Abstract
Objective
This study sought to investigate factors associated with opioid misuse-related emergency department (ED) visits among older adults and changes in outcomes associated with these visits, using multiple years of nationally representative data.
Methods
A retrospective analysis of the Nationwide Emergency Department Sample was conducted. Study inclusion was limited to adults aged 65 years and older. Diagnostic codes were used to identify opioid misuse disorder; sampling weights were used to adjust standard estimates of the errors. Descriptive and multivariate procedures were used to describe risk and visit outcomes.
Results
ED visits by older adults with opioid misuse identified in the ED increased sharply from 2006 to 2014, representing a nearly 220% increase over the study period. Opioid misuse was associated with an increased number of chronic conditions, greater injury risk, and higher rates of alcohol dependence and mental health diagnoses.
Conclusion
The steep increase in opioid misuse observed among older adult ED visits underscores the critical need for additional research to better understand the national scope and impact of opioid misuse on older adults, as well as to better inform policy responses to meet the needs of this particular age group.
Keywords: Emergency department, Hospital, Older adults, Opioid misuse, Opioid use, Substance abuse, Substance abuse disorder, Trends
Translational Significance
Findings demonstrate the breadth and scope of opioid misuse and dependence among older adults visiting emergency departments and indicate that targeted programs aimed at screening, intervention, and treatment specifically geared toward older adults are warranted. Results from this study also highlight the complexity of treating opioid dependence in this population, which reflect in part, high rates of coexisting mental health and other substance abuse disorders. When considered together, these findings underscore the pressing need for policy changes to increase access to long-term substance misuse treatment and support needs.
Recent estimates indicate that one third of all Medicare Part D participants received a prescription opioid in 2016, with more than 10% receiving long-term (3+ months) opioid prescriptions for noncancer-related pain (OIG, 2017). Despite recently issued Centers for Disease Control and Prevention (CDC) prescribing guidelines (CDC, 2016), the OIG (2017) found that more than 500,000 Medicaid beneficiaries with opioid prescriptions received excessively high dosages, issued over extended periods of time. Moreover, rising concern regarding increasing opioid prescription use among older adults (Campbell et al., 2010) and the potential consequences associated with opioid use, including falls (Blachman, Leipzig, Mazumdar, & Poeran, 2017), respiratory distress (Nagappa, Weingarten, Montandon, Sprung, & Chung, 2017), delirium (Swart, van der Zanden, Spies, de Rooij, & van Munster, 2017), and other adverse events (Chau, Walker, Pai, & Cho, 2008), has been overshadowed by the broader impact of the epidemic affecting younger adults, especially young- and middle-aged men (e.g., Economic Aspects of the Opioid Crisis, 2017; Erwin, 2017; Lasser, 2017).
Accordingly, increasing opioid misuse among older adults has unfolded against a national public health crisis, with more than 600,000 opioid-related deaths reported since 2000, and approximately 91 opioid-related deaths occurring each day across the United States (CDC, 2016). Described as the largest human-made epidemic in public health history (Kolodny et al., 2015; Okie, 2010), the opioid crisis has overwhelmed community and public health agencies, and stretched medical systems and first responders beyond capacity (NAS, 2017), with related expenditures exceeding $78 billion dollars annually (Florence, Zhou, Luo, & Xu, 2016), and contributing to overall declines in U.S. life expectancy (Dowell et al., 2017).
Although public policy and health experts have responded to the epidemic’s effects on younger populations by mobilizing resources and calling for action (Han, Compton, Jones, & Cai, 2015; Manchikanti, 2006), empirical research investigating national trends of opioid misuse among adults aged 65+ is lacking (Le Roux, Tang, & Drexler, 2016). This paucity exists despite older adults’ higher use of prescription opioids (Frenk, Porter, & Paulozzi, 2016), evidence of increasing misuse (SAMHSA, 2017), and risk associated with long-term use (Solomon et al., 2010). Moreover, the effort to understand the scope of the problem among older adults has been further limited by inconsistent definitions used in the extant literature, with age categories labeled, “older adults,” defined as 45+, 50+, 55+, and 60+ (Carew & Comiskey, 2018). Given differences in access and need of health care services associated with age, inconsistent definitions impede policy understanding, as well as basic knowledge about the impact of the crisis on older adults. Thus, research using standard definitions is vital to developing prevention strategies focused specifically on improving intervention and outreach for older adults with substance misuse disorders (Burgos-Chapman, Trevisan, & Sevarino, 2016), as well as for informing broader public policy discussions regarding opioid misuse among older adults.
In response, this study reports on an effort to describe population estimates of emergency department (ED) use and outcomes among older adults (aged 65+, aged 85+) with opioid misuse identified during patient encounters, using a large, nationally representative sample, capturing roughly one fifth of all ED visits in the United States (HCUP, 2015). The following three specific research aims guided the study approach: identifying patient characteristics associated with opioid misuse; conducting a trend analysis of change in ED visit rates over multiple years of study, and investigating factors associated with opioid misuse related outcomes, including hospitalization and death.
Conceptual Framework
Efforts to understand determinants of health care use and outcomes have drawn on the seminal theoretical work of R. Andersen and Newman’s (1973) Healthcare Utilization Model, which conceptualizes three broad sets of determining factors, including societal determinants, health service system determinants, and individual determinants. Individual determinants are further understood to include predisposing factors, need factors, and enabling factors. Conceptually, in terms of this study, sociodemographic factors, such as age and gender are understood to predispose ED use and are hypothesized to explain some of the variances in ED visit outcomes. Similarly, factors such as substance misuse disorders and levels of comorbidity are expected to drive the ED need as well as affect patient outcomes. Factors that impact access to care, such as income levels and insurance status, are further expected to enable health care service use and influence outcomes.
Findings from this study provide insight into the epidemiology of opioid misuse among older adult ED visits and related health outcomes.
Method
Data Source
Multiple years (2006, 2009, 2011, 2014) of nationally representative, cross-sectional data from the Nationwide Emergency Department Sample (NEDS) were used to retrospectively describe prevalence rates, risk factors, trends, and outcomes among opioid-related patient encounters by older adults. Data years 2006, 2009, and 2011 were available for study use from a previous study. To this data set, year 2014 was added to provide a more comprehensive picture of change in opioid misuse rates over time. Using a complex sampling design, NEDS is the largest all-inclusive payer source of de-identified U.S. ED visits available (HCUP, 2018a). Data are sampled annually and include discharges from roughly 953 participating hospitals with ED, sampled across 34 states and the District of Columbia. Sampling weights are available to adjust for design effects and permit national estimates of ED use and outcomes. Data elements include: ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) diagnoses and related diagnostic categorizations based on the Clinical Classification System, external cause of injury codes, injury indicators, chronic condition indicators, discharge disposition, patient characteristics, expected payment source, and region of location (additional information is available from https://www.hcup-us.ahrq.gov/).
Study Sample
For the purposes of this study, sample inclusion was restricted to ED visits by adults aged 65 years or older, resulting in 20,026,715, unweighted ED patient encounters. ICD-9-CM codes and E-codes were screened to identify ED visits related to opioid poisoning and dependence following the strategy developed by Weiss and colleagues (2017) to estimate all-age opioid misuse in the ED. ICD-9-CM codes included: 304.00–304.02; 304.70–304.72; 305.50–305.52; 965.00–965.02; 969.09; 970.1, and E-codes included: 850.0–850.2; 935.0–935.2; 940.1. Cases in which only an E-code was available without any additional diagnostic information on the record indicating opioid misuse were omitted from specification (n =757 unweighted cases). Using this strategy, 28,167 unweighted (n = 126,931 weighted) observations were identified as opioid-related ED visits by older adults.
Measures
Using the coding strategy described above, the study variable of interest, opioid misuse, was specified as a dichotomous measure indicating misuse versus no identified misuse. Study outcomes of interest included routine discharge from the ED (reference category), admission to the same hospital, and death. A fourth category, all other discharges, was included to account for all other dispositions in estimation procedures, including discharged against medical advice, discharged to other health care facilities, and unknown outcomes.
Data elements were recoded to specify sociodemographic characteristics, including a set of dummy variables indicating age categories (aged 65–74, aged 75–84, and aged 85 and older), and gender status (male vs female). The NEDS provides a set of indicators corresponding to each ICD-9-CM diagnostic field that flags diagnoses associated with chronic conditions using the AHRQ Chronic Condition Indicator software tool (HCUP, 2018b). From this set of indicators, a count of chronic conditions was specified to capture differences in need for services associated with multimorbidity (Prince et al., 2015). Alcohol-related disorders were identified using the HCUP Clinical Classification Software system, which classifies 260+ diagnostic groupings from available diagnostic information. Alcohol misuse disorders are a recognized and growing public health concern among older adults (Wu & Blazer, 2011), and have been identified as increasing health care service use (McLellan, Lewis, O’Brien, & Kleber, 2000). Given the long-term implications of injury on health care use and costs (Carter & Porell, 2011), injury-related patient encounters were identified using a dichotomous indicator released with the NEDS data files.
Income levels and insurance status have long been recognized as enabling access to health care service use and outcomes (R. M. Andersen, Davidson, & Baumeister, 2014). The NEDS includes information on the estimated median household income associated with the patient zip code of residence. Using this variable, a set of dummy variables was specified, including lowest quartile versus otherwise, middle quartiles versus otherwise, and highest quartile versus otherwise. In analytical procedures, middle quartiles served as the referent category. Insurance status was also specified as a set of dummy variables, including Medicare Primary Payer versus otherwise, Medicaid Primary Payer versus otherwise, and all other types of insurance serving as the reference category. Rural versus other locations was defined as a dichotomous measure to capture differences in access to health care associated with the location of residence (Chan, Hart, & Goodman, 2006).
The opioid epidemic has developed over multiple years, sweeping across geographic regions and populations over time (Quinones, 2015). Although a comprehensive investigation of these multifaceted, complex factors is beyond the scope of the current study, two sets of indicators were included to control for changes over time and region. A set of dummy variables was specified to indicate the year of patient data in bivariate and trend analyses. Also, a set of dummy variables indicating region (Northeast, Midwest, South, and West) of the country, was specified. Northeast served as the reference category in the analytical procedures.
Analytical Approach
Because only de-identified data were available, ED visits (also referred to as patient encounters) served as the unit of analysis. Descriptive and multivariate statistical techniques were used to examine opioid misuse among older adult patient encounters to the ED. Descriptive statistics are presented in Table 1. Data were pooled across all study years (2006, 2009, 2011, 2014) to identify significant differences in patient characteristics associated with opioid misuse as well as to compare outcomes across patient encounters by opioid misuse status. Differences in sample characteristics by visit type were calculated as the difference in percent between opioid-related ED visits and nonopioid-related ED visits. Table 2 presents significant differences in the change in population ED visit rates over time. The difference in population visit rates over time was evaluated using bivariate logistic regression models (Table 2).
Table 1.
Characteristics of ED Patient Visits by Older Adults With and Without Opioid Dependence
| Sample Characteristics | Nonopioid-related visits | Opioid-related visits | % Difference (nonopioid − opioid) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Percent | Weighted | Observed | Mean (SD) | Percent | Weighted | Observed | ||
| ED visit outcome | |||||||||
| Hospital admission | 38.9 | 34,912,481 | 7,833,318 | 68.8 | 87,327 | 19,351 | 29.9 | ||
| Visit ended in death | 2.7 | 2,490,064 | 549,380 | 1.6 | 2,078 | 461 | −1.1 | ||
| Patient visit characteristics | |||||||||
| Age | 77.4 (8.2) | 89,762,955 | 19,998,548 | 72.1 (6.7) | 126,931 | 28,167 | −5.3 | ||
| Age 65–74 | 40.7 | 36,611,071 | 8,171,350 | 71.0 | 90,070 | 19,926 | 30.3 | ||
| Age 75–84 | 36.5 | 32,795,853 | 7,302,115 | 22.2 | 28,171 | 6,308 | −14.3 | ||
| Age 85 and older | 22.7 | 20,356,031 | 4,525,083 | 6.8 | 8,690 | 1,933 | −15.9 | ||
| Sex | |||||||||
| Male | 41.1 | 37,189,583 | 8,270,124 | 43.0 | 55,672 | 12,257 | 1.9 | ||
| Female | 58.6 | 52,573,372 | 11,728,424 | 56.1 | 71,259 | 15,910 | −2.5 | ||
| Number of chronic conditions | 3.8 (3.3) | 89,762,955 | 19,998,548 | 6.6 (3.1) | 126,931 | 28,167 | 2.8 | ||
| Alcohol-related visit | 1.4 | 1,224,684 | 272,344 | 9.7 | 12,285 | 2,721 | 8.3 | ||
| Injury-related visit | 20.0 | 18,003,255 | 4,001,005 | 30.3 | 38,523 | 8,604 | 10.3 | ||
| Fall-related injury | 11.9 | 10,723,053 | 2,394,593 | 6.3 | 8,015 | 1,795 | −5.6 | ||
| Primary insurance status | |||||||||
| Medicare | 87.2 | 78,420,017 | 17,476,685 | 87.2 | 110,630 | 24,612 | 0.0 | ||
| Medicaid | 1.6 | 1,416,082 | 319,401 | 3.3 | 4,195 | 897 | 1.7 | ||
| Self-pay | 1.1 | 977,136 | 217,897 | 6.7 | 8,484 | 1,870 | 5.6 | ||
| Other | 10.0 | 8,949,720 | 1,984,565 | 2.9 | 3,622 | 788 | −7.1 | ||
| Income level | |||||||||
| Lowest quartile | 27.1 | 24,395,201 | 5,455,129 | 31.2 | 39,574 | 8,672 | 4.1 | ||
| Middle quartiles | 50.1 | 45,065,071 | 9,989,425 | 48.0 | 60,912 | 13,513 | −2.1 | ||
| Highest quartile | 20.6 | 18,475,445 | 4,145,772 | 17.8 | 22,648 | 5,149 | −2.8 | ||
| Unknown | 2.0 | 1,827,237 | 408,222 | 3.0 | 3,797 | 833 | 1.0 | ||
| Rural residence | |||||||||
| Rurally located | 21.0 | 18,876,914 | 3,992,601 | 16.8 | 21,294 | 4,375 | −4.2 | ||
| Not rurally located | 79.0 | 70,886,041 | 16,005,947 | 83.2 | 105,636 | 23,792 | 4.2 | ||
| Region | |||||||||
| Northeast | 19.3 | 17,345,553 | 3,751,643 | 17.0 | 21,554 | 4,675 | −2.3 | ||
| Midwest | 23.5 | 21,112,888 | 4,222,341 | 16.3 | 20,721 | 4,127 | −7.2 | ||
| South | 38.2 | 34,315,967 | 8,248,825 | 35.5 | 45,105 | 10,501 | −2.7 | ||
| West | 18.9 | 16,988,547 | 3,775,739 | 31.2 | 39,551 | 8,864 | 12.3 | ||
| Year | |||||||||
| 2006 | 22.6 | 20,337,883 | 4,396,992 | 11.1 | 14,047 | 2,994 | −11.5 | ||
| 2009 | 24.0 | 21,609,824 | 4,813,471 | 18.2 | 23,160 | 5,104 | −5.8 | ||
| 2011 | 25.6 | 22,971,902 | 5,171,171 | 27.0 | 34,311 | 7,640 | 1.4 | ||
| 2014 | 27.6 | 24,843,345 | 5,616,914 | 43.7 | 55,413 | 12,429 | 16.1 | ||
| All patient visits | 100.0 | 89,762,955 | 19,998,548 | 100.0 | 126,931 | 28,167 | n/a | ||
| Total sample observed | 20,026,715 | ||||||||
| Total sample weighted | 89,899,886 |
Notes. ED = emergency department. Descriptive statistics were calculated on the pooled sample of all four data years (2006, 2009, 2011, 2014). For each comparison, % difference was calculated as (opioid-related visits − nonopioid-related visits). Results from bivariate analyses were significant for all group comparisons (p < .001). n/a = not applicable.
Table 2.
Change Over Time in Patient Visit Rates Per 100,000 Population Among Older Adult ED Visits for Opioid Misuse (2006–2014)
| Sample Characteristics | Mean patient visit rate per 100,000 population 2006–2014 | Patient visit rate per 100,000 population 2006 | Patient visit rate per 100,000 population 2009 | Patient visit rate per 100,000 population 2011 | Patient visit rate per 100,000 population 2014 | % Change (2006–2014) | p Value for trend |
|---|---|---|---|---|---|---|---|
| Any opioid use | |||||||
| Total (n = 126,931) | 77.2 | 37.8 | 58.5 | 83.0 | 119.9 | 217.2 | <.001 |
| Males | 78.4 | 38.0 | 59.0 | 82.3 | 122.4 | 222.1 | <.001 |
| Females | 76.3 | 37.7 | 58.1 | 83.4 | 117.9 | 212.7 | <.001 |
| Aged 65–84 | 83.1 | 40.5 | 63.4 | 89.1 | 129.0 | 218.5 | <.001 |
| Aged 85 or older | 39.3 | 20.0 | 26.9 | 44.6 | 60.6 | 203.0 | <.001 |
| Alcohol-related visit | 7.5 | 3.6 | 6.1 | 8.1 | 11.2 | 211.1 | <.001 |
| Nonalcohol-related visit | 69.8 | 34.2 | 52.4 | 74.9 | 108.7 | 217.8 | <.001 |
| Injury-related visit | 23.4 | 11.7 | 17.8 | 27.0 | 34.6 | 195.7 | <.01 |
| Noninjury-related visit | 53.8 | 34.2 | 52.4 | 74.9 | 108.7 | 217.8 | <.01 |
| Visit resulted in hospitalization | 53.1 | 26.9 | 42.4 | 58.0 | 79.1 | 194.1 | <.001 |
| No hospitalization | 24.1 | 10.9 | 16.1 | 25.0 | 40.8 | 274.3 | <.001 |
| Patient visit ended in death | 1.1 | 0.6 | 0.8 | 1.1 | 1.5 | 150.0 | NS |
| No death occurred | 76.2 | 37.1 | 57.6 | 81.8 | 118.4 | 219.1 | <.001 |
Notes. Per capita population (100,000) rates of ED visits by older adults were estimated using US Intercensal Population Estimates from the US Census, available from https://www.census.gov/programs-surveys/popest/data/data-sets.html. Age and gender-specific population rates from these tables were used to calculate patient visit rates for age and gender categories. All other rates use population estimates for the entire 65+ population. NS = not significant.
Multiple logistic regression (Table 4, Model 1) was used to investigate risk factors associated with ED visits for opioid misuse. In this model, opioid misuse status is dichotomized (yes/no) and serves as the dependent variable. Multinomial logistic regression (Table 4, Model 2 and Model 3) was used to model the effect of opioid use on multiple categories of ED outcomes, including routine discharge from the ED, admission to an adjoining hospital, and the encounter ends in death. To better understand the impact of opioid misuse on each of these outcomes, the multinomial logistic regression model was estimated twice. In the initial specification (Model 2), opioid misuse served as the variable of study interest and the estimation procedures included all observations by adults aged 65 years and older. In the second approach (Model 3), the model was re-estimated after restricting the sample to only those observations in which opioid misuse was identified.
Table 4.
Patient Visit Outcomes Related to Opioid Misuse
| Sample Characteristics | Model 1: Logistic regression any opioid misuse (all 65+) | Model 2: Multinomial logistic regression visit outcomes (all 65+) | Model 3: Multinomial logistic regression visit outcomes (opioid-related visits only, 65+) | ||
|---|---|---|---|---|---|
| Opioid use vs no opioid misuse | Hospital admit vs routine discharge | Death occurred vs routine discharge | Hospital admit vs routine discharge | Death occurred vs routine discharge | |
| OR (95% CI) | RRR (95% CI) | RRR (95% CI) | RRR (95% CI) | RRR (95% CI) | |
| Patient visit characteristics | |||||
| Opioid misuse | 1.63 (1.55, 1.72)*** | 0.85 (0.72, 0.99)* | |||
| No opioid misuse | Referent | Referent | |||
| Age | |||||
| Age 65–74 | 6.75 (6.63, 7.27)*** | 0.64 (0.63, 0.64)*** | 0.37 (0.36, 0.38)*** | 0.83 (0.68, 1.01) | 0.28 (0.17, 0.47)*** |
| Age 75–84 | 2.16 (1.99, 2.34)*** | 0.75 (0.75, 0.76)*** | 0.56 (0.55, 0.57)*** | 0.89 (0.72, 1.11) | 0.51 (0.30, 0.88)* |
| Age 85 and older | Referent | Referent | Referent | Referent | Referent |
| Sex | |||||
| Female | 1.12 (1.07, 1.16)*** | 0.95 (0.95, 0.96)*** | 0.71 (0.70, 0.72)*** | 1.05 (0.95, 1.16) | 0.87 (0.63, 1.21) |
| Male | Referent | Referent | Referent | Referent | Referent |
| Number of chronic conditions | 1.27 (1.26, 1.28)*** | 1.74 (1.74, 1.74)*** | 1.52 (1.52, 1.52)*** | 1.54 (1.51, 1.56)*** | 1.49 (1.38, 1.53)*** |
| Alcohol-related visit | 2.88 (2.70, 3.07)*** | 1.80 (1.76, 1.83)*** | 1.33 (1.26, 1.39)*** | 1.25 (1.05, 1.49)* | 0.40 (0.68, 0.99)* |
| Injury-related visit | 2.89 (2.77, 3.02)*** | 0.83 (0.82, 0.83)*** | 0.59 (0.58, 0.60)*** | 2.51 (2.26, 2.80)*** | 2.69 (1.90, 3.80)*** |
| Primary insurance status | |||||
| Medicaid | 1.56 (1.41, 1.73)*** | 1.75 (1.72, 1.78)*** | 1.38 (1.32, 1.45)*** | 1.04 (.80, 1.33) | 1.56 (0.67, 3.67) |
| Other payment | 0.84 (0.79, 0.89)*** | 0.89 (0.88, 0.90)*** | 1.18 (1.15, 1.20)*** | 0.79 (0.67, 0.92)** | 1.01 (0.60, 1.72) |
| Medicare | Referent | Referent | Referent | Referent | Referent |
| Income level | |||||
| Lowest quartile | 1.26 (1.20, 1.31)*** | 1.01 (1.01, 1.02)*** | 0.99 (0.97, 1.00 | 0.92 (0.83, 1.01) | 0.77 (0.54, 1.11) |
| Highest quartile | 0.78 (0.74, 0.82)*** | 0.85 (0.84, 0.86)*** | 0.89 (0.88, 0.91)*** | 0.74 (0.66, 0.85)*** | 0.51 (0.31, 0.85)** |
| Other | Referent | Referent | Referent | Referent | Referent |
| Rural residence | |||||
| Rurally located | 0.99 (0.94, 1.04) | 0.78 (0.77, 0.781)*** | 1.04 (1.02, 1.06)*** | 0.85 (0.75, 0.97)* | 1.20 (0.80, 1.82) |
| Not rurally located | Referent | Referent | Referent | Referent | Referent |
| Region | |||||
| Midwest | 0.75 (0.70, 0.80)*** | 0.52 (0.51, 0.52)*** | 0.50 (0.49, 0.51)*** | 0.48 (0.41, 0.56)*** | 0.54 (0.29, 1.02) |
| South | 0.83 (0.78, 0.87)*** | 0.70 (0.70, 0.71)*** | 0.61 (0.60, 0.62)*** | 0.58 (0.51, 0.67)*** | 0.686 (0.393, 1.197) |
| West | 1.61 (1.52, 1.70)*** | 0.47 (0.47, 0.47)*** | 0.55 (0.54, 0.56)*** | 0.48 (0.42, 0.55)*** | 0.77 (0.44, 1.32) |
| Northeast | Referent | Referent | Referent | Referent | Referent |
Notes. Multinominal logistic models were adjusted for alternative outcomes to ensure all outcomes were accounted for in discrete categories. Results for this third category included transfers to short-term hospitals, nursing homes, and other healthcare facilities, and are available upon request. Estimation procedures relied on data from the year 2014 only (n = 5,629,343 unweighted cases in Models 1 and 2. Model 3 uses this same sample but also employs STATA’s SVY SUBPOP routine to adjust estimates of the standard errors. Although all cases are available for this purpose, the sample size of interest is n = 12,429). OR = odds ratios; RRR = relative risk ratio; CI = confidence interval.
*p < .05, **p < .01, ***p < .001.
In specifying models, both the multiple logistic regression model and the multinomial logistic regression models were calculated on data from the year 2014 to guard against reporting results from overpowered models (Kaplan, Chambers, & Glasgow, 2014). Although not reported here, estimates were repeated for each wave of data and compared, as well as on the full sample. In terms of effect size, direction, and significance, findings were consistent across models; thus, findings from the most recent year of data are presented. Construction of the analytical data files and statistical analyses were performed with STATA 15.1 (STATA, 2017). STATA routines for complex survey data were used for all analyses. STATA’s SVY commands with SUBPOP routines allow for the inclusion of design weights released each year with the NEDS data files and are necessary to adjust for potential sampling bias arising from the complex sampling design and to correctly calculate the standard errors of the estimates.
Results
Sample Characteristics
Across study years, 126,931 patient encounters to ED with at least one ICD-9-CM code indicating opioid misuse were made by adults aged 65 years or older (Table 1). However, the proportion of ED visits increased steeply over time. For example, data from 2006 accounted for 11% (n = 14,407) of observed opioid misuse ED visits, while data from 2014 accounted for 44% (n = 55,413) of observed opioid misuse ED visits. Findings suggest that by 2014, nearly 6.4 opioid-related ED visits by older adults were occurring every hour across the U.S. ED visits resulting in hospital admission were nearly 50% higher among patient encounters with opioid misuse identified in comparison with older adults with no opioid misuse identified. For example, among ED visits with opioid misuse, 68.8% resulted in hospitalization, whereas 38.9% of nonopioid ED visits ended in hospitalization, for an actual difference of 30% between the two groups. Despite the higher hospitalization rate, ED visits ending in death were lower among observations coded for opioid misuse (1.7%) than for other patient encounters (2.7%), perhaps reflecting in part, the younger age of those identified with opioid misuse. In comparison with nonopioid-related patient encounters, older adults diagnosed with opioid misuse tended to be younger (77.4 vs 72.1, p < .001). Furthermore, although nearly 23% of older adult ED visits were made by those aged 85 years or older among the general sample, only 6.8% of opioid-related patient encounters were identified among this age group. Despite being younger, older adults with opioid misuse tended to have twice as many chronic conditions (6.6 vs 3.8, p < .001), and were more frequently observed to have a history of alcohol misuse (9.7% vs 1.4%, p < .001). Moreover, injuries were more prevalent among older adults coded for opioid misuse in comparison with the older population in general (30.3% vs 20.0%, p < .001). Despite having higher injury rates, the type of injury was less often identified as fall-related (6.3% vs 11.9%, p < .000). Across the two groups, similar rates of Medicare participation were observed. However, among patient encounters identified as opioid-related, Medicaid (3.3 vs 1.6, p < .000) and self-pay (6.7 vs 1.1, p < .001) were more often expected to be the primary source of payment. Median zip code income levels appeared to be slightly lower among older adult visits coded for opioid misuse, but the overall difference across quartiles was modest, varying by a combined total of roughly 10%.
Descriptive statistics suggest variation exists in opioid-related ED visit rates across geographic regions. For example, more than 31% of opioid-related visits originated in the western region of the United States, while less than 19% of patient encounters from the general population did so (p < .001). Although the number of patient encounters observed by study year appeared relatively stable across study years, visits related to opioid use increased steeply over the same time period. For example, among all patient encounters with identified opioid misuse, less than 1/3 of these patient encounters occurred in years 2006 or 2009, combined, whereas more than 2/3 of all visits of this type occurred in years 2011 and 2014 (p < .001). This pattern is consistent with broader trends in opioid misuse for adults of all ages and may suggest that older adults have also been affected by increasing supplies of opioid drugs (Manchikanti et al., 2017).
ED Visit Rates Over Time
To further explore changes in opioid-related ED patient encounters by older adults, trend analyses by patient characteristics were conducted (Table 2). Findings indicate that the population visit rates by older adults identified as having at least one diagnostic code indicating opioid misuse increased 217% from 2006 to 2014 (p < .001). Increases in ED visit rates were observed across each wave of data, with opioid-related ED visit rates increasing from 37.8 visits per 100,000 adults aged 65 years and older in 2006 to 58.5 visits per 100,000 adults aged 65+ in 2009. A similar trend was observed between study years 2009 and 2011 (note the smaller time frame), with visit rates increasing to 83.0 visits per 100,000 older adults in 2011, and to 119.9 visits per 100,000 65+ in 2014. Although older female patients accounted for a larger proportion of all opioid-related patient encounters, over time, the proportion of patient encounters made by older men increased more sharply (p < .001). While most opioid-related patient encounters were made by adults between the ages of 65 and 84, change over time for those under and over aged 85 years increased similarly, with per capita visit rates increasing 203% from 2006 to 2014 among adults aged 85 and older (p < .001). Although opioid-related ED visits increased sharply during the study period among older adults, research available elsewhere relying on the same data source demonstrate that ED visits among 65+ remained roughly the same over time, with fluctuations reflecting only slight increases and decreases from year to year (Sun, Karaca, & Wong, 2018).
Proportionately, the rate of patient encounters identified with and without alcohol misuse appeared relatively unchanged across study years, with similar codependence observed among opioid-related patient encounters over time, suggesting that the increase in overall ED visit rates reflect changes in opioid misuse rather than alcohol misuse. Trend analyses indicated that although injury rates increased significantly among opioid-related patient encounters, patient encounters for noninjury related opioid rates increased more rapidly (p < .01). Plausible explanations for this finding could include increased awareness over time of opioid poisoning and dependence among older adults in the ED, or greater awareness in the community, leading to earlier intervention. Because this finding is difficult to interpret, caution is urged in generalizing study findings.
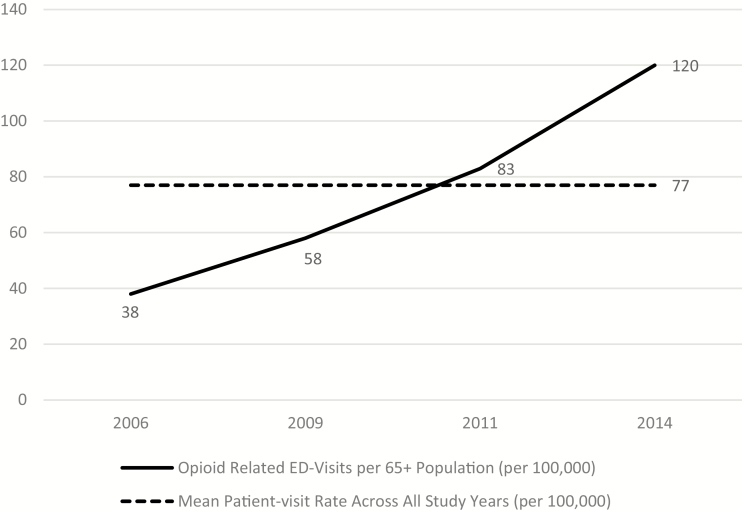
Considered together, trend analyses suggest that per capita visit rates for opioid misuse have increased sharply over the study period, with similar increases in visit rates among male and female older adults. Although adults aged 85 years and older hold lower visit rates in comparison with adults aged 65–84, overall trends suggest that the rate of increase over time is similar between the two age groups. Across all study years, the observed per capita patient visit rate for opioid misuse averaged 77 opioid-related visits per 100,000. However, as Figure 1 illustrates, a steep increase in national estimates of opioid-related visits occurred over time. For example, in 2006, estimates suggest that roughly 38 patient encounters per 100,000 adults aged 65+ occurred. By 2014, this increased to 120 patient encounters per 100,000 adults aged 65 and older.
Figure 1.
Growth in opioid-related ED visit among older adults (2006–2014).
To better understand the nature of opioid versus nonopioid-related ED visits, leading diagnoses flagged on the record as a chronic condition, excluding opioid misuse, were tabulated and ranked (Table 3), providing insight into differences in health care needs among the two groups. Several diagnoses were identified as leading chronic conditions across both groups, including essential hypertension, congestive heart failure, and chronic obstructive pulmonary diseases, although not in the same order of frequency. Important differences are observed, too. For example, older adults with identified opioid misuse were observed to more often have diagnostic codes indicating mood disorders, alcohol-related disorders, mental health/substance use history, respiratory failure, anxiety disorders, and nutritional deficiencies, ranking among the 5th, 9th, 11th, 13th, 14th, and 15th most frequently recorded diagnoses, respectively. Conversely, none of these diagnoses were observed among the general population’s leading 15 chronic conditions. Importantly, the higher prevalence of psychosocial diagnoses is consistent with the broader literature on substance misuse (Lai, Cleary, Sitharthan, & Hunt, 2015).
Table 3.
Most Frequently Listed Diagnoses Among Older Adults With and Without Opioid Misuse Indicator
| Opioid-related visits | Nonopioid-related visits | CCS label | ||
|---|---|---|---|---|
| Rank | Estimated percent | Rank | Estimated percent | |
| 1 | 16.8 | 1 | 30.8 | Essential hypertension (CCS 98) |
| 2 | 16.1 | 13 | 3.0 | Other nervous system disorders (CCS 95) |
| 3 | 16.0 | 7 | 9.7 | Chronic obstructive pulmonary disease and bronchiectasis (CCS 127) |
| 4 | 11.2 | 2 | 13.1 | Congestive heart failure; nonhypertensive (CCS 108) |
| 5 | 10.8 | — | <0.1 | Mood disorders (CCS 657) |
| 6 | 7.8 | 3 | 12.9 | Cardiac dysrhythmias (CCS 106) |
| 7 | 7.1 | 4 | 12.6 | Coronary atherosclerosis and other heart disease (CCS 101) |
| 8 | 6.6 | 5 | 12.0 | Diabetes mellitus without complication (CCS 49) |
| 9 | 4.6 | — | <0.1 | Alcohol-related disorders (CCS 660) |
| 10 | 4.5 | 9 | 5.5 | Hypertension with complications and secondary hypertension (CCS 99) |
| 11 | 4.2 | — | <0.1 | Screening and history of mental health and substance abuse codes (CCS 663) |
| 12 | 4.1 | 6 | 10.1 | Disorders of lipid metabolism (CCS 53) |
| 13 | 4.0 | — | 0.5 | Respiratory failure; insufficiency; arrest (adult) (CCS 131) |
| 14 | 2.6 | — | 1.6 | Anxiety disorders (CCS 651) |
| 15 | 2.2 | — | 1.6 | Nutritional deficiencies (CCS 52) |
| — | <0.1 | 8 | 6.8 | Delirium, dementia, and amnestic and other cognitive disorders (CCS 653) |
| — | 1.2 | 10 | 5.3 | Chronic kidney disease (CCS 158) |
| — | 1.2 | 11 | 3.8 | Esophageal disorders (CCS 138) |
| — | <0.1 | 12 | 3.7 | Thyroid disorders (CCS 48) |
| — | <0.1 | 14 | 2.0 | Conduction disorders (CCS 105) |
| — | 0.8 | 15 | 1.7 | Acute cerebrovascular disease (CCS 109) |
Note. CCS = Clinical Classification Software (available from https://www.hcup-us.ahrq.gov/toolssoftware/ccs/AppendixASingleDX.txt). Estimates were aggregated from across the first five chronic conditions listed on the record. The opioid misuse subpopulation does not include diagnostic codes indicating chronic opioid misuse, as this overlapped with subpopulation definition. Frequencies were aggregated across all study years.
Factors Associated With Opioid Misuse and Visit Outcomes
Results from multivariate analyses are presented in Table 4. Model 1 (first column) presents logistic regression odds ratios of patient characteristics associated with opioid misuse-related patient encounters. Findings suggest that the odds of opioid misuse among adults aged 65–74 years old are 6.75 times (p < .001) larger than otherwise similar adults aged 85 years and older. Likewise, the odds of opioid misuse among adults aged 75–84 years old were 2.16 times (p < .001) larger than their otherwise similar, adults aged 85 years and older. Patient encounters by older females were found to have roughly 12% greater odds of having opioid misuse identified during their ED visit, relative to otherwise similar males (OR = 1.12, p < .001). Findings indicated that risk of opioid misuse increased sharply as the number of chronic conditions increased. For example, with each additional chronic condition identified, the odds of opioid misuse increased by 27% (OR = 1.27, p < .001). Likewise, alcohol disorders and injury increased the risk of patient encounters being identified with opioid misuse as well. Patient encounters associated with alcohol dependence increased odds of opioid misuse being identified by roughly 188% (OR = 2.88, p < .001), while injury increased odds by 189% (OR = 2.89, p < .001).
Model 2 (Columns 2 and 3) present estimates of ED visit outcomes among the general sample using multinomial logistic regression. In this model, opioid misuse is specified as the variable of interest. Findings suggest that opioid misuse by older adults visiting the ED increases the relative risk of being admitted to the hospital versus routine discharge. For example, in comparison with older adult visits with no opioid misuse identified, risk among those with misuse was 63% greater, holding other factors constant (RRR = 1.63, p < .001). Conversely, opioid misuse was associated with lower odds of patient encounters ending in death versus routine discharge (RRR = 0.85, p < .05). This may reflect the association between age and study outcomes. Younger age among patient encounters appears protective, both lowering the relative risk of hospitalization (RRR = 0.64, p < .001) and death (RRR = 0.37, p < .001) versus routine discharge, respectively. Results in Model 3 (columns 4 and 5), also presenting estimates using multinomial logistic regression techniques, further support this interpretation. Here, only those patient encounters with identified opioid misuse are included. Findings from this model suggest that among older adult opioid-related patient encounters, being aged 65–74 decreases the relative risk of death versus routine discharge (RRR = 0.28, p < .001), holding other factors constant. Nonetheless, other plausible explanations exist. For example, immediate discharge may be more difficult given substance misuse, or overall severity associated with these hospitalizations may be lower than that of the general population.
Findings associated with injury-related visits do not support this conclusion. For example, for the general population of older adults, injury is associated with both lower risk of hospital admission and death (RRR = 0.83 and RRR = 0.59, p < 0.001, respectively), after adjusting for other factors. However, among patient encounters with opioid misuse, injury is associated with a much higher risk of hospitalization (RRR = 2.51, 0.001) and death (RRR = 2.69, p < 0.001), suggesting higher acuity levels among this select population. Moreover, after adjusting for opioid misuse status, risk of hospitalization and death are significantly elevated among ED patient encounters with higher counts of chronic conditions. For instance, estimates indicate that with each additional chronic condition, the risk of hospitalization relative to routine discharges increases 75% (RRR = 1.75, p < .001). A similar effect is observed among patient encounters identified with opioid misuse. Risk of hospitalization in this group increased 54% (RRR = 1.54, p < .001) with each additional chronic condition, holding other factors constant. A nearly identical pattern of results is observed when comparing risk of death across the multinomial logistic model estimates.
Model estimates indicate that enabling determinants, such as income levels and insurance rates, influence risk and outcomes in important ways. In comparison to those in the middle two income quartiles, patient encounters (Model 1) from high-income zip codes were less likely to be identified as having an opioid misuse disorder (OR = 0.78, p < .001), whereas those in the lowest income quartile held higher relative risk (OR = 1.26, p < .001), after adjusting for other factors. Moreover, for both older adults in general (Model 2) and those with opioid misuse specifically (Model 3), higher incomes were associated with lower risk of hospitalization (RRR = 0.85 and RRR = 0.89, p < .001) and death (RRR = 0.74, p < .001; RRR = 0.51, p < .01), respectively. The pattern of results for primary insurance payer was less clear. Overall, Medicaid as a primary payer is associated with greater odds of opioid misuse being identified (OR = 1.56, p < .001). But, findings also indicate that Medicaid is associated with higher hospitalization risk in general (RRR = 1.75, p < .001), but it was not significantly related to hospitalization in opioid-only–related patient encounters. Conversely, having a primary payer other than Medicare was associated with both lower risk of opioid misuse, as well as lower hospitalization risk (RRR = 0.89, p < .001) and among those with opioid misuse identified (RRR = 0.79, p < .01). Interestingly, having a primary payer other than Medicare was associated with a greater risk of death in the general study sample (RRR = 1.18, p < .001). However, similar findings were not observed among opioid misuse-related patient encounters.
Contrary to study expectations, rural location was not associated with greater odds of patient encounters being associated with opioid misuse. Further, for both samples of older adults, rural status was associated with lower hospitalization risk (RRR = 0.78, p < .001; RRR = 0.85, p < .05). Conversely, although rural location was associated with an increased risk of death among patient encounters in general (RRR = 1.04, p < .001), similar findings were not identified among patient encounters coded for opioid misuse. Given broader findings linking opioid misuse disorders to rural locations, caution is urged in interpreting these study findings.
Discussion and Policy Implications
The opioid crisis is one of the leading public health challenges of our time, affecting young and old alike. Despite a broader public health focus on younger populations, findings from this study underscore the challenge facing older adults. The precipitous increase in ED visit rates among older adults reported here, which more than tripled between 2006 and 2014, raises concern about the lack of focused attention for this age group. Moreover, findings from this study highlight the complexity and challenge of addressing the opioid crisis among older adults, including recognizing the increasing proportion struggling with multiple facets of substance misuse disorder, including co-occurring alcohol dependency, anxiety disorders, and mood disorders. From a policy perspective, these findings highlight the importance of the ED in identifying opioid misuse among older adults, especially in light of study estimates suggesting that nationally, 6.4 older adults with opioid misuse disorder visit the ED every hour, with more than half of these visits resulting in hospitalization. However, findings also point to the challenge of mounting an appropriate, well-informed, and targeted response to the problem. For example, although opioid misuse is often construed as unintentional and less common among older adults, results from this most likely capture two important aspects of the problem among older adults: unintended, relatively new patterns of opioid misuse among older adults as well as those with a longer history of substance misuse disorders (Cotton, Bryson, & Bruce, 2018). Further, given that those identified in the ED with opioid misuse tend to be the young-old, but present with twice as many chronic conditions on average, as well as with higher rates of coexisting mental health needs, effort to target interventions specifically toward this age group is needed. Importantly, because managing symptoms of withdrawal and other complications of opioid misuse are more challenging in the face of certain diagnoses, including hypertension, chronic obstructive pulmonary disorders, and heart failure (Carew & Comiskey, 2018), all of which were leading complications in this study, additional age-specific data are needed to guide interventions and treatment.
Individual determinants are important factors as well, requiring careful consideration in developing treatment and services. For example, despite the focus on men in broader discussions of opioid misuse, findings presented here underscore that women, too, are affected, with findings indicating that women held similar increases in opioid misuse ED visits over time, and that overall, women accounted for a higher proportion of ED visits coded for opioid misuse. Likewise, although a much smaller proportion of visits occur among the oldest-old, the population increase in ED visits by this age group was found to track closely to their younger counterparts, with nationally representative estimates suggesting opioid misuse in the ED increased 203% over the study period for this age group. Most likely, this statistic captures both those recently prescribed opioid drugs and those that have struggled with substance disorders for a lengthy period of time. Given statistics reported elsewhere with regard to increasing opioid misuse among younger populations, combined with information here suggesting steep increases in opioid misuse among adults aged 65–84 and by adults aged 85 years and older, it is likely that these trends will persist for several years into the future.
Findings also underscore the vital need for additional research to better understand how need and access to services vary as well; and how in turn, this affects older adults’ access to prevention and treatment. For example, given the impact of opioid misuse on hospitalization demonstrated in this study, vis-à-vis shifting health care services to the community, understanding the subsequent impact on aging services, outpatient care, and other community-based services, in addition to the health care system, is needed. For instance, study findings pointing to higher hospitalization risk among those with opioid misuse sustaining an injury, presumably affects not only hospital use, but also other services, such as first responder services, nursing home, and rehabilitation, as well. Moreover, current limits in prescription drug coverage for long-term opioid-dependence treatment (Cotton et al., 2018) raises concern that capacity to meet the needs of older adults with substance misuse disorders is underdeveloped, and that this lack of capacity may be exacerbated as demographics age, as suggested by the steep increase in misuse disorders among older adults presented here.
Limitations
Although findings provide much needed estimates of opioid misuse among older adults, several study limitations exist. Because this study relies on ED data, estimates presented here likely understate the scope of the problem. First, it is likely that many older adults with opioid misuse disorders seek treatment elsewhere, including physician’s offices, outpatient treatment centers, etc., while some elders struggling with opioid misuse have yet to seek treatment. Secondly, the data used for this study excludes persons dying before transfer for emergency services. Given the unexpected finding in this study of the effect of rural status on misuse and outcomes vis-à-vis national discussions, these forms of censoring may be particularly important in terms of study generalizability. Elsewhere, researchers have noted the analytical challenge in relying on ICD-9-CM codes assigned for purposes other than surveillance—the purpose of this study. Additionally, variation in the use of ICD-9-CM codes may lead to differences in coding strategies across ED and health care regions, affecting conclusions about the size and scope of the problem. This may be particularly important in terms of the use of E-codes on administrative records, which have been shown to vary widely across states and hospitals. Variation in recording diagnostic information associated with opioid misuse may vary regionally and over time, as well. Elsewhere, research has indicated reluctance to record sensitive information, especially among older adults. Conversely, however, growing awareness of opioid misuse, in general, may encourage greater effort by physicians and hospitals to record diagnostic information. In addition, because of the limits of clinical information available in administrative data, it is possible that some cases of opioid misuse identified here may be associated with patient encounters with co-occurring chronic pain, such as with some cancer diagnoses. However, given the lack of clinical data in the study data, a detailed analysis of chronic pain is not possible. Lastly, despite having multiple years of data, lack of a unique identifier across records both within and across years limited this study to a cross-sectional design, which may confound correlational and causal relationships.
Conclusion
National estimates of ED visits indicate that older adults are increasingly struggling with opioid misuse disorders, with increases in population ED visit rates mirroring or exceeding reported rates for younger populations (Weiss et al., 2017). Older adults identified in the ED with opioid misuse disorders typically present with twice as many chronic conditions, are more apt to struggle with alcohol and other mental health issues and sustain injuries severe enough to increase hospitalization and risk of death. Moreover, a subset of those affected may have limited resources to respond to their treatment needs, given broader policies in place that limit access to long-term treatment. Additional effort to understand the impact of opioid misuse on older adults and the agencies and services that they rely on is needed to mount a public health and policy response.
Funding
Funding for this work was provided by TU College of Health Professions.
Conflict of Interest
None reported.
References
- Andersen R. M., Davidson P. L., & Baumeister S. E (2014). Improving access to care. In Kominski G. F. (Ed.), Changing the US health care system: Key issues in health services policy and management (4th ed., pp. 33–69). San Francisco, CA: John Wiley and Sons; Retrieved from https://ebookcentral.proquest.com/lib/towson/reader.action?docID=1543235&ppg=367 [Google Scholar]
- Andersen R., & Newman J. F (1973). Societal and individual determinants of medical care utilization in the United States. The Milbank Memorial Fund Quarterly, 51(1), 95–124. doi: 10.2307/3349613 [DOI] [PubMed] [Google Scholar]
- Blachman N. L., Leipzig R. M., Mazumdar M., & Poeran J (2017). High-risk medications in hospitalized elderly adults: Are we making it easy to do the wrong thing? Journal of the American Geriatrics Society, 65(3), 603–607. doi: 10.1111/jgs.14703 [DOI] [PubMed] [Google Scholar]
- Burgos-Chapman I., Trevisan L. A., & Sevarino K (2016). Abuse of opioids and prescription medications. In Sullivan S. A. & Levin F. R. (Eds.), Addiction and the older patient (pp. 105–138). New York, NY: Oxford University Press. doi: 10.1093/med/9780199392063.001.0001 [DOI] [Google Scholar]
- Campbell C. I., Weisner C., Leresche L., Ray G. T., Saunders K., Sullivan M. D.,…Von Korff M (2010). Age and gender trends in long-term opioid analgesic use for noncancer pain. American Journal of Public Health, 100, 2541–2547. doi: 10.2105/AJPH.2009.180646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carew A. M., & Comiskey C (2018). Treatment for opioid use and outcomes in older adults: A systematic literature review. Drug & Alcohol Dependence, 182(1), 48–57. doi: 10.1016/j.drugalcdep.2017.10.007 [DOI] [PubMed] [Google Scholar]
- Carter M. W., & Porell F. W (2011). The effect of sentinel injury on Medicare expenditures over time. Journal of the American Geriatrics Society, 59(3), 406–416. doi: 10.1111/j.1532-5415.2010.03283.x [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) (2016). CDC guideline for prescribing opioids for chronic pain: United States, 2016 (pp. 1–49). MMWR. Retrieved from https://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm
- Chan L., Hart L. G., & Goodman D. C (2006). Geographic access to health care for rural Medicare beneficiaries. The Journal of Rural Health: Official Journal of the American Rural Health Association and the National Rural Health Care Association, 22, 140–146. doi: 10.1111/j.1748-0361.2006.00022.x [DOI] [PubMed] [Google Scholar]
- Chau D. L., Walker V., Pai L., & Cho L. M (2008). Opiates and elderly: Use and side effects. Clinical Interventions in Aging, 3, 273–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton B. P., Bryson W. C., & Bruce M. L (2018). Methadone maintenance treatment for older adults: Cost and logistical considerations. Psychiatric Services, 69(3), 338–340. doi: 10.1176/appi.ps.201700137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowell D., Arias E., Kochanek K., Anderson R., Guy G. P., Losby J. L., & Baldwin G (2017). Contribution of opioid-involved poisoning to the change in life expectancy in the United States, 2000–2015. JAMA, 318(11), 1065–1067. doi: 10.1001/jama.2017.9308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Economic Aspects of the Opioid Crisis (2017). Testimony before the Joint Economic Committee of the United States Congress, Senate, 115th Congress, June 8, 2017 (Testimony of Angus Deaton). Retrieved from https://www.jec.senate.gov/public/_cache/files/677125fc-a63b-43e3-b29f-37aecd8f2dd0/economic-aspects-of-the-opioid-crisis.pdf
- Erwin P. C. (2017). Despair in the American heartland? A focus on rural health. American Journal of Public Health, 107(10), 1533–1534. doi: 10.2105/ajph.2017.304029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florence C. S., Zhou C., Luo F., & Xu L (2016). The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Medical Care, 54, 901–906. doi: 10.1097/MLR.0000000000000625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenk S. M., Porter K. S., & Paulozzi L (2016). Prescription opioid analgesic use among adults: United States, 1999–2012 (No. 2015) US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; Retrieved from https://www.cdc.gov/nchs/data/databriefs/db189.pdf [Google Scholar]
- Han B., Compton W. M., Jones C. M., & Cai R (2015). Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003–2013. JAMA, 314(6), 1468–1478. doi: 10.1001/jama.2015.11859 [DOI] [PubMed] [Google Scholar]
- Healthcare Cost and Utilization Project (HCUP) (2015). Introduction to the HCUP Nationwide Emergency Department Samples (NEDS) 2015 Agency for Healthcare Research and Quality (AHRQ) Retrieved from https://www.hcupus.ahrq.gov/db/nation/neds/NEDS2015Introduction.pdf [PubMed] [Google Scholar]
- Healthcare Cost and Utilization Project (HCUP) (2018a). NEDS overview Agency for Healthcare Research and Quality (AHRQ) Retrieved from https://www.hcup-us.ahrq.gov/nedsoverview.jsp [PubMed] [Google Scholar]
- Healthcare Cost and Utilization Project (HCUP) (2018b). NEDS description of data elements Agency for Healthcare Research and Quality (AHRQ) Retrieved from https://www.hcup-us.ahrq.gov/db/vars/chronn/nedsnote.jsp [PubMed] [Google Scholar]
- Kaplan R. M., Chambers D. A., & Glasgow R. E (2014). Big data and large sample size: A cautionary note on the potential for bias. Clinical and Translational Science, 7, 342–346. doi: 10.1111/cts.12178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolodny A., Courtwright D. T., Hwang C. S., Kreiner P., Eadie J. L., Clark T. W., & Alexander G. C (2015). The prescription opioid and heroin crisis: A public health approach to an epidemic of addiction. Annual Review of Public Health, 36, 559–574. doi:10.1146/annurev- publhealth-031914-122957 [DOI] [PubMed] [Google Scholar]
- Lai H. M., Cleary M., Sitharthan T., & Hunt G. E (2015). Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug and Alcohol Dependence, 154, 1–13. doi: 10.1016/j.drugalcdep.2015.05.031 [DOI] [PubMed] [Google Scholar]
- Lasser K. E. (2017). Prescription opioid use among U.S. Adults: Our brave new world. Annals of Internal Medicine, 167, 351–352. doi: 10.7326/M17-1559 [DOI] [PubMed] [Google Scholar]
- Le Roux C., Tang Y., & Drexler K (2016). Alcohol and opioid use disorder in older adults: Neglected and treatable illnesses. Current Psychiatry Reports, 18, 87. doi: 10.1007/s11920-016-0718-x [DOI] [PubMed] [Google Scholar]
- Manchikanti L. (2006). Prescription drug abuse: What is being done to address this new drug epidemic? Testimony before the Subcommittee on Criminal Justice, Drug Policy and Human Resources. Pain Physician, 9(4), 287–321. doi: 10.1016/j.ygyno.2005.09.025 [DOI] [PubMed] [Google Scholar]
- Manchikanti L., Kaye A. M., Knezevic N. N., McAnally H., Slavin K., Trescot A. M., & Hirsch J (2017). Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician, 20(2S), S3–S92. Retrieved from http://www.painphysicianjournal.com/current/pdf?article=NDIwMg%3D%3D&journal=103 [PubMed] [Google Scholar]
- McLellan A. T., Lewis D. C., O’Brien C. P., & Kleber H. D (2000). Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. JAMA, 284, 1689–1695. doi: 10.1001/jama.284.13.1689 [DOI] [PubMed] [Google Scholar]
- Nagappa M., Weingarten T. N., Montandon G., Sprung J., & Chung F (2017). Opioids, respiratory depression, and sleep-disordered breathing. Best Practice & Research. Clinical Anaesthesiology, 31, 469–485. doi: 10.1016/j.bpa.2017.05.004 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine (NAS) (2017). Pain management and the opioid epidemic: Balancing societal and individual benefits and risks of prescription opioid use Retrieved from http://nationalacademies.org/hmd/reports/2017/pain-management-and-the-opioid-epidemic.aspx [DOI] [PubMed]
- Okie S. (2010). A flood of opioids, a rising tide of deaths. The New England Journal of Medicine, 363, 1981–1985. doi: 10.1056/NEJMp1011512 [DOI] [PubMed] [Google Scholar]
- Prince M. J., Wu F., Guo Y., Gutierrez Robledo L. M., O’Donnell M., Sullivan R., & Yusuf S (2015). The burden of disease in older people and implications for health policy and practice. Lancet (London, England), 385, 549–562. doi: 10.1016/S0140-6736(14)61347-7 [DOI] [PubMed] [Google Scholar]
- Quinones S. (2015). Dreamland: The true tale of America’s opiate epidemic. New York: Bloomsbury Press. doi: 10.1017/tam.2016.15 [DOI] [Google Scholar]
- Solomon D. H., Rassen J. A., Glynn R. J., Garneau K., Levin R., Lee J., & Schneeweiss S (2010). The comparative safety of opioids for nonmalignant pain in older adults. Archives of Internal Medicine, 170, 1979–1986. doi: 10.1001/archinternmed.2010.450 [DOI] [PubMed] [Google Scholar]
- STATA (2017). Stata statistical software: Release 15. College Station, TX: StataCorp LLC. [Google Scholar]
- Sun R., Karaca Z., & Wong H. S (2018). Trends in hospital emergency department visits by age and payer, 2006–2015. HCUP statistical brief #238 Rockville, MD: Agency for Healthcare Research and Quality; Retrieved from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb238-Emergency-Department-Age-Payer-2006–2015.jsp [Google Scholar]
- Swart L. M., van der Zanden V., Spies P. E., de Rooij S. E., & van Munster B. C (2017). The comparative risk of delirium with different opioids: A systematic review. Drugs & Aging, 34, 437–443. doi: 10.1007/s40266-017-0455-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Office of Inspector General (IOG) (2017). Opioids in Medicare part D: Concerns about extreme use and questionable prescribing (HHS Data Brief OEI-02-17-00250) Washington, DC: Retrieved from https://oig.hhs.gov/OEI/REPORTS/OEI-02-17-00250.pdf [Google Scholar]
- U.S. Department of Health and Human Services, The Substance Abuse and Mental Health Services Administration (SAMHSA) (2017). Opioid misuse increases among older adults Retrieved from https://www.samhsa.gov/data/sites/default/files/report_3186/Spotlight-3186.pdf
- Weiss A. J., Bailey M. K., O’Malley L., Barrett M. L., Elixhauser A., & Steiner C. A (2017). Patient characteristics of opioid-related inpatient stays and emergency department visits nationally and by state, 2014. HCUP Statistical Brief #224 Rockville, MD: Agency for Healthcare Research and Quality; Retrieved from www.hcup-us.ahrq.gov/reports/statbriefs/sb224-Patient-CharacteristicsOpioid-Hospital-Stays-ED-Visits-by-State.pdf [Google Scholar]
- Wu L. T., & Blazer D. G (2011). Illicit and nonmedical drug use among older adults: A review. Journal of Aging and Health, 23, 481–504. doi: 10.1177/0898264310386224 [DOI] [PMC free article] [PubMed] [Google Scholar]