Abstract
Objective:
To propose a new set of Japanese diagnostic reference levels (DRLs) and achievable doses (ADs) for 2017 and to verify the usefulness of Japanese DRLs (DRLs 2015) for CT, by investigating changes in the volume CT dose index (CTDIvol) from 2014 to 2017.
Methods:
Detailed information on the CT scan parameters used throughout Japan were obtained by questionnaire survey. The CTDIvol and dose-length product for the 11 commonest adult and 6 commonest paediatric CT examinations were surveyed and compared with 2014 data and DRLs 2015.
Results:
Evaluations of adult head (helical), and abdomen and pelvis without contrast agent, paediatric chest without contrast agent, and abdomen and pelvis without contrast agent showed a slightly lower mean CTDIvol in 2017 than in 2014 (t-test, p < 0.05). The interquartile range of CTDIvol for all 2017 examinations was lower than in 2014.
Conclusions:
This study verified the lower mean, 75th percentile, and interquartile range by investigating changes in the CTDIvol from 2014 to 2017. The DRLs 2015 contributed to CT radiation dose reduction.
Advances in knowledge:
The widespread implementation of iterative reconstruction algorithms and low-tube voltage in CT scanners is likely to facilitate further reduction in the CT radiation dose used in Japan. Although radiological technologists may require further education on appropriate CTDIvol and DLP usage, the DRLs 2015 greatly contributed to the reduction of the CT radiation dose used in Japan.
Introduction
Recently, CT using multidetector technology has become an important diagnostic examination method, as it supplies rapid multiplanar submillimetre resolution images of the whole body. However, CT is known to be a significant contributor to the individual and population exposure dose.1
Since estimates of the cancer risk attributable to the use of diagnostic X-rays have been reported,2,3 radiological technologists should aim to optimize scan parameters in order to avoid excessive radiation exposure.4,5 In 1990, the International Commission on Radiological Protection (ICRP) recommended the use of diagnostic reference levels (DRLs) for patients.6 It is intended for use as a simple test to identify situations in which the patient dose levels are unusually high.7 The ICRP emphasized that DRLs “are not for regulatory or commercial purposes, not a dose constraint, and not linked to limits or constraints”.8 DRLs are typically set at the 75th percentile of the dose distribution from a survey conducted across a broad user-base using a specified dose-measurement protocol
In 2014, Matsunaga et al1,9 surveyed the 75th percentile of the volume CT dose index (CTDIvol) and the effective doses for head, chest, and abdominal non-contrast CT examinations of adults and 5-year-old children, based on a nationally distributed questionnaire in Japan.9 In 2015, the Japanese DRLs (hereafter called “DRLs 2015”) for CT were established by the Japan Network for Research and Information on Medical Exposures, by cooperation of the related academic societies,10 for the first time. After their publication, the related academic societies gave numerous promotional lecture presentations throughout Japan to popularize the use of DRLs 2015, explaining the need for and methods used to achieve dose optimization. However, there are several issues with DRLs 2015. First, the DRLs 2015 were published based only on the 75th percentile of CTDIvol and the dose–length product (DLP) in Japan. If the typical dose used at an institution exceeds the 75th percentile, it is possible to review it to determine whether the dose is optimal, unless there is a clinically reasonable cause. Because only the 75th percentile was published, concrete countermeasures for cases falling below the 75th percentile were not reported. Second, no more than six adult and three paediatric CT examinations are listed in the DRLs 2015, and the DRLs 2015 do not contain information about paediatric CT examinations employing contrast agent.
One powerful tool in further optimization involves publishing the achievable dose (AD). The AD is an optimization goal, based on survey data, and is typically defined as the median value (50th percentile) of the dose distribution of standard techniques and technologies that are widely used.
The aim of this study was to propose a new set of Japanese DRLs and ADs for 2017 and to verify the usefulness of the DRLs 2015 by investigating changes in the CTDIvol from 2014 to 2017.
Methods and materials
National questionnaire survey
A questionnaire was sent to 3000 facilities throughout Japan by post. The data from each facility were collected; these data were the actual CTDIvol and/or DLP values displayed on CT equipment at each examination. The distributed questionnaire contained detailed questions on the CT scan parameters employed, including the manufacturer, specific CT scanner model, tube voltage (kV), tube current (mA), rotation time, number of detector rows, beam width, pitch factor, reconstruction algorithm [iterative reconstruction (IR) or filtered back projection (FBP)], and the number of phases used. In cases of modulated tube current, the mean of the overall slices (mean tube current) was recorded. The results of this questionnaire survey were collected from June to December 2017. The questionnaire used sought to obtain data for scanning performed on standard patients (adults: 50–60 kg, 5-year-old children: 15–20 kg)11 to obtain a representation of typical practice with non-contrast and contrast CT; the questionnaire did not include data on specialised examinations. For adults and 5-year-old children, the examination data are summarised in Table 1. “Acute abdomen” was described to differentiate between typical contrast CT examinations and specialised multiphase contrast CT examinations, such as liver, pancreas, and urinary organs. In this study, the collected CTDIvol and DLP were based on calibration with a 32-cm-diameter phantom for adult body examinations and with a 16-cm-diameter phantom for head and paediatric examinations.
Table 1.
CT examinations selected for study in this survey
| Examinations | Contrast agent | Note | |
| Adults | Head | Without | Routinenon-helical & helical |
| With | CT angiography | ||
| Chest | Without | Routine | |
| With | Tumor | ||
| Abdomen and pelvis | Without | Routine | |
| With | Acute abdomen | ||
| Coronary | Without | Routine | |
| With | Routine | ||
| Chestand pelvis | Without | Routine | |
| Liver | Without & with | Multiphase | |
| Whole-body | Without | Trauma | |
| Children(5 years) | Head | Without | Routine Non-helical & helical |
| With | Tumour | ||
| Chest | Without | Routine | |
| With | Tumour | ||
| Abdomen and pelvis | Without | Routine | |
| With | Acute abdomen | ||
Analysis of collected data
The data from the CT evaluations, including the CTDIvol and/or DLP values displayed on CT equipment at each examination, were entered into an Excel spreadsheet (Microsoft Corp., Redmond, WA). The first quartile (25th percentile), median (50th percentile), and third quartile (75th percentile) of CTDIvol and DLP values for each examination were calculated directly from the total dose distribution.
The statistical significance of differences between the two groups (IR vs FBP, voltages <120 kV vs voltages ≥120 kV, 2014 vs 2017 survey) was evaluated using Student’s or Welch’s t-test, following the F-test, which was used in the analysis of variance. Statistical analyses were performed using Student’s t-test when the two groups had equal variances, whereas Welch’s t-test was used for unequal variances. A p-value of <0.05 was considered to be statistically significant.
The results of this survey were compared with both the results of the 2014 survey by Matsunaga et al9 and the DRLs 2015 by Japan Network for Research and Information on Medical Exposures.10
Results
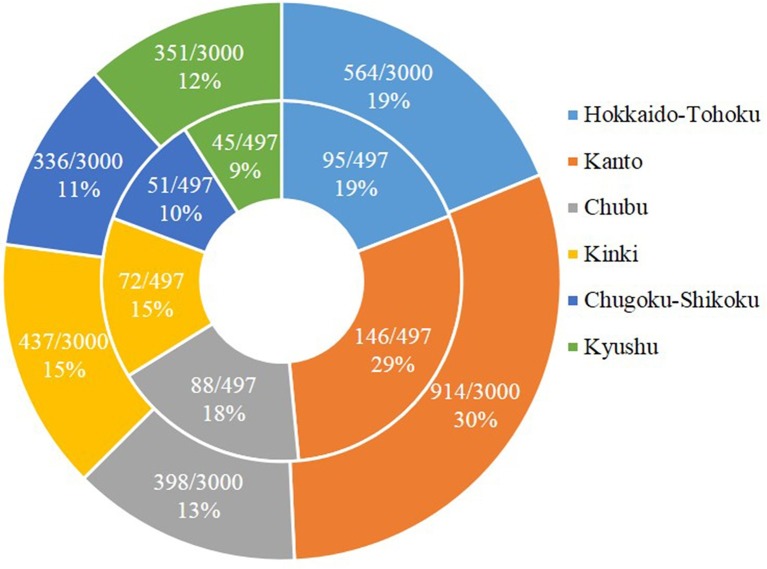
The questionnaire was sent to 3000 facilities, and responses were received from 497 (16.6%). Sufficient details on the CTDIvol and DLP were provided by 439 of the 497 facilities (Figure 1). The collected data for 4961 scanner protocols from 439 facilities were analysed in this study.
Figure 1.
The distribution of 3000 facilities in Japan, divided into six regions. The outside circle in Figure 1 indicates the distribution of the 3000 participating facilities distributed throughout Japan, while the inside circle indicates the distribution of responses received from 497 institutions. CTDIvol, volume CT dose index; DLP, dose–length product.
The distributions of CTDIvol and DLP for adults and 5-year-old children are summarized in Tables 2 and 3, respectively. The data are presented in terms of the number of data points, mean, coefficient of variation (CV), 25th percentile, AD (median), DRL (75th percentile), interquartile range (IQR; the difference between the 75th and 25th percentiles), and the ratio between the AD and DRL. The mean CTDIvol and DLP values for all examinations were higher than the medians.
Table 2.
Distributions of CTDIvol and DLP for adult CT examinations
| Examinations | n | Mean | CV (%) | 25th percentile | AD (Median) |
DRL (75th percentile) |
IQR | AD/DRL |
| Head without contrast agent | ||||||||
| CTDIvol (mGy) | 702 | 74.9 | 38.6 | 59.1 | 70.0 | 85.5 | 26.4 | 0.82 |
| DLP (mGy cm) | 706 | 1153.5 | 59.3 | 867.9 | 1097.0 | 1359.8 | 491.9 | 0.81 |
| Head (non-helical) without contrast agent | ||||||||
| CTDIvol (mGy) | 339 | 81.0 | 39.2 | 62.8 | 72.9 | 90.0 | 27.2 | 0.81 |
| DLP (mGy cm) | 341 | 1010.9 | 68.7 | 800.0 | 1001.7 | 1214.0 | 414.0 | 0.83 |
| Head (helical) without contrast agent | ||||||||
| CTDIvol (mGy) | 363 | 69.2 | 35.6 | 56.0 | 66.2 | 80.0 | 24.0 | 0.83 |
| DLP (mGy cm) | 365 | 1286.6 | 50.3 | 934.0 | 1235.0 | 1500.0 | 566.0 | 0.82 |
| Head CT angiography with contrast agent | ||||||||
| CTDIvol (mGy) | 301 | 92.8 | 155.7 | 35.0 | 52.3 | 73.5 | 38.5 | 0.71 |
| DLP (mGy cm) | 303 | 1027.0 | 72.1 | 584.4 | 858.0 | 1223.8 | 639.4 | 0.70 |
| Chest without contrast agent | ||||||||
| CTDIvol (mGy) | 452 | 12.0 | 76.5 | 7.7 | 10.0 | 14.3 | 6.6 | 0.70 |
| DLP (mGy cm) | 454 | 432.2 | 44.3 | 300.0 | 400.0 | 543.4 | 243.4 | 0.74 |
| Chest with contrast agent (tumour) | ||||||||
| CTDIvol (mGy) | 320 | 14.7 | 92.6 | 8.6 | 11.3 | 16.5 | 7.9 | 0.68 |
| DLP (mGy cm) | 322 | 597.4 | 70.1 | 355.3 | 476.1 | 652.7 | 297.4 | 0.73 |
| Abdomen and pelvis without contrast agent | ||||||||
| CTDIvol (mGy) | 431 | 15.1 | 48.6 | 10.0 | 13.7 | 18.2 | 8.2 | 0.75 |
| DLP (mGy cm) | 433 | 712.5 | 50.0 | 492.0 | 650.0 | 870.9 | 378.9 | 0.75 |
| Abdomen and pelvis with contrast agent (acute abdomen) | ||||||||
| CTDIvol (mGy) | 342 | 23.8 | 133.6 | 10.3 | 15.1 | 23.0 | 12.7 | 0.66 |
| DLP (mGy cm) | 345 | 1039.4 | 76.7 | 539.1 | 827.7 | 1253.3 | 714.2 | 0.66 |
| Coronary artery without contrast agent | ||||||||
| CTDIvol (mGy) | 210 | 10.2 | 153.8 | 3.2 | 5.5 | 9.8 | 6.6 | 0.56 |
| DLP (mGy cm) | 210 | 195.3 | 174.2 | 56.0 | 85.6 | 166.6 | 110.6 | 0.51 |
| Coronary artery with contrast agent | ||||||||
| CTDIvol (mGy) | 294 | 73.1 | 103.6 | 31.3 | 54.0 | 84.8 | 53.5 | 0.64 |
| DLP (mGy cm) | 294 | 945.7 | 72.0 | 450.5 | 823.1 | 1300.0 | 849.6 | 0.63 |
| Chest and pelvis without contrast agent | ||||||||
| CTDIvol (mGy) | 419 | 14.7 | 47.8 | 10.0 | 12.8 | 16.7 | 6.7 | 0.77 |
| DLP (mGy cm) | 421 | 953.4 | 38.9 | 700.0 | 882.0 | 1133.0 | 433.0 | 0.78 |
| Liver with non-contrast and contrast agent | ||||||||
| CTDIvol (mGy) | 351 | 46.6 | 177.2 | 11.4 | 17.4 | 44.9 | 33.4 | 0.39 |
| DLP (mGy cm) | 356 | 1605.1 | 252.2 | 487.4 | 1040.7 | 1795.2 | 1307.9 | 0.58 |
| Whole-body without contrast agent (trauma) | ||||||||
| CTDIvol (mGy) | 141 | 26.1 | 110.8 | 10.9 | 14.2 | 22.4 | 11.5 | 0.63 |
| DLP (mGy cm) | 142 | 1698.6 | 173.1 | 902.3 | 1147.0 | 1596.6 | 694.3 | 0.72 |
AD, achievable dose; CTDIvol, volume CT dose index; CV, coefficient of variation; DLP, dose–length product; DRL, diagnostic reference level; IQR, interquartile range;
n indicates the number of CTDIvol or DLP values.
Table 3.
Distributions of CTDIvol and DLP for 5-year-old child CT examinations (the weight range is restricted to 4–6 years11)
| Examinations | n | Mean | CV (%) | 25th percentile | AD (Median) |
DRL (75th percentile) |
IQR | AD/DRL |
| Head without contrast agent | ||||||||
| CTDIvol (mGy) | 333 | 41.5 | 56.0 | 30.0 | 38.1 | 47.6 | 17.6 | 0.80 |
| DLP (mGy cm) | 336 | 602.3 | 50.5 | 403.5 | 568.3 | 753.9 | 350.3 | 0.75 |
| Head (non-helical) without contrast agent | ||||||||
| CTDIvol (mGy) | 156 | 43.3 | 62.8 | 30.0 | 39.7 | 48.3 | 18.3 | 0.82 |
| DLP (mGy cm) | 158 | 506.2 | 53.9 | 357.0 | 486.7 | 649.8 | 292.8 | 0.75 |
| Head (helical) without contrast agent | ||||||||
| CTDIvol (mGy) | 177 | 39.9 | 47.7 | 30.0 | 37.9 | 46.7 | 16.7 | 0.81 |
| DLP (mGy cm) | 178 | 687.6 | 44.4 | 480.3 | 650.5 | 866.9 | 386.7 | 0.75 |
| Head with contrast agent (tumour) | ||||||||
| CTDIvol (mGy) | 98 | 42.1 | 61.4 | 28.9 | 37.1 | 47.3 | 18.3 | 0.78 |
| DLP (mGy cm) | 98 | 706.6 | 67.1 | 452.4 | 596.0 | 846.4 | 394.0 | 0.70 |
| Chest without contrast agent | ||||||||
| CTDIvol (mGy) | 145 | 7.2 | 116.0 | 3.2 | 5.0 | 8.5 | 5.3 | 0.59 |
| DLP (mGy cm) | 147 | 178.6 | 94.6 | 88.0 | 136.1 | 235.0 | 147.0 | 0.58 |
| Chest with contrast agent (tumour) | ||||||||
| CTDIvol (mGy) | 99 | 6.4 | 63.3 | 3.4 | 5.0 | 8.4 | 5.0 | 0.60 |
| DLP (mGy cm) | 99 | 175.8 | 70.8 | 97.6 | 144.6 | 232.3 | 134.7 | 0.62 |
| Abdomen and pelvis without contrast agent | ||||||||
| CTDIvol (mGy) | 150 | 8.6 | 101.8 | 3.4 | 5.8 | 11.2 | 7.8 | 0.52 |
| DLP (mGy cm) | 154 | 257.1 | 79.0 | 115.6 | 200.0 | 343.9 | 228.3 | 0.58 |
| Abdomen and pelvis with contrast agent (acute abdomen) | ||||||||
| CTDIvol (mGy) | 121 | 9.6 | 106.6 | 3.6 | 6.6 | 12.0 | 8.4 | 0.55 |
| DLP (mGy cm) | 121 | 340.9 | 100.3 | 129.7 | 250.0 | 410.4 | 280.7 | 0.61 |
AD, achievable dose; CV, coefficient of variation; CTDIvol, volume CT dose index; DLP, dose–length product; DRL, diagnostic reference level; IQR, interquartile range;
n indicates the number of CTDIvol or DLP values.
The median value (mean value) of the number of phases used for abdominal and pelvic CT with contrast agent (acute abdomen) and liver CT without and with contrast agent for adults were 2 (1.8) and 4 (3.6), respectively. The median number of phases used for liver CT with and without contrast agent (4) was the highest among contrast CT examinations. The median values of other contrast CT examinations for both adults and children were for a single phase.
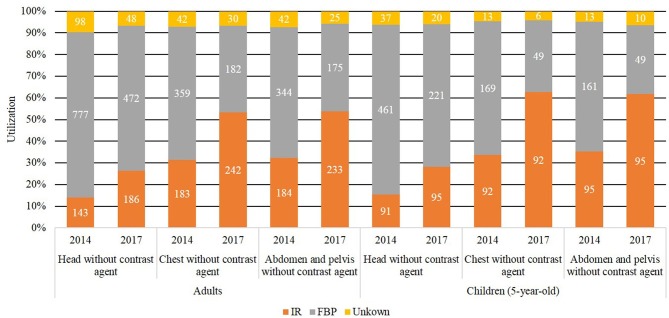
Figure 2 compares the utilization rate of the IR and FBP in this study with the results of the 2014 survey by Matsunaga et al.9 The rate of utilization of IR for each examination in adults and children in this study was increased as compared to the 2014 survey. Table 4 lists the mean CTDIvol and DLP for adult and paediatric examinations, classified in terms of the image analysis algorithm used: IR or FBP. For adult examinations using IR, both the mean CTDIvol and DLP values for chest evaluations without contrast agent, with contrast agent (tumour), abdomen and pelvis evaluations without contrast agent, coronary artery evaluations with contrast agent, and chest and pelvis evaluations without contrast agent examinations were significantly lower than those for adult examinations using FBP (t-test, p < 0.05, Table 4). For paediatric examinations using IR, both the mean CTDIvol and DLP values for evaluations of the head without contrast agent, head (helical) without contrast agent, and chest without contrast agent were significantly lower than those of paediatric examinations using FBP (t-test, p < 0.05, Table 4).
Figure 2.
Utilization rate of the IR. IR, iterative reconstruction.
Table 4.
Comparison of the distributions of CTDIvol and DLP using reconstruction algorithms
| CTDIvol (mGy) | DLP (mGy cm) | ||||||||||||
| n | Median | Mean | CV (%) |
Reduction Rate (%) |
p-value | n | Median | Mean | CV (%) |
Reduction Rate (%) |
p-value | ||
| Adults | Head without contrast agent | Head without contrast agent | |||||||||||
| IR | 186 | 63.6 | 65.0 | 33.9 | 17.2 | p < 0.05 | 186 | 1100.0 | 1137.7 | 54.4 | 3.5 | p = 0.45 | |
| FBP | 468 | 71.9 | 78.5 | 38.7 | 472 | 1105.4 | 1179.4 | 59.7 | |||||
| Head (non-helical) without contrast agent | Head (non-helical) without contrast agent | ||||||||||||
| IR | 77 | 67.7 | 69.2 | 37.7 | 17.7 | p < 0.05 | 77 | 1000.0 | 1009.8 | 33.6 | 2.5 | p = 0.68 | |
| FBP | 237 | 75.8 | 84.1 | 39.0 | 239 | 1016.0 | 1036.0 | 75.7 | |||||
| Head (helical) without contrast agent | Head (helical) without contrast agent | ||||||||||||
| IR | 109 | 61.2 | 62.0 | 29.2 | 14.8 | p < 0.05 | 109 | 1187.5 | 1228.0 | 60.7 | 7.4 | p = 0.22 | |
| FBP | 231 | 70.0 | 72.8 | 36.5 | 233 | 1292.5 | 1326.6 | 43.5 | |||||
| Head CT angiography with contrast agent | Head CT angiography with contrast agent | ||||||||||||
| IR | 154 | 45.7 | 95.3 | 159.1 | −3.0 | p = 0.87 | 156 | 744.3 | 967.1 | 68.1 | 13.0 | p = 0.11 | |
| FBP | 138 | 57.9 | 92.5 | 152.3 | 138 | 935.0 | 1111.0 | 74.9 | |||||
| Chest without contrast agent | Chest without contrast agent | ||||||||||||
| IR | 241 | 9.0 | 10.0 | 72.0 | 27.9 | p < 0.05 | 242 | 352.4 | 381.6 | 45.6 | 22.4 | p < 0.05 | |
| FBP | 181 | 12.5 | 13.8 | 56.8 | 182 | 485.0 | 491.6 | 39.8 | |||||
| Chest with contrast agent (tumour) | Chest with contrast agent (tumour) | ||||||||||||
| IR | 181 | 10.0 | 13.1 | 85.0 | 23.4 | p < 0.05 | 182 | 422.5 | 552.7 | 69.7 | 15.5 | p < 0.05 | |
| FBP | 125 | 13.9 | 17.1 | 99.1 | 126 | 559.6 | 653.8 | 71.8 | |||||
| Abdomen and pelvis without contrast agent | Abdomen and pelvis without contrast agent | ||||||||||||
| IR | 232 | 12.0 | 13.1 | 35.7 | 25.3 | p < 0.05 | 233 | 608.8 | 652.9 | 40.2 | 18.5 | p < 0.05 | |
| FBP | 174 | 15.0 | 17.6 | 53.0 | 175 | 700.0 | 801.2 | 55.8 | |||||
| Abdomen and pelvis with contrast agent (acute abdomen) | Abdomen and pelvis with contrast agent (acute abdomen) | ||||||||||||
| IR | 196 | 14.0 | 21.4 | 124.9 | 22.3 | p = 0.12 | 198 | 798.2 | 965.9 | 72.6 | 15.7 | p = 0.06 | |
| FBP | 131 | 16.9 | 27.5 | 142.6 | 132 | 865.6 | 1145.9 | 80.7 | |||||
| Coronary artery without contrast agent | Coronary artery without contrast agent | ||||||||||||
| IR | 124 | 6.0 | 10.2 | 163.2 | 4.6 | p = 0.83 | 124 | 88.7 | 189.7 | 171.8 | 12.3 | p = 0.60 | |
| FBP | 76 | 5.0 | 10.7 | 138.5 | 76 | 83.8 | 216.4 | 176.0 | |||||
| Coronary artery with contrast agent | Coronary artery with contrast agent | ||||||||||||
| IR | 187 | 50.4 | 61.9 | 100.8 | 33.6 | p < 0.05 | 187 | 685.0 | 787.4 | 69.1 | 35.7 | p < 0.05 | |
| FBP | 99 | 66.6 | 93.3 | 101.0 | 99 | 1050.0 | 1224.2 | 65.7 | |||||
| Chest and pelvis without contrast agent | Chest and pelvis without contrast agent | ||||||||||||
| IR | 232 | 11.7 | 12.8 | 46.3 | 24.6 | p < 0.05 | 233 | 835.5 | 884.7 | 37.5 | 15.9 | p < 0.05 | |
| FBP | 162 | 15.0 | 17.0 | 45.3 | 163 | 985.1 | 1052.2 | 37.3 | |||||
| Liver with non-contrast and contrast agent | Liver with non-contrast and contrast agent | ||||||||||||
| IR | 198 | 15.6 | 45.7 | 203.6 | 4.1 | p = 0.83 | 200 | 1057.5 | 1587.9 | 297.9 | 5.3 | p = 0.84 | |
| FBP | 138 | 19.9 | 47.6 | 144.6 | 141 | 974.9 | 1676.1 | 185.4 | |||||
| Whole-body without contrast agent (trauma) | Whole-body without contrast agent (trauma) | ||||||||||||
| IR | 81 | 12.8 | 22.2 | 103.1 | 24.0 | p = 0.15 | 82 | 1111.3 | 1439.7 | 70.8 | 27.6 | p = 0.40 | |
| FBP | 52 | 17.5 | 29.2 | 102.5 | 52 | 1275.0 | 1987.2 | 228.1 | |||||
| Children (5 years) | Head without contrast agent | Head without contrast agent | |||||||||||
| IR | 94 | 33.9 | 35.2 | 41.7 | 20.6 | p < 0.05 | 95 | 502.5 | 555.6 | 43.5 | 12.1 | p < 0.05 | |
| FBP | 219 | 40.6 | 44.3 | 59.4 | 221 | 599.0 | 632.0 | 51.3 | |||||
| Head (non-helical) without contrast agent | Head (non-helical) without contrast agent | ||||||||||||
| IR | 38 | 34.1 | 36.3 | 51.1 | 20.4 | p < 0.05 | 39 | 474.8 | 486.0 | 44.2 | 7.9 | p = 0.40 | |
| FBP | 109 | 41.1 | 45.6 | 65.8 | 110 | 499.3 | 527.4 | 53.9 | |||||
| Head (helical) without contrast agent | Head (helical) without contrast agent | ||||||||||||
| IR | 56 | 33.1 | 34.4 | 33.1 | 19.9 | p < 0.05 | 56 | 600.0 | 604.1 | 41.2 | 17.9 | p < 0.05 | |
| FBP | 110 | 40.0 | 42.9 | 51.4 | 111 | 680.0 | 735.6 | 44.8 | |||||
| Head with contrast material (tumour) | Head with contrast material (tumour) | ||||||||||||
| IR | 42 | 34.5 | 35.2 | 44.4 | 26.2 | p < 0.05 | 42 | 523.3 | 636.1 | 83.0 | 17.2 | p = 0.18 | |
| FBP | 55 | 41.9 | 47.7 | 64.1 | 55 | 655.8 | 767.9 | 55.4 | |||||
| Chest without contrast agent | Chest without contrast agent | ||||||||||||
| IR | 91 | 4.5 | 5.2 | 64.2 | 49.9 | p < 0.05 | 92 | 120.0 | 148.1 | 68.5 | 36.6 | p < 0.05 | |
| FBP | 48 | 7.0 | 10.4 | 123.5 | 49 | 169.0 | 233.4 | 105.6 | |||||
| Chest with contrast agent (tumour) | Chest with contrast agent (tumour) | ||||||||||||
| IR | 68 | 5.0 | 5.9 | 60.9 | 20.2 | p = 0.10 | 68 | 144.0 | 176.3 | 76.5 | 1.4 | p = 0.92 | |
| FBP | 29 | 5.5 | 7.5 | 65.2 | 29 | 148.0 | 178.7 | 56.9 | |||||
| Abdomen and pelvis without contrast agent | Abdomen and pelvis without contrast agent | ||||||||||||
| IR | 92 | 4.9 | 6.5 | 69.1 | 43.1 | p < 0.05 | 95 | 180.0 | 240.2 | 78.0 | 18.1 | p = 0.18 | |
| FBP | 48 | 8.0 | 11.5 | 114.5 | 49 | 200.0 | 293.3 | 82.6 | |||||
| Abdomen and pelvis with contrast agent (acute abdomen) | Abdomen and pelvis with contrast agent (acute abdomen) | ||||||||||||
| IR | 86 | 6.0 | 9.4 | 122.7 | −0.4 | p = 0.98 | 86 | 230.5 | 352.7 | 109.3 | −16.1 | p = 0.37 | |
| FBP | 32 | 7.6 | 9.4 | 62.4 | 32 | 280.0 | 303.9 | 65.2 | |||||
CTDIvol, volume CT dose index; DLP, dose–length product; CV, coefficient of variationIR, iterative reconstruction; FBP, filtered back projection;
n indicates the number of CTDIvol or DLP values.
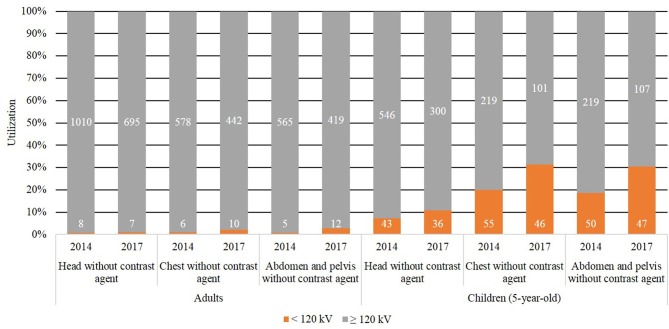
A tube voltage of 120 kV or more was used in the majority of facilities for all anatomical regions, including contrast agent examinations. However, voltages < 120 kV were used in a higher percentage of contrast agent examinations than non-contrast agent examinations; in particular, these voltages were used in a higher percentage of CT examinations of children than of adults. Figure 3 compares the utilization rate of tube voltages ≥ 120 kV and <120 kV in this study with the results of the 2014 survey by Matsunaga et al.9 The rate of utilization of voltages < 120 kV for each examination in adults and children in this study was increased as compared to the 2014 survey. The mean CTDIvol and DLP values for most CT examinations using voltages < 120 kV were significantly lower than those using ≥120 kV (t-test, p < 0.05, Table 5). In CT examinations using voltages < 120 kV, the utilization rate of IR was approximately 70%.
Figure 3.
Utilization rate of low-tube voltage CT.
Table 5.
Comparison of the distributions of CTDIvol and DLP classified in terms of tube voltage used
| CTDIvol (mGy) | DLP (mGy cm) | ||||||||||||
| n | Median | Mean | CV (%) |
Reduction rate (%) | p-value | n | Median | Mean | CV (%) |
Reduction rate (%) | p-value | ||
| Adults | Head without contrast agent | Head without contrast agent | |||||||||||
| kV <120 | 7 | 42.0 | 47.4 | 30.8 | 37.0 | p < 0.05 | 7 | 740.0 | 876.1 | 37.2 | 24.2 | p = 0.28 | |
| kV ≥120 | 691 | 70.1 | 75.2 | 38.4 | 695 | 1100.0 | 1155.1 | 59.4 | |||||
| Head CT angiography with contrast agent | Head CT angiography with contrast agent | ||||||||||||
| kV <120 | 41 | 32.0 | 46.0 | 99.3 | 55.1 | p < 0.05 | 42 | 547.3 | 658.8 | 67.2 | 40.2 | p < 0.05 | |
| kV ≥120 | 251 | 54.0 | 102.5 | 149.5 | 252 | 889.5 | 1101.0 | 69.2 | |||||
| Chest without contrast agent | Chest without contrast agent | ||||||||||||
| kV <120 | 10 | 8.9 | 8.5 | 32.3 | 29.1 | p < 0.05 | 10 | 325.0 | 340.1 | 37.6 | 21.6 | p = 0.12 | |
| kV ≥120 | 440 | 10.1 | 12.0 | 76.6 | 442 | 400.0 | 434.0 | 44.3 | |||||
| Chest with contrast agent (tumour) | Chest with contrast agent (tumour) | ||||||||||||
| kV <120 | 20 | 9.3 | 19.2 | 138.7 | −32.4 | p = 0.45 | 20 | 405.7 | 568.0 | 93.5 | 5.6 | p = 0.73 | |
| kV ≥120 | 296 | 11.5 | 14.5 | 85.2 | 298 | 478.3 | 601.8 | 68.3 | |||||
| Abdomen and pelvis without contrast agent | Abdomen and pelvis without contrast agent | ||||||||||||
| kV <120 | 12 | 9.0 | 9.6 | 38.7 | 36.8 | p < 0.05 | 12 | 445.0 | 497.8 | 35.8 | 30.8 | p < 0.05 | |
| kV ≥120 | 417 | 13.9 | 15.3 | 48.1 | 419 | 652.3 | 719.1 | 49.8 | |||||
| Abdomen and pelvis with contrast agent (acute abdomen) | Abdomen and pelvis with contrast agent (acute abdomen) | ||||||||||||
| kV <120 | 19 | 9.9 | 11.2 | 49.5 | 54.2 | p < 0.05 | 19 | 450.0 | 554.4 | 69.1 | 48.2 | p < 0.05 | |
| kV ≥120 | 322 | 15.6 | 24.5 | 132.7 | 325 | 850.9 | 1070.9 | 75.3 | |||||
| Coronary artery without contrast agent | Coronary artery without contrast agent | ||||||||||||
| kV <120 | 7 | 5.2 | 9.1 | 89.8 | 11.5 | p = 0.85 | 7 | 62.8 | 219.2 | 144.4 | −12.3 | p = 0.86 | |
| kV ≥120 | 202 | 5.6 | 10.2 | 154.5 | 202 | 88.0 | 195.3 | 175.0 | |||||
| Coronary artery with contrast agent | Coronary artery with contrast agent | ||||||||||||
| kV <120 | 35 | 34.0 | 36.2 | 74.1 | 53.8 | p < 0.05 | 35 | 492.0 | 516.0 | 77.6 | 49.0 | p < 0.05 | |
| kV ≥120 | 256 | 57.4 | 78.3 | 100.6 | 256 | 921.9 | 1011.8 | 68.3 | |||||
| Chest and pelvis without contrast agent | Chest and pelvis without contrast agent | ||||||||||||
| kV <120 | 10 | 10.5 | 10.4 | 17.1 | 29.4 | p < 0.05 | 10 | 781.4 | 761.8 | 24.9 | 20.5 | p < 0.05 | |
| kV ≥120 | 407 | 13.0 | 14.8 | 47.8 | 409 | 884.0 | 958.6 | 38.9 | |||||
| Liver with non-contrast and contrast agent | Liver with non-contrast and contrast agent | ||||||||||||
| kV <120 | 16 | 10.7 | 19.4 | 85.6 | 59.7 | p < 0.05 | 16 | 459.0 | 736.8 | 73.6 | 55.4 | p < 0.05 | |
| kV ≥120 | 330 | 17.7 | 48.0 | 175.2 | 335 | 1054.9 | 1653.6 | 250.2 | |||||
| Whole-body without contrast agent (trauma) | Whole-body without contrast agent (trauma) | ||||||||||||
| kV <120 | 5 | 11.6 | 12.2 | 27.6 | 54.1 | p < 0.05 | 5 | 1000.0 | 952.4 | 27.1 | 44.8 | p < 0.05 | |
| kV ≥120 | 136 | 14.5 | 26.6 | 110.2 | 137 | 1162.0 | 1725.8 | 173.2 | |||||
| Children (5 years) | Head without contrast agent | Head without contrast agent | |||||||||||
| kV <120 | 35 | 29.8 | 29.8 | 40.3 | 30.4 | p < 0.05 | 36 | 476.5 | 466.0 | 38.0 | 24.7 | p < 0.05 | |
| kV ≥120 | 298 | 39.3 | 42.9 | 55.6 | 300 | 596.6 | 618.6 | 50.4 | |||||
| Head (non-helical) without contrast agent | Head (non-helical) without contrast agent | ||||||||||||
| kV <120 | 14 | 25.0 | 28.2 | 54.6 | 37.2 | p < 0.05 | 14 | 435.0 | 405.8 | 47.6 | 21.5 | p = 0.14 | |
| kV ≥120 | 142 | 40.6 | 44.8 | 61.6 | 142 | 490.0 | 516.7 | 53.9 | |||||
| Head (helical) without contrast agent | Head (helical) without contrast agent | ||||||||||||
| kV <120 | 21 | 30.5 | 30.9 | 28.4 | 24.7 | p < 0.05 | 21 | 550.0 | 509.1 | 30.5 | 28.5 | p < 0.05 | |
| kV ≥120 | 156 | 38.3 | 41.1 | 48.0 | 157 | 663.8 | 711.5 | 44.0 | |||||
| Head with contrast material (tumour) | Head with contrast material (tumour) | ||||||||||||
| kV <120 | 12 | 30.9 | 31.9 | 22.9 | 26.8 | p < 0.05 | 12 | 524.5 | 555.0 | 54.9 | 23.7 | p = 0.24 | |
| kV ≥120 | 86 | 37.8 | 43.5 | 62.4 | 86 | 610.6 | 727.8 | 67.4 | |||||
| Chest without contrast agent | Chest without contrast agent | ||||||||||||
| kV <120 | 46 | 3.5 | 5.9 | 213.9 | 24.4 | p = 0.33 | 46 | 99.6 | 140.1 | 147.3 | 28.6 | p = 0.10 | |
| kV ≥120 | 99 | 5.7 | 7.8 | 69.2 | 101 | 160.0 | 196.2 | 74.8 | |||||
| Chest with contrast agent (tumour) | Chest with contrast agent (tumour) | ||||||||||||
| kV <120 | 32 | 3.6 | 5.0 | 68.6 | 29.0 | p < 0.05 | 32 | 114.6 | 132.1 | 60.8 | 33.3 | p < 0.05 | |
| kV ≥120 | 66 | 6.0 | 7.1 | 58.9 | 66 | 157.9 | 198.0 | 68.9 | |||||
| Abdomen and pelvis without contrast agent | Abdomen and pelvis without contrast agent | ||||||||||||
| kV <120 | 47 | 4.6 | 7.3 | 172.3 | 21.1 | p = 0.32 | 47 | 139.4 | 211.3 | 103.6 | 23.8 | p = 0.06 | |
| kV ≥120 | 103 | 7.0 | 9.2 | 70.2 | 107 | 240.0 | 277.3 | 69.8 | |||||
| Abdomen and pelvis with contrast agent (acute abdomen) | Abdomen and pelvis with contrast agent (acute abdomen) | ||||||||||||
| kV <120 | 43 | 4.0 | 6.2 | 96.7 | 46.3 | p < 0.05 | 43 | 151.8 | 215.6 | 75.2 | 47.8 | p < 0.05 | |
| kV ≥120 | 77 | 9.2 | 11.6 | 99.9 | 77 | 300.5 | 413.2 | 95.0 | |||||
CTDIvol, volume CT dose index; DLP, dose–length product;
n indicates the number of CTDIvol or DLP values.
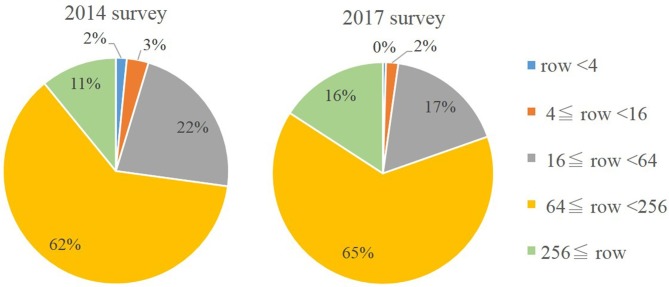
Multidetector row CT (MDCT) with 64 or more, but fewer than 256 rows, was most frequently used (65% of facilities), while MDCT with 16 or more, but fewer than 64 rows, or with 256 rows and more, were the second and third most frequently used, respectively. Figure 4 compares the number of detector rows in this study with the results of the 2014 survey by Matsunaga et al.9 The number of detector rows in this study were similar to the results of the 2014 survey. However, the use of MDCT with fewer than 16 rows was slightly decreased and the use of MDCT with 256 rows or more were slightly increased as compared to the 2014 survey.
Figure 4.
Distribution of CT scanners according to the number of detector rows. DRL, diagnostic reference level.
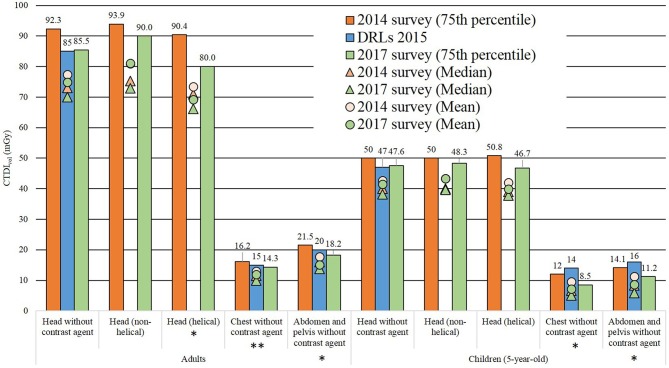
The changes in the mean CTDIvol values for each examination from 2014 to 2017 are given in Figure 5. For all examinations in 2017, the median and 75th percentile values were lower than or nearly identical to those published in 20149 and the DRLs 2015.10 The evaluations of adult head (helical), abdomen and pelvis without contrast agent, paediatric chest without contrast agent, and abdomen and pelvis without contrast agent showed a slightly lower mean CTDIvol in 2017 than in 2014 (t-test, p < 0.05).
Figure 5.
The CTDIvol obtained in this study for each examination compared with the CTDIvol values reported in 2014 survey and DRLs 2015. The DRLs 2015 are the Japanese DRLs for CT established by J-RIME in 2015.10 * t-test, p < 0.05. ** t-test, p = 0.05. CTDIvol, volume CT dose index; DRL, diagnostic reference level; IR, iterative reconstruction; J-RIME, Japan Network for Research and Information on Medical Exposures.
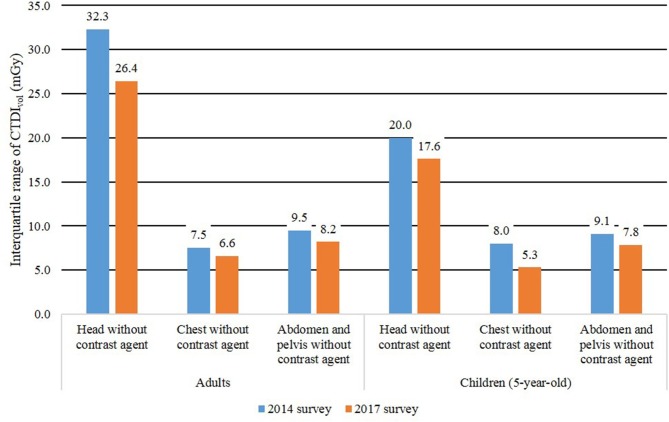
Figure 6 compares the IQR of the CTDIvol for each examination in this study with the results of the 2014 survey by Matsunaga et al.9 The IQR of CTDIvol for each examination in 2017 were lower than those in 2014.
Figure 6.
The interquartile range of CTDIvol for each examination compared with the 2014 survey. CTDIvol, volume CT dose index.
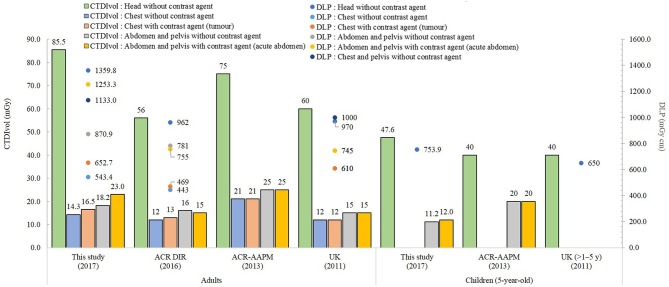
Figure 7 compares the DRL of the CTDIvol and DLP in this study, with the DRL taken from surveys conducted in other countries.12–14 The DRL for adult and paediatric head CT examinations in Japan were higher than the values of similar published studies originating from other countries.12–14
Figure 7.
Domestic and international diagnostic reference levels comparisons.12–14 This study was based on standard-sized (50–60 kg) patients. The ACR DIR13 are based on the size bin containing median-sized patients. (head: median lateral thickness was 15 cm; other: the water-equivalent diameter median diameter was 31 cm) American College of Radiology-the American Association of Physicists in Medicine (AAPM)14: patient lateral dimensions are for average patients of the specified age. UK12: no condition specified patient size. AAPM, AmericanAssociation of Physicists in Medicine; ACR, American College of Radiology; DIR, dose index registry.
Discussion
The ratio of DRLs and ADs in the CTDIvol for examinations of adults and 5-year-old children were identical to those of the DLPs for most examinations. However, the ratio of DRLs and ADs in the CTDIvol for liver examinations with and without contrast agent was too low when comparing the DLP. It is possible that the lack of knowledge among radiological technologists about the CTDIvol may underlie this decision. The actual DRL in the CTDIvol for liver evaluations with and without contrast agent would be lower. On the other hand, the DLP is a parameter involving the dose and scan length. The DRL in the DLP may be correctly reflected, since DLPs are not related to the number of phases.
The IQR for the CTDIvol and DLP for coronary artery examinations with contrast agent was higher than these values for other examinations. There were statistically significant differences in both the mean CTDIvol and DLP values for coronary artery evaluations with contrast agent between facilities employing IR or employing FBP algorithms (Table 4). Moreover, the dose gaps may have widened according to the scan method used in the different facilities. Prospective ECG gating allows the X-ray beams to be turned on during preselected phases in the cardiac cycles, and has been shown by various studies to reduce the radiation dose by 52 to 85%,15 while maintaining equivalent diagnostic accuracy, as compared with retrospective scanning. In the next survey of the CTDIvol and DLP values for coronary artery evaluations, with contrast agent, the scan method needs to evaluate prospective and retrospective ECG scanning separately.
Compared to the rates of reduction of CTDIvol when using the IR algorithm in adults in 2014 (12–28%), those in 2017 were high or nearly identical (14.1–27.9%). The adult CTDIvol and CVs when using the IR algorithm in 2017 were lower than or identical to those used in 2014, except for the CVs of chest evaluations. In 2014, Matsunaga et al9 reported that there were no statistically significant differences when using IR or FBP for any of the paediatric CT examinations, except for those involving the abdomen. However, the paediatric CTDIvol and CVs when using the IR algorithm in 2017 were markedly lower than those in 2014, except for the CVs of head (non-helical) examinations. Many facilities using the IR algorithm may reduce the diagnostic radiation dose in particular paediatric examinations. In recent years, the utilization rate of IR algorithms has been gradually increasing (Figure 2) and when these algorithms are widely employed in CT equipment, the diagnostic radiation dose could be further reduced.
Tube voltages < 120 kV were frequently used for paediatric CT examinations, including head examinations, in 2017. Moreover, the tube voltages < 120 kV were more frequently used to scan adults with or without contrast agent, perhaps because low-tube voltage CT came into widespread use for improving image quality. Furthermore, the implementation of the IR algorithm contributed to the spread of the low-tube voltage CT. In CT examinations using voltages < 120 kV, the utilization rate of IR was approximately 70%. Low-tube voltage results in higher X-ray absorbance by the body than high-tube voltage; low-tube voltage may thus not be suitable for patients with high body mass indices, because of increased image noise.16,17 Therefore, the combination of low-tube voltage and IR algorithm is widely used in CT equipment. Moreover, although the number of adult head CT examinations without contrast media using voltages < 120 kV was small, low-tube voltage CT was effective for reducing the CTDIvol and DLP in both adult and child evaluations. However, low-tube voltage CT is not necessarily better than tube voltages ≥ 120 kV. Because low-tube voltage CT may suffer from severe streak artifacts caused by metallic surgical materials or enhanced calcium artifacts,18 the radiological technologist should not select low-tube voltage without careful consideration. Attention should be given to reducing the radiation dose while obtaining image quality that is adequate for diagnosis.
In 2014, further optimization of CT examination protocols was required for adult head and abdominal examinations, as well as for paediatric chest and abdominal examinations.9 In terms of the CTDIvol values for adult and paediatric chest as well as abdominal and pelvic examinations, and the IQR of CTDIvol for each examination in 2017, many facilities had reduced their CT radiation doses after publication of the DRLs 2015. The data collected in this study differed from those obtained by surveys conducted in other countries12–14 in terms of population size, scanner types, examination techniques, and patients' weights. In terms of adult head examinations in Japan, many facilities are thought to use a protocol that evaluates early ischemic change, in a routine manner. The CT dose in the protocol for diagnosing acute phase cerebral infarction is higher than that for detecting cerebral haemorrhage. Although the weight of patients in our study was substantially lower than that in other studies, the DRL quantities were significantly higher in this study. This is likely due to a lack of dose optimization, rather than differences in examination techniques, as compared with other countries. With the aim of dose optimization, both ADs and DRLs are provided to encourage facilities to optimize the dose to a lower level than that indicated by the ADs and DRLs. However, the patient dose must not be reduced to such an extent that the images become non-diagnostic.13 When the facility's median DRL value is lower than the AD, the image quality might be affected adversely. Image quality should be considered as a greater priority when additional optimisation efforts are being considered.7
Although radiological technologists may require further education on appropriate CTDIvol and DLP usage, the DRLs 2015 greatly contributed to the reduction in the CT radiation dose used in Japan.
The collected data also included data obtained using automatic tube current modulation. The International Electrotechnical Commission (IEC) has defined CTDIvol for a tube current-modulated examination (in the standard 60601-2-44 Amd.1 edition 3 of the IEC19 ) as the CTDIvol based on a single average tube current value of the entire scan. However, some CT scanners used in Japan indicate the maximum CTDIvol value of the entire scan, because the IEC did not define CTDIvol for a tube current modulated examination until edition 2.1. Thus, it is possible that the CTDIvol values prior to edition 2.1 of the IEC standards were overestimated. DLP does not vary due to differences in the edition of the IEC standards.
Conclusion
In this report, a new set of Japanese DRLs and ADs for the 11 commonest adult and 6 commonest paediatric CT examinations were proposed, based on the results of a national questionnaire survey. This study verified the lower mean, 75th percentile, and IQR by investigating changes in the CTDIvol from 2014 to 2017. The DRLs 2015 contributed to CT radiation dose reduction. The widespread implementation of IR algorithms and low-tube voltage in CT scanners is likely to facilitate further reduction in the radiation dose used in CT in Japan.
Footnotes
Competing interests: The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Contributor Information
Yuta Matsunaga, Email: frankie217612@gmail.com.
Koichi Chida, Email: chida@med.tohoku.ac.jp.
Yuya Kondo, Email: 82017304@fujita-hu.ac.jp.
Kenichi Kobayashi, Email: k-koba@fujita-hu.ac.jp.
Masanao Kobayashi, Email: masa1121@fujita-hu.ac.jp.
Kazuyuki Minami, Email: kminami@fujita-hu.ac.jp.
Shoichi Suzuki, Email: ssuzuki@fujita-hu.ac.jp.
Yasuki Asada, Email: asada@fujita-hu.ac.jp.
REFERENCES
- 1.Matsunaga Y, Kawaguchi A, Kobayashi K, Kobayashi M, Asada Y, Minami K, et al. Effective radiation doses of CT examinations in Japan: a nationwide questionnaire-based study. Br J Radiol 2016; 89: 20150671. doi: 10.1259/bjr.20150671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berrington de González A, Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet 2004; 363: 345–51. doi: 10.1016/S0140-6736(04)15433-0 [DOI] [PubMed] [Google Scholar]
- 3.Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012; 380: 499–505. doi: 10.1016/S0140-6736(12)60815-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chida K, Ohno T, Kakizaki S, Takegawa M, Yuuki H, Nakada M, et al. Radiation dose to the pediatric cardiac catheterization and intervention patient. AJR Am J Roentgenol 2010; 195: 1175–9. doi: 10.2214/AJR.10.4466 [DOI] [PubMed] [Google Scholar]
- 5. The international commission on radiological protection. The 2007 recommendations of the international commission on radiological protection. ICRP publication 2007; 103: 1–321. [DOI] [PubMed] [Google Scholar]
- 6.The International Commission on Radiological Protection 1990 Recommendations of the international commission on radiological protection. ICRP publication 1991; 60: 1–201. [PubMed] [Google Scholar]
- 7. The international commission on radiological protection. Diagnostic reference levels in medical imaging. ICRP publication 2017; 135: 1–144. [DOI] [PubMed] [Google Scholar]
- 8.Ann ICRP The international commission on radiological protection. diagnostic reference levels in medical imaging: Review and additional advice. ICRP publication 2001; 31: 33–52. [PubMed] [Google Scholar]
- 9.Matsunaga Y, Kawaguchi A, Kobayashi K, Kinomura Y, Kobayashi M, Asada Y, et al. Survey of volume CT dose index in Japan in 2014. Br J Radiol 2015; 88: 20150219. doi: 10.1259/bjr.20150219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Japan Network for Research and Information on Medical Exposures Diagnostic reference levels based on latest surveys in Japan — Japan DRLs 2015; 2015. [Google Scholar]
- 11.Portal Site of Official Statistics of Japan (Internet home page). 2018. Available from: https://www.e-stat.go.jp/SG1/estat/eStatTopPortalE.do.
- 12.Shrimpton PC, Hillier MC, Meeson S, Golding SJ. Doses from computed tomography (CT) examinations in the UK – 2011 review about public health England. Public Heal Engl 2014: 1–123. [Google Scholar]
- 13.Kanal KM, Butler PF, Sengupta D, Bhargavan-Chatfield M, Coombs LP, Morin RL. U.S. diagnostic reference levels and achievable doses for 10 adult CT examinations. Radiology 2017; 284: 120–33. doi: 10.1148/radiol.2017161911 [DOI] [PubMed] [Google Scholar]
- 14.ACR–AAPM ACR-AAPM practice parameter for diagnostic reference levels and achievable doses in medical x-ray imaging. ACR 2013: 1–9. [Google Scholar]
- 15.Hsiao EM, Rybicki FJ, Steigner M. CT coronary angiography: 256-slice and 320-detector row scanners. Curr Cardiol Rep 2010; 12: 68–75. doi: 10.1007/s11886-009-0075-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feuchtner GM, Jodocy D, Klauser A, Haberfellner B, Aglan I, Spoeck A, et al. Radiation dose reduction by using 100-kV tube voltage in cardiac 64-slice computed tomography: a comparative study. Eur J Radiol 2010; 75: e51–e56. doi: 10.1016/j.ejrad.2009.07.012 [DOI] [PubMed] [Google Scholar]
- 17.Berlin SC, Weinert DM, Vasavada PS, Martinez-Rios C, Parikh RA, Wien MA, et al. Successful dose reduction using reduced tube voltage with hybrid iterative reconstruction in pediatric abdominal CT. AJR Am J Roentgenol 2015; 205: 392–9. doi: 10.2214/AJR.14.12698 [DOI] [PubMed] [Google Scholar]
- 18.Horiguchi J, Fujioka C, Kiguchi M, Yamamoto H, Kitagawa T, Kohno S, et al. Prospective ECG-triggered axial CT at 140-kV tube voltage improves coronary in-stent restenosis visibility at a lower radiation dose compared with conventional retrospective ECG-gated helical CT. Eur Radiol 2009; 19: 2363–72. doi: 10.1007/s00330-009-1419-1 [DOI] [PubMed] [Google Scholar]
- 19.International Electrotechnical Commission Commission. Medical electrical equipment, part 2-20 44: Particular requirements for the safety of x-ray equipment for computed21 tomography. IEC Publication No. 60601-2-44 Amd 3(3 ed). [Google Scholar]