Abstract
Sleep and social relationships are two key determinants of psychosocial health that undergo considerable change across the transition to motherhood. The current study investigated the bidirectional relationship between daytime Positive and Negative Social Interactions (PSIs & NSIs) and nighttime sleep quality on maternal mood across 1 week in the 3–6 month postpartum period. Sixty healthy, non-depressed first-time mothers completed 7-consecutive days of daily social interaction and sleep diaries. Results indicated that higher than average sleep quality buffered the effect of higher than average NSIs on maternal mood (i.e., buffered mood reactivity) and appeared to promote mood recovery following a particularly “bad day” (i.e., higher than average NSIs). In addition, although PSIs were more common than NSIs overall, the most frequent and positively rated PSIs were with baby as were the most frequent and negatively rated NSIs. To our knowledge, our results are the first to characterize the impact of PSIs on postpartum maternal mood, assess maternal-infant social interactions in daily diary study of postpartum social relationships, and demonstrate the role that maternal sleep quality plays in social discord-related mood reactivity and mood recovery processes in the 3–6 month postpartum period.
Keywords: Postpartum, Mood, Sleep quality, Social interactions, Daily diary
Introduction
The transition to motherhood can be an exciting and rewarding experience, however, it is also highly stressful and demanding. The birth of an infant brings about more widespread change than any other developmental phase of the family life cycle (Nystrom & Ohrling, 2004) and early researchers even characterized this transition as a crisis (Le Masters, 1959). Although many women make this transition without trouble, a small, but significant, number of women may be debilitated by their new role. Thus, it is important to identify modifiable factors that can minimize risk and promote psychosocial health during the postpartum period (Fowden et al., 2006; Gicquel et al., 2008; Kuh & Ben-Shlomo, 2004).
Two key determinants of psychosocial health in the general population, as well as in postpartum populations, are sleep and social relationships (Maxson et al., 2016; Uchino, 2006). Sleep is a fundamental biological need for humans and is significantly disrupted after the birth of a child. Postpartum sleep disruption has been linked to a number of deleterious maternal health outcomes, including postpartum depression (Boyce & Hickey, 2005; Dennis & Ross, 2005; D0rheim et al., 2009; Ross et al., 2004), poor adjustment to the maternal role (Bayer et al., 2007; Hiscock & Wake, 2001), and impaired mother-infant bonding (Morrell & Steele, 2003). Stable, supportive social relationships are also a critical resource for human health and well-being as well as one of the most robust predictors of maternal adjustment and well-being in the postpartum (Maxson et al., 2016). Importantly, the existing research on the impact of social relationships in the postpartum period has been limited, as many studies rely on cross-sectional study designs. Although previous studies of postpartum women have examined the independent roles of sleep and social relationships on various domains of psychosocial health (Lawson et al., 2015; Reid & Taylor, 2015; Schwab- Reese et al., 2017), no previous study has examined the bidirectional relationship between sleep and social relationships on postpartum maternal mood. This is a notable gap in the literature given that sleep disruption has been reliably linked with mood degradation in postpartum women (Bei et al., 2015) and may also have more insidious effects on mood stability by disrupting efforts to regulate emotion and manage the multiple demands of new motherhood. Accordingly, the purpose of the current study was to longitudinally examine the relationship between daytime social interactions and nighttime sleep quality on maternal mood in a sample of 60 healthy, non-depressed first-time mothers across 1 week in the 3–6 month postpartum period.
Sleep disruption and its downstream effects progress dynamically across the postpartum period. Due to infants’ polyphasic sleep cycle and nighttime care needs, maternal wake times may increase by as much as 20% across the first 6 weeks. As women progress through the first postpartum year, the decline in sleep duration may be less prevalent or problematic than the persistent degradation in sleep quality. By the third month postpartum, many infants begin to have a more consistent and predictable nocturnal sleep period (Figueiredo et al., 2016; Montgomery-Downs et al., 2010; Dørheim et al., 2009) and objective measurements of maternal sleep during this time indicate that durations of sleep return to the “normal range” for healthy adults (i.e., 7.2 h; Lillis et al., 2016; Montgomery-Downs et al., 2010; D0rheim et al., 2009). Importantly, these longer maternal sleep bouts have also been shown to be highly fragmented, with an average of 2 h of wakefulness per night (Montgomery-Downs et al., 2010). This fragmentation may partly explain the persistent link observed between low maternal mood and poor subjective sleep quality, even after controlling for a number of confounding factors, including objectively measured sleep duration (Park et al., 2013) and infant temperament (Goyal et al., 2009). As such, after the first 3 months postpartum, subjective sleep quality may reveal more about daytime functioning and adjustment to the maternal role than objective sleep duration estimates.
Just as sleep is a major factor in the adjustment to new parenthood, so too are social relationships a key determinant of postpartum psychosocial health. Social support and positive social interactions are related to positive mental health in the general population (Brown et al., 2003; Bur-man & Margolin, 1992; Coyne & DeLongis, 1986; Fin-cham, 2003; Revenson, 1994; Robles & Kiecolt-Glaser, 2003; Seeman et al., 1987; Tower et al., 2002) and have also been hypothesized to buffer the negative systemic effects of stress during the postpartum period (Gerin et al., 1995; Hammer, 1983). Indeed, perceived availability and actual provisions of emotional and physical support from partners have been found to be related to relationship satisfaction and maternal adjustment in the postpartum period (Burke, 2003; Majewski, 1987; Power & Parke, 1984; Shapiro et al., 2000). Conversely, many studies have documented that new mothers’ perceptions of inadequate support from their partners resulted in feelings of resentment and increased conflict (Belsky et al., 1986; Barclay et al., 1997; Hall, 1992; McBridge & Shore, 2001). Collectively these data illustrate that social relationships can have both a positive effect on functioning or act as another demand on interpersonal resources.
Extant measures of social support and partner support capture important but static impressions of the social environment. Repeated measurement strategies, such as Ecological Momentary Assessment (EMA) and daily diaries, are well-suited to capture the ebb and flow of social activity and psychosocial functioning, as well as the role of sleep-related changes in these processes. These more intensive daily assessment approaches have yielded interesting connections between sleep and social relationships. For instance, parenting self-efficacy and baby crying behavior contributed to decreased marital satisfaction and insomnia during the first year postpartum (Meijer & van den Wittenboer, 2007), and there is strong evidence for a bi-directional relationship between the quality of partner social interaction and sleep (Meijer & van den Wittenboer, 2007; Troxel, 2010; Troxel et al., 2007). Negative social interactions have also been linked with depressive symptoms in the postpartum. In a small study of postpartum women, measures of partner quality were inversely related to symptoms of depression while reports of arguments during the past week were related to higher levels of symptoms of depression (Page & Wilhelm, 2007). Although previous studies have used daily diary data to capture negative social interactions among adults in the postpartum, to our knowledge, no study has attempted to also measure positive social interactions in the postpartum period. This is a noteworthy oversight given the aforementioned demands of new motherhood and the well-documented buffering effect of positive social interactions on the stress process (Cohen & Hoberman, 1983). Furthermore, no previous study has investigated the impact of interaction between arguably the most intensely interactive social dyad in the postpartum: mother and baby. Omissions of entire classes of social interactions and relationships limit the scope of our understanding of the postpartum social milieu.
Along these lines, rather than viewing sleep quality as either a predictor or outcome of maternal adjustment-related difficulties, it may be more useful to consider the role of sleep quality as an intrapersonal-energetic resource that may enhance the ability to respond to the day-to-day social demands of new parenthood. Specifically, high quality sleep may serve as a resource that buffers the effect of stress or negative social interactions on maternal mood (i.e., mood reactivity). The effect of adequate sleep quality on mood reactivity has been observed in parents of children with autism (Estrela et al., 2017), Israeli college students (Lev Ari & Schulman, 2012), women with fibromyalgia (Hamilton et al., 2008), and women with migraines (Spierings et al., 1996). In addition, adequate sleep quality may also enhance recovery from a particularly stressful day on next-day mood, a process that has been demonstrated in women with chronic pain (Hamilton et al., 2007). These data collected from a wide range of populations paint a compelling picture about the intersection of social interactions, mood, and sleep. Examining the impact of the postpartum social milieu on a micro/day-to-day level may uncover how a broad spectrum of social interactions relates to other micro/day-to-day level processes, including maternal sleep.
Goals of the present study
The current study sought to improve upon the existing postpartum sleep and social environment literature by using a daily diary format to answer a number of questions about maternal social activity, sleep quality, and mood between 3 and 6 months postpartum. Using a repeated measurement design, we sought to examine the dynamic relationship of daily Positive Social Interactions and Negative Social Interactions (PSIs & NSIs; with Baby, Partner, Family Members, Friends, and Co-Workers) to maternal mood across 1 week in the 3–6-month postpartum period from a sample of 60 first-time mothers. We also examined whether nighttime sleep quality moderated the relationship between daily PSIs, NSIs, and mood. It was hypothesized that higher numbers of PSIs and lower numbers of NSIs would be related to higher daily Positive Affect and lower Negative Affect, respectively. In addition, we hypothesized there would be a “mood reactivity” effect, such that high sleep quality would buffer the effect NSIs on mood. Further, we expected that there would be a “mood recovery” effect, such that higher sleep quality would promote more positive mood states the following day.
Method
Participants and procedure
Our institution’s Review Board approved this study. Inclusion criteria were as follows: first-time mother, one 3–6 month-old infant, and a cohabitating/parenting partner. Exclusion criteria were as follows: (a) history of sleep disorders (self-reported); (b) endocrine or immune disorders; (c) current sleep medication use (d) history of psychosis or manic episodes; (e) current night shift occupation; (f) currently experiencing symptoms of a Major Depressive Episode (i.e., endorsed depressed mood and/or loss of interest/pleasure in normally enjoyable activities most days over the previous 2 weeks (American Psychiatric Association, 2013); or (g) baby was in the NICU. Participants were recruited from online advertisements, in-person announcements at maternal support groups and breastfeeding support groups, and via the distribution of flyers in a small college town and its nearby metropolitan community.
Participants were asked to choose a study week that was “fairly normal” (partner in town, self/baby not currently ill, no recent travel across multiple time zones, etc.). Following completion of baseline measures of relationship satisfaction, maternal functioning, social support, and loneliness, the main study procedures across the participation week for enrolled participants included completing a daily online morning survey about their previous nights’ sleep characteristics and completing a nightly online evening survey about their social interactions and mood experienced during the day. Participants were emailed Morning Sleep Diary and Evening Diary links via a secure online survey site (Qualtrics, 2018) that could be completed on any email-receiving device. Participants earned up to $50 for participation (inclusive of a $15 bonus for full study protocol adherence, of which 95% qualified). Demographic characteristics of the final sample (n = 60) have been previously reported (Lillis et al., 2016).
Measures
Daily diary measures
Positive and Negative Daily Interactions
The Evening Diary (completed prior to evening sleep) collected information related to Positive Social Interactions (PSIs) and Negative Social Interactions (NSIs) experienced throughout the day. The PSI and NSI items were modeled after the Interpersonal Stress and Life Event Inventory (ISLE), a social interaction instrument that measures interaction frequency/quality with partner, child, family, friends/acquaintances and co-workers (Zautra et al., 1986). The instrument was modified for a postpartum population to include baby-related questions using items drawn from the Childcare Activities Questionnaire (CCAQ) (Montague & Walker-Andrews, 2002).
PSI and NSI scores were then calculated by an index of frequency and quality of interactions. Daily PSIs were rated by participants on a 7-point Likert scale of enjoyment from 1 (not enjoyable at all) to 7 (extremely enjoyable). Daily NSIs were rated by participants on 7-point Likert scale of distress from 1 (not distressing at all) to 7 (extremely distressing). The sum of all PSIs and the sum of all NSIs were respectively calculated for each social relationship (i.e., Baby, Partner, Family Members, Friends, and Coworkers), across each day, and for each participant. The daily sum total of all PSIs and NSIs provided a total PSI score and a total NSI score. Please see Table 1 for presentation of discrete PSI and NSI items by social relationship category.
Table 1.
Descriptive statistics and variability estimates of PSIs and NSIs with baby, partner, family, friends and coworkers
| Positive social interaction event |
n (%) experienced event ≥ 1 time |
M (SD) days/week event happened |
M (SD) enjoyment rating (1–7 scale) |
|
|---|---|---|---|---|
| Baby PSIs | M (SD) = 18.93 (15.62) RMSSD (SD) = 7.55 (5.71) | |||
| Baby learned a new behavior | 39 (65%) | 1.05 (1.04) | 6.27 (1.41) | |
| Cuddled with baby | 60 (100%) | 6.92 (.43) | 6.53 (.57) | |
| Played with baby | 60 (100%) | 6.72 (.76) | 6.35 (.72) | |
| Dressed baby | 60 (100%) | 6.15 (1.15) | 5.62 (1.07) | |
| Bathed baby | 58 (96.67%) | 2.72 (1.73) | 5.65 (1.47) | |
| Had special bedtime with baby | 58 (96.67%) | 4.90 (2.10) | 5.68 (1.48) | |
| Partner PSIs | M (SD) = 6.75 (4.24) RMSSD (SD) = 3.54 (2.31) | |||
| Partner expressed love to you | 60 (100%) | 6.60 (.74) | 6.04 (.77) | |
| Received a gift from partner | 42 (70%) | 1.08 (1.09) | 5.86 (1.94) | |
| Celebrated special occasion with partner | 22 (36.66%) | .40 (.64) | 5.05 (2.36) | |
| Had a long conversation with partner | 58 (96.67%) | 3..07 (1.86) | 5.05 (2.36) | |
| Kissed or had intimate physical contact with partner | 60 (100%) | 5.65 (1.71) | 5.93 (.86) | |
| Family PSIs | M (SD) = .84 (.74) RMSSD (SD) = 1.37 (1.02) | |||
| Was praised by family member(s) | 38 (63.33%) | 2.71 (.30) | 4.98 (2.18) | |
| Was visited by family member(s) | 39 (65%) | 1.42 (1.55) | 4.74 (2.17) | |
| Spoke with family member(s) you haven’t spoken to in a long time | 28 (46.67%) | .58 (.81) | 4.61 (2.43) | |
| Family member(s) helped with a problem | 19 (31.67%) | .32 (.62) | 3.74 (2.85) | |
| Received gift from family member(s) | 28 (46.67%) | .43 (.65) | 4.32 (2.81) | |
| Family member(s) helped with childcare | 33 (55%) | .98 (1.41) | 4.68 (2.47) | |
| Friend PSIs | M (SD) = .92 (.73) RMSSD (SD) = 1.34 (.71) | |||
| Was complimented by friend(s) | 54 (90%) | 2.63 (1.82) | 5.82 (1.02) | |
| Went out with friend(s) | 42 (70%) | 1.25 (1.37) | 4.65 (2.51) | |
| Played a game with friend(s) | 7 (11.67%) | .12 (.37) | 4.00 (2.58) | |
| Went to a party with friend(s) | 44 (73.33%) | 1.17 (1.09) | 3.91 (2.63) | |
| Made new friend(s) | 20 (33.33%) | .71 (.10) | 4.15 (2.74) | |
| Coworker PSIs | M (SD) = .45 (.49) RMSSD (SD) = .70 (.60) | |||
| Was praised by coworkers | 24 (40.00%) | .50 (.77) | 4.52 (2.69) | |
| Coworker(s) helped you complete a project at work | 35 (58.33%) | 1.48 (1.71) | 5.41 (.91) | |
| Negative social interaction event |
n (%) experienced event ≥ 1 |
M (SD) days/week event happened |
M (SD) distress time rating (1–7 scale) |
|
|---|---|---|---|---|
| Baby NSIs | M (SD) = 3.84 (1.83) RMSSD (SD) = 2.67 (1.63) | |||
| Missed work or had to cancel plans because of baby | 22 (36.67%) | .52 (.96) | 3.74 (2.12) | |
| Had difficulty soothing baby | 53 (88.33%) | 2.00 (1.66) | 2.72 (1.59) | |
| Spent more time with baby than you had planned | 42 (70%) | 1.42 (1.41) | 5.11 (2.11) | |
| Responded to baby’s crying | 60 (100%) | 6.57 (.74) | 3.31 (1.60) | |
| Partner NSIs | M (SD) = .46 (.49) RMSSD (SD) = 1.08 (1.02) | |||
| Argued with partner | 25 (41.67%) | .58 (.83) | 1.97 (1.17) | |
| Was critical of partner | 38 (63.33%) | 1.13 (1.24) | 2.44 (1.23) | |
| Partner was critical of you | 39 (65%) | .77 (.93) | 1.61 (1.54) | |
| Partner was less affectionate than usual | 32 (53.33%) | .60 (.83) | 2.81 (1.57) | |
| Family NSIs | M (SD) = .02 (.07) RMSSD (SD) = .07 (.19) | |||
| Family member(s) criticized you | 2 (3.33%) | .05 (.29) | 2.75 (.35) | |
| Argued with family member(s) | 2 (3.33%) | .14 (.01) | 1.00 (.00) | |
| Saw family member(s) you didn’t want to see | 12 (20%) | .08 (.28) | 1.25 (1.91) | |
| Friend NSIs | M (SD) = .09 (.16) RMSSD (SD) = .25 (.39) | |||
| Did not hear from friend(s) you were expecting to hear from | 10 (16.67%) | .18 (.54) | 2.97 (2.14) | |
| Was criticized by friend(s) | 7 (11.67%) | .05 (.22) | 1.41 (2.00) | |
| Argued with friend(s) | 1 (1.67%) | .02 (.13) | 1.00 (.00) | |
| Encountered rude person(s) | 26 (43.33%) | .40 (.69) | 1.73 (1.65) | |
| Coworker NSIs | M (SD) = .07 (.17) RMSSD (SD) = .19 (.39) | |||
| Coworker(s) under your management failed you | 11 (18.33%) | .10 (.35) | .85 (1.29) | |
| Was criticized by coworker(s) | 16 (26.67%) | .43 (.02) | .94 (1.65) | |
| Your authority at work was decreased | 10 (16.67%) | .03 (.18) | .50 (1.08) | |
| Disagreed with coworker(s) | 17 (28.33%) | .25 (.82) | 1.51 (2.24) | |
Daily average descriptive statistics were calculated for each participant, for each variable, and then those individual values were averaged across the entire sample representing sample averages for the 7-day study period; M mean; SD standard deviation; RMSSD root mean squares of successive difference, an overall indicator of variability in the measure, higher values = greater variability. PSI items were rated by participants on a 7-point Likert scale of enjoyment from 1 (not enjoyable at all) to 7 (extremely enjoyable); NSI items were rated by participants on 7-point Likert scale of distress from 1 (not distressing at all) to 7 (extremely distressing)
Maternal Mood
Maternal mood was measured with composite daily Positive Affect (PA) and Negative Affect (NA) scores assessed in the Evening Diary with a modified form of the Profile of Mood States (POMS) (McNair, Lorr, & Droppleman, 1971). The original POMS is a 65-item wordlist that asks respondents to rate the degree to which an adjective describes their current mood state on a 5-point scale (1, not at all-5, extremely). The version of the POMS used for this study was shortened to 24 items from the original 65 based on previous daily diary research (Pressman et al., 2005; Usala & Hertzog, 1989). Participants were asked to rate how well each adjective described how they felt that day on a scale from 0 (not at all accurate) to 4 (extremely accurate). The PA composite score was derived from the mean of the following 13 adjectives: quiet, passive, happy, cheerful, relaxed, calm, active, lively, enthusiastic, trusting, helpful, attached, and loving. The NA composite score was derived from the mean of the following 11 items: jittery, nervous, unhappy, sad, drowsy, tired, intense, overwhelmed, stressed, bored, and lonely.
Sleep Quality
The Morning Sleep Diary (completed upon arising) collected information related to subjective sleep quality by asking participants to answer the following question, “On a scale from 1 to 7, where 1 is extremely poor and 7 is extremely good, how would you rate the quality of your sleep last night?” This question is similar to questions used to assess subjective sleep experience in longitudinal sleep research (King et al., 1997). We have previously reported on the objective sleep patterns and sleep duration estimates of this sample (Lillis et al., 2016).
Analytic strategy
Aggregated descriptive statistics were first conducted in order to examine frequencies of social interactions experienced during the day as well as generate overall averages for mood and sleep quality indices. In addition, Root Mean Squares of Successive Difference (RMSSD) values were calculated for all social interaction, mood, and sleep quality variables in order to generate an overall estimate of variability for each social interaction, mood, and sleep variable. Finally, bivariate correlations were conducted between baseline measures and aggregated means and RMSSD values of the daily diary social interaction, mood and sleep quality variables (see Table 1).
Given the nested nature of the data (i.e., repeated measures design) and the potential for variability to be present both at Level 1 (day-to-day, within person) and Level 2 (between persons), multilevel models were then used to investigate the longitudinal relationships between daytime social interactions, mood, and subjective sleep quality. Because Level 1 variables contain two sources of variance (differences between people and differences within person, across days), a “paired approach” was used for all Level 1 predictors in order to separate unique sources of variance (Affleck et al., 1999). Individual meancentered variables were created to represent a participant’s aggregated average score on a daily measure (which can be thought to reflect her “Average Day” on that particular measure). Within-person-deviation variables were then created to represent whether a participant’s score on a given day was higher or lower than her personal average for that measure (which can be thought to capture individual, day-to-day fluctuation in the measure). As such, pairs of individual meancentered and daily person-deviation variables were created for each Level 1 predictor variable used in analyses described below (i.e., Total Daily PSIs, Total Daily NSIs, Baby PSIs, Baby NSIs, Partner PSIs, Partner NSIs, Family PSIs, Family NSIs, Friend PSIs, Friend NSIs, Coworker PSIs, Coworker NSIs, and Sleep Quality).
Model Series #1
The first series of MLM analyses were performed on 60 Level 2 units (individual participants), each with 7 Level 1 units (7 days of observations per person). Model series #1 examined two separate equations, in which, fixed effects for individual-average and within-person deviation in Baby PSIs, Baby NSIs, Partner PSIs, Partner NSIs, Family PSIs, Family NSIs, Friend PSIs, Friend NSIs, Coworker PSIs, Coworker NSIs were regressed on Daily PA and then regressed on Daily NA.
Model Series #2 “Mood Reactivity”
Because sleep characteristics were always measured the morning after the collection of daily social interaction and mood variables, the resulting dataset for Model Series #2 included 60 Level 2 units, each with six Level 1 units (6 days of observations per person). Model series #2 examined our “Mood Reactivity” hypotheses with two separate equations, in which, fixed effects for individual-average and within-person deviation in “Todays” daily PSIs and NSIs, individual average and “Last Night’s”, within-person deviation in sleep quality, and an interaction between within-person deviation in total NSIs and Last Night’s, within-person deviation in sleep quality were regressed on “Today’s” PA and then regressed on “Today’s” NA.
Model Series #3 “Mood Recovery”
As noted above, because sleep characteristics were always measured the morning after the collection of daily social interaction and mood variables, the resulting dataset for Model Series #3 included 60 Level 2 units, each with six Level 1 units (6 days of observations per person). Model series #3 examined our “Mood Recovery” hypotheses with two separate equations, in which, fixed effects for individualaverage and within-person deviation in “Today’s” NSIs and “Tonight’s” sleep quality and an interaction between within-person deviation in “Today’s” NSIs and within- person deviation in “Tonight’s” sleep quality were regressed on “Tomorrow’s” PA and then regressed on “Tomorrow’s” NA. All the aforementioned models were estimated with SPSS software (IBM Corp, 2013) using an autoregressive (AR1) covariance structure and included a fixed and random intercept.
Missing Data
Participants completed nearly all Evening Diary items across all days of participation resulting in very low missing daily data. Randomly skipped items that factored into a total daily score were mean replaced (< .01% of all cases). No sleep quality ratings were missing from the Morning Sleep Diary.
Results
Descriptive results
Table 1 presents aggregated descriptive statistics and RMSSD values for PSIs and NSIs (as well as information on the frequencies and valences of specific types of PSI and NSI events for each social relationship category). With respect to daily PA and NA, participants had higher average daily PA (M = 2.05, SD = .52) than NA (M = .84, SD = .42). In addition, RMSSD values for daily PA and NA indicated that mood was generally stable in the sample during the study week. In regards to sleep quality, participants’ sleep quality was moderately variable (RMSSD = 1.49, SD = .64) and, on average, rated as a 4.55 (SD = .83) on a 1–7 scale (where 1 was extremely poor and 7 was extremely good).
In terms of daytime social interactions, participants reported about seven times as many PSIs than NSIs (M PSI = 36.99, SD = 19.27; M NSI = 5.90, SD = 2.13). Baby-related PSIs accounted for, on average, > 50% of all PSIs experienced during an average day and although NSIs were generally infrequent across partner, family, friend and coworker interactions, on average, the majority of total daily NSIs (> 78%) also arose from interactions with baby. In terms of overall variability of PSIs and NSIs, total daily PSIs were more variable (RMSSD = 10.28, SD = 5.82) than total daily NSIs (RMSSD = 3.38, SD = 1.83), which may similarly be explained by the high variability in PSIs with baby (RMSSD = 7.55, SD = 5.71) when compared to RMSSD estimates from other social relationship categories.
Multilevel model results
Model Series #1
Table 2 presents findings from concurrent multilevel models’ associations of total Daily PSIs and NSIs (individual averages and within-person deviations) by social relationship category regressed on Daily PA and NA. Significant individual-average effects were found for Daily PA, such that, higher individual-average numbers of Friend PSIs (B = .248, SE = .079) and lower individual-average numbers of Baby NSIs (B = −.071, SE = .033) were associated with higher Daily PA. In addition, significant within-person effects in social interactions were found for Daily PA, such that on days when participants had higher numbers of Partner PSIs (B = .014, SE = .005) and lower numbers of Partner NSIs (B = −.032, SE = .016), Family NSIs (B = - .403, SE = .121), and Coworker NSIs (B = − .174, SE = .055), their daily PA scores were higher (allp’s < .05).
Table 2.
Concurrent multilevel model associations of individual-average and within-person deviation in total daily PSIs and NSIs by social relationship category on daily positive affect and negative affect
| Model series #1 | Daily positive affect |
Daily negative affect |
||
|---|---|---|---|---|
| B | SE | B | SE | |
|
Fixed effects PSIs | ||||
| Intercept | 1.96** | .21 | .744** | .180 |
| Baby PSIs avg. | .005 | .004 | − .003 | .003 |
| Baby PSIs deviation | .003 | .003 | − .007** | .002 |
| Partner PSIs avg. | .015 | .016 | − .012 | .014 |
| Partner PSIs deviation | .014** | .005 | − .012** | .005 |
| Family PSIs avg. | .089 | .083 | − .022 | .072 |
| Family PSIs deviation | .023 | .014 | − .009 | .013 |
| Friend PSIs avg. | .248** | .079 | − .109 | .068 |
| Friend PSIs deviation | .022 | .016 | − .019 | .015 |
| Coworker PSIs avg. | − .111 | .122 | .021 | .106 |
| Coworker PSIs deviation | − .045 | .027 | .073** | .026 |
| NSIs | ||||
| Baby NSIs avg. | − .071* | .033 | .052 | .029 |
| Baby NSIs deviation | − .001 | .008 | .017* | .008 |
| Partner NSIs avg. | − .161 | .116 | .246* | .101 |
| Partner NSIs deviation | − .032* | .016 | .015 | .016 |
| Family NSIs avg. | .541 | .898 | .763 | .784 |
| Family NSIs deviation | − .403** | .121 | .374** | .116 |
| Friend NSIs avg. | − .311 | .360 | .168 | .315 |
| Friend NSIs deviation | − .071 | .054 | .039 | .052 |
| Coworker NSIs Avg. | .061 | .345 | − .114 | .301 |
| Coworker NSIs Deviation | − .174** | .055 | .119* | .053 |
| Random effects | ||||
| Intercept (Subject) | .131** | .032 | .099** | .024 |
Significant fixed-effects bolded and denoted with
when p = < .05 and
when p = < .01. Variables denoted with “Avg” are person-mean lefted and can be thought to reflect between-person differences in the variable or a participant’s “Average Day” on that variable. Variables denoted with “Deviation” represent within-person differences in the variable and can be thought to reflect a participant’s day-to-day fluctuation in the variable
In regards to Daily NA, the only significant individual-average effect found was for Partner NSIs, such that participants with higher average levels of Partner NSIs (B = .246, SE = 101) had significantly higher average levels of Daily NA. In regards to within-person deviation effects, a number of significant associations with Daily NA were observed. Specifically, on days when participants had lower numbers of Baby PSIs (B = −.007, SE = .002) and Partner PSIs (B = − .012, SE = .005) and higher numbers of Coworker PSIs (B = .073, SE = .026), Baby NSIs (B = .017, SE = .008), Family NSIs (B = .374, SE = .116), and Coworker NSIs (B = .119, SE = .053), their Daily NA scores were higher (all p’s < .05).
Model Series #2”Mood Reactivity” Main Effects for Daily PA
Table 3 presents findings from concurrent multilevel models’ associations of individual-average and within-person deviation in total Daily PSIs and NSIs, individual-average sleep quality as well as “last-night’s sleep quality” (meaning last night’s Sleep Quality deviation score), and an interaction between within-person deviation in NSIs with “Last Night’s sleep quality” regressed on Daily PA and NA. Higher individual-average levels of total Daily PSIs (B = .008, SE = .003) and sleep quality (B = .251, SE = .072) and lower individual-average levels of total Daily NSIs (B = - .083, SE = .027) were significantly associated with higher Daily PA. In addition, on days when participants had more PSIs than normal (B = .008, SE = .003), their Daily PA scores were higher. Similarly, on nights when participants had higher sleep quality than normal (B = .044, SE = .016), their PA scores were higher (allp’s < .05). Within-person deviation in NSIs and the interaction between within-person deviation in NSIs and “Last Night’s” within-person deviation in sleep quality on Daily PA were not significant (p > .05).
Table 3.
Multilevel models’ associations of individual-average and within-person deviation in daytime PSIs, NSIs, and Sleep quality on daytime positive affect and negative affect
| Model series #2 | ||||
|---|---|---|---|---|
| “Mood reactivity” | Positive affect “Today” |
Negative affect “Today” |
||
| B | SE | B | SE | |
| Fixed effects | ||||
| Intercept | 1.20** | .360 | 1.82** | .261 |
| Total daily PSIs avg. | .008** | .003 | − .004 | .002 |
| “Today’s” daily PSIs deviation | .008** | .002 | − .009** | .002 |
| Total daily NSIs avg. | − .083** | .027 | .060** | .020 |
| “Today’s” daily NSIs deviation | − .013 | .007 | .014* | .007 |
| Sleep quality avg. | .209** | .069 | − .248** | .052 |
| “Last Night’s” sleep quality deviation | .044** | .016 | − .045** | .016 |
| “Last Night’s” SQ Dev × daily NSIs dev | .011 | .006 | − .013* | .006 |
| Random effects | ||||
| Intercept (subject) | .127* | .037 | .069* | .023 |
| Model series #3 | ||||
|---|---|---|---|---|
| “Mood recovery” | Positive affect “Tomorrow” |
Negative affect “Tomorrow” |
||
| B | SE | B | SE | |
| Fixed effects | ||||
| Intercept | 1.22** | .364 | 1.81** | .282 |
| Total daily PSIs avg. | .008** | .003 | − .004 | .002 |
| “Today’s” PSIs deviation | .001 | .002 | .001 | .002 |
| Total daily NSIs Avg. | − .079* | .027 | .058** | .021 |
| “Today’s” NSIs deviation | .013 | .007 | − .019** | .007 |
| Sleep quality avg. | .201** | .069 | − .243** | .054 |
| “Tonight’s” sleep quality deviation | .049** | .016 | − .054** | .016 |
| SQ dev x daily NSIs dev | .019** | .006 | − .015** | .006 |
| Random effects Intercept (subject) | .140* | .042 | .070* | .023 |
Significant fixed-effects bolded and denoted with
when p = < .05 and
when p = < .01. Variables denoted with “Avg” are Person-Mean centered and can be thought to reflect between-person differences in the variable or a participant’s “Average Day” on that variable. Variables denoted with “Deviation” represent within-person differences in the variable and can be thought to reflect a participant’s day-to-day fluctuation in the variable
Model Series #2”Mood Reactivity” Main Effects for Daily NA
In regards to Daily NA, no significant individual-average effects were observed for total Daily PSIs, however, higher individual-average levels of NSIs (B = .060, SE = .020) were related to higher Daily NA. On days when participants had lower than average numbers of PSIs (B = − .009, SE = .002) and higher than average numbers of NSIs (B = .014, SE = .007), their NA was higher. In regards to effects of sleep quality, higher individual-average levels of sleep quality (B = − .248, SE = .052) were significantly associated with lower levels of Daily NA. In addition, on nights when participants had lower than average levels of sleep quality (B = − .045, SE = .016), their NA scores were higher.
Model Series #2”Mood Reactivity” Interaction Effects for Daily NA
A significant interaction was observed between within-person deviation in total Daily NSIs and “Last Night’s” within-person deviation in sleep quality on Daily NA (B = − .013, SE = .006). This finding suggests that within-person deviations in sleep quality moderated the relationship between within-person deviations in total Daily NSIs on Daily NA (for a visual representation of this interaction, please refer to Fig. 1). When plotting and probing interaction effects, one should consider both the significance and magnitude of the relationship between y (Daily NA) and x (within-person deviation in NSIs) at different conditional values of z (“Last Night’s,” within-person deviation in sleep quality) (Preacher et al., 2006).
Fig. 1.
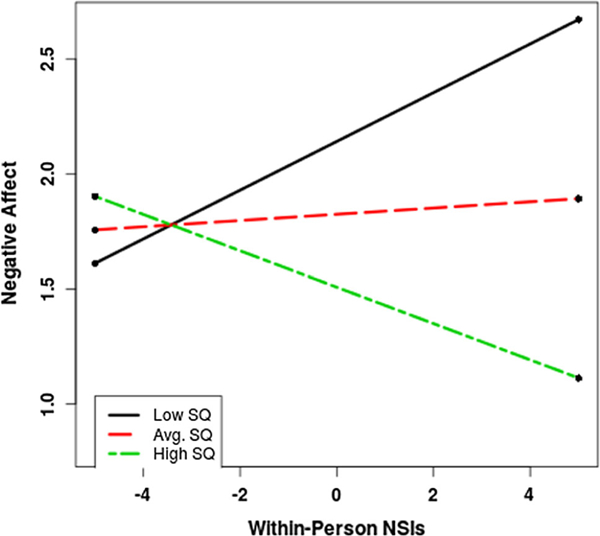
Interaction between “Last Night’s” within-person deviation in sleep quality and within-person deviation in total negative social interactions on daytime negative affect
The simple slopes for high and low conditional values of “Last Night’s” within-person deviation in sleep quality were significant. Specifically, on nights when participants had higher than their average level of sleep quality (B = − .079 SE = .013), the effect of higher within-person deviation in total Daily NSIs on NA was attenuated (i.e., daily NA was lower). Similarly, on nights when participants had lower than their average level of sleep quality (B = 0.106, SE = .013), the effect of higher within-person deviation in total Daily NSIs on NA was exacerbated (i.e., daily NA was higher). The region of significance calculated for this interaction indicated that values of “Last Night’s” within-person deviation in sleep quality, falling between .651 and 1.57, render the interaction nonsignificant and values outside this region render the interaction significant. Therefore, in this sample, a significant interaction existed if daily within-person deviation in sleep quality ratings exceeded 1.57 or were less than .651, (all p’s < .05).
Model Series #3 “Mood Recovery” Main Effects for Daily PA
Table 3 also presents findings from concurrent multilevel models’ associations of individual-average and within-person deviation in total Daily PSIs, NSIs, sleep quality, and an interaction between within-person deviation in NSIs with within-person deviation in sleep quality regressed on “Tomorrow’s” Daily PA and NA. After controlling for individual differences in the average relationship between NSIs, PSIs, Sleep Quality on PA, there were no significant effects for within-person deviations in PSIs or NSIs today on PA tomorrow. However, on nights when participants had higher sleep quality than normal (B = .049, SE = .016, “Tomorrow’s” PA scores were higher (all p’s < .05).
Model Series #3 “Mood Recovery” Interaction Effects for Daily PA.
A significant interaction was observed between within-person deviation in NSIs and within-person deviation in sleep quality on “Tomorrow’s” PA (B = .019, SE = .006; see Fig. 2). The simple slopes for high and low conditional values of within-person deviation in sleep quality on “Tomorrow’s” PA were significant. Specifically, higher than average levels of sleep quality (B = .149, SE = .014) buffered the effect of higher than average levels of NSIs on “Tomorrow’s” PA (i.e., PA was higher). Similarly, lower than average levels of sleep quality (B = − .124, SE = .014) exacerbated the effect of higher than average levels of NSIs on “Tomorrow’s” PA (i.e., PA was lower). The region of significance calculated for this interaction indicated that values of within-person deviation in sleep quality falling between − .954 and − .429 render the interaction nonsignificant and values outside this region render the interaction significant.
Fig. 2.
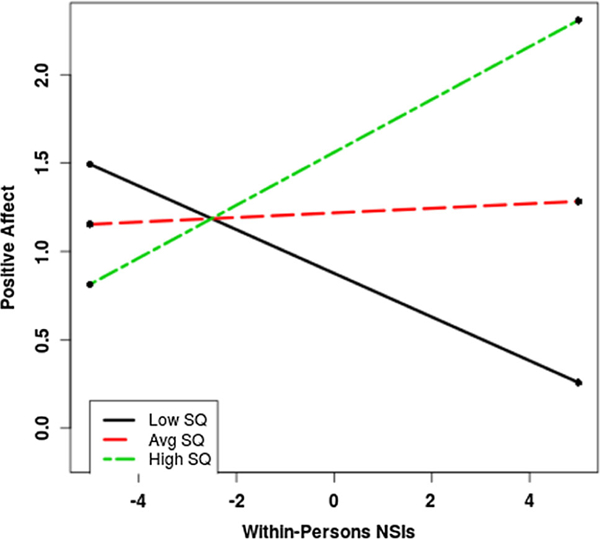
Interaction between within-person deviation in sleep quality and within-person deviation in total negative social interactions on “Tomorrow’s” positive affect
Model Series #3 “Mood Recovery” Main Effects for Daily NA.
In regards to Daily NA, after controlling for individual differences in the relationship of NSIs, PSIs, and Sleep Quality on NA, there were no significant within-person deviation effects for PSIs or NSIs on Daily NA. However, on nights when sleep quality was lower than normal (B = − .054, SE = .016), “Tomorrow’s” NA scores were higher.
Model Series #3 “Mood Recovery” Interaction Effects for Daily NA.
Finally, a significant interaction was observed between within-person deviation in total Daily NSIs and within-person deviation in sleep quality on Daily NA (B = − .015, SE = .006; see Fig. 3). The simple slopes for high and low conditional values of within-person deviation in sleep quality were significant. Specifically, on nights when participants had higher than their average level of sleep quality (B = − .125, SE = .013), the effect of higher within-person deviation in NSIs on “Tomorrow’s” NA was ameliorated (i.e., “Tomorrow’s” NA was lower). Similarly, on nights when participants had lower than their average level of sleep quality (B = .086, SE = .013), the effect of higher within-person deviation in NSIs on “Tomorrow’s” NA was exacerbated (i.e., “Tomorrow’s” NA was higher). The region of significance calculated for this interaction indicated that values of within-person deviation in sleep quality, falling between − 1.77 and − .954, render the interaction nonsignificant and values outside this region render the interaction significant.
Fig. 3.
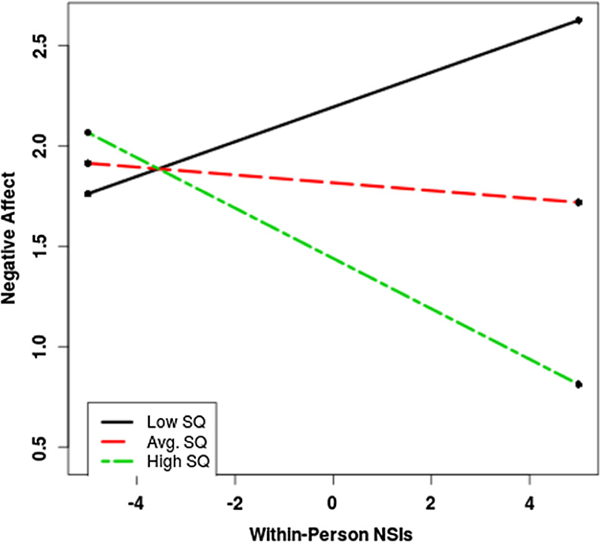
Interaction between within-person deviation in sleep quality and within-person deviation in total negative social Interactions on “Tomorrow’s” negative affect
Discussion
Findings from the current study highlight the dynamic interplay between sleep and social interactions on maternal mood in the postpartum period. To our knowledge, this is the first study to include PSIs and social interactions with baby in a daily diary of social relationships. In addition, our results are the first to demonstrate the role that maternal sleep quality plays in social discord-related mood reactivity and mood recovery processes in the 3–6 month postpartum period. Specifically, we found that high quality sleep buffered the effects of having a “bad day” (i.e., higher than average NSIs) on mood and also prevented the effects of having a bad day from carrying over from one day’s mood to the next. These results are consistent with previous studies examining the role of adequate sleep in mood regulation (Hamilton et al., 2007, 2008) as well as the literature on the bidirectional relationship between sleep and social interactions (Meijer & van den Wittenboer, 2007; Troxel, 2010; Troxel, et al., 2007).
It is important that the results of this study be included in the broader context of the postpartum period. The objective and subjective sleep patterns of this sample have been previously reported on (Lillis, 2014; Lillis et al., 2016). Although objective sleep patterns were not significantly related to maternal mood (Lillis, 2014), they did appear to differ as function of maternal work status, daytime health behaviors, and infant care choices (Lillis et al., 2016). For the sample overall, objective estimates of sleep duration were in the “normal range” for healthy adults (i.e., M = 7.2 h), which is consistent with other reports of objective sleep duration in the 3–6 month postpartum period (Montgomery-Downs et al., 2010; Dørheim et al., 2009). However, mothers in our sample who did not work outside the home were found to have longer objective sleep durations as well as longer sleep onset latencies (SOL). In addition, sleep continuity, as measured by self-reported arousals and objectively measured wake time after sleep onset (WASO), was worse for breastfeeding mothers and those who room-shared or co-slept with their babies at night. Mothers appeared to cope with the sleep disturbance in expected ways, including with napping and exercise. However, mothers who tended to nap more frequently or for longer durations had longer SOL. In contrast, mothers who exercised more frequently or for longer durations had longer nighttime sleep durations. It is noteworthy that these differences in maternal work status, daytime health behaviors, and infant care choices had minimal impact on sleep quality. In fact, the only negative predictor of sleep quality was sleeping in the same room as baby (i.e., sharing the room or bed with the infant).
Although our previous work showed that the impact of biopsychosocial predictors on sleep quality was minimal, the current study showed that the effect of sleep quality on psychosocial health was substantial. Consistent with studies of women with chronic pain (Hamilton et al., 2007, 2008), maternal sleep quality in the current study was a consistent predictor of emotional health and also affected the emotional impact of, and the ability to recover from, particularly bad days. As women transition from the intensive baby-care demands of the first 3 months post-partum to the more diffuse demands in the 3–6 month period and beyond, (which, for some women, includes returning to work and, for all women, a greater degree of engagement with the outside world), adequate sleep may serve as an important resource for when those social interactions do not go smoothly.
The importance of social interactions in the 3–6 month postpartum period was illustrated by the life-event measure used in this study. Consistent with previous daily life events research (Seidlitz & Diener, 1993; Zautra & Reich, 1983), we found that PSIs were more frequently reported than NSIs and consistently associated with more stable and positive mood states. This is one of the few studies to use a daily diary approach to characterize daily social interactions during the postpartum period and the only one to measure baby-related interactions. After examining the data, it is hard to overstate the importance of including baby-related social interactions in the measurement of the postpartum social milieu. Baby PSIs were the most frequent social interaction reported by our sample and cuddling and playing with baby were the most frequent and the most positively rated interactions of all PSIs. In addition, although participants frequently reported intimate contact with and expressions of love from their partners, these PSIs were rated, on average, less positively than the aforementioned PSIs with baby. Interestingly, the most frequent and the most strongly negatively rated NSIs were also with baby. This result may suggest an area of duality in the 3–6 month postpartum period; namely, that interactions with baby are both the most positive and the most negative of all social network members.
The good news for these new mothers was that the relationship of NSIs to mood was tempered by sleep quality. In other words, mothers appeared better able to cope with a bad day that could have included a fussy baby if they had good quality sleep the night before. Moreover, following a good night’s sleep, the effects of a bad day did not appear to carry over from one day to the next. Viewed another way, these data may help to explain the relationship of maternal sleep to postpartum depression. Poor quality sleep may heighten reactivity to NSIs (i.e., mood reactivity) and prevent recovery from a bad day (i.e., mood recovery). In the context of the mother-infant dyad, a difficult infant temperament combined with poor maternal sleep could easily form an entrenched positive feedback loop, with infant crying during the night disrupting mother’s sleep, leading to higher maternal negative affect during the day and greater difficulty coping with negative infant social interactions.
Our study also adds to the literature on impact of non-kin relationships in the postpartum. Although previous studies have found that interaction with kin members tends to increase after the birth of a child (Belsky & Rovine, 1984; Bost et al., 2002; Flaherty & Richman, 1989; Gameiro et al., 2010; Hammer et al., 1982; McCannell, 1987) and interactions with friends or other non-kin related adults tends to decrease (Bost et al., 2002; Hammer et al., 1982; McCannell, 1987; Stueve & Gerson, 1977), for mothers in our study, friend-related interactions were more common than family-related interactions and had a stronger up-side. Mothers in our sample rated the majority of PSIs with friends more favorably than PSIs with family and friend-related interactions were also found to be significant predictors of mood even after controlling for other relationship category interactions.
These novel findings related to non-kin social activity may be explained, in part, by the fact that most existing postpartum social relationship research is conducted within the first 3 months, when the impact of partner and family support might be more readily needed and provided. Although there is a fair amount of literature documenting the importance of general and partner-specific social support, there is almost no literature on the impact of adult-friendships during the postpartum period. In the absence of a literature base, anecdotal reports and the proliferation of support groups for new mothers (e.g., mommy and me classes, La Leche group meeting, mother-focused social media groups), suggest that new mothers benefit from friendships with other women during the postpartum period (Scott et al., 2001). Moreover, friendship support may have some distinct advantages over family support or partner support, in that, friendships may be less fraught with emotional baggage than family relationships (Coyne et al.1988), and friends often have the advantage of proximity whereas family members may live in distant states or other countries.
The current study should be evaluated in terms of its strengths and limitations. Although our use of daily diaries allowed us to examine within-person changes in sleep and social interactions, a week-long study still only provides a snapshot of the 3–6 month postpartum period. In addition, all of our data were collected through self-report, a methodology that has known biases and limitations. Future iterations of our study could be strengthened by adding other kinds of measurement modalities, including the collection of collateral information on sleep and social relationships in the 3–6 month postpartum period from coparenting partners. Further, although our sample was compliant with our study protocol resulting in very low missing data, they were also homogenous in terms of their ethnoracial makeup and socioeconomic status. As such, our results may not represent the postpartum experiences of more ethnoracially and economically diverse samples of women.
In summary, the results of the current study paint a picture of the 3–6 month postpartum period in which sleep and social relationships exert a substantial effect on maternal emotional health. For the women in our study, postpartum social relationships had both positive and negative effects on mood. These results suggest that interventions to improve psychosocial functioning during the 3–6 month postpartum period would do well to focus on improving sleep quality. Although the women in this study did not show evidence of symptoms of insomnia, behavioral interventions to increase sleep consolidation and reduce sleep onset latency might improve perceptions of sleep quality and, ultimately, mood. Although we cannot make definitive causal statements from passive correlational data, the findings of this study may nevertheless highlight high quality sleep as an intrapersonal resource that can enhance mood recovery or buffer mood reactivity amidst the daily social demands of new motherhood.
Acknowledgments
Funding Support for the study was provided by the University of Kansas General Research Fund, and NIH T32 035165 (MSZ).
Footnotes
Compliance with ethical standards
Human and animal rights and Informed consent This article does not contain any studies with animals performed by any of the authors. All procedures performed in studies involving human participants were in accordance with ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.Informed consent was obtained from all individual participants included in the study.
Conflict of interest Teresa A. Lillis, Nancy A. Hamilton, Sarah D. Pressman, Maisa S. Ziadni, Christina S. Khou, Lauren E. Boddy and Linzy M. Wagner declare that they have any conflicts to disclose.
References
- Affleck G, Zautra A, Tennen H, & Armeli S (1999). Multilevel daily process designs for consulting and clinical psychology: A preface for the perplexed. Journal of Consulting and Clinical Psychology, 67, 746. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Barclay L, Everitt L, Rogan F, Schmied V, & Wyllie A (1997). Becoming a mother—An analysis of women’s experience of early motherhood. Journal of Advanced Nursing, 25, 719–728. [DOI] [PubMed] [Google Scholar]
- Bayer JK, Hiscock H, Hampton A, & Wake M (2007). Sleep problems in young infants and maternal mental and physical health. Journal of Paediatrics and Child Health, 43, 66–73. [DOI] [PubMed] [Google Scholar]
- Bei B, Coo S, & Trinder J (2015). Sleep and mood during pregnancy and the postpartum period. Sleep Medicine Clinics,10,25–33. [DOI] [PubMed] [Google Scholar]
- Belsky J, & Rovine M (1984). Social-network contact, family support, and the transition to parenthood. Journal of Marriage and the Family, 46, 7. [Google Scholar]
- Belsky J, Ward MJ, & Rovine M (1986). Prenatal expectations, postnatal experiences, and the transition to parenthood In Brodzinsky DM (Ed.), Thinking about the family: Views of parents and children (pp. 119–145). New York, NY: Psychology Press. [Google Scholar]
- Bost K, Cox M, & Payne C (2002). Structural and supportive changes in couples’ family and friendship networks across the transition to parenthood. Journal of Marriage and the Family, 64, 14. [Google Scholar]
- Boyce P, & Hickey A (2005). Psychosocial risk factors to major depression after childbirth. Social Psychiatry and Psychiatric Epidemiology, 40, 605–612. [DOI] [PubMed] [Google Scholar]
- Brown SL, Nesse RM, Vinokur AD, & Smith DM (2003). Providing social support may be more beneficial than receiving it: Results from a prospective study of mortality. Psychological Science, 14, 320–327. [DOI] [PubMed] [Google Scholar]
- Burke L (2003). The impact of maternal depression on familial relationships. International Review of Psychiatry, 15, 243–255. [DOI] [PubMed] [Google Scholar]
- Burman B, & Margolin G (1992). Analysis of the association between marital relationships and health problems: An interactional perspective. Psychological Bulletin, 112, 39–63. [DOI] [PubMed] [Google Scholar]
- Cohen S, & Hoberman HM (1983). Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology, 13, 99–125. [Google Scholar]
- Coyne JC, & DeLongis A (1986). Going beyond social support: The role of social relationships in adaptation. Journal of Consulting and Clinical Psychology, 54, 454–460. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Wortman CB, & Lehman DR (1988). The other side of support: Emotional over involvement and miscarried helping In Gottlieb BH (Ed.), Marshaling social support: Formats, processes, and effects (pp. 305–330). Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- Dennis CL, & Ross L (2005). Relationships among infant sleep patterns, maternal fatigue, and development of depressive symptomatology. Birth, 32, 187–193. [DOI] [PubMed] [Google Scholar]
- Dørheim SK, Bondevik GT, Eberhard-Gran M, & Bjorvatn B (2009). Sleep and depression in postpartum women: A population-based study. Sleep, 32, 847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estrela C, Barker ET, Lantagne S, & Gouin JP (2017). Chronic parenting stress and mood reactivity: The role of sleep quality. Stress and Health, 34, 296–305. [DOI] [PubMed] [Google Scholar]
- Figueiredo B, Dias CC, Pinto TM, & Field T (2016). Infant sleep-wake behaviors at two weeks, three and six months. Infant Behavior and Development, 44, 169–178. [DOI] [PubMed] [Google Scholar]
- Fincham FD (2003). Marital conflict: Correlates, structure, and context. Current Directions in Psychological Science, 12, 23–27. [Google Scholar]
- Flaherty J, & Richman J (1989). Gender differences in the perception and utilization of social support: Theoretical perspectives and an empirical test. Social Science and Medicine, 28, 1221–1228. [DOI] [PubMed] [Google Scholar]
- Fowden AL, Giussani DA, & Forhead AJ (2006). Intrauterine programming of physiological systems: Causes and consequences. Physiology, 21, 29–37. [DOI] [PubMed] [Google Scholar]
- Gameiro S, Boivin J, Canavarro MC, Moura-Ramos M, & Soares I (2010). Social nesting: Changes in social network and support across the transition to parenthood in couples that conceived spontaneously or through assisted reproductive technologies. Journal of Family Psychology, 24, 175–187. [DOI] [PubMed] [Google Scholar]
- Germ W, Milner DV, Chawla S, & Pickering TG (1995). Social support as a moderator of cardiovascular reactivity in women: A test of the direct effects and buffering hypotheses. Psychosomatic Medicine, 57, 16–22. [DOI] [PubMed] [Google Scholar]
- Gicquel C, El-Osta A, & Le Bouc Y (2008). Epigenetic regulation and fetal programming. Best Practice and Research Clinical Endocrinology and Metabolism, 22, 1–16. [DOI] [PubMed] [Google Scholar]
- Goyal D, Gay C, & Lee K (2009). Fragmented maternal sleep is more strongly correlated with depressive symptoms than infant temperament at three months postpartum. Archives of Women’s Mental Health, 12, 229–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall WA (1992). Comparison of the experience of women and men in dual-earner families following the birth of their first infant. Image The Journal of Nursing Scholarship, 24, 33–38. [DOI] [PubMed] [Google Scholar]
- Hamilton NA, Affleck G, Tennen H, Karlson C, Luxton D, Preacher KJ, et al. (2008). Fibromyalgia: The role of sleep in affect and in negative event reactivity and recovery. Health Psychology, 27, 490. [DOI] [PubMed] [Google Scholar]
- Hamilton NA, Catley D, & Karlson C (2007). Sleep and the affective response to stress and pain. Health Psychology, 26, 288. [DOI] [PubMed] [Google Scholar]
- Hammer M (1983). “Core” and “extended” social networks in relation to health and illness. Social Science and Medicine, 17, 405–411. [DOI] [PubMed] [Google Scholar]
- Hammer M, Gutwirth L, & Phillips SL (1982). Parenthood and social networks. A preliminary view. Social Science and Medicine, 16, 2091–2100. [DOI] [PubMed] [Google Scholar]
- Hiscock H, & Wake M (2001). Infant sleep problems and postnatal depression: A community-based study. Pediatrics, 107, 1317–1322. [DOI] [PubMed] [Google Scholar]
- IBM Corp. (2013). IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. [Google Scholar]
- King AC, Oman RF, Brassington GS, Bliwise DL, & Haskell WL (1997). Moderate-intensity exercise and self-rated quality of sleep in older adults: A randomized controlled trial. Jama, 277(1), 32–37. [PubMed] [Google Scholar]
- Kuh D, & Ben-Shlomo Y (2004). A life course approach to chronic disease epidemiology (Vol. 2). Oxford: Oxford University Press. [PubMed] [Google Scholar]
- Lawson A, Murphy KE, Sloan E, Uleryk E, & Dalfen A(2015). The relationship between sleep and postpartum mental disorders: A systematic review. Journal of Affective Disorders, 176, 65–77. [DOI] [PubMed] [Google Scholar]
- Le Masters EE (1959). Parenthood as a crisis. Marriage and Family Living, 19, 352–355. [Google Scholar]
- Lev Ari L, & Shulman S (2012). Pathways of sleep, affect, and stress constellations during the first year of college: Transition difficulties of emerging adults. Journal of Youth Studies, 15, 273–292. [Google Scholar]
- Lillis TA (2014). Project MSSE: Maternal sleep and social environment in the short-term postpartum. Unpublished Doctoral Dissertation. University of Kansas, Lawrence KS. [Google Scholar]
- Lillis TA, Hamilton NA, Pressman SD, & Khou CS (2016). The association of daytime maternal napping and exercise with nighttime sleep in first-time mothers between 3 and 6 months postpartum. Behavioral Sleep Medicine. 10.1080/15402002.2016.1239580 [DOI] [PubMed] [Google Scholar]
- Majewski J (1987). Social support and the transition to the maternal role. Health Care for Women International, 8, 397–407. [DOI] [PubMed] [Google Scholar]
- Maxson PJ, Edwards SE, Valentiner EM, & Miranda ML(2016). A multidimensional approach to characterizing psychosocial health during pregnancy. Maternal and Child Health Journal, 20, 1103–1113. [DOI] [PubMed] [Google Scholar]
- McBridge A, & Shore C (2001). Women as mothers and grandmothers. Annual Review of Nursing Research, 19, 22. [PubMed] [Google Scholar]
- McCannell K (1987). Social networks and the transition to motherhood In Milardo R (Ed.), Families and Social Networks. Beverly Hills: Sage. [Google Scholar]
- McNair DM, Lorr M, & Droppleman LF (1971). Manual for the profile of mood states (POMS). San Diego: Educational and Industrial Testing Service. [Google Scholar]
- Meijer A, & van den Wittenboer G (2007). Contribution of infants’ sleep and crying to marital relationship of first-time parent couples in the 1st year after childbirth. Journal of Family Psychology, 21, 49–57. [DOI] [PubMed] [Google Scholar]
- Montague DPF, & Walker-Andrews AS (2002). Mothers, fathers, and infants: The role of person familiarity and parental involvement in infants’ perception of emotion expressions. Child Development, 73, 1339–1352. [DOI] [PubMed] [Google Scholar]
- Montgomery-Downs HE, Insana SP, Clegg-Kraynok MM, & Mancini LM (2010). Normative longitudinal maternal sleep: The first 4 postpartum months. American Journal of Obstetrics and Gynecology, 203, 465–e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrell J, & Steele H (2003). The role of attachment security, temperament, maternal perception, and care-giving behavior in persistent infant sleeping problems. Infant Mental Health Journal, 24, 447–468. [Google Scholar]
- Nystrom K, & Ohrling K (2004). Parenthood experiences during the child’s first year: Literature review. Journal of Advanced Nursing, 46, 319–330. [DOI] [PubMed] [Google Scholar]
- Page M, & Wilhelm MS (2007). Postpartum daily stress, relationship quality, and depressive symptoms. Contemporary Family Therapy, 29, 237–251. [Google Scholar]
- Park EM, Meltzer-Brody S, & Stickgold R (2013). Poor sleep maintenance and subjective sleep quality are associated with postpartum maternal depression symptom severity. Archives of Women’s Mental Health, 16, 539–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power T, & Parke R (1984). Social network factors and the transition to parenthood. Sex-Roles, 10, 23. [Google Scholar]
- Preacher KJ, Curran PJ, & Bauer DJ (2006). Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31, 437–448. [Google Scholar]
- Pressman SD, Cohen S, Miller GE, Barkin A, Rabin BS, & Treanor JJ (2005). Loneliness, social network size, and immune response to influenza vaccination in college freshmen. Health Psychology, 24, 297–306. [DOI] [PubMed] [Google Scholar]
- Qualtrics software. (2018). Copyright©. Qualtrics. Qualtrics and all other Qualtrics product or service names are registered trademarks or trademarks of Qualtrics, Provo, UT, USA. https://www.qualtrics.com. Accessed 4 Sept 2018.
- Reid KM, & Taylor MG (2015). Social support, stress, and maternal postpartum depression: A comparison of supportive relationships. Social Science Research, 54, 246–262. [DOI] [PubMed] [Google Scholar]
- Revenson TA (1994). Social support and marital coping with chronic illness. Annals of Behavioral Medicine, 16, 122–130. [Google Scholar]
- Robles TF, & Kiecolt-Glaser JK (2003). The physiology of marriage: Pathways to health. Physiology and Behavior, 79, 409–416. [DOI] [PubMed] [Google Scholar]
- Ross LE, Sellers EM, Gilbert Evans SE, & Romach MK (2004). Mood changes during pregnancy and the postpartum period: Development of a biopsychosocial model. Acta Psychi-atra Scandinavica, 109, 457–466. [DOI] [PubMed] [Google Scholar]
- Schwab-Reese LM, Schafer EJ, & Ashida S (2017). Associations of social support and stress with postpartum maternal mental health symptoms: Main effects, moderation, and mediation. Women and Health, 57, 723–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott D, Brady S, & Glynn P (2001). New mother groups as a social network intervention: consumer and maternal and child health nurse perspectives. The Australian Journal of Advanced Nursing: A Quarterly Publication of the Royal Australian Nursing Federation, 18, 23–29. [PubMed] [Google Scholar]
- Seeman TE, Kaplan GA, Knudsen L, Cohen R, & Guralnik J (1987). Social network ties and mortality among the elderly in the Alameda County Study. American Journal of Epidemiology, 126, 714–723. [DOI] [PubMed] [Google Scholar]
- Seidlitz L, & Diener E (1993). Memory for positive versus negative life events: Theories for the differences between happy and unhappy persons. Journal ofPersonality and Social Psychology, 64, 654. [DOI] [PubMed] [Google Scholar]
- Shapiro AF, Gottman JM, & Carrere S (2000). The baby and the marriage: Identifying factors that buffer against decline in marital satisfaction after the first baby arrives. Journal ofFamily Psychology, 14, 11. [DOI] [PubMed] [Google Scholar]
- Spierings EL, Sorbi M, Haimowitz BR, & Tellegen B (1996). Changes in daily hassles, mood, and sleep in the 2 days before a migraine headache. The Clinical Journal of Pain, 12, 38–42. [DOI] [PubMed] [Google Scholar]
- Stueve C, & Gerson K (1977). Personal relations across the lifecycle In Fischer C (Ed.), Networks and places: Social relations in the urban setting (pp. 79–88). New York: Free Press. [Google Scholar]
- Tower RB, Kasl SV, & Darefsky AS (2002). Types of marital closeness and mortality risk in older couples. Psychosomatic Medicine, 64, 644–659. [DOI] [PubMed] [Google Scholar]
- Troxel WM (2010). It’s more than sex: Exploring the dyadic nature of sleep and implications for health. Psychosomatic Medicine, 72, 578–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Robles TF, Hall M, & Buysse DJ (2007). Marital quality and the marital bed: Examining the covariation between relationship quality and sleep. Sleep Medicine Reviews,11,389–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino BN (2006). Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine, 29, 377–387. 10.1007/s10865-006-9056-5 [DOI] [PubMed] [Google Scholar]
- Usala PD, & Hertzog C (1989). Measurement of affective states in adults: Evaluation of an adjective rating scale instrument. Research on Aging, 11, 403–426. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Guarnaccia CA, & Dohrenwend BP (1986). Measuring small life events. American Journal of Community Psychology, 14, 629–655. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, & Reich JW (1983). Life events and perceptions of life quality: Developments in a two-factor approach. Journal of Community Psychology, 11, 121–132. [Google Scholar]


