends in the overuse of ambulatory health care services in the United States. JAMA Intern Med 2013;173:142–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilt TJ, Harris RP, Qaseem A. Screening for cancer: advice for high-value care from the American College of Physicians. Ann Intern Med 2015;162:718–725. [DOI] [PubMed] [Google Scholar]
- 10.Choosing Wisely. Promoting conversations between patients and clinicians http://www.choosingwisely.org/. Accessed April 10, 2017.
- 11.Krist AH, Jones RM, Woolf SH, et al. Timing of repeat colonoscopy: disparity between guidelines and endoscopists’ recommendation. Am J Prev Med 2007;33:471–478. [DOI] [PubMed] [Google Scholar]
- 12.Agency for Health care Research and Quality. Glossary: underuse, overuse, misuse https://psnet.ahrq.gov/glossary/u. Accessed October 18, 2014.
- 13.Center for Evidence Based Management. Critical appraisal of a survey https://www.cebma.org/wp-content/uploads/Critical-Appraisal-Questions-for-a-Survey.pdf. Accessed January 16, 2017.
- 14.Kruse GR, Khan SM, Zaslavsky AM, Ayanian JZ, Sequist TD. Overuse of colonoscopy for colorectal cancer screening and surveillance. J Gen Intern Med 2015; 30:277–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sheffield KM, Han Y, Kuo YF, Riall TS, Goodwin JS. Potentially inappropriate screening colonoscopy in Medicare patients: variation by physician and geographic region. JAMA Intern Med 2013;173:542–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Partin MR, Powell AA, Bangerter A, et al. Levels and variation in overuse of fecal occult blood testing in the Veterans Health Administration. J Gen Intern Med 2012;27:1618–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goodwin JS, Singh A, Reddy N, Riall TS, Kuo YF. Overuse of screening colonoscopy in the Medicare population. Arch Intern Med 2011;171:1335–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Powell AA, Saini SD, Breitenstein MK, et al. Rates and correlates of potentially inappropriate colorectal cancer screening in the Veterans Health Administration. J Gen Intern Med 2015;30:732–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Murphy CC, Sandler RS, Grubber JM, Johnson MR, Fisher DA. Underuse and overuse of colonoscopy for repeat screening and surveillance in the Veterans Health Administration. Clin Gastroenterol Hepatol 2016;14:436.e1–444.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Menees SB, Elliott E, Govani S, et al. The impact of bowel cleansing on follow-up recommendations in average-risk patients with a normal colonoscopy. Am J Gastroenterol 2014;109:148–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saini SD, Vijan S, Schoenfeld P, Powell AA, Moser S, Kerr EA. Role of quality measurement in inappropriate use of screening for colorectal cancer: retrospective cohort study. BMJ 2014;348:g1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carpentier MY, Vernon SW, Bartholomew LK, Murphy CC, Bluethmann SM. Receipt of recommended surveillance among colorectal cancer survivors: a systematic review. J Cancer Surviv 2013;7:464–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holden DJ, Jonas DE, Porterfield DS, Reuland D, Harris R. Systematic review: enhancing the use and quality of colorectal cancer screening. Ann Intern Med 2010;152: 668–676. [DOI] [PubMed] [Google Scholar]
- 24.Parmar R, Martel M, Rostom A, Barkun AN. Validated scales for colon cleansing: a systematic review. Am J Gastroenterol 2016;111:197–204. [DOI] [PubMed] [Google Scholar]
- 25.US Preventive Services Task Force. About the USPSTF https://www.uspreventiveservicestaskforce.org/Page/Name/about-the-uspstf. Accessed April 10, 2017.
- 26.Ransohoff DF, Sox HC. Clinical practice guidelines for colorectal cancer screening: new recommendations and new challenges. JAMA 2016;315:2529–2531. [DOI] [PubMed] [Google Scholar]
- 27.National Conference of State Legislatures. CON–Certificate of Need state laws http://www.ncsl.org/research/health/con-certificate-of-need-state-laws.aspx. Accessed December 20, 2016.
- 28.Iskandar H, Yan Y, Elwing J, Early D, Colditz GA, Wang JS. Predictors of poor adherence of US gastroenterologists with colonoscopy screening and surveillance guidelines. Dig Dis Sci 2015;60:971–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kadivar H, Goff BA, Phillips WR, Andrilla CH, Berg AO, Baldwin LM. Nonrecommended breast and colorectal cancer screening for young women: a vignette-based survey. Am J Prev Med 2012;43:231–239. [DOI] [PubMed] [Google Scholar]


