Abstract
Previous research has demonstrated that externalizing symptoms, cannabis use problems, and poor decision-making abilities are each independently related to risky sexual behavior (RSB). However, few studies have examined the joint effect of these factors on RSB among a sample of adolescents. The current study addresses this gap in the literature by examining how externalizing disorder symptoms, cannabis use, and decision-making abilities interact to predict RSB among a sample of adolescents (n = 204; mean age = 15.5) at-risk for escalation in cannabis use. Poisson regression was used for all analyses and simple slope difference tests were used for all post-hoc analyses. A greater number of externalizing symptoms, more problems from cannabis use, and more risk disadvantageous choices on the Cups Task (CT) total trials and more risk disadvantageous choices on the CT gain trials predicted greater RSB endorsement. Findings also highlight significant interactions between cannabis use problems and CT total and gain trial performance, as well as between cannabis use problems and externalizing symptoms in predicting RSB. Current treatment and prevention approaches to reduce RSB among adolescents may benefit from incorporating techniques that improve decision-making skills.
Keywords: cannabis, decision-making, externalizing disorders, risky sexual behavior
Introduction
Increases in risk-taking behaviors are often observed during adolescence, including risky sexual behaviors (RSB), defined here as sexual behaviors that can directly lead to STIs or unplanned pregnancies. Teens are at a greater risk of engaging in RSB compared to other ages, with young persons accounting for nearly half of the new sexually transmitted infections (STIs) diagnosed throughout the US (Satterwhite et al., 2013). Few studies have examined the association between neurocognitive performance and RSB and even fewer studies have examined this association among adolescents. However, leading developmental theories about adolescent risk-taking behavior focus on neurocognitive development as one of the main reasons for the increases observed in risk-taking behavior among this age group. Two of these theories are the “dual process” and “triadic” models, which share a common theme. Specifically, subcortical areas involved in reward-related behaviors reach peak development in adolescence, while the prefrontal cortex, involved in top-down control processes, does not reach full development until young adulthood (Casey, Jones, & Hare, 2008; Steinberg, 2008).
More recently, Feldstein Ewing and colleagues (2016) proposed a theory of the neural circuitry across brain systems for adolescent sexual decision-making. The theory includes communication between the ventral tegmental area, striatum, prefrontal cortex, limbic system, insula and anterior cingulate cortex. Many of the same brain regions proposed in the adolescent sexual decision-making model overlap with the models proposed for adolescent risk-taking, including the prefrontal cortex and limbic system. These regions, prefrontal cortex and limbic structures, are associated with risk-taking and reward-seeking behavior, like RSB. Decision-making, a neurocognitive ability supported by the prefrontal cortex, and particularly the orbitofrontal cortex, may account for individual differences in propensity for engagement in RSB among youth.
To date, most studies that have assessed the association between neurocognitive function and RSB have found that poorer executive functioning is associated with more RSB (Golub, Starks, Kowalczyk, Thompson, & Parsons, 2012; Huebner, McGarrity, Smith, Perry, Suchy, 2018; Ross, Duperrouzel, Vega, & Gonzalez, 2016). Decision-making, defined as making a choice with ambiguous consequences requiring a tradeoff between reward and risk (Bechara, 2005), is one facet of impulsivity and executive function. Currently, the literature on the association between decision-making and RSB have mixed results. First, poorer performance on the IGT has been found to moderate the association between substance use and other psychosocial factors and RSB, such that greater substance use is associated with more RSB (Schuster, Crane, Mermelstein, & Gonzalez, 2012; Ross, Coxe, Schuster, Rojas, & Gonzalez, 2015). Furthermore, Golub and colleagues (2012) reported that among a group of substance dependent adults, those who performed poorly on executive function tasks engaged in the greatest number of high risk sexual behavior and high risk sexual behavior under the influence.
In contrast, several studies have also found that better decision-making performance, on the IGT, is associated with greater engagement in sexual behavior (Rendina, Millar, Dash, Feldstein Ewing, & Parsons, 2018; Wardle, Gonzalez, Bechara, & Martin-Thormeyer, 2010). Among a sample of men who have sex with men, IGT performance moderated the association between sexual arousal and sexual engagement. Specifically, among men who had above average performance on the IGT there was a stronger association between arousal and engagement compared to the men who performed below average on the IGT (Rendine et al., 2018). Another study found that among HIV+ substance dependent individuals, emotional distress was associated with RSB, but only among those who performed better on the IGT (Wardle et al., 2010).
In addition to neurocognitive performance, there are several relevant psychosocial variables to consider in the context of RSB, which include externalizing disorders (i.e., oppositional defiant disorder (ODD) and conduct disorder (CD)) and cannabis use, (Flory, Molina, Pelham, Gnagy, & Smith, 2006; Ross, Coxe, Schuster, Rojas, & Gonzalez, 2015; Schuster et al., 2012). However, psychosocial and neurocognitive factors are rarely studied together to determine how they interact to influence RSB among adolescents. Importantly, cannabis use and RSB are both risk-taking behaviors, commonly initiated in adolescence. Furthermore, individuals with externalizing disorders are more likely to engage in risk-taking behavior, like substance use and RSB (Flory et al., 2006; Sibley et al., 2014) compared to individuals without externalizing disorder symptoms.
Externalizing disorder symptoms are one likely contributor to RSB. Individuals with externalizing disorders engage in greater amounts of RSB compared to those without an externalizing disorder. Individuals diagnosed in childhood are more likely to have earlier sexual initiation, a greater number of partners, and more sex under the influence of alcohol/drugs during adolescence. These individuals are also more likely to engage in greater amounts of RSB during adulthood (Flory et al., 2006).
Numerous studies have documented the association of illicit drug use with RSB (Biglan et al., 2004) as well as the association of negative consequences from drug use with RSB (Tapert, Aarons, Sedlar, & Brown, 2001). Others have reported a positive association between number of substance dependence symptoms, including cannabis, and more RSB (Ramrakha, Caspi, Dickson, Moffitt, & Paul, 2000; Tapert et al., 2001). Fewer studies have specifically evaluated the association between cannabis use and RSB. Of importance, addressing how cannabis use is associated with RSB is imperative given the large-scale changes in the legalization of cannabis across the US and the increase in use among adolescents (Johnston et al., 2018). However, among the few studies that have assessed cannabis use and RSB, cannabis use during the most recent sexual encounter was associated with not using a condom (Bryan, Schmiege, & Magnan, 2012). Mackesy-Amiti, Fendrich, and Johnson (2010) note that surprisingly few studies address the association between dysfunctional drug use and RSB.
Cannabis use among individuals with an externalizing disorder is common (Molina & Pelham, 2003; Sibley et al., 2014). Adolescents with externalizing disorders use cannabis more frequently and escalate to heavy use more quickly compared to adolescents without an externalizing disorder (Sibley et al., 2014). Individuals with externalizing disorders engage in illicit drug use at younger ages, continue engagement into adulthood, and a greater number meet criteria for a substance use disorder compared to individuals without an externalizing disorder (Molina & Pelham, 2003). Previous research has demonstrated that associations exist between externalizing symptoms, problems from cannabis use, and RSB but the associations between these factors are complex (Ross et al., 2015).
ADHD is characterized by executive dysfunction which includes impairments in planning and attention (Willcutt, Doyle, Nigg, Faraone, & Pennington, 2005). Yet, executive dysfunction is not always observed among those with ODD/CD (Clark, Prior, & Kinsella, 2000). Unfortunately, few studies have documented how symptoms of externalizing disorders interact with measures of executive functioning in predicting risky behavior. One measure of executive functioning that may be related to risk-taking behavior in individuals with externalizing disorders is decision-making. Across 37 studies, individuals with ADHD made more risky choices on decision-making tasks compared to individuals without ADHD, a trend towards significance was observed for a moderating influence of ODD/CD (Dekkers, Popma, van Rentergem, Bexkens, & Huizenga, 2016).
Although externalizing disorders, problems from cannabis use, and decision-making abilities have been shown to be associated with RSB (Flory et al., 2006; Ross et al., 2015; Schuster et al., 2012; Tapert et al., 2001), less is known about how these variables interact to predict RSB in adolescents. Previous research on this topic has primarily included young adult cannabis users and only one measure of decision-making (Ross et al., 2015; Schuster et al., 2012). The current study employed three different measures of decision-making, the Iowa Gambling Task (IGT), the Cups Task (CT), and the Game of Dice Task (GDT), each assessing different facets of decision-making performance. The IGT is different from the other two tasks in that the participant is unaware of which choices are risky and safe at the beginning of the task. The GDT and CT provide clear information to the participant about the probability of winning or losing. What differentiates the CT from the GDT is that the CT includes both “gain” and “loss” trials and allows for assessing risk advantageous and risk disadvantageous choices separately. Furthermore, fMRI studies suggest that performance on gambling tasks with ambiguous versus specified risk conditions rely on different brain regions. Huettel, Stowe, Gordon, Warner, and Platt (2006) reported activation in the lateral prefrontal under ambiguous risk conditions while activation was reported in the posterior parietal cortex when risk conditions were specified. The three decision-making tasks allow for the examination of the association between RSB and different types of decision-making. We will evaluate the unique contribution and interaction effects of externalizing symptoms, problems from cannabis use, and risk-taking among three separate decision-making tasks, as well as differences in risk-taking from “gain” and “loss” trials, in predicting RSB among adolescents. We hypothesized that 1) decision-making abilities, externalizing symptoms, and problems from cannabis use will all account for unique variance in predicting RSB, such that more problems from cannabis use, poorer decision-making performance, and more externalizing symptoms will predict more RSB; 2) decision-making abilities will moderate the association between problems from cannabis use and RSB, such that only at poorer levels of performance on the decision-making tasks will more problems from cannabis use predict more RSB; 3) decision-making abilities will moderate the association between externalizing symptoms and RSB, such that only at poorer levels of performance on the decision-making tasks will more externalizing symptoms predict more RSB.
Methods
Participants
Participants were 204 adolescents recruited from South Florida middle and high schools, flyers distributed throughout the city, and word-of-mouth. Participants in this study were part of a larger longitudinal study (PI: RG, R01 DA033156) designed to assess how decision-making performance may influence cannabis use trajectories. Participants in the study were screened (via phone) to obtain a sample consisting predominantly of adolescents at risk for escalation of cannabis use. Inclusion criteria consisted of being 14 to 17 years old at baseline, ability to read and write in English, and some use of alcohol, cigarettes, cannabis, or other drugs (although a small percentage of the sample, ≈10% was allowed to have no history of use). Participants were excluded for self-reported developmental disorders, birth complications, neurological disorders, or history of mood, or thought disorder. Participants were also excluded at screening for possible alcohol or cannabis use disorder as well as frequent or recent use of drugs other than alcohol, nicotine, or cannabis, although those that met criteria during the study visit were not excluded from the study. All participants underwent oral fluid toxicology testing during baseline and annual follow-up visits using an Intercept oral fluid drug test (OraSure Technologies, Inc.: Bethlehem, PA). The Institutional Review Board of Florida International University approved all study procedures and protocols. Participant assent and parental consent were obtained for all participants.
Measures
Demographic Information.
Demographic information collected included age, race/ethnicity, gender, years of education, and mother’s years of education.
Wide Range Achievement Test-Fourth Edition (WRAT4) Word Reading.
The WRAT word reading subtest assess letter identification and word decoding. The total score is used as a measure for estimated IQ (Wilkinson & Robertson, 2006).
Diagnostic Interview Schedule for Children (CDISC).
The CDISC is a highly structured diagnostic assessment used to assess a variety of mental health disorders. Adolescents were administered the youth version which included major depressive disorder, ADHD, and obsessive compulsive disorder (Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000).
Risky Sexual Behavior Questionnaire (RSBQ).
The RSBQ is a detailed measure used to assess RSB (Schuster et al., 2012) which was adapted from the AIDS Risk Behavior Assessment (Donenberg, Emerson, Bryant, Wilson, & Weber-Shifrin, 2001). The RSBQ queries past sexual history, including number of sexual partners, frequency of protection, lifetime number of consequences, and the frequency of drug and alcohol use during sex. The total score of the RSBQ was used as the measure for RSB.
Youth Self-Report (YSR).
The YSR is a commonly used and well-validated measure assessing syndrome based and DSM-oriented scales. Subscales include internalizing and externalizing symptoms. The total score of the externalizing symptoms subscale was used as the measure of externalizing disorder symptoms. One question included in the YSR externalizing subscale queries about drug use (i.e., “I use drugs for nonmedical purposes (don’t include alcohol or tobacco.”)) However, this question does not ask about problems related to cannabis use or other drug use. Thus, we retained this question in the total score calculated for the externalizing symptom subscale (Achenbach & Rescorla, 2001).
Marijuana Problems Scale (MPS).
The MPS is a 19-item scale developed to assess negative consequences as a result of cannabis use (Stephens, Roffman, & Curtin, 2000) across a variety of domains (e.g., relationships, occupational/educational achievement, and finances). Participants choose from three options which are 0 = no problem, 1 = minor problem, and 2 = serious problem. The measure has been used in studies with adolescents (Foster, Li, McClure, Sonne, & Gray, 2016) and has demonstrated adequate internal consistency (Stephens, Roffman, & Curtin, 2000). The total score (ranging from 0-38), calculated by summing the choices from the participant, was used as the measure of cannabis use problems.
Decision-Making.
Decision-making was assessed via three performance-based measures, all of which assess different facets of decision-making via computer. In order to ensure motivated responding and add realism to the gains and losses experienced during the decision-making tasks, participants won different prizes based on overall performance across all tasks.
Cups Tasks (CT).
The CT was created specifically to measure decision-making in children, and under conditions of specified risk (Levin & Hart, 2003). The CT consists of 54 trials that are considered either “gain” or “loss” trials. Participants are given a visual display of 2, 3, or 5 cups on the left and right side of the computer screen. Choices from one side always yield a definite reward/smaller loss, whereas choices from the opposite side provide a chance for a greater reward or loss. Gain trials have two options: 1) definite gain of one quarter or 2) the chance to win multiple quarters or no quarters. Loss trials also have two options: 1) definite loss of one quarter or 2) a chance to lose multiple quarters or no quarters. The total number of risk disadvantageous choices (i.e., those choices associated with lower expected value) across all trials was used to quantify risk-taking. We also separately analyzed the number of risk disadvantageous choices on the loss and gain trials, labeled as CT-total, CT-gain trials, and CT-loss trials.
Game of Dice Task (GDT).
The GDT assesses decision-making when the participant is given certain rules and probabilities for monetary gains and losses throughout the task (Brand et al., 2005) and has been used with adolescents (Drechsler, Rizzo, & Steinhausen, 2008). The task evaluates decision-making under conditions of specified risk. Participants predict the outcome of a dice roll by choosing from four different options (e.g., one number vs. multiple numbers). Options with more numbers (i.e., higher probability of winning) are associated with a lesser reward compared to those with one or two possible numbers (i.e., lower probability of winning). ‘Risky choices’ are the two options with the lowest probability of winning. Participants underwent 18 trials of this task and the total number of risky choices was used to quantify performance.
Iowa Gambling Task (IGT).
The IGT is different from the aforementioned tasks in that it assesses decision-making under conditions of ambiguous risk. The task was developed to measure poor judgment and impulsive decision-making typically seen in patients with lesions of the orbitofrontal cortex (Bechara, Damasio, Damasio, & Anderson, 1994). Participants are given a visual display of four decks of cards with instruction that some decks are better than others and that more choices from “good decks” will yield a positive net total while more choices from “bad decks” will yield a negative total. IGT net score (choices from good decks – bad decks) was used to quantify performance. The IGT has been successfully used with adolescents (Ernst et al., 2003).
Statistical Analysis
All analyses were conducted in SPSS 22 using Poisson regression, due the RSBQ-total low mean score (mean = 4.1, standard deviation = 5.6) and positive skewness, resembling count data (Coxe, West, & Aiken, 2009). Each analysis included externalizing symptoms-total, MPS-total, one of the three decision-making tasks, and the interaction of these variables predicting RSBQ-total all in the same model. All independent variables were mean-centered prior to analyses. DFBETAS were examined to determine if any outliers were present and outliers were flagged if DFBETAS values were greater than the absolute value of one. One outlier was present across all analyses (DFBETAS ranging from 1.02 to 1.85). Each analysis was conducted with and without the outlier, which did not produce significant differences in results. Thus, the analyses with the outlier included was reported. Simple slope difference tests were conducted for those analyses that were significant (or approached significance). All analyses were conducted using bootstrapping with 2000 replicates.
Age, grade, mother’s education, estimated IQ and race were included in a separate regression to determine if the variables significantly predicted RSBQ-total. None of the variables significantly predicted RSBQ-total (p> 0.13). Therefore, none of these variables were included as covariates.
Simple slope difference tests were used to follow-up all significant two-way interactions. CT-total performance was set at one standard deviation below the mean (labeled as “less risk-taking,” approximately 6 risky choices), at the mean (labeled as “average risk-taking,” approximately 10 risky choices) and one standard deviation above the mean (labeled as “more risk-taking,” approximately 14 risky choices). CT-gain trials was set at one standard deviation below the mean (labeled as “less risk-taking,” approximately 2 risky choices), at the mean (labeled as “average risk-taking,” approximately 5 risky choices), and one standard deviation above the mean (labeled as “more risk-taking,” approximately 7 risky choices). Externalizing symptoms were set at one standard deviation below the mean (labeled as “less externalizing symptoms,” approximately 6 externalizing symptoms), at the mean (labeled as “average externalizing symptoms,” approximately 14 externalizing symptoms) and one standard deviation above the mean (labeled as “more externalizing symptoms,” approximately 22 externalizing symptoms).
Results
Participant Characteristics
Oral fluid tests for recent drug use revealed that five participants had recently used cannabis, one participant had recently used cocaine and one participant had recently used amphetamines. Since few participants (n = 7) tested positive for recent drug use, all participants were included in the analyses regardless of drug test results. A majority of the participants were Hispanic/Latino. Few participants met diagnostic criteria for a psychiatric disorder based on the CDISC. The most common psychiatric disorders were CD (8.3%), obsessive-compulsive disorder (4.4%), and ADHD (3.4%). Participants self-reported, on average, between 7 to 14 symptoms of externalizing disorders. In addition, the mean scores reported by participants on the MPS (M = 3.05) are comparable to studies using a sample of college students (M = 2.38; Buckner & Schmidt, 2008). A mean score of three on the MPS suggest between one and three negative consequences, with varying severity, as a results of cannabis use. The mean score of the RSBQ-total score for our current sample (M = 4.06) was much lower than previously reported among an older sample of young adults (M = 17.82; Ross et al., 2015). Participant characteristics are shown in Table 1.
Table 1:
Participant characteristics
| n = 204 | |
|---|---|
| Age | 15.49 (0.68) |
| Years of Education | 9.26 (0.86) |
| Years of Education (Mother) | 14.14 (2.41) |
| WRAT-4 Reading Standard Score | 107.94 (14.46) |
| Ethnicity/race (%) | |
| Hispanic/Latino | 72.8 |
| Caucasian | 2.9 |
| African-American | 4.4 |
| More than one race | 18.6 |
| Other | 0.5 |
| Male (%) | 54.9 |
| Amount of Lifetime Nicotine (cigarettes; MD, IQR) | 0 (0, 3) |
| Amount of Lifetime Alcohol (1 serving; MD, IQR) | 10 (1, 65.5) |
| Amount of Lifetime Cannabis (g; MD, IQR) | 8.05 (0.51, 81.8) |
| Ever Used Cannabis (%) | 79.9 |
| Used Cannabis in Past Month (%) | 55.4 |
| Ever Used Alcohol (%) | 84.3 |
| Ever Used Nicotine (%) | 44.6 |
| Ever Used Other Drugs (%) | 33.5 |
| Marijuana Problems Scale Total Score | 3.05 (3.84) |
| Current Cannabis Abuse Diagnosis (%) | 11.7 |
| Current Cannabis Dependence Diagnosis (%) | 2.9 |
| Current Alcohol Abuse Diagnosis (%) | 1.0 |
| Current Alcohol Dependence Diagnosis (%) | 1.0 |
| Current Other Drug Abuse Diagnosis (%) | 0.0 |
| Current Other Drug Dependence Diagnosis (%) | 0.0 |
| Past Cannabis Abuse Diagnosis (%) | 14.2 |
| Past Cannabis Dependence Diagnosis (%) | 7.4 |
| Past Alcohol Abuse Diagnosis (%) | 2.9 |
| Past Alcohol Dependence Diagnosis (%) | 1.5 |
| Past Other Drug Abuse Diagnosis (%) | 1.5 |
| Past Other Drug Dependence Diagnosis (%) | 1.5 |
| Iowa Gambling Task | −1.37 (23.71) |
| Cups Task (number of risk disadvantageous choices) | 9.90 (4.00) |
| Game of Dice Task (risky choices) | 7.72 (5.20) |
| Risky Sexual Behavior Questionnaire Total Score | 4.06 (5.59) |
| Ever had oral sex (%) | 60.3 |
| Ever had vaginal sex (%) | 44.8 |
| Ever had anal sex (%) | 7.4 |
| Externalizing Problems Total Score (YSR) | 14.03 (8.05) |
Note: All values are means and standard deviations unless otherwise specified. WRAT = Word Reading Achievement Test, MD = median, IQR = interquartile range,
Main Effects
Externalizing symptoms and MPS-total had a significant positive association with RSBQ-total. More risk-taking on the CT-total (combined gain and loss trials) and CT-gain trials were approaching significance in predicting a higher RSBQ-total. Performance on the CT-loss trials, GDT, and IGT did not significantly predict RSBQ-total. A correlation matrix is shown in Table 2, main results are shown in Table 3, and results for CT-gain and CT-loss trials are shown in Table 4.
Table 2.
Correlation matrix of all variables included in analyses
| RSBQ-Total Score |
MPS-Total Score |
Externalizing Symptoms |
Cups Task | Game of Dice Task |
Iowa Gabling Task |
Cups Task- Gain |
Cups Task- Loss |
|
|---|---|---|---|---|---|---|---|---|
| RSBQ-Total Score | 1 | |||||||
| MPS-Total Score | 0.41** | 1 | ||||||
| Externalizing Symptoms Total Score | 0.22** | 0.34** | 1 | |||||
| Cups Task | 0.18* | 0.18* | 0.17* | 1 | ||||
| Game of Dice Task | −0.03 | 0.05 | 0.04 | 0.25** | 1 | |||
| Iowa Gambling Task | −0.08 | 0.02 | −0.05 | −0.14 | 0.08 | 1 | ||
| Cups Task-Gain | 0.13 | 0.11 | 0.16* | 0.82** | 0.11 | −0.07 | 1 | |
| Cups Task-Loss | 0.17* | 0.19** | 0.13 | 0.84** | 0.29** | −0.15* | 0.38** | 1 |
Note:
= p-value < 0.05,
= p-value < 0.01, RSBQ = Risky Sexual Behavior Questionnaire and MPS = Marijuana Problems Scale.
Table 3.
Summary of unstandardized regression coefficients for main and interaction effects predicting RSBQ-total score
| Unstandardized Regression Coefficient |
SE | p-value | |
|---|---|---|---|
| Externalizing Symptoms, MPS, and Cups Task | |||
| Externalizing Symptoms | 0.04 | 0.01 | <0.01 |
| MPS-Total | 0.05 | 0.03 | <0.01 |
| Cups Task | 0.04 | 0.02 | 0.07 |
| Externalizing Symptoms × MPS-Total | −0.01 | 0.003 | <0.01 |
| Externalizing Symptoms × Cups Task | −0.002 | 0.003 | 0.50 |
| MPS-Total × Cups Task | 0.01 | 0.01 | 0.06 |
| Externalizing Symptoms, MPS, and Game of Dice Task | |||
| Externalizing Symptoms | 0.03 | 0.01 | <0.01 |
| MPS-Total | 0.07 | 0.03 | <0.01 |
| Game of Dice Task | −0.01 | 0.02 | 0.65 |
| Externalizing Symptoms × MPS-Total | −0.003 | 0.003 | 0.25 |
| Externalizing Symptoms × Game of Dice Task | 0.00005 | 0.002 | 0.98 |
| MPS-Total × Game of Dice Task | −0.01 | 0.01 | 0.15 |
| Externalizing Symptoms, MPS, and Iowa Gambling Task | |||
| Externalizing Symptoms | 0.03 | 0.01 | <0.01 |
| MPS-Total | 0.08 | 0.03 | <0.01 |
| Iowa Gambling Task | −0.01 | 0.004 | 0.14 |
| Externalizing Symptoms × MPS-Total | −0.003 | 0.003 | 0.08 |
| Externalizing Symptoms × Iowa Gambling Task | 0.0004 | 0.0005 | 0.30 |
| MPS-Total × Iowa Gambling Task | −0.001 | 0.002 | 0.71 |
Note: MPS = Marijuana Problems Scale and SE = standard error. Bolded results indicate significance (p<0.05), italicized results indicate approaching significance (p<0.10).
Table 4.
Summary of unstandardized regression coefficients for main and interaction effects of Cups Task gain and loss trials predicting RSBQ-total score
| Unstandardized Regression Coefficient |
SE | p-value | |
|---|---|---|---|
| Externalizing Symptoms, MPS, and Cups Task-Gain | |||
| Externalizing Symptoms | 0.03 | 0.01 | <0.01 |
| MPS-Total | 0.08 | 0.02 | <0.01 |
| Cups Task-Gain | 0.06 | 0.04 | 0.09 |
| Externalizing Symptoms × MPS-Total | −0.01 | 0.003 | <0.01 |
| Externalizing Symptoms × Cups Task-Gain | −0.004 | 0.003 | 0.19 |
| MPS-Total × Cups Task-Gain | 0.02 | 0.01 | 0.08 |
| Externalizing Symptoms, MPS, and Cups Task-Loss | |||
| Externalizing Symptoms | 0.03 | 0.01 | <0.01 |
| MPS-Total | 0.05 | 0.03 | 0.06 |
| Cups Task-Loss | 0.05 | 0.04 | 0.18 |
| Externalizing Symptoms × MPS-Total | −0.003 | 0.003 | 0.10 |
| Externalizing Symptoms × Cups Task-Loss | −0.001 | 0.004 | 0.87 |
| MPS-Total × Cups Task-Loss | 0.01 | 0.01 | 0.27 |
Note: MPS = Marijuana Problems Scale and SE = standard error. Bolded results indicate significance (p<0.05), italicized results indicate approaching significance (p<0.10).
Decision-making as a moderator between problems from cannabis use and RSB.
Cups Task-Total.
The interaction between the MPS-total and CT-total performance on RSBQ-total approached statistical significance. Simple slope difference tests revealed that the MPS-total significantly predicted RSBQ-total; however, this association varied depending on CT-total performance. MPS-total significantly predicted RSBQ-total at levels of more risk-taking on the CT-total. The association between MPS-total and RSBQ-total was also significant at average levels of risk-taking on the CT-total. However, at levels of less risk-taking on the CT-total the association between MPS-total and RSBQ-total was not significant (see Figure 1).
Figure 1.
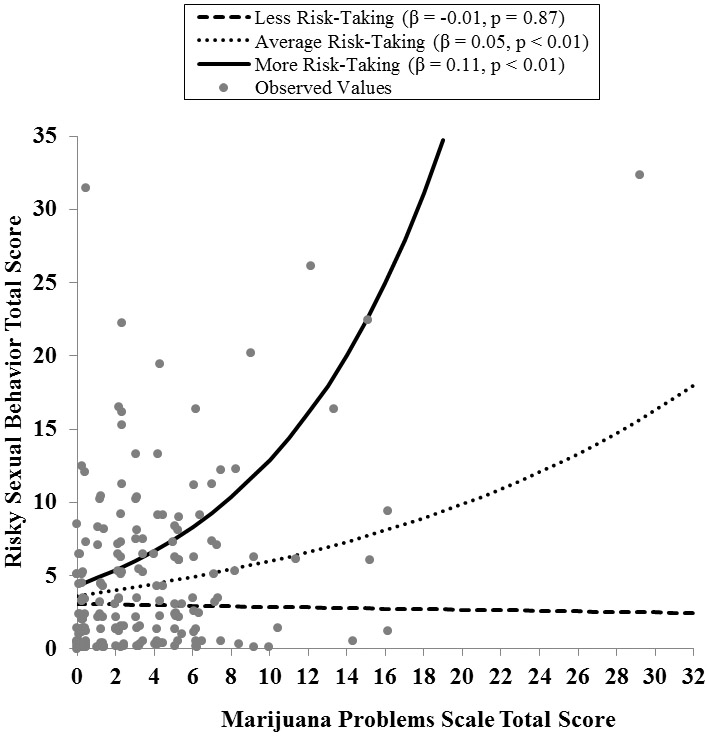
Simple slopes of the effects of MPS-total score on RSBQ-total score at different levels of risk-taking on the CT
Note: CT = cups task. Observed values are jittered.
Cups Task-Gain Trials.
The interaction between the MPS-total and CT-gain trials performance on RSBQ-total also approached statistical significance. Similar to the results of the CT-total, simple slope difference tests revealed that at average and more risk-taking on the CT-gain trials there was a positive significant association between MPS-total and RSBQ-total. The MPS-total and RSBQ-total were not significantly associated at levels of less risk-taking on the CT-gain trials. The patterns that emerged here are similar to the CT total (see Figure 2).
Figure 2.
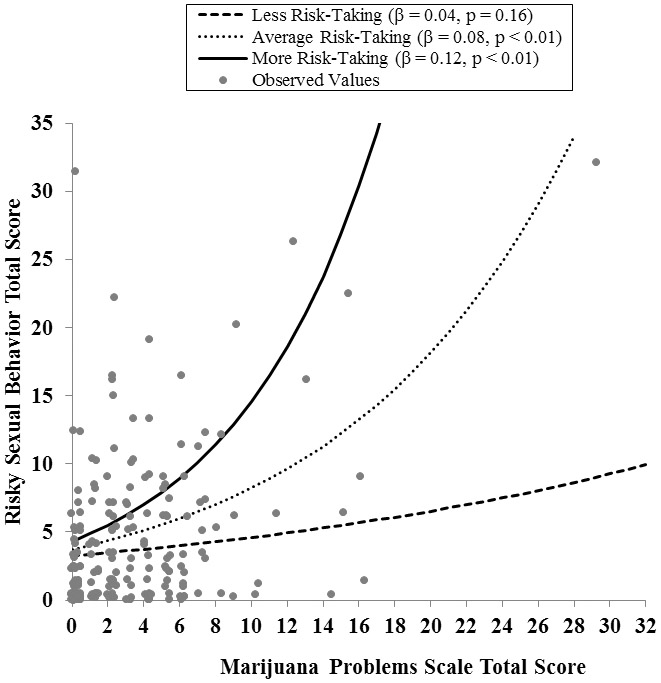
Simple slopes of the effects of MPS-total score on RSBQ-total score at different levels of risk-taking on the CT-gain trials
Note: CT = cups task. Observed values are jittered.
Cups Task-Loss Trials.
There was no evidence of an interaction between the MPS-total and CT-loss trials performance on RSBQ-total.
Game of Dice Task and Iowa Gambling Task.
The interaction between the MPS-total and GDT/IGT performance did not significantly predict RSBQ-total.
Decision-making as a moderator between externalizing symptoms and RSB.
We found no evidence that decision-making abilities moderate the association between externalizing symptoms and RSBQ-total.
Externalizing symptoms as a moderator between problems from cannabis use and RSB.
A significant interaction effect was observed between the MPS-total and externalizing symptoms in predicting RSBQ-total (only when the CT was included) and was approaching significance when the IGT was included. Simple slope difference tests revealed that at average (β = 0.05, SE = 0.03, p < 0.01) and less (β = 0.09, SE = 0.03, p < 0.01) externalizing symptoms, there is a significant positive association between MPS-total and RSBQ-total. However, at more externalizing symptoms (β = 0.01, SE = 0.03, p = 0.84), there is not a significant association between MPS-total and RSBQ-total.
Discussion
The current study examined how externalizing symptoms, problems from cannabis use, decision-making performance and the interactions among these variables influenced RSB. No studies, to our knowledge, have assessed the association between decision-making abilities and RSB among a sample of adolescents. Generally, externalizing symptoms, problems from cannabis use, and decision-making performance (only on the CT-total and CT-gain trails) predicted RSB. Interaction effects emerged between problems from cannabis use and CT performance as well as between externalizing symptoms and problems from cannabis use predicting RSB. Several of our hypotheses were supported by the results of the study, and results inconsistent with our hypotheses also emerged. Specifically, a positive association emerged between problems from cannabis use and RSB at high levels of risk-taking on the CT-total and CT-gain trials, followed by average levels of risk disadvantageous choices on the CT-total and CT-gain trials. At low levels of risk-taking on the CT-total and CT-gain trials, the association between problems from cannabis use and RSB was not significant. Additionally, an interaction emerged between problems from cannabis use and externalizing symptoms in predicting RSB. At low levels of externalizing symptoms, the strongest positive association emerged between problems from cannabis use and RSB, followed by average levels of externalizing symptoms. At high levels of externalizing symptoms, the positive association between problems from cannabis use and RSB approached significance.
The results from this study are consistent with previous research studies suggesting that more externalizing symptoms are associated with more RSB. Others have reported that adults with a childhood diagnosis of an externalizing disorder have a greater number of sexual partners and more unplanned pregnancies compared to adults without an externalizing disorder diagnosis (Flory et al., 2006). The current study extends these findings into adolescence.
Similarly, more problems from cannabis use were associated with more RSB. Findings are consistent with studies that have documented the association between substance use disorder symptoms and RSB (Ramrakha et al., 2000; Tapert et al., 2001). For example, adolescents involved in treatment for substance use disorders engaged in more RSB compared to a sample of community controls (Tapert et al., 2001). Generally, our findings are consistent with studies that have documented associations between RSB and amount, frequency, age of initiation of cannabis use, and substance use disorder symptoms despite relying specifically on an index of problematic cannabis use.
Unexpectedly, we did not find that poorer performance across decision-making tasks was invariably related to RSB. More risk-taking during the CT-total and CT-gain trials was associated with more RSB; this was not the case for the GDT or IGT. This could be due to the CT being the only task that differentiates risk advantageous and disadvantageous choices. Some research suggests that not all risk-taking during adolescence is impulsive or hazardous, and that some risk-taking may be advantageous for various reasons, like connecting with peers (Willoughby, Good, Adachi, Hamza, & Tavernier, 2014). Perhaps, it is only engagement in disadvantageous risk-taking that is associated with RSB among adolescents. Further investigation is necessary to clarify why results differ between the CT, GDT, and IGT. As previously mentioned, the CT was specifically designed to measure decision-making abilities, an aspect of executive functioning, in children and adolescents. Thus, our findings are consistent, only in part, with previous findings that poorer executive functioning is associated more RSB (Ross et al., 2016).
Interestingly, more risk disadvantageous choices on the CT-gain trials was approaching significance in being associated with RSB, however there was no significant association between CT-loss trials and RSB. These results suggest that adolescents who engage in more disadvantageous risk-taking for a potential reward are more likely to engage in RSB. Furthermore, more disadvantageous risk-taking to reduce the amount of reward lost was not associated with RSB. These results are logical given the inherent risk associated with engagement in RSB, but also the natural rewards as a result.
The CT and GDT were significantly correlated, while the IGT was not correlated with the either the CT or GDT. These findings are consistent with previous studies reporting non-significant correlations (ranging from 0.01 (Ross et al., 2016; Weller, Levin, & Bechara, 2010) to 0.57 (Brand, Recknor, Grabenhorst, & Bechara, 2007)) between the IGT and the GDT or CT. Furthermore, the IGT was designed to examine decision-making in adults, while the CT and GDT were designed for use in children and adolescents. In addition, the IGT, unlike the CT and GDT, assesses decision-making when the risky and safe choices are ambiguous. As such, the IGT is a more complex task compared to the CT and GDT, which may not be able to differentiate poor or better decision-making among children or adolescent samples.
Performance on the CT-total and the CT-gain trials appeared influential in the complex associations between decision-making, problems from cannabis use, and RSB. Specifically, more problems from cannabis use were associated with more RSB, at more and average levels of risk-taking on the CT-total and the CT-gain trials. At low levels of risk-taking, there was no association between problems from cannabis use and RSB. These findings suggest that less risk-taking on the CT may be protective against engaging in more RSB, regardless of problems experienced from cannabis use. This is consistent with another study of adults from our group that reported a significant positive association between amount of cannabis use and RSB, but only among individuals who performed worse on a decision-making task (Schuster et al., 2012).
Problems from cannabis use and externalizing symptoms interacted in predicting RSB. Specifically, at levels of less externalizing symptoms, there was a stronger association between problems from cannabis use and RSB compared to levels of average and high externalizing symptoms. Specifically, among individuals with no or minimal externalizing symptoms, more problems related to cannabis use were associated with more RSB. The association between problems from cannabis use and RSB was weaker at average and higher levels of externalizing symptoms. Individuals with externalizing disorders are more likely to engage in RSB compared to individuals without an externalizing disorder (Flory et al., 2006). However, several studies have also reported romantic relationship impairments among young adults with externalizing disorders (Canu & Carlson, 2007; Canu & Carlson, 2003; Canu, Tabor, Michael, Bazzini, & Elmore, 2014), which is not surprising given the well-documented social impairments among these individuals (Sibley, Evans, & Serpell, 2010). Specifically, young adults with ADHD are viewed as less desirable by confederates compared to young adults without ADHD (Canu & Carlson, 2003). Difficulties establishing romantic relationships and more overall risk-taking among individuals with externalizing disorders might, in part, account for these results.
The current study also had several limitations. First, participants in the current study were recruited to obtain a sample of adolescents who were at risk for escalation of cannabis use, and few participants met diagnostic criteria for an externalizing disorder (e.g., ADHD = 3.4%). Our results may have differed if we would have specifically recruited a sample with a more severe presentation of externalizing symptoms. However, given our reliance on a continuous measure of externalizing symptoms and based on the variability of responses observed, we hypothesize that these findings may generalize to patient groups that report externalizing symptoms. In general, adolescents with externalizing disorders are poorer reporters of their own competencies and symptoms (Smith, Pelham, Gnagy, Molina, & Evans, 2000). The current study utilized a self-report measure of externalizing symptoms and therefore may be less accurate compared to an informant report. Another limitation is the low mean score of the MPS, suggesting that participants in our sample did not experience many cannabis-related problems. This may have contributed to the small effects reported in our study. Lastly, we did not control for other substance use in our analyses (e.g., alcohol, nicotine, or other drug use), though the sample was recruited for their preference for cannabis and our primary measure of drug use-related behavior was specifically problems from cannabis use.
Determining what neurocognitive factors predict or moderate predictors of RSB in a high-risk population of adolescents will inform future prevention and intervention efforts. For example, in the current study, decision-making performance moderated the association between problems from cannabis use and RSB. Prevention and treatment programs may benefit from tailoring specifically to an adolescent’s decision-making abilities. In other words, interventions for adolescents who engage in less risk-taking on decision-making tasks would focus on reducing other relevant psychosocial factors, whereas adolescents who engage in average and greater risk-taking on decision-making tasks would benefit from cognitive training strategies. Unfortunately, few studies have examined the impact different intervention strategies have on executive function. Goal Management Training, a mindfulness-based approach, is effective at improving executive functioning among individuals who have experienced traumatic brain injuries (Levine et al., 2011). Incorporation of these strategies in the prevention and treatment of risk-taking behavior among adolescents may result in more successful outcomes.
Acknowledgements
This work was supported by grants R01 DA031176 (PI: Gonzalez), R01 DA033156 (PI: Gonzalez), and T32 DA017637 (PI: Hewitt) from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors have no other conflicts of interest to declare.
References
- Achenbach TM, & Rescorla LA. (2001). Manual for the ASEBA school-age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families. [Google Scholar]
- Bechara A (2005). Decision making, impulse control and loss of willpower to resist drugs: a neurocognitive perspective. Nature Neuroscience, 8 (11), 1458–1463. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio AR, Damasio H, & Anderson SW (1994). Insensitivity to future consequences following damage to human prefrontal cortex. Cognition, 50 (1), 7–15. [DOI] [PubMed] [Google Scholar]
- Biglan A, Brennan P, Foster S, Holder H, Miller T, & Cunningham P (2004). Helping adolescents at risk: Prevention of problem behaviors. New York, NY: The Guilford Press. [Google Scholar]
- Brand M, Fujiwara E, Borsutzky S, Kalbe E, Kessler J, & Markowitsch HJ (2005). Decision-making deficits of korsakoff patients in a new gambling task with explicit rules: associations with executive functions. Neuropsychology, 19(3), 267–277. [DOI] [PubMed] [Google Scholar]
- Brand M, Recknor EC, Grabenhorst F, & Bechara A (2007). Decisions under ambiguity and decisions under risk: Correlations with executive functions and comparisons of two different gambling tasks with implicit and explicit rules. Journal of Clinical and Experimental Neuropsychology, 29, 86–99. [DOI] [PubMed] [Google Scholar]
- Bryan AD, Schmiege SJ, & Magnan RE (2012). Marijuana use and risky sexual behavior among high-risk adolescents: Trajectories, risk factors, and event-level relationships. Developmental Psychology, 48 (5), 1429–1442. [DOI] [PubMed] [Google Scholar]
- Buckner JD, & Schmidt NB (2008). Marijuana effect expectancies: Relations to social anxiety and marijuana use problems. Additive Behaviors, 33 (11), 1477–1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canu WH, & Carlson CL (2007). Rejection sensitivity and social outcomes of young adult men with ADHD. Journal of Attention Disorders, 10 (3), 261–275. [DOI] [PubMed] [Google Scholar]
- Canu WH, & Carlson GL (2003). Differences in heterosocial behavior and outcomes of ADHD-symptomatic subtypes in a college sample. Journal of Attention Disorders, 6 (3), 123–133. [DOI] [PubMed] [Google Scholar]
- Canu WH, Tabor LS, Michael KD, Bazzini DG, & Elmore AL (2014). Young adult romantic couples’ conflict resolution and satisfaction varies with partner’s attention–deficit/hyperactivity disorder type. Journal of Marital and Family Therapy, 40 (4), 509–524. [DOI] [PubMed] [Google Scholar]
- Casey BJ, Jones RM, & Hare TA (2008). The adolescent brain. Annals of the New York Academy of Sciences, 1124 (1), 111–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark C, Prior M, & Kinsella GJ (2000). Do executive function deficits differentiate between adolescents with ADHD and oppositional defiant/conduct disorder? A neuropsychological study using the Six Elements Test and Hayling Sentence Completion Test. Journal of Abnormal Child Psychology, 28 (5), 403–414. [DOI] [PubMed] [Google Scholar]
- Coxe S, West SG, & Aiken LS (2009). The analysis of count data: A gentle introduction to Poisson regression and its alternatives. Journal of Personality Assessment, 91 (2), 121–136. [DOI] [PubMed] [Google Scholar]
- Dekkers TJ, Popma A, van Rentergem JAA, Bexkens A, & Huizenga HM (2016). Risky decision making in attention-deficit/hyperactivity disorder: A meta-regression analysis. Clinical Psychology Review, 45, 1–16. [DOI] [PubMed] [Google Scholar]
- Donenberg GR, Emerson E, Bryant FB, Wilson H, & Weber-Shifrin E (2001). Understanding AIDS-risk behavior among adolescents in psychiatric care: Links to psychopathology and peer relationships. Journal of the American Academy of Child & Adolescent Psychiatry, 40 (6), 642–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drechsler R, Rizzo P, & Steinhausen HC (2008). Decision-making on an explicit risk-taking task in preadolescents with attention-deficit/hyperactivity disorder. Journal of Neural Transmission, 115 (2), 201–209. [DOI] [PubMed] [Google Scholar]
- Ernst M, Grant SJ, London ED, Contoreggi CS, Kimes AS, & Spurgeon L (2003). Decision making in adolescents with behavior disorders and adults with substance abuse. American Journal of Psychiatry, 160 (1), 33–40. [DOI] [PubMed] [Google Scholar]
- Feldstein-Ewing SWF, Ryman SG, Gillman AS, Weiland BJ, Thayer RE, & Bryan AD (2016). Developmental cognitive neuroscience of adolescent sexual risk and alcohol use. AIDS and Behavior, 20 (1), 97–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flory K, Molina BSG, Pelham WE, Gnagy E & Smith B (2006). Childhood ADHD predicts risky sexual behavior in young adulthood. Journal of Clinical Child and Adolescent Psychology, 35 (4), 571–577. [DOI] [PubMed] [Google Scholar]
- Foster KT, Li N, McClure EA, Sonne SC, & Gray KM (2016). Gender differences in internalizing symptoms and suicide risk among men and women seeking treatment for cannabis use disorder from late adolescence to middle adulthood. Journal of Substance Abuse Treatment, 66, 16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golub SA, Starks TJ, Kowalczyk WJ, Thompson LI, & Parsons JT (2012). Profiles of executive functioning: Associations with substance dependence and risky sexual behavior. Psychology of Addictive Behaviors, 26(4), 895–905. 10.1037/a0029034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huebner DM, McGarrity LA, Smith TW, Perry NS, Suchy Y (2018). Changes in executive function following a stressful interpersonal task are associated with condomless anal intercourse among men who have sex with men. Annals of Behavioral Medicine, 52 (5), 406–411. 10.1093/abm/kax020. [DOI] [PubMed] [Google Scholar]
- Huettel SA, Stowe CJ, Gordon EM, Warner BT, & Platt ML (2006). Neural signatures of economic preferences for risk and ambiguity. Neuron, 49 (5), 765–775. 10.1016/j.neuron.2006.01.024. [DOI] [PubMed] [Google Scholar]
- Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, & Patrick ME (2018). Monitoring the Future national survey results on drug use: 1975-2017: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan. [Google Scholar]
- Levin IP, & Hart SS (2003). Risk preferences in young children: Early evidence of individual differences in reaction to potential gains and losses. Journal of Behavioral Decision Making, 16 (5), 397–413. [Google Scholar]
- Levine B, Schweizer TA, O’Connor C, Turner G, Gillingham S, Stuss DT, … Robertson IH (2011). Rehabilitation of executive functioning in patients with frontal lobe brain damage with goal management training. Frontiers in Human Neuroscience, 5 (9), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackesy-Amiti M, Fendrich M, & Johnson T (2010). Symptoms of substance dependence and risky sexual behavior in a probability sample of HIV-negative men who have sex with men in Chicago. Drug and Alcohol Dependence, 110(1-2), 38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BS, & Pelham WE (2003). Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. Journal of Abnormal Psychology, 112 (3), 497–507. [DOI] [PubMed] [Google Scholar]
- Ramrakha S, Caspi A, Dickson N, Moffitt TE, & Paul C (2000). Psychiatric disorders and risky sexual behaviour in young adulthood: Cross sectional study in birth cohort. BMJ, 321 (7256), 263–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendina JH, Millar BM, Dash G, Feldstein Ewing SW, & Parsons JT (2018) The somatic marker hypothesis and sexual decision making: Understanding the role of Iowa Gambling Task performance and daily sexual arousal on the sexual behavior of gay and bisexual men. Annals of Behavioral Medicine, 52 (5), 380–392. 10.1093/abm/kax006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross JM, Coxe S, Schuster RM, Rojas A, & Gonzalez R (2015). The moderating effects of cannabis use and decision making on the relationship between conduct disorder and risky sexual behavior. Journal of Clinical and Experimental Neuropsychology, 37 (3), 303–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross JM, Duperrouzel J, Vega M, & Gonzalez R (2016). The neuropsychology of risky sexual behavior. Journal of the International Neuropsychological Society, 22 (6), 586–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MCB, … Weinstock H (2013). Sexually transmitted infections among US women and men: Prevalence and incidence estimates, 2008. Sexually Transmitted Diseases, 40 (3), 187–193. [DOI] [PubMed] [Google Scholar]
- Schuster RM, Crane NA, Mermelstein R, & Gonzalez R (2012). The influence of inhibitory control and episodic memory on the risky sexual behavior of young adult cannabis users. Journal of International Neuropsychology, 18 (5), 827–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, & Schwab-Stone ME (2000). NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry, 39 (1), 28–38. [DOI] [PubMed] [Google Scholar]
- Sibley MH, Evans SW, & Serpell ZN (2010). Social cognition and interpersonal impairment in young adolescents with ADHD. Journal of Psychopathology and Behavioral Assessment, 32 (2), 193–202. [Google Scholar]
- Sibley MH, Pelham WE Jr, Molina BS, Coxe S, Kipp H, Gnagy EM, … Lahey BB (2014). The role of early childhood ADHD and subsequent CD in the initiation and escalation of adolescent cigarette, alcohol, and marijuana use. Journal of Abnormal Psychology, 123(2), 362–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith BH, Pelham WE Jr, Gnagy E, Molina B, & Evans S (2000). The reliability, validity, and unique contributions of self-report by adolescents receiving treatment for attention-deficit/hyperactivity disorder. Journal of Consulting and Clinical Psychology, 68 (3), 489–499. [DOI] [PubMed] [Google Scholar]
- Steinberg L (2008). A social neuroscience perspective on adolescent risk-taking. Developmental Review, 28 (1), 78–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens RS, Roffman RA, & Curtin L (2000). Comparison of extended versus brief treatments for marijuana use. Journal of Consulting and Clinical Psychology, 68 (5), 898–908. [PubMed] [Google Scholar]
- Tapert SF, Aarons GA, Sedlar GR, & Brown SA (2001). Adolescent substance use and sexual risk-taking behavior. Journal of Adolescent Health, 28 (3), 181–189. [DOI] [PubMed] [Google Scholar]
- Wardle MC, Gonzalez R, Bechara A, & Martin-Thormeyer EM (2010) Iowa Gambling Task performance and emotional distress interact to predict risky sexual behavior in individuals with dual substance and HIV diagnoses. Journal of Clinical and Experimental Neuropsychology, 32 (10), 1110–1121. DOI: 10.1080/13803391003757833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weller JA, Levin IP, & Bechara A (2010). Do individual differences in Iowa Gambling Task performance predict adaptive decision making for risky gains and losses? Journal of Clinical and Experimental Neuropsychology, 32, 141–150. [DOI] [PubMed] [Google Scholar]
- Wilkinson GS, & Robertson GJ (2006). Wide Range Achievement Test-Fourth Edition. Lutz, FL: Psychological Assessment Resources. [Google Scholar]
- Willcutt EG, Doyle AE, Nigg JT, Faraone SV, & Pennington BF (2005). Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biological Psychiatry, 57 (11), 1336–1346. [DOI] [PubMed] [Google Scholar]
- Willoughby T, Good M, Adachi PJC, Hamza C, & Tavernier R (2014). Examining the link between adolescent brain development and risk taking from a social–developmental perspective, Brain and Cognition, 89, 70–78. 10.1016/j.bandc.2014.07.006. [DOI] [PubMed] [Google Scholar]


